- 1Chengdu Women's and Children's Central Hospital, School of Medicine, University of Electronic Science and Technology of China, Chengdu, China
- 2School of Medicine, University of Electronic Science and Technology of China, Chengdu, China
- 3Department of Gynaecology and Obstetrics, Shanghai Tongren Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, China
- 4Psychosomatic Medical Center, The Fourth People's Hospital of Chengdu, Chengdu, China
Introduction: Although previous studies have shown that vaginal natural orifice transluminal endoscopic surgery (vNOTES) has the advantages of causing less pain, faster recovery, and better concealment of surgical incisions, which aligns with the concept of the day-care procedure, this approach poses a greater risk of damaging adjacent organs (i. e., rectum and bladder) due to its anatomical specificity. Moreover, the day-care procedure may lead to relatively less preoperative evaluation and postoperative care. Hence, it is necessary to explore the safety and effectiveness of vNOTES for ovarian cystectomy in the day-care procedure, to provide a theoretical basis for the wider development of vNOTES surgery.
Materials and methods: This retrospective study included 131 patients at our hospital who underwent ovarian cystectomy from September 2021 to October 2022. Based on the surgical approach, patients were classified into transumbilical laparoendoscopic single-site surgery (LESS) and vNOTES groups. The patients' demographic characteristics and follow-up data were collected during the perioperative period and 1-month postoperatively.
Results: Vaginal natural orifice transluminal endoscopic surgery has less postoperative exhaust time, a lower postoperative 6-hour pain score, and a lower incidence of analgesic drug use, with higher surgical conversion incidence. Multiple linear regression analysis showed that the surgical conversion, chocolate cyst, bilateral cyst, and pelvic adhesion increased the operation duration by ~43 (95% CI: 10.309, 68.152, p < 0.001), 15 (95% CI: 6.342, 45.961, p = 0.036), 10 (95% CI: 3.07, 40.166, p = 0.019), and 8 (95% CI: 4.555, 26.779, p = 0.035) min, respectively. Interestingly, vNOTES decreased the operation duration by ~8.5 min (95% CI: −18.313, −2.699, p = 0.033).
Conclusion: Vaginal natural orifice transluminal endoscopic surgery was equally safe and effective for ovarian cystectomy compared to LESS. vNOTES aligned with the concept of the day-care procedure due to its reduced postoperative pain, shorter exhaust time, and absence of scarring. However, surgeons should conduct a comprehensive preoperative evaluation and exclude patients suspected to have severe pelvic adhesions.
Introduction
An ovarian cyst, a common tumor of the female reproductive system, is caused by an abnormal endocrine system or genetic factors (1, 2). It has an incidence rate of 1.3–24.0%, with more than 90% being benign tumors (3, 4). Physiological ovarian cysts generally have no specific symptoms, except for complications, such as torsion and rupture, and do not require any special treatment (5–7). Ovarian cystectomy is often the recommended treatment for symptomatic physiological or pathological ovarian cysts.
With the development of medical devices and the popularization of minimally invasive concepts, patients prefer surgeries that offer better esthetic outcomes, including those that inflict no or smaller scar (8, 9), such as needleoscopic and percutaneous-assisted surgery (10, 11). Currently, the minimally invasive approaches for ovarian cystectomy are vaginal natural orifice transluminal endoscopic surgery (vNOTES) and transumbilical laparoendoscopic single-site surgery (TU-LESS) (12, 13). Meanwhile, enhanced recovery after surgery (ERAS) has developed rapidly, which optimizes the clinical path of perioperative treatment, reduces the stress response of surgical trauma, shortens hospital stay, and promotes rapid recovery of patients (14–16). Based on the ERAS concept, the day-care procedure further optimizes the disease diagnosis and treatment process, which allows patients to be admitted, operated, and discharged within 24 h (17–19). In the two approaches mentioned above, the incisions are hidden in the belly button with no postoperative scar in the vaginal area; thus, they are suitable for the day-care surgery because of their small trauma and quick recovery.
However, although previous studies have shown that vNOTES has the advantages of causing less pain, faster recovery, and better concealment of surgical incisions, this approach poses a greater risk of damaging adjacent organs (i.e., rectum and bladder) due to its anatomical specificity (20–22). Moreover, the day-care procedure may lead to relatively less preoperative evaluation and postoperative care (17, 19). Hence, it is necessary to explore the safety and effectiveness of vNOTES for ovarian cystectomy in the day-care procedure.
Therefore, we investigate the perioperative data of vNOTES for ovarian cystectomy in the day-care procedure and compare them with single-port laparoscopic surgery. The purpose of this study is to explore the safety and effectiveness of vNOTES for ovarian cystectomy in the day-care surgery. In addition, we provide the complete process of the day-care procedure and key points of vNOTES for ovarian cystectomy.
Materials and methods
Study design and participants
This study is part of a Longitudinal Vaginal Natural Orifice Transluminal Endoscopic Surgery Study (LovNOTESS) conducted in Chengdu (China Clinical Trials Registry ChiCTR2100053483) and approved by the Ethics Committee of Chengdu Women and Children's Central Hospital (No. 202130). This subgroup study only included the retrospective clinical data of patients with ovarian cysts (i.e., pathological or symptomatic physiological ovarian cysts, with a max diameter of the cyst being >5 cm) who sought surgical treatment in our hospital between September 2021 and October 2022. Ovarian cysts suspected before the operation or confirmed by postoperative pathology as malignant were excluded, and vaginal infection was a contraindication for vNOTES. TU-LESS or vNOTES was performed according to the patient's wishes. Each patient who chooses vNOTES should be evaluated in detail before the operation, and the vNOTES approach should be avoided in one of the following cases (23, 24): suspected as malignant tumor before the operation, vaginal infection, highly suspected of severe pelvic adhesions, and the lesion location beyond the scope of the instrument of vNOTES. The exclusion criteria of malignant tumors are systematically based on physical signs, imaging, and serum blood tests, which are mainly according to some international expert consensuses (25, 26). Before the surgery, each patient was informed of the surgical risks (i.e., bladder, ureter, and rectum injuries) and benefits, and then signed written informed consent.
Data collection
Information on all patients was collected from hospital databases, including patient age, body mass index (BMI), the maximum diameter of the cyst, previous pregnancy and abdominal surgery, surgical location, the total time to surgery (i.e., from cutaneous incision to closure), blood loss quantified by subjective visual quantification (27, 28), simultaneously conducting other surgeries, intraoperative complications (i.e., bladder, bowel, and vascular injury), conversion to another surgical procedure, perioperative decrease in serum hemoglobin, postoperative exhaust time, postoperative fever (i.e., any oral temperature≥ occurrence of 38.0°C ≥24 h postoperatively), hospital stay, and postoperative complications. All patients underwent an outpatient review 1 month postoperative to assess postoperative recovery and clinical data.
Standard operating procedures for vNOTES and TU-LESS
Preoperation
All surgeries were performed under general anesthesia, and the patient is placed in the bladder lithotomy position. To prevent infection, 1 g of cefmetazole is administered intravenously 30 min before the procedure. The vaginal and perineal areas are repeatedly disinfected with iodophor, and Foley catheters are inserted for all patients.
