- 1Institute of General Practice and Interprofessional Care, University Hospital Tuebingen, Tuebingen, Germany
- 2First Department of Medicine, Division of Angiology, Faculty of Medicine of the University of Heidelberg, University Medical Center Mannheim, Mannheim, Germany
- 3Practice for Traditional Chinese Medicine & Western Medicine, Oberschleissheim, Germany
- 4Institute of Medical Biometry, Department Medical Biometry, University of Heidelberg, Heidelberg, Germany
- 5Heidelberg School of Chinese Medicine, Heidelberg, Germany
Background: Globally, diabetes mellitus (DM) and peripheral artery disease (PAD) have an increasing incidence and a high prevalence and are both associated with high morbidity and complication rates, e.g., as chronic non-healing peripheral ulcers. Impaired macro- and microcirculation and peripheral neuropathy lead to an increased risk of foot ulcers and infections. These complications are difficult to treat, have a high risk of becoming chronic and often lead to lower limb amputation. The aim of this planned study was to investigate the potential effects of acupuncture on improving microcirculation in patients with Diabetic Foot Syndrome (DFS) and PAD.
Materials and methods: In 18 patients with chronic non-healing peripheral ulcers and diagnosed DM or PAD, data on 8 microcirculatory parameters were collected simultaneously on intact skin close to the wound margin. Microcirculation was assessed using an O2C device combining laser Doppler shift and white light spectroscopy (LEA Medizintechnik GmbH, Giessen, Germany). Unilateral and bilateral acupuncture was performed on the connecting line between acupuncture points Stomach 14 and Stomach 15.
Results: After unilateral acupuncture (ipsilateral to the wound side), a statistically significant improvement in 7 out of 8 microcirculatory parameters was demonstrated compared to baseline measurements before acupuncture. After bilateral acupuncture, there was an additional improvement and statistical significance in all parameters in both DFS and PAD patients.
Discussion: These results show an improvement in the microcirculation and peripheral blood flow at the edges of the wound. As impaired micro- and macrocirculation is considered to be a critical prognostic factor for the healing of a peripheral lesion, the intervention could have a positive impact on the healing of (chronic) peripheral wounds.
1 Introduction
Diabetes mellitus (DM) and peripheral artery disease (PAD) have an increasing incidence and a high prevalence worldwide. While around half a billion people currently suffer from diabetes, this figure is estimated to rise to more than three-quarters of a billion by 2045 (1). The situation is similar for PAD, the prevalence grew between 2000 and 2010 by 24% (2). In the meantime, far more than 200 million individuals are affected worldwide. The prevalence increases continuously with age. In high-income countries, it is estimated to be under 4% for men and women aged 40 to 44 years and over 20% for those over 80 years. The PAD prevalence is expected to continue to rise (3–5).
DM and PAD are both associated with high morbidity. Chronic non-healing peripheral ulcers, eventually combined with wound infections, are common in both patients with DM and patients with PAD. Diabetic foot syndrome (DFS) is one of the most clinically significant complications in patients with DM. Impaired blood flow and peripheral neuropathy increase the risk for foot ulcers and infections (6). People with diabetes mellitus have an estimated lifetime incidence of foot ulcers of up to 34% with frequent recurrences (7).
This is associated with a high economic burden. In the US, the treatment of diabetic foot syndrome is as expensive as that of carcinomas, with a comparable 5-year mortality rate (8). Recently, a large-scale study in Southeast Asia showed that coordinated care of patients with DFS from primary to tertiary care effectively reduces amputation rates (9). The data support the demand for a multi-disciplinary and interprofessional team approach in the management of DFS and lower extremity amputation prevention, as recommended by both the National Institute for Health and Care Excellence (NICE) and International Working Group on Diabetic Foot (IWGDF) guidelines (10, 11).
A common basic principle for the healing of a peripheral lesion is the restoration of impaired macro- and microcirculation, as this is considered to be a critical prognostic factor for wound healing (12–14). However, despite successful restoration of the macrocirculation, chronic wounds fail to heal in many cases. In a systematic review, wound healing was not achieved in 40% within 1 year in patients with DFS and PAD treated by endovascular or surgical therapy, and the major amputation rate was up to 10% (15). In addition, new treatment strategies are urgently needed for extremities at risk of amputation which cannot be revascularized for various reasons (16). In recent years, the crucial importance of microcirculation for limb preservation in both DFS and PAD has been emphasized. There is clear evidence that the microvascular function is altered first in the presence of risk factors associated with atherosclerosis (17). Even at the stage of intermittent claudication, microcirculation plays an important pathophysiological role (18). Patients with either diabetes or PAD demonstrate deteriorated cutaneous oxygen saturation at the plantar foot (19). Impaired microcirculation increases the risk of amputation in individuals with PAD by more than 20 times compared to those who neither have PAD nor microvascular disease (20). Therefore, interventions to improve cutaneous tissue oxygenation may be considered valuable therapy approaches to avoid complications and to promote the healing of chronic, non-healing peripheral ulcers.
One approach that might meet these criteria is acupuncture. It is a therapy from Traditional Chinese Medicine (TCM) and can be understood as reflex zone therapy, where certain areas of the body are stimulated with acupuncture needles (21, 22). Although the mechanisms of action of acupuncture have not yet been fully scientifically clarified, there are numerous publications that prove the effectiveness and efficacy of acupuncture (23–28). According to current studies, acupuncture can be used to increase peripheral microcirculation and skin blood perfusion (29–33). This effect may be useful in the therapy of DM and PAD patients with chronic ulcers. The aim of the study therefore was to investigate potential effects of acupuncture on microcirculation close to the wound margin in patients with DM or PAD.
2 Methods
2.1 Study design
We conducted a prospective, non-controlled pilot study to assess changes in microcirculation before and after intervention in patients with DM and PAD following unilateral or ipsilateral acupuncture.
The study was reviewed and approved by the Medical Ethics Committee II of the Mannheim Medical Faculty under the numbers 2013–546 N-MA and 2013–547 N-MA for the study in patients with PAD and DFS, respectively.
