- Department of Anesthesiology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
Since their advent, videolaryngoscopes have played an important role in various types of airway management. Lung isolation techniques are often required for thoracic surgery to achieve one-lung ventilation with a double-lumen tube (DLT) or bronchial blocker (BB). In the case of difficult airways, one-lung ventilation is extremely challenging. The purpose of this review is to identify the roles of videolaryngoscopes in thoracic airway management, including normal and difficult airways. Extensive literature related to videolaryngoscopy and one-lung ventilation was analyzed. We summarized videolaryngoscope-guided DLT intubation techniques and discussed the roles of videolaryngoscopy in DLT intubation in normal airways by comparison with direct laryngoscopy. The different types of videolaryngoscopes for DLT intubation are also compared. In addition, we highlighted several strategies to achieve one-lung ventilation in difficult airways using videolaryngoscopes. A non-channeled or channeled videolaryngoscope is suitable for DLT intubation. It can improve glottis exposure and increase the success rate at the first attempt, but it has no advantage in saving intubation time and increases the incidence of DLT mispositioning. Thus, it is not considered as the first choice for patients with anticipated normal airways. Current evidence did not indicate the superiority of any videolaryngoscope to another for DLT intubation. The choice of videolaryngoscope is based on individual experience, preference, and availability. For patients with difficult airways, videolaryngoscope-guided DLT intubation is a primary and effective method. In case of failure, videolaryngoscope-guided single-lumen tube (SLT) intubation can often be achieved or combined with the aid of fibreoptic bronchoscopy. Placement of a DLT over an airway exchange catheter, inserting a BB via an SLT, or capnothorax can be selected for lung isolation.
Introduction
In thoracic anesthesia, lung isolation techniques are often required to achieve one-lung ventilation. Double-lumen tubes (DLTs) are widely used in adult thoracic surgery because they provide reliable isolation and separate ventilation. However, owing to their large diameter, high rigidity, and complex configuration, it is not easy to intubate a DLT compared with a routine endotracheal tube (ETT); this difficulty is increased in the case of a difficult airway (1–3). In such cases, it is necessary to secure the airway and maintain oxygenation, and then consider the possibility of lung collapse (2, 3).
Since their advent, videolaryngoscopes have played an important role in airway management, including expected and unexpected difficult airways (4, 5). There are many reports on using videolaryngoscopes in DLT intubation, but their advantages in thoracic anesthesia are not as distinct as in other specialties (6–8). This review summarizes the techniques of videolaryngoscope-guided DLT intubation and discusses the roles of videolaryngoscopy in DLT intubation in normal airways compared with direct laryngoscopy. The different types of videolaryngoscopes for DLT intubation are also compared. In addition, we highlight several strategies to achieve one-lung ventilation in difficult airways using videolaryngoscopes.
Overview of Videolaryngoscopy
Videolaryngoscopy is a new type of laryngoscopy that incorporates video systems using micro-camera technology and optical or fiber optical guided transmission (9). GlideScope, invented by John A. Pacey, was the first videolaryngoscope and was officially introduced into clinical practice in 2001 (10). It was first published for resolving difficult intubation in 2003 (11). Various videolaryngoscopes have been developed since 2006. Most videolaryngoscopes contain a light source and an image sensor close to the blade tip. Instead of line of sight with a direct laryngoscope, the videolaryngoscope does not require alignment of the oral, pharyngeal, and laryngeal axes and enables the operator to visualize the glottis on the video screen. Videolaryngoscopy has several advantages over direct laryngoscopy (12, 13), such as a better view of the larynx, increased success rate of intubation, short intubation time, and less force required for intubation (14, 15). The videolaryngoscopy technique is also easy to learn especially for novices (16, 17).
In the past 20 years, videolaryngoscopy has played important roles in airway management (18). It has not only managed expected difficult airways (13, 19), such as in the case of morbid obesity, limited mouth opening, cervical immobility, and oropharyngeal masses, but also unexpected difficult airways (20). This method has also been successfully applied in obstetric anesthesia (21), pediatric anesthesia (22), emergent intubation (23), nasotracheal intubation (24), and awake intubation (25). Therefore, guidelines for difficult airway management have indicated that videolaryngoscopy can be applied as an initial approach for difficult intubation (26) or a rescue technique for unanticipated difficult intubation (18), and all anesthetists should be proficient with the use of a videolaryngoscope (5).
Videolaryngoscopes can be classified as non-channeled or channeled. For example, GlideScope (Verathon Inc, Bothell, WA, USA) (27), McGrath (Aircraft Medical, Edinburgh, UK) (28), Storz (Karl Storz, Tuttlingen, Germany) (29), UEscope (UE Medical Corp, Zhejiang, China) (30), and non-channeled King Vision (Ambu A/S, Ballerup, Denmark) (31) are non-channeled videolaryngoscopes. They are similar to a standard laryngoscope (Figure 1). However, it may be difficult to place the tube into the glottis despite obtaining a good laryngeal view when using these devices (18). This difficulty can be resolved by a rigid stylet. A pre-shaped tracheal tube is recommended to facilitate intubation (10, 20). Channeled videolaryngoscopes, such as Airtraq (Prodol Meditec, Vizcaya, Spain) (32, 33), Pentax Airway Scope (Nihon Kohden, Tokyo, Japan) (34), and King Vision (Ambu A/S, Ballerup, Denmark) (35), have a guiding channel. The lubricated ETT is preloaded into the guiding channel. The videolaryngoscope is inserted to obtain a glottic view in the midline, and the tube is then placed into the trachea through the channel.
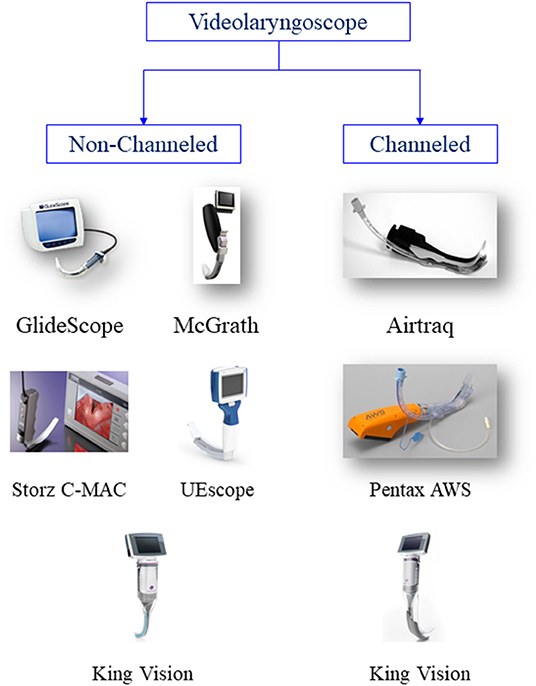
Figure 1. Classfication of videolaryngoscopes. GlideScope image courtesy of Verathon, USA. McGrath series 5 image courtesy of Aircraft Medical, UK. Airtraq image courtesy of Prodol Meditec, Spain. C-MAC image courtesy of KARL STORZ Endoscopy, Germany. UEscope image courtesy of UE Medical Corp, China. Pentax AWS, King Vision image courtesy of Ambu USA. Part of this figure is taken from Healy et al BMC Anesthesiol. 2012; 12: 32. ©2012 Healy et al.; licensee BioMed Central Ltd. Reproduced under the terms of its Creative Commons Attribution License (2.0).
In addition, based on the blade angle, videolaryngoscopes can be classified as standard or hyperangulated (36). The Storz V-Mac (37), Storz C-Mac (38), and McGrath MAC devices were designed using a standard laryngoscope blade but with a camera incorporated into the distal tip. After insertion of the blade into the mouth, the glottis can be viewed alongside the blade following the traditional method or on the monitor. GlideScope, McGrath Series 5, Storz D-blade, and Airtraq have hyperangulated blades. They can increase the field and angle of view with less neck flexion and improve the glottic view compared with direct laryngoscopy (27, 39).
Videostylets, such as Optiscope, Trachway, Shikani optical stylet, and Light Wand, are other types of videoscope (36). They differ from traditional laryngoscopes in design and intubating techniques, and they are not considered the first rescue choice after failed intubation with a direct laryngoscope (18). Although they have extensive advantages in limited mouth opening and cervical fixation cases, they are outside the scope of this review.
Key Points of Videolaryngoscope-Guided DLT Intubation
Many studies have reported the application of different types of videolaryngoscopes in DLT intubation, such as GlideScope (40, 41), McGrath (42), Airtraq (43, 44), CEL-100 (45), Pentax Airway Scope (46, 47), C-Mac D blade (48), King Vision (KVL) (49).
Generally, DLT intubation comprises four steps: glottis exposure using a videolaryngoscope, guiding the tip of the DLT into the glottis, advancing the tube through the glottis until it enters the appropriate main bronchus, and confirming the position of the DLT by fibreoptic bronchoscopy (FOB) (50). In the next section, we discuss GlideScope and Airtraq as typical examples of non-channeled and channeled videolaryngoscopes, respectively, to illustrate videolaryngoscope-guided DLT placement.
