- Department of Psychology and Center for Applied Neuroscience, University of Cyprus, Nicosia, Cyprus
Introduction: An essential element of quality aging is the maintenance of cognitive and psychosocial functioning. The principal objective of the present paper was to present the theoretical framework, content and process evaluation of a newly developed multi-dimensional group intervention designed to strengthen/improve areas of cognitive and psychosocial functioning in adults over 65.
Methods: The intervention implements multiple methodologies aiming to facilitate contextual integration of learned concepts and strategies derived from clinical psychology and rehabilitation. It moves seamlessly on the cognition–emotion axes and consists of five active ingredients selected to address challenges associated with aging: Memory Compensatory Strategies, Problem-Solving, Emotion Regulation, Mindfulness, and Locus of Control. Thirty participants joined the intervention group aged 65–75 years (M = 69.03; SD = 3.04). All 30 participants who were included in the intervention group completed the program.
Results: Results from the Participant Satisfaction Scale indicate that the program was perceived very positively by participants, who also reported implementing their newly learned strategies in activities of daily life. Furthermore, there was high correlation between internal locus of control and the learned strategies.
Discussion: The outcomes of this analysis indicate that the intervention is feasible and well tolerated by our target group. This multidimensional intervention may offer a valuable contribution to public health care and dementia prevention for older adults.
Clinical Trial Registration: [https://clinicaltrials.gov/ct2/results?cond=NCT01481246], identifier [NCT01481246].
Introduction
The increase in life expectancy and health concerns associated with demographic aging is of global interest. An essential element of quality aging is the maintenance of brain health and actions to prevent dementia (1).
The literature supports a biopsychosocial perspective aiming at the development and implementation of interventions that target concepts such as successful aging, active aging and healthy cognitive aging (2, 3). Common to all concepts, is the need to develop and maintain functional capacity of older people, emphasizing in psychosocial and cognitive factors.
In line with the biopsychosocial approach, there has been a growing interest in interventions that adopt a multidimensional approach to cognitive aging (4). Some studies used a multidimensional approach for raising awareness of modifiable factors that contribute to cognitive decline such as physical activity, nutrition, interpersonal relations, and stress management, showing a significant increase in raising awareness after the intervention, indicating the effectiveness of such educational programs (5, 6). Another study used everyday memory and metacognitive intervention to improve everyday functioning (7) by focusing on improving older adults’ ability to achieve cognitively challenging everyday life tasks. Results showed improvements in everyday memory functioning and extended functional independence. Hoogenhout et al. (8), focused on psychoeducation for cognitive health through the use of self-regulation over habitual behaviors that often interfere with daily functioning. Their findings indicated reductions in negative emotional reactions toward cognitive aging, which, they assert is a prerequisite for improved subjective cognitive functioning and well-being. Finally, Ruvalcaba and Merino (9) promoted quality of life, physical activity, improved nutrition and cognitive function, through the use of theoretical–practical intervention. Results showed improvements in self-efficacy for quality of life, physical activity, nutrition and cognitive function.
The present research is part of a systematic effort to design and implement interventions that promote healthy cognitive aging, targeting cognitive and psychosocial abilities. The new intervention extends previous research and integrates knowledge from clinical psychology and cognitive rehabilitation. It conceptualizes five active ingredients which are trained sequentially and in parallel and targets multiple outcomes. Furthermore, the intervention goes beyond the simple didactic mode of transmitting information, to the implementation of role-play and case scenarios from real life to provide opportunities for application of the new skills in the real-life context. At the same time, the intervention addresses a relatively stable component of personality, that of locus of control, whose modification is targeted through the intervention. The purpose of the present article, is to describe the intervention’s theoretical background, content and methodology in order to enable application and replication by researchers in cognitive and psychosocial rehabilitation. In addition, it provides information on the intervention’s feasibility and acceptability by the participants as recommended by the literature (8, 10, 11).
Integrating cognitive and psychosocial dimensions for the group intervention
The present novel multidimensional, non-pharmaceutical group intervention integrates key theoretical principles from clinical psychology and cognitive rehabilitation to improve cognitive and psychosocial functioning in adults over 65. The intervention moves seamlessly on the cognition–emotion axes and consists of five active ingredients selected to address challenges associated with aging: Memory Compensatory Strategies, Problem-Solving, Emotion Regulation, Mindfulness, and Locus of Control. These active ingredients were specifically selected as they are important for the cognitive and psychosocial well-being of older people and deficiencies in these areas may pose a threat to independent living and successful aging. The intervention integrated concepts of cognitive rehabilitation such as training in memory compensation strategies and problem-solving and from clinical psychology such as applied emotional regulation strategies, mindfulness, and locus of control, bringing to light the “hot” emotional aspects of executive functions (12). Hot executive functions include future-oriented cognitive processes relevant to environments or situations that can generate emotions and encompass motivation, decision making and social behaviors (13). Those connections between emotion and cognition help maximize functionality in daily life.
The above elements are important novel aspects of this intervention. As an example, previous interventions make reference to stress management through relaxation techniques (5) or the reduction of negative emotional reactions through positive thinking (14). The present intervention, in addition to relaxation to assist with stress management, incorporates concepts of mindfulness and emotion regulation in conjunction with problem-solving strategies, to build connections between emotion and cognition and to help maximize functionality in daily life.