2.2 Study population
Inpatients from the Department of Angiology and Diabetes-related Diseases at the Diakonissenkrankenhaus Mannheim, Germany, were selected according to the following inclusion and exclusion criteria.
2.2.1 Inclusion criteria
Patients with peripheral lesions of the lower limbs and diagnosed PAD Fontaine stages III-IV (34, 35) or DFS, Wagner-Armstrong classification stages 1–4 A-D (36) were included in the study. All study participants provided written informed consent in German language.
2.2.2 Exclusion criteria
Exclusion criteria were angiological intervention (e.g., percutaneous transluminal angioplasty or bypass surgery) within the previous 2 months, acute ischemia, vasoactive therapy within the previous 48 h, body temperature > 37.8°C or systemic signs of infection. Other exclusion criteria were skin disease in the area of the acupuncture point, oral anticoagulation therapy and women of childbearing age.
2.3 Intervention
The intervention is reported according to the STRICTA guidelines (37). Acupuncture was provided by two physicians with an additional specialization in acupuncture from the Medical Chamber Baden-Württemberg, Germany, or an equivalent of at least 200 teaching hours. Each acupuncturist had more than 10 years’ experience in acupuncture and TCM. The acupuncture treatment consisted of a single acupuncture session of approximately 5 minutes’ duration. The acupuncture was performed on the connecting line between the acupuncture points Stomach 14 (ST 14, 库房, kù fáng) and Stomach 15 (ST 15, 屋 翳, wū yì) (22). These points are located at the front of the chest in the first and second intercostal space respectively, on the mamillary line. The selected points were chosen based on principles of Chinese medical theory and supported by available evidence, as follows: (i) According to Chinese medical theory, points are selected based on their location along the same meridian (38). Acupuncture points on the Stomach meridian were chosen to target the back of the foot, where many chronic wounds in PAD and DFS are located. The Stomach meridian starts at the lateral side of the nose, runs through the chest and abdomen, extends to the front of the upper and lower leg, and ends at the back of the foot on the second toe (22). (ii) Additionally, a fundamental principle of acupuncture emphasizes the combination of local and distal points. Due to a relative contraindication for needling close to open wounds, only distal points were chosen for needling (22). (iii) The decision to use the region between these two points on the chest was further supported by clinical experience and observations within the author group, as understood in terms of internal evidence. Acupuncture was applied either unilaterally (ipsilateral to the wound side) or bilaterally (first ipsi- then contralateral) to the other half of the participants. A so-called sparrow-picking or blood-letting technique was used with standardized needles (Becton Dickinson B-D Micro Fine ™ + Demi insulin syringes 0.3 × 5 mm, 31 G) (32, 39, 40). The needles were inserted to their full length of 5 mm, no needle retention was used in this technique. No specific response (e.g., de qi) was sought. No other interventions (e.g., moxibustion, cupping, lifestyle advice) were given to the participants.
2.4 Micro-lightguide spectrophotometer (O2C)
Microcirculation was assessed using an Micro-lightguide Spectrophotometer (O2C device), which combines a laser Doppler shift and white light spectroscopy system (LEA Medizintechnik GmbH, Giessen, Germany) (41). A flat probe placed horizontally on the tissue collects data simultaneously from the tissue as a multi-channel system. Data collection was performed on the intact skin at the distance of 1 cm from the wound edge of the damaged tissue and covered a time interval from 3 min before acupuncture (= baseline measurement) until 10 min after acupuncture. Due to potential movement artifacts, data recorded 30 s each before and after the acupuncture treatment were excluded from data analysis. Microcirculation was assessed using the following microperfusion parameters: oxygen saturation of hemoglobin (SO2), relative amount of hemoglobin (rHb), relative blood flow (Flow) and blood flow velocity (Velo). SO2 was expressed as a percentage, rHb, Flow and Velo in arbitrary units (AU). These four parameters were measured at 3 mm (S) and 8 mm (D) depth, resulting in a total of 8 parameters (e.g., Velo S (superficial 3 mm) and Velo D (deep 8 mm)). In cases of diabetic microangiopathy, the O2C device has been shown to provide reliable data and valid non-invasive measurements of tissue oxygenation and microvascular blood flow (42, 43).
2.5 Statistical analysis
Linear mixed models were used to assess the influence of acupuncture on the eight microcirculatory parameters. These models included each measured parameter as a dependent variable, acupuncture (baseline/unilateral acupuncture/ bilateral acupuncture) and disease (PAD/DFS) as fixed factors, and patient as a random factor. The inclusion of patient as a random factor ensures that the clustered data structure is considered in the statistical model (measurements clustered within patients). An additional linear mixed model explored the difference in the effects of acupuncture between PAD and DFS patients by including an interaction term between acupuncture and disease. Restricted maximum likelihood was used to fit all models. Effect estimates were calculated along with p-values and 95% confidence intervals of the profile likelihood type. Due to the exploratory nature of the study, no adjustment for multiple testing was made. P-values less than 0.05 were considered statistically significant. R version 3.4.21 with the packages ‘lme4’ and ‘lmerTest’ was used for statistical analysis.
3 Results
3.1 Patient characteristics: sociodemographic and clinical characteristics
A total of n = 18 patients were included in the pilot study, thereof n = 9 with DFS and n = 9 with PAD. Two thirds of the participants were male (n = 12) and one third female (n = 6). Age of the participants ranged from 55 to 92 years, with a mean of 77 years (SD 9.5). Additional clinical characteristics of the study population are shown in Table 1.