GlideScope: A Non-channeled Videolaryngoscope
Since its introduction in 2001, GlideScope has been one of the most extensively studied videolaryngoscopes for DLT intubation. GlideScope provides superior glottis views to direct laryngoscopy; however, it can often be difficult to place the DLT into the glottis and advance the tube into the trachea when using GlideScope (40, 51) and other non-channeled videolaryngoscopes (7, 45). Several tips can be used to facilitate DLT intubation using GlideScope.
1. A pre-shaped DLT with a malleable stylet following the curve of the GlideScope should be used (40, 52). An appropriate stylet angle may lead to fewer failed intubation attempts and less airway trauma. Stylets with a 90° angle resulted in easier and faster intubation than those with a 60° angle using the GlideScope in single lumen tube (SLT) intubation (53, 54). Owing to the thick diameter of the DLT, manipulation inside the oropharyngeal space is restricted. Adjusting the DLT into the glottis was more difficult than the placement of the SLT. Hernandez and Wong (40) first described the successful use of GlideScope for DLT placement in a patient with a potentially difficult airway. They recommended bending the stylet of the DLT at 16–20 cm proximal to the tip to follow the curve of the GlideScope. Bustamante et al. (52) and Hsu et al. (41) recommended pre-curving the tube at the distal 10–12 cm of the DLT. The GlideRite DLT Stylet is a semi-rigid intubating stylet recommended by Bussieres et al. (55, 56). However, the optimal shape and angle of the stylet required for successful DLT intubation with GlideScope have not been determined in a randomized controlled study.
2. Sequentially rotate the tube to the desired depth when advancing the DLT. After the distal DLT passes through the vocal cord, difficulty can arise when attempting to advance it with GlideScope, because the distal concavity is directed anteriorly to the tracheal wall, and the axis of the bronchial lumen is nearly perpendicular to the axis of the trachea. Bustamante et al. (52) recommended that after the tip of the bronchial lumen engages in the glottis, the stylet should be removed, and the DLT should be rotated 180° counter-clockwise to facilitate passage of the bronchial cuff. An additional 90° clockwise rotation should then be performed to align the DLT with the left main bronchus. Hsu et al. (57) also reported a modified technique. After the DLT was inserted through the vocal cords, the DLT was advanced gently by rotating in a 90° clockwise direction until resistance was noted. The modified technique saves intubation time and reduces the severity of post-intubation complications, compared with the 180° clockwise rotation of the DLT during the placement of a DLT using GlideScope.
3. Sequential rotation could increase the risk of incorrect tube positioning during videolaryngoscope-guided DLT placement (58). For example, the tip of left-sided DLT could be migrated into the right bronchus. It is important to confirm the DLT position using FOB.
4. Take care to avoid the tracheal cuff scraping by the teeth during DLT insertion.
Airtraq: A Channeled Videolaryngoscope
Hirabayashi and Seo (43) first reported the successful use of Airtraq for DLT intubation in 2007 and recommended Airtraq as an alternative approach for DLT placement.
The Airtraq videolaryngoscope with a guiding channel offers multiple options for visualizing the glottis, including a direct view, AWDR video system, A-360 Wi-Fi camera, universal adapter for smartphones, or Endo cam connection (59–61). The side channel can accommodate a tube with an external diameter of ≤ 19 mm, which allows for the placement of DLTs of 28–41 Fr. The inner surface of the side channel is treated with a concavo-convex pattern to reduce tube friction.
For Airtraq-guided DLT intubation, remove the original stylet, lubricate the DLT and channel, then preload the tube into the channel before intubation. Airtraq is inserted into the midline of the patient's mouth to slide it over the center of the tongue until the glottis structures are identified (16). Once the bronchial cuff passes through the glottis, the DLT is rotated 90° counter-clockwise and further advanced until resistance is felt. The tube is separated from the channel, and the laryngoscope is removed from the mouth (62, 63). Finally, the position of the DLT is checked using FOB. As the DLT was loaded in the channel during Airtraq-guided DLT intubation, one distinct advantage is that Airtraq has zero tracheal cuff rupture, compared with the Macintosh, GlideScope and non-channel KVL (64).
Comparison of Videolaryngoscopy and Direct Laryngoscopy for DLT Intubation in Normal Airways
To date, 19 prospective randomized controlled studies have reported the efficacy of six videolaryngoscopes for DLT intubation compared with the Macintosh laryngoscope (Table 1) in patients with predicted normal airways. The main outcomes included glottic view, intubation time, success rate, intubation difficulty score, incidence of malposition, postoperative sore throat, hoarseness, related complications, and intubation-related stress response. Except that videolaryngoscopy can provide a better view of the glottis than the Macintosh, other findings were inconsistent between different studies. This heterogeneity may be attributed to the performer's experience, type of videolaryngoscope used, and primary outcome definition.
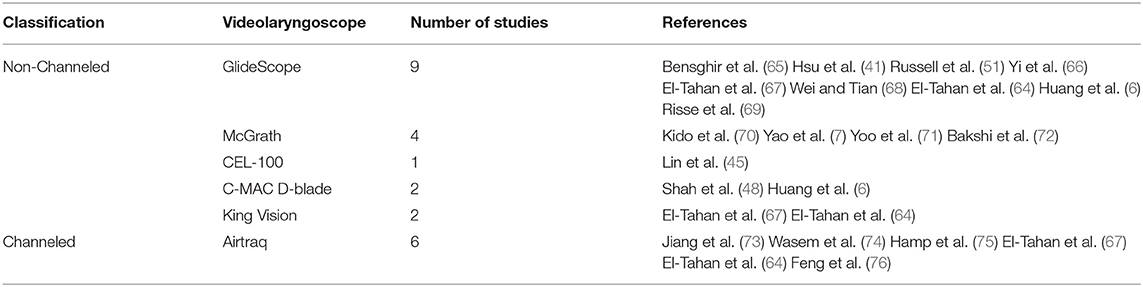
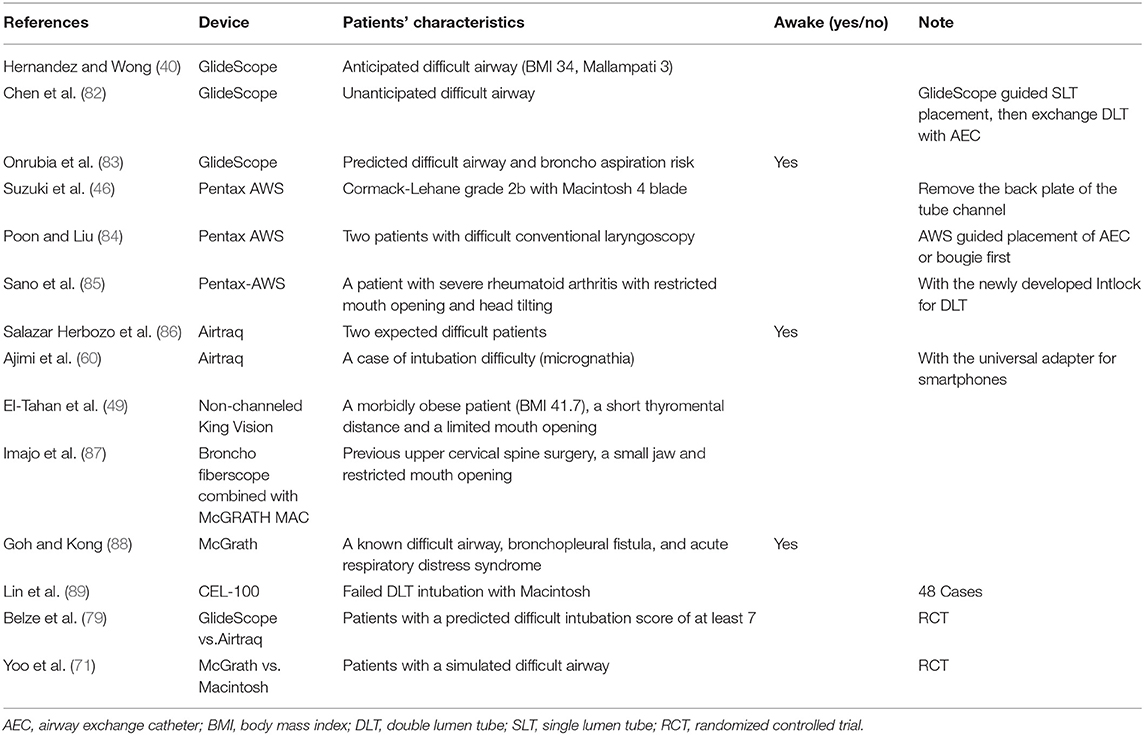
Table 1. Randomized controlled trials on videolaryngoscope vs. the Macintosh laryngoscope for double lumen tube intubation.
Two studies demonstrated that GlideScope provided a shorter intubation time and a lower incidence of sore throat and hoarseness than the Macintosh laryngoscope (41, 65). In contrast, Russell et al. (51) reported that GlideScope for DLT intubation resulted in a longer intubation time, increased intubation difficulty, and increased incidence of intubation-related complications. These contradictory results may be explained by the diversity of operator experience in using GlideScope for DLT intubation. Yi et al. (66) also reported that GlideScope prolonged the DLT intubation time compared with Macintosh, although it improved the exposure of the glottis because the method is more complex.