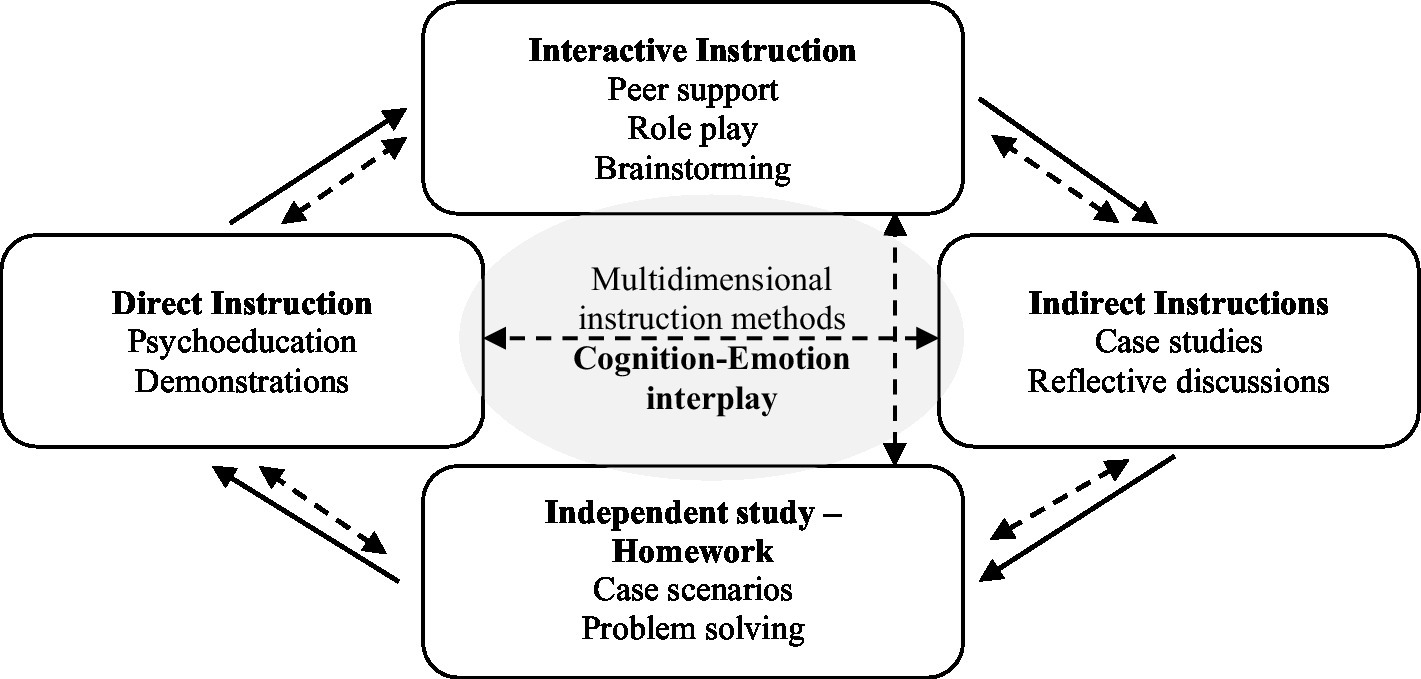
Participants were trained on the interplay between cognition and emotion and the 10-week group intervention incorporated didactic (psychoeducational) methodologies, role-play, peer support, and take-home exercises for contextual integration of learned concepts and strategies. Figure 1 presents the multidimensional instruction methods used. Each session begins with direct instruction, which continues with interactive instruction and indirect instruction and concludes with independent study. In all methods, both cognitive and emotional processes are trained. During the program, the various teaching methods are aligned to positively reinforce each other. For example, during training in the use of Memory Compensation Strategies, interactive teaching methods such as role play and peer support, reinforce indirect teaching such as case studies, which in turn facilitate the participant’s ability to complete homework and in turn reinforce indirect teaching methods such reflective discussions in the next session. Figure 2 presents the conceptual framework of the design of the intervention. The following sections provide a description of the key active ingredients and the primary outcome measures associated with each ingredient.
Memory compensation strategies
Since memory problems are the most obvious complaints in older people (15), most interventions have focused on strengthening the mnemonic function and the implementation of compensatory strategies. Memory Compensation Strategies (MCS) refer to a group of mechanisms through which individuals can continue to perform well in complex tasks despite having experienced deficits or reductions in memory capacity (16). MCS were incorporated as a key cognitive strategy aiming to train participants to develop effective strategies that support effective information coding (17). Participants were trained in the use of eight internal (e.g., semantic correlation and repetition) and external strategies (e.g., notes and placing reminders) derived from educational psychology (18), and cognitive rehabilitation (19, 20). Importantly, the new intervention encouraged participants through in-house and takes home exercises to learn and incorporate new MCS strategies in addition to their established ones. Improvement in this area was measured by “Scale of Implementation of Memory Compensation Strategies (21).”
Problem solving strategies
Along with MCS, Problem-solving (PS) training is an important aspect of cognitive interventions designed to enhance cognitive and psychosocial functioning (19, 22). PS is considered a component of executive functioning, a cognitive domain which, like memory, is also vulnerable to the effects of healthy aging (23–25). Older adults without neurodegenerative disease or mild cognitive decline, may demonstrate difficulties in problem solving and decision making (22, 26, 27).
The present study presented and trained participants in a five-step PS process as part of the “Think & Act” section. The PS training included four phases: (a) Brainstorming: participants were guided in generating possible and alternative solutions to solve a problem; (b) Planning and organization: individuals were guided in evaluating and comparing the solutions created and in defining the analytical implementation strategy for the selected solution; (c) Role play: practicing the strategies to scenarios presented by the researcher during the session; and (d) Generalization: applying their newly learned skills to a real-life problem at home as part of their homework assignment.
As part of the PS training, participants were guided in identifying areas of possible improvement for their overall health. Lifestyle factors such as nutrition and physical activities/movement were targeted as overall strategies promoting physical health and well-being. Specifically, deficiencies in those areas were identified individually for each participant and were approached with the PS process in order to implement positive changes to overall health. Improvement in this area was measured by “Problem-Solving Inventory” (28, 29).
Emotional regulation strategies
Emotional regulation (ER) is an important element of effective problem solving (30) and a key dimension of psychosocial functioning. ER is also considered an indicator of positive adaptation to the negative aspects of aging (31). ER was included in this study as a ‘hot’ area of executive functioning (32, 33) with the aim of enhancing psychosocial and cognitive functionality. ER was addressed through the “Stop & Relax” process which incorporated key elements of regulating emotions as described by Gratz and Roemer (34). Participants were trained to recognize, name and accept emotions but also to use diaphragmatic breathing in order to relax, reduce physical arousal and implement effective PS strategies using the “Think & Act” techniques. They were asked to maintain a weekly diary of emotional clarity with the aim of identifying and accepting emotions as well as practicing diaphragmatic breathing weekly. Improvement in this area was measured by “Difficulties in Emotion Regulation Scale” (34, 35).
