- 1Centre for Health Management and Policy Research, School of Public Health, Cheeloo College of Medicine, Shandong University, Jinan, China
- 2National Health Committee (NHC) Key Lab of Health Economics and Policy Research, Shandong University, Jinan, China
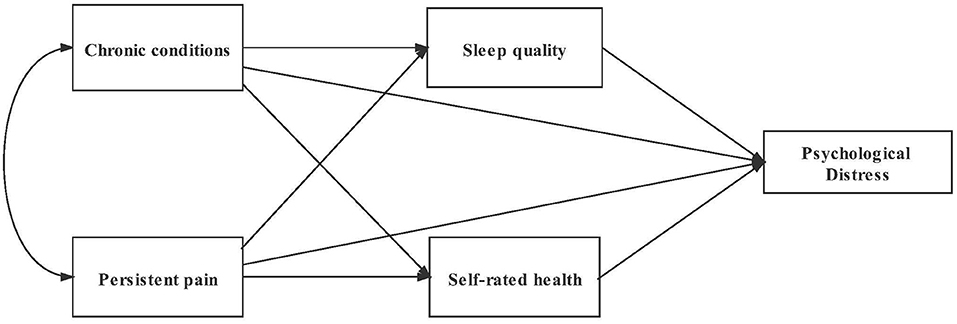
Psychological distress were found to be associated with chronic conditions and persistent pain. However, few studies explored the underlying pathways between them. This study aimed to analyze the path of chronic conditions and persistent pain on psychological distress through sleep quality and self-rated health. A total of 2,748 rural older people in Shandong, China were included in this study. Path analysis was performed by using Mplus 8.3 to examine the associations between chronic conditions, persistent pain, sleep quality, self-rated health, and psychological distress after adjusting for age, gender, education, and household income. The prevalence of psychological distress among the older adults in this study was 47.49%. Chronic conditions and persistent pain were indirectly associated with psychological distress through six mediating pathways: (1) the path from chronic conditions to psychological distress through sleep quality (β = 0.041, 95%CI: 0.015–0.067) and self-rated health (β = 0.064, 95%CI: 0.038–0.091), respectively, and a chain mediation existed (β = 0.007, 95% CI: 0.000–0.014); (2) the path of persistent pain and psychological distress through sleep quality (β = 0.058, 95% CI: 0.014–0.102) and self-rated health (β = 0.048, 95% CI: 0.000–0.096), respectively, also the chain mediation found (β = 0.009, 95% CI: 0.005–0.014). Psychological distress was associated with chronic conditions and persistent pain through decreased sleep quality and self-rated health among Chinese rural older people. Multi-pronged targeted intervention should be taken for older adults with chronic conditions and persistent pain.
Introduction
Population aging is accelerating worldwide, especially in China, where the total older population will exceed 400 million and the proportion of older adults will exceed 30% by 2050 (1). Meanwhile, there were more than one-third of the Chinese older population had a high risk of severe psychological distress (PD) symptoms (2). PD is defined as a state of emotional distress, characterized by depression, and anxiety symptoms. It is widely employed to reflect the mental health of people (3). Previous studies found that rural older adults had worse mental health than those in urban areas (4, 5). There were 38.8% of Chinese rural seniors had a high degree of PD, which was higher than the rate of urban older adults (22.2%) (2). Previous studies demonstrated that PD was associated with a high risk of suicide ideas, plans, and behaviors, especially among the older population (6–8). PD was also related to all-cause mortality (9). Exploring risk factors and their pathways to PD is critical to improving mental health, preventing adverse health outcomes, and reducing mortality.
Among the risk factors of PD, chronic conditions, and persistent pain were common among the older population (2, 10–12). The status that one person with two or more chronic conditions was defined as multimorbidity (13, 14), which was found to be a risk factor of PD among older adults. According to previous studies, multimorbid older adults had higher PD levels compared to those without multimorbidity (11, 15). Persistent pain is another important risk factor for mental health among older adults (16). Previous studies found that there was a higher risk of PD for older people with persistent pain (10, 17, 18). Additionally, chronic conditions and persistent pain often coexisted among numerous older people. Persistent pain was frequently interwoven with other physical or mental health problems (19, 20). The relationship between chronic conditions and PD, persistent pain and PD, have been demonstrated, respectively, in previous studies. But the potential associations are still unclear, and the association with PD when chronic conditions and persistent pain coexist has not been explored.
Psychological distress theory has been proposed by many scholars (21–23). It could be concluded that stressors (e.g., physical disorders or life events) stimulate the body through mediating mechanisms (e.g., stress perceiving and cognitive evaluation), and result in mental health problems [e.g., psychological distress; (22)]. According to this theory, chronic stress such as chronic conditions and persistent pain could be regarded as stressors (24). They were also found to be related to decreased sleep quality and worse self-rated health (25–28). It is considerable that sleep quality and self-rated health might play mediating roles in the associations between stressors and PD (22). Poor self-rated health was found to be associated with higher odds of PD among older adults (25, 29). Several studies had revealed that the number of chronic conditions had a strong association with self-rated health among older people (26, 30). Furthermore, a study conducted among older Chinese and older Korean Americans indicated that self-rated health played a mediating role between chronic conditions and depressive symptoms in both groups (31). Thus, self-rated health might be a mediator in the relationship between chronic conditions and PD in this study. Also, persistent pain was another risk factor related to poor self-rated health according to previous studies (26, 27, 32–34). As such, self-rated health might be one mediator for persistent pain and PD.
Sleep quality could be another mediator on the basis of psychological distress theory (22). There were significant correlations between mental disorders and sleep problems among older adults (28, 35, 36). As for chronic conditions, high prevalence of chronic diseases has been found to be associated with poor sleep quality (37, 38). Therefore, sleep quality may play a mediating role in the relationship between chronic conditions and PD. Further, previous research has indicated that persistent pain may result in sleep disturbance among older people (27, 39). It has been found that pain intensity was associated with sleep-related issues (40). The relationship between pain catastrophizing and depression among older Korean adults had been explored, and sleep quality was one of the mediators (41). Consequently, sleep quality could be one mediator for the relationship between persistent pain and PD.
