- 1Department of Biomedical and Biotechnological Sciences, University of Catania, Catania, Italy
- 2Department of Clinical and Experimental Medicine, University of Messina, Messina, Italy
Pituitary adenylate cyclase-activating polypeptide (PACAP) modulates glutamatergic synaptic transmission and plasticity in the hippocampus, a brain area with a key role in learning and memory. In agreement, several studies have demonstrated that PACAP modulates learning in physiological conditions. Recent publications show reduced PACAP levels and/or alterations in PACAP receptor expression in different conditions associated with cognitive disability. It is noteworthy that PACAP administration rescued impaired synaptic plasticity and learning in animal models of aging, Alzheimer’s disease, Parkinson’s disease, and Huntington’s chorea. In this context, results from our laboratory demonstrate that PACAP rescued metabotropic glutamate receptor-mediated synaptic plasticity in the hippocampus of a mouse model of fragile X syndrome (FXS), a genetic form of intellectual disability. PACAP is actively transported through the blood–brain barrier and reaches the brain following intranasal or intravenous administration. Besides, new studies have identified synthetic PACAP analog peptides with improved selectivity and pharmacokinetic properties with respect to the native peptide. Our review supports the shared idea that pharmacological activation of PACAP receptors might be beneficial for brain pathologies with cognitive disability. In addition, we suggest that the effects of PACAP treatment might be further studied as a possible therapy in FXS.
Introduction
Pituitary adenylate cyclase-activating polypeptide (PACAP) was initially discovered in ovine hypothalamus as an endocrine regulator (Miyata et al., 1989). PACAP is highly expressed in the brain and in peripheral tissues in two forms of 38 and 27 amino acid residues, PACAP-38 and PACAP-27 (Arimura et al., 1991; Koves et al., 1991). In the present review, “PACAP” refers to PACAP-38, the most abundant form in the brain (Arimura et al., 1991; Vaudry et al., 2009). We will specifically indicate PACAP-38 and PACAP-27 to underline differences between the two forms.
Pituitary adenylate cyclase-activating polypeptide activates two main classes of G protein-coupled receptors: PAC1 and VPAC (Vaudry et al., 2009). PAC1 is PACAP specific, with a high nanomolar affinity for PACAP and a 1,000-fold lower affinity for the structurally related vasoactive intestinal peptide (VIP). VPAC receptors include VPAC1 and VPAC2 subtypes, with equally high nanomolar affinity for PACAP and VIP. PAC1 and VPAC receptors are expressed in peripheral tissues and in the central nervous system (CNS), where PAC1 is the most abundant (Jolivel et al., 2009). All PACAP/VIP receptors are positively coupled to adenylate cyclase; PAC1 receptors can also activate phospholipase C and Ca2+ release. The brain localization, pharmacological features, signal transduction mechanisms, and biological effects of PACAP/VIP receptors are described in details in excellent reviews (Dickson and Finlayson, 2009; Vaudry et al., 2009; Harmar et al., 2012; Hirabayashi et al., 2018).
In the CNS, PACAP is a neurotrophic and a neuroprotective factor regulating differentiation of neuronal precursors, promoting neuronal survival, and exerting neuroprotective effects after brain damage (Arimura et al., 1994; Shioda and Nakamachi, 2015; Reglodi et al., 2018c). Acting on the brain, PACAP also regulates important physiological functions, among which are feeding (Sekar et al., 2017), circadian rhythm (Holland et al., 2018), body temperature (Tan et al., 2016), learning, and memory (see below). We will initially describe the physiological role of PACAP on learning and then highlight recent findings showing an involvement of PACAP in cognitive disability. Finally, we will discuss the possibility to use PACAP as a pharmacological tool in conditions of learning impairment.
Pituitary Adenylate Cyclase-Activating Polypeptide Modulates Hippocampal Synaptic Transmission, Synaptic Plasticity, and Learning in Physiological Conditions
Pituitary adenylate cyclase-activating polypeptide receptors are highly expressed in rat hippocampus (Shioda et al., 1997; Jaworski and Proctor, 2000; Joo et al., 2004). On cultured hippocampal neurons, PACAP stimulated axon outgrowth (Ogata et al., 2015) and increased the size and density of dendritic spines (Hayata-Takano et al., 2019). Accordingly, PACAP-deficient mice displayed a reduced hippocampal spine density with respect to wild type (Hayata-Takano et al., 2019), indicating an important role of PACAP on synapse formation.
Pituitary adenylate cyclase-activating polypeptide increases the firing rate of hippocampal neurons (Di Mauro et al., 2003; Liu et al., 2003) and inhibits potassium currents responsible for membrane repolarization (Taylor et al., 2014; Gupte et al., 2015), which likely accounts for PACAP-induced increase in intrinsic excitability. Importantly, PACAP modulates hippocampal synaptic transmission and plasticity (Yang et al., 2010) and hippocampus-dependent learning (Borbely et al., 2013). In CA1 neurons, PACAP dose dependently modulates glutamate-mediated transmission (Kondo et al., 1997; Roberto et al., 2001; Ciranna and Cavallaro, 2003; Ster et al., 2009), exerting different effects on AMPA (Costa et al., 2009; Toda and Huganir, 2015) and NMDA receptor-mediated synaptic responses (Yaka et al., 2003; Macdonald et al., 2005). PACAP also stimulates acetylcholine release in the rodent hippocampus (Masuo et al., 1993), which in turn affects glutamate-mediated transmission (Roberto and Brunelli, 2000; Roberto et al., 2001; Pecoraro et al., 2017).
Pituitary adenylate cyclase-activating polypeptide-deficient mice show reduced long-term depression (LTP) in the dentate gyrus (Matsuyama et al., 2003) and impaired memory (Ago et al., 2013; Takuma et al., 2014). Impaired hippocampal LTP was also observed in PAC1 receptor-deficient mice (Otto et al., 2001; Matsuyama et al., 2003), together with a specific deficit in contextual fear conditioning, an index of associative memory, but not in Morris water maze test performance, indicative of spatial discrimination (Sauvage et al., 2000; Otto et al., 2001). In wild-type rats, intravenous injection of PACAP improved spatial memory (Ladjimi et al., 2019); direct infusion of PACAP in the hippocampus and amygdala improved learning in contextual fear conditioning (Schmidt et al., 2015); intracerebroventricular administration of PACAP exerted bi-directional effects (initial impairment and later improvement) on fear conditioning memory (Meloni et al., 2016, 2018) and, at low doses, improved learning in passive avoidance response test (Sacchetti et al., 2001).
