- 1UCD Perinatal Research Centre, University College Dublin, The National Maternity Hospital, Dublin, Ireland
- 2Department of Obstetrics & Gynecology, Royal College of Surgeons in Ireland, Rotunda Hospital, Dublin, Ireland
- 3School of Computer Science, University College Dublin, Dublin, Ireland
Objective: To investigate the use of a virtual reality learning environment (VRLE) to enhance medical student knowledge of postpartum hemorrhage (PPH) emergency management and insertion of a postpartum balloon.
Methods: A randomized control trial involving medical students from University College Dublin, Ireland. Participants were randomly allocated to the intervention group (VRLE tutorial) or control group (PowerPoint tutorial on the same topic). All participants completed pre-learning experience and post-learning experience surveys. Both groups were timed and assessed on postpartum balloon insertion technique on a model pelvis. The primary outcome was assessment of student knowledge. Secondary outcomes included confidence levels, time taken to complete the task, technique assessment, satisfaction with the learning environment, and side effects of VR.
Results: Both learning experiences significantly (p < 0.001) enhanced student performance on the post-learning experience multiple choice questionnaire, with no difference between the intervention and control groups. In the intervention group, time for task completion was significantly less compared to the control group (1–2 min vs. 2–3 min, p = 0.039). Both learning experiences significantly (p < 0.001) enhanced student confidence, with no significant difference between intervention and control groups. 100% of the students using the VRLE enjoyed the experience, and 82.4% were very likely to recommend use of VRLE in medical education. 94.1% of the students felt the VRLE was beneficial over didactic teaching.
Conclusion: Receiving formal instruction, regardless of format, enhances students’ knowledge and confidence of the topic covered. Students who received instruction via the VRLE assembled the postpartum balloon faster than students who received didactic teaching. VR may be beneficial in teaching hands-on procedural skills in obstetrics and gynecology education.
1 Introduction
Postpartum hemorrhage (PPH) remains a leading cause of maternal mortality and morbidity worldwide (1). Prompt recognition and initiation of emergency management and resuscitation is crucial to reduce morbidity (1). The most common cause of PPH is uterine atony (1), and where uterotonic medications fail, balloon tamponade is a simple, effective, and potentially life-saving measure (2). Therefore, PPH emergency management is a critical concept in undergraduate obstetrics and gynecology teaching in order to prepare our future physicians for clinical practice.
Unfortunately, due to the sensitive nature of many aspects of clinical obstetrics and gynecology, medical students often find it difficult to get hands-on clinical experience in the specialty (3). Additionally, the centre in which students attend their clinical placements may have varying birth rates, making PPH a potentially rare event for students to encounter during the course of their clinical placement (4). During emergency situations, medical students are often silent observers, reducing their exposure to critical aspects of PPH emergency management (3). Therefore, simulated clinical environments are increasingly part of the medical school curriculum, in order to foster development of essential skills in prompt resuscitation, emergency management and communication in advance of clinical practice (5). Simulated clinical environments offer an opportunity to gain knowledge and confidence in emergency management skills, with the ultimate goal of preparing participants for prompt recognition and management of PPH, in order to improve patient outcomes (4). Additionally, simulated clinical environments provide students with an opportunity to practice hands-on skills which may not be commonly encountered (3), such as insertion of a postpartum balloon for uterine tamponade. These simulated clinical environments offer students a safe place to make mistakes, without risking patient safety in the clinical environment (4).
As technology has advanced and educational technology has become more accessible, virtual reality (VR) is increasingly being used to improve the educational experience (6). VR technology creates an immersive environment in which the participant can explore and manipulate multimedia sensory environments in real-time (7). VR has the potential to enhance the simulated clinical environment by creating a real-life multisensory clinical learning environment. Learning through simulation and VR utilises the constructivist educational theory, whereby learners construct knowledge through their interaction with the learning environment, rather than passively taking in information (8). VR learning tools are often self-directed, and promote active engagement of the student to navigate their own learning experience, thus resulting in the student forming their own knowledge through a self-regulated process (9). Additionally, VR has the benefit of supporting knowledge acquisition for procedural skills, where the user can repeat procedural steps hands-on through the VR headset as many times as required for the individual learner to feel confident with the procedure (10), facilitating practice without the risk of patient harm (11).
Therefore, the objective of our study was to assess the value of using VR in simulating training for medical students in management of PPH and insertion of a postpartum balloon for uterine tamponade. The topic of PPH was chosen as it is an emergency situation, and a critical concept to understand at the undergraduate level. Additionally, we were able to consolidate generalizable resuscitation skills, and introduce the procedural component of a postpartum balloon for uterine tamponade, which students’ would rarely see during their clinical placements. We hypothesized that VR would enhance the student learning experience and improve the insertion technique of the postpartum balloon, compared with traditional didactic teaching methods.
2 Materials and methods
A randomized control trial (RCT) of students in the clinical years of the undergraduate (6-year program) and graduate entry (4-year program) medical degree programs at University College Dublin (UCD) was conducted over 5 days from October 15–19, 2023. Graduate entry medical students are those who have completed a primary degree, and are now undertaking medicine as a second degree. Ethical approval for this study was obtained from the University College Dublin Research Ethics Committee.
2.1 Participants
Similar to previous successful studies conducted at the UCD Perinatal Research Centre, medical students were invited to take part in the study via class announcements on the university’s e-learning platform (12, 13), and announcements made during clinical placement. The announcements gave a brief overview of the study, without giving specific details of the content to be covered. Interested students contacted the study team via email, and an information leaflet and consent form was sent to each student for review. All students in the clinical years of study at UCD were eligible for participation, except those younger than 18 years of age, or with a medical condition including cardiac (e.g., pacemakers), binocular vision abnormalities, psychiatric disorders or epilepsy. Informed written consent from all participants was obtained on arrival to the teaching space. Participants were advised they could withdraw consent to participate at any time.
