- 1Departments of Medicine and Geriatrics, University of Montreal, Montreal QC, Canada
- 2Research Center of the Geriatric University Institute of Montreal, Montreal QC, Canada
- 3Division of Geriatric Medicine, Department of Medicine, Sir Mortimer B. Davis Jewish General Hospital and Lady Davis Institute for Medical Research, McGill University, Montreal QC, Canada
- 4Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore, Singapore
- 5Education and Wellness Department of the Montreal Museum of Fine Arts, Montreal, QC, Canada
- 6Faculty of Arts and Science, Concordia University, Montreal, QC, Canada
Background: Museums can be instrumental in fostering social inclusion and may improve the overall health of the older population. Over the course of the 2019 coronavirus pandemic, many older adults suffered as a result of confinement measures, which may have accelerated the processes that lead to physical frailty and increased mental health risks. This study aims to examine whether a 3-month cycle of weekly virtual tours of the Montreal Museum of Fine Arts (MMFA) may have improved feelings of social inclusion, wellbeing and quality of life, and reduced physical frailty in older adults living within the community of Montreal.
Methods and design: A total of 106 older adults, who were community-dwellers living in Montreal (Quebec, Canada), were recruited for a randomized controlled trial in two parallel groups (intervention with n = 53 vs control with n = 53) between January and April 2022. The intervention consisted of a 3-month cycle of weekly virtual museum tours of the MMFA. Social isolation, wellbeing, quality of life and frailty were evaluated using validated scales that were assessed on a web platform at baseline (M0) and after 3 months (M3) in the intervention group. The control group completed the same assessment according to the same schedule. The outcomes were the mean scores at M0 and M3, and changes in mean scores between M0 and M3.
Results: The intervention group showed significant improvements in their social isolation, wellbeing, quality of life and frailty scores when compared to the control group, the highest benefits being observed with frailty.
Conclusion: The results suggest that the 3-month cycle of weekly virtual MMFA tours may improve social inclusion, physical and mental health in community-dwelling older adults living in Montreal.
Trial registration: https://clinicaltrials.gov/ct2/show/NCT05046288, identifier NCT05046288.
Background
Over the past 2 years of the coronavirus disease 2019 (COVID-19) pandemic (1), physical distancing was deployed as a preventive public health measure to reduce the transmission of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This physical distancing had at least two unintended consequences for older adults. First, these measures often deprived older people of face-to-face access to social activities and social networks, which often led to an increase in their social isolation (2). Second, in many countries, such as Canada, there was an increased demand for access to the health care system and community resources, which could not always be met (3, 4). This combination of an increase in social isolation and increased pressure on the healthcare system and community organizations often led to a degradation in physical and mental health, making older adults frail and increasing their risk of adverse outcomes (5). For instance, research suggests that older adults who experience social isolation are at a greater risk for incident morbidities, which can contribute to greater physical frailty and even premature death (5, 6). Conversely, physical frailty itself may also increase social isolation (5). Moreover, it has been demonstrated that older adults' wellbeing and quality of life are impacted negatively by both social isolation and physical frailty (5–8). This highlights the need for innovative interventions that promote the social inclusion of older adults, especially in the wake of 2 years of the COVID-19 pandemic.
Systematic reviews of quantitative studies have attempted to evaluate the effectiveness of interventions designed to increase the social inclusion, and sense of connectedness, of older adults experiencing social isolation (8–15). Due to the heterogeneity of interventions and their results, to date, there has been no conclusive evidence on the effectiveness of specific strategies to increase social inclusion in this population.
Further research is required to determine what “works” to improve social inclusion. These systematic reviews do, however, point to three key characteristics of effective interventions. First, group activities have a greater effect than those performed alone (8–12). Second, engaging participants in goal-oriented endeavors, rather than in passive activities with no explicit purpose, appears to be more effective in increasing feelings of social inclusion (12–15). Third, activities that include a creative component (such as arts-based activities) evoke positive emotions that are beneficial (15). Moreover, cultural interventions predicated on any type of arts-based activity have been shown to have beneficial effects that may improve people's quality of life (16, 17).
