- 1Shenzhen Hospital of Guangzhou University of Chinese Medicine (Futian), Shenzhen, China
- 2Guangzhou University of Chinese Medicine, Guangzhou, China
- 3Shenzhen Polytechnic University, Shenzhen, China
- 4Department of Rehabilitation Medicine, Shenzhen Hospital, Southern Medical University, Shenzhen, China
Background: From the end of 2019 to December 2023, the world grappled with the COVID-19 pandemic. The scope and ultimate repercussions of the pandemic on global health and well-being remained uncertain, ushering in a wave of fear, anxiety, and worry. This resulted in many individuals succumbing to fear and despair. Acupoint massage emerged as a safe and effective alternative therapy for anxiety relief. However, its efficacy was yet to be extensively backed by evidence-based medicine. This study aimed to enhance the clinical effectiveness of acupoint massage and extend its benefits to a wider population. It undertakes a systematic review of the existing randomized controlled trials (RCTs) assessing the impact of acupoint massage on anxiety treatment, discussing its potential benefits and implications. This research aims to furnish robust evidence supporting anxiety treatment strategies for patients afflicted with COVID-19 disease and spark new approaches to anxiety management.
Objectives: This study evaluates the evidence derived from randomised controlled trials (RCTs), quantifies the impact of acupressure on anxiety manifestations within the general population, and proposes viable supplementary intervention strategies for managing COVID-19 related anxiety.
Materials and methods: This review included RCTs published between February 2014 and July 2023, that compared the effects of acupressure with sham control in alleviating anxiety symptomatology as the outcome measure. The studies were sourced from the multiple databases, including CINAHL, EBM Reviews, Embase, Medline, PsycINFO, Scopus and Web of Science. A meta-analysis was performed on the eligible studies, and an overall effect size was computed specifically for the anxiety outcome. The Cochrane Collaboration Bias Risk Assessment Tool (RevMan V5.4) was employed to assess bias risk, data integration, meta-analysis, and subgroup analysis. The mean difference, standard mean deviation, and binary data were used to represent continuous outcomes.
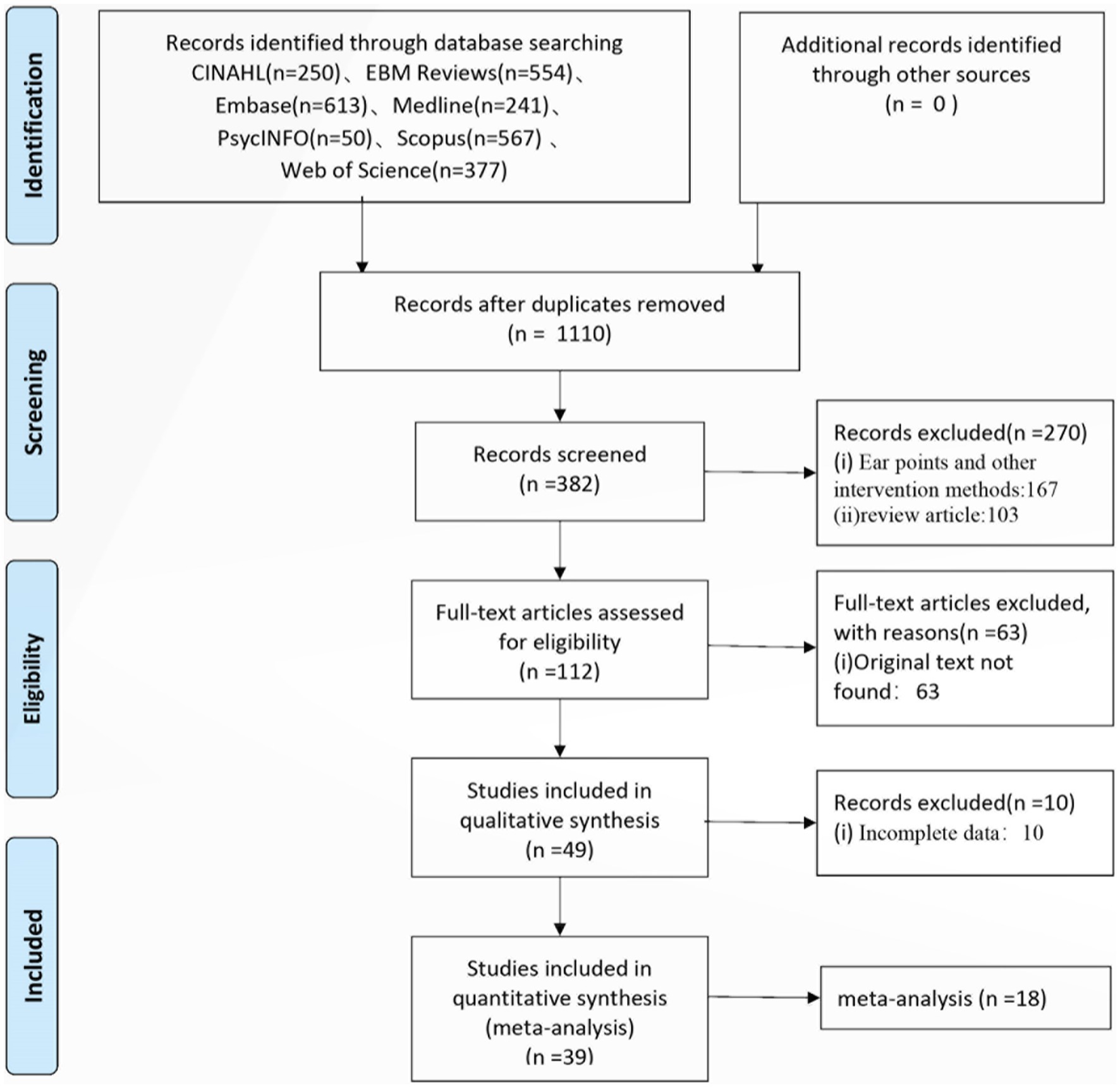
Results: Of 1,110 studies of potential relevance, 39 met the criteria for inclusion in the meta-analysis. The majority of the studies reported a positive effect of acupressure in assuaging anticipatory anxiety about treatment. Eighteen studies were evaluated using the STAI scale. The acupressure procedures were thoroughly documented, and studies exhibited a low risk of bias. The cumulative results of the 18 trials showcased a more substantial reduction in anxiety in the acupressure group compared to controls (SMD = −5.39, 95% CI −5.61 to −5.17, p < 0.01). A subsequent subgroup analysis, based on different interventions in the control group, demonstrated improvement in anxiety levels with sham acupressure in improving changes in anxiety levels (SMD −1.61, 95% CI: −2.34 to −0.87, p < 0.0001), and blank controls (SMD −0.92, 95% CI: −2.37 to 0.53, p = 0.22).
Conclusion: In the clinical research of traditional Chinese medicine treatment of anxiety, acupressure demonstrated effectiveness in providing instant relief from anxiety related to multiple diseases with a medium effect size. Considering the increasing incidence of anxiety caused by long COVID, the widespread application of acupressure appears feasible. However, the results were inconsistent regarding improvements on physiological indicators, calling for more stringent reporting procedures, including allocation concealment, to solidify the findings.
Introduction
The widespread impact of the COVID-19 pandemic has brought a myriad of challenges which can be stressful and overwhelming, causing psychological distress requiring urgent interventions. As per a World Health Organization survey, over 93% of countries worldwide reported increased demand mental health services (1). A survey revealed that over 40% respondents reported experiencing at least one adverse mental health condition, including anxiety during the COVID-19 pandemic—United States (2). Anxiety, a common affliction during this pandemic, affects everyone from frontline worker to individuals in nursing centers. While medications including benzodiazepines can address anxiety, they often present undesirable side effects. Therefore, the exploration of alternative, effective treatments to alleviate anxiety is of crucial clinical importance. Acupoint massage, a non-drug treatment based on traditional Chinese medicine, offers a promising solution. The technique of pressing acupoints with fingers or non-invasive tools is simple to operate and is not limited by external factors such as equipment and location. It is especially promising. Many scholars have reported that acupoint massage is safe and effective in relieving various mental and physical diseases. In our belief that the acupoint massage could be used widely in clinical treatment, this will eventually benefit people worldwide. Its simplicity and independence from extensive equipment make it convenient and universally applicable. Numerous studies have reported the safety and effectiveness of acupoint massage in mitigating various mental and physical conditions. This study aims to conduct a systematic review of acupuncture massage’s efficacy in treating anxiety, analyzing its value and advantages, especially during the current global long COVID, and provided solid evidence to formulate effective anxiety-related treatments.
Materials and methods
Study search
Electronic medical databases, including CINAHL, EBM Reviews, Embase, Medline, PsycINFO, Scopus and Web of Science were explored to gather clinical studies investigating acupuncture’s impact on anxiety management, with changes in anxiety symptoms as the primary outcomes. The keywords used in each database were (anxi* or nervous* or worry or worried or uneas* or apprehensi* or fret* or angst* or fear* or disquiet* or distress* or stress* or strain*) AND (acupressure or chih-ya or shiatsu or shiatzu or zhi-ya or finger-massage or finger-pressure or Tui-Na). All capturing studies published between February 2014 and July 2023.
Study selection
Inclusion criteria were formulated using the PICO (Population, Intervention, Context and Outcome) tool (3). The inclusion criteria in this review were as follows:
1. Study design: clinical studies such as case report, case series, case-control study, nonrandomized controlled trial, and randomized controlled trial (RCT).
2. Used acupressure as the sole intervention compared with the control condition of either sham control or standard control (e.g., education).
3. Population and area: no limitation.
4. Grouping: intervention: acupressure; comparison: no limitation.
5. Outcome: both qualitative and quantitative outcomes, including the Hamilton Anxiety Rating Scale and the State-Trait Anxiety Inventory (STAI) were used to assess anxiety severity.