2.2 Randomization
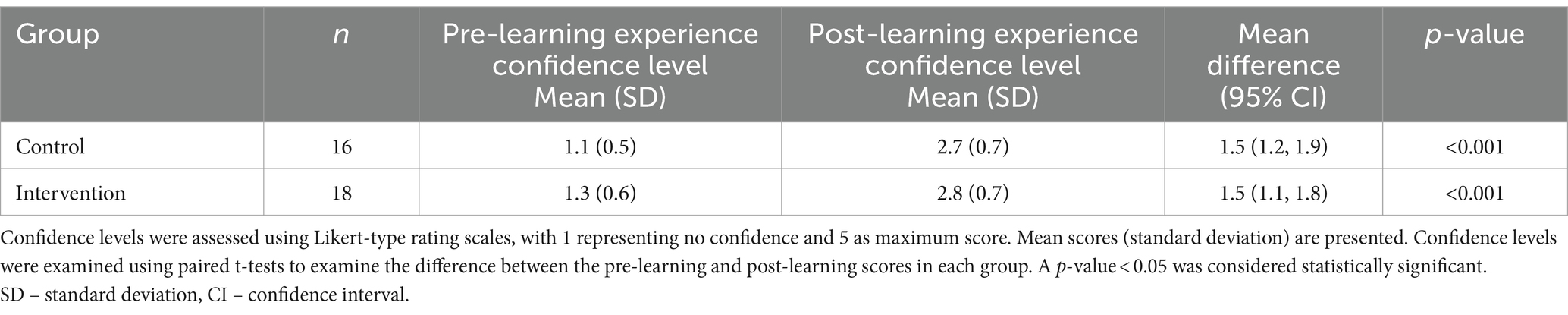
Figure 1 depicts the randomization and allocation process for the study. Participants were randomly allocated to intervention or control groups through the use of sequentially numbered, opaque, sealed envelopes. The researcher conducting the study was not blinded to the group allocation given the nature of the study design, however, allocation was prospectively concealed to the students.
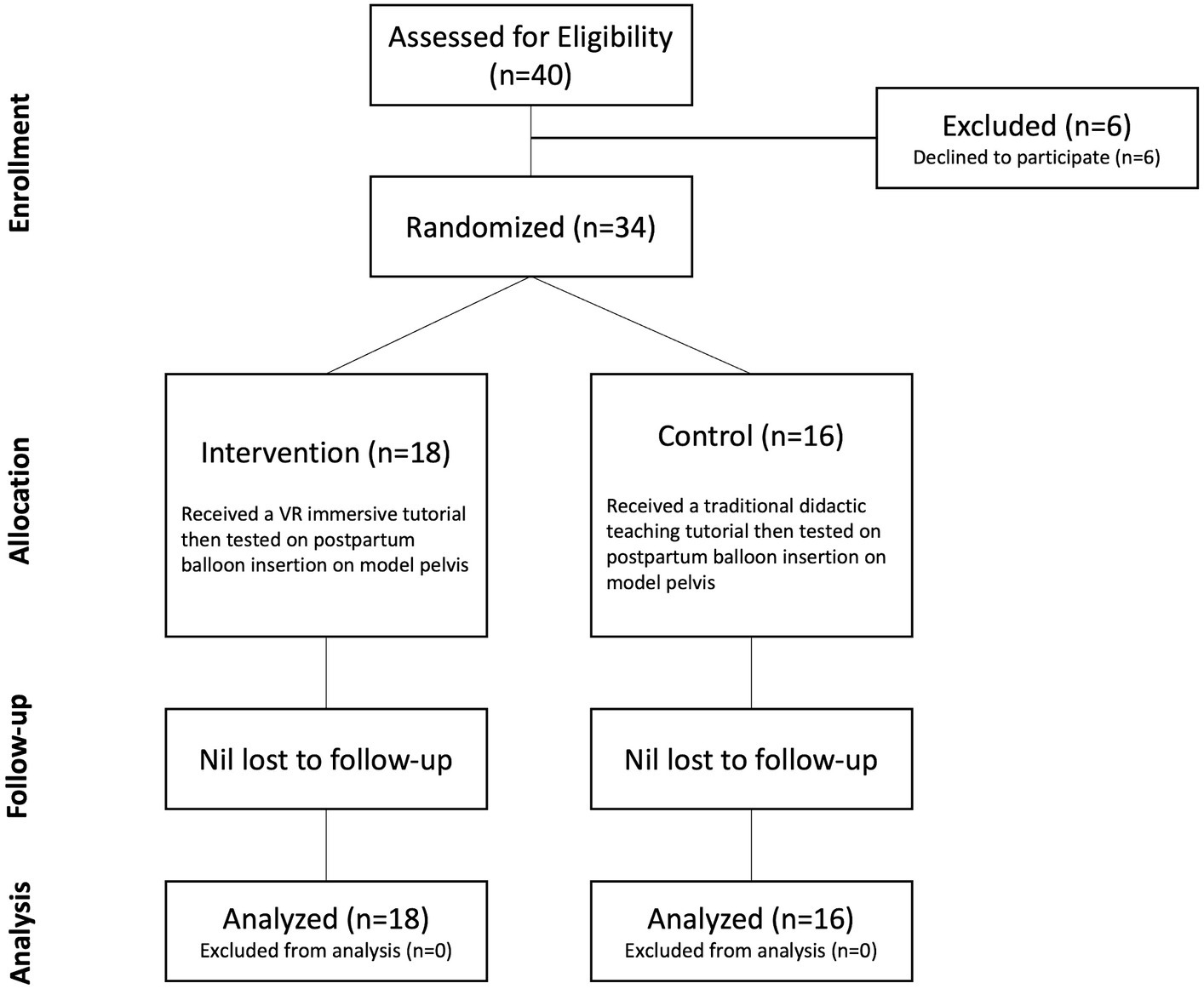
Figure 1. CONSORT (Consolidated Standards of Reporting Trials) diagram depicting the randomization and allocation process. VR – virtual reality.
2.3 Intervention and control groups
The intervention learning experience involved an immersive VR tutorial lasting for fifteen minutes, using an Oculus Lens-2 VR head-mounted display, designed to teach background material regarding PPH management and step-wise procedural instruction of postpartum balloon insertion. The VR learning environment (VRLE) was designed in collaboration with the UCD School of Computer Science and Magos, a company based in Athens, Greece, specializing in creation of VR programmes. Students assigned to the intervention group used the Oculus Headsets to participate in an interactive tutorial on PPH background, emergency management, and postpartum balloon insertion (Figure 2). Participants then carried out postpartum balloon insertion on a model pelvis, and were marked on insertion technique and time taken to complete insertion. All participants completed pre-learning experience and post-learning experience questionnaires, including multiple-choice questions (MCQ) regarding PPH knowledge and management, prior experience of PPH and VR, satisfaction with the learning experience, and attitudes towards use of VR in medical education.