A socially-inclusive society enables all to remain engaged in collective daily life for as long as possible as they age (18). The concept of social inclusion implies on-going, meaningful participation in society. Providing occasions and places where individuals may participate in shared activities are key attributes of an inclusive society. Because they offer a variety of opportunities to participate meaningfully in arts-based group activities - from guided tours to lectures and workshops - museums may fulfill such a role, fostering a sense of social inclusion. Indeed, the potential of museums to improve the social inclusion of older adults experiencing social isolation has been demonstrated in a British study on “museums as spaces for wellbeing.”1 Since 2015, a participatory, arts-based workshop series has been offered by the Montreal Museum of Fine Arts (MMFA, Montreal, Quebec, Canada) (19). In an examination of this program, it was demonstrated that an intervention involving art creation in a group setting at the MMFA improved the wellbeing, quality of life and health condition of community-dwelling older adults in Montreal (19). Building on this initial study, in 2019, we then co-developed an arts-based activity with the MMFA, consisting of weekly guided tours carried out over a 3-month cycle. Because of physical distancing requirements during the COVID-19 pandemic, these guided tours were adapted into virtual guided tours. The impacts and effects of such virtual tours on older adults experiencing social isolation had never been examined. We hypothesized that weekly virtual MMFA tours could reduce social isolation and improve the wellbeing, quality of life and health condition, including the physical frailty, of older adults living in Montreal. This study thus aims to examine whether a 3-month cycle of weekly virtual tours of the MMFA may have improved feelings of social inclusion, wellbeing and quality of life, and reduced physical frailty in older adults living within the community of Montreal.
Methods
Design
The study was a uni-center (Center Intégré Universitaire de Santé et des Services Sociaux du Center-Sud-de-l'ile-de-Montréal, Quebec, Canada) randomized controlled trial (RCT) in two parallel groups (i.e., intervention group, which participated in virtual MMFA tours vs control group, which did not participate in virtual MMFA tours). The control group participants were asked to avoid participation in any arts-based activity 3 months ahead of the study and over the 3-month period of the study itself. Participants were aware of the intervention, and therefore not “blinded” due to the nature of the intervention, which required their explicit commitment to a 3-month cycle of weekly virtual MMFA tours. All staff members of the research team involved in the RCT phases (i.e., recruitment, assessment, and follow-up) were blinded to the allocation of intervention, except one staff member who was responsible for the randomization list. Participants were randomly allocated into intervention and control groups by block randomization with block sizes of 1:1. Randomization lists were established using the N'Query randomization software. This RCT is registered on the ClinicalTrials.gov website (project number NCT05046288) and followed the CONSORT guidelines for RCTs (20).
Population
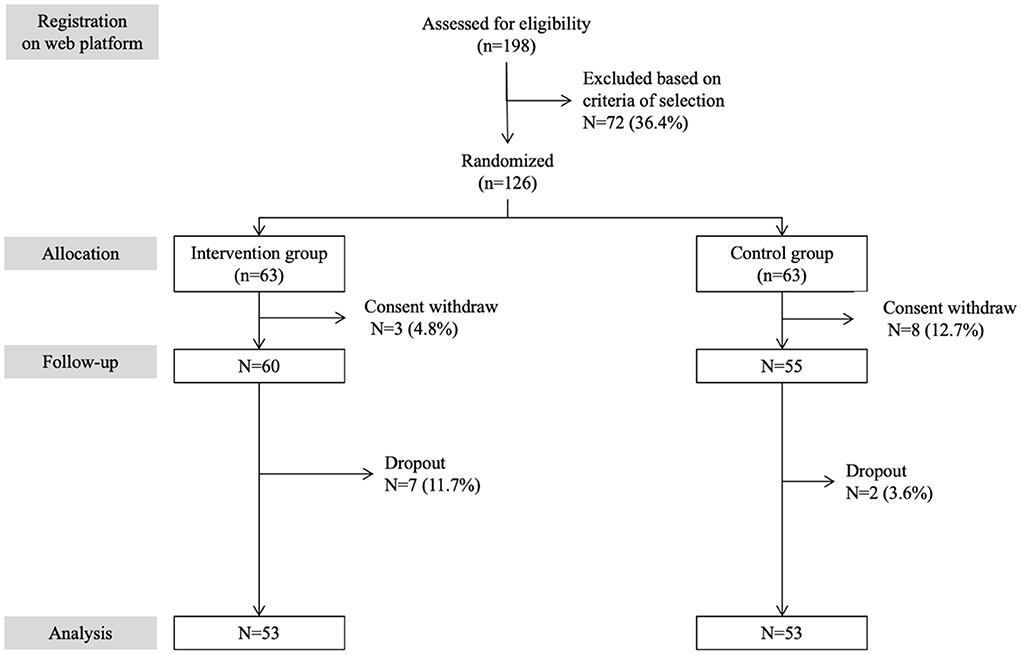
A total of 106 participants were enrolled and completed the full study between January and April of 2022. The inclusion criteria were as follows: aged 65 and over with a life expectancy over 6 months (according to a free software that incorporates socio-demographic, cardio-vascular risk factors, physical activity and income characteristics)2, experiencing social isolation as defined by the 11-item Duke Social Support Index (DSSI) score ≤ 28/33 (see footnote 1), living at home in the urban area of Montreal (Quebec, Canada), able to communicate and write in the language of the recruitment center (i.e., French, English or Chinese) and able to consent to participate in the study. The participants were screened using information provided by community associations in Montreal. They were informed that a clinical study on the effects of weekly virtual MMFA tours on social inclusion, wellbeing, quality of life and health condition was launched by the MMFA in partnership with the Research Center of the Geriatric University Institute of Montreal (CRIUGM; Montreal, Quebec, Canada) and that the MMFA and CRIUGM were recruiting participants. Potential participants registered via their neighborhood associations on the CRIUGM website. If they needed more information on the study, they had the option of calling someone at the CRIUGM. A total of 198 individuals registered on the web platform. They were contacted by a staff member of the research team for an interview by phone. During this phone call, the objective of the study and its procedures were explained and the selection criteria for participants were validated. Following these calls, 72 (36.4%) of potential participants were excluded because of the selection criteria and 126 (63.6%) individuals were enrolled, signed the consent form, and randomized into intervention (n = 63) and control (n = 63) groups. Among them, 11 (8.7%; 3 in the intervention and 8 in the control group) withdrew their consent before the baseline assessment. In total, 115 (91.3%) participants (60 in the intervention group and 55 in the control group) underwent the full baseline assessment. Seven (6.1%) participants in the intervention group and 2 (1.7%) in the control group dropped out over the 3-month period of the study. There was no significant difference in baseline characteristics between the group of participants who withdrew their consent and dropped out, and the group of those who completed the study (data not shown). Figure 1 shows a flow diagram detailing participant selection and follow-up in the RCT.
