- 1Neuroscience-Inspired Policy Initiative, Organization for Economic Co-operation and Development (OECD) and the PRODEO Institute, Paris, France
- 2Global Brain Health Institute, University of California, San Francisco (UCSF), San Francisco, CA, United States
- 3Trinity College Dublin, Dublin, Ireland
- 4Department of Medicine, Stanford Hospital, Stanford, CA, United States
- 5The PRODEO Institute, San Francisco, CA, United States
- 6Cognitive Neuroscience Center (CNC), Universidad de San Andrés, Buenos Aires, Argentina
- 7Latin American Brain Health (BrainLat), Universidad Adolfo Ibáñez, Santiago, Chile
- 8National Scientific and Technical Research Council (CONICET), Buenos Aires, Argentina
- 9Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles (UCLA), Los Angeles, CA, United States
- 10The Institute for Mental and Physical Health and Clinical Translation (IMPACT), Deakin University, Geelong, VIC, Australia
- 11Department of Psychiatry, University of Melbourne, Melbourne, VIC, Australia
- 12Orygen Youth Health, University of Melbourne, Melbourne, VIC, Australia
- 13The Florey Institute for Neuroscience and Mental Health, University of Melbourne, Melbourne, VIC, Australia
- 14Department of Psychiatry and Behavioral Sciences, Baylor College of Medicine, Houston, TX, United States
Dementia prevention interventions that address modifiable risk factors for dementia require extensive lifestyle and behavior changes. Strategies are needed to enhance engagement and personalization of the experience at a population level. Precision Population Brain Health aims to improve brain health across the lifespan at a population level. Psychographic segmentation is a core component of Precision Population Brain Health with untapped potential. Psychographic segmentation applies behavioral and social sciences to understanding people’s motivations, values, priorities, decision making, lifestyles, personalities, communication preferences, attitudes, and beliefs. Integrating psychographic segmentation into dementia care could provide a more personalized care experience and increased patient engagement, leading to improved health outcomes and reduced costs. Psychographic segmentation can enhance patient engagement for dementia and shift the clinical paradigm from “What is the matter?” to “What matters to you?” Similar benefits of psychographic segmentation can be provided for dementia caregivers. Developing dementia prevention programs that integrate psychographic segmentation could become the basis for creating a shared framework for prevention of non-communicable diseases and brain health disorders at a population level. Integrating psychographic segmentation into digital health tools for dementia prevention programs is especially critical to overcome current suboptimal approaches. Applying psychographic segmentation to dementia prevention has the potential to help people feel a sense of empowerment over their health and improve satisfaction with their health experience—creating a culture shift in the way brain health is approached and paving the way toward Precision Population Brain Health.
Introduction
The dearth of clinically established dementia therapeutics emphasizes the importance of prevention approaches (Rabinovici, 2021). The 2020 Lancet Commission on dementia prevention, intervention, and care identified 12 modifiable risk factors for dementia and developed a life-course model of dementia prevention based on these factors (Livingston et al., 2020). The risk factors are less education, hypertension, hearing impairment, smoking, obesity, depression, physical inactivity, diabetes, low social contact, excessive alcohol consumption, traumatic brain injury (TBI), and air pollution (Livingston et al., 2020). Modifying these 12 risk factors might prevent or delay up to 40% of dementias and maybe even more in low-income and middle-income countries where around two-thirds of people with dementia live (Livingston et al., 2020; Patterson, 2018). Dementia prevention interventions that address modifiable risk factors for dementia, such as the Finnish geriatric intervention study to prevent cognitive impairment and disability (FINGER) (Ngandu et al., 2015), require extensive lifestyle and behavior changes. Consequently, strategies are needed to enhance engagement and personalization of the experience at a population level.
Precision Population Brain Health aims to improve brain health across the lifespan at a population level. It fuses Precision Brain Health (Fernandes et al., 2017; Frisoni et al., 2020) and Population Brain Health (UCSF Center for Population Brain Health, 2021). Engagement and personalization at a population level is key to Precision Population Brain Health. For Precision Population Brain Health to be achieved, insights from various disciplines must be combined. For example, for efforts such as widespread dementia prevention, platform technologies (e.g., telemedicine, apps) and frontier technologies (e.g., genomics, AI, robotics), creative care, culturally competent care, personalization techniques, and behavior design must be combined to address social determinants and other modifiable risk factors for dementia.