3.2 Unilateral and bilateral acupuncture in pre-post comparison in patients with DFS and PAD
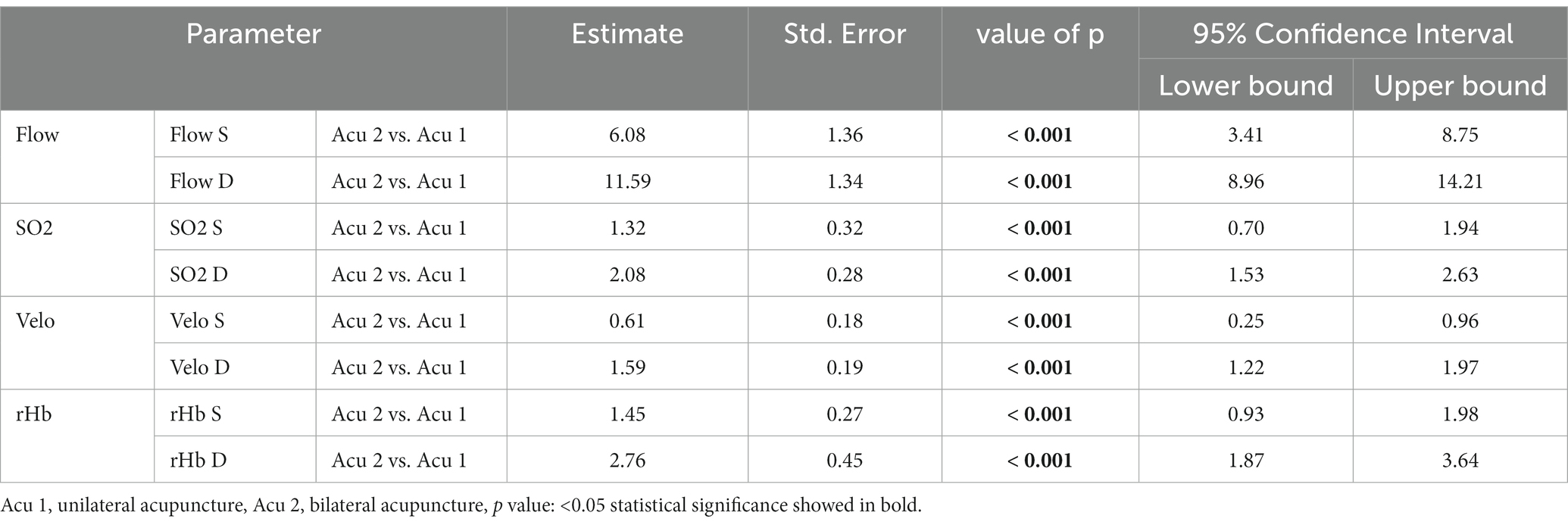
After unilateral acupuncture (ipsilateral to the wound side), a statistically significant improvement in seven out of eight microcirculatory parameters (superficial and deep Flow, Velo and rHb as well as in deep S02) could be demonstrated in both patients with PAD and DFS with chronic non-healing peripheral ulcers compared to baseline measurements before acupuncture. With unilateral acupuncture alone, superficial SO2 measurements did not show a statistically significant improvement. However, bilateral acupuncture (first ipsi-, then contralateral) led to statistically significant improvements in all eight microcirculatory parameters s compared to baseline measurements. When comparing unilateral versus bilateral acupuncture in patients with both DFS and PAD, an additional improvement in all parameters was observed after bilateral acupuncture. Further details are shown in Tables 2, 3.
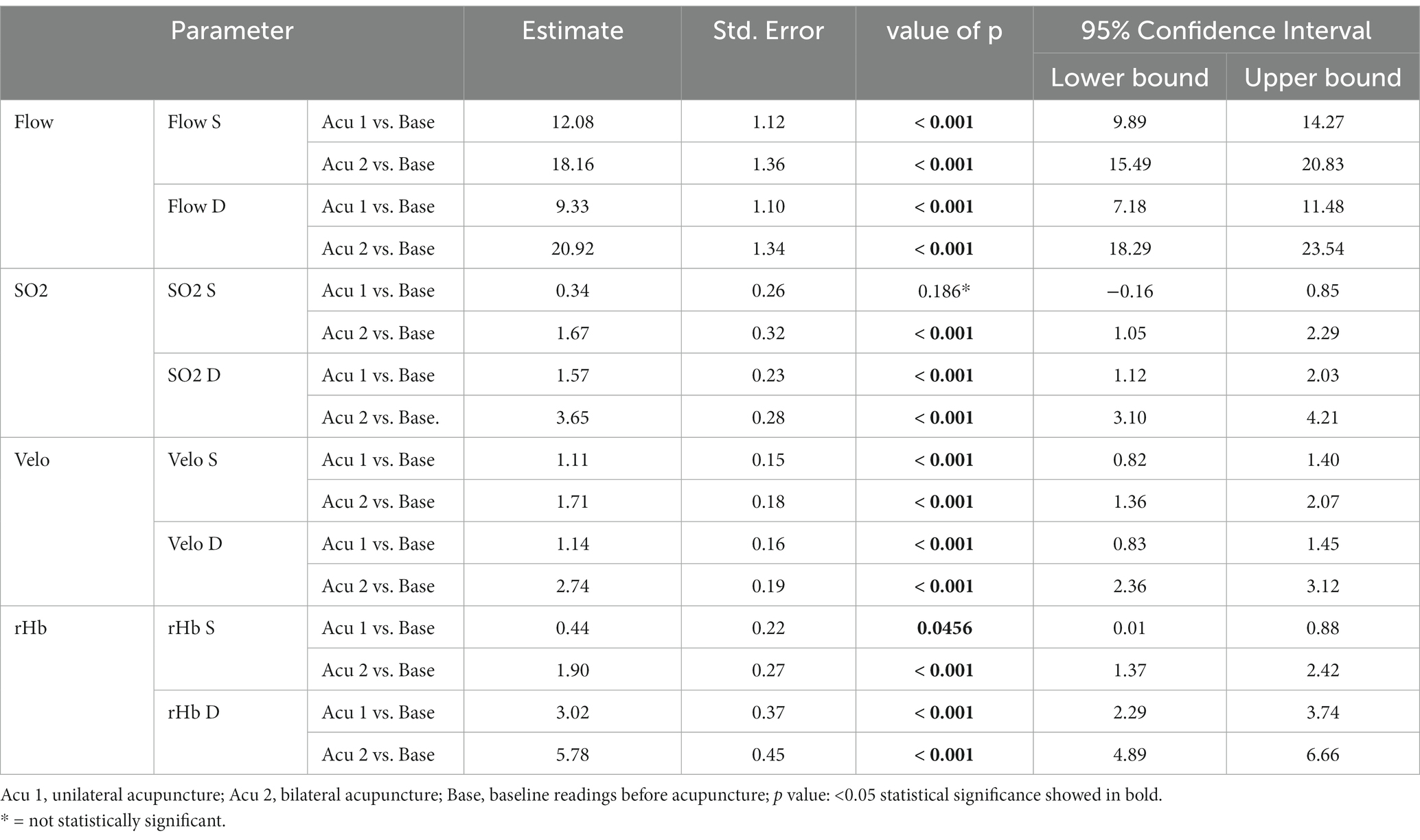
Table 2. Difference between baseline measurements (Base), unilateral acupuncture (Acu 1) and bilateral acupuncture (Acu 2).
