- 1Eye Clinic, Department of Neurosciences, Psychology, Drug Research and Child Health (NEUROFARBA), University of Florence, Florence, Italy
- 2Division of Geriatric and Intensive Care Medicine, Azienda Ospedaliero Universitaria Careggi, and Department of Experimental and Clinical Medicine, University of Florence, Florence, Italy
Cataract is a leading cause of visual impairment in old age. Lens opacification is notoriously associated with several geriatric conditions, including frailty, fall risk, depression and cognitive impairment. The association is largely attributable to visual impairment, while other mechanisms, associated with extraocular comorbidity and lifestyle, might partly explain this correlation. Available literature suggests that cataract surgery may be effective in decreasing fall risk, improving depressive symptoms and limiting the risk of cognitive impairment and dementia incidence, although intervention studies on these outcomes are still limited. In this review we also emphasize the need to move from the concept of visual acuity to functional vision, especially in the context of the geriatric patient. Research is needed regarding the effect on the cited outcomes of different cataract treatment strategies, such as systematic bilateral versus monolateral surgery and use of different intraocular lenses.
Introduction
Cataract is the partial or total opacification of the lens, usually progressive and irreversible, leading to loss of vision with medical, social and economic implications. Typically occurring with advancing age, it is a frequent cause of age-related blindness and it is reversible through surgery (1).
It is estimated that 95 million people worldwide are affected by cataract (2). In 2020, the leading worldwide causes of blindness in patients aged 50 years and older were: cataract, followed by glaucoma, under-corrected refractive error, age-related macular degeneration, and diabetic retinopathy (3). To underline the importance of the disease, cataract is responsible for 50% of cases of blindness in middle- and low-income countries, which have poor access to primary care compared to 5% in developed countries (2, 4). The World Health Organization has estimated that with population growth and progressive aging in future years there will be an increase of visual impairment attributable to cataract (5). Furthermore, up to two-thirds of adults with visually significant cataract have been estimated to be undiagnosed, and half of these cases have bilateral visual impairment, often resulting in significant functional impairment (6). Overall, the cited data underline the huge and probably underestimated impact of cataract on visual functioning of older adults. The present narrative review is aimed at assessing the association of cataract with different aspects of health status of aging population, including frailty, falls, fracture, depressive symptoms, and cognitive impairment. Accordingly, we describe potential impact of cataract surgery in old age, and discuss synergies between ophthalmologic and geriatric care possibly resulting in a reduced burden of the disease.
Cataract, frailty, falls and fractures
Cataract and frailty
Frailty is defined as a clinical state in which there is an increase in an individual’s susceptibility to developing negative health-related events when exposed to endogenous or exogenous stressors (7). Two main models have been established to define frailty: the physical frailty phenotype proposed by Linda Fried and the deficit accumulation index elaborated by Kenneth Rockwood (8).
However it is defined, frailty is associated with an increased risk of adverse events, including mortality, disability, and hospital admission. Falls are included among frailty-associated adverse events and, in turn, are associated with fragility fractures, head trauma, disability and mortality risk.
The possible role of cataract as a global frailty biomarker is underlined by data which shows an association with mortality risk (9). Nevertheless, data regarding the association between cataract surgery and mortality are not consistent. In fact, some results suggest a reduced mortality risk after cataract surgery (10), other works show a reduced mortality risk only among the patients who gained better visual acuity (11); on the contrary, some studies suggest a neutral effect after adjusting for confounders (12). Finally, a cohort study has also documented a greater mortality risk among patients that underwent cataract surgery (13).
As a matter of fact, cataract and frailty are both correlated with aging and often coexist. Beyond the parallelism due to demographic factors, an association has been identified between visual impairment and incident physical frailty, independently of coexistent diseases and possible confounders (14); in this work, visual impairment was correlated with a future development of frailty after a 4-year follow-up among non-frail older patients, placing cataract as the most common reversible cause of visual impairment.
On the other hand, a specific association has been detected between cataract and physical frailty in cross-sectional studies, also independently of visual impairment (15), suggesting shared biological mechanisms which include similar age-associated biochemical alterations involving the lens and skeletal muscle protein structures. The cited authors found an association between nuclear cataract in men and a slower gait time (p = 0.01) as well as a poorer frailty index score (p = 0.01); however cortical and posterior subcapsular cataract in women was correlated with a lower peak expiratory flow rate (p < 0.01). Consistently, in a different sample of community-dwelling older patients, there was a significant difference in cataract risk between non-frail (31%), prefrail (37%), and frail groups (42%) (16).
In specific conditions the association between cataract and frailty has known biological explanation. For example, pseudoexfoliation (PEX) syndrome is associated both with an increased risk of nuclear cataract and cataract surgery and with a higher prevalence of cardio- and cerebrovascular disorders, sensorineural hearing loss and Alzheimer-related dementia (17–21). Moreover, posterior subcapsular cataracts may be associated with diabetes mellitus and with steroid treatment, which in turn may correlate with frailty risk independently of lens opacification (22). Other mechanisms, including similar protein aging in lens and in muscle, have been suggested to explain the potential role of cataract as frailty biomarker independently of low vision (15). Further research in this field is needed.