Psychographic segmentation is a core component of Precision Population Brain Health with untapped potential. Psychographic segmentation applies behavioral and social sciences to understanding people’s motivations, values, priorities, decision making, lifestyles, personalities, communication preferences, attitudes, and beliefs (Samuel, 2016). Complementing demographic and socioeconomic segmentation, psychographic segmentation enables people to be divided into sub-groups based on shared psychological characteristics. Since the 1970s, psychographic segmentation has been used by the world’s most successful consumer product and retail companies to understand and influence consumer behavior. It is commonly leveraged by the corporate sector to better understand employees and build more successful organizations. Psychographic segmentation has potential to improve dementia prevention initiatives and to provide a more ecological, decision making-oriented evaluation of both people with dementia and their caregivers.
Psychographic Segmentation for Health
Psychographic segmentation has only recently started to be used for healthcare applications. Currently, many healthcare programs are one-size-fits-all or are based on a shared diagnosis. This often does not lead to high adoption rates of recommended behaviors. This highlights a need for personalization, creating an opportunity for psychographic segmentation to increase patient engagement and improve outcomes (Hardcastle and Hagger, 2015). Applying psychographic segmentation to healthcare enables organizations within healthcare to understand—and classify accordingly—if individual consumers take a proactive or reactive approach to health and wellness; want many or few choices; want traditional and/or alternative medicine; prioritize others’ health and wellness over their own; and more. For example, if someone lives in the “here and now” and does not prioritize their long-term health, messages from a health system may be sent via text instead of email and include language that emphasizes living for today, clear first steps, and immediacy. Companies including Frame Health and PatientBond have been key to actioning and scaling psychographic segmentation within healthcare, including capturing psychographic data and integrating it into electronic health records (EMRs) and customer relationship management platforms (CRMs) (Frame Health, 2021; PatientBond, 2021a). In partnership with Frame Health for example, CVS, UnitedHealthcare, and Cedars-Sinai Medical Center were able to increase patient signups for a medication adherence program by 38% and decrease pharmacy all time by 22% using Frame Health’s personalized call strategies and scripts (Frame Health, 2020). As another example, in partnership with PatientBond, a top health system was able to reduce hospital readmissions for congestive heart failure by 90% using PatientBond’s digital system (PatientBond, 2020).
However, the use of psychographic segmentation for dementia—along with brain health more broadly—remains nascent. Integrating psychographic segmentation into dementia care could provide a more personalized care experience and increased patient engagement, leading to improved health outcomes and reduced costs (Laurance et al., 2014). Psychographic segmentation has the opportunity to enhance patient engagement for dementia and to “change the clinical paradigm from ‘What is the matter?’ to ‘What matters to you?”’ (Edgman-Levitan et al., 2013).
Psychographic Segmentation for Dementia Prevention
Due to the complex, multifactorial, and heterogeneous nature of dementia, there has been increasing interest in multidomain interventions for dementia prevention (Andrieu et al., 2015). Multidomain interventions target several risk factors and mechanisms simultaneously and may be required for optimal preventative effects (Rosenberg et al., 2020b). The first large-scale randomized controlled trials (RCTs) of multidomain interventions include the Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER) trial and the Multidomain Alzheimer Preventive Trial (MAPT).
In FINGER, participants received a 2-year multidomain lifestyle intervention consisting of physical training, cognitive training, nutritional counseling, and cardiovascular monitoring (Kivipelto et al., 2013; Ngandu et al., 2015). In MAPT, participants received a 3-year multidomain lifestyle intervention consisting of cognitive training, physical activity counseling, and nutritional counseling with either an omega-3 supplement or placebo (Andrieu et al., 2017). For multidomain interventions such as FINGER and MAPT, adherence is key (Coley et al., 2019). Greater personalization, such as considering participant characteristics and motivations and taking a precision prevention approach, is critical to increase adherence (Coley et al., 2019; Rosenberg et al., 2020a; Solomon et al., 2021). In other words, a psychographic segmentation approach to prevention is needed.