Wasem et al. (74) found no significant differences between Airtraq and Macintosh regarding intubation time or the number of attempts required for successful DLT insertion; however, a higher incidence of hoarseness was observed with Airtraq. Other studies have also reported that videolaryngoscopes are not superior to the conventional Macintosh laryngoscope for DLT intubation in patients with anticipated normal airways (7, 44, 64, 75, 77).
In a systematic review and meta-analysis, Liu et al. (58) found that videolaryngoscopy provided a higher success rate of DLT intubation at the first attempt and lower incidences of intubation-related injuries and sore throat. However, videolaryngoscopy increased the incidence of DLT mispositioning. According to the performer's experience, the subgroup analysis showed the success rate at the first attempt with a videolaryngoscope was higher than that with a Macintosh laryngoscope for experienced performers. However, this advantage was not observed in novices. Additionally, the time to DLT intubation was comparable between the videolaryngoscope and the Macintosh laryngoscope. However, the reported outcomes were highly heterogeneous, likely due to the different definitions and types of videolaryngoscopes used in the studies.
Kim et al. (78) performed a network meta-analysis of 23 studies. The patients were classified into four groups according to the types of the laryngoscopes: channeled videolaryngoscope, non-channeled videolaryngoscope, videostylet, and Macintosh laryngoscope. They found that most videoscopes showed higher success rates in the first attempt but an increased risk of DLT malposition than Macintosh. Videolaryngoscopes, particularly non-channeled videolaryngoscopes, seemed time-consuming compared to Macintosh. Channeled videolaryngoscope was also associated with a higher risk of oral mucosal injury but did not increase the risk of sore throat.
Compared with the Macintosh laryngoscope, the lifting forces on the base of the tongue were reduced with the videolaryngoscope (15). However, the cardiovascular response following DLT intubation was not analyzed in the meta-analysis. There are three studies on the cardiovascular response following DLT intubation, but the conclusions differ. Hamp et al. (75) found that arterial blood pressure, heart rate, and catecholamine levels were comparable after DLT intubation using Airtraq and Macintosh. Wei and Tian (68) reported that GlideScope induced milder circulatory fluctuations than did Macintosh according to the change in systolic blood pressure. Feng et al. (76) found that Airtraq-guided DLT intubation required a higher EC50 of remifentanil for inhibiting cardiovascular responses compared to Macintosh when induced with a target-controlled infusion of propofol. This indicated that the cardiovascular response during DLT intubation was more intense with Airtraq videolaryngoscopy than with direct laryngoscopy.
Taken together, compared with a direct laryngoscope, the significant advantage of videolaryngoscope-guided DLT intubation is that it improves glottis exposure and increases the success rate at the first attempt. It does not show any advantage in intubation time; moreover, it increases the incidence of DLT mispositioning in patients with normal airways. Thus, videolaryngoscopy is suitable for DLT intubation. However, it is not considered as the first choice for patients with anticipated normal airways, particularly for anaesthesiologists with limited experience in videolaryngoscope-guided DLT intubation.
Comparison of Different Types of Videolaryngoscopes for DLT Intubation
There are some differences among the different types of videolaryngoscopes. A channeled videolaryngoscope provides an adjacent passage to advance the DLT toward the glottis but limits the ability to manipulate the tube. A non-channeled videolaryngoscope, particularly one with an angulated blade, requires a stylet preshaped to follow the curve of the blade, and the extreme angulation of these blades may complicate tube delivery into the trachea. Eight studies have compared videolaryngoscopes for DLT intubation, mainly focusing on the comparison between channeled and non-channeled, such as Airtraq vs. GlideScope or McGrath Series 5 (Table 2). There is no consensus regarding which videolaryngoscope is optimal for DLT intubation.
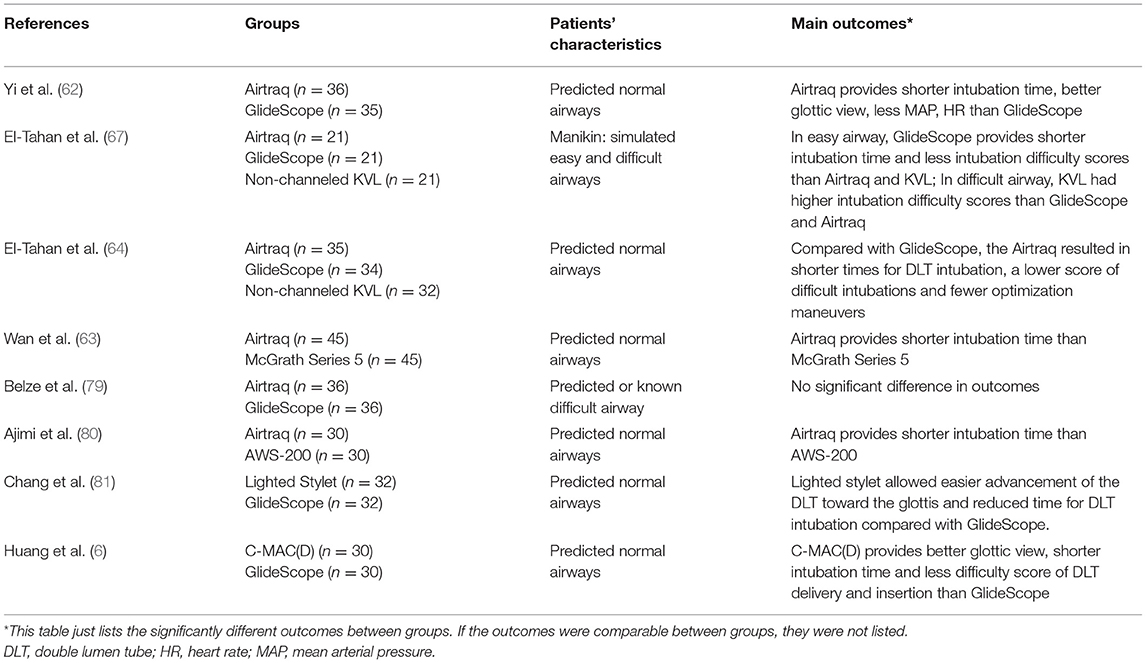
Table 2. Random controlled studies comparing different types of videolaryngoscopes for double lumen tube intubation.
Consistently, Yi et al. (62), El-Tahan et al. (64), and Wan et al. (63) reported that Airtraq provided more rapid intubation of DLT than GlideScope or McGrath; however, the success rates at the first attempt, intubation difficulty score, DLT malpositioning, and intubation-related complications were comparable. The authors attributed the longer intubation time to the use of a molded stylet and a steering technique. These results are different from a manikin study (67) in which they found a longer intubation time and greater intubation difficulty with Airtraq than with GlideScope. The authors attributed the contrary findings to the diversity of prior operator experience and the inherent problems (e.g., high resistance because of the simulator material) in all manikin studies. In addition, El-Tahan et al. study (64) has shown that the Airtraq had an advantage in avoiding tracheal cuff ruptures during insertion of the DLT, compared with GlideScope and non-channel KVL, but a network meta-analysis showed the oral mucosal damage occurred most frequently with the channeled videolaryngoscope (78).
Both Airtraq and AWS-200 are channeled videolaryngoscopes. A recent study (80) described that DLT intubation was quicker with Airtraq than with AWS-200. The authors explained that the difference was attributed to the shape and special treatment of the side channel with Airtraq.
Both GlideScope and C-MAC(D) are non-channeled videolaryngoscopes. The blade of GlideScope has an angulation of 60°, while the C-MAC(D) videolaryngoscope has an angulation of 40°. In the study by Huang et al. (6), the DLT insertion time was shorter with C-MAC(D) than with GlideScope. However, they found no differences in the success rate, DLT malposition, and incidences of intubation-related complications.
All of the above studies were performed in normal airways. Belze et al. (79) enrolled elective thoracic patients with a predicted difficult intubation score of ≥7 and compared the efficacy of GlideScope and Airtraq for DLT intubation. They found no differences in the overall success rate, visualization of the glottis, intubation time, and side effects between the two videolaryngoscopes. Thus, the success rate of DLT intubation for difficult airways is not dependent on the videolaryngoscope used.
Taken together, current evidence does not indicate which videolaryngoscope is superior to others for DLT intubation in glottic view, intubation success, first attempt intubation, and incidence of mispositioning. Although a slight difference in intubation time can be observed between different videolaryngoscopes, there was not much clinical significance.
Choices of Videolaryngoscope in Managing Difficult Airways in Thoracic Surgery
Difficult airways can be divided into the following five categories: difficult facemask or supraglottic airway (SGA) ventilation, difficult SGA placement, difficult laryngoscopy, difficult tracheal intubation, and failed intubation (26). In thoracic surgery, difficult airways are very challenging. The first challenge lies in securing the airway and maintaining oxygenation; the second involves achieving one-lung isolation using DLT or a bronchial blocker (BB) (3). Due to the distinct advantages of videolaryngoscopy, several options can be considered for managing difficult thoracic airways with videolaryngoscopes (Figure 2).