Dysregulation of Pituitary Adenylate Cyclase-Activating Polypeptide Functions in Conditions of Cognitive Impairment
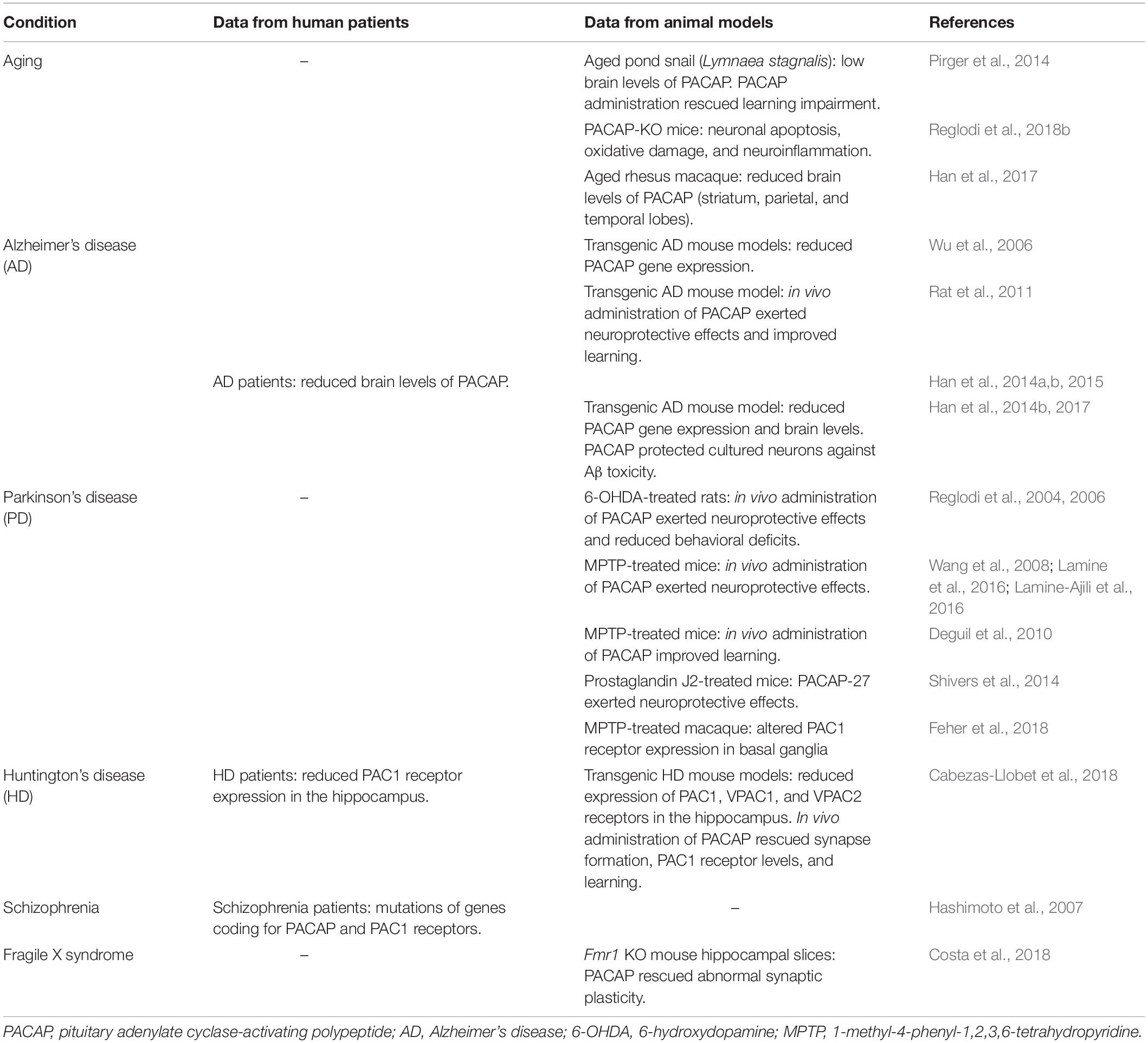
Recent studies show reduced brain levels of PACAP and/or altered PACAP receptor expression in cognitive deficit (Table 1). PACAP-KO mice display neuronal apoptosis, oxidative damage, and neuroinflammation similar to those observed at old age; thus, PACAP deficiency has been proposed as a model of premature aging (Reglodi et al., 2018b). Accordingly, age-related cognition impairment was associated with reduced levels of PACAP in rhesus macaque brain (Han et al., 2017) and in an invertebrate model of aging, in which memory loss was rescued by activation of PAC1 receptors (Pirger et al., 2014).
Defects in PACAP-mediated functions are well documented in Alzheimer’s disease (AD), the most devastating neurodegenerative disease leading to memory loss and dementia. Reduced PACAP levels were observed in the brain of different transgenic AD mouse models (Wu et al., 2006; Han et al., 2014b, 2017) and in cortical brain samples from AD patients, where PACAP levels were inversely related to the amount of amyloid plaques and neurofibrillary tangle, as well as to dementia rating scores (Han et al., 2014a). Reduced PACAP levels and altered PAC1 receptor expression in the brain of AD patients were detected since early stages of the progressive neurodegeneration characterized by mild cognitive impairment (Han et al., 2015). Interestingly, besides exerting a neuroprotective role, PACAP stimulates a non-amyloidogenic processing pathway of amyloid precursor protein (APP) (Kojro et al., 2006), suggesting that PACAP might be used in AD therapy. Administration of PACAP has proven to be effective against Aβ-induced toxicity in different AD mouse models (Rat et al., 2011; Han et al., 2014b). Intranasal administration of PACAP to APP-transgenic mice increased brain expression of PACAP and PACAP receptors, stimulated the production of neurotrophic and antiapoptotic factors [brain-derived neurotrophic factor (BDNF) and Bcl-2], enhanced the expression of the Aβ-degrading enzyme neprilysin, and improved learning (Rat et al., 2011). Accordingly, VIP decreased amyloid plaques and prevented brain atrophy in the 5xFAD mouse model of AD (Korkmaz et al., 2018). The same authors suggest that VIP-mediated neuroprotective effects might also be used for therapy of Parkinson’s disease (PD) (Korkmaz and Tuncel, 2018).