Based on the psychological distress theoretical framework and previous evidence, we make the following hypotheses: chronic conditions and persistent pain were regarded as the stressors; sleep quality and self-rated health were treated as mediating factors, and the psychological response was the appearance of PD. The hypothesized model of this study included six pathways (Figure 1). The mediating effects of sleep quality and self-rated health would be examined. In addition, some researches had shown that sleep quality was associated with self-rated health among people over 18 years old (42, 43). We would include the relationship in our analysis, to confirm whether the chain mediating effects exist.
Materials and Methods
Study Design and Sample
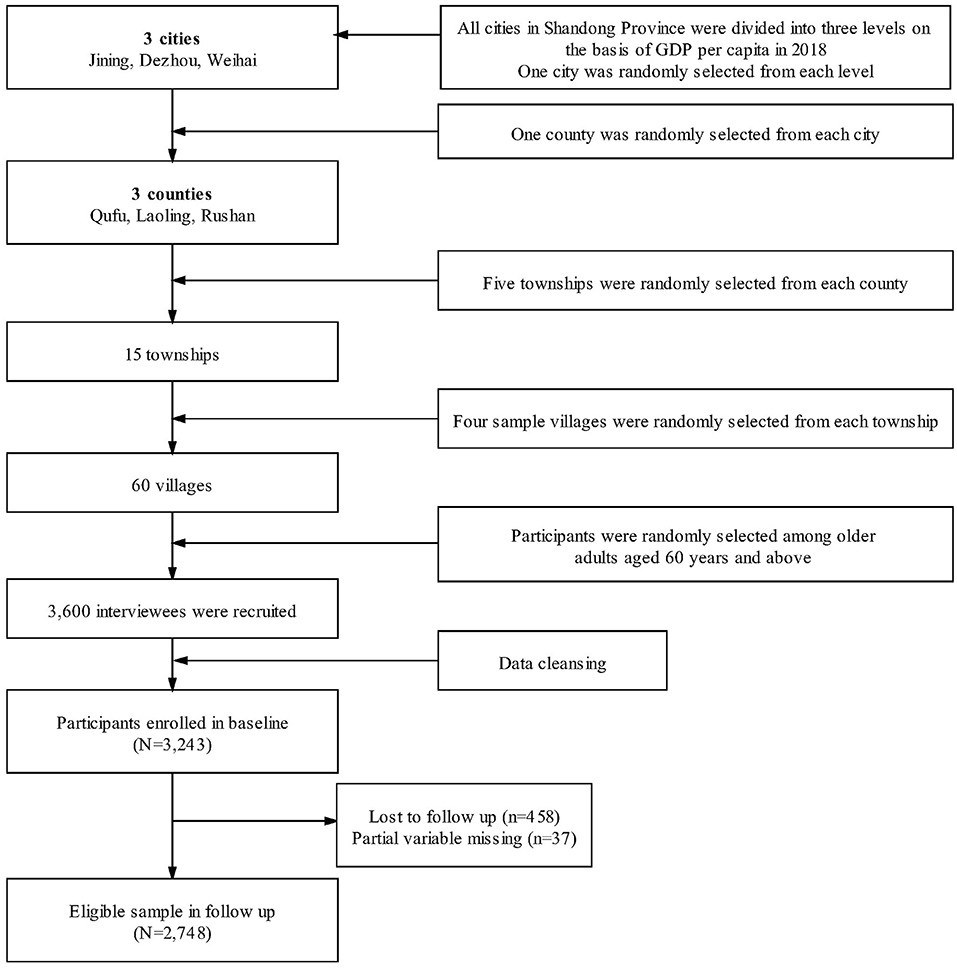
This study was based on the Shandong Rural Elderly Health Cohort (SREHC), an ongoing longitudinal study conducted in the second-most populous province in China. SREHC takes the population of 60 years old and above in rural Shandong as the research subjects, aims to investigate seniors' health status, and deal with the problem of population aging. The baseline survey was conducted from May to June in 2019, and the follow-up survey was conducted from August to September in 2020. In this study, we used the follow-up data.
A three-stage stratified random sampling method was employed to select participants at baseline (Figure 2). Firstly, all counties of Shandong province were divided into three groups on the basis of GDP per capita (2018). Secondly, one county was selected randomly from each group. Three counties (Rushan, Qufu, Laoling, respectively, represented high, medium, and low level county) were chosen as the study sites. After that, five townships were randomly selected from each sampled county. Thirdly, four villages were chosen randomly from each township. Older adults aged 60 years and above were investigated in each sample village. In total, 3,600 individuals were recruited and 3,243 completed the whole survey, with a response rate of 90.05% (44). Among the 3,243 respondents in the baseline survey, 2,785 participated in the follow-up survey in 2020 (45). After excluding 37 respondents whose core variables were missing, we finally included 2,748 respondents in this study. Of all basic characteristics and core variables, there was no significant difference between the respondents included in this study and those not.
We collected information through a structured questionnaire. A face-to-face survey was conducted by well-trained investigators in both two surveys. Completed questionnaires were carefully checked by the supervisors after the interview each day to ensure quality. Ethical approval was received from the Institutional Review Board at the authors' University.
Measures
Chronic Conditions
In this study, we used the number of chronic diseases to represent chronic conditions. It was categorized into three groups: no chronic condition, one chronic condition, and multimorbidity (chronic conditions ≥2) (12). According to the classification of World Health Organization (46), 12 types of chronic disease were considered, including hypertension, dyslipidemia, diabetes or elevated blood sugar, malignant tumors, chronic lung disease, liver disease, heart disease, stroke, kidney disease, stomach or digestive system disease, arthritis or rheumatism, and asthma.
Persistent Pain
The persistent pain was measured by the question “Do you feel pain for a long time (longer than 6 months or more)?” The answer included “yes” and “no” (47). This tool was widely used to evaluate the prevalence of persistent pain (48).
Self-Rated Health
Self-rated health was measured by a question of “In general terms, how would you assess your health status?” The answer included “good,” “quite good,” “normal,” “rather poor,” and “poor.” The respondents with good or quite good self-rated health were classified as having good self-rated health, and those with rather poor or poor were classified as having poor self-rated health (32). It was a widely used predictor to assess subjective health (49).
Sleep Quality
We used the Chinese version of the Pittsburgh Sleep Quality Index (PSQI), which has good reliability and validity (50). This scale consists of 19 items and is categorized into 7 dimensions, including sleep duration, sleep disturbance, sleep latency, daytime dysfunction, sleep efficiency, overall sleep quality, and use of sleeping medication. Each of these is scored from 0 to 3. The total PSQI score ranged from 0 to 21, higher scores indicated worse sleep quality (51). The respondents' PSQI score <7 represented good sleep quality; those ≥7 indicated poor sleep quality (52).