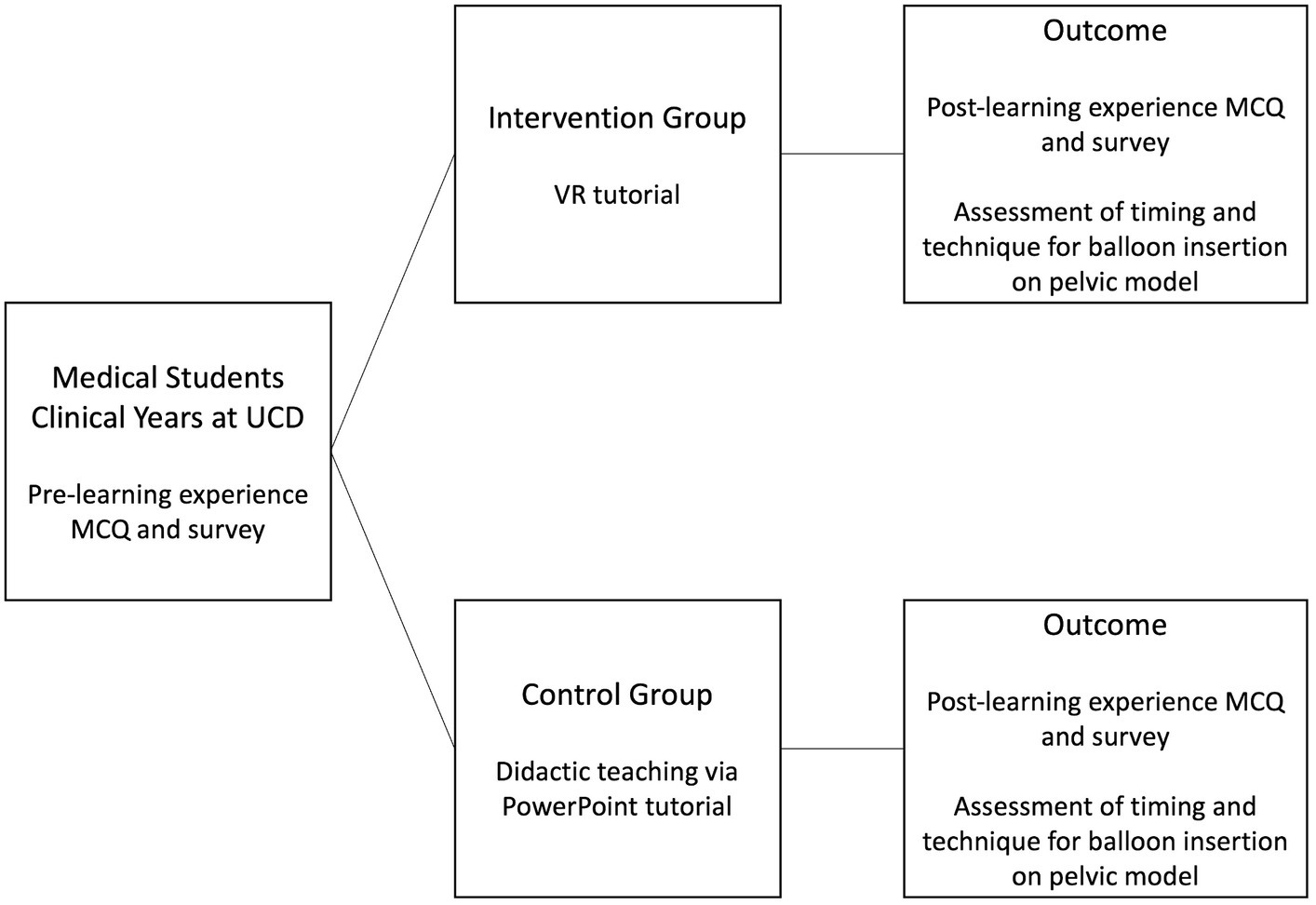
Figure 2. Study design. Pictorial representation of the study design and outcomes. UCD – University College Dublin, MCQ – multiple choice questionnaire, VR – virtual reality.
The control group underwent a traditional didactic learning experience consisting of PowerPoint presentation (Figure 2). The factual content of the traditional tutorial replicated the VRLE tutorial. The traditional tutorial was conducted by the same clinical tutor for the purpose of consistency in the teaching, and lasted for fifteen minutes. Once students had completed the didactic learning experience, they were asked to carry out postpartum balloon insertion on a model pelvis, and were marked on insertion technique and time taken to complete insertion. All participants completed pre-learning experience and post-learning experience questionnaires, including multiple-choice questions regarding PPH knowledge and management, prior experience of PPH and VR, satisfaction with the learning experience and attitudes towards the use of VR in medical education.
2.4 Outcomes
The primary outcome was student knowledge regarding PPH management, as measured by MCQ scores pre-learning experience compared to MCQ scores post-learning experience. Pre-specified secondary outcomes included time taken to complete the task, technique for postpartum balloon insertion, improvement in confidence levels, virtual reality-side effects and satisfaction with the learning experience. Each participant underwent objective, timed assessment of balloon insertion technique on the model pelvis to assess if there was a difference for either learning experience. Confidence levels of managing PPH and postpartum balloon insertion were assessed pre- and post-learning experience. The intervention group was asked to complete a questionnaire regarding side-effects experienced while using the VR headsets. All students were asked a series of questions regarding their attitudes towards the use of VR in medical education and satisfaction with the learning experience.
2.5 Statistical analysis
Data collected was entered and coded into Microsoft Excel. Statistical analysis was performed using SPSS software package (version 27; SPSS, Chicago, Illinois). Descriptive statistics were calculated as frequency and percentage for categorical data or mean and standard deviation for normally distributed variables. The paired t-test was used to compare mean scores for the MCQ and confidence levels pre- and post-learning experience. Independent t-test was used to compare the technique assessment between the intervention and control groups. Chi-square test of independence was used to assess the difference between categorical variables, including timing of insertion of the postpartum balloon on the model pelvis, as the timings were grouped categorically in increments of one minute on the assessment survey. Statistical significance was defined as a p-value <0.05.
3 Results
A total of 40 medical students expressed interest in participating in the study, and were screened for eligibility – 6 students ultimately declined to participate. 34 students were randomly allocated, 18 to the intervention (VRLE) group, and 16 to the control group receiving didactic teaching only (Figure 1). There were no participants lost to follow up and none excluded from the analysis.