Parkinson’s disease, a neurodegenerative disorder characterized by loss of dopaminergic neurons in the substantia nigra, primarily affects motor control and also involves cognition deficit (Aarsland et al., 2017). A new study shows a decreased PAC1 receptor expression in basal ganglia in a macaque model of PD (Feher et al., 2018), suggesting that reduced PACAP function contributes to neurodegeneration and PACAP might become a promising tool for PD therapy (Reglodi et al., 2017). Administration of PACAP to rats treated with the neurotoxin 6-hydroxydopamine (6-OHDA), a model of PD, prevented degeneration of nigral dopaminergic neurons and rescued behavioral deficits (Reglodi et al., 2004, 2006). Likewise, in a different murine PD model [mice treated with 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)], intravenous injection of PACAP-27 prevented neuronal loss in the substantia nigra (Wang et al., 2008) and rescued learning deficit (Deguil et al., 2010). Still in MPTP-treated mice, PACAP treatment exerted neuroprotective effects in the substantia nigra (Lamine et al., 2016) and reduced abnormal autophagy, a mechanism that might contribute to neuronal death (Lamine-Ajili et al., 2016). PACAP-27 also prevented dopaminergic neuronal loss and motor deficit in prostaglandin J2-treated mice, another proposed PD model (Shivers et al., 2014).
A reduced expression of all PACAP receptor subtypes was observed in two different mouse models of Huntington’s disease (HD), an inherited degenerating motor and cognitive disease, and PAC1 receptors were downregulated in postmortem hippocampal samples from HD patients (Cabezas-Llobet et al., 2018). Remarkably, intranasal administration of PACAP to HD mice increased PAC1 receptor expression, stimulated BDNF production, reduced the formation of huntingtin aggregates, prevented the loss of hippocampal glutamatergic synapses, and improved memory (Cabezas-Llobet et al., 2018).
Finally, mutations of the genes coding for PACAP and for PAC1 receptors were found in schizophrenic patients together with reduced hippocampal volume and impaired memory (Hashimoto et al., 2007). Schizophrenia involves dysregulation of brain dopaminergic system (Weinstein et al., 2017). Interestingly, genetic ablation of D3 receptors increased the expression of PACAP and PACAP receptors in mouse hippocampus and enhanced memory (Marzagalli et al., 2016), suggesting a close interplay between PACAP and dopamine on learning and memory.
Pituitary Adenylate Cyclase-Activating Polypeptide Rescues Synaptic Plasticity in a Mouse Model of Fragile X Syndrome
Fragile X syndrome (FXS) is a genetic form of intellectual disability affecting 1/4,000 males and 1/6,000 females. FXS patients show cognitive and language deficits; subgroups of patients also display autistic features, epilepsy, attention deficit and hyperactivity disorder (ADHD), and mood disorders (Bardoni et al., 2006; Maurin et al., 2014; Gross et al., 2015; Hagerman et al., 2017). FXS is caused by transcriptional silencing of the FMR1 gene coding for fragile X mental retardation protein (FMRP) (Verkerk et al., 1991), an mRNA-binding protein mostly functioning as a repressor (Garber et al., 2006) and in some cases as an enhancer (Bechara et al., 2009) of protein translation (Darnell and Klann, 2013). Hundreds of mRNAs have been identified as FMRP targets, particularly mRNAs coding for proteins involved in synapse development and function (Bassell and Warren, 2008; Bear et al., 2008). Cortical neurons from Fmr1 knock out (Fmr1 KO) animal models of FXS (Comery et al., 1997) and FXS patients (Irwin et al., 2000) display an increased density of dendritic spines, with a long and thin morphology reminiscent of immature filopodia. Abnormal dendritic spine morphology has crucial consequences on synaptic function. Many alterations of glutamate-mediated synaptic transmission and plasticity were found in the brain of Fmr1 KO mice. Among the first discovered, hippocampal LTP induced by metabotropic glutamate receptors (mGluR-LTD) is abnormally enhanced (Huber et al., 2002). Exaggerated mGluR-LTD led to formulation of the “mGluR theory” of FXS, pointing out excessive signaling downstream activation of mGluRs (Bear et al., 2004). In Fmr1 KO neurons, mGluRs also show altered cell-surface mobility, abnormal coupling to NMDA receptors, and impaired mGluR-LTD of NMDA-mediated synaptic currents (Aloisi et al., 2017). Other malfunctions of glutamatergic synapses in Fmr1 KO mouse brain include a reduced coupling of mGluRs to Homer proteins (Giuffrida et al., 2005), a reduced NMDA/AMPA ratio (Yun and Trommer, 2011; Gocel and Larson, 2012; Aloisi et al., 2017), and altered NMDA-dependent plasticity (Uzunova et al., 2014; Bostrom et al., 2015). An increased expression of Ca2+-permeable AMPA receptors was recently found in human neural precursors derived from FXS patients (Achuta et al., 2018). Inhibitory synapses are also affected in the brain of FXS animal models, with a deficit of GABAergic inhibition (Martin et al., 2014; Braat and Kooy, 2015) and abnormal functioning of GABAA receptors (He et al., 2014).
At a cellular level, FMRP absence is associated with dysregulation of many signaling pathways, among which upregulation of PI3K/Akt/mTOR pathway (Sharma et al., 2010; Huber et al., 2015), overactivation of GSK3 (Min et al., 2009), and altered MAPK/ERK signaling (Kim et al., 2008; Osterweil et al., 2010). The large amount of data now available on the molecular basis of FXS provides several cues for a possible therapy of FXS, currently under investigation (Santoro et al., 2012; Sethna et al., 2014; Gross et al., 2015; Castagnola et al., 2017). Each proposed strategy might be useful in subsets of FXS patients, owing to a large individual heterogeneity with respect to the type and severity of symptoms (Jacquemont et al., 2014).