Cataract and fall risk
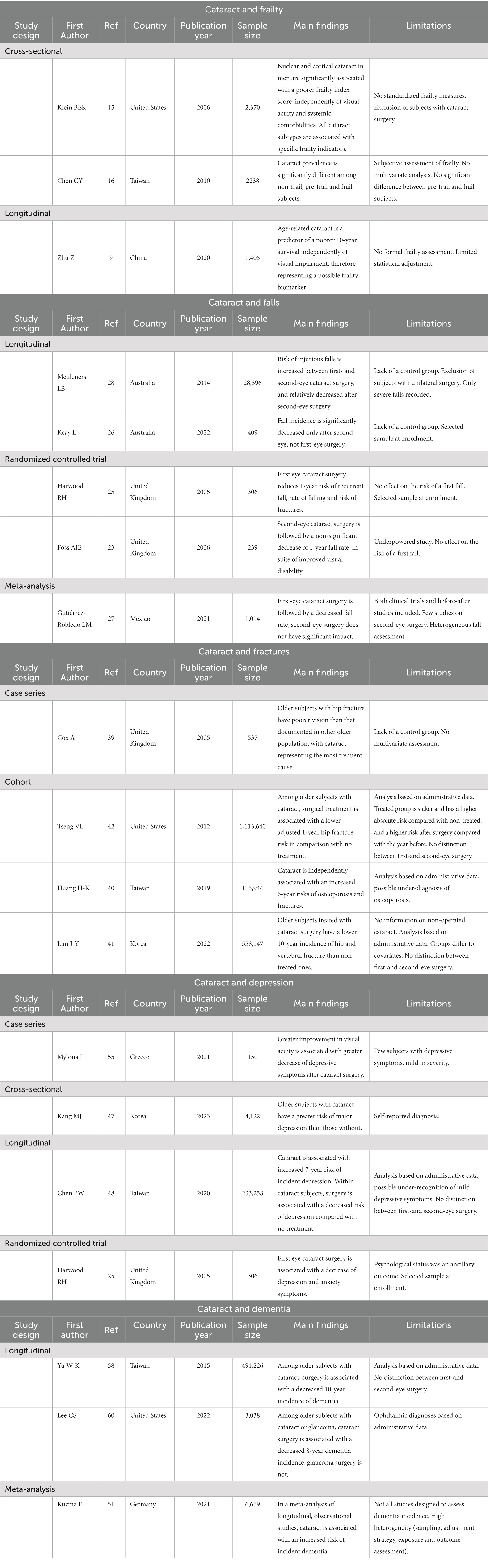
Several observational and some randomized studies have examined the association between cataract surgery and fall risk (23–28). Table 1 summarizes the main studies cited in this review.
Normal aging is accompanied by visual dysfunctions that correlate with fall risk, including reduced visual acuity, reduced contrast sensitivity, reduced depth perception, visual field contraction and prolonged glare recovery (29). Similarly, several specific age-associated ocular diseases have a well-established correlation with recurring fall events, with cataract being both the most prevalent, as previously discussed, and one of the most easily treatable, at least in economically-stable countries.
Vision contributes not only to the detection of tripping hazards on the ground, but also to a patient’s posture and balance through visual-sensory inputs modulated at the cerebellar level, where they are integrated with a proprioceptive signal. Good vision is also associated with high levels of physical activity, thus suggesting its enabling effect on health through the biomechanical benefits of physical exercise on the musculoskeletal system, resulting in a lower fall risk (30). Consistent with these data, a large multinational study has observed a graded association between vision impairment severity and sarcopenia (i.e., loss of muscle mass in old age) (31).
Most literature shows that first-eye cataract surgery reduces the risk of falls in older people, but the effect of second-eye cataract surgery is less clear (25, 27, 32).
Some studies have been summarized in a recent meta-analysis, which documented that fall risk could be reduced by one third after cataract extraction (in comparison with the pre-surgery period), although a significant between-study heterogeneity was observed (27). These data are consistent with the single randomized controlled trial that reported a significant reduction of rate of falls among randomized patients undergoing expedited surgery compared with a postponed-list group, in a 12-month follow-up (25). Moreover, the treatment group showed a better outcome with regard to anxiety, depression and quality of life. Conversely, no significant fall rate decrease was observed after second-eye surgery, both in observational studies and in a single, although underpowered, randomized clinical trial, in spite of a decrease in visual disability and increase in quality of life observed in the latter study (23, 27). Somehow at odds with the cited data, a large Australian observational study found an increase in fall rate during the 2 years following first-eye cataract surgery, while waiting for the second-eye surgery, with a relative decrease only after the treatment of the second eye (28). These data are consistent with a US population-based study showing that, after a 2-year follow-up, older patients undergoing monolateral cataract surgery had a greater decline in motor function in comparison with a general older population without severe visual impairment, while this decline was not observed in the subgroup undergoing bilateral surgery (33). A recent cohort Australian study on patients referred for bilateral cataract surgery, confirmed an absolute decrease in the fall rate only after the second intervention (26). This is consistent with data that show an association between stereopsis and fall risk, which is even more important than that observed for visual acuity, thus suggesting that good binocular vision, which can be attained with bilateral surgery, may be needed to minimize fall risk (23, 34). On the whole, cited data suggest that cataract is a marker of increased risk of motor impairment and fall risk, possibly beyond vision impairment, and that a bilateral correction is probably needed to achieve a substantial risk reduction, while patients undergoing monolateral surgery may show a paradoxical increase in fall risk.
Yet more research is needed to support a systematic policy of bilateral surgery to decrease fall risk in an aging population (35).
Cataract and hip fractures
Approximately one in three community-dwelling individuals over the age of 65 reports at least one fall event per year, with this risk proportionally increasing with age, determining in 5–10% of cases fragility fractures and 1–2% of cases hip fractures, also due to the frequent coexistence of osteoporosis (36).
Nevertheless, the role of osteoporosis over the years has been downplayed. Siris et al., using data from NORA (National Osteoporosis Risk Assessment), examined a population of almost 150.000 white, postmenopausal women aged 50 to 104 years (mean age 64.5 years) and observed that 82% of postmenopausal women with fractures had T-scores higher than −2.5, the threshold value below which osteoporosis is diagnosed (37). This makes it clear that reduced bone mineral density (BMD) is not actually as decisive as we might think in hip fracture development. The most recent literature points out that BMD and risk of falling independently increase fracture risk, with a need for multifactorial interventions for primary and secondary prevention of fragility fractures (36).
