- 1Research and Development Unit, Hammersmith and Fulham Primary Care Network, London, United Kingdom
- 2Faculty of Medicine, Imperial College London, London, United Kingdom
Introduction
In the evolving healthcare narrative, the pronounced relationship between environmental shifts and human health reflects the global impacts of climate change. These include rising temperatures, erratic weather patterns, and increasing natural disasters, affecting not only our physical environment but also our collective mental wellbeing. The WHO predicts that between 2030 and 2050, climate change will result in ~250,000 additional deaths per year, with significant implications for mental health (1).
Climate change and mental health: a growing concern
The effects of these environmental disruptions ripple through communities, inducing anxiety, stress, and trauma (2). Now, more than ever, this connection of climate change and mental health is demanding attention. The significance lies not just in acknowledging this connection but in understanding its multifaceted implications, especially within primary care settings.
Simultaneously, the subtle, long-term changes brought about by global warming also weigh heavily on mental wellbeing (2). Watching landscapes alter, hometowns become uninhabitable, and traditional ways of life dissolve can foster solastalgia, the emotional distress caused by environmental change in one's home environment (3–5).
Growing up amidst dramatic climate shifts, children and adolescents face unique psychological challenges, including early-onset anxiety and a pervasive sense of hopelessness (6, 7). Furthermore, these chronic stresses potentially exacerbate pre-existing mental health conditions and create a cascade of challenges that could persist into adulthood.
The deepening crisis of climate change permeates numerous aspects of our lives (6). Yet, its complex relationship with mental health remains inadequately explored, particularly within primary care setting. The multifaceted effects of climate change, from direct physical impacts such as droughts and floods to the subtler, indirect consequences like diminished community cohesion due to forced relocations, exacerbate a spectrum of mental health challenges. These span from episodic distress and anxiety to long-term conditions like depression and PTSD (8, 9).
Challenges and opportunities in primary care
At the frontline of healthcare delivery, primary care is crucial in understanding and addressing the barriers to integrating mental health care amidst climate change. These barriers include lack of training, resource constraints, and insufficient policy support. Conversely, facilitators such as interdisciplinary collaboration, robust policy frameworks, and community engagement can significantly enhance this integration (10).
The significance of clearly identifying the key stakeholders crucial for effectively implementing these recommendations is universally acknowledged. As such, this opinion paper is directed not only at primary care practitioners but also at primary care networks, professional associations, health ministries, and policymakers. Each entity plays a vital and distinct role in embedding considerations of climate change into mental health care (11).
The primary care setting, with its emphasis on holistic, patient-centered care, is uniquely positioned to detect, address, and support those struggling with climate-related psychological distress (12, 13). Physicians, nurse practitioners, and healthcare workers at this level often have an ongoing relationship with patients, allowing for the detection of subtle behavioral shifts and the provision of timely interventions.
However, achieving this requires integrating a new dimension into primary care, an awareness and understanding of the environmental context. Just as a primary care physician might inquire about personal and occupational stresses, the discussion must expand to include environmental anxieties and exposures. Regular screenings, not just for traditional ailments but also for signs of environmental distress, can aid in early detection and management (14). Additionally, given the community-centered nature of primary care, physicians can also play an instrumental role in fostering community resilience, advocating for community-based support systems and interventions that cater to collective traumas and anxieties.
Integrating climate change-related mental health care within primary care settings presents unique challenges and opportunities. The barriers include the current lack of specific training for primary care providers in addressing environmental impacts on mental health, the limited availability of mental health resources, and the overarching need for more supportive healthcare policies (15). However, facilitators are also emerging, such as increased awareness of climate change impacts, growing advocacy for mental health services, and the development of new interdisciplinary training programs that include environmental health. Addressing these factors effectively requires a coordinated effort from healthcare providers, policymakers, and the community at large (Table 1).