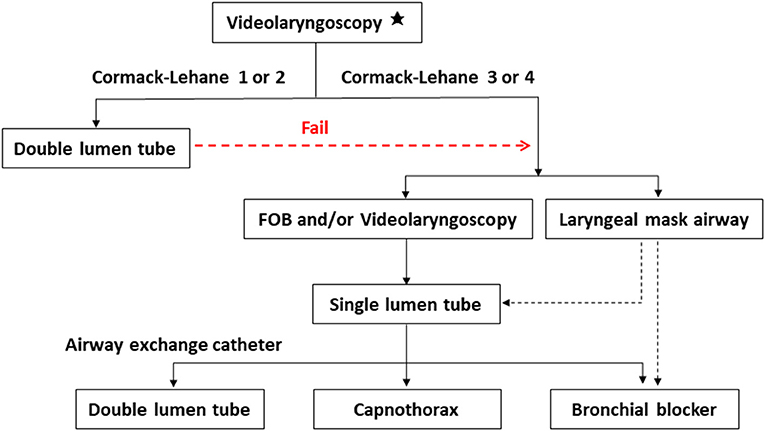
Figure 2. Several strategies to achieve one-lung ventilation in difficult airways using videolaryngoscopes. *Backward, upward and rightward pressure of larynx (BURP) maneuver is used to improve glottic exposure if required. Using videolaryngoscopy, the glottic view is determined according to Cormack-Lehane classification. Grade 1, most of the glottis is visible; grade 2, partial glottis is visible; grade 3, only the epiglottis is visible; grade 4, not even the epiglottis can be seen. If the glottic view is adequate, a double lumen tube is placed with the guide of videolaryngoscope. In case of failure or inadequate glottic view, a single lumen tube is placed with FOB and/or videolaryngoscope, or the patient is secured with a laryngeal mask airway. Then one-lung ventilation is achieved through exchange of a double lumen tube over an airway exchange catheter, inserting a bronchial blocker, or capnothorax. FOB: fibreoptic bronchoscopy.
Videolaryngoscope-Guided DLT Intubation
Several case reports (40, 46, 49, 60) have reported that videolaryngoscopes successfully managed the DLT intubation for patients with difficult airways (Table 3). Lin et al. (89) reported that in cases of difficult laryngoscopy and failed DLT intubation with Macintosh, using the CEL-100 videolaryngoscope improved the glottic view with a ~90% success rate for DLT insertion. A recent randomized clinical trial (71) reported that the McGrath videolaryngoscope provided a better glottic view and decreased the overall DLT intubation difficulty score in patients with simulated difficult airways through manual in-line stabilization of the cervical spine. Belze et al. (79) reported no difference in the overall success rates, glottic visualization, intubation time, and side effects between GlideScope and Airtraq for DLT intubation in difficult airways.
Based on a detailed evaluation of the airway history, physical examination, and additional evaluation in cases of anticipated difficult laryngoscopy or difficult intubation, if a DLT is applicable, the performer may reasonably choose a videolaryngoscope as a primary intubation tool. The choice of videolaryngoscope is based on individual experience, preference, and availability. Studies have demonstrated a correlation between intubation success and the operator's proficiency in the device rather than the device used (58, 79).
If the glottic view is adequate, but guiding the tip of the DLT into the glottis or advancing the tube pass through the glottis is difficult, videolaryngoscopy combined with FOB may be an effective approach. In the study by Imajo et al. (87), Lai and Wu (90), a fibreoptic bronchoscope was used as a stylet and placed through the bronchial lumen. Under videolaryngoscopy observation, they guided the tip of the tube to the glottis using FOB and facilitated DLT intubation. This hybrid method has an additional benefit of real-time visualization of all procedures, allowing the anaesthesiologist to ensure successful and safe intubation. For patients with restricted neck movement or limited mouth opening, a videostylet may be a useful alternative tool for DLT placement (91, 92).
Although awake fibreoptic DLT intubation is a good airway management option for an anticipated difficult airway, it has several disadvantages, such as the difficulty of the technique, and anatomical structures, such as upper airway soft tissue resistance, which can make it difficult to intubate. Previous reports (83, 86, 93) have described several alternatives to FOB, such as GlideScope, Airtraq, and videostylets that can be effectively used in patients with difficult airways for awake DLT intubation.
Videolaryngoscope-Guided SLT Intubation
It is more difficult to intubate a DLT than a standard SLT. For anaesthesiologists with limited experience in thoracic anesthesia, although videolaryngoscopes can improve glottic exposure in patients with difficult airways, videolaryngoscope-guided DLT intubation can fail (82). Videolaryngoscope-guided SLT placement is familiar to most anaesthesiologists. In this situation, the first choice is to secure the airway with an SLT under videolaryngoscope guidance. Otherwise, the combined use of videolaryngoscopy and FOB can be used for SLT intubation (94). Therefore, we must now consider how to achieve lung isolation. In the following section, several strategies are considered for lung isolation after successful SLT insertion.
SLT Exchange for DLT Using an Airway Exchange Catheter
Airway exchange catheters (AECs) are an important airway-assisted tool for thoracic anesthesia. For patients with difficult airways who require one-lung ventilation, one commonly used option is to intubate with an SLT and then exchange it with a DLT over an AEC. If postoperative ventilation is necessary, the AEC is also used to exchange the DLT for an SLT.
Chen et al. (82) reported a case of an unanticipated difficult airway in which GlideScope-guided DLT intubation failed in two attempts, while the SLT was successfully inserted on the first attempt. The DLT was then successfully placed over an AEC under the guidance of GlideScope. Poon and Liu (84) described using an AEC alongside AWS-S100 guidance for DLT placement in two cases of difficult laryngoscopy. Although the tracheal tube guiding channel of the disposable rigid blade (PBlade) used in this study cannot accommodate DLTs, Airway Scope can guide bougies or AECs into the trachea and then railroad a DLT over them.
McLean et al. (95) reported a failure rate for exchanging an SLT with DLT of 40%. Tube impingement on the arytenoids or epiglottis is often encountered during the exchange of the DLT over an AEC. The fit of the AEC in the DLT is vital and should be checked before use (82). Further, videolaryngoscopy can be used to visualize the railroading process of the DLT over an AEC. It can also lift the supraglottic tissue to avoid resistance while advancing the DLT into the trachea. Mort and Braffett (96) compared conventional and videolaryngoscopes for ETT exchange in high-risk, difficult airways; they observed that videolaryngoscopy-based ETT exchange over an AEC provided efficient and timely ETT passage and fewer attempts due to improved glottic visualization.
Although McLean et al. (95) reported that the failure rate for postoperative DLT to SLT exchange was 0%, this result should be interpreted cautiously. If DLT placement is extremely difficult, it can be continued to maintain ventilation after surgery until the patient is fully awake. Suzuki et al. (97) reported that using two AECs reduced the risk of tube impingement into the trachea during DLT to SLT exchange.
SLT With BBs
Tube exchange has a failure risk not only from DLT to SLT, but also from SLT to DLT. This could also be associated with pneumothorax (95). It is more convenient to use BBs in such cases, another commonly used option for one-lung ventilation (98). BBs are advantageous when a DLT cannot be used, such as in pediatric patients undergoing thoracic surgery, in whom only nasotracheal intubation is possible, and patients with tracheal tumors or abnormalities. Another advantage is that BBs can provide a selective block of the pulmonary segment and postoperative tube exchange is unnecessary.
There are two methods for BB placement: intraluminal and extraluminal. Briefly, in intraluminal placement, the BB is typically inserted into the lumen of the SLT, along with an FOB to guide the BB to an optimal position. Thus, intraluminal placement of BBs requires a large SLT diameter. Intraluminal BB placement seems easy after SLT insertion, but it is difficult to control the BB and FOB simultaneously, even when a large tube is used (99).
Extraluminal BB placement has been described in adults and children (100, 101). Templeton et al. (99) reported that extraluminal BB placement was safe, adequate to excellent surgical exposure, and faster than intraluminal placement. However, it may be difficult to place the BB in cases of poor glottic exposure using the Macintosh laryngoscope. Recently, several reports described successful extraluminal BB and SLT placement via videolaryngoscopy (102, 103). As the BB is very thin and long, it is difficult to control the direction during extraluminal placement under videolaryngoscopy. A guiding tube can be self-made from a routine tracheal tube using an Airtraq videolaryngoscope (103). In children aged <2 years, a 5F Arndt BB was bent at a 35–45° angle at 1.5 cm proximal to the balloon when using Storz C-MAC (104). These tips are very useful for extraluminal BB placement under videolaryngoscopy.
The VivaSight™ SLT, in combination with a BB, is a new method for one-lung ventilation. VivaSight™ SLT is a new generation ETT that incorporates a high-resolution imaging camera and a light source at its tip. It has been reported for BB placement without the aid of FOB and can provide real-time and continuous monitoring of the BB position (105–107).
Rapid lung collapse with a BB is not associated with the type of device used but with the method of use (108). For example, when using an FIO2 of 1.0 before one-lung ventilation, an apnoeic period of 30–60 s at the time of the pleural incision by disconnection of the breathing circuit and transient deflation of the BB balloon results in rapid lung collapse (109).