Psychological Distress
Psychological distress was examined by Kessler Psychological Distress Scale (K10), which has been widely used to assess psychological health for older adults (3), and the Chinese version of K10 has been confirmed to have good reliability and validity (53). The scale mainly focuses on the PD of the respondents in the past 30 days. It contained 10-items and each item contained a 5-point Likert item. The total score for the scale ranged from 10 to 50 points, higher scores represented a higher risk of mental disorder. Finally, it was divided into 3 levels: no/low level, mild level, and moderate/severe level (53, 54).
Covariates
Sociodemographic characteristics included age, gender, marital status, education, and economic status. In this study, age was divided into 60–, 70–, and 80+ years, gender included male and female, education included illiteracy or semiliterate, primary school, junior school, and senior school or above. Economic status was estimated by household income of last year. Quartile 1 was the poorest and Quartile 4 was the richest.
Statistical Analysis
SPSS 24.0 (IBM, New York, NY, USA) and Mplus 8.3 (Muthén & Muthén, Los Angeles, CA, USA) were used to analyze the data. Firstly, frequency and percentage were used to describe the demographic characteristics of the respondents. Then we used the Chi-square tests and Kruskal-Wallis tests to compare the differences of PD degrees across different subgroups. Secondly, Spearman's correlation analysis and Chi-square tests were used to examine the correlation among all variables. Finally, we used Mplus 8.3 to test the hypothesized models with and without the pathway of sleep quality to self-rated health, respectively. Based on the results of univariate analysis and previous studies, the basic characteristics related to PD and mediators were, respectively, regarded as their covariates. Past research typically had shown that demographic characteristics (including age, gender, marital status, education, and economic status) were associated with sleep quality, self-rated health, and PD, respectively (14, 32, 37, 41). The WLSMV estimator was employed in this model because it has been found to perform well for path analysis with ordinal or categorical dependent variables (55, 56). The fit index and its acceptable value of the model including Normed Chi-square (χ2/DF <5), root mean square error of approximation (RMSEA <0.08), standardized root mean square residual (SRMR <0.05), Tucker-Lewis index (TLI), and comparative fit index (CFI >0.90) (57, 58). All statistical analyses set a statistically significant threshold with P < 0.05.
Results
Characteristics of Participants
The percentages of respondents identified as no/low, mild, and moderate/severe PD were 52.51% (n = 1,443), 27.77% (n = 763), and 19.72% (n = 542), respectively (Table 1). There were 1,305 (47.49%) respondents who had mild and above degrees of PD. Of the 2,748 respondents, 1,745 were female (63.50%), 2,026 have been married (73.73%), and 1,143 were illiterate (41.59%). The majority of them had more than one chronic condition (75.15%), without persistent pain (58.33%), had poor sleep quality (67.21%), and had good self-rated health status (58.33%).
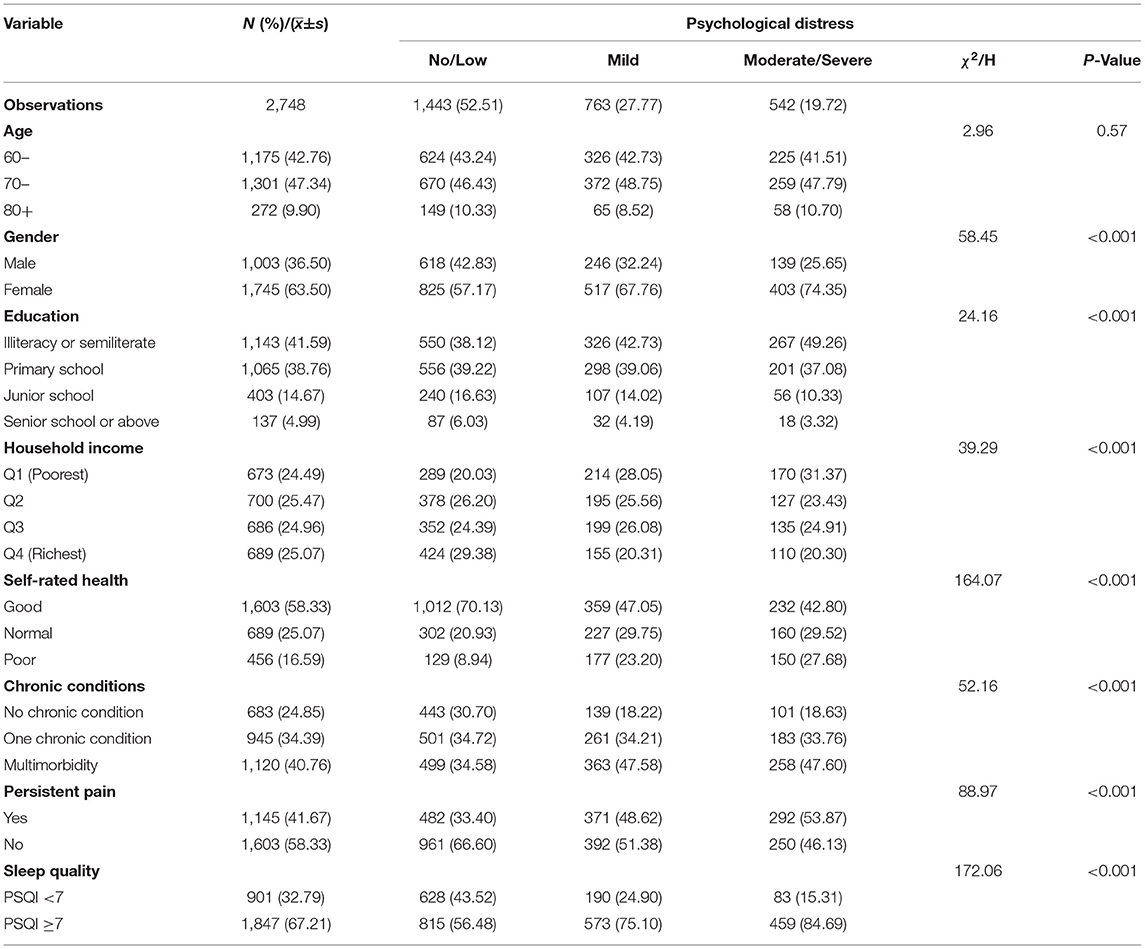
Table 1. Characters associated with psychological distress among the older adults in Shandong, China, 2020.