Studies like animal mechanism endeavors, case reports, self-controlled, non-RCTs, random crossover studies, and quasi-randomized trials were excluded.
Data extraction
Two researchers independently extracted data from the included studies using pre-arranged standardized forms. Extracted data included author information, study designs, sample size, average age of participants, interventions, treatment periods, acupressure points used, experimental and control intervention regimens, outcome measures results, and adverse events. The primary outcome for this review was defined as the change in anxiety level before and immediately after the intervention, evaluated by various scales such as the Visual Analogue Scale for Anxiety (VAS-A), State-Trait Anxiety Inventory (STAI), and many others. Secondary outcomes encompassed measurements such as blood pressure, heart rate, blood oxygen, The Modified Yale Preoperative Anxiety Scale (MYPAS), GAD-7, Quality of Life, and others. Two researchers independently reviewed the searched articles and selected relevant studies, with disagreement resolved through discussions among the research team.
Data synthesis and statistical analysis
Meta-analysis was conducted only on studies that demonstrated similar clinical characteristics and had no domain rated as high risk according to the Cochrane risk of bias assessment. Heterogeneity among studies was evaluated by calculating the I2 statistic and χ2 test (assessing the p-value) using Review Manager 5 (V.5.4, The Nordic Cochrane Centre, Copenhagen). Significant heterogeneity was considered when the p-value was <0.10 and I2 > 50%, whereupon a random-effects model was employed for data synthesis. The standardised mean differences (SMDs) with 95% CIs were used for continuous outcomes. The overall effect size was calculated based on the pooled SMD, with Cohen’s categories—0.20, 0.50 and 0.80—interpreted as small, medium and large effects, respectively (4).
Quality assessment
The methodological quality of identified studies was also assessed according to the quality domains in the Cochrane risk of bias tool. It was used to evaluate the following:
1. Random sequence generation.
2. Allocation concealment.
3. Blinding of participants and personnel.
4. Blinding of outcome assessment incomplete outcome data.
5. Selective reporting.
6. Any other sources of bias.
Each domain was rated as “high” (seriously weakens confidence in the results), “unclear” or “low” (unlikely to seriously alter the result). Given the difficulties in blinding the personnel administering acupressure, we only assessed only the blinding of participants and outcome assessments. To follow the guidelines recommended by the Cochrane Back Review Group, a compliance threshold of <50% of the criteria was associated with bias (5). Studies meeting at least four domains without serious flaws were deemed to have a low risk of bias. Disagreements were resolved by discussion or by a third reviewer (HWHT). Where necessary, attempts were made to contact authors for additional information.