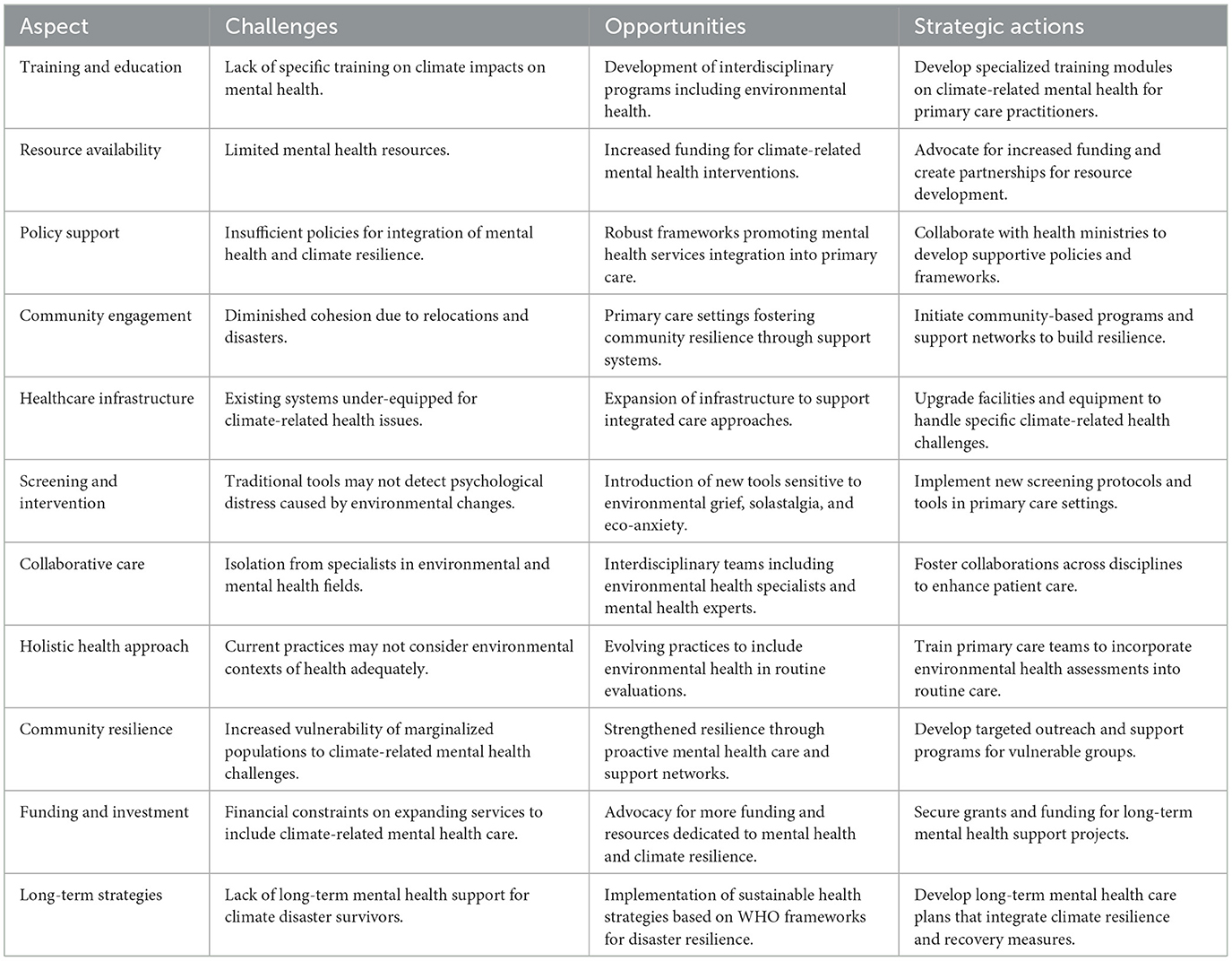
Table 1. Strategic framework for integrating climate resilience into mental health care in primary care settings.
While the connection between climate change and mental health is clear, considering other factors such as genetics and personal traumas is crucial. We must also ponder whether primary care should handle these specialized issues alone. Additionally, burdening the already strained primary care sector with climate-related mental health challenges might dilute care quality. Is it worth considering a specialized avenue for such issues, separate from primary care? The variability in individual responses to environmental stressors underscores the need for fostering resilience (16). Moreover, the financial and logistical challenges of overhauling primary care to accommodate this new dimension require careful consideration.