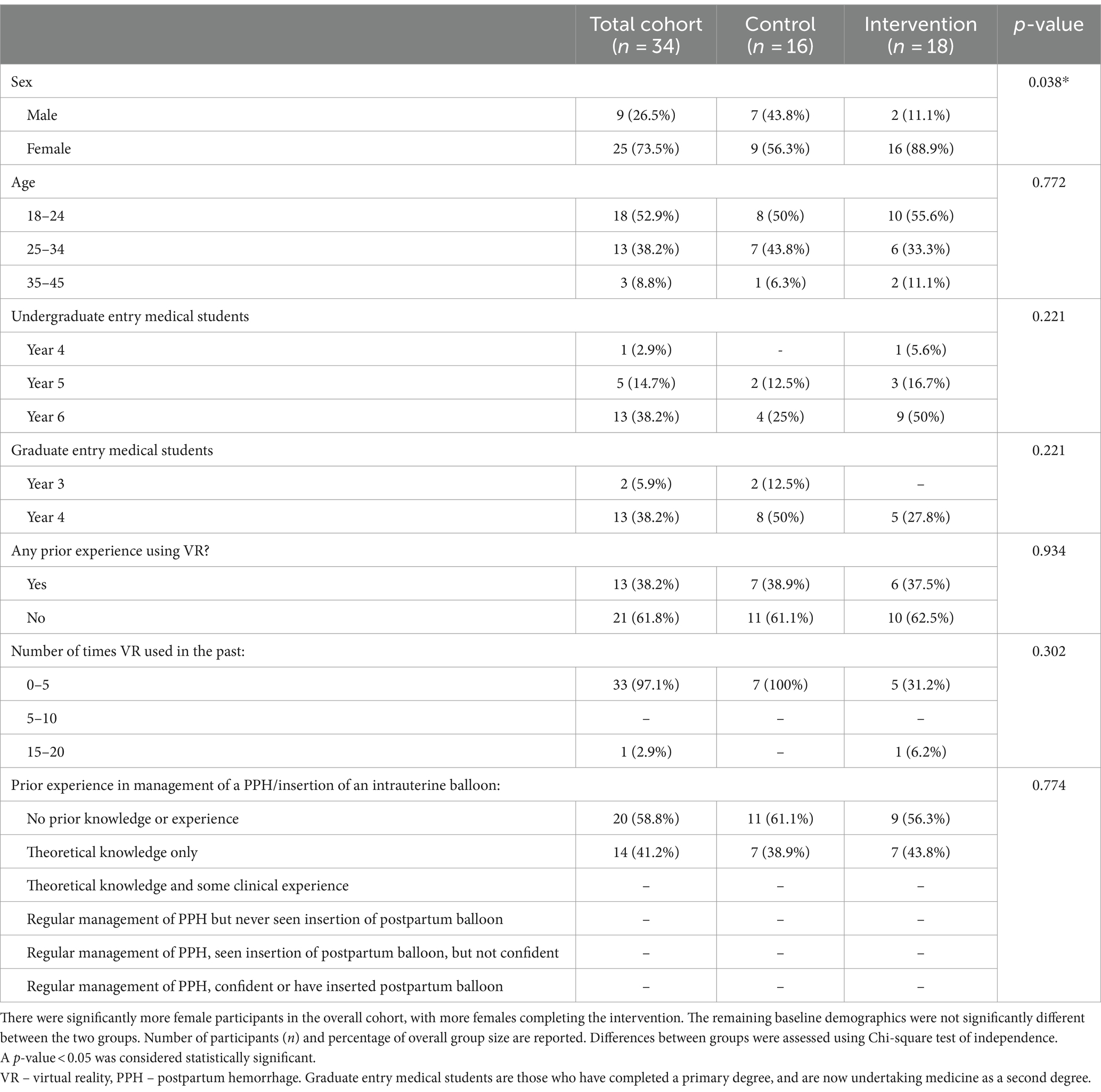
Table 1 outlines the background demographics of the study participants. In the total cohort, 25 participants (73.5%) were female, and 9 participants (26.5%) were male. The majority of participants (52.9%) were between the ages of 18 and 24 years, with 38.2% of participants between the ages of 25 and 34 years. 19 participants were from the undergraduate medicine course, of which 13 (38.2% of the total cohort) were in the final year of the program. 15 participants were from the graduate medicine course, of which 13 (38.2% of the total cohort) were in the final year of the program. 61.8% of the total cohort had no prior experience using VR at the time of the study, with only 1 participant having used VR 15–20 times in the past. In terms of familiarity with PPH, 58.8% of the participants had no prior knowledge or experience of PPH, and 41.2% of the participants had only theoretical knowledge of PPH. Similar to the demographics of the overall cohort, there were significantly (p = 0.038) more females in the intervention group (Table 1). The remaining participant demographics were not significantly different between intervention and control groups.
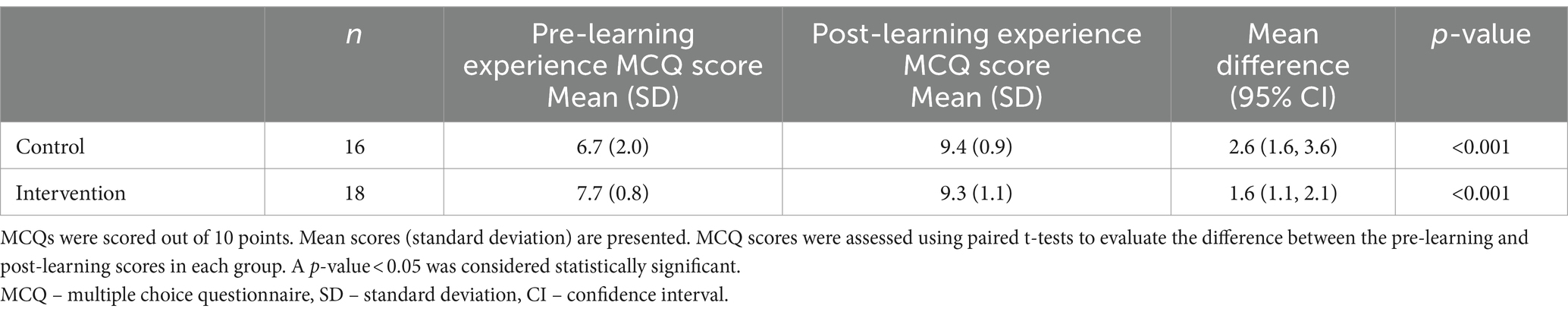
With regards to the primary outcome testing student knowledge of PPH management, there was no significant difference in the mean MCQ score between the intervention or control groups when assessed before and after the learning experiences (Table 2). We noted a significant (p < 0.001) increase in mean MCQ score in both the intervention and control groups when comparing the pre- and post-learning experience MCQ scores (Table 3).