Intervention
The intervention consisted of a 3-month cycle of weekly virtual MMFA guided tours. Each visit was performed with a group of 6 to 8 participants and a trained guide, for a total of 8 groups. Participants met once a week over the 3-month period and participated in a 45-minute virtual guided tour via the videoconferencing platform Zoom, using their own digital device. An additional 15-minute period dedicated to informal discussion (to allow for more socializing) was proposed after each tour (this extra discussion time was optional).
Regardless of the topics or the themes covered, each visit was standardized and separated into three consecutive phases: presentation of the visit objectives, a dialogic-style tour with trained museum guides, and an open-ended discussion after the tour. The tour content consisted of a combination of images of artworks (e.g., paintings, sculpture, decorative pieces), live discussions animated by the tour guides, ancillary information on the artworks or artists from tour guides, and pre-recorded videos about specific works or artists. The amount and difficulty of information presented to participants was increased each month over the 3-month cycle of guided museum tours.
Each weekly guided tour was unique and led by a single museum guide. One guide was assigned to each group of 8 participants for all 12 visits. Additionally, one member of the research team was assigned to each group to oversee the research components of the tour, participate in a virtual ethnography, manage participants' potential technical issues (e.g., difficulties connecting to the Zoom meeting, issues with sound, display) and assist in the presentation of the visual content (images and videos).
Assessment
Baseline assessment
The baseline assessment was performed at participants' place of living via a web platform using standardized procedures and digital questionnaires before (M0) the first tour with support by phone if needed. Both the intervention and control groups performed the baseline assessment. The participants' socio-demographic characteristics (i.e., age, sex, ethnicity, place of living) were recorded. Social isolation was assessed using the 11-item Duke Social Support Index (DSSI) (21). The index comprises two subscales: social interaction (i.e., frequency of interactions) and subjective support (i.e., satisfaction with emotional support provided). DSSI scores range from 11 to 33, with higher scores indicating higher levels of social inclusion. Wellbeing was assessed using the Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS) self-administered questionnaire (22), which is composed of 14 positively-worded items and produces scores ranging from 14 (i.e., none of the time) to 70 (i.e., all the time). EuroQol-5D (EQ-5D) was used to assess health-related quality of life (23). This tool is composed of a questionnaire examining physical health issues, with scores ranging from 0 (i.e., no issue) to 25 (i.e., worst issues), and a visual analog scale (VAS) assessing self-perceived health, ranging from 0 (i.e., worst health imaginable) to 100 (i.e., best health imaginable). Physical and mental frailty was assessed using the Center of Excellence Self-AdMinistered questionnaire (CESAM) (19, 24). Using 20 close-ended questions, CESAM examines different subdomains of mental and physical health: weight loss; polypharmacy (i.e., number of therapeutic classes taken on a daily basis ≥ 5); vision, hearing and memory problems; home support; activities of daily living (ADL) and instrumental activities of daily living (IADL) (25, 26); mood; practice of regular physical activity; and history of falls in the past 12 months. CESAM was filled out by the participants themselves under the supervision of Principal Investigator representatives. The total health frailty score ranges from 0 (i.e., best health condition) to 18 (i.e., worst health condition).
Follow-up assessments
DSSI, WEMWBS, EQ-5D and CESAM questionnaires were repeated after the twelfth (M3) tour in intervention and control groups. Like the baseline assessment, all questionnaires were completed online at participants' place of living with support by phone if needed. After the M3 assessment, the participants in the control group were offered a complimentary virtual MMFA tour to compensate them for their compliance and restraint from art and museum-going activities during the period of the study.