Intraoperation
In the TU-LESS group, an incision is made 2 cm at the umbilicus. Then, multiple instrument access ports are inserted through the incision (Beijing Aerospace Cardi Technology Development Institute, HK-TH-60.4TY). In the vNOTES group, an incision was made 1.5 cm at the posterior cervical vault. The operating platform is still built with multiple instrument access ports.
The following steps are the same for both groups. Pneumoperitoneum was generated by CO2 blowing up to 14 mmHg and visualized using a 10 mm 30-degree rigid laparoscope (Karl Storz GmbH & Co. KG, Tuttlingen, Germany). After separating the ovarian cyst from the surrounding tissue, part of the cortex along the long axis of the cyst was cut off using scissors to separate the cortex from the cyst wall. Once the cyst was removed, the remaining ovarian tissue was sutured with an absorbable thread, and an oophoroplasty was performed.
In the following situations, for example intraoperative damage to large vessels or important organs, bleeding volume > 500 ml, change the surgical method; vNOTES was converted to transabdominal single-port laparoscopic surgery, while single-port laparoscopic surgery was converted to multiport surgery. In the event of any life-threatening vascular injury, open surgery was performed.
Peritoneal adhesions were assessed and classified according to the Nair scoring system. Adhesions are divided into four degrees according to the degree of adhesion between the two viscera and viscera and abdominal wall. Abdominal and vaginal wounds are closed with 2–0 absorbent sutures and 2–0 barbed absorbable sutures, respectively. In the TU-LESS and vNOTES groups, drainage tubes were not routinely placed.
Standard day-care procedure
Preadmission
Selection of suitable patients for the day-care surgery in the outpatient clinic. Exclude those who are suspected of severe pelvic adhesions, malignant tumors, or are not suitable for the day-care surgery.
Conduct preoperative testing in the outpatient setting (including blood examination, tumor markers, pretransfusion antibody screen, coagulation function, urination and leucorrhea routine, human chorionic gonadotropin, electrocardiogram, chest radiograph, and gynecological, abdominal, and urological ultrasounds).
Conduct preoperative evaluation, including the patient's general condition and anesthesia evaluation.
Inform patients of the specific admission time and precautions, such as 8-h fasting and water deprivation before admission, and the complete day-care procedure.
Hospitalization
The surgery was performed after completing the preoperative evaluation of the patient. After the surgery, the catheter is pulled out immediately, and regular postoperative nursing is carried out.
Post-discharge
Assess whether the patient meets the discharge criteria (i.e., usually discharged the morning after surgery). If there are any postoperative complications, such as fever, nausea, or vomiting, the patient is discharged on the third day after treatment and observation.
Ensure that patients and their families understand postoperative care and provide written precautions and follow-up arrangements.
Provide postoperative support and perform regular postoperative follow-ups (i.e., on the 7th day and 1 month after surgery).
Statistical analysis
All statistical analyses were performed using SPSS version 25.0 (IBM, Armonk, NY, USA). Continuous variables are expressed as means and standard deviations and analyzed using the Student's t-test, the corrected Student's t-test, one-way ANOVA, or a non-parametric test. Categorical variables are expressed as counts and percentages and analyzed using either the chi-square or Fisher's exact test. Multivariable linear regression analysis was used to assess the influencing factor of intraoperative bleeding, operative time, exhaust time, and postoperative 6-h pain score. Covariates were selected according to the different variables in the univariate analysis and factors reported in previous studies that would affect the dependent variable. All tests were double-tailed; a p-value of <0.05 was considered statistically significant.
Results
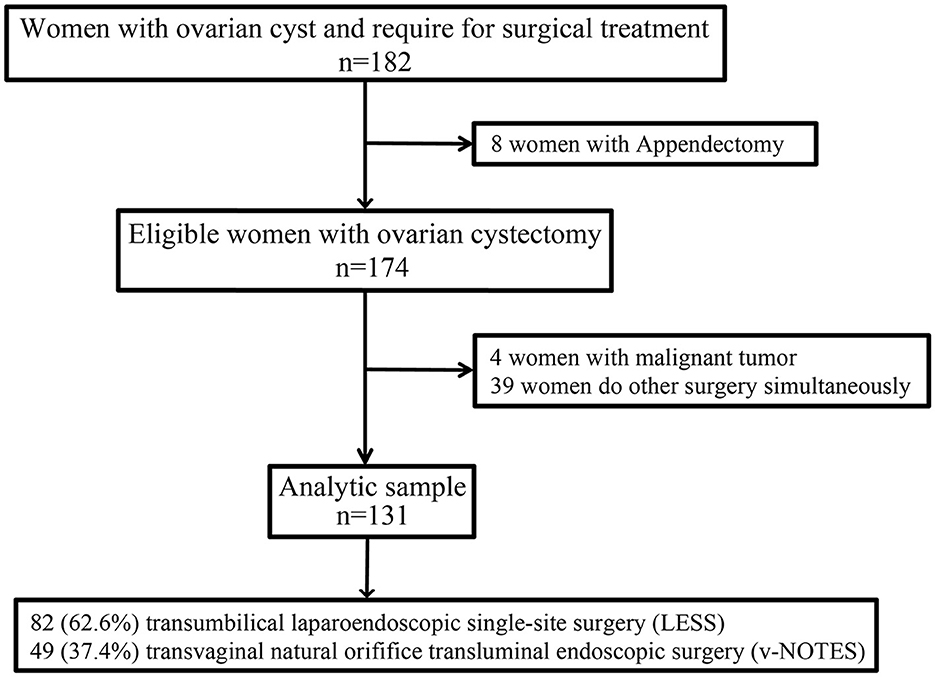
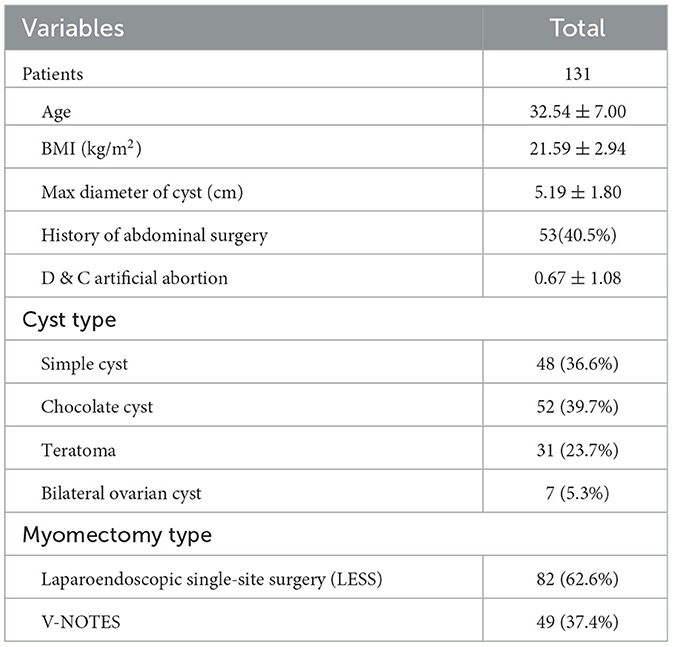
The selection process of the study population is shown in Figure 1. A total of 182 patients with ovarian cysts from our hospital were initially recruited. After excluding patients who had simultaneous surgery and malignant tumor, the final analysis included 131 patients; of which, 82 (62.6%) underwent LESS and 49 (37.4%) underwent vNOTES. Noteworthy, four patients were excluded due to final malign pathology. The characteristics of the patients are presented in Table 1. The average age of patients at recruitment, BMI, and a maximum diameter of cysts was 32.54 ± 7.00 years, 21.59 ± 2.94 kg/m2, and 5.19 ± 1.80 cm, respectively. Among these patients, 53 (40.5%) had undergone abdominal surgery, 7 (5.3%) had undergone bilateral ovarian cysts, and 52 (39.7%) had undergone chocolate cysts.