Results
A total of 2,652 articles were initially identified. Afterward, 1,542 duplicates were excluded, and the remaining 1,110 underwent title and abstract review. In this step, 382 irrelevant articles were removed, leaving 103 full-text articles for review. Sixty-three articles were excluded due to unavailability of full text, 10 due to unclear data, 3 non-Chinese or non-English articles were removed, and 5 non-randomized controlled trials (RCTs) were also excluded. Finally, 39 RCTs (6–44) were included in this review (Table 1).
Study characteristics
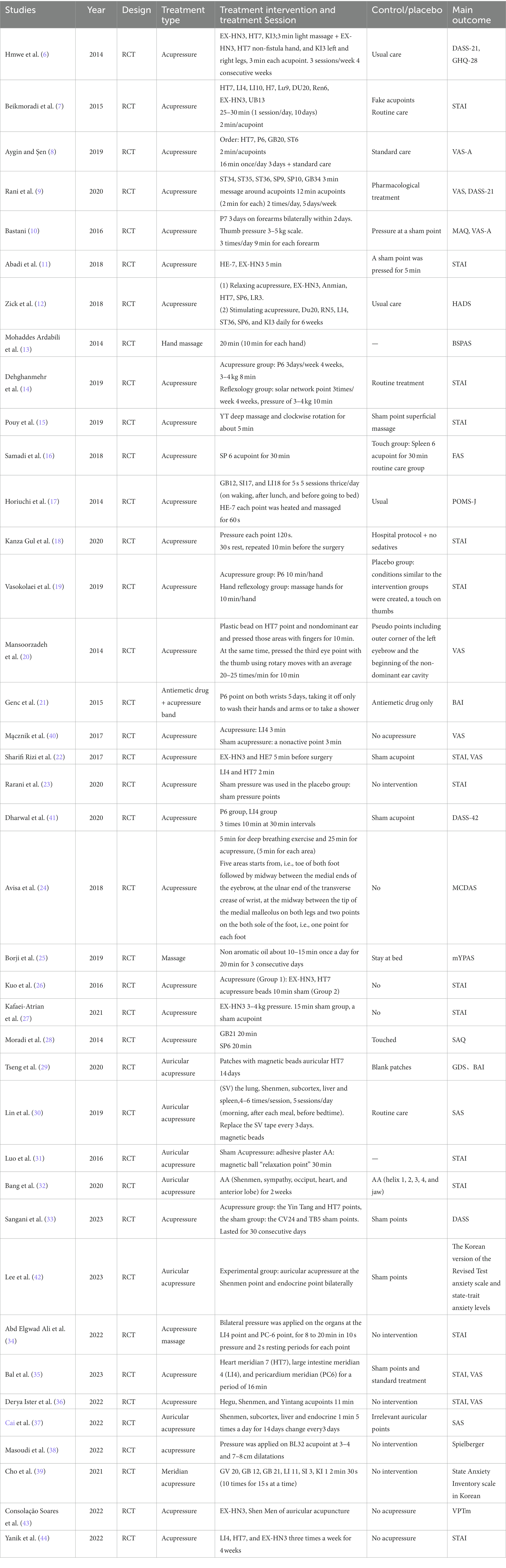
This Meta-analysis included 39 RCT articles and a total of 3,395 cases, with 1902 and 1,493 cases in the test and control groups, respectively. The study participants mainly consisted of two categories: healthy individuals and patients. The healthy group included women in labor, parents of children undergoing surgery, military personnel, college students and so on. The patient group included pre-and post-surgical patients, cancer survivors, hemodialysis patients, burns, sports injuries and so on. Anxiety was evaluated using several indicators, including STAI, VAS-A, DASS-42, DASS-21, MAQ, HADS, BSPAS, FAS, POMS-J, Beck Anxiety, BAI, MCDAS, mYPAS, SAQ, GAD-7, PQOL, SAS, GDS, and various physiological parameters. Of these, the STAI and VAS were the most commonly applied (see Table 1).
Quality critical appraisal
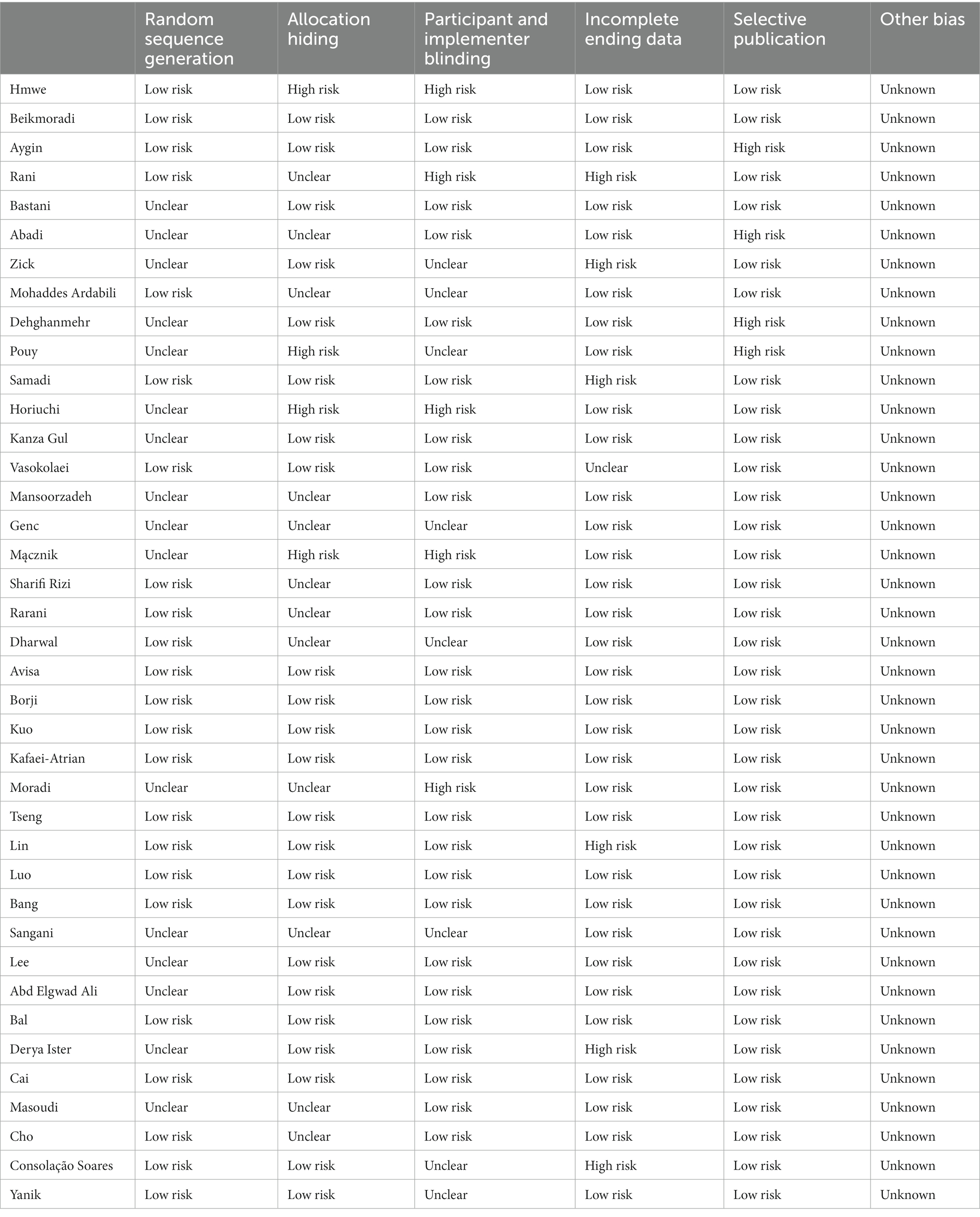
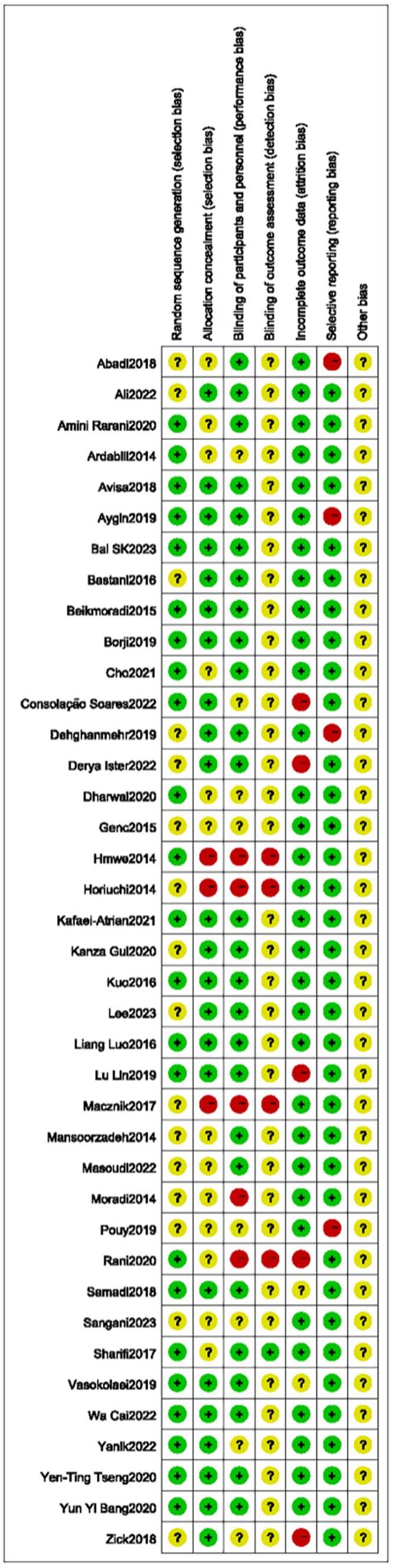
Twenty-four (6–9, 13, 16, 19, 22–25, 29–32, 44) of the included RCTs were evaluated as having a low risk of bias in the randomization sequence generation, based on detailed description of randomization methods. Sixteen trials (10–12, 14, 15, 17, 18, 20, 21, 26–28, 33–36, 38, 40, 42) lack detailed information, resulting in an unclear risk of bias in randomization. Four trials (6, 15, 17, 40) used open randomization of random numbers table, resulting in a high risk of bias in concealment. Twelve trials (9, 11, 13, 20–23, 28, 33, 39, 41, 43) without sufficient detail were regarded as having an unclear risk of bias in allocation concealment. The remaining trials were evaluated as having a low risk of bias in allocation concealment.
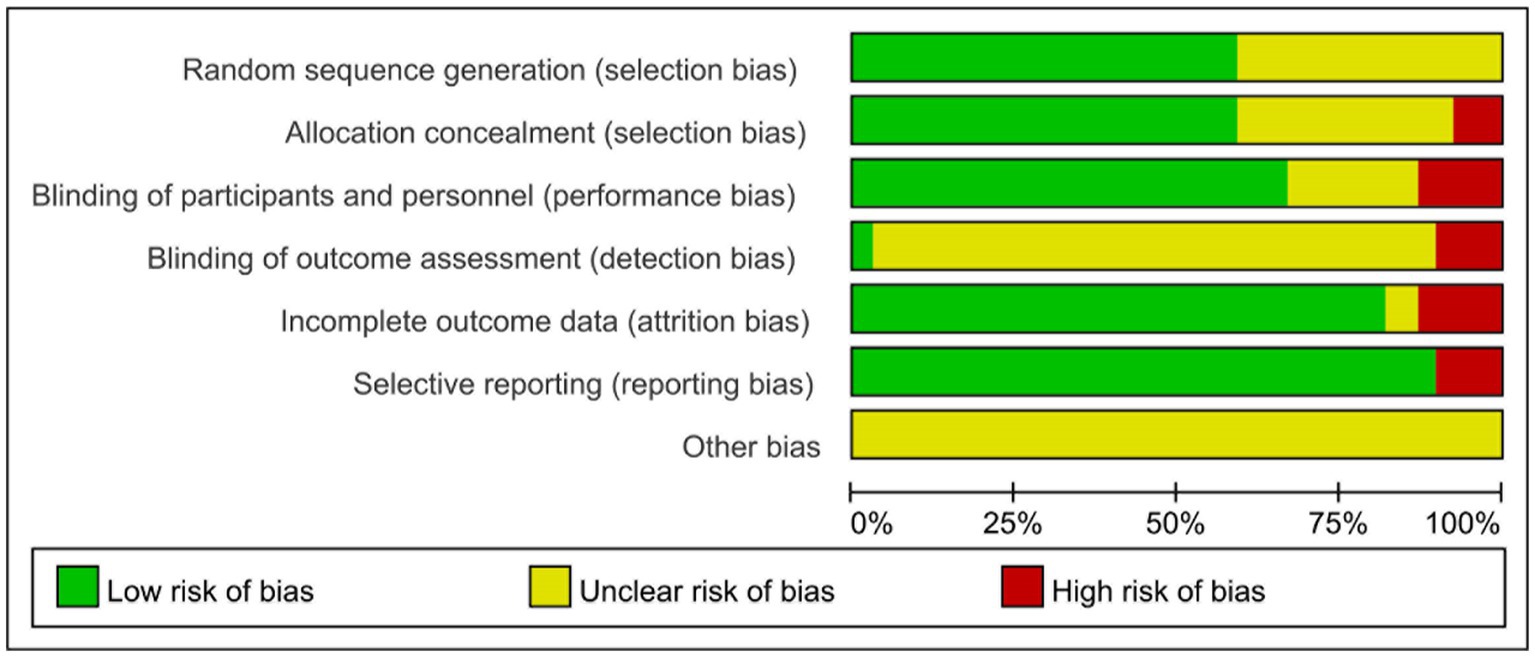
Only one (6) of the 39 studies described the blinding method for outcome evaluators. Eight studies (12, 13, 15, 21, 33, 41, 44, 45) did not describe blinding methods, and five (6, 9, 17, 22, 30) indicated that assessors were not blinded. Six studies (9, 12, 16, 30, 36, 43) exhibited a high risk of data integrity. One trial (19) without sufficient detail was considered as having an unclear risk of bias in allocation concealment. Four studies (8, 11, 14, 15) selectively report results, indicating in a high risk of bias. Other studies (20, 23, 36–38, 40) had registered online with specified outcomes, leading to a low risk of bias in selective reporting. All trials had an unknown risk in other sources of bias. Details of the risk of bias were summarized in Table 2, (Figures 1, 2).