Interestingly, early observations on FXS patients and latest findings on FXS animal models have pointed out a downregulation of the cyclic adenosine monophosphate (cAMP) pathway, originating a “cAMP theory” of FXS (Kelley et al., 2008). A recent study shows that the mRNA coding for phosphodiesterase 2A (PDE2A), a cAMP-degrading enzyme, is among the most prominent targets of FMRP (Maurin et al., 2018a). In the brain of Fmr1 KO mice, PDE2A is overexpressed and overactive, causing reduced cAMP formation and dysregulation of cAMP downstream signaling (Maurin et al., 2018b). In line with this, synaptic plasticity, learning, and behavior in Fmr1 KO mice are rescued by agonists of serotonin 5-HT7 receptors, positively coupled to adenylate cyclase (Costa et al., 2012, 2015, 2018; Ciranna and Catania, 2014), by PDE4 inhibitors (Choi et al., 2015, 2016), and by a selective PDE2A inhibitor (Maurin et al., 2018b). Of note, inhibition of PDE2A also corrected abnormal dendritic spine morphology of cortical neurons from Fmr1 KO mice (Maurin et al., 2018b). All these data confirm a deficit in cAMP-mediated signaling in Fmr1 KO neurons and demonstrate that pharmacological manipulations increasing cAMP levels can rescue synaptic morphology and function, learning, and behavior in animal models of FXS.
Pituitary adenylate cyclase activating polypeptide is a potent stimulator of adenylate cyclase activity (Miyata et al., 1989; Vaudry et al., 2009). Consistent with the cAMP hypothesis of FXS, we found that PACAP reversed mGluR-LTD in the CA3-CA1 hippocampal synapse in wild-type mice and reduced exaggerated mGluR-LTD in Fmr1 KO, thus correcting a synaptic defect typically observed in FXS mouse models (Costa et al., 2018). This result offers novel suggestions for a possible therapy of FXS, for which no specific cure is presently available. In future studies, it would be interesting to test if PACAP can correct other abnormal features in Fmr1 KO neurons (dendrite development, synapse formation and function, ion channel expression, membrane excitability, and intracellular signaling) and rescue learning and behavior when administered in vivo to Fmr1 KO mice.
Dysregulation of cyclic nucleotide pathways was found at different levels (synthesis, functioning, and/or degradation by PDE) in aging and age-related cognitive decline (Kelly, 2018). Accordingly, inhibition of PDE activity improved memory in animal models of AD (Gulisano et al., 2018) and HD (Saavedra et al., 2013) and seems to prevent memory loss in elderly humans and in AD patients (Prickaerts et al., 2017). As indicated above, in FXS, the cAMP pathway is also dysregulated, and increasing cAMP rescues several phenotypes. Therefore, altered cAMP signaling might be a common feature in cognitive deficits of very different origin, in which administration of PACAP might be beneficial.
Systemic Administration Routes for Effective Brain Delivery of Pituitary Adenylate Cyclase-Activating Polypeptide
Pituitary adenylate cyclase activating polypeptide-38 is actively transported into the brain across the blood–brain barrier (BBB) by a saturable carrier, whereas PACAP-27 passes the BBB by transmembrane diffusion (Banks et al., 1993). After intravenous administration, the amount of PACAP-38 brain uptake was high enough to exert neuroprotective effects (Banks et al., 1996). The rate of PACAP-38 transport varies largely in different brain areas, with maximal uptake in the hypothalamus and in the hippocampus (Nonaka et al., 2002), and can be altered in pathological conditions (Banks et al., 1998; Nonaka et al., 2002; Rhea et al., 2018).
On the other side, PACAP-38 and PACAP-27 are transported out of the brain by a common efflux mechanism, reducing their brain levels (Banks et al., 1993). It is noteworthy that antisense inhibition of peptide transport system-6 (PTS-6) improved brain uptake and neuroprotective effects of PACAP-27 in murine models of AD and stroke (Dogrukol-Ak et al., 2009), suggesting that inhibition of PTS-6 efflux component might become a therapeutic strategy to enhance central effects of PACAP.
Some issues were raised about intravenous administration of PACAP to humans: PACAP-38 induced headache in healthy and migraine-suffering subjects (Schytz et al., 2009). Headache was also reported after intravenous infusion of PACAP-27 to healthy subjects (Ghanizada et al., 2019a) and migraine patients (Ghanizada et al., 2019b).
Other issues against intravenous administration of PACAP concern metabolic stability and selectivity. In fact, PACAP-38 showed a very short half-life (<5 min) in human plasma in vitro, being converted by the blood enzyme dipeptidyl peptidase IV into shorter peptides that behave as PACAP receptor antagonists, whereas PACAP-27 was relatively stable (Bourgault et al., 2008).
Besides, parenteral administration of PACAP can induce undesired peripheral actions, among which are cardiovascular (Runcie et al., 1995; Farnham et al., 2012) and hormonal effects (Tsutsumi et al., 2002). To overcome these limitations, new synthetic agonists of PACAP receptors have been developed with improved metabolic stability, higher brain uptake, selectivity for PAC1 receptors (the predominant PACAP receptors in the CNS), and reduced side effects (Bourgault et al., 2008; Dejda et al., 2011; Doan et al., 2011; Lamine et al., 2016).
Another strategy exploits conjugation of PACAP with a TAT peptide, improving passage through the BBB (Yu et al., 2012a, b). Carrier vesicles can also be used to protect peptides from blood-degrading enzymes (Dufes et al., 2004).
Administration routes for brain delivery of PACAP are illustrated in details in a recent review (Reglodi et al., 2018a). A promising non-invasive and easy route is intranasal application, by which PACAP reaches the brain fast and effectively in rodents, exerting neuroprotective effects in mouse models of AD (Rat et al., 2011; Nonaka et al., 2012) and HD (Cabezas-Llobet et al., 2018). Intranasal administration of PACAP was also tested on human volunteers, showing good safety and tolerability (Doberer et al., 2007; Reglodi et al., 2018a) with only mild local adverse reactions (Kinhult et al., 2003). Interestingly, headache was not reported after intranasal application of PACAP-38 (Doberer et al., 2007), suggesting this route as a valuable alternative to intravenous administration.
Concluding Remarks
Pituitary adenylate cyclase activating polypeptide plays an important role in learning and has a therapeutic potential in cognition deficits associated with disruption of cyclic nucleotide signaling. We suggest that the effects of PACAP might also be studied for a possible therapy of FXS, in which a deficit in cAMP formation and downstream signaling were evidenced. For future translational applications, it would be interesting to test in vivo effects of PACAP on learning and behavioral deficits in FXS animal models.