Mindfulness
Mindfulness refers to the present-oriented attention within the self (e.g., body sense, thoughts, feelings) and outside (environment) without criticism (36). Research on mindfulness indicates that it is a beneficial modality for ER, EF, and memory (37–40). However, research on mindfulness and aging is understudied. The present study incorporated mindfulness as part of ER and the “Stop & Relax” procedures to facilitate emotional functioning, problem-solving, executive functioning, and memory performance. The combination of ER and mindfulness is thought to have an additive effect as compared to using each of the two in isolation. The implementation of mindfulness and other strategies addressed in the program, aimed at improving locus of control. Improvement in this area was measured by “Mindful Attention Awareness Scale” (41, 42).
Internal locus of control
Locus of Control (LC) is a psychological construct that evaluates beliefs about one’s ability to influence situations in their lives (internal LC) or whether these are left to external forces (external LC) (43). Research suggests that biological aging interferes with the sense of control in older people (44, 45). This decrease in perceptual control is clearly related to the increasing diffusion of age-related barriers and restrictions, such as biological and social changes (e.g., retirement, reduced incomes, cognitive changes, bereavement) (46).
LC may be modifiable in response to both life events and after training (46, 47). The present intervention integrates LC in all aspects of the program by empowering participants to gain knowledge the various aspects of aging, on implementing strategies for healthy physical and cognitive aging and applying methods to promote memory, PS and ER. Participants were encouraged to discuss personal obstacles and were guided to take systematic guidance actions in order to improve life outcomes and reduce beliefs that their lives depend on external factors (luck, strong others). The shift from external LC to internal LC could facilitate the implementation of cognitive and emotional strategies to promote healthy cognitive aging. Improvement in this area was measured by “Multidimensional Locus of Control” (29).
The aim of the present study was the implementation of a multi-dimensional group intervention designed to strengthen areas of cognitive and psychosocial functioning in adults over 65. The intervention implements multiple methodologies aiming to facilitate contextual integration of learned concepts and strategies derived from clinical psychology and rehabilitation. The intervention is novel as it moves seamlessly on the cognition–emotion axes and consists of five active ingredients selected to address challenges associated with aging: Memory Compensatory Strategies, Problem-Solving, Emotion Regulation, Mindfulness, and Locus of Control. It was hypothesized that participants would perceive the intervention as a useful approach to improve cognitive and emotional functioning and that those who demonstrated high levels of internal locus of control would report greater engagement in implementing their new knowledge in activities of daily living.
Methods
Participants
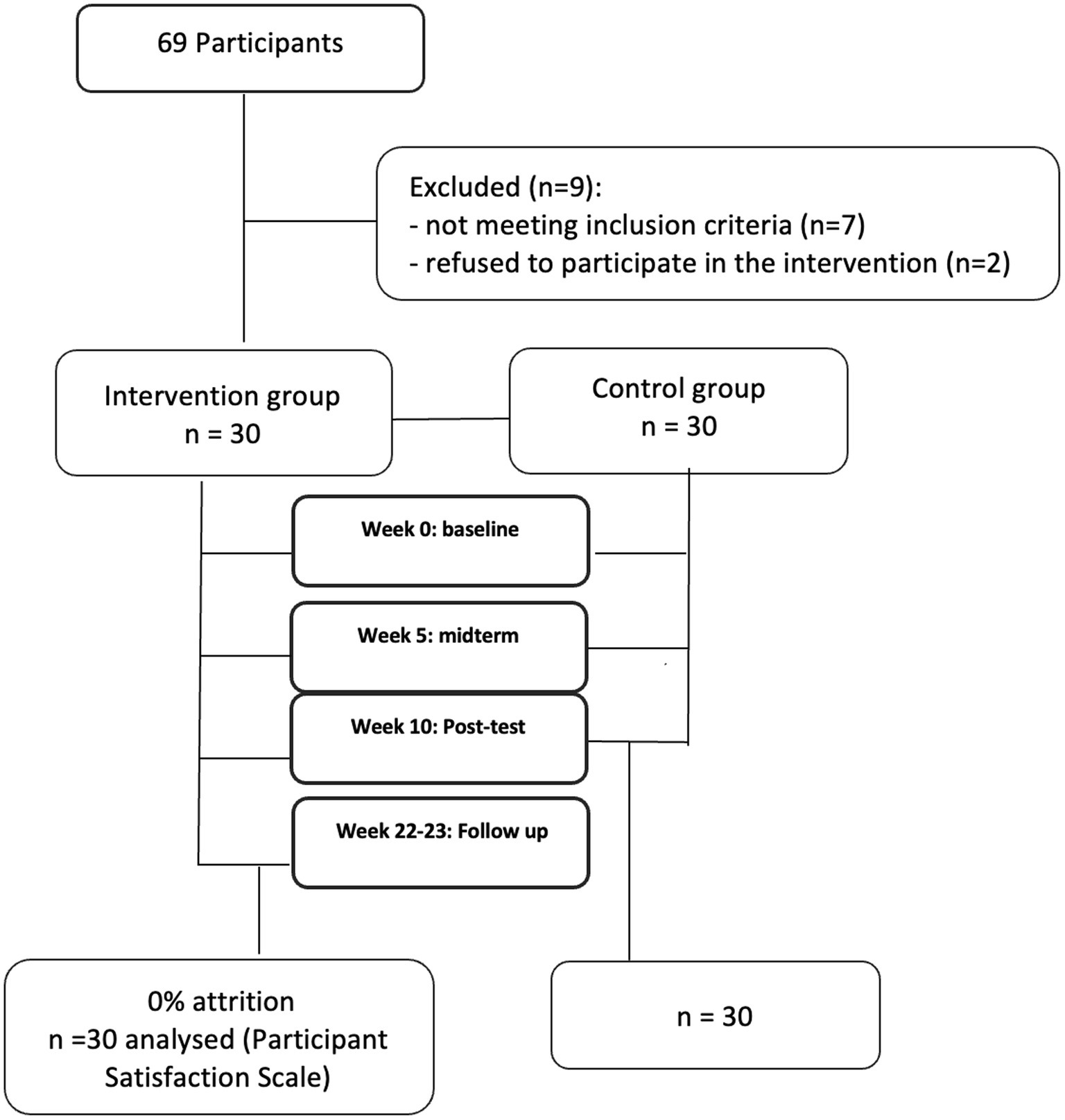
Sixty-nine community dwellers were initially recruited to participate in this study. Nine people were excluded due to non-compliance with the admission and exclusion criteria. This research was incorporated into the Neurocognitive Study of Aging (NEUROAGE) which is the first systematic and longitudinal study of cognitive aging in Cyprus (NCT01481246) (24, 48).