3.3 Acupuncture in patients with DFS versus PAD
Table 4 shows the different results of the acupuncture intervention in patients with PAD compared to patients with DFS for unilateral and bilateral acupuncture compared to baseline measurements before acupuncture. For all superficial measurements (3 mm depth), better results could be shown for single and bilateral acupuncture in patients with DFS compared to patients with PAD (values marked with ∞ in Table 4). For the deep measurements (8 mm depth), an inverse trend could be found. After unilateral acupuncture, SO2 and Velo measurements were better in patients with DFS compared to PAD. On the contrary, Flow and rHb measurements were better in PAD compared to DFS (values marked with ∆ in Table 4). Measurements of blood flow showed the most distinct differences between patients with DFS and PAD. In addition, with bilateral acupuncture, all deep measurements showed better results in PAD than in DFS. Although there were some trends, not every difference shown between patients with DFS and PAD reached statistical significance. Figure 1 shows the mean values for the differences in treatment effect along with 95% confidence intervals in the acupuncture intervention between patients with PAD and DFS in unilateral acupuncture and bilateral acupuncture when compared to baseline measurements before acupuncture.
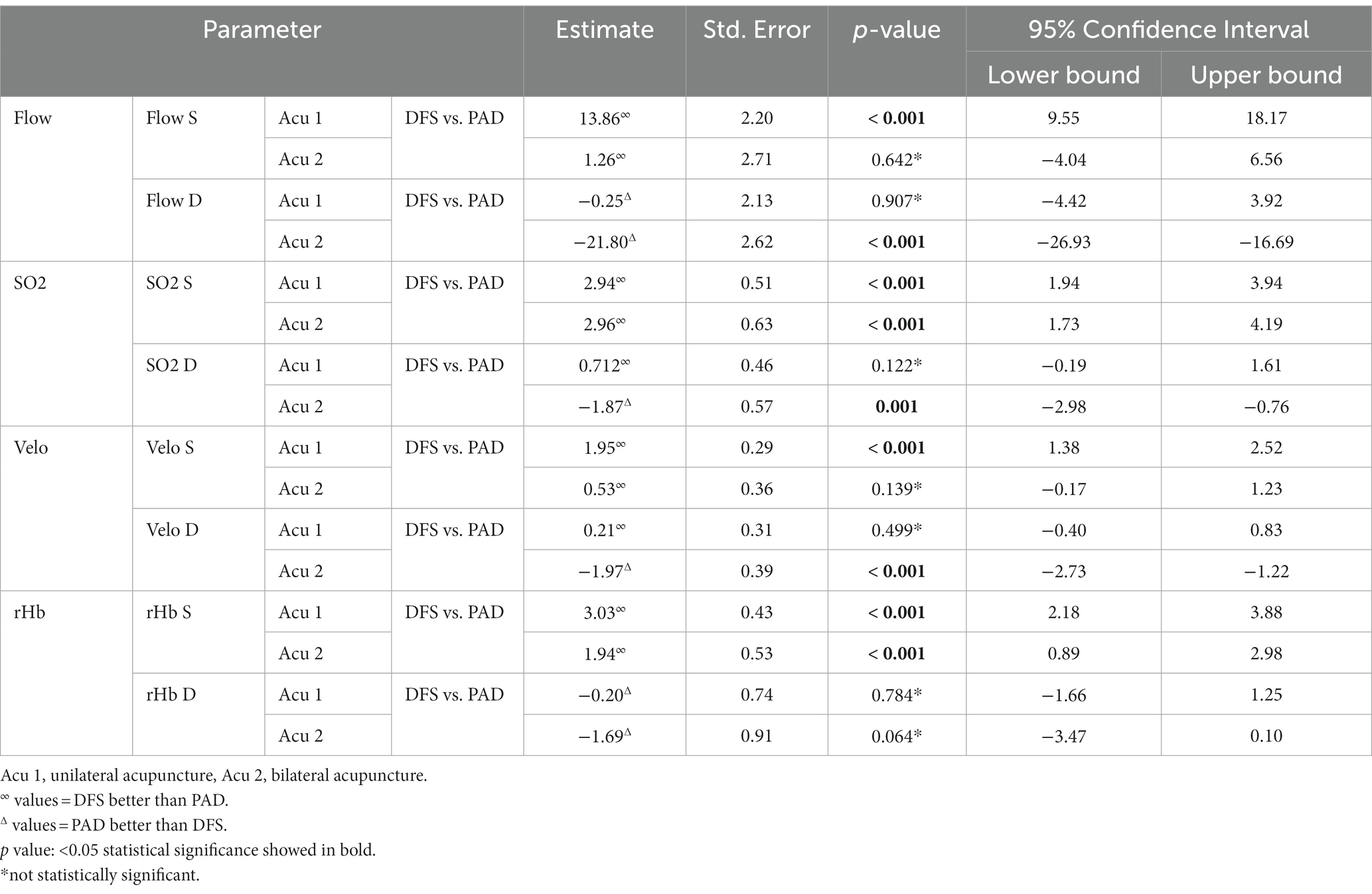
Table 4. Difference in acupuncture intervention for patients with DFS versus PAD in unilateral acupuncture (Acu 1) and bilateral acupuncture (Acu 2) when compared to baseline measurements before acupuncture.