Pituitary adenylate cyclase activating polypeptide is brain permeant and has already proved to be safe on healthy humans and thus might be tested in clinical trials. To improve PACAP brain uptake, it would be worth focusing on new selective PAC1 receptor agonists with enhanced metabolic stability, on delivery carriers, and/or on suitable administration routes.
Author Contributions
LCi designed and directed the research projects and wrote the manuscript. LCo performed the experiments and data analysis, and contributed to the manuscript preparation.
Funding
The present work was financed by Telethon Foundation (grant GGP13145) and by Università di Catania, Italy (grant Chance 2017).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Aarsland, D., Creese, B., Politis, M., Chaudhuri, K. R., Ffytche, D. H., Weintraub, D., et al. (2017). Cognitive decline in Parkinson disease. Nat. Rev. Neurol. 13, 217–231. doi: 10.1038/nrneurol.2017.27
Achuta, V. S., Moykkynen, T., Peteri, U. K., Turconi, G., Rivera, C., Keinanen, K., et al. (2018). Functional changes of AMPA responses in human induced pluripotent stem cell-derived neural progenitors in fragile X syndrome. Sci. Signal 11:eaan8784. doi: 10.1126/scisignal.aan8784
Ago, Y., Hiramatsu, N., Ishihama, T., Hazama, K., Hayata-Takano, A., Shibasaki, Y., et al. (2013). The selective metabotropic glutamate 2/3 receptor agonist MGS0028 reverses psychomotor abnormalities and recognition memory deficits in mice lacking the pituitary adenylate cyclase-activating polypeptide. Behav. Pharmacol. 24, 74–77. doi: 10.1097/FBP.0b013e32835cf3e5
Aloisi, E., Le Corf, K., Dupuis, J., Zhang, P., Ginger, M., Labrousse, V., et al. (2017). Altered surface mGluR5 dynamics provoke synaptic NMDAR dysfunction and cognitive defects in Fmr1 knockout mice. Nat. Commun. 8:1103. doi: 10.1038/s41467-017-01191-2
Arimura, A., Somogyvari-Vigh, A., Miyata, A., Mizuno, K., Coy, D. H., and Kitada, C. (1991). Tissue distribution of PACAP as determined by RIA: highly abundant in the rat brain and testes. Endocrinology 129, 2787–2789. doi: 10.1210/endo-129-5-2787
Arimura, A., Somogyvari-Vigh, A., Weill, C., Fiore, R. C., Tatsuno, I., Bay, V., et al. (1994). PACAP functions as a neurotrophic factor. Ann. N. Y. Acad. Sci. 739, 228–243. doi: 10.1111/j.1749-6632.1994.tb19825.x
Banks, W. A., Kastin, A. J., and Arimura, A. (1998). Effect of spinal cord injury on the permeability of the blood-brain and blood-spinal cord barriers to the neurotropin PACAP. Exp. Neurol. 151, 116–123. doi: 10.1006/exnr.1998.6786
Banks, W. A., Kastin, A. J., Komaki, G., and Arimura, A. (1993). Passage of pituitary adenylate cyclase activating polypeptide1-27 and pituitary adenylate cyclase activating polypeptide1-38 across the blood-brain barrier. J. Pharmacol. Exp. Ther. 267, 690–696.
Banks, W. A., Uchida, D., Arimura, A., Somogyvari-Vigh, A., and Shioda, S. (1996). Transport of pituitary adenylate cyclase-activating polypeptide across the blood-brain barrier and the prevention of ischemia-induced death of hippocampal neurons. Ann. N. Y. Acad. Sci. 805, 270–277. doi: 10.1111/j.1749-6632.1996.tb17489.x
Bardoni, B., Davidovic, L., Bensaid, M., and Khandjian, E. W. (2006). The fragile X syndrome: exploring its molecular basis and seeking a treatment. Expert Rev. Mol. Med. 8, 1–16. doi: 10.1017/s1462399406010751
Bassell, G. J., and Warren, S. T. (2008). Fragile X syndrome: loss of local mRNA regulation alters synaptic development and function. Neuron 60, 201–214. doi: 10.1016/j.neuron.2008.10.004
Bear, M. F., Dolen, G., Osterweil, E., and Nagarajan, N. (2008). Fragile X: translation in action. Neuropsychopharmacology 33, 84–87. doi: 10.1038/sj.npp.1301610
Bear, M. F., Huber, K. M., and Warren, S. T. (2004). The mGluR theory of fragile X mental retardation. Trends Neurosci. 27, 370–377. doi: 10.1016/j.tins.2004.04.009
Bechara, E. G., Didiot, M. C., Melko, M., Davidovic, L., Bensaid, M., Martin, P., et al. (2009). A novel function for fragile X mental retardation protein in translational activation. PLoS Biol. 7:e16. doi: 10.1371/journal.pbio.1000016
Borbely, E., Scheich, B., and Helyes, Z. (2013). Neuropeptides in learning and memory. Neuropeptides 47, 439–450. doi: 10.1016/j.npep.2013.10.012
Bostrom, C. A., Majaess, N. M., Morch, K., White, E., Eadie, B. D., and Christie, B. R. (2015). Rescue of NMDAR-dependent synaptic plasticity in fmr1 knock-out mice. Cereb. Cortex 25, 271–279. doi: 10.1093/cercor/bht237
Bourgault, S., Vaudry, D., Botia, B., Couvineau, A., Laburthe, M., Vaudry, H., et al. (2008). Novel stable PACAP analogs with potent activity towards the PAC1 receptor. Peptides 29, 919–932. doi: 10.1016/j.peptides.2008.01.022
Braat, S., and Kooy, R. F. (2015). Insights into GABAAergic system deficits in fragile X syndrome lead to clinical trials. Neuropharmacology 88, 48–54. doi: 10.1016/j.neuropharm.2014.06.028