Psychographic segmentation has the potential to improve the adherence and effectiveness of multidomain interventions for dementia prevention. For instance, a few example segments of psychographic segmentation include the following (see Figure 1 for more) (PatientBond, 2021b): (1) Self-achiever, people who are highly receptive to health information; (2) priority juggler, people who are generally not engaged in getting health care information for themselves and whose family or peer influence is important; and (3) Willful endurers, people who live in the here and now and are least engaged with their health. The engagement strategies will need to be varied and personalized for each segment. For example, outreach materials and participation strategies for self-achievers may be centered around the theme of achieving a goal, whereas for priority jugglers, a sense of how the family/other people will benefit and evoking commitment and duty will be essential. For the willful endurers, messages that center around living for today and create a sense of urgency will be important. The method of communication may differ with certain segments preferring text messaging, emails, or physical mail. Different versions of dementia preventions programs could be developed for different psychographic profiles. Since dementia prevention requires multifactorial efforts across the lifespan, these methods of enhancing engagement and personalization through psychographic segmentation are key and a powerful addition to researchers’ and health providers’ toolkits.
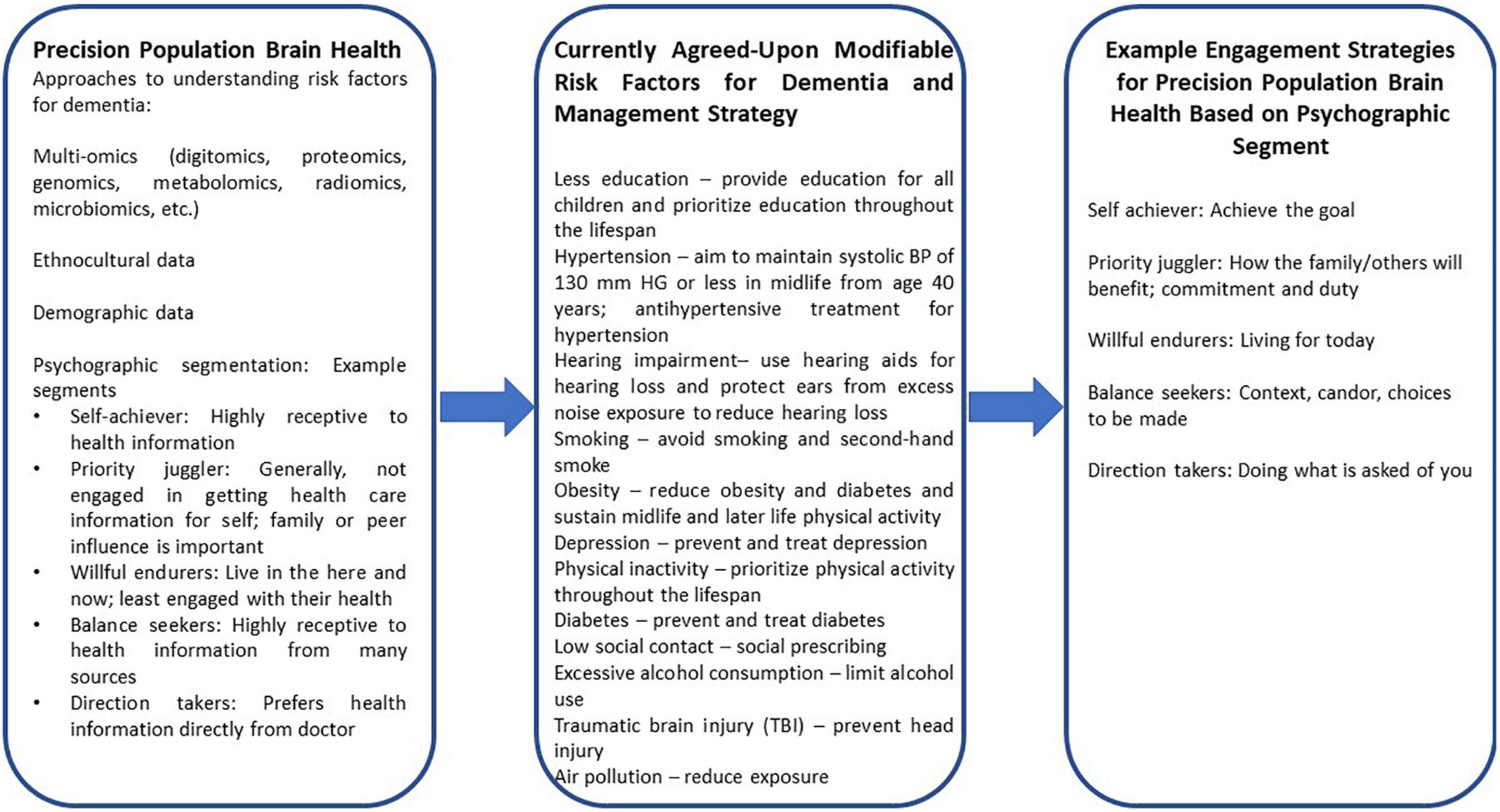
Figure 1. Examples of how psychographic segmentation can enable a Precision Population Brain Health approach to care through addressing modifiable risk factors of dementia and enhancing patient engagement.