Meta analysis results
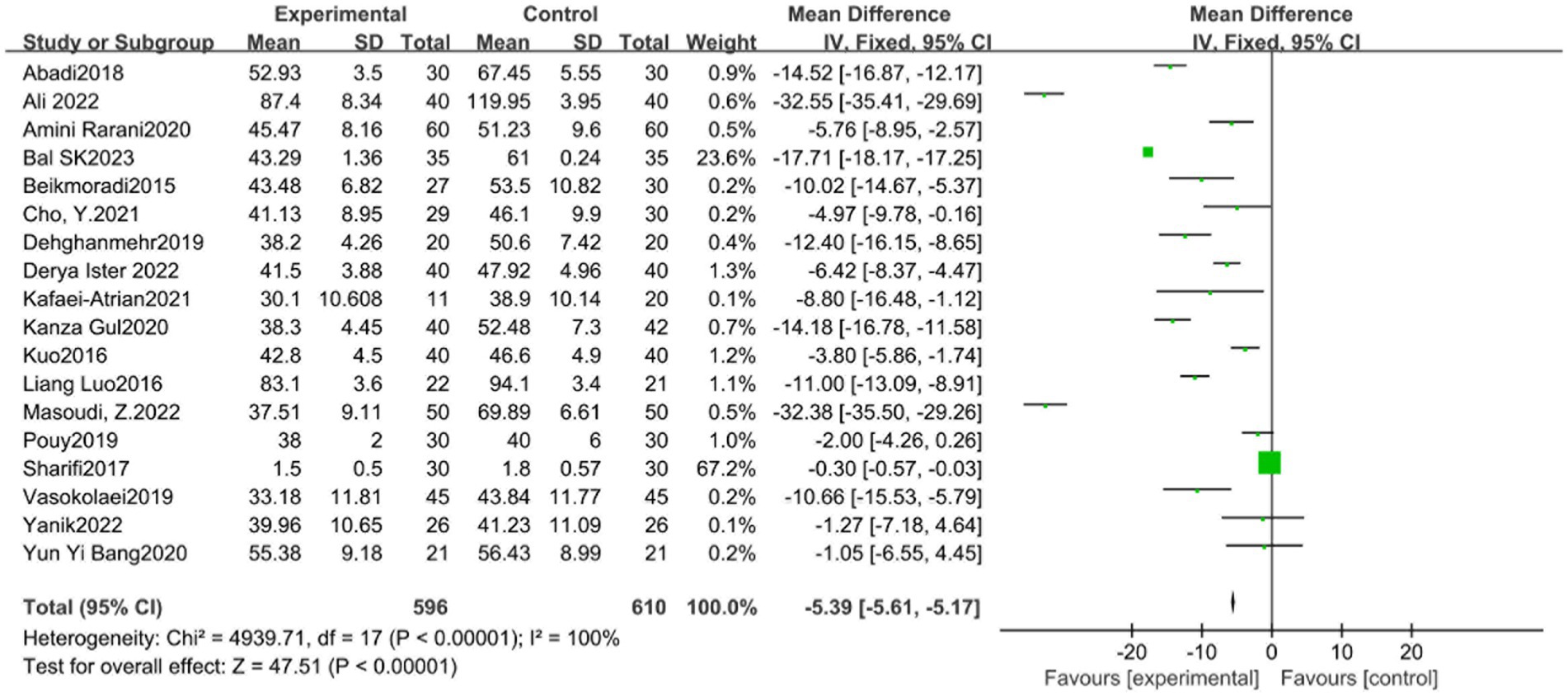
STAI scale
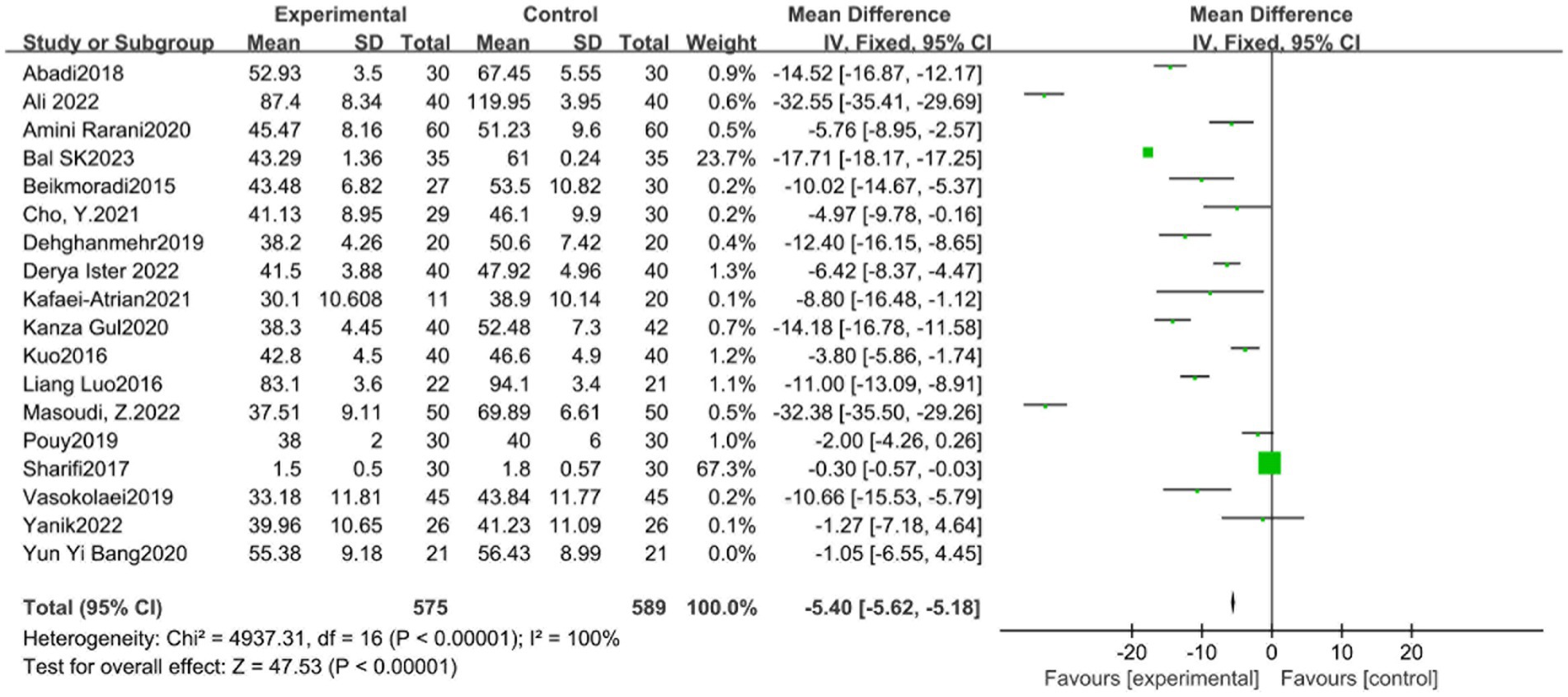
The STAI scale included 18 studies. The experimental group (596 cases) and the control group (610 cases) demonstrated significant heterogeneity among the studies (p < 0.00001, I2 = 100%), as shown in Figure 3. Sensitivity analysis showed that the study of Sharifi Rizi et al. (6, 15, 17, 40) may be the primary source of heterogeneity. Heterogeneity among studies decreased after the exclusion of this reference (p < 0.00001, I2 = 100%). Given the source of heterogeneity was related to the differences in the study subjects, subgroup analysis was conducted according to the characteristics of the study subjects (group 1 patients and group 2 non-patients). The analysis results showed significant difference between the experimental group (SMD = −5.39, 95% CI: −5.61 to −5.17, p < 0.01) and the control group (SMD = −5.40, 95% CI: −5.62 to −5.18, p < 0.01) in both subgroups. However, the funnel plot (Figure 4) suggested potential publication bias, thereby reducing the credibility of the conclusion.
VAS scale
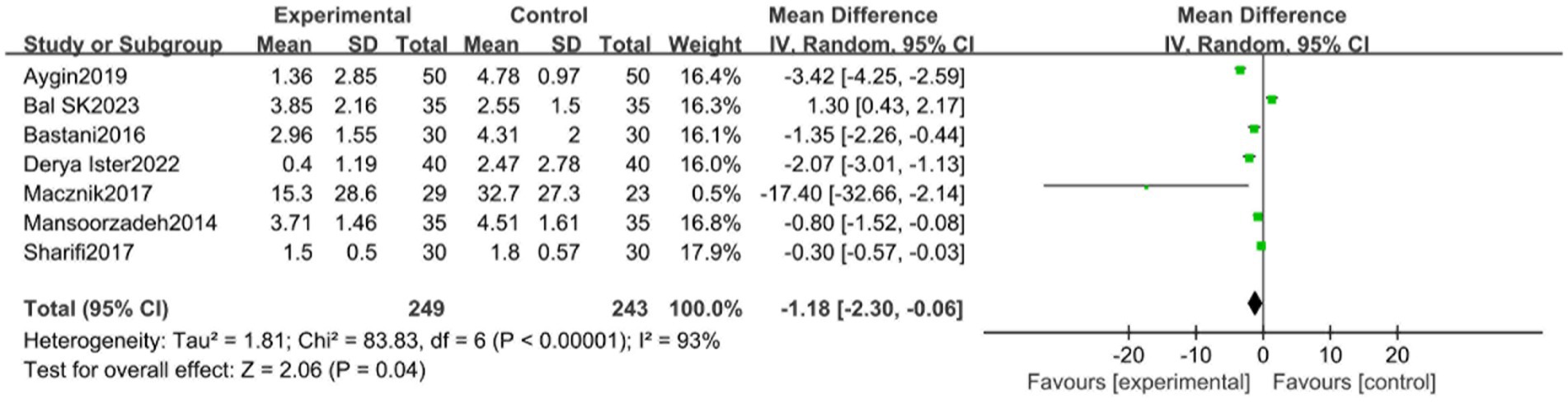
In assessing the Visual Analogue Scale (VAS), a total of 6 studies were incorporated. These studies, divided into an experimental group (249 participants) and a control group (243 participants), demonstrated significant heterogeneity (p < 0.00001, I2 = 93%), as illustrated in Figure 5. Sensitivity analysis identified the study by Aygin et al. (8) as a potential source of heterogeneity. Upon its exclusion, the heterogeneity among studies decreased (p < 0.00001, I2 = 87%).
SAS scale
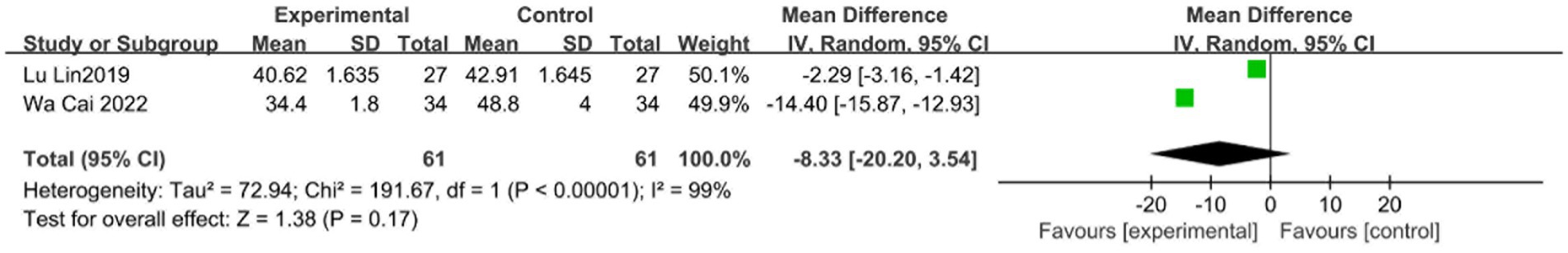
Two studies were included in the evaluation of the Self-Rating Anxiety Scale (SAS). Both the experimental group (61 participants) and the control group (61 participants) displayed significant heterogeneity among the studies (p < 0.00001, I2 = 99%), as depicted in Figure 6.