One area for further study is represented by the relationship between visual impairment, including cataract and fractures, with the aim of identifying effective prevention strategies. It has been clearly demonstrated that blindness (defined as a best corrected visual acuity ≤20/500 in the better eye) increases the risk of hip and vertebral fractures (38). Among conditions of visual impairment, untreated cataract has been identified as the main cause of hip fracture in a UK sample (39). In a Taiwanese matched cohort study cataract was associated with an increased risk of hip and vertebral fractures over a 6.4-year follow-up (40). To note, patients with cataract had a greater baseline comorbidity and an increased risk of osteoporosis incidence during follow-up, suggesting it may represent a frailer population, beyond visual impairment (40). Little data, and no specifically designed intervention studies, are available regarding the association between cataract surgery and hip fractures. In the previously cited Taiwanese study, patients undergoing cataract surgery showed a decreased fracture risk in comparison with those with non-operated cataract. A recent nationwide Korean cohort study confirmed that older patients who underwent cataract surgery showed a lower incidence of hip and vertebral fragility fractures than those who did not (41). In a previous Medicare cohort study, patients that underwent surgery in comparison with patients with non-operated cataract had similar hip fracture rates in a 12-month follow-up period. However, patients in the surgery group were older, had more severe comorbidity and disability and were more frequently affected by severe cataract and, after adjusting for these covariates, hip fracture rate was significantly lower in the surgery group, with an absolute risk difference of about 0.2% per year, and more beneficial effects observed among older patients, more advanced cataract and greater comorbidity (42). Overall, these studies suggest that cataract surgery in elderly patients may reduce and prevent the incidence of hip and vertebral fragility fractures. No study has compared fracture risk associated with first- and second-eye cataract surgery.
Cataract, depression and cognitive impairment
Depression is common in old age and is typically associated with chronic disease and multimorbidity, psychosocial adversity, cognitive impairment and disability (43).
Several studies have shown an association between depression in old age and visual disturbances, including cataract. The association between low vision and depression may be explained by reduction in daily activity, such as reading, loss of autonomy, difficult social interaction and loss of self-esteem (44). A recent metanalysis has identified a huge 25% prevalence of depression in samples of patients referred to eye clinics and low vision rehabilitation centers. The prevalence of depression was even higher, estimated as 33%, in the subgroup of studies that did not adopt exclusion criteria, and dropped to 18% when patients with comorbidity, mainly cognitive impairment, were excluded (45). A French cohort study has shown that patients with low vision have a threefold increase of depression risk in a 10-year follow-up, but that patients with depression have a 60% increased risk of vision impairment incidence (46). Regarding the specific effect of cataract, its diagnosis has been recently associated with a 65% increase of major depression risk in the cross-sectional analysis of a representative sample of older Korean citizens (47). Moreover, cataract was specifically associated with a 78% increase of depression risk after a 7.8-year follow-up in a propensity score matched cohort study in Taiwan (48).
Several studies have recently examined the association between vision impairment and risk of cognitive decline. A recent metanalysis has observed an association of low vision with an increased risk of cognitive impairment and dementia incidence (49). A dose–response association has been observed in a large UK cohort, with dementia risk being greatest among patients with severe vision impairment (50). In a meta-analysis that compared the risk of cognitive impairment between different causes of low vision, cataract and diabetic retinopathy were associated with an increased risk of dementia and Alzheimer’s disease (51).
Regarding cataract surgery, some studies suggest that it can improve depressive symptoms and anxiety and may be associated with a decreased risk of cognitive impairment (52–54). In a previously cited cohort study, subjects with cataract undergoing surgery had a 25% less depression risk in comparison with untreated ones over a 7.8-year follow-up (48). Moreover, data from the previously-cited randomized controlled study on expedited cataract surgery have shown a significant decrease in depression and anxiety in the early treatment group (25). Of notice, an association has been observed between visual acuity improvement and depressive symptoms decrease after phacoemulsification, thus highlighting the importance of successful surgery for this specific outcome (55).
Data have been less consistent over the years regarding the association between cataract surgery and risk of cognitive impairment, as older studies reported no significant effects on neuropsychological functions (56, 57), while more recent ones showed a protective association on cognitive impairment and dementia risk (58). A small study conducted using functional magnetic resonance imaging suggested functional and morpho-structural improvements in visual and cognitive-related brain areas after cataract surgery (59). In a large US cohort including older patients (mean age 74) with a diagnosis of cataract and glaucoma, cataract surgery was independently associated with a significant decrease in dementia risk in a 7.8-year follow-up, while glaucoma surgery was not (60).
A recent systematic review and meta-analysis focusing on psychiatric and neuropsychological assessments provided further evidence that cataract surgery has a positive effect not only on depressive symptoms but also on cognitive function in older patient (61).
Discussion
Visual acuity is the main parameter evaluated in ophthalmology to monitor visual progress of a medical or surgical treatment. The term “visual acuity” refers to the ability of the human eye to detect and perceive the smallest details of an object at a given distance (62, 63). Normal visual acuity depends on the transparency of the eye’s dioptric media, the correction of any refractive defect, and the integrity of the macula and optic pathways. However, it is now well established that visual acuity provides only raw data on the overall functioning of sight, indeed it does not consider a patient’s ability to use his or her visual apparatus within a complex and dynamic socio-cultural environment (64, 65). The visual acuity test with Snellen tables is a high-contrast test: recognizing black letters on a white background allows even a patient with low contrast sensitivity to achieve 20/20 (66). Moreover, high visual acuity can be found in patients with severe peripheral visual field deficit: despite high performance using Snellen’s table, a patient with visual field defect may have difficulty relating to the outside world and is potentially limited in a large number of daily activities, implying reduced quality of life and poor social and occupational functioning (67).