Immediate and long-term psychological impacts
To appreciate the gravity of the matter, one need only observe the aftermath of climate-related disasters (6). The turmoil following such events isn't merely the visible destruction, but also the invisible scars borne by survivors. Natural disasters resulting in personal loss, loss of loved ones, loss of homes, and loss of a sense of security. While the physical reconstruction following these climate-change disasters might be swift, the psychological wounds often linger, giving rise to PTSD, depression, and increased suicidal ideation (13). Furthermore, the anticipation and uncertainty surrounding future disasters contribute to chronic anxiety, fostering feelings of helplessness and pessimism among vulnerable populations.
To further complicate the landscape of mental health in the context of climate change, it is crucial to acknowledge that these impacts do not occur in a vacuum but rather exacerbate existing health inequalities. Vulnerable and marginalized populations, often burdened disproportionately by socio-economic and health disparities, face a heightened risk of adverse mental health outcomes (17). This recognition is critical for primary care practitioners, who must navigate these compounded challenges when implementing mental health interventions in an era marked by environmental distress.
In the immediate aftermath of climate-related disasters, the surge in acute stress reactions and post-traumatic stress disorder (PTSD) among affected populations is well-documented. A study by Lowe et al. (3) in the wake of Hurricane Sandy highlighted significant increases in PTSD symptoms among residents in the most affected areas. These findings underscore the urgent need for primary care practitioners to be equipped with strategies to address the immediate mental health impacts of climate-related disasters.
Beyond the immediate aftermath, the long-term psychological impacts of climate-related disasters manifest as chronic mental health conditions, including prolonged depression, anxiety disorders, and sustained PTSD. A longitudinal study by Norris et al. (7) on the long-term effects of natural disasters found that a significant portion of affected individuals exhibited persistent symptoms of depression and PTSD several years post-disaster. Moreover, a review by Hayes et al. (8) highlighted that the anticipation of future climate-related events could lead to chronic stress and anxiety, further exacerbating the long-term mental health challenges faced by communities. These studies emphasize the complex, enduring mental health repercussions of climate change, reinforcing the need for long-term mental health support strategies within primary care settings.
Integrating climate resilience into healthcare systems
In this context, the WHO's “Operational Framework for Building Climate Resilient Health Systems” (15) and “Health Emergency and Disaster Risk Management Framework” (16) are pivotal in guiding our approaches to integrate climate resilience into primary care systems. These frameworks offer valuable insights into how health systems can anticipate, respond to, and recover from climate-related disruptions, ensuring sustained mental health support.
To address the profound impact of climate change on mental health, primary care physicians must update their training to include climate-related mental health insights. They should integrate environmental stress screenings into routine check-ups and establish connections with mental health specialists trained in ecological grief and solastalgia.
Integrating insights from environmental science, psychology, sociology, and public health into primary care can significantly enhance our approach to climate-induced mental health issues (4–6). Environmental scientists highlight the direct link between increased exposure to natural disasters and the escalation of mental health conditions, emphasizing the need for primary care practitioners to be vigilant in recognizing symptoms related to environmental stressors (11). Psychologists bring attention to the concept of eco-anxiety and solastalgia, psychological states that are becoming increasingly prevalent as individuals grapple with the rapid changes in their natural environments and the loss of their homes to climate change (18). This nuanced understanding of climate-related psychological distress is crucial for primary care providers in identifying and addressing these emerging mental health concerns.
From a sociological perspective, the disruption of social networks and community cohesion due to environmental disasters can exacerbate feelings of isolation and depression, making it imperative for primary care settings to incorporate social support mechanisms in their response to climate-related mental health challenges (12). Public health research further underscores the importance of a multidisciplinary approach, advocating for the integration of mental health services within primary care to provide a more holistic and accessible form of care for those affected by climate change (11). By adopting a cross-disciplinary perspective, primary care can evolve into a more resilient and responsive system, capable of addressing the complex interplay between climate change and mental health.
To effectively integrate the imperative of addressing climate-induced mental health issues within primary care, policy recommendations are crucial. Such programs would equip practitioners with the skills needed to address climate-related anxieties, solastalgia, and other psychological impacts of climate change (3, 6). Moreover, healthcare infrastructure must be adapted to support these initiatives, potentially requiring the expansion of mental health services within primary care settings and the establishment of interdisciplinary teams that include environmental scientists and mental health specialists (2, 4).