Outcome measures
The primary outcome was captured by the DSSI score. The secondary outcomes were captured by the scores of WEMWBS, EQ-5D and CESAM. For each outcome, the mean score at M0 and M3, and changes in mean score between M0 and M3 {using the formula [(score M3 – score M0) / (score M3 + score M0) /2] × 100} were used (19).
Ethical considerations
Participants were included after giving written, informed consent for research. The study was approved by the CIUSSS Center-Sud-de-l'Île-de-Montréal (Quebec, Canada) Research Ethics Committee (# 2022-1338 – CÉR VN 21-22-08).
Statistics
Means, standard deviations (SD), frequencies and percentages are used to describe participants' characteristics. Inter- and intra-group comparisons were performed using unpaired or paired t-tests, and Chi-squared tests, as appropriate. Multiple linear regressions were used to examine the association between variations of each questionnaire's score (used as dependent variables with separated models for each score) and the intervention (used as independent variables), were adjusted according to participants' baseline characteristics. P-values less than 0.05 were considered statistically significant for linear regressions. All statistics were performed using SPSS (version 23.0; SPSS, Inc., Chicago, IL).
Results
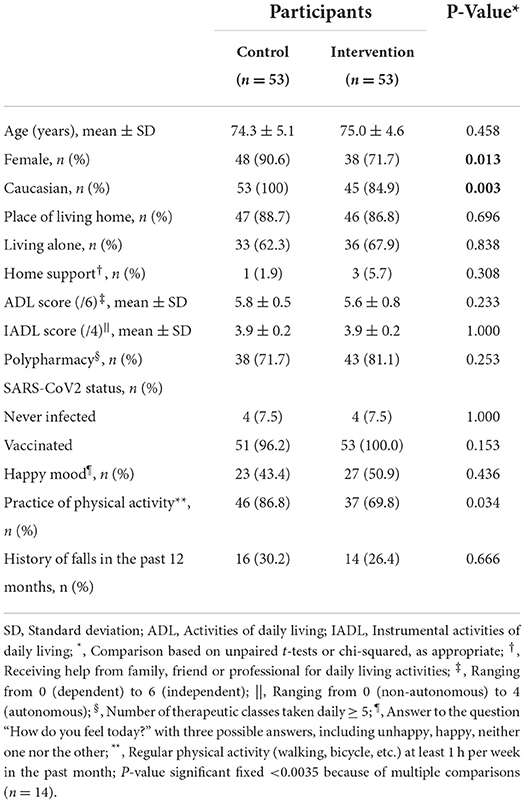
As shown in Table 1, there was no significant difference between groups for participants' baseline characteristics, except for sex and ethnicity. There were fewer females and Caucasians in the intervention group compared to the control group (P ≤ 0.013). There were significant greater mean scores for DSSI, EQ-5D and CESAM (P ≤ 0.001) at M3 compared to M0 in the intervention group (Table 2). There was only a trend (P = 0.059) for greater WEMWBS mean scores in the intervention group. No significant change in all scales' scores between M0 and M3 was found in the control group. Inter-group comparisons showed that DSSI, WEMWBS, EQ-5D and CESAM mean scores were significantly higher in the intervention group compared to the control group at M3 (P < 0.033), while significant difference was found at M0. Table 3 shows that participation in weekly virtual MMFA tours was significantly associated with improvements in all scales (P ≤ 0.012).
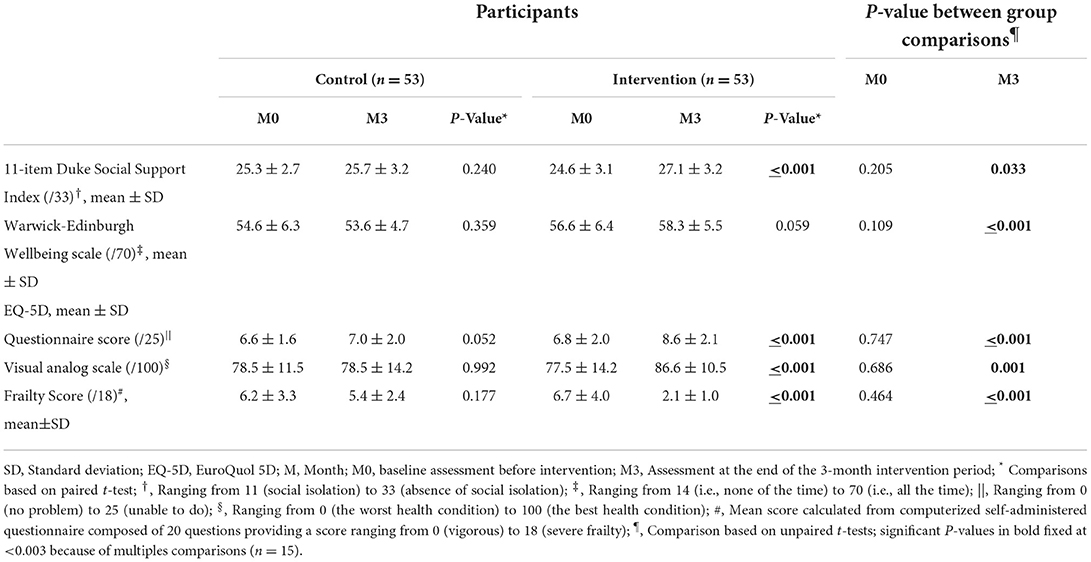
Table 2. Comparisons of mean values of scales assessing social isolation, wellbeing, quality of life and frailty between control and intervention groups (n = 106).