Cabezas-Llobet, N., Vidal-Sancho, L., Masana, M., Fournier, A., Alberch, J., Vaudry, D., et al. (2018). Pituitary adenylate cyclase-activating polypeptide (PACAP) enhances hippocampal synaptic plasticity and improves memory performance in Huntington’s Disease. Mol. Neurobiol. 55, 8263–8277. doi: 10.1007/s12035-018-0972-5
Castagnola, S., Bardoni, B., and Maurin, T. (2017). The search for an effective therapy to treat fragile X syndrome: dream or reality? Front. Synaptic Neurosci. 9:15. doi: 10.3389/fnsyn.2017.00015
Choi, C. H., Schoenfeld, B. P., Bell, A. J., Hinchey, J., Rosenfelt, C., Gertner, M. J., et al. (2016). Multiple drug treatments that increase cAMP signaling restore long-term memory and aberrant signaling in fragile X syndrome models. Front. Behav. Neurosci. 10:136. doi: 10.3389/fnbeh.2016.00136
Choi, C. H., Schoenfeld, B. P., Weisz, E. D., Bell, A. J., Chambers, D. B., Hinchey, J., et al. (2015). PDE-4 inhibition rescues aberrant synaptic plasticity in drosophila and mouse models of fragile X syndrome. J. Neurosci. 35, 396–408. doi: 10.1523/JNEUROSCI.1356-12.2015
Ciranna, L., and Catania, M. V. (2014). 5-HT7 receptors as modulators of neuronal excitability, synaptic transmission and plasticity: physiological role and possible implications in autism spectrum disorders. Front. Cell Neurosci. 8:250. doi: 10.3389/fncel.2014.00250
Ciranna, L., and Cavallaro, S. (2003). Opposing effects by pituitary adenylate cyclase-activating polypeptide and vasoactive intestinal peptide on hippocampal synaptic transmission. Exp. Neurol. 184, 778–784. doi: 10.1016/s0014-4886(03)00300-5
Comery, T. A., Harris, J. B., Willems, P. J., Oostra, B. A., Irwin, S. A., Weiler, I. J., et al. (1997). Abnormal dendritic spines in fragile X knockout mice: maturation and pruning deficits. Proc. Natl. Acad. Sci. U.S.A. 94, 5401–5404. doi: 10.1073/pnas.94.10.5401
Costa, L., Santangelo, F., Li Volsi, G., and Ciranna, L. (2009). Modulation of AMPA receptor-mediated ion current by pituitary adenylate cyclase-activating polypeptide (PACAP) in CA1 pyramidal neurons from rat hippocampus. Hippocampus 19, 99–109. doi: 10.1002/hipo.20488
Costa, L., Sardone, L. M., Bonaccorso, C. M., D’Antoni, S., Spatuzza, M., Gulisano, W., et al. (2018). Activation of serotonin 5-HT7 receptors modulates hippocampal synaptic plasticity by stimulation of adenylate cyclases and rescues learning and behavior in a mouse model of fragile X syndrome. Front. Mol. Neurosci. 11:353. doi: 10.3389/fnmol.2018.00353
Costa, L., Sardone, L. M., Lacivita, E., Leopoldo, M., and Ciranna, L. (2015). Novel agonists for serotonin 5-HT7 receptors reverse metabotropic glutamate receptor-mediated long-term depression in the hippocampus of wild-type and Fmr1 KO mice, a model of Fragile X Syndrome. Front. Behav. Neurosci. 9:65. doi: 10.3389/fnbeh.2015.00065
Costa, L., Spatuzza, M., D’Antoni, S., Bonaccorso, C. M., Trovato, C., Musumeci, S. A., et al. (2012). Activation of 5-HT7 serotonin receptors reverses metabotropic glutamate receptor-mediated synaptic plasticity in wild-type and Fmr1 knockout mice, a model of Fragile X syndrome. Biol. Psychiatry 72, 924–933. doi: 10.1016/j.biopsych.2012.06.008
Darnell, J. C., and Klann, E. (2013). The translation of translational control by FMRP: therapeutic targets for FXS. Nat. Neurosci. 16, 1530–1536. doi: 10.1038/nn.3379
Deguil, J., Chavant, F., Lafay-Chebassier, C., Perault-Pochat, M. C., Fauconneau, B., and Pain, S. (2010). Neuroprotective effect of PACAP on translational control alteration and cognitive decline in MPTP parkinsonian mice. Neuro. Res. 17, 142–155. doi: 10.1007/s12640-009-9091-4
Dejda, A., Seaborn, T., Bourgault, S., Touzani, O., Fournier, A., Vaudry, H., et al. (2011). PACAP and a novel stable analog protect rat brain from ischemia: insight into the mechanisms of action. Peptides 32, 1207–1216. doi: 10.1016/j.peptides.2011.04.003
Di Mauro, M., Cavallaro, S., and Ciranna, L. (2003). Pituitary adenylate cyclase-activating polypeptide modifies the electrical activity of CA1 hippocampal neurons in the rat. Neurosci. Lett. 337, 97–100. doi: 10.1016/s0304-3940(02)01316-2
Dickson, L., and Finlayson, K. (2009). VPAC and PAC receptors: from ligands to function. Pharmacol. Ther. 121, 294–316. doi: 10.1016/j.pharmthera.2008.11.006
Doan, N. D., Bourgault, S., Dejda, A., Letourneau, M., Detheux, M., Vaudry, D., et al. (2011). Design and in vitro characterization of PAC1/VPAC1-selective agonists with potent neuroprotective effects. Biochem. Pharmacol. 81, 552–561. doi: 10.1016/j.bcp.2010.11.015
Doberer, D., Gschwandtner, M., Mosgoeller, W., Bieglmayer, C., Heinzl, H., and Petkov, V. (2007). Pulmonary and systemic effects of inhaled PACAP38 in healthy male subjects. Eur. J. Clin. Invest 37, 665–672. doi: 10.1111/j.1365-2362.2007.01832.x