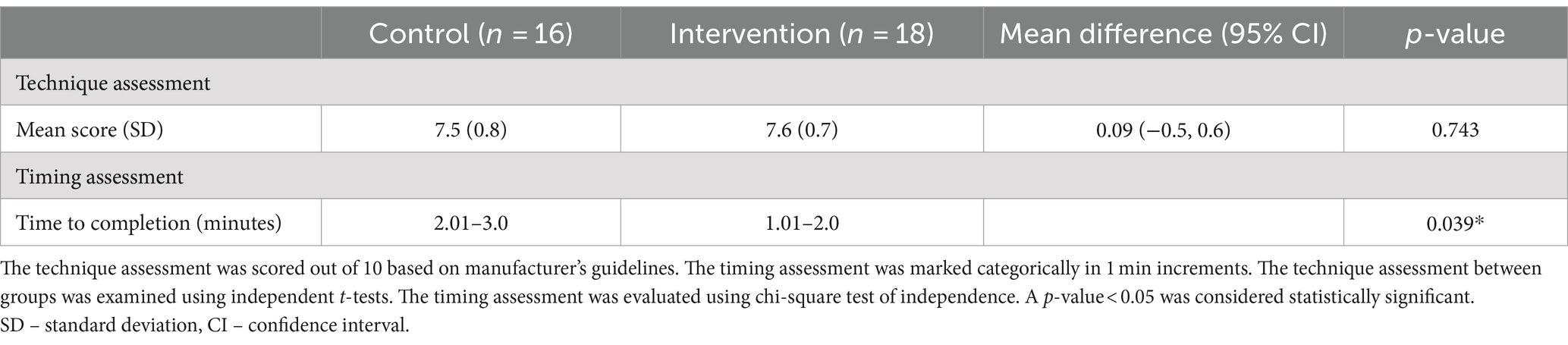
In terms of secondary outcomes, students were assessed on their ability to correctly assemble the components of a postpartum balloon and time taken to do so on a model pelvis. With regards the technique assessment, there was no difference in the mean score obtained between intervention or control groups (Table 4). We noted that students who participated in the intervention VRLE group assembled the postpartum balloon significantly (p = 0.039) faster [1.01–2 min vs. 2.01–3 min], compared with the control group (Table 4).
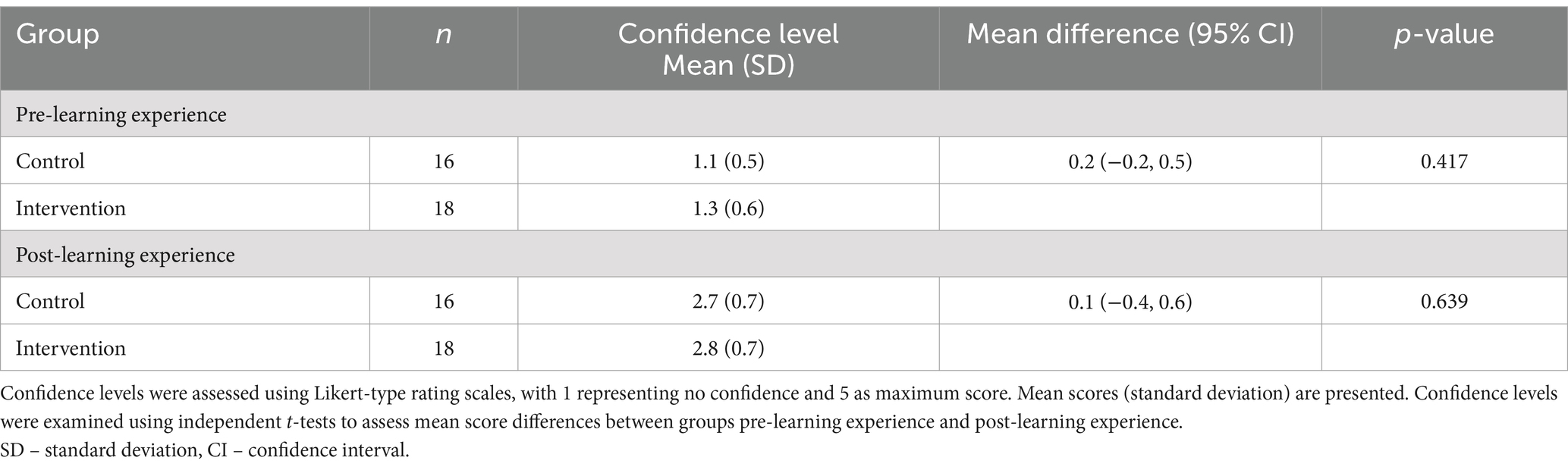
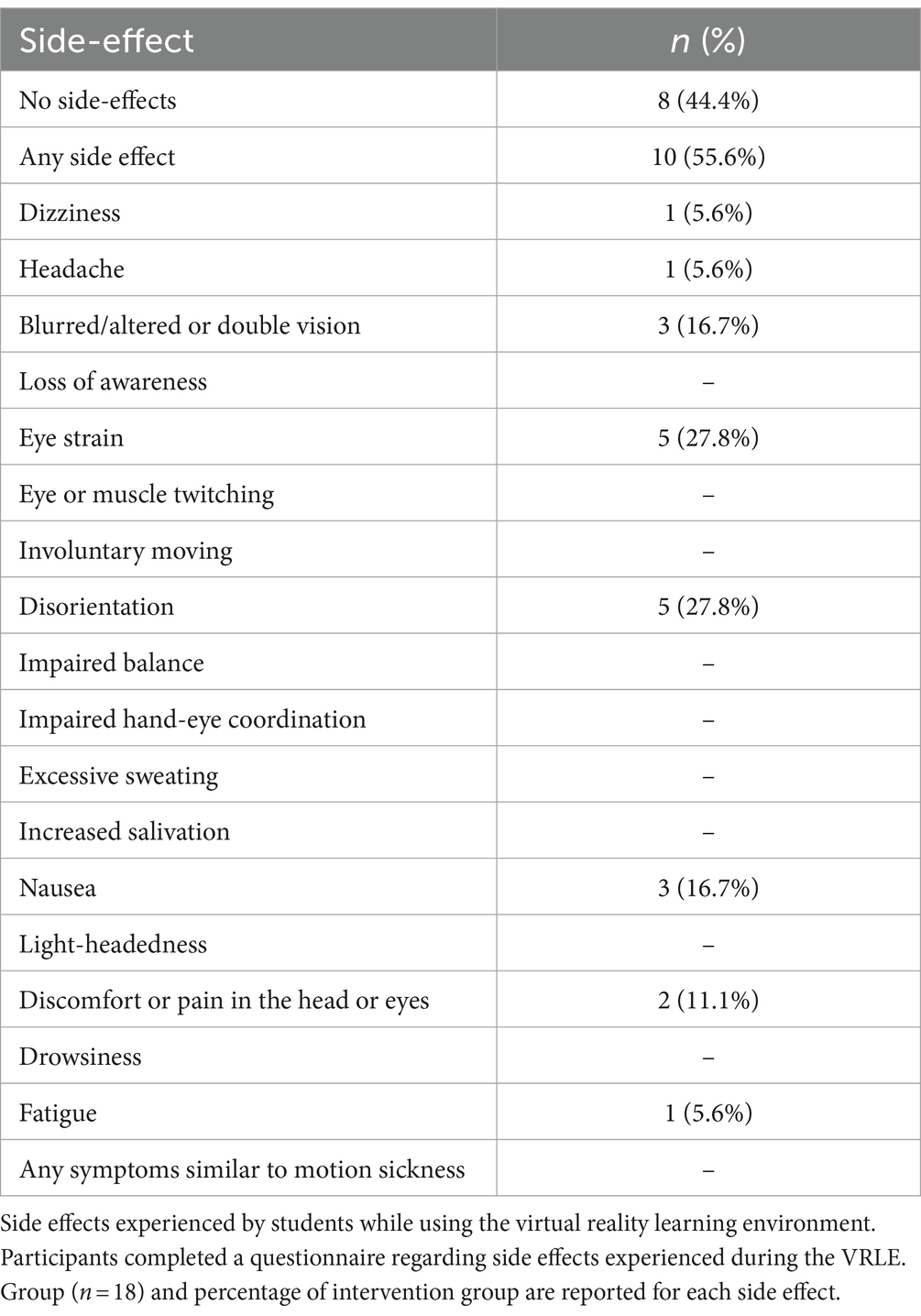
With regards to confidence levels, there was no significant difference in the mean confidence level between the intervention or control group when assessed before and after the learning experiences (Table 5). We noted a significant (p < 0.001) improvement in mean confidence level following the learning experience, in both the intervention and control groups (Table 6). Ultimately, 33 out of 34 participants (97%) felt that their overall confidence improved following training in PPH management and postpartum balloon insertion.
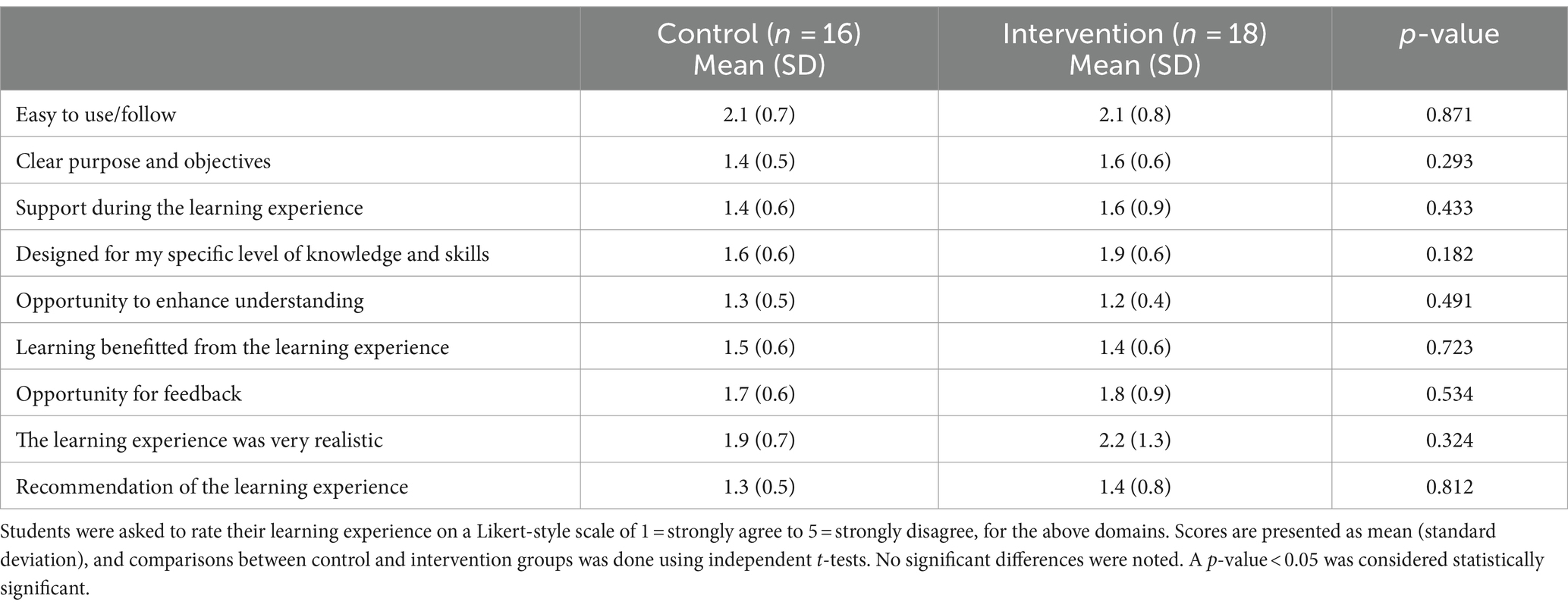
Table 7 describes the side effects experienced by students during the VRLE. 44.4% of those who used the VRLE experienced no side effects. Of those who did experience side effects, the most commonly reported symptoms were eye strain (27.8%), disorientation (27.8%), blurred/altered or double vision (16.7%), and nausea (16.7%).
Table 8 describes student satisfaction with elements common to both learning experiences. Overall, students were highly satisfied with both learning experiences, with mean ratings for each domain ranging from “agree” to “strongly agree” on the Likert-style scale. There was no difference in student satisfaction between the intervention and control group.
In relation to the students’ views regarding the use of VR in medical education, 91.8% of participants agreed that VR technology could be useful as a learning tool in teaching obstetrics and gynecology topics to medical students. Of those who experienced the VRLE, 82.4% of participants were very likely to recommend its use in university and training in obstetrics and gynecology. 94.1% of the participants felt that the VRLE was beneficial over didactic teaching, and 100% of the participants who experienced the VRLE enjoyed the learning experience.