The remaining 60 participants were randomly assigned into the intervention and control groups. Thirty people joined the intervention group, of which 19 were women and 11 men aged 65–75 years (M = 69.03; SD = 3.04). The control group also consisted of 30 people, 21 of whom were women and nine men, aged 65–75 (M = 70.12; TA = 3.51). The level of education was quantified as the number of years of formal education achieved by each participant and ranged from 8 to 17 years (M = 11.7, SD = 2.11) for the intervention group, and for the control group (M = 11.76, TA = 2.02). The two groups were matched on key demographic variables as well as on the Mini-Mental State Examination performance (M = 28.31, SD = 1.80 for the intervention group and M = 28.06, SD = 1.95 for the control group). Figure 3 is the CONSORT diagram.
The inclusion criteria for all participants were the following: (1) Native Greek speakers; (2) males and females over the age of 60; (3) Good general health with no previous history of neurological disorder such as head trauma, stroke or neurodegenerative disorder; (4) No emotional or psychiatric disorder as defined by the Diagnostic-Statistical Manual of Mental Disorders, Fifth Edition (DSM-V); (5) Results on neurocognitive tasks falling within the normal range as derived from normative data of the NEUROAGE (within 1 and − 1 z scores).
Measures
Participants were initially evaluated with the neurocognitive evaluation lasting about 2 hours, which examined the general mental function, memory, executive functions and language as described by our previous work (24, 48). This evaluation was conducted to ensure normal cognitive function for the study participations.
In addition to the neurocognitive evaluation, the study implemented the following primary outcome (dependent) measures relevant to the theoretical components of the intervention and were administered at baseline, posttest and follow-up:
1. Multidimensional Locus of Control Inventory (29, 49).
2. Problem-Solving Inventory (28, 29).
3. Difficulties in Emotion Regulation Scale (34, 35).
4. Scale of Implementation of Memory Compensation Strategies (21).
5. Mindful Attention Awareness Scale (41, 42).
Participant satisfaction scale
For the purpose of this intervention, a questionnaire consisting of 18 statements was created to investigate the satisfaction of participants in key areas of the intervention and their ability to apply the new knowledge and skills in their daily lives. The questionnaire consists of three parts. The first part consists of statements in which participants rate their satisfaction with general aspects of the intervention such as the topics addressed in the meetings, the organization and preparation of the instructor and satisfaction with the instructor. Questions could be answered on a 5-point scale (1 = very dissatisfied, 5 = very satisfied). The second part consists of statements assessing the degree of agreement on issues specific to the intervention such as gaining knowledge on healthy cognitive aging, on overall motivation to increase locus of control, and the effectiveness of the group format. Questions could be answered on a 5-point scale (1 = disagrees absolutely, 5 = agrees absolutely). The third part includes statements to evaluate their ability to apply strategies learned during the program in their daily lives (i.e., memory, problem-solving, and Emotion regulation strategies). Questions could be answered on a 5-point scale (1 = poor, 5 = very good). A high internal consistency of the questionnaire was identified in the sample, with Cronbach’s a determined 0.91. Participant Satisfaction Scale was administered at the end of the intervention (10 week).
Multidimensional locus of control inventory
The Greek version of the Multidimensional Locus of Control was used (29). The scale consists of 24 items scored on a six-point Likert scale, ranging from −3 (Strongly Disagree) to +3 (Strongly Agree). The scale yields three distinct factors: Internality, Powerful Others, and Chance. Each subscale produces a unique score by adding up the eight responses and adding to the sum a constant of +24 to eliminate negative sums. Therefore, each respondent received three scores (each one ranging from 0 to 48) indicative of his/her relative view on each of the three dimensions. An individual could score high or low on all three dimensions. Acceptable internal consistency of the questionnaire was identified in the present sample, with Cronbach’s a determined 0.84 for Internality, 0.79 for Powerful Others, and 0.83 for Chance.
Study design
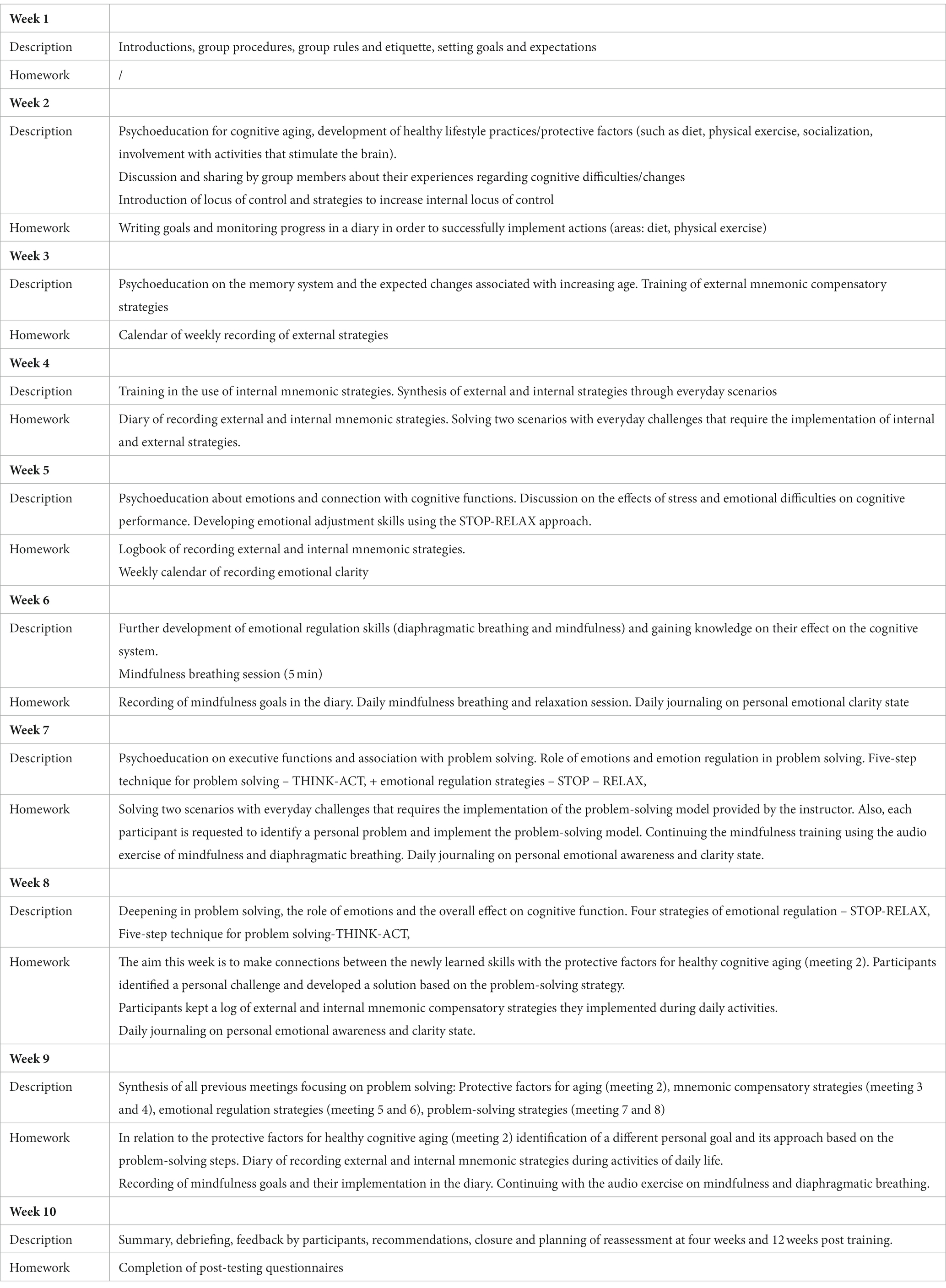
Participants were assigned into five groups of 6 people. The intervention was conducted weekly over ten, 90-min sessions, with a mid-point evaluation (at five weeks) and a post-treatment assessment at the end of the intervention. There was a follow-up assessment on the dependent measures 12 weeks after the end of the intervention. To reduce response bias error, all participants completed the questionnaire anonymously and privately; they placed the completed questionnaire in an envelope containing a unique code that was then used to manage the data.
Intervention procedures