To support these changes, increased funding for research into the mental health effects of climate change is essential. This would enable the development of evidence-based interventions and screening tools specifically designed to detect climate-related psychological distress. Policymakers must prioritize the integration of climate change and mental health considerations into healthcare planning and resource allocation to ensure that primary care settings are adequately equipped to respond to this emerging challenge (Table 1) (6, 9).
Stakeholder roles and policy recommendations
Ultimately, to navigate the broad implications of climate-induced mental health challenges, it is imperative to engage diverse stakeholders (19, 20). Professional associations can lead in developing guidelines and training modules for practitioners. Ministries of health and primary care networks can facilitate the integration of these guidelines into practice and ensure that sufficient resources are allocated. Individual primary care providers are crucial as they are often the first point of contact for individuals experiencing climate-related distress.
To further strengthen the support system within primary care, it is essential to direct practitioners to existing evidence-based clinical guidelines that address common mental health conditions, ensuring adherence to best practices. Concurrently, recognizing the unique challenges posed by climate-related psychoterratic syndromes, there is a critical need to develop and integrate new evidence-based interventions (21, 22). These should not only focus on psychological aspects but also consider broader ecological and societal impacts, thereby providing a comprehensive response to the multifaceted nature of these disorders. This dual approach will ensure that primary care settings are equipped to address both traditional and emerging mental health challenges effectively.
Following the directives of the WHO's “Mental Health and Climate Change: Policy Brief” (23), this paper advocates for targeted mental health strategies that address the psychological impacts of climate change. These strategies should include enhancing the capacities of primary care practitioners to manage climate-induced psychological distress, as recommended by WHO/WONCA's “Integrating Mental Health into Primary Care: A Global Perspective” (24). This guide serves as a crucial resource for implementing integrated mental health services at the primary care level, ensuring that mental health considerations are not overlooked in the face of environmental challenges.
To enact meaningful change, it is essential to delineate the responsibilities of various key stakeholders: primary care networks and agencies must implement these policies and resources at a local level, ensuring that primary care facilities are prepared to handle the increasing mental health load due to climate change. Professional associations should advocate for and develop specialized training and resources to equip healthcare providers with the necessary tools to address climate-related mental health issues (25). While, ministries of health need to create supportive policies and funding mechanisms that enable the integration of mental health considerations into the primary care settings. Furthermore, individual healthcare providers are on the frontlines, required to apply new knowledge and resources in their daily practice to detect and manage climate-related psychological distress.
To overcome these barriers, policy recommendations should focus on developing and implementing training programs tailored to the needs of primary care practitioners, enhancing funding for mental health resources, and fostering a policy environment that supports integrated care approaches (26). Leveraging facilitators involves promoting interdisciplinary collaboration between environmental scientists, mental health specialists, and primary care providers, and harnessing community engagement to build resilient healthcare systems that can withstand and adapt to the challenges posed by climate change.
Innovative models for climate-related mental health care
To effectively incorporate climate-related mental health into primary care, innovative models must be developed. One such model could involve the integration of new screening tools specifically designed to detect signs of climate-related psychological distress. These tools would be sensitive to the nuanced ways in which environmental changes impact mental health, enabling early identification and intervention (16, 19, 25). For instance, the use of questionnaires that assess feelings of environmental grief, anxiety related to climate change, and symptoms of solastalgia could become standard practice in patient evaluations. This approach not only acknowledges the direct impacts of climate change on mental wellbeing but also validates the patient's experiences, facilitating a more empathetic and comprehensive care strategy (21, 22).
Furthermore, the primary care setting should evolve to incorporate environmental health into routine patient history taking. By asking patients about their environmental exposures, concerns, and the perceived impact of climate change on their wellbeing, healthcare providers can gain valuable insights into the environmental determinants of health. Additionally, establishing partnerships with environmental health specialists can enhance the primary care provider's ability to address these complex issues. Such collaborations could lead to interdisciplinary care teams capable of addressing both the psychological and environmental aspects of patient health, ensuring a holistic approach to care (11, 19, 26). These innovative care models, rooted in a deep understanding of the interconnectedness of environmental changes and mental health, have the potential to transform primary care into a more responsive and effective system for addressing the mental health challenges posed by climate change.