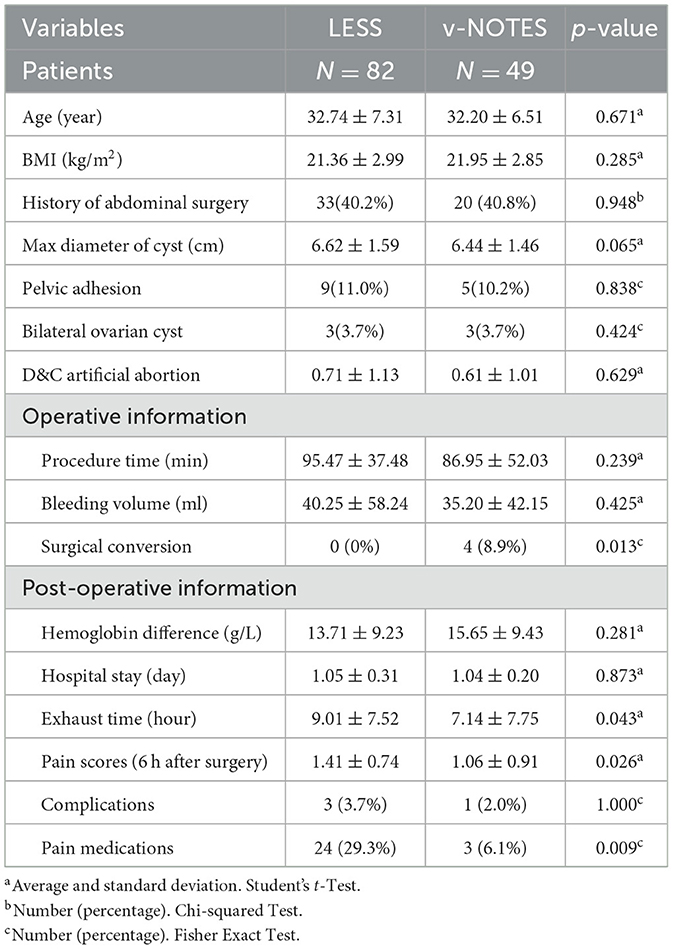
Further analysis of perioperative data showed that there were no significant differences between the two groups for age, BMI, abdominal surgery history, maximum cyst diameter, operation time, intraoperative bleeding, hospital stay, and postoperative complications. In vNOTES, this group had less postoperative exhaust time, a lower postoperative 6-hour pain score, and a lower incidence of analgesic drug use, with a higher surgical conversion incidence. During the postoperative follow-up (1 week and 1 month after surgery), four patients were found to have complications: one patient with febrile, one patient with anemia and transfusion, and one patient with poor wound healing in the LESS group, while one patient with febrile in the vNOTES group. All four complications occurred within 1 week after surgery and were cured in the outpatient department without re-operation (Table 2).
The operation duration reflects the effectiveness of the surgery. The multiple linear regression analysis showed that the operation duration was correlated with the operation approach, surgical conversion, chocolate cyst, bilateral cyst, and pelvic adhesion. The surgical conversion, chocolate cyst, bilateral cyst, and pelvic adhesion increased the operation duration by ~43 (95% confidence interval [CI]: 10.309, 68.152, p < 0.001), 15 (95% CI: 6.342, 45.961, p = 0.036), 10 (95% CI: 3.07, 40.166, p = 0.019), and 8 (95% CI: 4.555, 26.779, p = 0.035) min, respectively. Interestingly, vNOTES decreased the operation duration by ~8.5 min (95% CI: −18.313, −2.699, p = 0.033) (Figure 2).
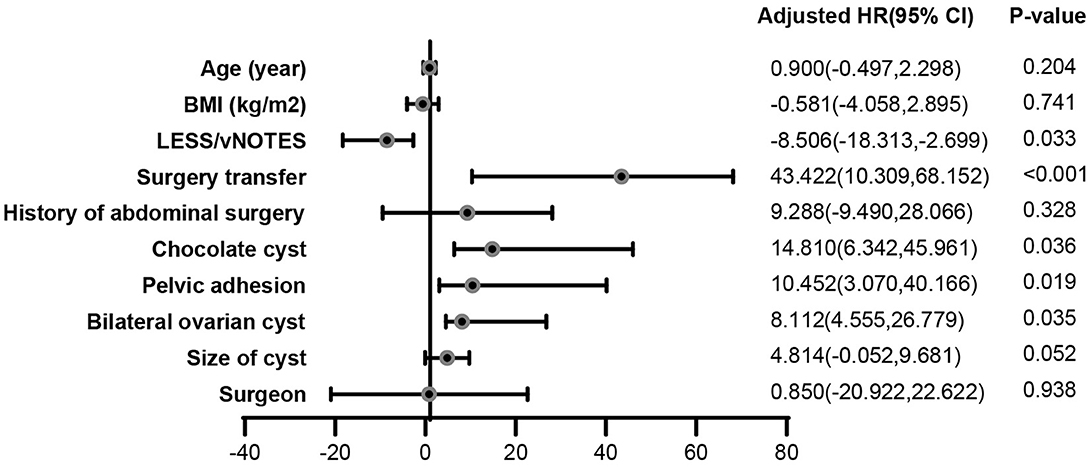
Figure 2. Impact of surgical characteristics on operation duration. The multiple linear regression analysis showed that the operation duration was correlated with the operation approach, surgical conversion, chocolate cyst, bilateral cyst, and pelvic adhesion. The surgical conversion, chocolate cyst, bilateral cyst, and pelvic adhesion increased the operation duration by ~43 (95% confidence interval [CI]: 10.309, 68.152, p < 0.001), 15 (95% CI: 6.342, 45.961, p = 0.036), 10 (95% CI: 3.07, 40.166, p = 0.019), and 8 (95% CI: 4.555, 26.779, p = 0.035) min, respectively. Interestingly, vNOTES decreased the operation duration by ~8.5 min (95% CI: −18.313, −2.699, p = 0.033).