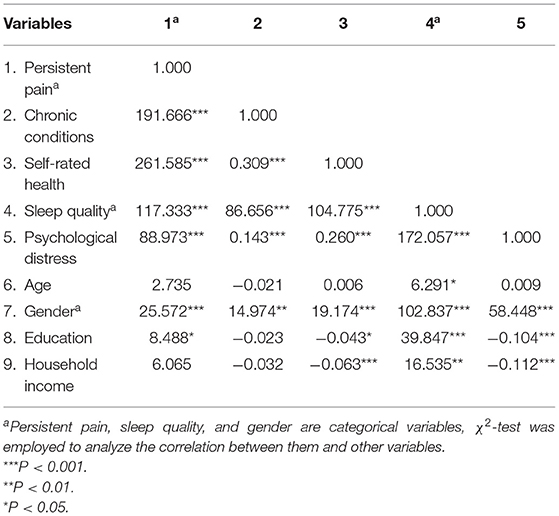
Bi-Variate Correlation of Variables
The correlation matrix of the main variables and covariates is shown in Table 2. Persistent pain (χ2 = 88.973, P < 0.001), chronic conditions (r = 0.143, P < 0.001), self-rated health (r = 0.260, P < 0.001), and sleep quality (χ2 = 117.333, P < 0.001) were all positively related to PD. Older adults with persistent pain, more than one chronic condition, poor self-rated health status, and poor sleep quality were more likely to have severer PD. Age, gender, education, and household income were considered as covariates. The association between covariates and sleep quality, self-rated health, and PD were also shown in Table 2.
Path Analysis
The hypothesized path analysis model was tested (Figure 3). It had the Normed Chi-square of 1.95, the RMSEA was 0.019, the TLI was 0.988, the CFI was 0.957, and the SRMR was 0.045, which presented a good global fit.
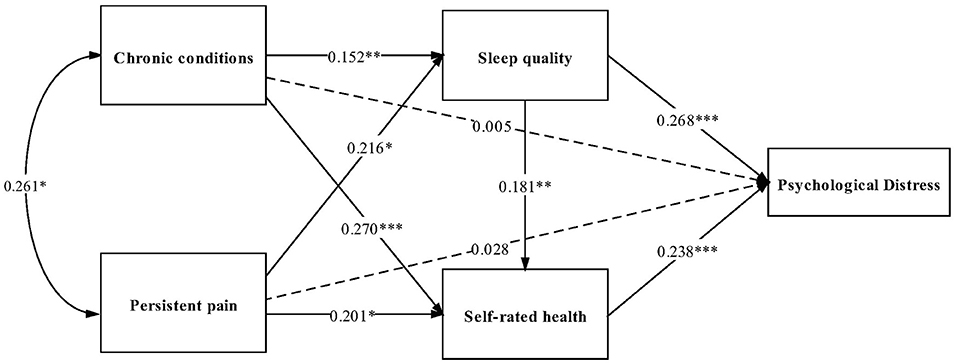
Figure 3. Path analysis of psychological distress among the older adults in Shandong, China, 2020. Standard path coefficients are shown. ***P < 0.001, **P < 0.01, and *P < 0.05.
As shown in Table 3, no significantly direct effect was found between chronic conditions and PD, while the significantly indirect effect of sleep quality (Estimate = 0.041, 95%CI: 0.015–0.067) and self-rated health (Estimate = 0.064, 95%CI: 0.038–0.091), respectively, existed in the association of chronic conditions and PD. The chain mediation of sleep quality and self-rated health on chronic conditions and PD were significant (Estimate = 0.007, 95%CI: 0.000–0.014). The total mediating effect of chronic conditions on PD was 95.73% (Estimate = 0.112, 95%CI: 0.058–0.166). For persistent pain, it had no significant direct effect on PD. Sleep quality (Estimate = 0.058, 95%CI: 0.014–0.102) and self-rated health (Estimate = 0.048, 95%CI: 0.000–0.096), respectively, played the mediating roles between persistent pain and PD. Additionally, sleep quality and self-rated health acted as chain mediators between persistent pain and PD (Estimate = 0.009, 95%CI: 0.005–0.014). The total indirect effect of persistent pain through sleep quality and self-rated health on PD was 80.42% (Estimate = 0.115, 95%CI: 0.023–0.207).
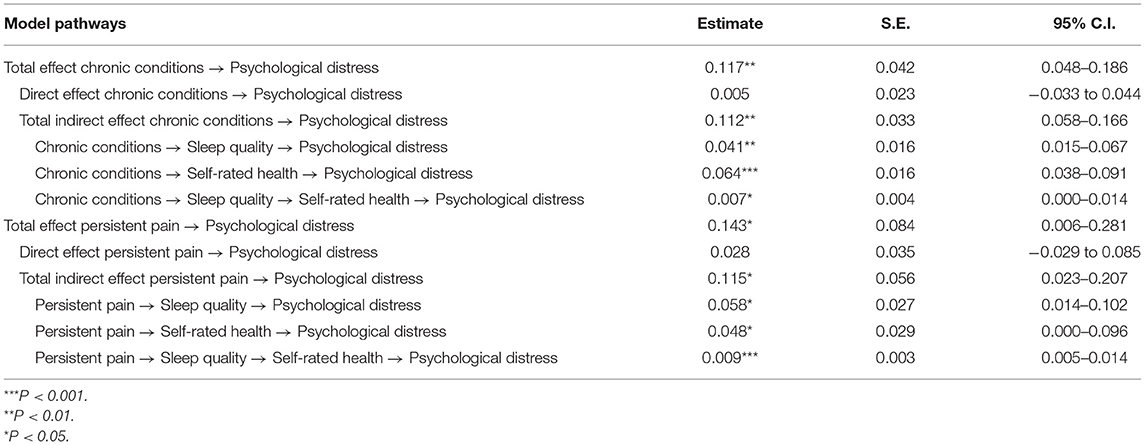
Table 3. Standardized effects on psychological distress from path analysis among the older adults in Shandong, China, 2020.