Concerning the cataract patient, visual acuity is used to address surgical indication. In Europe, for example, it is customary to advise patients with visual acuity of 6/12 or less in one or both eyes to undergo surgery (68). However, this advice has clear limits: a patient with preserved visual acuity but affected by a posterior subcapsular cataract may experience bothersome nighttime glare at the sight of traffic lights, therefore for a nighttime driver, even with high VA, a subcapsular cataract can severely limit his or her functioning and merit expedited surgery. Indeed, the National Institute of Health and Care Excellence guidelines for the management of cataracts established that the assessment of visual acuity as an indication for cataract surgery fails to recognize other visual impairments that may limit the activities of daily living and hence require intervention (69).
Nevertheless, cataract surgery can have intraoperative or postoperative complications, such as endophthalmitis, posterior capsular ruptures, IOL (intra-ocular lens) dislocations, refractive errors, endothelial damage and dry eye (70–73). Even though nowadays these complications are rare, they can affect the postoperative visual outcomes and quality of life. Therefore, the patients should be informed of these risks, but it has to be pointed out that the benefits of surgery very often overcome the possible complications in visually-impaired individuals.
It is also necessary to consider the visual system as binocular. Precise correction of 1 eye by an IOL (intra ocular lens) while waiting for the contralateral eye to be treated could lead to non-negligible anisometropia and sometimes diplopia. This phenomenon could partly explain the increased incidence of falls and fractures after cataract surgery that is documented in some studies, although it cannot be ruled out that phacoemulsification induces patients to consider themselves freer, thus leading them to perform more activities and expose themselves to the risk of falling.
Regarding fall risk, it is reported that multiple “fallers” usually have decreased vision, as indicated by all visual tests, with impaired depth perception, contrast sensitivity and low-contrast visual acuity being the strongest risk factors (74).
There are a few older studies in literature that have found that visual impairment is not a predictor for the risk of falling in old age (75–78). However, most of these studies only assessed a limited aspect of the global visual functioning, that it to say visual acuity. Other studies showed a lack of association between fracture risk and visual impairment when only visual acuity was evaluated (79).
Lastly, patients’ necessities in relation to his or her daily activities must be taken into account when choosing which IOL to implant. For example, a classic monofocal IOL may provide perfect distance visual acuity but limit the range of action at intermediate and close distances. In the context of fall risk and femur fracture, the intermediate distance is perhaps the most impactful. Recognizing an obstacle requires good contrast sensitivity (especially at night), sense of depth, color perception, motion perception, good visual processing speed as well as an optimal binocular field of view. All these factors fall under the concept of functional vision, and should be evaluated synergistically to develop a “cataract frailty index” that could select patients at risk of falling, on whom preventive action can be taken with tailored surgical strategies (80).
Comparison of different intraocular lenses regarding visual impairment, visual function and patient satisfaction are becoming available (81, 82). Similar studies addressing outcomes which are specifically relevant to older populations, such as fall incidence, depressive symptoms and cognitive impairment, are needed to guide clinicians’ choice.
To summarize what has been said so far, cataracts increase the risk of developing frailty, falls, fractures, depression and cognitive impairment, and reduce the percentage of functional reserve of an individual over time. Functional reserve refers to a patient’s residual capacity to perform his or her physiological activities (83). It is conceivable that by assessing functional vision instead of visual acuity, surgery should be planned within an early “window of opportunity” to prevent the aforementioned geriatric adverse events.
A limitation of our review is the narrative design: further systematic reviews are necessary in order to better describe the current knowledge on the different aspects of this topic.
Conclusion
Cataract is a primary cause of visual impairment worldwide and, among older subjects, is associated with frailty, fall risk, depressive symptoms, and neurocognitive decline. Due to the high prevalence and the frequent lack of recognition of lens opacification, a systematic screening of visual impairment with a timely referral to the ophthalmologist is advised to prevent progression to bilateral visual impairment and possibly prevent negative health outcomes. In particular, it is necessary to include visual performance in comprehensive geriatric assessment, in order to identify subjects at risk and to develop questionnaires or clinical indices to assess the impact of functional vision on daily activities. The introduction of visual assessment in geriatric clinical practice would allow an appropriate referral to the ophthalmologists, with the aim to decide, with a greater clinical awareness, whether cataract extraction is indicated.
On the other hand, ophthalmologists should adopt a comprehensive approach to older subjects, keeping a focus on individual priorities, global autonomy and cognitive difficulties, and tailoring the IOL choice beyond visual function. Indication for surgery should be considered in relation not only to visual acuity, but also to the functional vision assessment, daily needs and individual priorities. A geriatric referral may be helpful for the ophthalmologist to decide regarding surgery in complex cases, including those with cognitive decline and multimorbidity. After surgery a joint geriatric and ophthalmologic follow-up may allow the assessment of treatment effects on different domains of health status, and may possibly help decision regarding second-eye surgery in frail older subjects.
Generally speaking, cataract surgery should be encouraged for both visual recovery and prevention of negative health-related events in frail patients or those with neurocognitive impairment. However, several research areas remain to be addressed with the aim of identifying the most effective strategies to reduce the global health impact of cataract. In particular, it is conceivable that the protective effect of cataract treatment on functional impairment, falls incidence and dementia risk may be time-dependent, with the need to identify a “window of opportunity” for surgery, before the frailty process becomes irreversible. Therefore, valid and easy-to-use screening instruments of visual impairment, focusing on the impact on daily activities, are needed in primary care and routine geriatric practice. Moreover, the specific role of different intervention strategies, such as systematic bilateral versus unilateral surgery or use of different intraocular lenses, deserves further studies. Most important, future intervention studies should increasingly include global health outcomes, such as disability and quality of life, falls and fracture incidence, depressive symptoms and cognitive impairment.