Conclusion
The integration of primary care, mental health, and climate change has broad implications for the medical community and society at large (9). For the medical field, it signifies a paradigm shift where healthcare doesn't just respond to symptoms but also to the environmental contexts inducing them. It implies a potential surge in patients presenting with mental health issues linked to climate anxieties, necessitating a reorientation of healthcare strategies, resources, and training to cater to this emergent patient population. Beyond individual health, it also indicates a larger societal dialogue, prompting communities to struggle with collective psychological traumas induced by a shifting environment (10). The broader implications reverberate through policy, education, and community health initiatives, emphasizing the interconnectedness of our environment, wellbeing, and healthcare structures (25, 26).
To ensure a sustainable approach to mental health in the face of climate change, it is imperative to draw upon established frameworks like the WHO's “Health Emergency and Disaster Risk Management Framework” (16). This framework not only provides a blueprint for health systems to handle acute and long-term health challenges arising from climate disasters but also emphasizes the importance of integrating these strategies into primary care practices. Such integration ensures that mental health responses are swift, effective, and culturally sensitive, tailored to the needs of affected communities.
Concluding, while the challenges loom large, they also present a unique chance for reinvention. The goal is to shape a proactive primary care system, poised to address the deep-seated mental impacts of our changing climate.
Author contributions
WJ: Conceptualization, Formal analysis, Methodology, Resources, Visualization, Writing—original draft, Writing—review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organisation. Climate Change and Health. (2021). Available online at: https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health (accessed April 28, 2024).
2. Lawrance EL, Thompson R, Newberry Le Vay J, Page L, Jennings N. The impact of climate change on mental health and emotional wellbeing: a narrative review of current evidence, and its implications. Int Rev Psychiatr. (2022) 34:443–98. doi: 10.1080/09540261.2022.2128725
3. Lowe SR, Sampson L, Gruebner O, Galea S. Psychological resilience after Hurricane Sandy: the influence of individual- and community-level factors on mental health after a large-scale natural disaster. PLoS ONE. (2015) 10:e0125761. doi: 10.1371/journal.pone.0125761
4. Redwood-Campbell L, Abrahams J. Primary health care and disasters-the current state of the literature: what we know, gaps and next steps. Prehosp Disaster Med. (2011) 26:184–91. doi: 10.1017/S1049023X11006388
5. Burns P, Douglas K, Hu W. Primary care in disasters: opportunity to address a hidden burden of health care. Med J Austr. (2019) 210:297–9. doi: 10.5694/mja2.50067
6. Burns P, FitzGerald G, Hu W, Aitken P, Douglas K. General practitioners' roles in disaster health management: perspectives of disaster managers. Prehosp Disast Med. (2022) 37:124–31. doi: 10.1017/S1049023X21001230
7. Norris FH, Friedman MJ, Watson PJ. 60,000 disaster victims speak: part II. Summary and implications of the disaster mental health research. Psychiatry. (2002) 65:240–60. doi: 10.1521/psyc.65.3.240.20169
8. Hayes K, Blashki G, Wiseman J, Burke S, Reifels L. Climate change and mental health: risks, impacts and priority actions. Int J Ment Health Syst. (2018) 12:28. doi: 10.1186/s13033-018-0210-6
9. Walinski A, Sander J, Gerlinger G, Clemens V, Meyer-Lindenberg A, Heinz A. The effects of climate change on mental health. Dtsch Arztebl Int. (2023) 120:117–24. doi: 10.3238/arztebl.m2022.0403
10. van Nieuwenhuizen A, Hudson K, Chen X, Hwong AR. The effects of climate change on child and adolescent mental health: clinical considerations. Curr Psychiatry Rep. (2021) 23:88. doi: 10.1007/s11920-021-01296-y
11. Freedy JR, Simpson WM. Disaster-related physical and mental health: a role for the family physician. Am Fam Physician. (2007) 15:841–6.