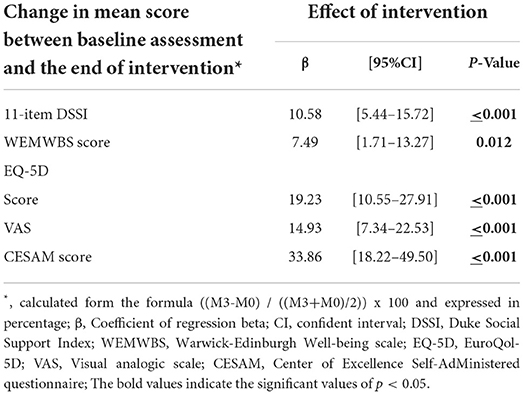
Table 3. Multiple linear regressions showing the association of intervention (i.e., 3-month period of virtual guided tour, independent variable) and changes in mean score between baseline assessment and end of intervention for 11-item Duke Social Support Index, Warwick-Edinburgh Wellbeing scale, EuroQol-5D and Center of Excellence Self-AdMinistered questionnaire scores adjusted for baseline participant's characteristics (n = 106).
Discussion
The findings of this RCT show that the 3-month cycle of weekly virtual MMFA tours had multidimensional benefits in participating older adults. Social isolation decreased and both physical and mental health improved significantly.
The decrease in social isolation reported in our study is consistent with the results of previous studies, which have shown that arts-based activities can reduce social isolation, and that these interventions are most effective when they are practiced in a group setting and actively engage participants (10–13). In addition, a meta-analysis previously demonstrated that interventions that focus on changing a person's perceptions and that stimulate positive emotions are more beneficial than those that focus on building social ties (15). Furthermore, interventions involving cultural activities, such as the visual arts, regardless of artistic genre or type of activity, have demonstrable benefits including the generation of positive emotions, which have been shown to improve wellbeing, self-esteem and quality of life (16, 17). We suggest that it is for all these reasons that we observed significant social and health benefits in our RCT.
Social isolation is a major problem in Canadian society. The proportion of Canadians aged 65 and over who report experiencing social isolation is high: in 2018, it was estimated to be around 20% of the older population, representing 1.5 million people (27, 28). Social isolation in combination with health challenges, which are often prevalent as we age, expose older individuals and the wider community to a variety of adverse outcomes with deleterious effects (5, 6). For instance, lack of contact between members of a family or within society may hamper or break down intergenerational relationships, increasing feelings of social isolation (29, 30). The physical and mental health issues known to arise as a result of social isolation may increase people's needs for health and social services, which puts pressure on those who work in these systems. This may in turn increase service expenditures (5, 6). Indeed, in 2016, the International Federation on Aging reported that “the main new problem facing seniors in Canada is maintaining their social contacts and activities” (31). This highlights the need for effective interventions that promote the social inclusion of older adults before they experience social isolation. The 3-month cycle of weekly virtual MMFA tours examined in our study seems to be one example of an intervention that effectively created social connection, the opposite of social isolation.
Many museums offer participatory arts-based activities (19, 32–37). The United Kingdom was one of the first countries to consider museums as partners in social and health policy. This gave rise to a consortium known as National Alliance for Museums, Health and Wellbeing, “(2015-2018), which became a driving force in the British Ministry of Health and Social Services 1 and is now known as the Culture, Health and Wellbeing Alliance. The interventions offered in British museums are most often interactive and participatory group activities 1. In the same period in Canada, the MMFA began developing participatory, arts-based activities in 2015 (19). Like their British counterparts, the MMFA focused on participatory, art-making workshops, for which improvements in the quality of life and wellbeing of community-dwelling older adults, as well as a reduction in their physical frailty, were reported (19, 31, 32). Our RCT reproduces and confirms previous studies that demonstrate the benefits of thoughtful, interactive, participatory arts-based programming on the physical and mental health of older adults interested in art and culture. The observation that arts-based activities can be beneficial to physical and mental health is not a new one, as exemplified by the field of art therapy (32–35). Improvements in wellbeing and quality of life have been reported in patients with cancer, neuropsychiatric diseases, or physical disabilities (32, 35). Unlike previous studies, this investigation of the MMFA and the guided tours that they developed during the COVID-19 pandemic is the first time, to the best of our knowledge, that these benefits have been documented and reported on virtual museum tours. Taken together, these findings suggest that arts-based activities, even when delivered online, retain their health benefits for older adults. A causal explanation of these complex health benefits is likely attributable to the dynamic interaction between wellbeing, health-related quality of life and physical health. Indeed, a sequence of health benefits has been suggested in previous studies (19). To summarize, the positive experiences engendered by arts-based activities delivered online may improve wellbeing, which improves quality of life and finally, physical and mental health when they incorporate into this virtual environment the principles mentioned previously: an emphasis on group activities; goal-oriented, purposive endeavors; and activities with a creative component.