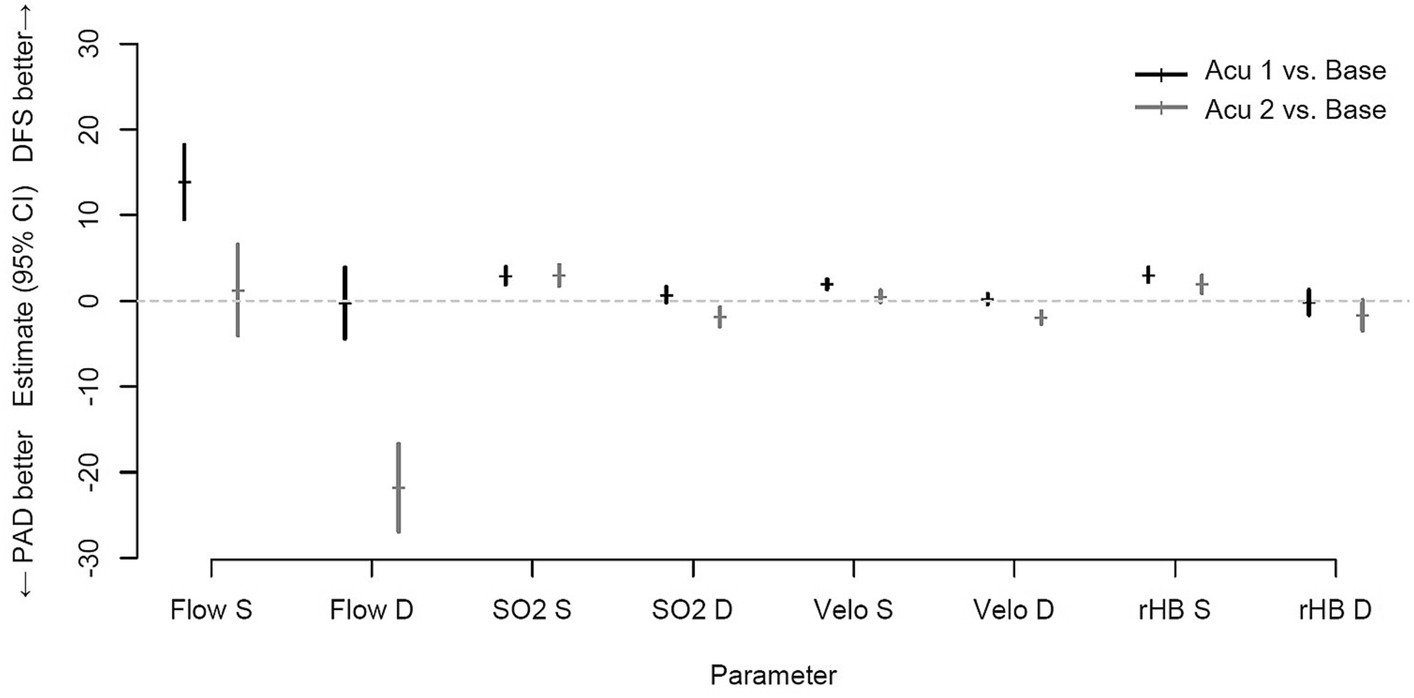
Figure 1. Mean outcome differences with 95% confidence intervals in acupuncture intervention between patients with PAD and DFS in unilateral acupuncture (Acu 1) and bilateral acupuncture (Acu 2).
4 Discussion
After unilateral acupuncture (ipsilateral to the wound side), a statistically significant improvement in seven out of eight microcirculatory parameters (SO2, rHb, Flow and Velo) was demonstrated at 3 mm and 8 mm depths compared to baseline measurements before acupuncture. These results correspond to an increase in microcirculation around the wound margin. Impaired micro- and macrocirculation is considered a critical prognostic factor for the healing of a peripheral lesion (12–14). Beside arterial revascularization as main therapeutic option, there is limited evidence for non-revascularization interventions including, e.g., Prostanoids (16). Although recommended to accelerate ulcer healing, pain reduction and amputation prevention in PAD (44, 45), Alprostadil (prostaglandin E1) failed to show superiority over placebo in a placebo-controlled randomized multicenter trial (46). Therefore, the results of this study must be interpreted with great caution when considering their clinical implications in wound healing. Nevertheless, acupuncture may have a positive influence on wound healing in (chronic) peripheral wounds. As numerous studies have explored acupuncture’s impact on microcirculation, including capillary blood flow, indicating potential improvements under specific conditions (47–49). However, the precise mechanisms underlying acupuncture’s effects on microcirculation remain under investigation. Some research proposes various mechanisms, including the release of neurotransmitters (e.g., nitric oxide), activation of mast cells and regulation of the autonomic nervous system among others (50–55). When comparing the results of the acupuncture intervention between patients with DFS and PAD, better results could be shown for superficial measurements in patients with DFS. However, for deep measurements, a more pronounced improvement was seen in patients with PAD compared to DFS. Although these differences are only a trend, as they did not reach statistical significance for every microcirculatory parameter measured, the reason for these differences is not clear. Our findings in patients with DFS are consistent with those recently published by Sang et al., who showed that diabetic patients with arteriosclerotic wounds of the lower extremity had a significant reduction in lesion size after 8 weeks of treatment with electroacupuncture (56). An exact explanation of the precise acupuncture mechanisms of our observed effects can only be hypothesized. We would suggest that the observed results could be mainly due to regulatory effects of the autonomic nervous system, which is known to regulate, e.g., perfusion and vasodilation (57). On the other hand we would rather rule out that the effects are mainly due to effects on segmental innervation, as the needle insertion point was in the at the cervicothoracic region, whereas the observed effects on microcirculation were in the lumbar or pelvic innervation region. Further studies should address these issues.