DASS scale
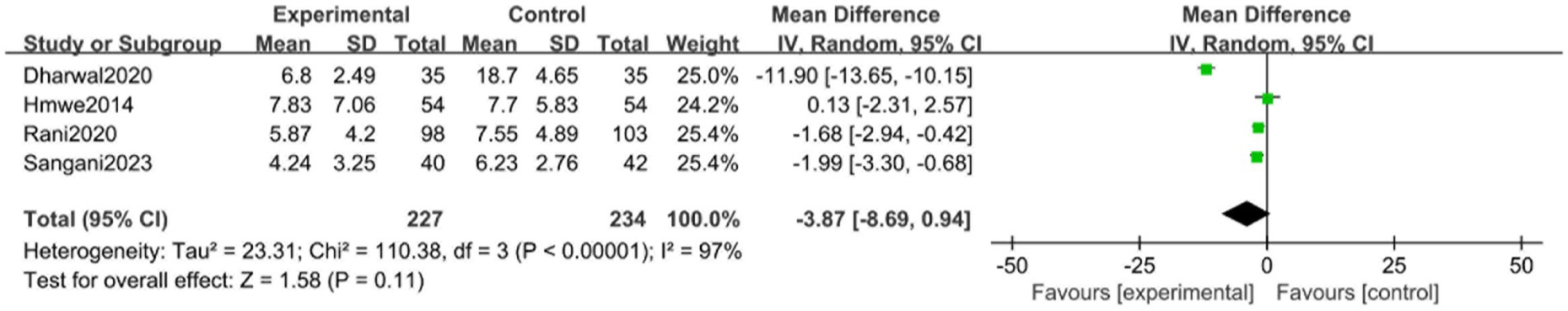
Four studies were included in the evaluation of the Depression Anxiety and Stress Scale (DASS-21/DASS-42). With 227 participants in both the experimental group and the control group, there was significant heterogeneity across the studies (p < 0.00001, I2 = 97%), as indicated in Figure 7. Sensitivity analysis indicated the study of Dharwal et al. (41) as a possible cause of heterogeneity. Once this reference was excluded, heterogeneity among studies decreased (p < 0.00001, I2 = 12%).
BAI scale
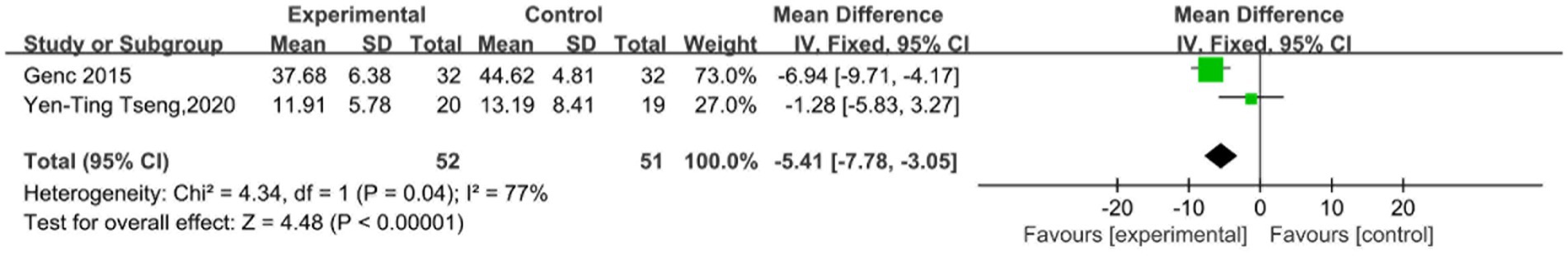
In assessing the Beck Anxiety Inventory (BAI), two studies were included, encompassing an experimental group (61 participants) and a control group (52 participants). These studies showed heterogeneity (p < 0.00001, I2 = 77%), as shown in Figure 8.
Similarly, VAS, SAS, DASS, and BAI scales included studies demonstrating significant heterogeneity (p < 0.00001, I2 > 75% for all scales). Sensitivity analyses and exclusion of certain studies decreased heterogeneity in each scale. Nine studies evaluated anxiety using HADS (12), BSPAS (13), FAS (16), POMS-J (17), MCDAS (24), mYPAS (25), SAQ (28), RTA (42), and VPTm (43). They were excluded because they were not representative and had fewer than two studies included, making them unsuitable for bias risk assessment.
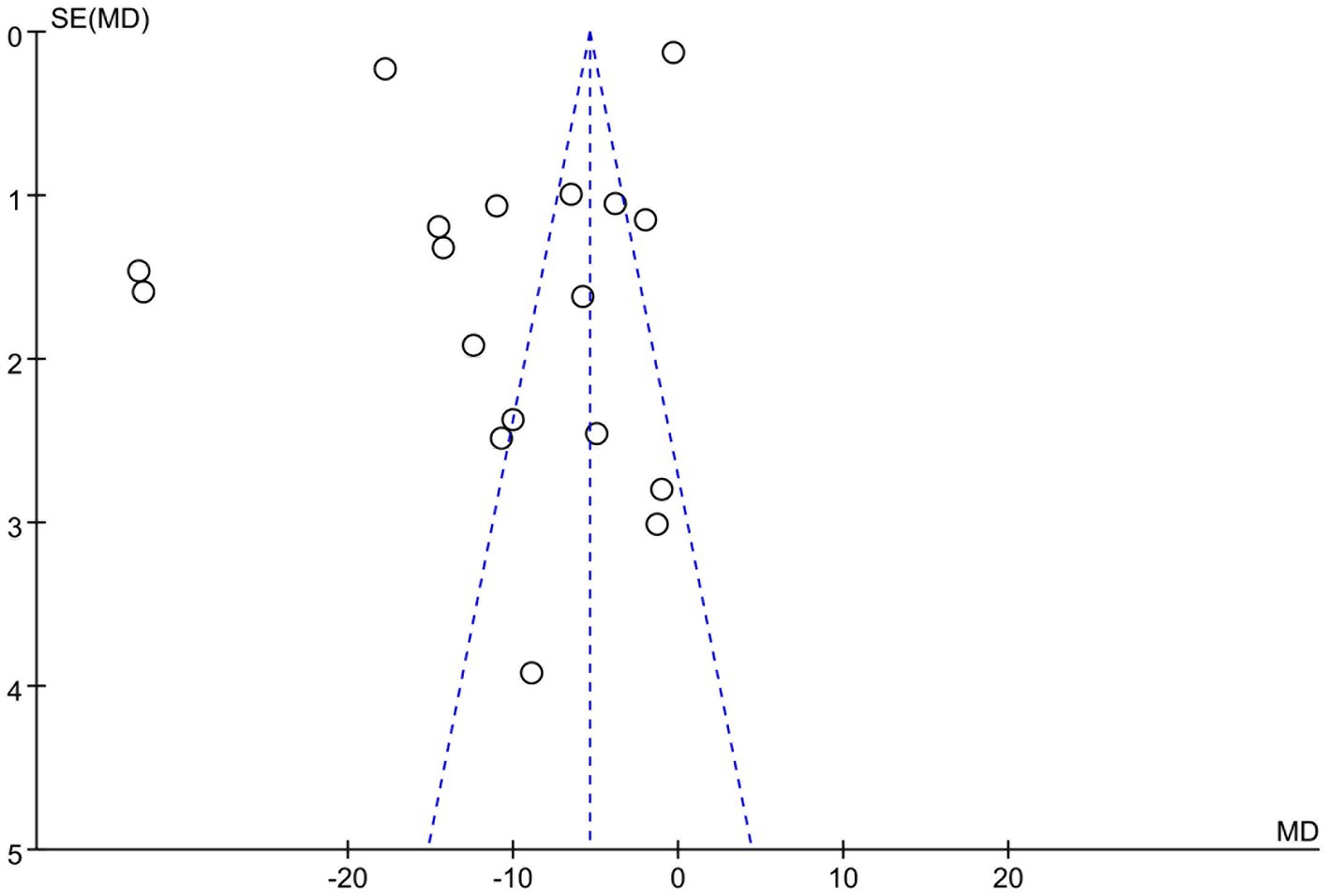
Sensitivity analysis and publication bias
Sensitivity analysis suggested that the main sources of heterogeneity came from the studies of Aygin and Şen (8), Rani et al. (9) and Sharifi Rizi et al. (22), as I2 decreased to 51% after their removal (Figure 9). The funnel plot of changes in anxiety levels was symmetric, indicating no detectable publication bias (Figure 4).
Subgroup analysis
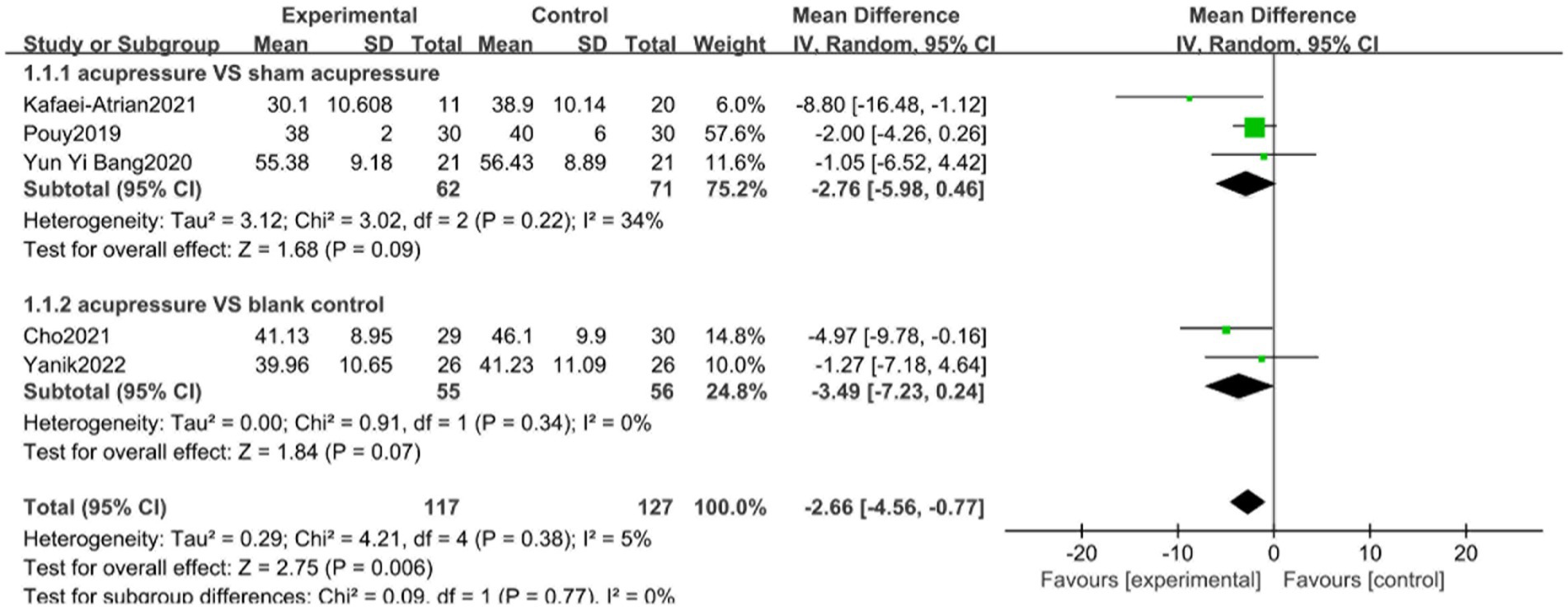
Subgroup analysis was conducted to verify whether different interventions in the control group would influence changes in anxiety levels. According to the STAI subgroup analysis, the therapeutic effect of the acupressure group on anxiety levels was higher than that of the sham intervention group and blank control group, with low heterogeneity between groups (I2 = 0%, p = 0.77) (Figure 10). Three trials (15, 27, 32) including 133 patients using random effects models demonstrated that acupressure was more effective than sham acupressure in improving changes in anxiety levels (SMD −2.76, 95% CI: −5.98 to 0.46, p = 0.09). Two trials (39, 44) compared acupressure and blank controls in assessing the effect on changes in anxiety levels, but results were significantly different (SMD −3.49, 95% CI: −7.23 to 0.24, p = 0.07).