The RCT design and the standardization of the 3-month cycle of weekly virtual MMFA tours were the main strengths of our study. However, some limitations need to be considered. First, the RCT was carried out in the older population living exclusively in Montreal. Second, even if benefits were reported for social isolation, physical and mental health, it is not possible to identify and isolate respective causal mechanisms. For example, mental and physical health benefits may result from the break in social isolation experienced because of participants', engagement in the study itself. Third, how much “control” we had over the control group was impossible to monitor with precision. Over the study period, the control group may have been exposed to activities that may have influenced the RCT outcomes. We tried to limit this effect by asking the control group participants to withhold participation any in arts-related interventions and social programs over the study period. No participants in the control group reported arts-related or social program activities, however, it was beyond our mandate to monitor. Fourth, there were significant differences between the intervention and control groups' baseline characteristics. In both groups there was a high proportion of females. However, this proportion differed significantly, with fewer females in the intervention group. Sex is a biological characteristic that may differentially impact the outcomes assessed in our RCT. Furthermore, there were also fewer Caucasians in the intervention group and this difference in ethnicity also could affect the results. However, it should be noted that all linear regression models were adjusted based on these baseline characteristics in order to limit their impact.
Conclusion
Our RCT suggests that a 3-month cycle of weekly virtual MMFA tours may decrease social isolation, foster a sense of connectedness and, thereby, improve mental and physical health in community-dwelling older adults. Like other arts-based activities, this particular program, delivered online, appears to have been an effective digital cultural intervention to mitigate social isolation and the progression of physical frailty, positioning museums as key stakeholders for social and health prevention, and for fostering social connectedness, in the aging population.
Data availability statement
The datasets used and analyzed in the current study will be made available by the corresponding author upon reasonable request. Requests should be sent to the corresponding author: OB, PhD; Research Centre of the Geriatric University Institute of Montreal, Montreal, QC, Canada; b2xpdmllci5iZWF1Y2hldEB1bW9udHJlYWwuY2Eu All requests need a cover letter explaining the objective, justification, and referent Ethics Committee.
Ethics statement
The study received approval from the CIUSSS Centre-Sud-de-l'Île-de-Montréal (Quebec, Canada) Research Ethics Committee approved the study (# 2022-1338 – CÉR VN 21-22-08). The patients/participants provided their written informed consent to participate in this study.
Author contributions
OB: principal investigator, study conception and design, obtaining funding, drafting the manuscript, revision of the manuscript, and final approval of the manuscript. JM, KG, CL, and KS: drafting the manuscript, revision of the manuscript, and final approval of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This trial was funded by Fonds de Recherche du Québec Société et culture; Actions concertées / Action sur le vieillissement actif de la population au Québec / Projet de recherche-action – Project 281107. The funding source had no role in the design of the nor on execution, data management, analyses, interpretation, or publication of the results.
Acknowledgments
We thank the museum guides and all members of the Direction of Education and Wellness of the MMFA. We thank also Amy Lee, the Chinese mandarin translator, all the members of the Service à la Famille Chinoise du Grand Montréal, Annie-Hélène Samson and the involved students of Dawson College.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ADL, Activities of daily living; CRIUGM, Research Center of the Geriatric University Institute of Montreal; CESAM, Center of Excellence Self-AdMinistred questionnaire; DSSI, Duke Social Support Index; EQ-5D, EuroQol-5D; IADL, Instrumental activities of daily living; MMFA, Montreal Museum of Fine Arts; VAS, visual analogic scale; WEMWBS, Warwick-Edinburgh Mental Wellbeing Scale.