4.1 Strengths and limitations
Owing to the exploratory design of this pilot study, there are several limitations that need to be considered when interpreting the results. Due to the small sample size, this study did not include a control group (e.g., sham acupuncture or a control group). This also led to a lack of randomization and blinding of patients. However, as the data recorded before the acupuncture intervention were considered as the baseline measurement, a comparison of the microcirculatory parameters before and after the acupuncture intervention could be implemented in the data analysis. As there was no follow-up in this study, only an immediate acupuncture effect could be demonstrated. As the study used a specific needling technique, it’s important to note that the results may not necessarily be applicable to other types of needling or the use of different stimulation methods. Therefore, it is not possible to say how long the effects of acupuncture may last. Whether the measured statistically significant improvement in microcirculatory parameters leads to a clinically significant improvement, resulting in faster healing of chronic peripheral wounds, remains uncertain. Further studies should include a larger sample size, a control group, different needling techniques and ideally, assessments of clinical parameters of wound healing (e.g., wound size with length and width) over a longer period of time, due to the chronicity of lower limb ulcers.
The strength of this study is the investigation of a pragmatic acupuncture approach with a comparatively feasible acupuncture intervention for a worldwide relevant problem of non-healing chronic peripheral wounds in patients with DFS or PAD. As no prior diagnosis according to TCM criteria is required before the acupuncture intervention, it may be a quick and effective method that could potentially be easily implemented and performed during routine medical consultations for both inpatients and outpatients. As no adverse events were reported during the trial, this acupuncture intervention can be considered safe, despite the small sample size. Based on the extensive data available, the overall risk of complications from acupuncture is considered to be very low. No adverse events (e.g., pneumothorax) have been reported in the literature for the acupuncture points used, Stomach 14 and Stomach 15 (58, 59).
These results show an improvement in the microcirculation and peripheral blood flow at the edges of the wound. As impaired micro- and macrocirculation is considered to be the most important prognostic factor for the healing of a peripheral lesion, the intervention may have a positive impact on the healing of (chronic) peripheral wounds.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the author on reasonable request in anonymised form in accordance with the institutional regulations and the General Data Protection Regulation.
Ethics statement
The studies involving humans were approved by Medical Faculty Mannheim, Medical Ethics Commission II (Nr. 2013-546N-MA and 2013-547N-MA). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JV: Conceptualization, Data curation, Investigation, Writing – original draft. MS: Investigation, Writing – review & editing. CD: Investigation, Writing – review & editing. JK: Data curation, Formal analysis, Methodology, Validation, Visualization, Writing – review & editing. KA: Conceptualization, Resources, Supervision, Validation, Writing – review & editing. HG: Conceptualization, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or authorship of this article. They recieved support for the publication from the Open Access Publishing Fund of the University of Tübingen.
Acknowledgments
During the preparation of this work the authors used DeepL and ChatGPT to improve language editing. After using these tools, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1. Sun, H, Saeedi, P, Karuranga, S, Pinkepank, M, Ogurtsova, K, Duncan, BB, et al. IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. (2022) 183:109119. doi: 10.1016/j.diabres.2021.109119
2. Fowkes, FGR, Rudan, D, Rudan, I, Aboyans, V, Denenberg, JO, McDermott, MM, et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet. (2013) 382:1329–40. doi: 10.1016/S0140-6736(13)61249-0
3. Song, P, Rudan, D, Zhu, Y, Fowkes, FJI, Rahimi, K, Fowkes, FGR, et al. Global, regional, and national prevalence and risk factors for peripheral artery disease in 2015: an updated systematic review and analysis. Lancet Glob Health. (2019) 7:e1020–30. doi: 10.1016/S2214-109X(19)30255-4
4. Criqui, MH, and Aboyans, V. Epidemiology of peripheral artery disease. Circ Res. (2015) 116:1509–26. doi: 10.1161/CIRCRESAHA.116.303849
5. Nehler, MR, Duval, S, Diao, L, Annex, BH, Hiatt, WR, Rogers, K, et al. Epidemiology of peripheral arterial disease and critical limb ischemia in an insured national population. J Vasc Surg. (2014) 60:686–695.e2. doi: 10.1016/j.jvs.2014.03.290
6. van Netten, JJ, Bus, SA, Apelqvist, J, Lipsky, BA, Hinchliffe, RJ, Game, F, et al. Definitions and criteria for diabetic foot disease. Diabetes Metab Res Rev. (2020) 36:e3268. doi: 10.1002/dmrr.3268
7. Armstrong, DG, Boulton, AJM, and Bus, SA. Diabetic foot ulcers and their recurrence. N Engl J Med. (2017) 376:2367–75. doi: 10.1056/NEJMra1615439
8. Armstrong, DG, Swerdlow, MA, Armstrong, AA, Conte, MS, Padula, WV, and Bus, SA. Five year mortality and direct costs of care for people with diabetic foot complications are comparable to cancer. J Foot Ankle Res. (2020) 13:16. doi: 10.1186/s13047-020-00383-2
9. Lo, ZJ, Tan, E, Chandrasekar, S, Ooi, D, Liew, H, Ang, G, et al. Diabetic foot in primary and tertiary (DEFINITE) care: a health services innovation in coordination of diabetic foot ulcer (DFU) care within a healthcare cluster −18-month results from an observational population health cohort study. Int Wound J. (2023) 20:1609–21. doi: 10.1111/iwj.14016
10. IWGDF. (2019). Guidelines on the prevention and management of diabetic foot disease. Available at: (https://iwgdfguidelines.org/guidelines-2019/)
11. National institute for health and care excellence clinical guideline (CG147). (2020). Peripheral arterial disease: diagnosis and management. Available at: (https://www.nice.org.uk/Guidance/CG147)