SLT With Capnothorax
Traditionally, lung isolation offers excellent surgical exposure during thoracic surgery. However, some complications are associated with one-lung ventilation, such as hypoxemia, bronchoalveolar injury, and postoperative pulmonary complications (110, 111). SLT intubation and CO2 insufflation of artificial pneumothorax were introduced into thoracoscopy very early. In 1994, Wolfer et al. (112) studied the effects of CO2 insufflation on haemodynamic parameters during thoracoscopy and reported promising results. SLT intubation and CO2 insufflation have been previously described in various thoracoscopic procedures (113, 114), including thoracoscopic esophagectomy (115, 116), and have proven to be feasible, efficient, and safe. SLT intubation and CO2 insufflation can be an alternative to one-lung ventilation for minimally invasive thoracic surgery, particularly when expertise for DLT placement is unavailable or when an operation is very short and simple, such as pleural effusion drainage and pleural biopsies (117). Yeh and Hsu reported an alternative method to achieve lung isolation using artificial pneumothorax under spontaneous breathing with ETT placement in patients with limited mouth opening (118).
When dealing with unanticipated difficult airways, if videolaryngoscopy fails, a laryngeal mask airway or surgical airway can be considered to secure the airway (5). An SLT can be inserted via the intubating laryngeal mask airway, and then a BB can be used to achieve one-lung ventilation. Alternatively, a BB can be directly inserted via the laryngeal mask airway (119, 120). For patients with tracheostomy, shortened DLTs or BBs can be considered to achieve lung isolation (2, 121).
Conclusion
Videolaryngoscopy plays an important role in thoracic airway management. Either non-channeled or channeled videolaryngoscope is suitable for DLT intubation. It can improve glottis exposure and increase the success rate at the first attempt. However, it has no advantage in saving intubation time and increases the incidence of DLT mispositioning for patients with normal airways. Thus, it is not considered as the first choice for patients with anticipated normal airways. Current evidence does not indicate which videolaryngoscope is super to another one for DLT intubation. The choice of videolaryngoscope is based on individual experience, preference, and availability. For patients with difficult airways, videolaryngoscope provides multiple options to achieve one-lung ventilation. Due to the distinct advantages in glottic view, videolaryngoscope-guided DLT intubation is a primary and effective method. Nevertheless, it requires training, particularly for novices and anaesthesiologists with limited experience in videolaryngoscope-guided DLT intubation. In case of failure, videolaryngoscope-guided SLT intubation can be achieved because it is familiar to every anesthetist or combined with the aid of fibreoptic bronchoscopy. Placement of a DLT over an AEC, inserting a BB via an SLT, or capnothorax can be selected for lung isolation.
Author Contributions
WY and CZ: conception or design of the work. ML and WY: literature review and draft of the manuscript. CZ and AL: critical revision of the manuscript. WY: take responsibility for data integrity and accuracy of the data analysis. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by a grant from the National Natural Science Foundation of P.R. China (No. 82171228 to WY) and a grant from China National Key R&D Program (No. 2020YFC2009002 to AL).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Corso RM, De Fazio C, Ornigotti E, Maitan S, Piraccini E, Sorbello M. Incidence of difficult airway in thoracic anesthesia practice. Minerva Anestesiol. (2018) 84:1421–2. doi: 10.23736/S0375-9393.18.13079-3
2. Brodsky JB. Lung separation and the difficult airway. Br J Anaesth. (2009) 103(Suppl. 1):i66–75. doi: 10.1093/bja/aep262
3. Collins SR, Titus BJ, Campos JH, Blank RS. Lung isolation in the patient with a difficult airway. Anesth Analg. (2018) 126:1968–78. doi: 10.1213/ANE.0000000000002637
4. Apfelbaum JL, Hagberg CA, Connis RT, Abdelmalak BB, Agarkar M, Dutton RP, et al. 2022 American society of anesthesiologists practice guidelines for management of the difficult airway. Anesthesiology. (2022) 136:31–81. doi: 10.1097/ALN.0000000000004002
5. Frerk C, Mitchell VS, McNarry AF, Mendonca C, Bhagrath R, Patel A, et al. Difficult airway society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. (2015) 115:827–48. doi: 10.1093/bja/aev371
6. Huang P, Zhou R, Lu Z, Hang Y, Wang S, Huang Z. GlideScope(R) versus C-MAC(R)(D) videolaryngoscope versus Macintosh laryngoscope for double lumen endotracheal intubation in patients with predicted normal airways: a randomized, controlled, prospective trial. BMC Anesthesiol. (2020) 20:119. doi: 10.1186/s12871-020-01012-y
7. Yao WL, Wan L, Xu H, Qian W, Wang XR, Tian YK, et al. A comparison of the McGrath(R) Series 5 videolaryngoscope and Macintosh laryngoscope for double-lumen tracheal tube placement in patients with a good glottic view at direct laryngoscopy. Anaesthesia. (2015) 70:810–7. doi: 10.1111/anae.13040
8. Russell TM, Hormis A, Rotherham NHSFT. Should the Glidescope video laryngoscope be used first line for all oral intubations or only in those with a difficult airway? a review of current literature. J Perioper Pract. (2018) 28:322–33. doi: 10.1177/1750458918788985
9. Berkow LC, Morey TE, Urdaneta F. The technology of video laryngoscopy. Anesth Analg. (2018) 126:1527–34. doi: 10.1213/ANE.0000000000002490
10. Cooper RM, Pacey JA, Bishop MJ, McCluskey SA. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anaesth. (2005) 52:191–8. doi: 10.1007/BF03027728
11. Cooper RM. Use of a new videolaryngoscope (GlideScope) in the management of a difficult airway. Can J Anaesth. (2003) 50:611–3. doi: 10.1007/BF03018651
12. Lewis SR, Butler AR, Parker J, Cook TM, Schofield-Robinson OJ, Smith AF. Videolaryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation: a cochrane systematic review. Br J Anaesth. (2017) 119:369–83. doi: 10.1093/bja/aex228
13. Pieters BMA, Maas EHA, Knape JTA, van Zundert AAJ. Videolaryngoscopy vs. direct laryngoscopy use by experienced anaesthetists in patients with known difficult airways: a systematic review and meta-analysis. Anaesthesia. (2017) 72:1532–41. doi: 10.1111/anae.14057
14. Cordovani D, Russell T, Wee W, Suen A, Cooper RM. Measurement of forces applied using a Macintosh direct laryngoscope compared with a glidescope video laryngoscope in patients with predictors of difficult laryngoscopy: a randomised controlled trial. Eur J Anaesthesiol. (2019) 36:221–6. doi: 10.1097/EJA.0000000000000901
15. Russell T, Khan S, Elman J, Katznelson R, Cooper RM. Measurement of forces applied during Macintosh direct laryngoscopy compared with GlideScope(R) videolaryngoscopy. Anaesthesia. (2012) 67:626–31. doi: 10.1111/j.1365-2044.2012.07087.x
16. Maharaj CH, Higgins BD, Harte BH, Laffey JG. Evaluation of intubation using the Airtraq or Macintosh laryngoscope by anaesthetists in easy and simulated difficult laryngoscopy–a manikin study. Anaesthesia. (2006) 61:469–77. doi: 10.1111/j.1365-2044.2006.04547.x
17. Herbstreit F, Fassbender P, Haberl H, Kehren C, Peters J. Learning endotracheal intubation using a novel videolaryngoscope improves intubation skills of medical students. Anesth Analg. (2011) 113:586–90. doi: 10.1213/ANE.0b013e3182222a66
18. Aziz MF, Brambrink AM, Healy DW, Willett AW, Shanks A, Tremper T, et al. Success of intubation rescue techniques after failed direct laryngoscopy in adults: a retrospective comparative analysis from the multicenter perioperative outcomes group. Anesthesiology. (2016) 125:656–66. doi: 10.1097/ALN.0000000000001267
19. Aziz MF, Dillman D, Fu R, Brambrink AM. Comparative effectiveness of the C-MAC video laryngoscope versus direct laryngoscopy in the setting of the predicted difficult airway. Anesthesiology. (2012) 116:629–36. doi: 10.1097/ALN.0b013e318246ea34
20. Shippey B, Ray D, McKeown D. Use of the McGrath videolaryngoscope in the management of difficult and failed tracheal intubation. Br J Anaesth. (2008) 100:116–9. doi: 10.1093/bja/aem303
21. Howle R, Onwochei D, Harrison SL, Desai N. Comparison of videolaryngoscopy and direct laryngoscopy for tracheal intubation in obstetrics: a mixed-methods systematic review and meta-analysis. Can J Anaesth. (2021) 68:546–65. doi: 10.1007/s12630-020-01908-w