Discussion
By using path analysis, chronic conditions and persistent pain, respectively, had indirect positive associations with PD through sleep quality and self-rated health. Meanwhile, the chain mediation of sleep quality and self-rated health existed. The hypothesis model was partially verified. It is crucial for older people to keep in good mental health, while the influencing factors of mental health are diverse and the mechanism is complex. This study explores the pathways of risk factors on PD, and provides systematic inspiration for mental health management and intervention among older adults. The highlight is that not only the mediation of sleep quality and self-rated health exist, but also the chain mediations are found.
Chronic Conditions to PD
Older adults who suffered one chronic condition or multimorbidity had higher odds of PD than those without chronic conditions. There were three pathways between chronic conditions and PD. Older adults with chronic conditions were more likely to have PD through poor sleep quality. In accordance with other studies, people with multimorbidity reported more PD symptoms, and trouble sleeping had the greatest effect size among all depressive items (11). A cross-sectional study showed a dose-dependent correlation between the number of chronic diseases and the sleep disturbances index (59). Sleep disorders had been demonstrated to precipitate mental health problems among older adults (28). Further, older adults with chronic conditions were more likely to have PD through poor self-rated health. Previous studies showed that the number of chronic conditions was one of the determinants of self-rated health among the older population (30). The result was supported by a study finding that the relationship between physical impairments and depression in the elderly was mediated by self-rated health (60). Older adults with chronic conditions had a worse subjective perception of physical health, which in turn affects their mental health status (15, 60). Additionally, older people with chronic conditions were more likely to have PD through poor sleep quality and poor self-rated health. Sleep disorders were common in many chronic conditions, as well as occurred in populations with mental health problems (61). Preliminary evidence indicated that poor sleep quality was associated with poor self-rated health (62, 63). A study conducted among U.S. Hispanic older adults reported that sleep quality was associated with chronic conditions, self-rated physical health and mental health, and self-rated happiness (64). The specific path of those variables was first explored in our research. Older people with chronic conditions would have poor sleep quality, which might exacerbate negative thoughts, then influenced their mental health status, even increased the risk of suicide (65). The potential biological mechanism indicated that some chronic diseases may cause changes in the brain regions and neurotransmitters that control sleep, as well as the drugs for controlling the chronic symptoms influenced the sleep quality (61). Once sleep disorders appeared, the self-rated health status might be affected, and a series of PD symptoms such as confusion, frustration, or depression would aggravate (61, 64). The total mediating effect of chronic conditions on PD was 95.73%, which indicated that our mediators played critical roles to explain the relationship between chronic conditions and PD.
Persistent Pain to PD
Results from our study indicated that older adults who suffered persistent pain had higher odds of PD than those without lasting pain. There were three pathways between persistent pain and PD. Older adults with persistent pain were more likely to suffer PD through poor sleep quality. Consistent with previous studies, insomnia, and poor sleep quality were highly correlated with persistent pain especially in female subjects (66, 67). A person's sleep amount strongly affected the symptoms of mental disorders. Sleep disorders like deprivation and disruption can result in psychotic states of paranoia, hallucinations, or mania among vulnerable groups (61). Moreover, older adults with persistent pain were more likely to have PD through poor self-rated health. A Chinese study consistent with our finding that self-rated health and perceived social support in series partly explained the association between persistent pain and depression (68). According to the cognitive-behavioral mediation model, persistent pain might bring about a negative bias of personal health perceptions, which could lead to emotional distress such as depression (18). Furthermore, our findings revealed that older people with persistent pain were more likely to have PD through poor sleep quality and poor self-rated health. Pain was related to the feelings of losing independence and autonomy. People would be influenced by the realization of physical or mental limitations when their routine life changed, which may lead to poorer self-rated health (69). While poor self-rated health was associated with PD (68, 69). Besides, the biological mechanism of pain and mental disorders had already been demonstrated. Chronic pain stimulation resulted in a series of changes within the brain, which will produce anxiety and depression motivations or pain-related behaviors, and then mental illness appeared (70). There was a study revealed that Neuroticism and maladaptive coping strategies were the mediation between the serotonin transporter gene-linked polymorphic region (5HTT-LPR) and symptoms of anxiety and depression among elite athletes (71). This genetic polymorphism could be similar among aging population. The total indirect effect of persistent pain on PD was 80.43%, which presented that sleep quality and self-rated health were non-negligible in explaining the potential association between chronic conditions and PD.
To our knowledge, this is the first study to comprehensively investigate the underlying association of chronic conditions and PD, persistent pain and PD, as well as the mediating effect of self-rated health and sleep quality on this relationship among the Chinese rural older people. It provides a scientific basis for early detection and prevention of PD, especially for the key group of health care management, which is of high theoretical and practical significance. Thus, it is necessary to strengthen the prevention of PD among rural elderly. First of all, older adults with chronic conditions, especially with multimorbidity and persistent pain, should be regarded as the key group for regular mental health surveillance and counseling services, mental health education, and other various effective intervention measures should be carried out. Furthermore, considering the mediating effects of sleep quality and self-rated health, more attention should be paid to the regular screening of sleep quality and health status evaluation, so as to resolve the older adults' sleep problems and improve their self-rated health status.
This study had several limitations. Firstly, the causal relationships between variables were still unclear. Because this is a cross-sectional study, we did not include “persistent pain” in our baseline survey so that we used the follow-up data. Prospective studies were needed to verify the effects of chronic conditions, persistent pain, sleep quality, self-rated health on PD in further investigation. Secondly, recall bias might exist because the main variables we used were self-reported. Thirdly, we only investigated the relationship between the number of chronic diseases and PD, and did not consider the duration and severity of chronic conditions. Previous study showed that the duration and severity of chronic conditions were associated with PD (72). And we did not include the pain intensity and functional limitations in this study, which were also related to PD symptoms (18, 39). These variables will be considered in further study.
Nearly half of the rural elderly reported at least mild PD in this study. Among rural older people, sleep quality, and self-rated health were found to play partial mediating roles in the association of both chronic conditions and PD, persistent pain and PD. Efforts should be taken to control the prevalence of PD. When intervening for older adults with chronic conditions and persistent pain, sleep, and self-rated health could be considered as the key targets of intervention.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Institutional Review Board at Shandong University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
CZ participated in conceptualization, writing—review and editing, funding acquisition, and supervision. JL (2nd author), YW, and ZW were responsible for methodology. DZ, WL, JL (6th author), ZL, CY, and ZG participated in formal analysis and investigation. SY participated in investigation and writing—original draft preparation. All authors have read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (71774104, 71473152, and 71974117), the China Medical Board (16-257), Cheeloo Youth Scholar Grant, Shandong University (IFYT1810 and 2012DX006), and NHC Key Laboratory of Health Economics and Policy Research (NHC-HEPR2019014).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors are grateful to all participants for their effort. The authors thank the work of the students from the Shandong University School of Public Health. The authors appreciate the officials of local health agencies and staff at the study sites for their cooperation. The authors are grateful to Dr. H. K. Li for the statistical guidance and valuable suggestions.