Footnotes
1. ^https://www.google.ca/search?sxsrf=ACYBGNTU3BtvG3NM3zq7ZcuxogmZxn45qA%3A1580848264124&source=hp&ei=iNQ5XreMBfCh_Qb4pb-YAg&q=2018+English+Alliance+of+Museums+for+Health+and+Wellbeing&oq=2018+English+Alliance+of+Museums+for+Health+and+Wellbeing&gs_l=psy-ab.3.0.0.1306.9211.0.12174.0.0.6.0.0.0.124.745.10j1.0.0.0.0.0.0.0.0.0.1j2..gws-wiz.0.0.0.0.0.0.0i131j0j35i39j0i22i30j0i22i10i30.z4JigKYWf4U&ved=0ahUKEwi38OXZ3rjnAhXwUN8KHfjSDyMQ4dUDCAs&uact=5#spf=1580848276734
2. ^https://www.blueprintincome.com/tools/life-expectancy-calculator-how-long-will-i-live/
References
1. Epton T, Ghio D, Ballard LM, Allen SF, Kassianos AP, Hewitt R, et al. Interventions to promote physical distancing behaviour during infectious disease pandemics or epidemics: a systematic review. Soc Sci Med. (2022) 303:114946. doi: 10.1016/j.socscimed.2022.114946
2. Ernst M, Niederer D, Werner AM, Czaja SJ, Mikton C, Ong AD, et al. Loneliness before and during the COVID-19 pandemic: a systematic review with meta-analysis. Am Psychol. (2022) (in press). doi: 10.31234/osf.io/wjx5v
3. Beauchet O, Cooper-Brown L, Ivensky V, Launay CP. Telemedicine for housebound older persons during the Covid-19 pandemic. Maturitas. (2020) 142:8–10. doi: 10.1016/j.maturitas.2020.06.024
4. Launay CP, Cooper-Brown L, Ivensky V, Beauchet O. Frailty phenotype of homebound montreal older community dwellers during the COVID-19 pandemic: results of a cross-sectional population study. J Frailty Aging. (2021) 10:191–2. doi: 10.14283/jfa.2020.69
5. Morley JE, Vellas B, Van Kan GA, Anker SD, Bauer JM, Bernabei R, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. (2013) 14:392–7. doi: 10.1016/j.jamda.2013.03.022
6. Mitnitski AB, Rutenberg AD, Farrell S, Rockwood K. Aging, frailty and complex networks. Biogerontology. (2017) 18:433–46. doi: 10.1007/s10522-017-9684-x
7. Fédération internationale du vieillissement. Current emerging issues facing older Canadians. 2014. (2012) Available online at: https://www.ifa-fiv.org/wp-content/uploads/2012/12/current-and-emerging-issues-facing-older-canadians-final-report-30-march-2012.pdf (accessed October 2019).
8. Courtin E, Knapp M. Social isolation, loneliness and health in old age: a scoping review. Health Soc Care Commun. (2017) 25:799–812. doi: 10.1111/hsc.12311
9. Cotterell N, Buffel T, Phillipson C. Preventing social isolation in older people. Maturitas. (2018) 113:80–4 doi: 10.1016/j.maturitas.2018.04.014
10. Chipps J, Jarvis MA, Ramlall S. The effectiveness of e-interventions on reducing social isolation in older persons: a systematic review of systematic reviews. J Telemed Telecare. (2017) 23:817–27. doi: 10.1177/1357633X17733773
11. Landeiro F, Barrows P, Nuttall Musson E, Gray AM, Leal J. Reducing social isolation and loneliness in older people: a systematic review protocol. BMJ Open. (2017) 7:e013778. doi: 10.1136/bmjopen-2016-013778
12. Gardiner C, Geldenhuys G, Gott M. Interventions to reduce social isolation and loneliness among older people: an integrative review. Health Soc Care Commun. (2018) 26:147–57. doi: 10.1111/hsc.12367
13. Cattan M, White M, Bond J, Learmouth A. Preventing social isolation and loneliness among older people: a systematic review of health promotion interventions. Ageing Soc. (2005) 25:41. doi: 10.1017/S0144686X04002594
14. Dickens AP, Richards SH, Greaves CJ, Campbell JL. Interventions targeting social isolation in older people: a systematic review. BMC Public Health. (2011) 11:647. doi: 10.1186/1471-2458-11-647
15. Masi CM, Chen HY, Hawkley LC, Cacioppo JT, A. meta-analysis of interventions to reduce loneliness. Pers Soc Psychol Rev. (2011) 15:219–66. doi: 10.1177/1088868310377394
16. Jensen A, Bonde LO. The use of arts interventions for mental health and wellbeing in health settings. Perspect Public Health. (2018) 138:209–14. doi: 10.1177/1757913918772602
17. Jensen A. Beyond the borders: the use of art participation for the promotion of health and well-being in Britain and Denmark. Arts Health. (2013) 5:204–15. doi: 10.1080/17533015.2013.817448
18. Shannon K, Bail K, Neville S. Dementia-friendly community initiatives: an integrative review. J Clin Nurs. (2019) 28:2035–45. doi: 10.1111/jocn.14746
19. Beauchet O, Bastien T, Mittelman M, Hayashi Y, Ho A. Participatory art-based activity, community-dwelling older adults and changes in health condition: Results from a pre-post intervention, single arm, prospective and longitudinal study. Maturitas. (2020) 134:8–14. doi: 10.1016/j.maturitas.2020.01.006
20. Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. Int J Surg. (2012) 10:28–55. doi: 10.1016/j.ijsu.2011.10.001
21. Koenig HG, Westlund RE, George LK, Hughes DC, Blazer DG, Hybels C. Abbreviating the duke social support index for use in chronically ill elderly individuals. Psychosomatics. (1993) 34:61–9. doi: 10.1016/S0033-3182(93)71928-3
22. Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The warwick-edinburgh mental well-being scale (WEMWBS): development and UK validation. Health Qual Life Outcomes. (2007) 5:63. doi: 10.1186/1477-7525-5-63
23. Brooks P. EuroQol: the current state of play. Health Policy. (1996) 37:53–72. doi: 10.1016/0168-8510(96)00822-6
24. Beauchet O, Launay CP, Merjagnan C, Kabeshova A, Annweiler C. Quantified self and comprehensive geriatric assessment: older adults are able to evaluate their own health and functional status. PLoS ONE. (2014) 9:e100636. doi: 10.1371/journal.pone.0100636
25. Best Practices in Nursing Care to Older Adults. The Hartford Institute for Geriatric Nursing. New York University, College of Nursing. Available online at: www.hartfordign.org (accessed October 2019).