Psychographic Segmentation for Digital Technologies for Dementia
Both in-person and digital dementia prevention programs could extensively benefit by integrating psychometric segmentation into their approach. With the proliferation of digital health tools for dementia prevention programs, it is especially important to integrate psychographic segmentation into these technologies. When describing hallmarks of digital health initiatives that have not lived up to their potential, Dr. Brennan Spiegel, Director of Health Services Research at Cedars-Sinai Health System, points toward not giving patients optimal messaging, not inviting patients in the most compelling way, and a lack of patient engagement as being problematic (Fry and Mukherjee, 2018) – all of which could have been helped by psychographic segmentation. He further noted that with digital health tools “Creating the tech isn’t the hard part…the hard part is using the tech to change patient behavior” (Pagoto and Hekler, 2018). Psychometric segmentation is highly compatible with current applications of behavioral insights across the health system, especially for nudging (Hansen et al., 2016; Benartzi et al., 2017). Such interventions can be boosted by the development behavioral research in policy domains to increase effectiveness, economic growth, and competitiveness (Sunstein, 2016). The combination of technology and psychometry are a powerful force to change behavior that should be ethically addressed to avoid technocracy and “psychocracy” (Feitsma, 2018). Integrating psychometric segmentation into digital health tools for dementia may help address these challenges.
Psychographic Segmentation for Caregivers
Psychographic segmentation can also improve the lives of caregivers for people with dementia. For example, a recent study explored how people balance caregiving with other family and employment responsibilities by considering their personal characteristics and their informal caregiving network (Neubert et al., 2018). Applying psychographic segmentation could expand this study and lead to a more comprehensive understanding of a caregiver’s needs. Additionally, better understanding of a caregiver’s motivations and personality through psychographic segmentation can be used to develop personalized strategies to mitigate caregiver burden and prevent burnout.