The intervention was designed as 90-min weekly group meetings lasting 10 weeks. The intervention was developed by a doctoral-level licensed and certified academic speech-language pathologist with expertise in cognitive-communication disorders (F.C.) and a doctoral student in Clinical Psychology (A.C.) also licensed in School Psychology, who facilitated all sessions. Another graduate-level researcher monitored the process in each session with the aim of confirming that all groups and meetings followed the same content and procedures. The meetings were originally planned to be conducted in person. However, due to the restrictions implemented to control the spread of COVID-19, the intervention was transformed into an online format. Study participants were trained in person in the use of the Rakuten Viber online platform. This specific platform was selected as participants were more familiar with it and several were using it already in their daily lives. It has numerous options; e.g. it has high-quality video call, better voice quality with less noise throughout all bandwidths, in comparison with other free platforms and provides group chat rooms (50). These elements make this platform suitable for teleconferencing purposes. Viber also provides official desktop version for the apps that can be used in laptops or personal computers. In addition, a family member familiar with the specific platform was available to offer technical support at home during the start of each session. Participants received printed packets of materials required for the program in advance of each group session.
Presentation format
Each session began with a presentation, followed by direct practice in the use of the proposed strategies through scenarios provided by the researchers as well as through scenarios derived from their personal experience. The content was organized hierarchically aiming to connect the theoretical principles for memory, problem-solving, emotion regulation, and locus of control through psychoeducation and contextual training via role play, repetition, and weekly homework with real-life scenarios. The intervention was adaptive in that, e.g., success in week 8 was partly dependent on mastering content from week 2. The intervention’s content is listed in Table 1.
Statistical analyses
To investigate the satisfaction of participants in key areas of the intervention and their ability to apply the new knowledge and skills in their daily lives, standard descriptive statistics were utilized, including means, standard deviations and percentages. Pre and post-testing was conducted for all the primary outcome measures and mid-point assessment was conducted for the locus of control and memory strategies. For the purpose of the present study which was to explore potential associations between locus of control (LC) and the self-assessment of participants’ ability to apply their newly trained strategies upon completion of the intervention (at post-test), the post test measures were analyzed. Pearson’s correlations coefficients were performed to examine the relationships. All analyses were carried out with SPSS (version 27).
Results
Attrition rate
All 30 participants who were included in the intervention group completed the program. Most of them (94%) attended all 10 sessions. Three participants missed one session and one participant missed two sessions due to illness or family obligations.
Responses to the participant satisfaction scale
Participant responses regarding the general aspects of the intervention indicate that the majority of participants (90%) were extremely satisfied with the meeting topics (M = 4.90, SD = 0.30), with the organization and preparation of the instructor (97%, M = 4.96, SD = 0.30), and support provided by the instructor (96.7% M = 4.96, SD = 0.18). A high percentage of participants (86.7%) strongly agreed that the meetings were a positive experience (M = 4.88, SD = 0.34).
Participants reported high levels of satisfaction for gaining new knowledge and skills. Specifically, 87% indicated that the meetings met their expectations for receiving information related to cognitive health (M = 4.50, SD = 0.57) and 90% reported that the meetings met their expectations in developing new skills (M = 4.90, SD = 0.30). Specifically, 86.7% reported that they gained knowledge about risk factors for pathological aging (M = 4.86, SD = 0.34) and 86.7% that they learned applied strategies they can use in everyday life (M = 4.83, SD = 0.42). Most of the participants (76.3%) reported that the meetings motivated them to take control of their life and 76.7% felt motivated to take action for their cognitive health (M = 4.76, SD = 0.43). Finally, 63.3% indicated that they applied the general strategies they learned during the intervention for good cognitive health (e.g., healthy diet and exercise) (M = 4.56, SD = 0.42).
Regarding the group format of the intervention, 83.3% of participants strongly agreed that this format was optimal (M = 4.80, SD = 0.48) and the majority (66.7%) felt a strong connection with their group peers (MM = 4.66, SD = 0.59), and 63.7% felt supported by them (M = 4.30, SD = 0.66). In Table 2, the means, standard deviations, and percentages for all questions are presented in detail.