13. WHO. (2010). Diabetes mellitus: fact sheet N°31. Available at:http://www.who.int/mediacentre/factsheets/fs312/en/.
14. Leitlinie, NV. Typ-2-Diabetes - Präventions- und Behandlungsstrategien für Fußkomplikationen In: BK Bundesärztekammer and F AdWM, editors. Nationale Versorgungs Leitlinie. Berlin: Springer (2010)
15. Forsythe, RO, Apelqvist, J, Boyko, EJ, Fitridge, R, Hong, JP, Katsanos, K, et al. Effectiveness of revascularisation of the ulcerated foot in patients with diabetes and peripheral artery disease: a systematic review. Diabetes Metab Res Rev. (2020) 36:e3279. doi: 10.1002/dmrr.3279
16. Ruemenapf, G, Morbach, S, and Sigl, M. Therapeutic alternatives in diabetic foot patients without an option for revascularization: a narrative review. J Clin Med. (2022) 11:2155. doi: 10.3390/jcm11082155
17. Marcoccia, A, Klein-Weigel, PF, Gschwandtner, ME, Wautrecht, JC, Matuska, J, Rother, U, et al. Microcirculatory assessment of vascular diseases. Vasa. (2020) 49:175–86. doi: 10.1024/0301-1526/a000851
18. Hamburg, NM, and Creager, MA. Pathophysiology of intermittent claudication in peripheral artery disease. Circ J. (2017) 81:281–9. doi: 10.1253/circj.CJ-16-1286
19. Kabbani, M, Rotter, R, Busche, M, Wuerfel, W, Jokuszies, A, Knobloch, K, et al. Impact of diabetes and peripheral arterial occlusive disease on the functional microcirculation at the plantar foot. Plast Reconstr Surg Glob Open. (2013) 1:e48. doi: 10.1097/GOX.0b013e3182a4b9cb
20. Beckman, JA, Duncan, MS, Damrauer, SM, Wells, QS, Barnett, JV, Wasserman, DH, et al. Microvascular disease, peripheral artery disease, and amputation. Circulation. (2019) 140:449–58. doi: 10.1161/CIRCULATIONAHA.119.040672
21. Greten, HJ. Kursbuch Traditionelle Chinesische Medizin. 3rd ed. Stuttgart/New York: Thieme (2017).
22. Deadman, P, Al-Khafaji, M, and Baker, K. A manual of acupuncture. Seattle: Eastland Press (2001).
23. Zhao, L, Chen, J, Li, Y, Sun, X, Chang, X, Zheng, H, et al. The long-term effect of acupuncture for migraine prophylaxis: a randomized clinical trial. JAMA Intern Med. (2017) 177:508–15. doi: 10.1001/jamainternmed.2016.9378
24. Vickers, AJ, Vertosick, EA, Lewith, G, Mac Pherson, H, Foster, NE, Sherman, KJ, et al. Acupuncture for chronic pain: update of an individual patient data meta-analysis. J Pain. (2017) 19:455–74. doi: 10.1016/j.jpain.2017.11.005
25. Brinkhaus, B, Ortiz, M, Witt, CM, Roll, S, Linde, K, Pfab, F, et al. Acupuncture in patients with seasonal allergic rhinitis: a randomized trial. Ann Intern Med. (2013) 158:225–34. doi: 10.7326/0003-4819-158-4-201302190-00002
27. WHO. WHO - acupuncture: Review and analysis of reports on controlled clinical trials. Geneva: World Health Organization (2002).
28. Cheong, KB, Zhang, JP, Huang, Y, and Zhang, ZJ. The effectiveness of acupuncture in prevention and treatment of postoperative nausea and vomiting--a systematic review and meta-analysis. PLoS One. (2013) 8:e82474. doi: 10.1371/journal.pone.0082474
29. Litscher, G. Bioengineering assessment of acupuncture, part 2: monitoring of microcirculation. Crit Rev Biomed Eng. (2006) 34:273–94. doi: 10.1615/CritRevBiomedEng.v34.i4.10
30. Litscher, G, Wang, L, Huber, E, and Nilsson, G. Changed skin blood perfusion in the fingertip following acupuncture needle introduction as evaluated by laser Doppler perfusion imaging. Lasers Med Sci. (2002) 17:19–25. doi: 10.1007/s10103-002-8262-9
31. Wang, L, Huang, T, Zhang, W, and Litscher, G. Violet laser acupuncture--part 2: effects on peripheral microcirculation. J Acupunct Meridian Stud. (2011) 4:24–8. doi: 10.1016/S2005-2901(11)60004-6
32. Doenitz, CA, Anjos, A, Efferth, T, Greten, T, and Greten, HJ. Can heat and cold be parameterized? Clinical data of a preliminary study. Zhong Xi Yi Jie He Xue Bao. (2012) 10:532–7. doi: 10.3736/jcim20120508
33. Min, S, Lee, H, Kim, SY, Park, JY, Chae, Y, Lee, H, et al. Local changes in microcirculation and the analgesic effects of acupuncture: a laser Doppler perfusion imaging study. J Altern Complement Med. (2015) 21:46–52. doi: 10.1089/acm.2013.0442
34. Fontaine, R, Kim, M, and Kieny, R. Surgical treatment of peripheral circulation disorders. Helv Chir Acta. (1954) 21:499–533.
35. Norgren, L, Hiatt, WR, Dormandy, JA, Nehler, MR, Harris, KA, Fowkes, FG, et al. Inter-society consensus for the management of peripheral arterial disease. J Vasc Surg. (2007) 26:81–157. doi: 10.1016/j.jvs.2006.12.037
36. Wagner, FW Jr. The dysvascular foot: a system for diagnosis and treatment. Foot Ankle. (1981) 2:64–122. doi: 10.1177/107110078100200202
37. Mac Pherson, H, Altman, DG, Hammerschlag, R, Li, Y, Wu, T, White, A, et al. Revised standards for reporting interventions in clinical trials of acupuncture (STRICTA): extending the CONSORT statement. Acupuncture in medicine: journal of the British medical acupuncture. Society. (2010) 28:83–93. doi: 10.1136/aim.2009.001370