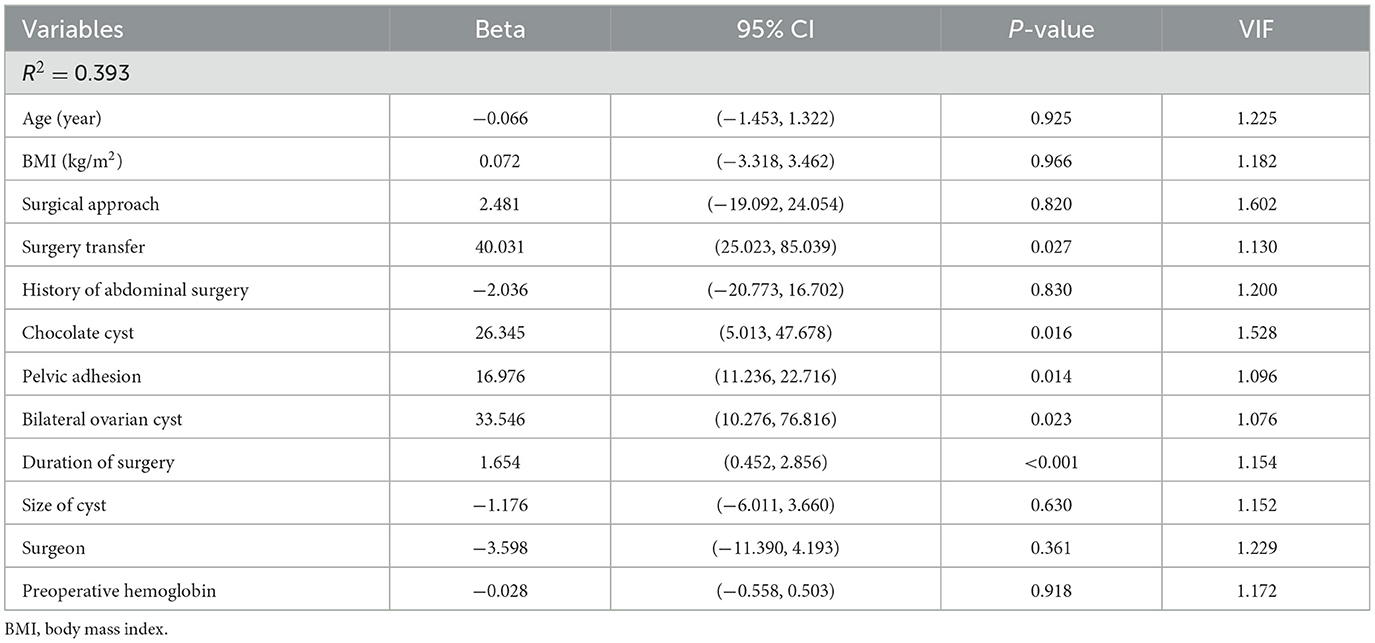
Intraoperative blood loss is an important measure of the safety of surgery. The multiple linear regression analysis showed that the amount of intraoperative bleeding was positively correlated with surgical conversion, chocolate cyst, bilateral cyst, pelvic adhesion, and operation time. The surgical conversion, chocolate cyst, and bilateral cyst increased intraoperative bleeding volume by ~40 (95% CI: 25.023, 85.039, p = 0.027), 26 (95% CI: 5.013, 47.678, p = 0.016), and 33 (95% CI: 10.276,76.816, p = 0.023) ml, respectively. Meanwhile, the bleeding volume increased by ~1.7 ml when the duration of surgery increased by 1 min (95% CI: 0.452, 2.856, p < 0.001) and 17 ml when pelvic adhesion increased by 1 grade (95% CI: 11.236, 22.716, p = 0.014) (Table 3).
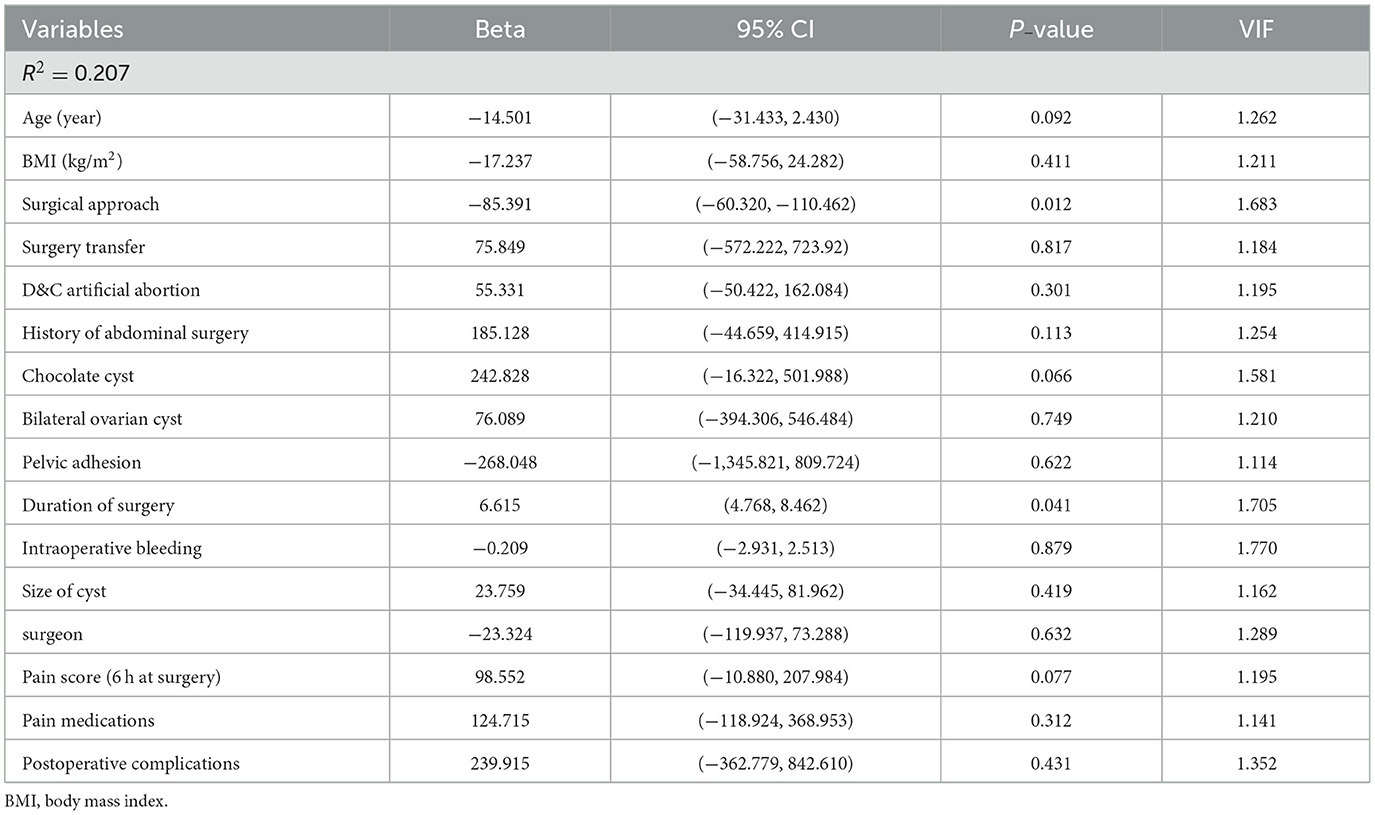
In the vNOTES group, the postoperative exhaust time was significantly shorter than that of the LESS group. The multiple linear regression analysis revealed that the postoperative exhaust time was correlated with surgical approach and duration. vNOTES reduced the postoperative exhaust time by ~85 min (95% CI: −60.320, −110.462, p = 0.012), while the exhaust time increased by ~7 min when the duration of surgery increased by 1 min (95% CI: 4.768, 8.462, p = 0.041) (Table 4).