4 Discussion
4.1 Main findings
The objective of our randomized control trial was to pilot the use of a VRLE to enhance medical students’ knowledge of PPH management and insertion of a postpartum balloon for uterine tamponade. Receiving formal instruction, regardless of format, enhanced students’ knowledge of PPH emergency management. Both learning experiences (VRLE and didactic teaching session) enhanced student performance on the post-learning experience MCQ. Additionally, students who participated in the VRLE were quicker at insertion of the postpartum balloon insertion on the model pelvis. Both learning experiences (VRLE and didactic teaching session) also improved student confidence with PPH management, as assessed on the post-learning experience survey. While 55.6% of VRLE participants did experience side-effects of VR, none of them were significant enough to cease the learning experience.
4.2 Comparison with existing literature
Similar to previous studies examining the use of VR in embryology, and anatomy, including fetal and pelvic anatomy (12, 14, 15), no significant differences were demonstrated in the post-learning experience knowledge scores when VRLE was compared to didactic teaching. Previous research has demonstrated that learners who use a VRLE complete tasks significantly quicker than those who used other forms of learning (12, 16). We also found that our students who used the VRLE completed the assessment on the model pelvis quicker than the control group.
Simulation training in obstetrics and gynecology has demonstrated positive effects on the knowledge and skills obtained by the participants and improves overall satisfaction and self-confidence with the content taught through simulation (3). Similar to simulation training, our results suggest that a VRLE has the potential to enhance the knowledge and skills of the students and improve their self-rated confidence levels with the material. It has been suggested that VR may function as an alternative to simulated clinical environments (17).
Medical students find immersive technology, such as VR, very enjoyable to use and adds to their overall learning experience (12, 13, 18). Previous research has demonstrated that students who are motivated and engaged by novel learning methods are more likely to retain knowledge, and may have improved learning outcomes (19). Similarly, we found high levels of satisfaction among students who used the VRLE, with 100% of the students enjoying the experience and 82.4% very likely to recommend the use of VRLE in medical education in the future.
4.3 Implications for the future
Through this RCT, we have highlighted that a VRLE is an acceptable format in which to promote student engagement with concepts in obstetrics and gynecology. It is important to note that medical students are adult learners, and adults are more independent in their learning processes, striving for higher levels of autonomy and self-directed learning (20). In order to support this drive for self-directed learning, intrinsic motivation is required, which can be achieved when the student believes that the learning outcome is relevant to their practice (21). Therefore, the use of a VRLE specifically designed to achieve relevant learning outcomes may be beneficial to enhance student engagement and knowledge retention.
Additionally, VR has the potential to play a key role in creating a learning environment for acquisition of clinical skills in a safe environment (7). Medical education relies heavily on continued practice of procedural skills necessary to begin a clinical career (7). However, in obstetrics and gynecology, this can be very difficult for medical students to achieve due to the sensitive and occasionally invasive nature of the specialty (3). Additionally, medical students require increased exposure to emergency situations in order to prepare them for their clinical practice in the future (3). Therefore, VR is uniquely positioned to create an immersive simulated clinical environment in which students can practice procedural skills as many times as necessary to enhance preparedness for their future clinical careers.
4.4 Strengths and Limitations
A strength of this study is that it is a randomized control trial assessing the use of a VRLE in enhancing medical student knowledge of an important emergency management topic, and assessing its use for teaching rarely encountered procedural skills. A limitation of the current study is the small sample size, which may have led us to be under-powered to discover differences in knowledge acquisition. Additionally, as in previous studies (12, 13, 15), side-effects due to cybersickness are acknowledged as a limitation to the use of VR technology. However, with advancement of VR technology, and repeated exposure to the technology, side effects are expected to decrease (22). Additionally, the cost of VR is acknowledged as a potential barrier to widespread use. Thus far, VR in medical education has not been widely available due to high costs and lack of evidence of its efficacy (23). Once the VRLE has been developed, it can be used repeatedly without further development costs, however it is acknowledged that regular maintenance and software updates are required to ensure function of the VR headsets. Of note, recent technological advancements have reduced the cost of VR headsets, making them more affordable (24). Future studies with larger cohorts of medical students could further explore the use of the VRLE as learning tools for medical students, especially for procedural skills.
5 Conclusion
Receiving formal instruction, regardless of format, enhances students’ knowledge and confidence of the topic covered. Students who received instruction via the VRLE assembled the postpartum balloon faster than students who received didactic teaching. Use of VRLE in medical education represents an acceptable learning environment in which to engage students in order to enhance the overall learning experience. VR may be beneficial in teaching hands-on procedural skills in obstetrics and gynecology education.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by University College Dublin Research Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
KD: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing, Project administration. GD: Data curation, Writing – original draft, Writing – review & editing, Formal analysis. AM: Conceptualization, Methodology, Project administration, Writing – review & editing. DK: Conceptualization, Software, Writing – review & editing, Methodology. SH: Funding acquisition, Supervision, Writing – review & editing, Conceptualization, Validation. EM: Software, Supervision, Writing – review & editing, Validation. FM: Conceptualization, Funding acquisition, Methodology, Supervision, Writing – review & editing, Project administration, Validation.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by funding by the University College Dublin, Ireland and The National Maternity Hospital, Dublin, Ireland. Virtual reality headsets were previously purchased by University College Dublin, and the postpartum balloon insertion programme was created using funding from University College Dublin. Cook Medical provided the model pelvis for participant assessment, but did not contribute to the funding of this study.