Author contributions
RM, SS, and EM wrote the first draft of the manuscript. EF, MC, and CV wrote sections of the manuscript. All authors contributed to conception, design of the review, manuscript revision, read, and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.Asbell, PA, Dualan, I, Mindel, J, Brocks, D, Ahmad, M, and Epstein, S. Age-related cataract. Lancet. (2005) 365:599–609. doi: 10.1016/S0140-6736(05)70803-5
2.Liu, Y-C, Wilkins, M, Kim, T, Malyugin, B, and Mehta, JS. Cataracts. Lancet. (2017) 390:600–12. doi: 10.1016/S0140-6736(17)30544-5
3.GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the right to sight: an analysis for the global burden of disease study. Lancet Glob Heal. (2021) 9:e144–60. doi: 10.1016/S2214-109X(20)30489-7
4.Khanna, R, Pujari, S, and Sangwan, V. Cataract surgery in developing countries. Curr Opin Ophthalmol. (2011) 22:10–4. doi: 10.1097/ICU.0b013e3283414f50
5.WHO. Visual Impairment and Blindness. (2019). Available at: https://www.who.int/en/news-room/fact-sheets/detail/blindness-and-visualimpairment
6.Chua, J, Lim, B, Fenwick, EK, Gan, AT, Tan, AG, Lamoureux, E, et al. Prevalence, risk factors, and impact of undiagnosed visually significant cataract: the Singapore epidemiology of eye diseases study. PLoS One. (2017) 12:e0170804. doi: 10.1371/journal.pone.0170804
7.Cesari, M, Calvani, R, and Marzetti, E. Frailty in older persons. Clin Geriatr Med. (2017) 33:293–303. doi: 10.1016/j.cger.2017.02.002
8.Clegg, A, Young, J, Iliffe, S, Rikkert, MO, and Rockwood, K. Frailty in elderly people. Lancet. (2013) 381:752–62. doi: 10.1016/S0140-6736(12)62167-9
9.Zhu, Z, Wang, L, Scheetz, J, and He, M. Age-related cataract and 10-year mortality: the Liwan eye study. Acta Ophthalmol. (2020) 98:e328–32. doi: 10.1111/aos.14258
10.Fong, CS, Mitchell, P, Rochtchina, E, Teber, ET, Hong, T, and Wang, JJ. Correction of visual impairment by cataract surgery and improved survival in older persons: the Blue Mountains eye study cohort. Ophthalmology. (2013) 120:1720–7. doi: 10.1016/j.ophtha.2013.02.009
11.Fong, CS-U, Mitchell, P, Rochtchina, E, de Loryn, T, Tan, AG, and Wang, JJ. Visual impairment corrected via cataract surgery and 5-year survival in a prospective cohort. Am J Ophthalmol. (2014) 157:163–170.e1. doi: 10.1016/j.ajo.2013.08.018
12.Zhu, Z, Wang, L, Young, CA, Huang, S, Chang, BHW, and He, M. Cataract-related visual impairment corrected by cataract surgery and 10-year mortality: the Liwan eye study. Invest Ophthalmol Vis Sci. (2016) 57:2290–5. doi: 10.1167/iovs.15-17673
13.Tseng, VL, Chlebowski, RT, Yu, F, Cauley, JA, Li, W, Thomas, F, et al. Association of Cataract Surgery with Mortality in older women: findings from the Women’s health initiative. JAMA Ophthalmol. (2018) 136:3–10. doi: 10.1001/jamaophthalmol.2017.4512
14.Liljas, AEM, Carvalho, LA, Papachristou, E, de Oliveira, C, Wannamethee, SG, Ramsay, SE, et al. Self-reported vision impairment and incident prefrailty and frailty in English community-dwelling older adults: findings from a 4-year follow-up study. J Epidemiol Community Health. (2017) 71:1053–8. doi: 10.1136/jech-2017-209207
15.Klein, BEK, Klein, R, and Knudtson, MD. Frailty and age-related cataract. Ophthalmology. (2006) 113:2209–12. doi: 10.1016/j.ophtha.2006.04.035
16.Chen, C-Y, Wu, S-C, Chen, L-J, and Lue, B-H. The prevalence of subjective frailty and factors associated with frailty in Taiwan. Arch Gerontol Geriatr. (2010) 50:S43–7. doi: 10.1016/S0167-4943(10)70012-1
17.Terracciano, L, Cennamo, M, Favuzza, E, Julia, L, Caporossi, O, and Mencucci, R. An in vivo confocal microscopy study of corneal changes in pseudoexfoliation syndrome. Eur J Ophthalmol. (2019) 29:555–60. doi: 10.1177/1120672118803850
18.You, QS, Xu, L, Wang, YX, Yang, H, Ma, K, Li, JJ, et al. Pseudoexfoliation: normative data and associations: the Beijing eye study 2011. Ophthalmology. (2013) 120:1551–8. doi: 10.1016/j.ophtha.2013.01.020
19.Kanthan, GL, Mitchell, P, Burlutsky, G, Rochtchina, E, and Wang, JJ. Pseudoexfoliation syndrome and the long-term incidence of cataract and cataract surgery: the blue mountains eye study. Am J Ophthalmol. (2013) 155:83–88.e1. doi: 10.1016/j.ajo.2012.07.002
20.Wang, W, He, M, Zhou, M, and Zhang, X. Ocular pseudoexfoliation syndrome and vascular disease: a systematic review and meta-analysis. PLoS One. (2014) 9:e92767. doi: 10.1371/journal.pone.0092767
21.Temporale, H, Karasińska-Kłodowska, A, Turno-Kręcicka, A, Morawska-Kochman, M, Dorobisz, K, Dudek, K, et al. Evaluating the hearing of patients with Pseudoexfoliation syndrome. Adv Clin Exp Med. (2016) 25:1215–21. doi: 10.17219/acem/62919
22.Delcourt, C, Cristol, JP, Tessier, F, Léger, CL, Michel, F, and Papoz, L. Risk factors for cortical, nuclear, and posterior subcapsular cataracts: the POLA study. Pathologies Oculaires Liées à l’Age. Am J Epidemiol. (2000) 151:497–504. doi: 10.1093/oxfordjournals.aje.a010235