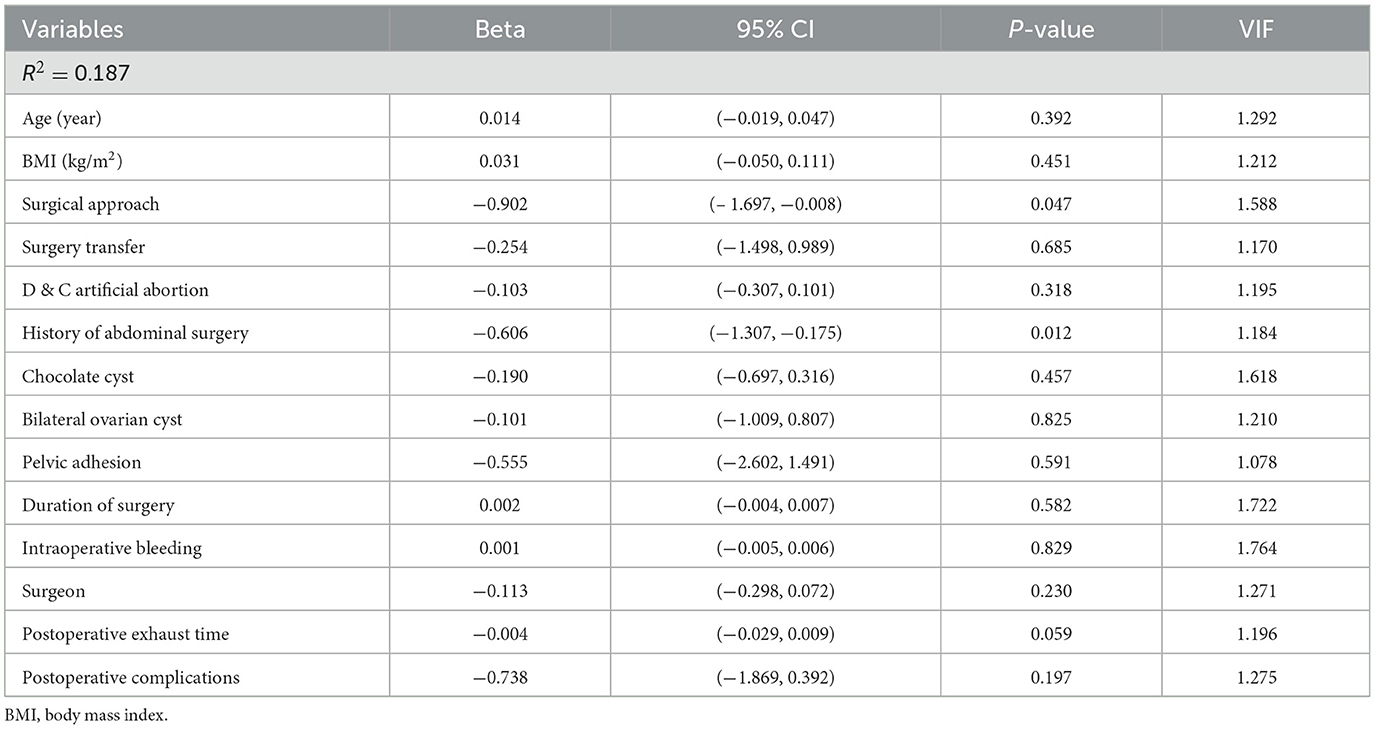
Further multivariate linear regression revealed that the 6-h postoperative pain score was correlated with the operation approach and abdominal surgery history. vNOTES reduced the 6-h postoperative pain score by ~0.9 (95% CI: −1.697, −0.008, p = 0.047) and previous abdominal surgery history reduced the score by ~0.6 (95% CI: −1.037, −0.175, p = 0.012) (Table 5).
Discussion
Vaginal natural orifice transluminal endoscopic surgery has advantages, such as reduced postoperative pain, shorter exhaust time and hospital stay, and absence of postoperative scar, which aligns with the concept of the day-care surgery (12, 29). In this retrospective preliminary study, we compared the perioperative data of vNOTES for ovarian cystectomy in the day-care procedure with those of single-port laparoscopic surgery. We also outlined the advantages and disadvantages of LESS and vNOTES for ovarian cystectomy in the day-care procedure, which could lay a theoretical basis for future vNOTES surgery in a wider area.
In our cohort, there was no significant difference between the vNOTES and LESS groups in terms of intraoperative bleeding volume, operation time, and incidence of postoperative complications, which suggested that ovarian cystectomy via vNOTES in the day-care procedure has the same safety threshold as LESS. However, the conversion rate of surgery, which indicates the effectiveness of surgery, was significantly different between the two groups. In the vNOTES group, the surgical conversion rate was higher than that previously reported, which was attributed to the presence of pelvic adhesions. It was difficult to penetrate the pelvic cavity during the surgery. If vNOTES was continued, there is a risk of damage to adjacent organs; thus, it was switched to LESS. During LESS, the posterior wall of the uterus was tightly adhered to the pelvis, sealing the pelvis. Notably, the four patients had chocolate cysts. Due to the timely transit during surgery, no damage to the adjacent organs occurred, and there was no significant difference in the complication rate between the two groups. Therefore, surgeons should conduct a more comprehensive preoperative evaluation on patients who choose to undergo vNOTES, such as those with multiple abdominal surgeries and chocolate cysts (23, 30). Our study also included careful inquiry of dysmenorrhea history and gynecological physical examination to assess uterine activity and tenderness of the surface nodules of the sacral ligaments (24, 31). Moreover, multi-parameter scores for ovarian tumors (such as ESGO/ISUOG/IOTA/ESGE) (32) may be used to evaluate endometriosis to find severe adhesion before surgery. In addition, vaginal ultrasound can also be used to evaluate the sliding of the uterus on the anterior wall of the rectum in real-time. If severe pelvic adhesion is suspected after evaluations, vNOTES should be avoided (13, 33–35).