Conclusion
Applying psychometric segmentation to dementia prevention endeavors can improve the entire spectrum of care. Psychometric segmentation accounts for an individual’s unique values, motivations, priorities, lifestyle, personality, and beliefs as well as behavioral change. Thus, personalization and patient engagement can be at the heart of care. In addition to improved health outcomes and reduced costs due to dementia, developing dementia prevention programs that integrate psychographic segmentation could become the basis for creating a shared framework for prevention of non-communicable diseases and brain health disorders at a population level (O’Neil et al., 2015). Applying psychometric segmentation to dementia prevention endeavors has the potential to help people feel a sense of empowerment over their health and improve satisfaction with their health experience—creating a culture shift in the way brain health is approached and paving the way toward Precision Population Brain Health.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
ES led the manuscript development. ES and HE co-developed the idea that led to the beginning of this manuscript. All authors contributed to the idea development, writing, and editing of this manuscript and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Andrieu, S., Coley, N., Lovestone, S., Aisen, P. S., and Vellas, B. (2015). Prevention of sporadic Alzheimer’s disease: lessons learned from clinical trials and future directions. Lancet Neurol. 14, 926–944. doi: 10.1016/S1474-4422(15)00153-2
Andrieu, S., Guyonnet, S., Coley, N., Cantet, C., Bonnefoy, M., and Bordes, S. (2017). Effect of long-term omega 3 polyunsaturated fatty acid supplementation with or without multidomain intervention on cognitive function in elderly adults with memory complaints (MAPT): a randomised, placebo-controlled trial. Lancet Neurol. 16, 377–389. doi: 10.1016/S1474-4422(17)30040-6
Benartzi, S., Beshears, J., Milkman, K. L., Sunstein, C. R., Thaler, R. H., Shankar, M., et al. (2017). Should governments invest more in nudging? Psychol. Sci. 28, 1041–1055. doi: 10.1177/0956797617702501
Coley, N., Ngandu, T., Lehtisalo, J., Soininen, H., Vellas, B., Richard, E., et al. (2019). Adherence to multidomain interventions for dementia prevention: data from the FINGER and MAPT trials. Alzheimers Dement. 15, 729–741. doi: 10.1016/j.jalz.2019.03.005
Edgman-Levitan, S., Brady, C., and Howitt, P. (2013). “Partnering with patients, families, and communities for health: A global imperative,” in Report of The Patient and Family Engagement Working Group 2013, Doha.
Feitsma, J. N. P. (2018). The behavioural state: critical observations on technocracy and psychocracy. Policy Sci. 51, 387–410. doi: 10.1007/s11077-018-9325-5
Fernandes, B. S., Williams, L. M., Steiner, J., Leboyer, M., Carvalho, A. F., and Berk, M. (2017). The new field of ‘precision psychiatry’. BMC Med. 15:80. doi: 10.1186/s12916-017-0849-x
Frame Health (2021). Available online at: https://www.framehealth.com/ (accessed September 2, 2021).
Frame Health (2020). Frame Health Case Study: Persona-Based Communication Increases Patient Enrollment In A CVS, UnitedHealthcare, And Cedars-Sinai Medication Adherence Program. 2020. Available online at: https://www.framehealth.com/health-plans/ (accessed September 2, 2021).
Frisoni, G. B., Molinuevo, J. L., Altomare, D., Carrera, E., Barkhof, F., Berkhof, J., et al. (2020). Precision prevention of Alzheimer’s and other dementias: anticipating future needs in the control of risk factors and implementation of disease-modifying therapies. Alzheimers Dement. 16, 1457–1468. doi: 10.1002/alz.12132
Fry, E., and Mukherjee, S. (2018). Tech’s Next Big Wave: Big Data Meets Biology. Available online at: https://fortune.com/2018/03/19/big-data-digital-health-tech/ (accessed September 2, 2021).
Hansen, P. G., Skov, L. R., and Skov, K. L. (2016). Making healthy choices easier: regulation versus nudging. Annu. Rev. Public Health 37, 237–251. doi: 10.1146/annurev-publhealth-032315-021537
Hardcastle, S. J., and Hagger, M. S. (2015). Psychographic profiling for effective health behavior change interventions. Front. Psychol. 6:1988. doi: 10.3389/fpsyg.2015.01988
Kivipelto, M., Solomon, A., Ahtiluoto, S., Ngandu, T., Lehtisalo, J., Antikainen, R., et al. (2013). The Finnish Geriatric Intervention Study to Prevent Cognitive Impairment and Disability (FINGER): study design and progress. Alzheimers Dement. 9, 657–665. doi: 10.1016/j.jalz.2012.09.012
Laurance, J., Henderson, S., Howitt, P. J., Matar, M., Al Kuwari, H., Edgman-Levitan, S., et al. (2014). Patient engagement: four case studies that highlight the potential for improved health outcomes and reduced costs. Health Affairs 33, 1627–1634. doi: 10.1377/hlthaff.2014.0375
Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., Banerjee, S., et al. (2020). Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 396, 413–446. doi: 10.1016/S0140-6736(20)30367-6
Neubert, L., König, H. H., and Brettschneider, C. (2018). Seeking the balance between caregiving in dementia, family and employment: study protocol for a mixed methods study in Northern Germany. BMJ Open 8:e019444. doi: 10.1136/bmjopen-2017-019444
Ngandu, T., Lehtisalo, J., Solomon, A., Levälahti, E., Ahtiluoto, S., Antikainen, R., et al. (2015). A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomised controlled trial. Lancet 385, 2255–2263. doi: 10.1016/S0140-6736(15)60461-5
O’Neil, A., Jacka, F. N., Quirk, S. E., Cocker, F., Taylor, C. B., Oldenburg, B., et al. (2015). A shared framework for the common mental disorders and non-communicable disease: key considerations for disease prevention and control. BMC Psychiatr. 15:15. doi: 10.1186/s12888-015-0394-0
Pagoto, S., and Hekler, E. (2018). Is Digital Health A Behavioral Science?. Available online at: https://medcitynews.com/2018/05/is-digital-health-a-behavioral-science/?rf=1 (accessed September 2, 2021).