23.Foss, AJE, Harwood, RH, Osborn, F, Gregson, RM, Zaman, A, and Masud, T. Falls and health status in elderly women following second eye cataract surgery: a randomised controlled trial. Age Ageing. (2006) 35:66–71. doi: 10.1093/ageing/afj005
24.Nevitt, MC, Cummings, SR, Kidd, S, and Black, D. Risk factors for recurrent nonsyncopal falls. A prospective study. JAMA. (1989) 261:2663–8. doi: 10.1001/jama.261.18.2663
25.Harwood, RH, Foss, AJE, Osborn, F, Gregson, RM, Zaman, A, and Masud, T. Falls and health status in elderly women following first eye cataract surgery: a randomised controlled trial. Br J Ophthalmol. (2005) 89:53–9. doi: 10.1136/bjo.2004.049478
26.Keay, L, Ho, KC, Rogers, K, McCluskey, P, White, AJ, Morlet, N, et al. The incidence of falls after first and second eye cataract surgery: a longitudinal cohort study. Med J Aust. (2022) 217:94–9. doi: 10.5694/mja2.51611
27.Gutiérrez-Robledo, LM, Villasís-Keever, MA, Avila-Avila, A, Medina-Campos, RH, Castrejón-Pérez, RC, and García-Peña, C. Effect of cataract surgery on frequency of falls among older persons: a systematic review and meta-analysis. J Ophthalmol. (2021) 2021:1–7. doi: 10.1155/2021/2169571
28.Meuleners, LB, Fraser, ML, Ng, J, and Morlet, N. The impact of first- and second-eye cataract surgery on injurious falls that require hospitalisation: a whole-population study. Age Ageing. (2014) 43:341–6. doi: 10.1093/ageing/aft177
29.Erdinest, N, London, N, Lavy, I, Morad, Y, and Levinger, N. Vision through healthy aging eyes. Vision. (2021) 5:46. doi: 10.3390/vision5040046
30.Rietdyk, S, Ambike, S, Amireault, S, Haddad, JM, Lin, G, Newton, D, et al. Co-occurrences of fall-related factors in adults aged 60 to 85 years in the United States National Health and nutrition examination survey. PLoS One. (2022) 17:e0277406. doi: 10.1371/journal.pone.0277406
31.Smith, L, López-Sánchez, GF, Jacob, L, Barnett, Y, Pardhan, S, Veronese, N, et al. Objectively measured far vision impairment and sarcopenia among adults aged ≥ 65 years from six low- and middle-income countries. Aging Clin Exp Res. (2021) 33:2995–3003. doi: 10.1007/s40520-021-01841-y
32.Keay, L, Palagyi, A, McCluskey, P, Lamoureux, E, Pesudovs, K, Lo, S, et al. Falls in older people with cataract, a longitudinal evalUation of impact and riSk: the FOCUS study protocol. Inj Prev. (2014) 20:e7. doi: 10.1136/injuryprev-2013-041124
33.Lee, BS, Munoz, BE, West, SK, and Gower, EW. Functional improvement after one- and two-eye cataract surgery in the Salisbury eye evaluation. Ophthalmology. (2013) 120:949–55. doi: 10.1016/j.ophtha.2012.10.009
34.Lord, SR. Visual risk factors for falls in older people. Age Ageing. (2006) 35:ii55–9. doi: 10.1093/ageing/afl085
35.Sheppard, WEA, McCarrick, D, Wilkie, RM, Baraas, RC, and Coats, RO. A systematic review of the effects of second-eye cataract surgery on motor function. Front. Aging. (2022) 3, 2022:866823. doi: 10.3389/fragi.2022.866823
36.Baim, S, and Blank, R. Approaches to fracture risk assessment and prevention. Curr Osteoporos Rep. (2021) 19:158–65. doi: 10.1007/s11914-021-00659-x
37.Siris, ES, Chen, YT, Abbott, TA, Barrett-Connor, E, Miller, PD, Wehren, LE, et al. Bone mineral density thresholds for pharmacological intervention to prevent fractures. Arch Intern Med. (2004) 164:1108–12. doi: 10.1001/archinte.164.10.1108
38.Choi, HG, Lee, JK, Lee, MJ, Park, B, Sim, S, and Lee, S-M. Blindness increases the risk for hip fracture and vertebral fracture but not the risk for distal radius fracture: a longitudinal follow-up study using a national sample cohort. Osteoporos Int. (2020) 31:2345–54. doi: 10.1007/s00198-020-05475-0
39.Cox, A, Blaikie, A, MacEwen, CJ, Jones, D, Thompson, K, Holding, D, et al. Visual impairment in elderly patients with hip fracture: causes and associations. Eye (Lond). (2005) 19:652–6. doi: 10.1038/sj.eye.6701610
40.Huang, H-K, Lin, S-M, Loh, C-H, Wang, J-H, and Liang, C-C. Association between cataract and risks of osteoporosis and fracture: a Nationwide cohort study. J Am Geriatr Soc. (2019) 67:254–60. doi: 10.1111/jgs.15626
41.Lim, J-Y, Yoo, J-I, Kim, RB, Koo, HJ, Kong, GM, and Ha, Y-C. Comparison of the incidence rates of hip and vertebral fragility fractures according to cataract surgery in elderly population: a nationwide cohort study. Arch Osteoporos. (2022) 17:30. doi: 10.1007/s11657-021-01018-0
42.Tseng, VL, Yu, F, Lum, F, and Coleman, AL. Risk of fractures following cataract surgery in Medicare beneficiaries. JAMA. (2012) 308:493–501. doi: 10.1001/jama.2012.9014
43.Alexopoulos, GS. Depression in the elderly. Lancet. (2005) 365:1961–70. doi: 10.1016/S0140-6736(05)66665-2