The difficulty of vNOTES lies in the establishment process (i.e., the approach and lesion exposure processes). The previous study showed that the operation duration is longer in vNOTES than that in LESS (36–38). However, in this cohort, the vNOTES group had a shorter operating duration, which may be due to the advantage of the visual field. Ovarian cysts, especially teratomas, can be directly assessed via the incision of vNOTES; therefore, we consider that vNOTES has an advantage over LESS for ovarian cystectomy. Consistent with the study of Giovanni Buzzaccarini et al., the new target of clinical trials should be to assess the appropriateness of vNOTES in selected populations, with the aim of maximizing the potential benefits of this technique compared to other approaches (39). For obese women and/or for women with large uteri, vNOTES may be particularly effective and safe (40). Moreover, for giant teratoma, specimen retrieval still represents an issue. Vaginal muscles have better ductility, making it easier to take out some large specimens, which may be another advantage of vNOTES (41, 42).
Consistent with previous studies, we also found that the vNOTES group had shorter postoperative exhaust times than that of the LESS group (43, 44), which may be due to the following reasons. First, vNOTES surgery is performed in the pelvis and has little effect on the upper abdomen. Second, before surgery, the small intestine is pushed to the true pelvic level. Therefore, the surgical instruments do not repeatedly contact the intestine, reducing irritation to the intestine. In addition, blood collects between the endoscopic body and the target area due to the upward viewing angle of surgery. Furthermore, the blood is constantly washed during the procedure to ensure clear vision. The postoperative residual blood volume in the abdominal cavity is significantly reduced, chemical irritation and inflammatory factors are reduced, and bowel function recovers faster (45–47).
Moreover, the vNOTES group experienced milder postoperative pain than that of the LESS group (33, 48, 49), which may be due to the vaginal fornix being innervated by visceral nerves and is not sensitive to pain. vNOTES also avoids damaging the abdominal wall, which occurs in LESS due to trocar puncture. Furthermore, the operation time of vNOTES was relatively shorter than that of LESS for ovarian cystectomy, which reduced the stimulation of the diaphragm by abdominal gas. Milder postoperative pain allows patients to get out of bed earlier, which promotes the recovery of gastrointestinal function after surgery, resulting in earlier postoperative exhaust.
Based on the ERAS concept, the day-care procedure requires surgeons to choose a surgical approach that is less damaging to the patient to ensure less postoperative pain, shorter exhaust time, faster recovery, and safer discharge within 24 h. Moreover, scarless surgery is the current trend of gynecological surgery; the vNOTES approach conceals the incision, avoids abdominal damage, and reduces the occurrence of incision hernia, which invokes psychologically minimal invasive effects and allows for the rapid recovery of patients.
The strength of this study is that it specifically studies the population and standard operating procedures for vNOTES. Participants were screened using rigorous inclusion and exclusion criteria. Patients who had other surgeries simultaneously or malignant ovarian cysts were excluded. This study compared the comprehensive perioperative data of the two latest surgical methods, LESS and vNOTES, for ovarian cystectomy, and preliminarily confirmed the effectiveness and safety of vNOTES. In addition, all patients underwent an outpatient review 1-month postoperatively to assess postoperative recovery and obtain complete clinical data, resulting in a relatively comprehensive study design. Moreover, our hospital has implemented vNOTES since 2018, and there are nearly 2,000 vNOTES cases per year in the last 2 years; thus, all operations were performed according to a standardized surgical procedure.
The pilot study enhances our understanding of LESS and vNOTES for ovarian cystectomy. However, our study had several limitations. First, the sample size of this study was relatively small compared to similar studies of multiport and LESS. Second, this study is retrospective, and vNOTES has been widely used in gynecology for only 5 years. Prospective follow-up of patients after ovarian cystectomy can provide further insight into short- and long-term complications and the potential impact of vNOTES on sexual function, pregnancy, and vaginal delivery. Therefore, a large-scale multicenter study involving more patients and different types of gynecological diseases is needed to further promote the widespread use of vNOTES.
Conclusion
Vaginal natural orifice transluminal endoscopic surgery was equally safe and effective for ovarian cystectomy compared to that of LESS. vNOTES aligned with the concept of the day-care procedure due to its reduced postoperative pain, shorter exhaust time, and absence of scarring. However, surgeons should conduct a comprehensive preoperative evaluation and exclude patients who are suspected to have severe pelvic adhesions.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
YLin, YJ, and XG conducted the study and provided funding resources. XL and AX analyzed the data and drafted the manuscript. HW, YLiu, LW, JL, JY, ZY, JZ, LH, TL, and YLi critically revised the manuscript. All authors have accepted responsibility for the entire content of this submitted manuscript and approved submission.
Funding
Financial support for this study was provided by Chengdu Science and Technology Bureau (Nos: 2021-YF0500530-SN and 2021-YF0500868-SN) and Chengdu Municipal Health Commission (No: 2021074). The funding agencies did not have any role in the design of the study, collection, analysis, and interpretation of data, and in writing the manuscript.
Acknowledgments
The authors would like to thank all the participants and researchers who contributed to this cohort study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Xu X, Chen Y, Yu Q, Wang J, Xu P, Zhu L, et al. The presence of living endometrial cells in ovarian endometriotic cyst fluid may contribute to the recurrence of endometriosis after surgical excision of endometriomas. J Ovarian Res. (2022) 15:89. doi: 10.1186/s13048-022-01018-9