Discussion
Of the total of 3,395 studies reviewed, including 39 randomized controlled trials, 103 systematic reviews and 18 meta-analysis (Figure 11), acupressure was found to be an effective intervention for anxiety. Sham acupressure and blank controls are typically designed to help mitigate bias when assessing acupressure’s specific effects. According to the results of subgroup analysis, the acupressure group displayed a higher therapeutic effect on anxiety levels than the sham intervention group and the blank control group.
Current treatments on anxiety
Anxiety symptoms typically encompass both physical and psychological manifestations such as excessive worry, fatigue, muscle or jaw tension, sleep difficulties, increased heart rate, and sweating. Severe anxiety may also induce symptoms like nausea, headaches, and lack of concentration. To alleviate these symptoms, many individuals resort to use medication including benzodiazepines (45), non-benzodiazepines and anti-anxiety antidepressants, which can potentially lead to side effects and dependency (46, 47). Psychotherapy, through physical and verbal communication, can establish a positive doctor-patient relationship, guiding and aiding patients to alter detrimental behavior habits, cognitive concepts and psychological states (48).
Physical therapy methods such as massage, acupuncture, transcranial magnetic stimulation treatment can also alleviate anxiety and soothe the body and mind. Studies suggest that acupuncture and electroacupuncture can effectively treat anxiety either independently or as adjuncts to pharmacological therapy (49). Acupuncture therapy may reduce preoperative patient anxiety (50). rTMS presents as a feasible therapeutic option for high-prevalence neuropsychiatric dysfunctions and contributes to our understanding of pathological and neuropsychological adaptation processes (51).
Other treatments include practices like yoga, jogging, tai chi and other aerobic exercises, as well as distraction by studying, listening to music, painting, etc., which can all contribute to treating anxiety disorders. Meta-analyses and systematic reviews have shown that these interventions can improve symptoms of depression and anxiety disorders (52).
Effects of acupressure on anxiety
Acupressure, an ancient nonpharmacological technique used for symptom management, involves the application of steady, gentle pressure on one or more of the body’s 365 energy points across 12 meridians, thereby creating balance and releasing energy. Simple to administer and requiring no instruments, acupressure is suitable for various demographics, from children to the elderly, and can aid in managing clinical symptoms such as dyspnea, pain, insomnia, nausea and vomiting. From a scientific perspective, acupressure aims to influence the sympathetic and parasympathetic systems through pressure application, thereby releasing neurotransmitters and mediators (53), and ultimately relieving anxiety. Studies indicate that acupressure is effective for generalized anxiety disorder and provides lasting benefits (54).
Mechanism of acupressure on anxiety
The etiology and pathogenesis of anxiety disorder are complex, believed to involve a variety of factors including genetics, neurobiochemistry, neuroimaging, sex hormones, constitution and other reasons (55–57). Contemporary studies propose that the pathogenesis of anxiety disorder primarily encompasses neurotransmitter hypothesis and neuroendocrine dysfunction hypothesis, specifically the serotonin system, the hypothalamic-pituitary-adrenal (HPA) axis (58), and hypothalamic-pituitary-gonadal (HPG) axis activity (59).
The potential mechanism of acupressure and its treatment of anxiety remains unclear. Most existing literature focuses on general clinical summaries or efficacy observations, and few studies delving into basic research. Acupressure is believed to stimulate specific points on the body, regulating human function, balancing yin and yang, relieving fatigue, and preventing disease (59). The temple can regulate the autonomic nervous system, compensate the heart, and calm the mind. The product of the three yin, involving the liver, spleen, kidney meridians, can have soothing effects. Acupressure massage, grounded in meridian acuity theology, uses massage as the main treatment method, serving as a preventative and therapeutic approach (46). The primary physiological reasons involved in the massage stimulation process might include the stimulation of serotonin to alleviate pain or emotional discomfort and/or expected psychological responses to stress or perceived environmental threats. Acupressure massage has been shown to reduce heart rate, pulse rate and blood pressure by suppressing the sympathetic nerve and activating the parasympathetic nerve, thus relieving anxiety (60).
Mechanism of acupressure on anxiety recent advances in animal models of anxiety, have greatly enhanced our understanding of the potential mechanisms of acupoint therapy in treating anxiety disorders. Four potential mechanisms have been proposed: it may be related to the up-regulation of atrial natriuretic peptide (ANP) expression and downregulation of C-type natriuretic peptide (CNP) expression in the peripheral adrenal medulla, which in turn inhibits the release of corticosterone (CORT) and the activity of hypothalamic-pituitary-adrenal axis (HPA) (61). Acupressure may inhibit the elevation of amygdala-like norepinephrine (NE) and 3-methoxy-4-hydroxyphenylethylene glycol (MHPG), induced by acute restraint stress (ARS), and prevent the enhancement of tyrosine hydroxylase protein and mRNA expression in the central nucleus of amygdala (CeA) (62). Acupressure can also significantly reduced depressive-like behaviors caused by chronic unpredictable stress (CUS), and the expression of certain NLRP3 and mature IL-1b (63). Lastly, following Tuina, anxiety-like behaviors were efficiently reduced, and the hyperactivity of the HPA axis was efficiently inhibited, along with enhanced GR expression in the hippocampus and lung (64).
Intervention population
Although the effectiveness of acupressure in relieving STAI has been confirmed, the heterogeneity is relatively large. This could be attributed to the wide range of research subjects included in this study, encompassing healthy individuals such as expectant mothers, parents of children awaiting surgery, military personnel, and college students, as well as patients with various pre- and post-surgery, cancer, hemodialysis, burns, sports injuries. However, subgroup analysis did not indicate a decrease in heterogeneity. This could be due to factors such as the choice of acupuncture points and massage duration.
Strengths and limitations
The global spread of COVID-19 has triggered numerous social issues related to health, economy, and society, all of which are important factors contributing to anxiety. To our knowledge, acupressure is a viable method for relieving anxiety. Amid widespread pandemic widespread concerns, acupressure serves massage as a practical treatment strategy with numerous advantages: it is easily implemented, cost-effective, safe, devoid of toxic side effects, and easy acceptance by people readily accepted by different age groups and populations.
Our study benefits from several strengths. Firstly, we focused our review on the effect of acupressure as a standalone treatment, excluding studies involving mixed therapies, and conducted a subgroup study of sham acupressure or blank control in the control group to verify whether acupressure’s effectiveness in treating anxiety. Secondly, our review included 39 RCTS with larger sample sizes and a variety of acupressure points. Compared with previous studies, our study included patients of varying ages, encompassing both diseased and non-diseased populations, thus providing strong evidence supporting the hypothesis that acupressure is effective in treating anxiety. Thirdly, the included studies were conducted at multiple locations and in different countries, covering a diverse range of ethnicities and cultures, potentially reducing selection bias and improving external validity. Fourthly, we conducted sensitivity analysis and funnel plot, indicating that the meta-analysis was stable, robust, and free from publication bias. Lastly, most of the studies were longitudinal, with one having a follow-up period of 1 year, which lends further support to the clinical practice of acupressure in the treatment of patients with anxiety.
However, there are limitations to consider when interpreting these results. This review only included RCTs, thereby excluding observational and non-randomized studies. Most of the included studies did not feature follow-up evaluations, preventing a comprehensive meta-analysis of acupressure’s long-term effects. The overall quality of the studies was low, particularly concerning allocation concealment and participant and personnel blindness. Furthermore, this review only included English-language, excluding potential insights from non-English sources.
Implications for further research
Acupressure demonstrates promising application prospects. However, a unified and standardized acupoint selection plan is lacking, and there are limited studies conducting in-depth analyses from an anti-anxiety mechanism perspective. Future research would benefit from a more standardized approach to acupressure point selection, alongside more extensive studies examining the anti-anxiety mechanisms involved.
Conclusion
Acupressure has a beneficial overall effect of acupressure in relieving anxiety. Considering the increasing incidence of anxiety caused by long COVID, acupressure represents an ideal treatment strategy. Its unique convenience and cost-effectiveness can expand its application and provide relief to a larger population suffering from anxiety. Further rigorous research focusing on the mechanisms behind its anti-anxiety effects, as well as well-designed studies to reinforce these findings, are necessary.