Applying trained skills
The majority (60–90%) of participants rated their ability to apply their newly learned strategies very highly. Specifically, their ability to apply Memory Compensation Strategies in their daily life was on average 4.73 (SD = 0.52) on a 5-point scale. Their ability to apply Emotion Regulation and Problem-Solving strategies in daily life was evaluated as 4.86 (SD = 0.43) and 4.55(SD = 0.50) respectively. Lastly, their ability to apply general life-style modification strategies to promote overall health (physical exercise and diet) was also rated highly 4.33 (SD = 0.54) on a 5-point scale.
Association between locus of control and application of trained skills
The internal LC subscale showed a positive correlation with the Memory Compensation Strategies, r(28) = 0.48, p < 0.001, Problem-Solving, r(28) = 0.74, p < 0.001, Emotion Regulation, r(28) = 0.64, p < 0.001 and general modification strategies for brain and cognitive health such as physical exercise and diet, r(28) = 0.58, p < 0.05. These findings indicate that individuals who reported an internal LC also reported greater engagement in using strategies trained by the program.
Discussion
The present novel multidimensional group intervention integrates key theoretical principles from cognitive rehabilitation and clinical psychology. This is one of the first multidimensional, non-pharmaceutical, theory driven interventions focusing on healthy adults over 65 with the purpose to strengthen/improve areas of cognitive and psychosocial functioning. The principal objective of the present paper was to present the theoretical framework of this intervention, the process of the program and results from the evaluation that was carried out to investigate participant satisfaction and implementation of their newly learned strategies in their daily lives. The outcomes of this analysis indicate that the intervention is feasible and well tolerated by our target group. Participants were committed to this intervention, as shown by zero dropout.
The intervention incorporated multiple methodologies for contextual integration of learned concepts and strategies: The current intervention adds to existing multidimensional psychoeducational interventions on cognitive aging which were mostly educational (5, 6, 8) through the implementation of multiple methodologies for contextual integration of active components. Specifically, direct instruction through psychoeducation, indirect instruction such as case studies, reflective discussions, interactive instruction such as role-play, peer support, online chatting, and independent study via take-home exercises, journals, and case scenarios were integrated during the 10-week period. Results indicate that participants were satisfied with the implementation strategy of the present intervention and with their ability to gain knowledge and apply their newly learned skills.
The intervention incorporated five key active ingredients: Memory Compensation Strategies (MCS), Problem-Solving (PS), Emotion Regulation (ER), Mindfulness, and Locus of Control (LC), in order to address challenges associated with healthy aging. The present findings suggest that, upon completion of the program, participants were able to apply their new knowledge and skills in activities of their daily life, upon completion of the program.
Internal LC, a key ingredient of the present intervention, was associated with participant engagement and their ability to use skills and strategies trained during the program in everyday life. Key aspects of internal locus of control were incorporated in all meetings through active engagement and investment in the learning process. Participants were systematically guided to take action during the group sessions and in their daily lives and to improve their cognitive and psychosocial functioning. Results from the satisfaction questionnaire indicate that most participants reported motivation to take control and action to improve their life. In fact, higher levels of internal LC increased the likelihood of engagement in using strategies trained by the program. This finding has important implications for interventions targeting healthy older adults, since internal LC may maximize the likelihood of active participation in the rehabilitation process by applying compensatory strategies to improve cognition and emotional functioning such as problem-solving and emotion regulation (51).
Another important element of the study was the group format as the delivery modality of the intervention. The group format encouraged the interaction of the participants, elements that potentially contributed to the commitment of the group. The overwhelming majority of participants reported satisfaction with the group format and a connection with their teammates. These results are consistent with a recent meta-analysis showing that interventions produce maximum benefits when participants train in groups (52). The present intervention is conducive to a group format as it offers an opportunity for participants to support each other, increase motivation and allow people to share their emotions and concerns about their cognitive and everyday problems.
Another component of the group intervention in this study was the online delivery method. As mentioned, the online platform was selected as the delivery method in response to the pandemic and the requirement for physical distancing during COVID-19. The present online intervention promoted social interaction during the meetings and the opportunity for online chatting between weekly sessions, creating rapport among the group participants. Findings indicate that the creation of online chats for the group members should be an important consideration when organizing and designing such programs, even if the delivery of the intervention is in the conventional in person format.
In summary, the present study indicates that this theory driven group intervention is feasible and well tolerated by the study participants. Based on the process evaluation and satisfaction results, participants were satisfied with the implementation strategy of the intervention and their ability to gain knowledge and most importantly apply their newly learned skills in their daily life. The current study described the background and content of the intervention program in detail to enable application and replication by other clinicians and researchers. We are currently collecting follow-up data from our study participants and we will be disseminating the outcomes of the intervention to the research community in future publications. In conclusion, the intervention program that was described in the current paper may offer a valuable contribution to the design of a multidimensional intervention and contribution to public health care for older adults, especially in the face of our rapidly aging Western society.
Data availability statement
The datasets presented in this article are not readily available because the dataset used in this study belongs to an ongoing research project. Therefore, no data can be shared. Requests to access the datasets should be directed to AC, ZHIuY2hhZGppa3lwcmlhbm91QGdtYWlsLmNvbQ== and FC, Zm9maWNAdWN5LmFjLmN5.
Ethics statement
The studies involving human participants were reviewed and approved by Cyprus National Bioethics Committee. The patients/participants provided their written informed consent to participate in this study.
Author contributions
AC conceptualized and designed the project, coordinated the data collection, analyzed data, and wrote the manuscript. FC conceptualized and designed the project, supervised the data collection, analysis, and wrote the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was co-funded by the European Regional Development Fund and the Republic of Cyprus through the Research and Innovation Foundation (EXCELLENCE/1216/0404).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bondi, MW, Edmonds, EC, and Salmon, DP. Alzheimer’s disease: past, present, and future. J Int Neuropsychol Soc. (2017) 23:818–31. doi: 10.1017/S135561771700100X
2. Mendoza-Ruvalcaba, NM, and Arias-Merino, ED. “I am active”: effects of a program to promote active aging. Clin Interv Aging. (2015) 10:829–37. doi: 10.2147/CIA.S79511
3. Taghdisi, MH, Estebsari, F, Rahimi Foroushani, A, Eftekhar Ardebili, H, Shojaeizadeh, D, Dastoorpoor, M, et al. The educational program based on the successful aging approach in elders health-promoting behaviors: a clinical trial study. Razi J Med Sci. (2014) 21:26–36.