Dogrukol-Ak, D., Kumar, V. B., Ryerse, J. S., Farr, S. A., Verma, S., Nonaka, N., et al. (2009). Isolation of peptide transport system-6 from brain endothelial cells: therapeutic effects with antisense inhibition in Alzheimer and stroke models. J. Cereb. Blood Flow Metab. 29, 411–422. doi: 10.1038/jcbfm.2008.131
Dufes, C., Gaillard, F., Uchegbu, I. F., Schatzlein, A. G., Olivier, J. C., and Muller, J. M. (2004). Glucose-targeted niosomes deliver vasoactive intestinal peptide (VIP) to the brain. Int. J. Pharm. 285, 77–85. doi: 10.1016/j.ijpharm.2004.07.020
Farnham, M. M., Lung, M. S., Tallapragada, V. J., and Pilowsky, P. M. (2012). PACAP causes PAC1/VPAC2 receptor mediated hypertension and sympathoexcitation in normal and hypertensive rats. Am. J. Physiol. Heart Circ. Physiol. 303, H910–H917. doi: 10.1152/ajpheart.00464.2012
Feher, M., Gaszner, B., Tamas, A., Gil-Martinez, A. L., Fernandez-Villalba, E., Herrero, M. T., et al. (2018). Alteration of the PAC1 receptor expression in the basal ganglia of MPTP-induced parkinsonian macaque monkeys. Neuro. Res. 33, 702–715. doi: 10.1007/s12640-017-9841-7
Garber, K., Smith, K. T., Reines, D., and Warren, S. T. (2006). Transcription, translation and fragile X syndrome. Curr. Opin. Genet. Dev. 16, 270–275. doi: 10.1016/j.gde.2006.04.010
Ghanizada, H., Al-Karagholi, M. A., Arngrim, N., Ghanizada, M., Larsson, H. B. W., Amin, F. M., et al. (2019a). Effect of pituitary adenylate cyclase-activating polypeptide-27 on cerebral hemodynamics in healthy volunteers: a 3T MRI study. Peptides 121:170134. doi: 10.1016/j.peptides.2019.170134
Ghanizada, H., Al-Karagholi, M. A., Arngrim, N., Olesen, J., and Ashina, M. (2019b). PACAP27 induces migraine-like attacks in migraine patients. Cephalalgia 12:333102419864507. doi: 10.1177/0333102419864507
Giuffrida, R., Musumeci, S., D’Antoni, S., Bonaccorso, C. M., Giuffrida-Stella, A. M., Oostra, B. A., et al. (2005). A reduced number of metabotropic glutamate subtype 5 receptors are associated with constitutive homer proteins in a mouse model of fragile X syndrome. J. Neurosci. 25, 8908–8916. doi: 10.1523/jneurosci.0932-05.2005
Gocel, J., and Larson, J. (2012). Synaptic NMDA receptor-mediated currents in anterior piriform cortex are reduced in the adult fragile X mouse. Neuroscience 221, 170–181. doi: 10.1016/j.neuroscience.2012.06.052
Gross, C., Hoffmann, A., Bassell, G. J., and Berry-Kravis, E. M. (2015). Therapeutic strategies in fragile X syndrome: from bench to bedside and back. Neurotherapeutics 12, 584–608. doi: 10.1007/s13311-015-0355-9
Gulisano, W., Tropea, M. R., Arancio, O., Palmeri, A., and Puzzo, D. (2018). Sub-efficacious doses of phosphodiesterase 4 and 5 inhibitors improve memory in a mouse model of Alzheimer’s disease. Neuropharmacology 138, 151–159. doi: 10.1016/j.neuropharm.2018.06.002
Gupte, R. P., Kadunganattil, S., Shepherd, A. J., Merrill, R., Planer, W., Bruchas, M. R., et al. (2015). Convergent phosphomodulation of the major neuronal dendritic potassium channel Kv4.2 by pituitary adenylate cyclase-activating polypeptide. Neuropharmacology 101, 291–308. doi: 10.1016/j.neuropharm.2015.10.006
Hagerman, R. J., Berry-Kravis, E., Hazlett, H. C., Bailey, DB Jr., Moine, H., Kooy, R. F., et al. (2017). Fragile X syndrome. Nat. Rev. Dis. Primers 3:17065. doi: 10.1038/nrdp.2017.65
Han, P., Caselli, R. J., Baxter, L., Serrano, G., Yin, J., Beach, T. G., et al. (2015). Association of pituitary adenylate cyclase-activating polypeptide with cognitive decline in mild cognitive impairment due to Alzheimer disease. JAMA Neurol. 72, 333–339. doi: 10.1001/jamaneurol.2014.3625
Han, P., Liang, W., Baxter, L. C., Yin, J., Tang, Z., Beach, T. G., et al. (2014a). Pituitary adenylate cyclase-activating polypeptide is reduced in Alzheimer disease. Neurology 82, 1724–1728.
Han, P., Tang, Z., Yin, J., Maalouf, M., Beach, T. G., Reiman, E. M., et al. (2014b). Pituitary adenylate cyclase-activating polypeptide protects against beta-amyloid toxicity. Neurobiol. Aging 35, 2064–2071. doi: 10.1016/j.neurobiolaging.2014.03.022
Han, P., Nielsen, M., Song, M., Yin, J., Permenter, M. R., Vogt, J. A., et al. (2017). The impact of aging on brain pituitary adenylate cyclase activating polypeptide, pathology and cognition in mice and rhesus macaques. Front. Aging Neurosci. 9:180. doi: 10.3389/fnagi.2017.00180
Harmar, A. J., Fahrenkrug, J., Gozes, I., Laburthe, M., May, V., Pisegna, J. R., et al. (2012). Pharmacology and functions of receptors for vasoactive intestinal peptide and pituitary adenylate cyclase-activating polypeptide: IUPHAR review 1. Br. J. Pharmacol. 166, 4–17. doi: 10.1111/j.1476-5381.2012.01871.x
Hashimoto, R., Hashimoto, H., Shintani, N., Chiba, S., Hattori, S., Okada, T., et al. (2007). Pituitary adenylate cyclase-activating polypeptide is associated with schizophrenia. Mol. Psychiatry 12, 1026–1032.