PatientBond (2021a). Available online at: https://www.patientbond.com/ (accessed September 2, 2021).
PatientBond (2021b). Psychographic Segmentation and its Practical Application in Patient Engagement and Behavior Change: A PatientBond Whitepaper. Holladay, UT: PatientBond.
PatientBond (2020). Patient Bond Case Study: Breakthroughs in Patient Engagement and Behavior Change- Reducing Hospital Readmissions and Promoting Prevention of Cardiovascular Events. Holladay, UT: PatientBond.
Rabinovici, G. D. (2021). Controversy and progress in Alzheimer’s Disease-FDA approval of aducanumab. N. Engl. J. Med. 385, 771–774. doi: 10.1056/NEJMp2111320
Rosenberg, A., Mangialasche, F., Ngandu, T., Solomon, A., and Kivipelto, M. (2020b). Multidomain interventions to prevent cognitive impairment. alzheimer’s disease, and dementia: from FINGER to World-Wide FINGERS. J. Prev. Alzheimers Dis. 7, 29–36. doi: 10.14283/jpad.2019.41
Rosenberg, A., Coley, N., Soulier, A., Kulmala, J., Soininen, H., Andrieu, S., et al. (2020a). Experiences of dementia and attitude towards prevention: a qualitative study among older adults participating in a prevention trial. BMC Geriatr. 20:99. doi: 10.1186/s12877-020-1493-4
Samuel, A. (2016). Psychographics are just as important for marketers as demographics. Harv. Bus. Rev. 11:1.
Solomon, A., Stephen, R., Altomare, D., Carrera, E., Frisoni, G. B., Kulmala, J., et al. (2021). Multidomain interventions: state-of-the-art and future directions for protocols to implement precision dementia risk reduction. a user manual for Brain Health Services—part 4 of 6. Alzheimers Res. Ther. 13, 1–15. doi: 10.1186/s13195-021-00875-8
Sunstein, C. R. (2016). The council of psychological advisers. Annu. Rev. Psychol. 67, 713–737. doi: 10.1146/annurev-psych-081914-124745
UCSF Center for Population Brain Health (2021). Available online at: https://popbrain.ucsf.edu/ (accessed September 2, 2021).
Keywords: psychographic segmentation, precision/personalized medicine, population health, dementia prevention, patient engagement
Citation: Smith E, Ibanez A, Lavretsky H, Berk M and Eyre HA (2021) Psychographic Segmentation: Another Lever for Precision Population Brain Health. Front. Aging Neurosci. 13:783297. doi: 10.3389/fnagi.2021.783297
Received: 25 September 2021; Accepted: 19 November 2021;
Published: 08 December 2021.
Edited by:
Frauke Beyer, Max Planck Institute for Human Cognitive and Brain Sciences, GermanyReviewed by:
Ruth Stephen, University of Eastern Finland, FinlandCraig Speelman, Edith Cowan University, Australia
Copyright © 2021 Smith, Ibanez, Lavretsky, Berk and Eyre. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Erin Smith, ZXJpbi5zbWl0aEBnYmhpLm9yZw==
 Erin Smith
Erin Smith Agustin Ibanez
Agustin Ibanez Helen Lavretsky
Helen Lavretsky Michael Berk
Michael Berk Harris A. Eyre
Harris A. Eyre