2. Choi P W, So W W, Yang J, Liu S, Tong K K, Kwan K M, et al. MicroRNA-200 family governs ovarian inclusion cyst formation and mode of ovarian cancer spread. Oncogene. (2020) 39:4045–60. doi: 10.1038/s41388-020-1264-x
3. Meng B, Xu M. Pelvic artificial isolation with ultrasound-guided fluid: a new technique in ovarian endometriotic cyst transabdominal sclerotherapy. Med Sci Monit. (2022) 28:e937855. doi: 10.12659/MSM.937855
4. Mantecon O, George A, DeGeorge C, McCauley E, Mangal R, Stead T S, et al. A case of hemorrhagic ovarian cyst rupture necessitating surgical intervention. Cureus. (2022) 14:e29350. doi: 10.7759/cureus.29350
5. Idris S, Daud S, Ahmad Sani N, Tee Mei Li S. A case of twisted ovarian cyst in a young patient and review of the literature. Am J Case Rep. (2021) 22:e933438. doi: 10.12659/AJCR.933438
6. Wang L, Jiang YJ. Rupture of ovarian endometriotic cyst complicated with endometriosis: a case report. World J Clin Cases. (2021) 9:8524–30. doi: 10.12998/wjcc.v9.i28.8524
7. Elgazar A, Awad A K. Triple presentation of acute appendicitis, Meckel's diverticulum, and hemorrhagic ovarian cyst: a rare case report and literature review. Int J Surg Case Rep. (2021) 87:106462. doi: 10.1016/j.ijscr.2021.106462
8. Kao CC, Duscher D. Advanced endoscopic techniques in Asian facial rejuvenation. Clin Plast Surg. (2023) 50:51–60. doi: 10.1016/j.cps.2022.07.008
9. Leal SC, Dame-Teixeira N, Barbosa CB, Kominami PAA, Raposo F, Nakagawa EMT, et al. Minimum intervention oral care: defining the future of caries management. Braz Oral Res. (2022) 36:e135. doi: 10.1590/1807-3107bor-2022.vol36.0135
10. Gueli Alletti S, Rossitto C, Perrone E, Cianci S, De Blasis I, Fagotti A, et al. Needleoscopic conservative staging of borderline ovarian tumor. J Minim Invasive Gynecol. (2017) 24:529–30. doi: 10.1016/j.jmig.2016.10.009
11. Perrone E, Rossitto C, Fanfani F, Cianci S, Fagotti A, Uccella S, et al. Percutaneous-assisted vs. laparoscopic hysterectomy: a prospective comparison. Gynecol Obstet Invest. (2020) 85:318–26. doi: 10.1159/000509877
12. Baekelandt J, Noori N, Hofmann L, Mansoor A, Kapurubandara S. Standardised step by step approach to adnexectomy by vaginal natural orifice transluminal endoscopic surgery. Eur J Obstet Gynecol Reprod Biol. (2022) 274:160–5. doi: 10.1016/j.ejogrb.2022.05.021
13. Huang L, Lin Y H, Yang Y, Gong Z L, He L. Comparative analysis of vaginal natural orifice transluminal endoscopic surgery vs. transumbilical laparoendoscopic single-site surgery in ovarian cystectomy. J Obstet Gynaecol Res. (2021) 47:757–64. doi: 10.1111/jog.14603
14. Huang T, Wang J, Chen Y, Ye Z, Fang Y, Xia Y. Knowledge, attitude and application towards fast track surgery among operating room paramedics: a cross-sectional study. BMC Health Serv Res. (2022) 22:1401. doi: 10.1186/s12913-022-08817-2
15. Thompson A R, Glick H, Rubalcava N S, Vernamonti J P, Speck K E. Implementation science fundamentals: pediatric surgery enhanced recovery after surgery protocol for pectus repair. J Surg Res. (2022) 283:313–23. doi: 10.1016/j.jss.2022.10.018
16. Levy B E, Castle J T, Ebbitt L M, Kennon C, McAtee E, Davenport D L, et al. Opioid use after colorectal resection: identifying preoperative risk factors for postoperative use. J Surg Res. (2022) 283:296–304. doi: 10.1016/j.jss.2022.10.051
17. Parab SR, Khan MM. Is day care tonsillectomy a safe procedure? Indian J Otolaryngol Head Neck Surg. (2019) 71:918–22. doi: 10.1007/s12070-019-01587-0
18. Baekelandt JF, De Mulder PA, Le Roy I, Mathieu C, Laenen A, Enzlin P, et al. Hysterectomy by transvaginal natural orifice transluminal endoscopic surgery vs. laparoscopy as a day-care procedure: a randomised controlled trial. BJOG. (2019) 126:105–13. doi: 10.1111/1471-0528.15504
19. Badami KN. Commentary: evolution of vitrectomy as day care procedure. Indian J Ophthalmol. (2018) 66:1143. doi: 10.4103/ijo.IJO_1098_18
20. Baekelandt J, Kapurubandara S. A novel approach using vaginal natural orifice transluminal endoscopic surgery (vNOTES) to repair a symptomatic uterine isthmocele. Fertil Steril. (2022) 119:328–30. doi: 10.1016/j.fertnstert.2022.11.016
21. Reddy H, Kim SW, Plewniak K. Applications of vaginal natural orifice transluminal endoscopic surgery (vNOTES) in gynecologic surgery. Curr Opin Obstet Gynecol. (2022) 34:220–6. doi: 10.1097/GCO.0000000000000799
22. Hui M, Schwartzenburg C, Bhalwal A. Utility of vaginal natural orifice transluminal endoscopic surgery for permanent sterilization after failed attempt at bilateral tubal ligation at the time of previous cesarean section. J Minim Invasive Gynecol. (2022) 29:1138–9. doi: 10.1016/j.jmig.2022.07.007
23. Housmans S, Stuart A, Bosteels J, Deprest J, Baekelandt J. Standardized 10-step approach for successfully performing a hysterectomy via vaginal natural orifice transluminal endoscopic surgery. Acta Obstet Gynecol Scand. (2022) 101:649–56. doi: 10.1111/aogs.14367
24. Kale A, Mat E, Basol G, Gundogdu EC, Aboalhasan Y, Yildiz G, et al. A new and alternative route: transvaginal natural orifice transluminal endoscopic scarless surgery (vaginal natural orifice transluminal endoscopic surgery) for class 2 and class 3 obese patients suffering from benign and malignant gynecologic pathologies. Surg Innov. (2022) 29:730–41. doi: 10.1177/15533506221074628
25. Andreotti R F, Timmerman D, Strachowski L M, Froyman W, Benacerraf B R, Bennett G L, et al. O-RADS US risk stratification and management system: a consensus guideline from the ACR ovarian-adnexal reporting and data system committee. Radiology. (2020) 294:168–85. doi: 10.1148/radiol.2019191150
26. Expert Panel on Women's I, Atri M, Alabousi A, Reinhold C, Akin E A, Benson C B, et al. ACR appropriateness criteria ((R)) clinically suspected adnexal mass, no acute symptoms. J Am Coll Radiol. (2019) 16:S77–S93. doi: 10.1016/j.jacr.2019.02.011
27. Rairdin A, Fotouhi F, Zhang J, Mueller D S, Ganapathysubramanian B, Singh A K, et al. Deep learning-based phenotyping for genome wide association studies of sudden death syndrome in soybean. Front Plant Sci. (2022) 13:966244. doi: 10.3389/fpls.2022.966244
28. Ha-Wissel L, Yasak H, Huber R, Zillikens D, Ludwig R J, Thaci D, et al. Case report: optical coherence tomography for monitoring biologic therapy in psoriasis and atopic dermatitis. Front Med. (2022) 9:995883. doi: 10.3389/fmed.2022.995883
29. Noh J J, Kim M S, Kang J H, Jung J H, Chang C S, Jeon J, et al. Comparison of surgical outcomes of hysterectomy by vaginal natural orifice transluminal endoscopic surgery (vNOTES) vs. single-port access (SPA) surgery. J Pers Med. (2022) 12:875. doi: 10.3390/jpm12060875