38. Yang, C, and He, S. Acupuncture therapeutic. Shanghai: Shanghai Scientific & Technical Publishers (1994).
40. Zhao, JP, Piao, YZ, and Wang, J. Effect of acupuncture combined with blood-letting by a three-edged needle on 50 cases of Bell's palsy at the acute stage. J Tradit Chin Med. (2010) 30:118–21. doi: 10.1016/S0254-6272(10)60026-X
41. Medizintechnik, L. Lea Medizintechnik GmbH. Hessen: Gesellschaft mit beschränkter Haftung (2018).
42. Beckert, S, Witte, MB, Konigsrainer, A, and Coerper, S. The impact of the micro-lightguide O2C for the quantification of tissue ischemia in diabetic foot ulcers. Diabetes Care. (2004) 27:2863–7. doi: 10.2337/diacare.27.12.2863
43. Forst, T, Hohberg, C, Tarakci, E, Forst, S, Kann, P, and Pfutzner, A. Reliability of lightguide spectrophotometry (O2C) for the investigation of skin tissue microvascular blood flow and tissue oxygen supply in diabetic and nondiabetic subjects. J Diabetes Sci Technol. (2008) 2:1151–6. doi: 10.1177/193229680800200625
44. Hirsch, AT, Haskal, ZJ, Hertzer, NR, Bakal, CW, Creager, MA, Halperin, JL, et al. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic). J Am Coll Cardiol. (2006) 47:1239–312. doi: 10.1016/j.jacc.2005.10.009
45. Norgren, L, Hiatt, WR, Dormandy, JA, Nehler, MR, Harris, KA, and Fowkes, FGR. Inter-society consensus for the Management of Peripheral Arterial Disease (TASC II). Eur J Vasc Endovasc Surg. (2007) 33:S1–S75. doi: 10.1016/j.ejvs.2006.09.024
46. Lawall, H, Pokrovsky, A, Checinski, P, Ratushnyuk, A, Hamm, G, Randerath, O, et al. Efficacy and safety of Alprostadil in patients with peripheral arterial occlusive disease Fontaine stage IV: results of a placebo controlled randomised multicentre trial (ESPECIAL). Eur J Vasc Endovasc Surg. (2017) 53:559–66. doi: 10.1016/j.ejvs.2016.12.035
47. Wang, H, Wang, L, Shi, X, Qi, S, Hu, S, Tong, Z, et al. Electroacupuncture at Zusanli prevents severe scalds-induced gut ischemia and paralysis by activating the cholinergic pathway. Evid Based Complement Alternat Med. (2015) 2015:787393:1–6. doi: 10.1155/2015/787393
48. Huang, T, Yang, LJ, Zhang, WB, Jia, SY, Tian, YY, Wang, GJ, et al. Observation of microvascular perfusion in the Hegu (LI4) Acupoint area after Deqi acupuncture at Quchi (LI11) Acupoint using speckle laser blood flow scanning technology. Evid Based Complement Alternat Med. (2012) 2012:604590:1–4. doi: 10.1155/2012/604590
49. Silbereisen, C. Effekte der Akupunktur auf die metabolisch induzierte Vasodilatation bei chronischen Rauchern-Untersuchung mittels Venenverschlussplethysmographie. Munich: Medizinische Fakultät (2005).
51. Kimura, K, Takeuchi, H, Yuri, K, and Wakayama, I. Effects of nitric oxide synthase inhibition on cutaneous vasodilation in response to acupuncture stimulation in humans. Acupunct Med. (2013) 31:74–80. doi: 10.1136/acupmed-2012-010177
52. Hsiao, SH, and Tsai, LJ. A neurovascular transmission model for acupuncture-induced nitric oxide. J Acupunct Meridian Stud. (2008) 1:42–50. doi: 10.1016/S2005-2901(09)60006-6
53. Wang, G, Litscher, D, Tian, Y, Gaischek, I, Jia, S, Wang, L, et al. Acupoint activation: response in microcirculation and the role of mast cells. Medicines. (2014) 1:56–63. doi: 10.3390/medicines1010056
54. Zhang, Z-J, Wang, X-M, and McAlonan, GM. Neural acupuncture unit: a new concept for interpreting effects and mechanisms of acupuncture. Evid Based Complement Alternat Med. (2012) 2012:429412. doi: 10.1155/2012/429412
55. Li, QQ, Shi, GX, Xu, Q, Wang, J, Liu, CZ, and Wang, LP. Acupuncture effect and central autonomic regulation. Evid Based Complement Alternat Med. (2013) 2013:267959. doi: 10.1155/2013/267959
56. Sang, P, Zhao, J, and Yang, H. The efficacy of electroacupuncture in among early diabetic patients with lower limb arteriosclerotic wounds. Int Wound J. (2023). doi: 10.1111/iwj.14526
57. Widmaier, E, Raff, H, and Strang, KT. Vander's human physiology. New York: McGraw-Hill Education (2022).
58. Wu, J, Hu, Y, Zhu, Y, Yin, P, Litscher, G, and Xu, S. Systematic review of adverse effects: a further step towards modernization of acupuncture in China. Evid Based Complement Alternat Med. (2015) 2015:432467:1–19. doi: 10.1155/2015/432467
Keywords: peripheral artery disease (PAD), diabetes mellitus, acupuncture, chronic wounds, microcirculation, diabetic foot syndrome (DFS)
Citation: Valentini J, Sigl M, Dunckel C, Krisam J, Amendt K and Greten HJ (2024) Can acupuncture increase microcirculation in peripheral artery disease and diabetic foot syndrome? – a pilot study. Front. Med. 11:1371056. doi: 10.3389/fmed.2024.1371056
Edited by:
Christian S. Kessler, Immanuel Hospital Berlin, GermanyReviewed by:
Joanna Dietzel, Charité University Medicine Berlin, GermanyThomas Rampp, Kliniken Essen-Mitte, Germany
Copyright © 2024 Valentini, Sigl, Dunckel, Krisam, Amendt and Greten. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jan Valentini, amFuLnZhbGVudGluaUBtZWQudW5pLXR1ZWJpbmdlbi5kZQ==
 Jan Valentini
Jan Valentini Martin Sigl
Martin Sigl Cornelia Dunckel3
Cornelia Dunckel3 Johannes Krisam
Johannes Krisam Henry Johannes Greten
Henry Johannes Greten