22. Fiadjoe JE, Kovatsis P. Videolaryngoscopes in pediatric anesthesia: what's new? Minerva Anestesiol. (2014) 80:76–82.
23. Jaber S, De Jong A, Pelosi P, Cabrini L, Reignier J, Lascarrou JB. Videolaryngoscopy in critically ill patients. Crit Care. (2019) 23:221. doi: 10.1186/s13054-019-2487-5
24. Jiang J, Ma DX Li B, Wu AS, Xue FS. Videolaryngoscopy versus direct laryngoscopy for nasotracheal intubation: a systematic review and meta-analysis of randomised controlled trials. J Clin Anesth. (2019) 52:6–16. doi: 10.1016/j.jclinane.2018.08.029
25. Alhomary M, Ramadan E, Curran E, Walsh SR. Videolaryngoscopy vs. fibreoptic bronchoscopy for awake tracheal intubation: a systematic review and meta-analysis. Anaesthesia. (2018) 73:1151–61. doi: 10.1111/anae.14299
26. Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice guidelines for management of the difficult airway: an updated report by the American society of anesthesiologists task force on management of the difficult airway. Anesthesiology. (2013) 118:251–70. doi: 10.1097/ALN.0b013e31827773b2
27. Agro F, Barzoi G, Montecchia F. Tracheal intubation using a Macintosh laryngoscope or a GlideScope in 15 patients with cervical spine immobilization. Br J Anaesth. (2003) 90:705–6. doi: 10.1093/bja/aeg560
28. Shippey B, Ray D, McKeown D. Case series: the McGrath videolaryngoscope–an initial clinical evaluation. Can J Anaesth. (2007) 54:307–13. doi: 10.1007/BF03022777
29. Cavus E, Neumann T, Doerges V, Moeller T, Scharf E, Wagner K, et al. First clinical evaluation of the C-MAC D-blade videolaryngoscope during routine and difficult intubation. Anesth Analg. (2011) 112:382–5. doi: 10.1213/ANE.0b013e31820553fb
30. Xue FS, Yang BQ, Liu YY, Li HX, Yang GZ. Current evidences for the use of uescope in airway management. Chin Med J. 2017) 130:1867–75. doi: 10.4103/0366-6999.211536
31. Akihisa Y, Maruyama K, Koyama Y, Yamada R, Ogura A, Andoh T. Comparison of intubation performance between the king vision and Macintosh laryngoscopes in novice personnel: a randomized, crossover manikin study. J Anesth. (2014) 28:51–7. doi: 10.1007/s00540-013-1666-9
32. Maharaj CH, O'Croinin D, Curley G, Harte BH, Laffey JG. A comparison of tracheal intubation using the airtraq or the Macintosh laryngoscope in routine airway management: a randomised, controlled clinical trial. Anaesthesia. (2006) 61:1093–9. doi: 10.1111/j.1365-2044.2006.04819.x
33. Dhonneur G, Ndoko S, Amathieu R, Housseini LE, Poncelet C, Tual L. Tracheal intubation using the Airtraq in morbid obese patients undergoing emergency cesarean delivery. Anesthesiology. (2007) 106:629–30. doi: 10.1097/00000542-200703000-00027
34. Suzuki A, Toyama Y, Katsumi N, Kunisawa T, Sasaki R, Hirota K, et al. The Pentax-AWS((R)) rigid indirect video laryngoscope: clinical assessment of performance in 320 cases. Anaesthesia. (2008) 63:641–7. doi: 10.1111/j.1365-2044.2008.05452.x
35. Murphy LD, Kovacs GJ, Reardon PM, Law JA. Comparison of the king vision video laryngoscope with the macintosh laryngoscope. J Emerg Med. (2014) 47:239–46. doi: 10.1016/j.jemermed.2014.02.008
36. McNarry AF, Patel A. The evolution of airway management - new concepts and conflicts with traditional practice. Br J Anaesth. (2017) 119:i154–66. doi: 10.1093/bja/aex385
37. Kaplan MB, Ward DS, Berci G. A new video laryngoscope-an aid to intubation and teaching. J Clin Anesth. (2002) 14:620–6. doi: 10.1016/S0952-8180(02)00457-9
38. Cavus E, Kieckhaefer J, Doerges V, Moeller T, Thee C, Wagner K. The C-MAC videolaryngoscope: first experiences with a new device for videolaryngoscopy-guided intubation. Anesth Analg. (2010) 110:473–7. doi: 10.1213/ANE.0b013e3181c5bce5
39. Lai HY, Chen IH, Chen A, Hwang FY, Lee Y. The use of the GlideScope for tracheal intubation in patients with ankylosing spondylitis. Br J Anaesth. (2006) 97:419–22. doi: 10.1093/bja/ael133
40. Hernandez AA, Wong DH. Using a Glidescope for intubation with a double lumen endotracheal tube. Can J Anaesth. (2005) 52:658–9. doi: 10.1007/BF03015787
41. Hsu HT, Chou SH, Wu PJ, Tseng KY, Kuo YW, Chou CY, et al. Comparison of the GlideScope(R) videolaryngoscope and the Macintosh laryngoscope for double-lumen tube intubation. Anaesthesia. (2012) 67:411–5. doi: 10.1111/j.1365-2044.2011.07049.x
42. Yao WL, Wang XR, Xu H, Zhang Y, Zhang CH. McGrath(®) series 5 videolaryngoscope evaluation for double-lumen tube intubation. Anaesthesia. (2014) 69:646–7. doi: 10.1111/anae.12720
43. Hirabayashi Y, Seo N. The Airtraq laryngoscope for placement of double-lumen endobronchial tube. Can J Anaesth. (2007) 54:955–7. doi: 10.1007/BF03026807
44. Chastel B, Perrier V, Germain A, Seramondi R, Roze H, Ouattara A. Usefulness of the Airtraq DL videolaryngoscope for placing a double-lumen tube. Anaesth Crit Care Pain Med. (2015) 34:89–93. doi: 10.1016/j.accpm.2014.06.004
45. Lin W, Li H, Liu W, Cao L, Tan H, Zhong Z, et al. randomised trial comparing the CEL-100 videolaryngoscope(TM) with the Macintosh laryngoscope blade for insertion of double-lumen tubes. Anaesthesia. (2012) 67:771–6. doi: 10.1111/j.1365-2044.2012.07137.x
46. Suzuki A, Kunisawa T, Iwasaki H. Double lumen tube placement with the pentax-airway scope. Can J Anaesth. (2007) 54:853–4. doi: 10.1007/BF03021719
47. Yamazaki T, Ohsumi H. The airway scope is a practical intubation device for a double-lumen tube during rapid-sequence induction. J Cardiothorac Vasc Anesth. (2009) 23:926. doi: 10.1053/j.jvca.2008.12.015
48. Shah SB, Bhargava AK, Hariharan U, Mittal AK, Goel N, Choudhary M, et al. Randomized clinical trial comparing the standard mcintosh laryngoscope and the C-Mac D blade video laryngoscope for double lumen tube insertion for one lung ventilation in onco surgical patients. Indian J Anaesth. (2016) 60:312–8. doi: 10.4103/0019-5049.181591
49. El-Tahan M, Doyle DJ, Khidr AM, Hassieb AG. Case report: double lumen tube insertion in a morbidly obese patient through the non-channelled blade of the king vision () videolaryngoscope. F1000Res. (2014) 3:129. doi: 10.12688/f1000research.4481.3
50. Yao WL, Zhang CH. Macintosh laryngoscopy for double-lumen tube placement - a reply. Anaesthesia. (2015) 70:1206–8. doi: 10.1111/anae.13227
51. Russell T, Slinger P, Roscoe A, McRae K, Van Rensburg A. A randomised controlled trial comparing the GlideScope((R)) and the Macintosh laryngoscope for double-lumen endobronchial intubation. Anaesthesia. (2013) 68:1253–8. doi: 10.1111/anae.12322
52. Bustamante S, Parra-Sanchez I, Apostolakis J. Sequential rotation to insert a left double-lumen endotracheal tube using the GlideScope. Can J Anaesth. (2010) 57:282–3. doi: 10.1007/s12630-009-9243-2
53. Jones PM, Turkstra TP, Armstrong KP, Armstrong PM, Cherry RA, Hoogstra J, et al. Effect of stylet angulation and endotracheal tube camber on time to intubation with the GlideScope. Can J Anaesth. (2007) 54:21–7. doi: 10.1007/BF03021895
54. Dupanovic M, Isaacson SA, Borovcanin Z, Jain S, Korten S, Karan S, et al. Clinical comparison of two stylet angles for orotracheal intubation with the GlideScope video laryngoscope. J Clin Anesth. (2010) 22:352–9. doi: 10.1016/j.jclinane.2009.10.008
55. Bussieres JS, Martel F, Somma J, Morin S, Gagne N. A customized stylet for GlideScope(R) insertion of double lumen tubes. Can J Anaesth. (2012) 59:424–5. doi: 10.1007/s12630-012-9671-2
56. Bussieres JS, Somma J, Rousseau A, Harvey L. Use of the GlideScope((R)) for double-lumen endobronchial intubation. Anaesthesia. (2014) 69:181–2. doi: 10.1111/anae.12581
57. Hsu HT, Chou SH, Chou CY, Tseng KY, Kuo YW, Chen MC, et al. A modified technique to improve the outcome of intubation with a left-sided double-lumen endobronchial tube. BMC Anesthesiol. (2014) 14:72. doi: 10.1186/1471-2253-14-72
58. Liu TT, Li L, Wan L, Zhang CH, Yao WL. Videolaryngoscopy vs. Macintosh laryngoscopy for double-lumen tube intubation in thoracic surgery: a systematic review and meta-analysis. Anaesthesia. (2018) 73:997–1007. doi: 10.1111/anae.14226
59. Ajimi J, Nishiyama J, Masuda R, Shibata T, Furuya H, Hosoi S, et al. Usefulness of the universal adapter for smartphones® in a Mannequin study. Tokai J Exp Clin Med. (2018) 43:139–42.
60. Ajimi J, Nishiyama J, Masuda R, Hosoi S, Sakamoto R, Murata T, et al. Successful intubation using the airtraq double lumen® with the universal adapter for smartphones® in a case of intubation difficulty. Tokai J Exp Clin Med. (2018) 43:143–7.