Acknowledgments
The authors would like to sincerely thank all of the medical students for their participation in the study, the research centre, and the research team for their ongoing support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Mavrides, EAS, Chandraharan, E, Collins, P, Green, L, Hunt, BJ, Riris, S, et al. Prevention and Management of Postpartum Haemorrhage: Green-top guideline no. 52. BJOG. (2017) 124:e106–49. doi: 10.1111/1471-0528.14178
2. Purandare, CN, Nazareth, AK, Ryan, G, and Purandare, NC. Role of balloon tamponade as a therapeutic non-surgical tool in controlling obstetric and gynecological hemorrhage in low-resource countries. J Obstet Gynaecol India. (2022) 72:285–90. doi: 10.1007/s13224-022-01662-7
3. Tauscher, A, Stepan, H, Todorow, H, and Rotzoll, D. Interteam PERINAT—interprofessional team collaboration in undergraduate midwifery and medical education in the context of obstetric emergencies: presentation of simulation scenarios and empirical evaluation results. GMS J Med Educ. (2023) 40:Doc20. doi: 10.3205/zma001602
4. Minehart, RD, and Gallin, H. Postpartum hemorrhage: the role of simulation. Best Pract Res Clin Anaesthesiol. (2022) 36:433–9. doi: 10.1016/j.bpa.2022.11.002
5. Shore, EM, Davidson, A, Arnason, M, Kara, H, Shah, A, and Shah, R. Bridging the gap: incorporating simulation into obstetrics and Gynaecology undergraduate medical education. J Obstet Gynaecol Can. (2019) 41:191–196.e2. doi: 10.1016/j.jogc.2018.03.016
6. Jin, J, and Bridges, SM. Educational technologies in problem-based learning in health sciences education: a systematic review. J Med Internet Res. (2014) 16:e251. doi: 10.2196/jmir.3240
7. Ryan, GV, Callaghan, S, Rafferty, A, Higgins, MF, Mangina, E, and McAuliffe, F. Learning outcomes of immersive Technologies in Health Care Student Education: systematic review of the literature. J Med Internet Res. (2022) 24:e30082. doi: 10.2196/30082
8. McGaghie, WC, and Harris, IB. Learning theory foundations of simulation-based mastery learning. Simul Healthc. (2018) 13:S15–20. doi: 10.1097/SIH.0000000000000279
9. Taylor, DC, and Hamdy, H. Adult learning theories: implications for learning and teaching in medical education: AMEE guide no. 83. Med Teach. (2013) 35:e1561–72. doi: 10.3109/0142159X.2013.828153
10. Izard, SG, Juanes, JA, Garcia Penalvo, FJ, Estella, JMG, Ledesma, MJS, and Ruisoto, P. Virtual reality as an educational and training tool for medicine. J Med Syst. (2018) 42:50. doi: 10.1007/s10916-018-0900-2
11. Graafland, M, Schraagen, JM, and Schijven, MP. Systematic review of serious games for medical education and surgical skills training. Br J Surg. (2012) 99:1322–30. doi: 10.1002/bjs.8819
12. Kane, D, Ryan, G, Mangina, E, and McAuliffe, FM. A randomized control trial of a virtual reality learning environment in obstetric medical student teaching. Int J Med Inform. (2022) 168:104899. doi: 10.1016/j.ijmedinf.2022.104899
13. Ryan, G, Rafferty, A, Murphy, J, Higgins, MF, Mangina, E, and McAuliffe, FM. Virtual reality learning: a randomized controlled trial assessing medical student knowledge of fetal development. Int J Gynaecol Obstet. (2023) 162:292–9. doi: 10.1002/ijgo.14684
14. Arents, V, de Groot, PCM, Struben, VMD, and van Stralen, KJ. Use of 360 degrees virtual reality video in medical obstetrical education: a quasi-experimental design. BMC Med Educ. (2021) 21:202. doi: 10.1186/s12909-021-02628-5
15. Ryan, G, Callaghan, S, Rafferty, A, Murphy, J, Higgins, M, Barry, T, et al. Virtual reality in midwifery education: a mixed methods study to assess learning and understanding. Nurse Educ Today. (2022) 119:105573. doi: 10.1016/j.nedt.2022.105573
16. Nickel, F, Brzoska, JA, Gondan, M, Rangnick, HM, Chu, J, Kenngott, HG, et al. Virtual reality training versus blended learning of laparoscopic cholecystectomy: a randomized controlled trial with laparoscopic novices. Medicine (Baltimore). (2015) 94:e764. doi: 10.1097/MD.0000000000000764
17. Birkham, SL, Calogiuri, G, and Martinsen, R. Advancing immersive virtual reality-based simulation practices: developing an evidence-based and theory-driven pedagogical framework for VR-based simulations of non-technical skills among healthcare professionals. Interact Learn Environ. (2023):1–13. doi: 10.1080/10494820.2023.2186896
18. Guetterman, TC, Sakakibara, R, Baireddy, S, Kron, FW, Scerbo, MW, Cleary, JF, et al. Medical Students' experiences and outcomes using a virtual human simulation to improve communication skills: mixed methods study. J Med Internet Res. (2019) 21:e15459. doi: 10.2196/15459
19. Huang, H-M, Rauch, U, and Liaw, S-S. Investigating learners’ attitudes toward virtual reality learning environments: based on a constructivist approach. Comput Educ. (2010) 55:1171–82. doi: 10.1016/j.compedu.2010.05.014
20. Zigmont, JJ, Kappus, LJ, and Sudikoff, SN. Theoretical foundations of learning through simulation. Semin Perinatol. (2011) 35:47–51. doi: 10.1053/j.semperi.2011.01.002
21. Ryan, RM, and Deci, EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. (2000) 55:68–78. doi: 10.1037/0003-066X.55.1.68
22. Kim, J, Luu, W, and Palmisano, S. Multisensory integration and the experience of scene instability, presence and cybersickness in virtual environments. Comput Hum Behav. (2020) 113:106484:106484. doi: 10.1016/j.chb.2020.106484
23. Farra, SL, Gneuhs, M, Hodgson, E, Kawosa, B, Miller, ET, Simon, A, et al. Comparative cost of virtual reality training and live exercises for training Hospital Workers for Evacuation. Comput Inform Nurs. (2019) 37:446–54. doi: 10.1097/CIN.0000000000000540
Keywords: medical education, obstetrics and gynecology, virtual reality learning environment, postpartum hemorrhage, balloon tamponade
Citation: Dunlop K, Dillon G, McEvoy A, Kane D, Higgins S, Mangina E and McAuliffe FM (2024) The virtual reality classroom: a randomized control trial of medical student knowledge of postpartum hemorrhage emergency management. Front. Med. 11:1371075. doi: 10.3389/fmed.2024.1371075
Edited by:
Fedde Scheele, VU Amsterdam, NetherlandsReviewed by:
Bhavani Veasuvalingam, International Medical University, MalaysiaMarja Dijksterhuis, Amphia Ziekenhuis, Netherlands
Copyright © 2024 Dunlop, Dillon, McEvoy, Kane, Higgins, Mangina and McAuliffe. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fionnuala M. McAuliffe, Zmlvbm51YWxhLm1jYXVsaWZmZUB1Y2QuaWU=
 Kristyn Dunlop1
Kristyn Dunlop1 Grace Dillon
Grace Dillon Daniel Kane
Daniel Kane Eleni Mangina
Eleni Mangina Fionnuala M. McAuliffe
Fionnuala M. McAuliffe