30. Zhang S, Dong Z, Liu J, Qin Z, Wang H, Bao M, et al. Safety and feasibility of vaginal delivery in full-term pregnancy after transvaginal-natural orifice transluminal endoscopic surgery: a case series. Front Surg. (2022) 9:888281. doi: 10.3389/fsurg.2022.888281
31. Tavano I, Housmans S, Bosteels J, Baekelandt J. Pregnancy outcome after vaginal natural orifice transluminal endoscopic surgery, a first retrospective observational cohort study. Gynecol Obstet Invest. (2021) 86:432–7. doi: 10.1159/000517834
32. Timmerman D, Planchamp F, Bourne T, Landolfo C, du Bois A, Chiva L, et al. ESGO/ISUOG/IOTA/ESGE consensus statement on pre-operative diagnosis of ovarian tumors. Int J Gynecol Cancer. (2021) 31:961–82. doi: 10.1136/ijgc-2021-002565
33. Behnia-Willison F, Nguyen T, Rezaeimotlagh A, Baekelandt J, Hewett P J. Middle Eastern women's attitudes and expectations towards vaginal natural orifice transluminal endoscopic surgery (vNOTES): a survey-based observational study. Surg Endosc. (2021) 35:6865–72. doi: 10.1007/s00464-020-08193-0
34. Yang H, Yang M, Ransford A, Zi D. Vaginal hysterectomy combined with transvaginal natural orifice transluminal endoscopic surgery bilateral adnexectomy: a case report. J Int Med Res. (2020) 48:300060520981263. doi: 10.1177/0300060520981263
35. Puisungnoen N, Yantapant A, Yanaranop M. Natural orifice transluminal endoscopic surgery-assisted vaginal hysterectomy vs. total laparoscopic hysterectomy: a single-center retrospective study using propensity score analysis. Gynecol Minim Invasive Ther. (2020) 9:227–30. doi: 10.4103/GMIT.GMIT_130_19
36. Park S J, Kim H S, Yim G W. Comparison of vaginal natural orifice transluminal endoscopic surgery (vNOTES) and laparoendoscopic single-site (LESS) hysterectomy on postoperative pain reduction: a randomized pilot study. Pain Ther. (2021) 10:1401–11. doi: 10.1007/s40122-021-00300-w
37. Baekelandt J, De Mulder P A, Le Roy I, Mathieu C, Laenen A, Enzlin P, et al. Adnexectomy by vaginal natural orifice transluminal endoscopic surgery vs. laparoscopy: results of a first randomised controlled trial (NOTABLE trial). BJOG. (2021) 128:1782–91. doi: 10.1111/1471-0528.16838
38. Kapurubandara S, Lowenstein L, Salvay H, Herijgers A, King J, Baekelandt J. Consensus on safe implementation of vaginal natural orifice transluminal endoscopic surgery (vNOTES). Eur J Obstet Gynecol Reprod Biol. (2021) 263:216–22. doi: 10.1016/j.ejogrb.2021.06.019
39. Buzzaccarini G, Stabile G, Torok P, Petousis S, Mikus M, Della Corte L, et al. Surgical approach for enlarged uteri: further tailoring of vNOTES hysterectomy. J Invest Surg. (2022) 35:924–5. doi: 10.1080/08941939.2021.1967528
40. Buzzaccarini G, Noventa M, D'Alterio MN, Terzic M, Scioscia M, Schafer SD, et al. vNOTES hysterectomy: can it be considered the optimal approach for obese patients? J Invest Surg. (2022) 35:868–9. doi: 10.1080/08941939.2021.1939467
41. Lagana A S, Casarin J, Uccella S, Garzon S, Cromi A, Guerrisi R, et al. Outcomes of in-bag transvaginal extraction in a series of 692 laparoscopic myomectomies: results from a large retrospective analysis. J Minim Invasive Gynecol. (2022) 29:1331–8. doi: 10.1016/j.jmig.2022.09.009
42. Lagana A S, Vitagliano A, Casarin J, Garzon S, Uccella S, Franchi M, et al. Transvaginal vs. port-site specimen retrieval after laparoscopic myomectomy: a systematic review and meta-analysis. Gynecol Obstet Invest. (2022) 87:177–83. doi: 10.1159/000525624
43. Liu Y, Huyang S, Tan H, He Y, Zhou J, Li X, et al. Using mindfulness to reduce anxiety and depression of patients with fever undergoing screening in an isolation ward during the COVID-19 outbreak. Front Psychol. (2021) 12:664964. doi: 10.3389/fpsyg.2021.664964
44. Nulens K, Kempenaers R, Baekelandt J. Hysterectomy via vaginal Natural Orifice Transluminal Endoscopic Surgery in virgin patients: a first feasibility study. J Obstet Gynaecol. (2022) 42:116–21. doi: 10.1080/01443615.2020.1867972
45. Evangelisti G, Barra F, Centurioni M G, D'Alessandro G, Alessandri F, Ferrero S. Vaginal natural orifice transluminal endoscopic surgery (NOTES) for treating benign adnexal diseases: past results and future developments. J Invest Surg. (2022) 35:409–10. doi: 10.1080/08941939.2020.1843205
46. Baekelandt J, Kapurubandara S. Benign gynaecological procedures by vaginal natural orifice transluminal endoscopic surgery (vNOTES): complication data from a series of 1000 patients. Eur J Obstet Gynecol Reprod Biol. (2021) 256:221–4. doi: 10.1016/j.ejogrb.2020.10.059
47. Alay I, Kaya C, Cengiz H, Yildiz S, Aslan O, Yasar L, et al. Apical pelvic organ prolapse repair via vaginal-assisted natural orifice transluminal endoscopic surgery: Initial experience from a tertiary care hospital. Asian J Endosc Surg. (2021) 14:346–52. doi: 10.1111/ases.12863
48. Dubuisson J, Claver M, Constantin F. Transvaginal natural orifice transluminal endoscopic surgery (vNOTES) for high uterosacral ligament suspension of the vaginal cuff (with video). Gynecol Obstet Fertil Senol. (2021) 49:941–2. doi: 10.1016/j.gofs.2021.02.009
Keywords: transvaginal natural orifice endoscopic surgery, ovarian cystectomy, ovarian cyst, transumbilical laparoendoscopic single-site surgery, day-care procedure
Citation: Xie A, Li X, Huang J, Wang H, Liu Y, Wang L, Liao J, Yu J, Yan Z, Zhang J, Huang L, Liu T, Li Y, Lin Y, Jia Y and Gan X (2023) Transvaginal natural orifice endoscopic surgery for ovarian cystectomy: a more suitable surgical approach for the day-care procedure. Front. Med. 10:1164970. doi: 10.3389/fmed.2023.1164970
Received: 13 February 2023; Accepted: 07 April 2023;
Published: 18 May 2023.
Edited by:
Laurentiu Cornel Pirtea, Victor Babes University of Medicine and Pharmacy, RomaniaReviewed by:
Mehmet Murat Seval, Ankara University, TürkiyeCristian Furau, Vasile Goldiş Western University of Arad, Romania
Claudia Mehedintu, Carol Davila University of Medicine and Pharmacy, Romania
Copyright © 2023 Xie, Li, Huang, Wang, Liu, Wang, Liao, Yu, Yan, Zhang, Huang, Liu, Li, Lin, Jia and Gan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yujian Jia, MjM2NjQwMzY2QHFxLmNvbQ==; Yonghong Lin, bGlueWhjZDIwMTFAMTYzLmNvbQ==; Xiaoqin Gan, YW1hbmRpbmUyMDIxQDE2My5jb20=
†These authors have contributed equally to this work
 Aijie Xie1,2†
Aijie Xie1,2† Xin Li
Xin Li Juan Huang
Juan Huang Yonghong Lin
Yonghong Lin