Author contributions
ZP: Formal analysis, Writing – review & editing. YZ: Writing – original draft. ZY: Writing – original draft, Methodology. HZ: Writing – review & editing. ZL: Writing – original draft, Data curation. MX: Writing – review & editing, Funding acquisition, Resources. SC: Writing – review & editing, Funding acquisition, Resources. RL: Writing – review & editing, Project administration, Supervision.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work has been sponsored by Chinese Medicine Key Medical Specialties Construction Project of Shenzhen Municipal Health Commission (grant no. ZYTS019).
Conflict of interest
The authors declare that the conduct of this study does not involve any commercial or financial relationships that could be interpreted as potential conflicts of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Pandey, K, Thurman, M, Johnson, SD, Acharya, A, Johnston, M, Klug, EA, et al. Mental health issues during and after COVID-19 vaccine era. Brain Res Bull. (2021) 176:161–73. doi: 10.1016/j.brainresbull.2021.08.012
2. Czeisler, M, Lane, RI, Petrosky, E, Wiley, JF, Christensen, A, Njai, R, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:1049–57. doi: 10.15585/mmwr.mm6932a1
3. Nishikawa-Pacher, A . Research questions with PICO: a universal mnemonic. Publications. (2022) 10:21. doi: 10.3390/publications10030021
4. Frankot, M, Mueller, PM, Young, ME, and Vonder, HC. Statistical power and false positive rates for interdependent outcomes are strongly influenced by test type: implications for behavioral neuroscience. Neuropsychopharmacology. (2023) 48:1612–22. doi: 10.1038/s41386-023-01592-6
5. Son, S, Yoo, BR, Lee, SG, Kim, WK, and Jung, JM. Full-endoscopic versus minimally invasive lumbar interbody fusion for lumbar degenerative diseases: a systematic review and meta-analysis. J Korean Neurosurg Soc. (2022) 65:539–48. doi: 10.3340/jkns.2021.0168
6. Hmwe, NT, Subramanian, P, Tan, LP, and Chong, WK. The effects of acupressure on depression, anxiety and stress in patients with hemodialysis: a randomized controlled trial. Int J Nurs Stud. (2015) 52:509–18. doi: 10.1016/j.ijnurstu.2014.11.002
7. Bikmoradi, A, Najafi, F, Roshanaei, G, Esmaeil, ZP, Khatibian, M, and Ahmadi, A. Acupressure and anxiety in cancer patients. Iran Red Crescent Med J. (2015) 17:e25919. doi: 10.5812/ircmj.25919
8. Aygin, D, and Şen, S. Acupressure on anxiety and sleep quality after cardiac surgery: a randomized controlled trial. J Perianesth Nurs. (2019) 34:1222–31. doi: 10.1016/j.jopan.2019.03.014
9. Rani, M, Sharma, L, Advani, U, and Kumar, S. Acupressure as an adjunct to pharmacological treatment for depression, anxiety, and stress in patients with knee osteoarthritis. J Acupunct Meridian Stud. (2020) 13:129–35. doi: 10.1016/j.jams.2020.07.001
10. Bastani, F . Effect of acupressure on maternal anxiety in women with gestational diabetes mellitus: a randomized clinical trial. Clin Nurs Res. (2016) 25:325–41. doi: 10.1177/1054773815579344
11. Abadi, F, Abadi, F, Fereidouni, Z, Amirkhani, M, Karimi, S, and Najafi, KM. Effect of acupressure on preoperative cesarean section anxiety. J Acupunct Meridian Stud. (2018) 11:361–6. doi: 10.1016/j.jams.2018.07.001
12. Zick, S, Schrepf, A, Hasset, A, Sen, A, and Harris, R. Depression, anxiety, and pain as potential mediators and moderators of self administered acupressure’s effect on fatigue and sleep quality in breast cancer survivors. Psycho-oncology. (2018) 27:74. doi: 10.1002/pon.4623
13. Mohaddes Ardabili, F, Purhajari, S, Najafi Ghzeljeh, T, and Haghani, H. The effect of shiatsu massage on underlying anxiety in burn patients. World J Plast Surg. (2015) 4:36–9.
14. Dehghanmehr, S, Sargazi, GH, Biabani, A, Nooraein, S, and Allahyari, J. Comparing the effect of acupressure and foot reflexology on anxiety and depression in hemodialysis patients: a clinical trial. Med Surg Nurs J. (2019) 8:e100386. doi: 10.5812/msnj.100386
15. Pouy, S, Etebarian, A, Saeidi, S, and Majidi, S. Evaluating the effectiveness of acupressure on anxiety of mothers in a pediatric surgical waiting area: a randomized clinical trial. Anaesth Crit Care Pain Med. (2019) 23:23–7.
16. Samadi, P, Alipour, Z, and Lamyian, M. The effect of acupressure at spleen 6 acupuncture point on the anxiety level and sedative and analgesics consumption of women during labor: a randomized, single-blind clinical trial. Iran J Nurs Midwifery Res. (2018) 23:87–92. doi: 10.4103/ijnmr.IJNMR_199_16
17. Horiuchi, S, Tsuda, A, Honda, Y, Kobayashi, H, Naruse, M, and Tsuchiyagaito, A. Mood changes by self-administered acupressure in Japanese college students: a randomized controlled trial. Global J Health Sci. (2015) 7:40–4. doi: 10.5539/gjhs.v7n4p40
18. Kanza Gul, D, and Solt, KA. Effects of acupressure on preoperative acute anxiety in cesarean section under spinal anesthesia: a double-blind randomized controlled study. Holist Nurs Pract. (2020) 34:356–64. doi: 10.1097/HNP.0000000000000413
19. Vasokolaei, ZR, Rejeh, N, Heravi-Karimooi, M, Tadrisi, SD, Saatchi, K, Poshtchaman, Z, et al. Comparison of the effects of hand reflexology versus acupressure on anxiety and vital signs in female patients with coronary artery diseases. Healthcare. (2019) 7:26. doi: 10.3390/healthcare7010026
20. Mansoorzadeh, KH, Afazel, MR, Taghadosi, M, and Gilasi, HR. The effect of acupressure on anxiety and dysrhythmia in patients undergoing cardiac catheterization. Life Sci J. (2014) 11:153–7.
21. Genc, F, and Tan, M. The effect of acupressure application on chemotherapy-induced nausea, vomiting, and anxiety in patients with breast cancer. Palliat Support Care. (2015) 13:275–84. doi: 10.1017/S1478951514000248
22. Sharifi Rizi, M, Shamsalinia, A, Ghaffari, F, Keyhanian, S, and Naderi, NB. The effect of acupressure on pain, anxiety, and the physiological indexes of patients with cancer undergoing bone marrow biopsy. Complement Ther Clin Pract. (2017) 29:136–41. doi: 10.1016/j.ctcp.2017.09.002
23. Rarani, SA, Rajai, N, and Sharififar, S. Effects of acupressure at the P6 and LI4 points on the anxiety level of soldiers in the Iranian military. BMJ Mil Health. (2021) 167:177–81. doi: 10.1136/jramc-2019-001332
24. Avisa, P, Kamatham, R, Vanjari, K, and Nuvvula, S. Effectiveness of acupressure on dental anxiety in children. Pediatr Dent. (2018) 40:177–83.
25. Borji, M, Pouy, S, Yaghobi, Y, and Nabi, BN. Effectiveness of acupressure on anxiety of children undergoing anesthesia. Int J Adolesc Med Health. (2019) 33. doi: 10.1515/ijamh-2018-0177
26. Kuo, SY, Tsai, SH, Chen, SL, and Tzeng, YL. Auricular acupressure relieves anxiety and fatigue, and reduces cortisol levels in post-caesarean section women: a single-blind, randomised controlled study. Int J Nurs Stud. (2016) 53:17–26. doi: 10.1016/j.ijnurstu.2015.10.006
27. Kafaei-Atrian, M, Mirbagher-Ajorpaz, N, Sarvieh, M, Sadat, Z, Asghari-Jafarabadi, M, and Solhi, M. The effect of acupressure at third liver point on the anxiety level in patients with primary dysmenorrhea. Iran J Nurs Midwifery Res. (2016) 21:142–6. doi: 10.4103/1735-9066.178233
28. Moradi, Z, Akbarzadeh, M, Moradi, P, Toosi, M, and Hadianfard, MJ. The effect of acupressure at GB-21 and SP-6 acupoints on anxiety level and maternal-fetal attachment in primiparous women: a randomized controlled clinical trial. Nurs Midwifery Stud. (2014) 3:e19948. doi: 10.17795/nmsjournal19948
29. Tseng, YT, Chen, IH, Lee, PH, and Lin, PC. Effects of auricular acupressure on depression and anxiety in older adult residents of long-term care institutions: a randomized clinical trial. Geriatr Nurs. (2021) 42:205–12. doi: 10.1016/j.gerinurse.2020.08.003
30. Lin, L, Zhang, Y, Qian, HY, Xu, JL, Xie, CY, Dong, B, et al. Auricular acupressure for cancer-related fatigue during lung cancer chemotherapy: a randomised trial. BMJ Support Palliat Care. (2021) 11:32–9. doi: 10.1136/bmjspcare-2019-001937
31. Luo, L, Dai, Q, Mo, Y, Yan, Y, Qian, M, Zhuang, X, et al. The effect of auricular acupressure on preoperative anxiety in patients undergoing gynecological surgery. Int J Clin Exp Med. (2016) 9:4065–70.