References
2. China Health Retirement Report. (2019). Available online at: http://charls.pku.edu.cn/pages/doc/111/zh-cn.html (accessed August 24, 2021).
3. Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. (2002) 32:959–76. doi: 10.1017/s0033291702006074
4. Sun J, Lyu S. Social participation and urban-rural disparity in mental health among older adults in China. J Affect Disord. (2020) 274:399–404. doi: 10.1016/j.jad.2020.05.091
5. Min L, Jizhi G, Junjie J, Yuhang Z, Shanju H, Lihui Z, et al. Status of mental health among aging population in rural areas of Shandong Province. Chin J Health Educ. (2016) 32:888–91. doi: 10.16168/j.cnki.issn.1002-9982.2016.10.006
6. Zhao D, Li J, Hao W, Yuan Y, Yu C, Jing Z, et al. The relationship between activities of daily living and suicidal ideation among Chinese rural older adults: a multiple mediation model through sleep quality and psychological distress. Aging. (2020) 12:22614–25. doi: 10.18632/aging.103857
7. Jing Z, Li J, Fu PP, Wang Y, Yuan Y, Zhao D, et al. Physical multimorbidity and lifetime suicidal ideation and plans among rural older adults: the mediating role of psychological distress. BMC Psychiatry. (2021) 21:78. doi: 10.1186/s12888-021-03087-4
8. Ge D, Sun L, Zhou C, Qian Y, Zhang L, Medina A. Exploring the risk factors of suicidal ideation among the seniors in Shandong, China: a path analysis. J Affect Disord. (2017) 207:393–7. doi: 10.1016/j.jad.2016.09.031
9. Yang L, Zhao M, Magnussen CG, Veeranki SP, Xi B. Psychological distress and mortality among US adults: prospective cohort study of 330 367 individuals. J Epidemiol Commun Health. (2020) 74:384–90. doi: 10.1136/jech-2019-213144
10. Feeney SL. The relationship between pain and negative affect in older adults: anxiety as a predictor of pain. J Anxiety Disord. (2004) 18:733–44. doi: 10.1016/j.janxdis.2001.04.001
11. Spangenberg L, Forkmann T, Brähler E, Glaesmer H. The association of depression and multimorbidity in the elderly: implications for the assessment of depression. Psychogeriatrics. (2011) 11:227–34. doi: 10.1111/j.1479-8301.2011.00375.x
12. Marengoni A, Angleman S, Melis R, Mangialasche F, Karp A, Garmen A, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. (2011) 10:430–9. doi: 10.1016/j.arr.2011.03.003
13. Calderón-Larrañaga A, Vetrano DL, Welmer AK, Grande G, Fratiglioni L, Dekhtyar S. Psychological correlates of multimorbidity and disability accumulation in older adults. Age Ageing. (2019) 48:789–96. doi: 10.1093/ageing/afz117
14. Jiao C, Leng A, Nicholas S, Maitland E, Wang J, Zhao Q, et al. Multimorbidity and mental health: the role of gender among disease-causing poverty, rural, aged households in China. Int J Environ Res Public Health. (2020) 17:8855. doi: 10.3390/ijerph17238855
15. Gould CE, O'Hara R, Goldstein MK, Beaudreau SA. Multimorbidity is associated with anxiety in older adults in the Health and Retirement Study. Int J Geriatr Psychiatry. (2016) 31:1105–15. doi: 10.1002/gps.4532
16. Rashedi V, Asadi-Lari M, Foroughan M, Delbari A, Fadayevatan R. Mental health and pain in older adults: findings from urban HEART-2. Commun Mental Health J. (2017) 53:719–24. doi: 10.1007/s10597-017-0082-2
17. McCurry SM, Von Korff M, Vitiello MV, Saunders K, Balderson BH, Moore AL, et al. Frequency of comorbid insomnia, pain, and depression in older adults with osteoarthritis: predictors of enrollment in a randomized treatment trial. J Psychos Res. (2011) 71:296–9. doi: 10.1016/j.jpsychores.2011.05.012
18. Turk DC, Okifuji A, Scharff L. Chronic pain and depression: role of perceived impact and perceived control in different age cohorts. Pain. (1995) 61:93–101. doi: 10.1016/0304-3959(94)00167-d
19. Phongtankuel V, Amorapanth PX, Siegler EL. Pain in the geriatric patient with advanced chronic disease. Clin Geriatr Med. (2016) 32:651–61. doi: 10.1016/j.cger.2016.06.008
20. Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the international classification of diseases (ICD-11). Pain. (2019) 160:19–27. doi: 10.1097/j.pain.0000000000001384
21. Miller GE, Chen E, Zhou ES. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychol Bull. (2007) 133:25–45. doi: 10.1037/0033-2909.133.1.25
22. Kessler RC, Price RH, Wortman CB. Social factors in psychopathology: stress, social support, and coping processes. Ann Rev Psychol. (1985) 36:531–72. doi: 10.1146/annurev.ps.36.020185.002531
23. Slavich GM, Irwin MR. From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychol Bull. (2014) 140:774–815. doi: 10.1037/a0035302
24. Guerriero F, Reid MC. Linking persistent pain and frailty in older adults. Pain Med. (2020) 21:61–6. doi: 10.1093/pm/pnz174
25. Blay SL, Andreoli SB, Fillenbaum GG, Gastal FL. Depression morbidity in later life: prevalence and correlates in a developing country. Am J Geriatr Psychiatry. (2007) 15:790–9. doi: 10.1097/JGP.0b013e3180654179
26. Simonsson B, Molarius A. Self-rated health and associated factors among the oldest-old: results from a cross-sectional study in Sweden. Archiv Public Health. (2020) 78:6. doi: 10.1186/s13690-020-0389-2
27. Molton IR, Terrill AL. Overview of persistent pain in older adults. Am Psychol. (2014) 69:197–207. doi: 10.1037/a0035794
28. Campos Costa I, Nogueira Carvalho H, Fernandes L. Aging, circadian rhythms and depressive disorders: a review. Am J Neurodegener Dis. (2013) 2:228–46.