61. Ynineb Y, Boglietto E, Bonnet F, Quesnel C, Garnier M. Face-to-face double-lumen tube intubation with the airtraq video laryngoscope for emergency thoracic surgery: a case report. Semin Cardiothorac Vasc Anesth. (2022) 26:90–4. doi: 10.1177/10892532211007664
62. Yi J, Gong Y, Quan X, Huang Y. Comparison of the Airtraq laryngoscope and the GlideScope for double-lumen tube intubation in patients with predicted normal airways: a prospective randomized trial. BMC Anesthesiol. (2015) 15:58. doi: 10.1186/s12871-015-0037-5
63. Wan L, Liao M, Li L, Qian W, Hu R, Chen K, et al. McGrath Series 5 videolaryngoscope vs Airtraq DL videolaryngoscope for double-lumen tube intubation: a randomized trial. Medicine. (2016) 95:e5739. doi: 10.1097/MD.0000000000005739
64. El-Tahan MR, Khidr AM, Gaarour IS, Alshadwi SA, Alghamdi TM, Al'ghamdi A. A comparison of 3 videolaryngoscopes for double-lumen tube intubation in humans by users with mixed experience: a randomized controlled study. J Cardiothorac Vasc Anesth. (2018) 32:277–86. doi: 10.1053/j.jvca.2017.08.009
65. Bensghir M, Alaoui H, Azendour H, Drissi M, Elwali A, Meziane M, et al. Faster double-lumen tube intubation with the videolaryngoscope than with a standard laryngoscope. Can J Anaesth. (2010) 57:980–4. doi: 10.1007/s12630-010-9372-7
66. Yi J, Huang Y, Luo A. Comparison of glidescope video-laryngoscope and Macintosh laryngoscope for double-lumen tube intubation [Chinese]. Chin J Anesthesiol. (2013) 33:201–4. doi: 10.3760/cma.j.issn.0254-1416.2013.02.018
67. El-Tahan MR, Al'ghamdi AA, Khidr AM, Gaarour IS. Comparison of three videolaryngoscopes for double-lumen tubes intubation in simulated easy and difficult airways: a randomized trial. Minerva Anestesiol. (2016) 82:1050–8. doi: 10.1053/j.jvca.2016.03.069
68. Wei W, Tian M. Double-lumen tube intubation using video laryngoscopy causes a milder cardiovascular response compared to classic direct laryngoscopy. Pak J Med Sci. (2016) 32:35–9. doi: 10.12669/pjms.321.9044
69. Risse J, Schubert AK, Wiesmann T, Huelshoff A, Stay D, Zentgraf M, et al. Videolaryngoscopy versus direct laryngoscopy for double-lumen endotracheal tube intubation in thoracic surgery - a randomised controlled clinical trial. BMC Anesthesiol. (2020) 20:150. doi: 10.1186/s12871-020-01067-x
70. Kido H, Komasawa N, Matsunami S, Kusaka Y, Minami T. Comparison of McGRATH MAC and Macintosh laryngoscopes for double-lumen endotracheal tube intubation by anesthesia residents: a prospective randomized clinical trial. J Clin Anesth. (2015) 27:476–80. doi: 10.1016/j.jclinane.2015.05.011
71. Yoo JY, Park SY, Kim JY, Kim M, Haam SJ, Kim DH. Comparison of the McGrath videolaryngoscope and the Macintosh laryngoscope for double lumen endobronchial tube intubation in patients with manual in-line stabilization: a randomized controlled trial. Medicine. (2018) 97:e0081. doi: 10.1097/MD.0000000000010081
72. Bakshi SG, Gawri A, Divatia JV. McGrath MAC video laryngoscope versus direct laryngoscopy for the placement of double-lumen tubes: a randomised control trial. Indian J Anaesth. (2019) 63:456–61. doi: 10.4103/ija.IJA_48_19
73. Jiang Q, Zhang X, Xu M. Comparison the Airtraq and Macintosh laryngoscopes for placement of double-lumen endobranchial tube [Chinese]. J Clin Anesth. (2011) 27:870–2.
74. Wasem S, Lazarus M, Hain J, Festl J, Kranke P, Roewer N, et al. Comparison of the Airtraq and the Macintosh laryngoscope for double-lumen tube intubation: a randomised clinical trial. Eur J Anaesthesiol. (2013) 30:180–6. doi: 10.1097/EJA.0b013e32835fe574
75. Hamp T, Stumpner T, Grubhofer G, Ruetzler K, Thell R, Hager H. Haemodynamic response at double lumen bronchial tube placement - Airtraq vs. MacIntosh laryngoscope, a randomised controlled trial. Heart Lung Vessel. (2015) 7:54–63.
76. Feng M, Qiu J, Qian W, Wan L, Zhang C, Yao W. Effect-site concentration of remifentanil for inhibiting cardiovascular responses to double-lumen tube intubation with Airtraq videolaryngoscopy: a comparison with Macintosh laryngoscopy. J Clin Anesth. (2020) 60:97–8. doi: 10.1016/j.jclinane.2019.09.009
77. Purugganan RV, Jackson TA, Heir JS, Wang H, Cata JP. Video laryngoscopy versus direct laryngoscopy for double-lumen endotracheal tube intubation: a retrospective analysis. J Cardiothorac Vasc Anesth. (2012) 26:845–8. doi: 10.1053/j.jvca.2012.01.014
78. Kim YS, Song J, Lim BG, Lee IO, Won YJ. Different classes of videoscopes and direct laryngoscopes for double-lumen tube intubation in thoracic surgery: a systematic review and network meta-analysis. PLoS ONE. (2020) 15:e0238060. doi: 10.1371/journal.pone.0238060
79. Belze O, Lepage E, Bazin Y, Kerourin P, Fusciardi J, Remerand F, et al. Glidescope versus Airtraq DL for double-lumen tracheal tube insertion in patients with a predicted or known difficult airway: a randomised study. Eur J Anaesthesiol. (2017) 34:456–63. doi: 10.1097/EJA.0000000000000655
80. Ajimi J, Nishiyama J, Masuda R, Shibata T, Suzuki T. AWS-200 for double-lumen endotracheal tube intubation: a prospective randomized clinical trial. Tokai J Exp Clin Med. (2018) 43:161–7.
81. Chang JE, Kim H, Min SW, Lee JM, Ryu JH, Yoon S, et al. A randomized controlled trial comparing the utility of lighted stylet and glidescope for double-lumen endobronchial intubation. J Cardiothorac Vasc Anesth. (2018) 32:290–6. doi: 10.1053/j.jvca.2017.10.009
82. Chen A, Lai HY, Lin PC, Chen TY, Shyr MH. GlideScope-assisted double-lumen endobronchial tube placement in a patient with an unanticipated difficult airway. J Cardiothorac Vasc Anesth. (2008) 22:170–2. doi: 10.1053/j.jvca.2007.04.006
83. Onrubia X, Lluch-Oltra A, Armero R, Baldo J. Use of GlideScope for double lumen endotracheal tube insertion in an awake patient with difficult airway. Rev Esp Anestesiol Reanim. (2014) 61:346–8. doi: 10.1016/j.redar.2013.05.010
84. Poon KH, Liu EH. The airway scope for difficult double-lumen tube intubation. J Clin Anesth. (2008) 20:319. doi: 10.1016/j.jclinane.2008.02.003
85. Sano H, Komasawa N, Minami T. Efficacy of the Pentax-AWS Airwayscope with a newly developed Intlock for a double-lumen tracheal tube. J Clin Anesth. (2016) 34:373–4. doi: 10.1016/j.jclinane.2016.05.032
86. Salazar Herbozo E, Planas A, Ramasco F, Gómez Rice A, Catalán P. Double lumen tube insertion in awake patients through the AirTraq laryngoscope in 2 cases of expected difficult airway. Rev Esp Anestesiol Reanim. (2011) 58:315–7. doi: 10.1016/S0034-9356(11)70068-8
87. Imajo Y, Komasawa N, Minami T. Efficacy of bronchofiberscope double-lumen tracheal tube intubation combined with McGRATH MAC for difficult airway. J Clin Anesth. (2015) 27:362. doi: 10.1016/j.jclinane.2015.03.012
88. Goh QY, Kong A. Videolaryngoscope-assisted double-lumen endotracheal tube intubation in an awake patient with known difficult airway and bronchopleural fistula: a case report. A A Pract. (2020) 14:e01186. doi: 10.1213/XAA.0000000000001186
89. Lin WQ, Quan SB, Liu WJ, Zhang TH, Li HT, Zhong ZJ, et al. Evaluation of the CEL-100 videolaryngoscope(TM) for double-lumen tracheal tube insertion after failure using the Macintosh laryngoscope. Anaesthesia. (2012) 67:1232–6. doi: 10.1111/j.1365-2044.2012.07261.x
90. Lai HC, Wu ZF. Easier double-lumen tube placement using real-time video laryngoscopy and wireless video fiberoptic bronchoscopy. J Clin Anesth. (2019) 55:132–3. doi: 10.1016/j.jclinane.2018.12.023
91. Kim YR, Jun BH, Kim JA. The use of the clarus video system for double-lumen endobronchial tube intubation in a patient with a difficult airway. Korean J Anesthesiol. (2013) 65:85–6. doi: 10.4097/kjae.2013.65.1.85