44.Klauke, S, Sondocie, C, and Fine, I. The impact of low vision on social function: the potential importance of lost visual social cues. J Optom. (2022) 16:3–11. doi: 10.1016/j.optom.2022.03.003
45.Parravano, M, Petri, D, Maurutto, E, Lucenteforte, E, Menchini, F, Lanzetta, P, et al. Association between visual impairment and depression in patients attending eye clinics: a meta-analysis. JAMA Ophthalmol. (2021) 139:753–61. doi: 10.1001/jamaophthalmol.2021.1557
46.Carrière, I, Delcourt, C, Daien, V, Pérès, K, Féart, C, Berr, C, et al. A prospective study of the bi-directional association between vision loss and depression in the elderly. J Affect Disord. (2013) 151:164–70. doi: 10.1016/j.jad.2013.05.071
47.Kang, MJ, Do, KY, Park, N, Kang, MW, and Jeong, KS. The risk of major depressive disorder due to cataracts among the Korean elderly population: results from the Korea National Health and nutrition examination survey (KNHANES) in 2016 and 2018. Int J Environ Res Public Health. (2023) 20:1547. doi: 10.3390/ijerph20021547
48.Chen, PW, Liu, PP, Lin, SM, Wang, JH, Huang, HK, and Loh, CH. Cataract and the increased risk of depression in general population: a 16-year nationwide population-based longitudinal study. Sci Rep. (2020) 10:13421. doi: 10.1038/s41598-020-70285-7
49.Shang, X, Zhu, Z, Wang, W, Ha, J, and He, M. The association between vision impairment and incidence of dementia and cognitive impairment: a systematic review and meta-analysis. Ophthalmology. (2021) 128:1135–49. doi: 10.1016/j.ophtha.2020.12.029
50.Zhu, Z, Shi, D, Liao, H, Ha, J, Shang, X, Huang, Y, et al. Visual impairment and risk of dementia: the UK biobank study. Am J Ophthalmol. (2022) 235:7–14. doi: 10.1016/j.ajo.2021.08.010
51.Kuźma, E, Littlejohns, TJ, Khawaja, AP, Llewellyn, DJ, Ukoumunne, OC, and Thiem, U. Visual impairment, eye diseases, and dementia risk: a systematic review and meta-analysis. J Alzheimers Dis. (2021) 83:1073–87. doi: 10.3233/JAD-210250
52.Gray, CS, Karimova, G, Hildreth, AJ, Crabtree, L, Allen, D, and O’connell, JE. Recovery of visual and functional disability following cataract surgery in older people: Sunderland cataract study. J Cataract Refract Surg. (2006) 32:60–6. doi: 10.1016/j.jcrs.2005.07.040
53.Meuleners, LB, Hendrie, D, Fraser, ML, Ng, JQ, and Morlet, N. The impact of first eye cataract surgery on mental health contacts for depression and/or anxiety: a population-based study using linked data. Acta Ophthalmol. (2013) 91:e445–9. doi: 10.1111/aos.12124
54.Miyata, K, Yoshikawa, T, Morikawa, M, Mine, M, Okamoto, N, Kurumatani, N, et al. Effect of cataract surgery on cognitive function in elderly: results of Fujiwara-Kyo eye study. PLoS One. (2018) 13:e0192677. doi: 10.1371/journal.pone.0192677
55.Mylona, I, Aletras, V, Ziakas, N, and Tsinopoulos, I. Successful cataract surgery leads to an improvement in depressive symptomatology. Ophthalmic Res. (2021) 64:50–4. doi: 10.1159/000508954
56.Grodstein, F, Chen, J, and Hankinson, SE. Cataract extraction and cognitive function in older women. Epidemiology. (2003) 14:493–7. doi: 10.1097/01.ede.0000083503.34133.8c
57.Anstey, KJ, Lord, SR, Hennessy, M, Mitchell, P, Mill, K, and von Sanden, C. The effect of cataract surgery on neuropsychological test performance: a randomized controlled trial. J Int Neuropsychol Soc. (2006) 12:632–9. doi: 10.1017/S1355617706060954
58.Yu, W-K, Chen, Y-T, Wang, S-J, Kuo, S-C, Shia, B-C, and Liu, CJ-L. Cataract surgery is associated with a reduced risk of dementia: a nationwide population-based cohort study. Eur J Neurol. (2015) 22:1370–7. doi: 10.1111/ene.12561
59.Lin, H, Zhang, L, Lin, D, Chen, W, Zhu, Y, Chen, C, et al. Visual restoration after cataract surgery promotes functional and structural brain recovery. EBioMedicine. (2018) 30:52–61. doi: 10.1016/j.ebiom.2018.03.002
60.Lee, CS, Gibbons, LE, Lee, AY, Yanagihara, RT, Blazes, MS, Lee, ML, et al. Association between cataract extraction and development of dementia. JAMA Intern Med. (2022) 182:134–41. doi: 10.1001/jamainternmed.2021.6990
61.Pellegrini, M, Bernabei, F, Schiavi, C, and Giannaccare, G. Impact of cataract surgery on depression and cognitive function: systematic review and meta-analysis. Clin Exp Ophthalmol. (2020) 48:593–601. doi: 10.1111/ceo.13754
62.Kniestedt, C, and Stamper, RL. Visual acuity and its measurement. Ophthalmol Clin N Am. (2003) 16:155–70. doi: 10.1016/S0896-1549(03)00013-0
63.Bailey, IL, and Lovie-Kitchin, JE. Visual acuity testing. From the laboratory to the clinic. Vis Res. (2013) 90:2–9. doi: 10.1016/j.visres.2013.05.004
64.Kaido, M, Dogru, M, Ishida, R, and Tsubota, K. Concept of functional visual acuity and its applications. Cornea. (2007) 26:S29–35. doi: 10.1097/ICO.0b013e31812f6913
65.Yamaguchi, T, Negishi, K, and Tsubota, K. Functional visual acuity measurement in cataract and intraocular lens implantation. Curr Opin Ophthalmol. (2011) 22:31–6. doi: 10.1097/ICU.0b013e3283414f36