29. Chang-Quan H, Xue-Mei Z, Bi-Rong D, Zhen-Chan L, Ji-Rong Y, Qing-Xiu L. Health status and risk for depression among the elderly: a meta-analysis of published literature. Age Ageing. (2010) 39:23–30. doi: 10.1093/ageing/afp187
30. Damian J, Ruigomez A, Pastor V, Martin-Moreno JM. Determinants of self assessed health among Spanish older people living at home. J Epidemiol Commun Health. (1999) 53:412–6. doi: 10.1136/jech.53.7.412
31. Jang Y, Yoon H, Li M, Park NS, Chiriboga DA, Wu B, et al. Self-rated health as a mediator between physical health conditions and depressive symptoms in older Chinese and Korean Americans. PLoS ONE. (2021) 16:e0245136. doi: 10.1371/journal.pone.0245136
32. Mäntyselkä PT, Turunen JH, Ahonen RS, Kumpusalo EA. Chronic pain and poor self-rated health. JAMA. (2003) 290:2435–42. doi: 10.1001/jama.290.18.2435
33. Wang C, Pu R, Ghose B, Tang S. Chronic musculoskeletal pain, self-reported health and quality of life among older populations in South Africa and Uganda. Int J Environ Res Public Health. (2018) 15:2806. doi: 10.3390/ijerph15122806
34. Yao Y, Liu M, Yang SS, Wang JH, Zhu Q, Chen XP, et al. [Study on self-rated health and related factors in centenarians in Hainan province]. Chin J Epidemiol. (2018) 39:264–7. doi: 10.3760/cma.j.issn.0254-6450.2018.03.003
35. Yu J, Rawtaer I, Fam J, Jiang MJ, Feng L, Kua EH, et al. Sleep correlates of depression and anxiety in an elderly Asian population. Psychogeriatrics. (2016) 16:191–5. doi: 10.1111/psyg.12138
36. Papadimitriou GN, Linkowski P. Sleep disturbance in anxiety disorders. Int Rev Psychiatry. (2005) 17:229–36. doi: 10.1080/09540260500104524
37. Chen X, Wang SB, Li XL, Huang ZH, Tan WY, Lin HC, et al. Relationship between sleep duration and sociodemographic characteristics, mental health and chronic diseases in individuals aged from 18 to 85 years old in Guangdong province in China: a population-based cross-sectional study. BMC Psychiatry. (2020) 20:455. doi: 10.1186/s12888-020-02866-9
38. Wang S, Wu Y, Ungvari GS, Ng CH, Forester BP, Gatchel JR, et al. Sleep duration and its association with demographics, lifestyle factors, poor mental health and chronic diseases in older Chinese adults. Psychiatry Res. (2017) 257:212–8. doi: 10.1016/j.psychres.2017.07.036
39. Chen Q, Hayman LL, Shmerling RH, Bean JF, Leveille SG. Characteristics of chronic pain associated with sleep difficulty in older adults: the Maintenance of Balance, Independent Living, Intellect, and Zest in the Elderly (MOBILIZE) Boston study. J Am Geriatr Soc. (2011) 59:1385–92. doi: 10.1111/j.1532-5415.2011.03544.x
40. Artner J, Cakir B, Spiekermann JA, Kurz S, Leucht F, Reichel H, et al. Prevalence of sleep deprivation in patients with chronic neck and back pain: a retrospective evaluation of 1016 patients. J Pain Res. (2013) 6:1–6. doi: 10.2147/jpr.s36386
41. Lee KE, Ryu H, Chang SJ. The effect of pain catastrophizing on depression among older Korean adults with chronic pain: the mediating role of chronic pain interference and sleep quality. Int J Environ Res Public Health. (2020) 17:8716. doi: 10.3390/ijerph17238716
42. Štefan L, Juranko D, Prosoli R, Barić R, Sporiš G. Self-reported sleep duration and self-rated health in young adults. J Clin Sleep Med. (2017) 13:899–904. doi: 10.5664/jcsm.6662
43. Oftedal S, Kolt GS, Holliday EG, Stamatakis E, Vandelanotte C, Brown WJ, et al. Associations of health-behavior patterns, mental health and self-rated health. Prevent Med. (2019) 118:295–303. doi: 10.1016/j.ypmed.2018.11.017
44. Jing Z, Li J, Wang Y, Ding L, Tang X, Feng Y, et al. The mediating effect of psychological distress on cognitive function and physical frailty among the elderly: evidence from rural Shandong, China. J Affect Disord. (2020) 268:88–94. doi: 10.1016/j.jad.2020.03.012
45. Wang Y, Fu P, Li J, Jing Z, Wang Q, Zhao D, et al. Changes in psychological distress before and during the COVID-19 pandemic among older adults: the contribution of frailty transitions and multimorbidity. Age Ageing. (2021) 50:1011–8. doi: 10.1093/ageing/afab061
46. World Health Organization. Non-Communicable Diseases. Available online at: https://www.who.int/topics/noncommunicable_diseases/zh/ (accessed August 24, 2021).
47. American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons. Pharmacological management of persistent pain in older persons. Pain Med. (2009) 10:1062–83. doi: 10.1111/j.1526-4637.2009.00699.x
48. Lohman MC, Whiteman KL, Greenberg RL, Bruce ML. Incorporating persistent pain in phenotypic frailty measurement and prediction of adverse health outcomes. J Gerontol Ser A Biol Sci Med Sci. (2017) 72:216–22. doi: 10.1093/gerona/glw212
49. Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. (1997) 38:21–37. doi: 10.2307/2955359
50. Xianchen L, Maoqin T, Lei H, Aizhen W, Hongxin W, Guifang Z, et al. Reliability and validity of the Pittsburgh sleep quality index. Chin J Psychiatry. (1996) 29:103–7.
51. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
52. Del Brutto OH, Mera RM, Sedler MJ, Zambrano M, Nieves JL, Cagino K, et al. The effect of age in the association between frailty and poor sleep quality: a population-based study in community-dwellers (the Atahualpa project). J Am Med Direct Assoc. (2016) 17:269–71. doi: 10.1016/j.jamda.2015.12.009
53. Chengchao Z, Jie C, Ting W, Qianqian P, Jiangjiang H, Wengui Z, et al. Reliability and validity of 10-item Kessler Scale (K10) Chinese version in evaluation of mental health status of Chinese population. Chin J Clin Psychol. (2008) 16:627–9. doi: CNKI:SUN:ZLCY.0.2008-06-026
54. Andrews G, Slade T. Interpreting scores on the Kessler Psychological Distress Scale (K10). Austral N Zeal J Public Health. (2001) 25:494–7. doi: 10.1111/j.1467-842x.2001.tb00310.x
55. Beauducel A, Herzberg PY. On the performance of maximum likelihood versus means and variance adjusted weighted least squares estimation in CFA. Struct Equ Model Multidisc J. (2006) 13:186–203. doi: 10.1207/s15328007sem1302_2
56. Hoyle RH, Gottfredson NC. Sample size considerations in prevention research applications of multilevel modeling and structural equation modeling. Prevent Sci. (2015) 16:987–96. doi: 10.1007/s11121-014-0489-8
57. Zhonglin W, Jietai H, Marsh HW. Structural equation model testing: cutoff criteria for goodness of fit indices and Chi-square test. Acta Psychol Sin. (2004) 36:186–94. doi: 10.1007/BF02911031
58. Marsh HW, Hau K-T, Wen Z. In search of golden rules: comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler's (1999) findings. Struct Equ Model Multidisc J. (2004) 11:320–41. doi: 10.1207/s15328007sem1103_2
59. Koyanagi A, Garin N, Olaya B, Ayuso-Mateos JL, Chatterji S, Leonardi M, et al. Chronic conditions and sleep problems among adults aged 50 years or over in nine countries: a multi-country study. PLoS ONE. (2014) 9:e114742. doi: 10.1371/journal.pone.0114742
60. Olawa BD, Adebayo SO, Mokuolu BO, Umeh CS, Omolayo BO. Physical health burdens and emotional distress in later life: the mediating effects of self-rated health. Aging Mental Health. (2020) 24:15–21. doi: 10.1080/13607863.2018.1506748
61. What Is Sleep and Why Is It Important? American Sleep Association. Available online at: https://www.sleepassociation.org/about-sleep/what-%20is-sleep/ (accessed August 24, 2021).
62. Magee CA, Caputi P, Iverson DC. Relationships between self-rated health, quality of life and sleep duration in middle aged and elderly Australians. Sleep Med. (2011) 12:346–50. doi: 10.1016/j.sleep.2010.09.013
63. Haseli-Mashhadi N, Dadd T, Pan A, Yu Z, Lin X, Franco OH. Sleep quality in middle-aged and elderly Chinese: distribution, associated factors and associations with cardio-metabolic risk factors. BMC Public Health. (2009) 9:130. doi: 10.1186/1471-2458-9-130
64. Roncoroni J, Wu Whitaker S, Wippold G. Sociodemographic and health correlates of sleep in U.S. Hispanic older adults. Sleep Med. (2020) 68:213–7. doi: 10.1016/j.sleep.2020.01.007
65. Ma X, Xiang YT, Cai ZJ, Li SR, Xiang YQ, Guo HL, et al. Lifetime prevalence of suicidal ideation, suicide plans and attempts in rural and urban regions of Beijing, China. Austral N Zeal J Psychiatry. (2009) 43:158–66. doi: 10.1080/00048670802607170
66. Afolalu EF, Ramlee F, Tang NKY. Effects of sleep changes on pain-related health outcomes in the general population: a systematic review of longitudinal studies with exploratory meta-analysis. Sleep Med Rev. (2018) 39:82–97. doi: 10.1016/j.smrv.2017.08.001
67. Zhang J, Lam SP, Li SX, Tang NL, Yu MWM, Li AM, et al. Insomnia, sleep quality, pain, and somatic symptoms: sex differences and shared genetic components. Pain. (2012) 153:666–73. doi: 10.1016/j.pain.2011.12.003
68. Chen Y, Wu M, Zeng T, Peng C, Zhao M, Xiao Q, et al. Effect of pain on depression among nursing home residents: serial mediation of perceived social support and self-rated health. A cross-sectional study. Geriatr Gerontol Int. (2020) 20:1234–40. doi: 10.1111/ggi.14067
69. Mulsant BH, Ganguli M, Seaberg EC. The relationship between self-rated health and depressive symptoms in an epidemiological sample of community-dwelling older adults. J Am Geriatr Soc. (1997) 45:954–8. doi: 10.1111/j.1532-5415.1997.tb02966.x
70. Usdin TB, Dimitrov EL. The effects of extended pain on behavior: recent progress. Neuroscientist. (2016) 22:521–33. doi: 10.1177/1073858416633104
71. Altamura M, Iuso S, D'Andrea G, D'Urso F, Piccininni C, Angelini E, et al. Maladaptive coping strategies and neuroticism mediate the relationship between 5HTT-LPR polymorphisms and symptoms of anxiety in elite athletes. Clin Neuropsychiatry. (2019) 16:62–71. doi: 10.1101/493320
Keywords: psychological distress, chronic conditions, persistent pain, older adults, rural
Citation: Yang S, Li J, Zhao D, Wang Y, Li W, Li J, Li Z, Wei Z, Yan C, Gui Z and Zhou C (2021) Chronic Conditions, Persistent Pain, and Psychological Distress Among the Rural Older Adults: A Path Analysis in Shandong, China. Front. Med. 8:770914. doi: 10.3389/fmed.2021.770914
Received: 05 September 2021; Accepted: 11 October 2021;
Published: 02 November 2021.
Edited by:
Jeremy M. Jacobs, Hadassah Medical Center, IsraelReviewed by:
Tomasz Kostka, Medical University of Lodz, PolandCristoforo Pomara, University of Catania, Italy
Copyright © 2021 Yang, Li, Zhao, Wang, Li, Li, Li, Wei, Yan, Gui and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chengchao Zhou, emhvdWNoZW5nY2hhb0BzZHUuZWR1LmNu
 Shijun Yang
Shijun Yang Jie Li
Jie Li Dan Zhao
Dan Zhao Yi Wang
Yi Wang Wenjuan Li1
Wenjuan Li1 Chen Yan
Chen Yan Chengchao Zhou
Chengchao Zhou