12. Cianconi P, Betrò S, Janiri L. The impact of climate change on mental health: a systematic descriptive review. Front Psychiatry. (2020) 11:74. doi: 10.3389/fpsyt.2020.00074
13. Palinkas LA, O'Donnell ML, Lau W, Wong M. Strategies for delivering mental health services in response to global climate change: a narrative review. Int J Environ Res Public Health. (2020) 17:8562. doi: 10.3390/ijerph17228562
14. Woodland L, Ratwatte P, Phalkey R, Gillingham EL. Investigating the health impacts of climate change among people with pre-existing mental health problems: a scoping review. Int J Environ Res Public Health. (2023) 20:5563. doi: 10.3390/ijerph20085563
15. WHO. Operational Framework for Building Climate Resilient Health Systems. Geneva: WHO (2015). Available online at: https://www.who.int/publications/i/item/9789241565073 (accessed April 28, 2024).
16. WHO. Health Emergency and Disaster Risk Management Framework. (2019). Available online at: https://iris.who.int/handle/10665/326106 (accessed April 28, 2024).
17. Berry HL, Bowen K, Kjellstrom T. Climate change and mental health: a causal pathways framework. Int J Public Health. (2010) 55:123–32. doi: 10.1007/s00038-009-0112-0
18. Stein BD, Myers D. Emotional sequelae of disasters: a primary care physician's guide. J Am Med Women's Assoc. (1999) 54:60–4.
19. Tupou T, Tiatia-Siau J, Newport C, Langridge F, Tiatia S. Is the concept of solastalgia meaningful to pacific communities experiencing mental health distress due to climate change? An initial exploration. Int J Environ Res Public Health. (2023) 20:7041. doi: 10.3390/ijerph20227041
20. Tabe-Ojong MPJ, Boakye JA, Muliro M. Mitigating the impacts of floods using adaptive and resilient coping strategies: the role of the emergency Livelihood Empowerment Against Poverty program (LEAP) in Ghana. J Environ Manage. (2020) 270:110809. doi: 10.1016/j.jenvman.2020.110809
21. Reay L, Burns P. The role of primary health networks and general practitioners in disasters: nepean blue mountains primary health network's preparedness guide. Prehosp Disast Med. (2019) 34:67. doi: 10.1017/S1049023X19001481
22. Crompton D, Shakespeare-Finch J, FitzGerald G, Kohleis P, Young R. Mental health response to disasters: is there a role for a primary care-based clinician? Prehosp Disast Med. (2022) 37:706–11. doi: 10.1017/S1049023X22001194
23. WHO. Mental Health and Climate Change: Policy Brief . (2021). Available online at: https://www.who.int/publications/i/item/9789240045125 (accessed April 28, 2024).
24. WHO/WONCA. Integrating Mental Health Into Primary Care: A Global Perspective. Geneva: WHO (2008). Available online at: https://www.who.int/publications/i/item/9789241563680 (accessed April 28, 2024).
25. National Disaster Mental Health and Wellbeing Framework. Supporting the Wellbeing of all Australians in Times of Disaster Through the National Disaster Mental Health and Wellbeing Framework. (2023). Available online at: https://nema.gov.au/about-us/budget-2023-24/Mental-Health-Wellbeing-Framework (accessed April 28, 2024).
26. Australian Government. National Health and Climate Strategy. (2023). Available online at: https://www.health.gov.au/resources/publications/national-health-and-climate-strategy?language=en (accessed April 28, 2024).
Keywords: healthcare, mental health, environmental, climate change, natural disaster
Citation: Jerjes W (2024) Climate's silent impact: reframing primary care in the era of environmental distress. Front. Med. 11:1384786. doi: 10.3389/fmed.2024.1384786
Received: 10 February 2024; Accepted: 06 May 2024;
Published: 15 May 2024.
Edited by:
Michael Tong, Australian National University, AustraliaReviewed by:
Lennart Reifels, The University of Melbourne, AustraliaCopyright © 2024 Jerjes. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Waseem Jerjes, d2FzZWVtLmplcmplc0BuaHMubmV0
 Waseem Jerjes
Waseem Jerjes