66.Packer, M, Fine, IH, and Hoffman, RS. Functional vision, wavefront sensing, and cataract surgery. Int Ophthalmol Clin. (2003) 43:79–91. doi: 10.1097/00004397-200343020-00009
67.Hawkins, AS, Szlyk, JP, Ardickas, Z, Alexander, KR, and Wilensky, JT. Comparison of contrast sensitivity, visual acuity, and Humphrey visual field testing in patients with glaucoma. J Glaucoma. (2003) 12:134–8. doi: 10.1097/00061198-200304000-00008
68.Day, AC, Wormald, R, Coronini-Cronberg, S, and Smith, R. The Royal College of ophthalmologists’ cataract surgery commissioning guidance: executive summary. Eye (Lond). (2016) 30:498–502. doi: 10.1038/eye.2015.271
69.NICE. Cataracts in Adults: Management Guidance. NICE Guidel 77. (2017) Available at: www.nice.org.uk/guidance/ng77
70.Day, AC, Donachie, PH, Sparrow, JM, and Johnston, RL. The Royal College of Ophthalmologists' National Ophthalmology Database study of cataract surgery: report 1, visual outcomes and complications. Eye (Lond). (2015 Apr) 29:552–60. doi: 10.1038/eye.2015.3
71.Althiabi, S, Aljbreen, AJ, Alshutily, A, and Althwiny, FA. Postoperative endophthalmitis after cataract surgery: an update. Cureus. (2022) 14:e22003. doi: 10.7759/cureus.22003
72.Durr, GM, and Ahmed, IIK. Intraocular lens complications: Decentration, uveitis-glaucoma-Hyphema syndrome, opacification, and refractive surprises. Ophthalmology. (2021) 128:e186–94. doi: 10.1016/j.ophtha.2020.07.004
73.Mencucci, R, Vignapiano, R, Rubino, P, Favuzza, E, Cantera, E, Aragona, P, et al. Iatrogenic dry eye disease: dealing with the conundrum of post-cataract discomfort. A P.I.C.a.S.S.O. board narrative review. Ophthalmol Ther. (2021) 10:211–23. doi: 10.1007/s40123-021-00332-7
74.Lord, SR, and Dayhew, J. Visual risk factors for falls in older people. J Am Geriatr Soc. (2001) 49:508–15. doi: 10.1046/j.1532-5415.2001.49107.x
75.Tinetti, ME, Speechley, M, and Ginter, SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. (1988) 319:1701–7. doi: 10.1056/NEJM198812293192604
76.Campbell, AJ, Borrie, MJ, and Spears, GF. Risk factors for falls in a community-based prospective study of people 70 years and older. J Gerontol. (1989) 44:M112–7. doi: 10.1093/geronj/44.4.M112
77.Lord, SR, Clark, RD, and Webster, IW. Physiological factors associated with falls in an elderly population. J Am Geriatr Soc. (1991) 39:1194–200. doi: 10.1111/j.1532-5415.1991.tb03574.x
78.Lord, SR, Clark, RD, and Webster, IW. Visual acuity and contrast sensitivity in relation to falls in an elderly population. Age Ageing. (1991) 20:175–81. doi: 10.1093/ageing/20.3.175
79.Testa, G, De Salvo, S, Boscaglia, S, Montemagno, M, Longo, A, Russo, A, et al. Hip fractures and visual impairment: is there a cause-consequence mechanism? J Clin Med. (2022) 11:143926. doi: 10.3390/jcm11143926
80.Ribeiro, F, Cochener, B, Kohnen, T, Mencucci, R, Katz, G, Lundstrom, M, et al. Definition and clinical relevance of the concept of functional vision in cataract surgery ESCRS position statement on intermediate vision: ESCRS functional vision working group. J Cataract Refract Surg. (2020) 46:S1–3. doi: 10.1097/j.jcrs.0000000000000096
81.Blancafort Alias, S, Del Campo, CZ, Salvador-Miras, I, Luna Mariné, S, Gómez Prieto, MJ, Liñán Martín, F, et al. Exploring vision-related quality of life: a qualitative study comparing patients’ experience of cataract surgery with a standard Monofocal IOL and an enhanced Monofocal IOL. Clin Ophthalmol. (2022) 16:1641–52. doi: 10.2147/OPTH.S358386
82.Mencucci, R, Cennamo, M, Venturi, D, Vignapiano, R, and Favuzza, E. Visual outcome, optical quality, and patient satisfaction with a new monofocal IOL, enhanced for intermediate vision: preliminary results. J Cataract Refract Surg. (2020) 46:378–87. doi: 10.1097/j.jcrs.0000000000000061
Keywords: cataract, cataract surgery, functional vision, quality of vision, elderly, frailty, intraocular lenses, accidental falls
Citation: Mencucci R, Stefanini S, Favuzza E, Cennamo M, De Vitto C and Mossello E (2023) Beyond vision: Cataract and health status in old age, a narrative review. Front. Med. 10:1110383. doi: 10.3389/fmed.2023.1110383
Edited by:
Hao Chen, Affiliated Eye Hospital to Wenzhou Medical University, ChinaReviewed by:
Francesco Maria D’Alterio, Imperial College Healthcare NHS Trust, United KingdomJacqueline Chua, Singapore National Eye Center, Singapore
Copyright © 2023 Mencucci, Stefanini, Favuzza, Cennamo, De Vitto and Mossello. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rita Mencucci, cml0YS5tZW5jdWNjaUB1bmlmaS5pdA==
 Rita Mencucci
Rita Mencucci Simone Stefanini
Simone Stefanini Eleonora Favuzza
Eleonora Favuzza Michela Cennamo
Michela Cennamo Chiara De Vitto1
Chiara De Vitto1 Enrico Mossello
Enrico Mossello