4. Zanjari, N, Sani, MS, Chavoshi, MH, Rafiey, H, and Shahboulaghi, FM. Successful aging as a multidimensional concept: an integrative review. Med J Islam Repub Iran. (2017) 31:686–91. doi: 10.14196/mjiri.31.100
5. Estebsari, F, Taghdisi, MH, Foroushani, AR, Ardebili, HE, and Shojaeizadeh, D. An educational program based on the successful aging approach on health-promoting behaviors in the elderly: a clinical trial study. Iran Red Crescent Med J. (2014) 16:e16314. doi: 10.5812/ircmj.16314
6. Hsu, HC, Kuo, T, Lin, JP, Hsu, WC, Yu, CW, Chen, YC, et al. A cross-disciplinary successful aging intervention and evaluation: comparison of person-to-person and digital-assisted approaches. Int J Environ Res Public Health. (2018) 15:913. doi: 10.3390/ijerph15050913
7. Pearman, A, Lustig, E, Hughes, ML, and Hertzog, C. Initial evidence for the efficacy of an everyday memory and metacognitive intervention. Innov Aging. (2020) 4:igaa054. doi: 10.1093/geroni/igaa054
8. Hoogenhout, EM, de Groot, RH, Van der Elst, W, and Jolles, J. Effects of a comprehensive educational group intervention in older women with cognitive complaints: a randomized controlled trial. Aging Ment Health. (2012) 16:135–44. doi: 10.1080/13607863.2011.598846
9. Ruvalcaba, NM, and Arias-Merino, ED. “I am active”: effects of a program to promote active aging. Clin Interv Aging. (2015) 10:829. doi: 10.2147/CIA.S79511
10. Miller, CJ, Smith, SN, and Pugatch, M. Experimental and quasi-experimental designs in implementation research. Psychiatry Res. (2020) 283:112452. doi: 10.1016/j.psychres.2019.06.027
11. Proctor, E, Silmere, H, Raghavan, R, Hovmand, P, Aarons, G, Bunger, A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health Serv Res. (2011) 38:65–76. doi: 10.1007/s10488-010-0319-7
12. Zelazo, PD, Qu, L, and Kesek, AC. Hot executive function: Emotion and the development of cognitive control. In: Calkins SD, Bell MA, editors. Child development at the intersection of emotion and cognition. American Psychological Association. (2010). p. 97–111.
13. Zelazo, PD, and Carlson, SM. Hot and cool executive function in childhood and adolescence: Development and plasticity. Child development perspectives. (2012) 6:354–60.
14. Mendoza-Ruvalcaba, NM, and Fernández-Ballesteros, R. Effectiveness of the vital aging program to promote active aging in Mexican older adults. Clinical interventions in aging. (2016) 1631–44.
15. Mitchell, AJ, Beaumont, H, Ferguson, D, Yadegarfar, M, and Stubbs, B. Risk of dementia and mild cognitive impairment in older people with subjective memory complaints: meta-analysis. Acta Psychiatr Scand. (2014) 130:439–51. doi: 10.1111/acps.12336
16. Farias, ST, Gravano, J, Weakley, A, Schmitter-Edgecombe, M, Harvey, D, Mungas, D, et al. The everyday compensation (EComp) questionnaire: construct validity and associations with diagnosis and longitudinal change in cognition and everyday function in older adults. J Int Neuropsychol Soc. (2020) 26:303–13. doi: 10.1017/S135561771900119X
17. Kinsella, GJ, Ames, D, Storey, E, Ong, B, Pike, KE, Saling, MM, et al. Strategies for improving memory: a randomized trial of memory groups for older people, including those with mild cognitive impairment. J Alzheimers Dis. (2016) 49:31–43. doi: 10.3233/JAD-150378
18. Oxford, R. Language Learning Strategies What Every Teacher Should Know. Boston, MA: Heinle & heinle Publishers (1990).
19. Cicerone, KD, Goldin, Y, Ganci, K, Rosenbaum, A, Wethe, JV, Langenbahn, DM, et al. Evidence-based cognitive rehabilitation: systematic review of the literature from 2009 through 2014. Arch Phys Med Rehabil. (2019) 100:1515–33. doi: 10.1016/j.apmr.2019.02.011
20. Lin, P, LaMonica, HM, Naismith, SL, and Mowszowski, L. Memory compensation strategies in older people with mild cognitive impairment. J Int Neuropsychol Soc. (2020) 26:86–96. doi: 10.1017/S1355617719000912
21. Chadjikyprianou, A. Cognitive Aging: Development of an Intervention Program to Increase Cognitive and Psychosocial Functioning. Nicosia: University of Cyprus, Faculty of Social Sciences and Education, Cyprus (2022).
22. Nguyen, CM, Chen, KH, and Denburg, NL. The use of problem-solving therapy for primary care to enhance complex decision-making in healthy community-dwelling older adults. Front Psychol. (2018) 9:870. doi: 10.3389/fpsyg.2018.00870
23. Drigas, A, and Karyotaki, M. Executive functioning and problem solving: a bidirectional relation. Int J Eng Pedagogy. (2019) 9:76–98. doi: 10.3991/ijep.v9i3.10186
24. Constantinidou, F, Christodoulou, M, and Prokopiou, J. The effects of age and education on executive function and oral naming performance in Greek Cypriot adults. The neurocognitive study for the aging. Folia Phoniatr Logop. (2012) 64:187–98. doi: 10.1159/000340015
25. Giogkaraki, E, Michaelides, MP, and Constantinidou, F. The role of cognitive reserve in cognitive aging: results from the neurocognitive study on aging. J Clin Exp Neuropsychol. (2013) 35:1024–35. doi: 10.1080/13803395.2013.847906
26. Sproten, A, Diener, C, Fiebach, C, and Schwieren, C. Aging and decision making: How aging affects decisions under uncertainty (No. 508). Discussion Paper Series. (2010).