26. Pérès K, Chrysostome V, Fabrigoule C, Orgogozo JM, Dartigues JF, Barberger-Gateau P. Restriction in complex activities of daily living in MCI: impact on outcome. Neurology. (2006) 67:461–6. doi: 10.1212/01.wnl.0000228228.70065.f1
27. Gouvernement du Canada. Rapport sur l'isolement social des aînés, 2013-2014. Disponible en ligne. Available online at: https://www.canada.ca/fr/conseil-national-aines/programmes/publications-rapports/2014/isolement-social-aines/page05.html (accessed October 2019).
28. Statistic Canada. Une population vieillissante. 2018. Disponible en ligne. Available online at: https://www150.statcan.gc.ca/n1/pub/11-402-x/2010000/pdf/population-fra.pdf (accessed October 2019).
29. O'Rourke HM, Collins L, Sidani S. Interventions to address social connectedness and loneliness for older adults: a scoping review. BMC Geriatr. (2018) 18:214. doi: 10.1186/s12877-018-0897-x
30. Medical Advisory Secretariat. Social isolation in community-dwelling seniors: an evidence-based analysis. Ont Health Technol Assess Ser. (2008) 8:1–49.
31. Fédération internationale du vieillissement. Current Emerging Issues Facing Older Canadians. (2012). Available online at: https://www.ifa-fiv.org/wp-content/uploads/2012/12/current-and-emerging-issues-facing-older-canadians-final-report-30-march-2012.pdf (accessed October 2019).
32. Perruzza N, Kinsella EA. Creative arts occupations in therapeutic practice: a review of the literature. Br J Occup Therapy. (2010) 73:261–8. doi: 10.4276/030802210X12759925468943
33. Deshmukh SR, Holmes J, Cardno A. Art therapy for people with dementia. Cochrane Database Syst Rev. (2018) 9:CD011073. doi: 10.1002/14651858.CD011073.pub2
34. Todd C, Camic PM, Lockyer B, Thomson LJM, Chatterjee HJ. Museum-based programs for socially isolated older adults: understanding what works. Health Place. (2017) 48:47–55. doi: 10.1016/j.healthplace.2017.08.005
35. Camic PM, Chatterjee HJ. Museums and art galleries as partners for public health interventions. Perspect Public Health. (2013) 133:66–71. doi: 10.1177/1757913912468523
36. Beauchet O, Cooper-Brown LA, Hayashi Y, Deveault M, Launay CP. Improving the mental and physical health of older community-dwellers with a museum participatory art-based activity: results of a multicentre randomized controlled trial. Aging Clin Exp Res. (2022) (in press). doi: 10.1007/s40520-022-02139-3
Keywords: older adults, social isolation, art, museum, wellbeing, quality of life, frailty
Citation: Beauchet O, Matskiv J, Galery K, Goossens L, Lafontaine C and Sawchuk K (2022) Benefits of a 3-month cycle of weekly virtual museum tours in community dwelling older adults: Results of a randomized controlled trial. Front. Med. 9:969122. doi: 10.3389/fmed.2022.969122
Received: 14 June 2022; Accepted: 14 July 2022;
Published: 16 August 2022.
Edited by:
Giovanni Maga, National Research Council (CNR), ItalyReviewed by:
Lina Ma, Capital Medical University, ChinaPınar Soysal, Bezmiâlem Vakif Üniversitesi, Turkey
Copyright © 2022 Beauchet, Matskiv, Galery, Goossens, Lafontaine and Sawchuk. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Olivier Beauchet, b2xpdmllci5iZWF1Y2hldEB1bW9udHJlYWwuY2E=
 Olivier Beauchet
Olivier Beauchet Jacqueline Matskiv2
Jacqueline Matskiv2 Linda Goossens
Linda Goossens Kim Sawchuk
Kim Sawchuk