92. Subramani S, Poopalalingam R. Bonfils assisted double lumen endobronchial tube placement in an anticipated difficult airway. J Anaesthesiol Clin Pharmacol. (2014) 30:568–70. doi: 10.4103/0970-9185.142867
93. Seo H, Lee G, Ha SI, Song JG. An awake double lumen endotracheal tube intubation using the clarus video system in a patient with an epiglottic cyst: a case report. Korean J Anesthesiol. (2014) 66:157–9. doi: 10.4097/kjae.2014.66.2.157
94. Sharma D, Kim LJ, Ghodke B. Successful airway management with combined use of Glidescope videolaryngoscope and fiberoptic bronchoscope in a patient with cowden syndrome. Anesthesiology. (2010) 113:253–5. doi: 10.1097/ALN.0b013e3181dfd334
95. McLean S, Lanam CR, Benedict W, Kirkpatrick N, Kheterpal S, Ramachandran SK. Airway exchange failure and complications with the use of the cook airway exchange catheter(R): a single center cohort study of 1177 patients. Anesth Analg. (2013) 117:1325–7. doi: 10.1213/ANE.0b013e3182a7cd3d
96. Mort TC, Braffett BH. Conventional versus video laryngoscopy for tracheal tube exchange: glottic visualization, success rates, complications, and rescue alternatives in the high-risk difficult airway patient. Anesth Analg. (2015) 121:440–8. doi: 10.1213/ANE.0000000000000825
97. Suzuki A, Uraoka M, Kimura K, Sato S. Effects of using two airway exchange catheters on laryngeal passage during change from a double-lumen tracheal tube to a single-lumen tracheal tube. Br J Anaesth. (2007) 99:440–3. doi: 10.1093/bja/aem183
98. Campos JH. An update on bronchial blockers during lung separation techniques in adults. Anesth Analg. (2003) 97:1266–74. doi: 10.1213/01.ANE.0000085301.87286.59
99. Templeton TW, Morris BN, Goenaga-Diaz EJ, Forest DJ, Hadley R, Moore BA, et al. A prospective comparison of intraluminal and extraluminal placement of the 9-french arndt bronchial blocker in adult thoracic surgery patients. J Cardiothorac Vasc Anesth. (2017) 31:1335–40. doi: 10.1053/j.jvca.2017.02.188
100. Sekhon AP, Nishiguchi BK, Maldonado Y, Harter RL. Extraluminal placement of an arndt bronchial blocker through a tracheal stoma. J Cardiothorac Vasc Anesth. (2016) 30:e14–5. doi: 10.1053/j.jvca.2015.09.020
101. Stephenson LL, Seefelder C. Routine extraluminal use of the 5F arndt endobronchial blocker for one-lung ventilation in children up to 24 months of age. J Cardiothorac Vasc Anesth. (2011) 25:683–6. doi: 10.1053/j.jvca.2010.04.020
102. Liu Z, Yang X, Jia Q. One-lung ventilation in a patient with a large mass on the glottis: a case report. Medicine. (2018) 97:e12237. doi: 10.1097/MD.0000000000012237
103. Yao W, Qiu J, Wan L, Zhang C. A modified method of extraluminal placement of the 9 Fr arndt bronchial blocker guided by airtraq videolaryngoscopy in adult thoracic surgery. J Cardiothorac Vasc Anesth. (2019) 33:1173–5. doi: 10.1053/j.jvca.2018.10.029
104. Templeton TW, Downard MG, Simpson CR, Zeller KA, Templeton LB, Bryan YF. Bending the rules: a novel approach to placement and retrospective experience with the 5 french arndt endobronchial blocker in children <2 years. Paediatr Anaesth. (2016) 26:512–20. doi: 10.1111/pan.12882
105. Qiu J, Feng M, Zhang C, Yao W. VivaSight™ single-lumen tube guided bronchial blocker placement for one-lung ventilation in a patient with a tracheal tumor under video-assisted transthoracic surgery: a case report. BMC Anesthesiol. (2019) 19:2. doi: 10.1186/s12871-018-0677-3
106. Moritz A, Schreiner W, Schmidt J. One-lung ventilation after rapid-sequence intubation: a novel approach using an ETView tracheoscopic ventilation tube for placement of an EZ-Blocker without bronchoscopy. J Clin Anesth. (2016) 29:48–9. doi: 10.1016/j.jclinane.2015.10.013
107. Granell Gil M, Solís Albamonte P, Córdova Hernández C, Cobo I, Guijarro R, de Andrés Ibañez JA. Intubation in two patients with difficult airway management and tracheal stenosis after tracheostomy in thoracic surgery. Rev Esp Anestesiol Reanim. (2018) 65:347–50. doi: 10.1016/j.redar.2017.12.013
108. Grocott HP. Optimizing lung collapse with a bronchial blocker: it's not what you use, but how you use it. J Cardiothorac Vasc Anesth. (2018) 32:e93–4. doi: 10.1053/j.jvca.2018.03.006
109. Bussieres JS, Moreault O, Couture EJ, Provencher S. Optimizing lung collapse with a bronchial blocker: it's not what you use, but how you use it, part II. J Cardiothorac Vasc Anesth. (2019) 33:255. doi: 10.1053/j.jvca.2018.09.025
110. Blank RS, Colquhoun DA, Durieux ME, Kozower BD, McMurry TL, Bender SP, et al. Management of one-lung ventilation: impact of tidal volume on complications after thoracic surgery. Anesthesiology. (2016) 124:1286–95. doi: 10.1097/ALN.0000000000001100
111. Lohser J, Slinger P. Lung injury after one-lung ventilation: a review of the pathophysiologic mechanisms affecting the ventilated and the collapsed lung. Anesth Analg. (2015) 121:302–18. doi: 10.1213/ANE.0000000000000808
112. Wolfer RS, Krasna MJ, Hasnain JU, McLaughlin JS. Hemodynamic effects of carbon dioxide insufflation during thoracoscopy. Ann Thorac Surg. (1994) 58:407–8. doi: 10.1016/0003-4975(94)92215-2
113. Caso R, Kelly CH, Marshall MB. Single lumen endotracheal intubation with carbon dioxide insufflation for lung isolation in thoracic surgery. Surg Endosc. (2019) 33:3287–90. doi: 10.1007/s00464-018-06614-9
114. Sancheti MS, Dewan BP, Pickens A, Fernandez FG, Miller DL, Force SD. Thoracoscopy without lung isolation utilizing single lumen endotracheal tube intubation and carbon dioxide insufflation. Ann Thorac Surg. (2013) 96:439–44. doi: 10.1016/j.athoracsur.2013.04.060
115. Ninomiya I, Okamoto K, Fushida S, Oyama K, Kinoshita J, Takamura H, et al. Efficacy of CO2 insufflation during thoracoscopic esophagectomy in the left lateral position. Gen Thorac Cardiovasc Surg. (2017) 65:587–93. doi: 10.1007/s11748-017-0816-7
116. Lin M, Shen Y, Feng M, Tan L. Is two lung ventilation with artificial pneumothorax a better choice than one lung ventilation in minimally invasive esophagectomy? J Thorac Dis. (2019) 11:S707–12. doi: 10.21037/jtd.2018.12.08
117. Cerfolio RJ, Bryant AS, Sheils TM, Bass CS, Bartolucci AA. Video-assisted thoracoscopic surgery using single-lumen endotracheal tube anesthesia. Chest. (2004) 126:281–5. doi: 10.1378/chest.126.1.281
118. Yeh PH, Hsu PK. An alternative method to achieve one-lung ventilation by surgical pneumothorax in difficult lung isolation patient: a case report. J Anesth. (2016) 30:328–30. doi: 10.1007/s00540-015-2125-6
119. Sawasdiwipachai P, Boonsri S, Suksompong S, Prowpan P. The uses of laryngeal mask airway ProSeal and endobronchial blocker for one lung anesthesia. J Anesth. (2015) 29:660–5. doi: 10.1007/s00540-015-2004-1
120. Nakanishi T, Toriumi T. A novel method to overcome technical problems with a combination of laryngeal mask airway and bronchial blocker in thoracic surgery. J Cardiothorac Vasc Anesth. (2021) 35:3453–4. doi: 10.1053/j.jvca.2021.02.063
Keywords: videolaryngoscope, one-lung ventilation, double-lumen tube, bronchial blocker, difficult airways
Citation: Yao W, Li M, Zhang C and Luo A (2022) Recent Advances in Videolaryngoscopy for One-Lung Ventilation in Thoracic Anesthesia: A Narrative Review. Front. Med. 9:822646. doi: 10.3389/fmed.2022.822646
Received: 26 November 2021; Accepted: 17 May 2022;
Published: 13 June 2022.
Edited by:
Ata Murat Kaynar, University of Pittsburgh, United StatesReviewed by:
Antonella Cotoia, University of Foggia, ItalyJakob Wittenstein, University Hospital Carl Gustav Carus, Germany
Rakesh Garg, All India Institute of Medical Sciences, India
Copyright © 2022 Yao, Li, Zhang and Luo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenlong Yao, d2x5YW84MkAxMjYuY29t
 Wenlong Yao
Wenlong Yao Meihong Li
Meihong Li Ailin Luo
Ailin Luo