27. Wood, S, and Lichtenberg, PA. Financial capacity and financial exploitation of older adults: research findings, policy recommendations and clinical implications. Clin Gerontol. (2017) 40:3–13. doi: 10.1080/07317115.2016.1203382
28. Heppner, PP, and Petersen, CH. The development and implications of a personal problem-solving inventory. J Couns Psychol. (1982) 29:66–75. doi: 10.1037/0022-0167.29.1.66
29. Kourmousi, N, Xythali, V, and Koutras, V. Reliability and validity of the multidimensional locus of control IPC scale in a sample of 3668 Greek educators. Soc Sci. (2015) 4:1067–78. doi: 10.3390/socsci4041067
30. Hannula, MS. Emotions in problem solving In:. Selected Regular Lectures from the 12th International Congress on Mathematical Education. New York: Springer International Publishing (2015). 269–88.
31. Knight, M, and Ponzio, A. The effects of emotion regulation on explicit memory depend on strategy and testing method. Emotion. (2013) 13:1041–54. doi: 10.1037/a0033533
32. Zelazo, PD, and Cunningham, WA. Executive function: mechanisms underlying emotion regulation In: JJ Gross, editor. Handbook of Emotion Regulation. New York: The Guilford Press (2007). 135–58.
33. Zelazo, PD. Executive function and psychopathology: a neurodevelopmental perspective. Annu Rev Clin Psychol. (2020) 16:431–54. doi: 10.1146/annurev-clinpsy-072319-024242
34. Gratz, KL, and Roemer, L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. (2004) 26:41–54. doi: 10.1023/B:JOBA.0000007455.08539.94
35. Mitsopoulou, E, Kafetsios, K, Karademas, E, Papastefanakis, E, and Simos, PG. The Greek version of the difficulties in emotion regulation scale: testing the factor structure, reliability and validity in an adult community sample. J Psychopathol Behav Assess. (2013) 35:123–31. doi: 10.1007/s10862-012-9321-6
36. Kabat-Zinn, J. The liberative potential of mindfulness. Mindfulness. (2021) 12:1555–63. doi: 10.1007/s12671-021-01608-6
37. Jha, AP, Denkova, E, Zanesco, AP, Witkin, JE, Rooks, J, and Rogers, SL. Does mindfulness training help working memory ‘work’better? Curr Opin Psychol. (2019) 28:273–8. doi: 10.1016/j.copsyc.2019.02.012
38. Lueke, A, and Lueke, N. Mindfulness improves verbal learning and memory through enhanced encoding. Mem Cogn. (2019) 47:1531–45. doi: 10.3758/s13421-019-00947-z
39. Nien, JT, Wu, CH, Yang, KT, Cho, YM, Chu, CH, Chang, YK, et al. Mindfulness training enhances endurance performance and executive functions in athletes: an event-related potential study. Neural Plast. (2020) 2020:1–12. doi: 10.1155/2020/8213710
40. Zhou, H, Liu, H, and Deng, Y. Effects of short-term mindfulness-based training on executive function: divergent but promising. Clin Psychol Psychother. (2020) 27:672–85. doi: 10.1002/cpp.2453
41. Brown, KW, and Ryan, RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. (2003) 84:822–48. doi: 10.1037/0022-3514.84.4.822
42. Mantzios, M, Wilson, JC, and Giannou, K. Psychometric properties of the Greek versions of the self-compassion and mindful attention and awareness scales. Mindfulness. (2015) 6:123–32. doi: 10.1007/s12671-013-0237-3
43. Lefcourt, HM. Locus of Control: Current Trends in Theory and Research. Hove: Psychology Press (2014).
44. Infurna, FJ, and Mayer, A. The effects of constraints and mastery on mental and physical health: conceptual and methodological considerations. Psychol Aging. (2015) 30:432–48. doi: 10.1037/a0039050
45. Mirowsky, J, and Ross, CE. Life course trajectories of perceived control and their relationship to education. Am J Sociol. (2007) 112:1339–82. Sheppes. doi: 10.1086/511800
46. Anderson, E, Cochrane, A, Golding, J, and Nowicki, S. Locus of control as a modifiable risk factor for cognitive function in midlife. Aging (Albany NY). (2018) 10:1542–55. doi: 10.18632/aging.101490
47. Georgescu, D, Duiu, A, Cheiban, T, Mazilu, T, Rotariu, A, Toma, D, et al. The relationship between locus of control, personal behavior, self-efficacy and resilience. Romanian J Cogn Behav Therapy Hypnosis. (2019) 6:1–12.
48. Chadjikyprianou, A, Hadjivassiliou, M, Papacostas, S, and Constantinidou, F. The neurocognitive study for the aging: longitudinal analysis on the contribution of sex, age, education and APOE ɛ4 on cognitive performance. Front Genet. (2021) 12:531. doi: 10.3389/fgene.2021.680531
49. Levenson, H. Multidimensional locus of control in psychiatric patients. J Consult Clin Psychol. (1973) 41:397–404. doi: 10.1037/h0035357
50. Sutikno, T, Handayani, L, Stiawan, D, Riyadi, MA, and Subroto, IMI. WhatsApp, viber and telegram: which is the best for instant messaging? Int J Elect Comput Eng. (2016) 6:2088–8708. doi: 10.11591/ijece.v6i3.10271
51. Constantinidou, F, and Kennedy, M. Traumatic brain injury In: P Coppens and I Papademetriou, editors. Aphasia and Neurogenic Communication Disorders, 3rd Edn. Boston, MA: Jones & Bartlett Publishers (2022).
Keywords: intervention, aging, cognitive aging, psychosocial functioning, cognitive functioning, emotion regulation, memory compensation strategies, locus of control
Citation: Chadjikyprianou A and Constantinidou F (2023) A new multidimensional group intervention for cognitive and psychosocial functioning for older adults: Background, content, and process evaluation. Front. Med. 10:1161060. doi: 10.3389/fmed.2023.1161060
Edited by:
Takao Yamasaki, Minkodo Minohara Hospital, JapanReviewed by:
Briana Nicole Sprague, University of Pittsburgh, United StatesDavid Eugene Vance, University of Alabama at Birmingham, United States
Copyright © 2023 Chadjikyprianou and Constantinidou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fofi Constantinidou, Zm9maWNAdWN5LmFjLmN5
†ORCID: Fofi Constantinidou https://orcid.org/0000-0002-7928-8363
 Andreas Chadjikyprianou
Andreas Chadjikyprianou Fofi Constantinidou
Fofi Constantinidou