32. Bang, YY, and Park, H. Effects of auricular acupressure on the quality of sleep and anxiety in patients undergoing cardiac surgery: a single-blind, randomized controlled trial. Appl Nurs Res. (2020) 53:151269. doi: 10.1016/j.apnr.2020.151269
33. Sangani, NJ, Rahimi, H, Mirzaei, SMM, BahramiTaghanaki, H, and Vagharseyyedin, SA. Effect of acupressure on anxiety, stress, and depression among the primary family caregivers of the patients with stroke. J Holist Nurs Midwifery. (2023) 33:113–21. doi: 10.32598/jhnm.33.2.2303
34. Abd Elgwad Ali, IS, Ali, ZH, and Hasan, SN. The effect of acupressure on severity of pain and level of anxiety for patients post coronary artery bypass graft. Afr J Nurs Midwifery. (2022) 5:91–110. doi: 10.52589/AJHNM-FQOINTFB
35. Bal, SK, and Gun, M. The effects of acupressure on pain, anxiety and vital signs in patients undergoing coronary angiography: a randomized and sham-controlled trial. Explore. (2023). doi: 10.1016/j.explore.2023.07.001
36. Derya Ister, E, and Altinbas, Y. The effect of acupressure on anxiety and pain among patients undergoing coronary angiography: a randomized controlled trial. Holist Nurs Pract. (2022) 36:E57–63. doi: 10.1097/HNP.0000000000000553
37. Cai, W, Zhang, K, Wang, GT, Li, J, Wei, XY, Ma, W, et al. Effects and safety of auricular acupressure on depression and anxiety in isolated COVID-19 patients: a single-blind randomized controlled trial. Front Psychiatry. (2022) 13:1041829. doi: 10.3389/fpsyt.2022.1041829
38. Masoudi, Z, Kasraeian, M, and Akbarzadeh, M. Assessment of educational intervention and acupressure during labor on the mother’s anxiety level and arterial oxygen pressure of the umbilical cord of infants (PO2). A randomized controlled clinical trial. J Educ Health Promot. (2022) 11:86. doi: 10.4103/jehp.jehp_685_20
39. Cho, Y, Joo, JM, Kim, S, and Sok, S. Effects of meridian acupressure on stress, fatigue, anxiety, and self-efficacy of shiftwork nurses in South Korea. Int J Environ Res Public Health. (2021) 18:4199. doi: 10.3390/ijerph18084199
40. Mącznik, AK, Schneiders, AG, Athens, J, and Sullivan, SJ. Does acupressure hit the mark? A three-arm randomized placebo-controlled trial of acupressure for pain and anxiety relief in athletes with acute musculoskeletal sports injuries. Clin J Sport Med. (2017) 27:338–43. doi: 10.1097/JSM.0000000000000378
41. Dharwal, J, Srinivasan, P, and Kanika, SJ. Effect of acupressure on anxiety among patients undergoing hemodialysis in selected hospitals of Ambala, Haryana: a randomized controlled trial. Appl Nurs Res. (2020) 11:345–51.
42. Lee, E, and Park, JH. Effect of acupressure on pre-exam anxiety in nursing students. Altern Ther Health Med. (2023) 29:158–63.
43. Consolação Soares, ME, de Souza, AA, Lagares Pinto, IC, Araújo Barbosa, LS, Borsatto, MC, and Galo, R. Effect of acupressure on dental anxiety in children: a pilot study for a randomized clinical trial. J Acupunct Meridian Stud. (2022) 15:307–13. doi: 10.51507/j.jams.2022.15.5.307
44. Yanik, TC, Kanat, C, Karaman, A, Yilmaz, SG, and Ugras, GA. Effect of acupressure on senior nursing students’ anxiety during the COVID-19 pandemic: a randomized controlled clinical trial. Int J Caring Sci. (2023) 16:218–25.
45. Balon, R, and Starcevic, V. Role of benzodiazepines in anxiety disorders. Adv Exp Med Biol. (2020) 1191:367–88. doi: 10.1007/978-981-32-9705-0_20
46. Shyken, JM, Babbar, S, Babbar, S, and Forinash, A. Benzodiazepines in Pregnancy. Clin Obstet Gynecol. (2019) 62:156–67. doi: 10.1097/GRF.0000000000000417
47. Dubovsky, SL, and Marshall, D. Benzodiazepines remain important therapeutic options in psychiatric practice. Psychother Psychosom. (2022) 91:307–34. doi: 10.1159/000524400
48. Dickson, SJ, Kuhnert, RL, Lavell, CH, and Rapee, RM. Impact of psychotherapy for children and adolescents with anxiety disorders on global and domain-specific functioning: a systematic review and meta-analysis. Clin Child Fam Psychol Rev. (2022) 25:720–36. doi: 10.1007/s10567-022-00402-7
49. Amorim, D, Brito, I, Caseiro, A, Figueiredo, JP, Pinto, A, Macedo, I, et al. Electroacupuncture and acupuncture in the treatment of anxiety—a double blinded randomized parallel clinical trial. Complement Ther Clin Pract. (2022) 46:101541. doi: 10.1016/j.ctcp.2022.101541
50. Tong, QY, Liu, R, Zhang, K, Gao, Y, Cui, GW, and Shen, WD. Can acupuncture therapy reduce preoperative anxiety? A systematic review and meta-analysis. J Integr Med. (2021) 19:20–8. doi: 10.1016/j.joim.2020.10.007
51. Rodrigues, PA, Zaninotto, AL, Neville, IS, Hayashi, CY, Brunoni, AR, Teixeira, MJ, et al. Transcranial magnetic stimulation for the treatment of anxiety disorder. Neuropsychiatr Dis Treat. (2019) 15:2743–61. doi: 10.2147/NDT.S201407
52. Saeed, SA, Cunningham, K, and Bloch, RM. Depression and anxiety disorders: benefits of exercise, yoga, and meditation. Am Fam Physician. (2019) 99:620–7.
53. Hou, PW, Hsu, HC, Lin, YW, Tang, NY, Cheng, CY, and Hsieh, CL. The history, mechanism, and clinical application of auricular therapy in traditional Chinese medicine. Evid Based Complement Alternat Med. (2015) 2015:1–13. doi: 10.1155/2015/495684
54. Chen, SR, Hou, WH, Lai, JN, Kwong, JSW, and Lin, PC. Effects of acupressure on anxiety: a systematic review and meta-analysis. J Integr Complement Med. (2022) 28:25–35. doi: 10.1089/jicm.2020.0256
55. Chellappa, SL, and Aeschbach, D. Sleep and anxiety: from mechanisms to interventions. Sleep Med Rev. (2022) 61:101583. doi: 10.1016/j.smrv.2021.101583
56. Di Iorio, CR, Carey, CE, Michalski, LJ, Corral-Frias, NS, Conley, ED, Hariri, AR, et al. Hypothalamic-pituitary-adrenal axis genetic variation and early stress moderates amygdala function. Psychoneuroendocrinology. (2017) 80:170–8. doi: 10.1016/j.psyneuen.2017.03.016
57. Au, DW, Tsang, HW, Ling, PP, Leung, CH, Ip, PK, and Cheung, WM. Effects of acupressure on anxiety: a systematic review and meta-analysis. Acupunct Med. (2015) 33:353–9. doi: 10.1136/acupmed-2014-010720
58. Juruena, MF, Eror, F, Cleare, AJ, and Young, AH. The role of early life stress in HPA axis and anxiety. Adv Exp Med Biol. (2020) 1191:141–53. doi: 10.1007/978-981-32-9705-0_9
59. Pawluski, JL, Swain, JE, and Lonstein, JS. Neurobiology of peripartum mental illness. Handb Clin Neurol. (2021) 182:63–82. doi: 10.1016/B978-0-12-819973-2.00005-8
60. Tsai, YH, Wu, SY, Hu, WL, Lai, YR, Tsao, Y, Yen, KT, et al. Immediate effect of non-invasive auricular acupoint stimulation on the performance and meridian activities of archery athletes: a protocol for randomized controlled trial. Medicine. (2021) 100:e24753. doi: 10.1097/MD.0000000000024753
61. Yao, H, Wei, D, Cai, D, Yu, S, Zhang, C, Wei, J, et al. Effects of acupuncture on ANP and CNP in adrenal gland and CORT in plasma in rats with chronic emotional stress anxiety. Zhongguo Zhen Jiu. (2016) 36:169–74.
62. Zhao, Z, Kim, SC, Liu, H, Zhang, J, Wang, Y, Cho, IJ, et al. Manual acupuncture at PC6 ameliorates acute restraint stress-induced anxiety in rats by normalizing amygdaloid noradrenergic response. Evid Based Complement Alternat Med. (2017) 2017:1–8. doi: 10.1155/2017/4351723
63. Yue, N, Li, B, Yang, L, Han, QQ, Huang, HJ, Wang, YL, et al. Electro-acupuncture alleviates chronic unpredictable stress-induced depressive- and anxiety-like behavior and hippocampal neuroinflammation in rat model of depression. Front Mol Neurosci. (2018) 11:149. doi: 10.3389/fnmol.2018.00149
Keywords: COVID-19, acupuncture, acupressure, anxiety, meta-analysis
Citation: Peng Z, Zheng Y, Yang Z, Zhang H, Li Z, Xu M, Cui S and Lin R (2024) Acupressure: a possible therapeutic strategy for anxiety related to COVID-19: a meta-analysis of randomized controlled trials. Front. Med. 11:1341072. doi: 10.3389/fmed.2024.1341072
Edited by:
César Fernández-de-las-Peñas, Rey Juan Carlos University, SpainReviewed by:
Hector Wing Hong Tsang, Hong Kong Polytechnic University, Hong Kong SAR, ChinaHuangHsi Chen, Chung Shan Medical University Hospital, Taiwan
Copyright © 2024 Peng, Zheng, Yang, Zhang, Li, Xu, Cui and Lin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shaoyang Cui, aGVyYjEwN0BxcS5jb20=;Run Lin, MTE0MTcyNzMyNEBxcS5jb20=
†These authors have contributed equally to this work and share first authorship
 Zhihua Peng1†
Zhihua Peng1† Zeyu Yang
Zeyu Yang Shaoyang Cui
Shaoyang Cui Run Lin
Run Lin