Hayata-Takano, A., Kamo, T., Kijima, H., Seiriki, K., Ogata, K., Ago, Y., et al. (2019). Pituitary adenylate cyclase-activating polypeptide modulates dendritic spine maturation and morphogenesis via microRNA-132 upregulation. J. Neurosci. 39, 4208–4220. doi: 10.1523/JNEUROSCI.2468-18.2019
He, Q., Nomura, T., Xu, J., and Contractor, A. (2014). The developmental switch in GABA polarity is delayed in fragile X mice. J. Neurosci. 34, 446–450. doi: 10.1523/JNEUROSCI.4447-13.2014
Hirabayashi, T., Nakamachi, T., and Shioda, S. (2018). Discovery of PACAP and its receptors in the brain. J. Headache Pain 19:28. doi: 10.1186/s10194-018-0855-1
Holland, P. R., Barloese, M., and Fahrenkrug, J. (2018). PACAP in hypothalamic regulation of sleep and circadian rhythm: importance for headache. J. Headache Pain 19:20. doi: 10.1186/s10194-018-0844-4
Huber, K. M., Gallagher, S. M., Warren, S. T., and Bear, M. F. (2002). Altered synaptic plasticity in a mouse model of fragile X mental retardation. Proc. Natl. Acad. Sci. U.S.A. 99, 7746–7750. doi: 10.1073/pnas.122205699
Huber, K. M., Klann, E., Costa-Mattioli, M., and Zukin, R. S. (2015). Dysregulation of mammalian target of rapamycin signaling in mouse models of autism. J. Neurosci. 35, 13836–13842. doi: 10.1523/JNEUROSCI.2656-15.2015
Irwin, S. A., Galvez, R., and Greenough, W. T. (2000). Dendritic spine structural anomalies in fragile-X mental retardation syndrome. Cereb. Cortex 10, 1038–1044. doi: 10.1093/cercor/10.10.1038
Jacquemont, S., Berry-Kravis, E., Hagerman, R., von Raison, F., Gasparini, F., Apostol, G., et al. (2014). The challenges of clinical trials in fragile X syndrome. Psychopharmacology 231, 1237–1250. doi: 10.1007/s00213-013-3289-0
Jaworski, D. M., and Proctor, M. D. (2000). Developmental regulation of pituitary adenylate cyclase-activating polypeptide and PAC(1) receptor mRNA expression in the rat central nervous system. Brain Res. Dev. Brain Res. 120, 27–39. doi: 10.1016/s0165-3806(99)00192-3
Jolivel, V., Basille, M., Aubert, N., de Jouffrey, S., Ancian, P., Le Bigot, J. F., et al. (2009). Distribution and functional characterization of pituitary adenylate cyclase-activating polypeptide receptors in the brain of non-human primates. Neuroscience 160, 434–451. doi: 10.1016/j.neuroscience.2009.02.028
Joo, K. M., Chung, Y. H., Kim, M. K., Nam, R. H., Lee, B. L., Lee, K. H., et al. (2004). Distribution of vasoactive intestinal peptide and pituitary adenylate cyclase-activating polypeptide receptors (VPAC1, VPAC2, and PAC1 receptor) in the rat brain. J. Comp. Neurol. 476, 388–413. doi: 10.1002/cne.20231
Kelley, D. J., Bhattacharyya, A., Lahvis, G. P., Yin, J. C., Malter, J., and Davidson, R. J. (2008). The cyclic AMP phenotype of fragile X and autism. Neurosci. Biobehav. Rev. 32, 1533–1543. doi: 10.1016/j.neubiorev.2008.06.005
Kelly, M. P. (2018). Cyclic nucleotide signaling changes associated with normal aging and age-related diseases of the brain. Cell Signal 42, 281–291. doi: 10.1016/j.cellsig.2017.11.004
Kim, S. H., Markham, J. A., Weiler, I. J., and Greenough, W. T. (2008). Aberrant early-phase ERK inactivation impedes neuronal function in fragile X syndrome. Proc. Natl. Acad. Sci. U.S.A. 105, 4429–4434. doi: 10.1073/pnas.0800257105
Kinhult, J., Adner, M., Uddman, R., and Cardell, L. O. (2003). Pituitary adenylate cyclase-activating polypeptide, effects in the human nose. Clin. Exp. Allergy 33, 942–949.
Kojro, E., Postina, R., Buro, C., Meiringer, C., Gehrig-Burger, K., and Fahrenholz, F. (2006). The neuropeptide PACAP promotes the alpha-secretase pathway for processing the Alzheimer amyloid precursor protein. FASEB J. 20, 512–514. doi: 10.1096/fj.05-4812fje
Kondo, T., Tominaga, T., Ichikawa, M., and Iijima, T. (1997). Differential alteration of hippocampal synaptic strength induced by pituitary adenylate cyclase activating polypeptide-38 (PACAP-38). Neurosci. Lett. 221, 189–192. doi: 10.1016/s0304-3940(96)13323-1
Korkmaz, O. T., Ay, H., Aytan, N., Carreras, I., Kowall, N. W., Dedeoglu, A., et al. (2018). Vasoactive intestinal peptide decreases beta-amyloid accumulation and prevents brain atrophy in the 5xFAD mouse model of Alzheimer’s Disease. J. Mol. Neurosci. 68, 389–396. doi: 10.1007/s12031-018-1226-8
Korkmaz, O. T., and Tuncel, N. (2018). Advantages of vasoactive intestinal peptide for the future treatment of Parkinson’s Disease. Curr. Pharm. Des. 24, 4693–4701. doi: 10.2174/1381612825666190111150953
Koves, K., Arimura, A., Gorcs, T. G., and Somogyvari-Vigh, A. (1991). Comparative distribution of immunoreactive pituitary adenylate cyclase activating polypeptide and vasoactive intestinal polypeptide in rat forebrain. Neuroendocrinology 54, 159–169. doi: 10.1159/000125864
Ladjimi, M. H., Barbouche, R., Ben Barka, Z., Vaudry, D., Lefranc, B., Leprince, J., et al. (2019). Comparison of the effects of PACAP-38 and its analog, acetyl-[Ala(15), Ala(20)] PACAP-38-propylamide, on spatial memory, post-learning BDNF expression and oxidative stress in rat. Behav. Brain Res. 359, 247–257. doi: 10.1016/j.bbr.2018.10.023
Lamine, A., Letourneau, M., Doan, N. D., Maucotel, J., Couvineau, A., Vaudry, H., et al. (2016). Characterizations of a synthetic pituitary adenylate cyclase-activating polypeptide analog displaying potent neuroprotective activity and reduced in vivo cardiovascular side effects in a Parkinson’s disease model. Neuropharmacology 108, 440–450. doi: 10.1016/j.neuropharm.2015.05.014
Lamine-Ajili, A., Fahmy, A. M., Letourneau, M., Chatenet, D., Labonte, P., Vaudry, D., et al. (2016). Effect of the pituitary adenylate cyclase-activating polypeptide on the autophagic activation observed in in vitro and in vivo models of Parkinson’s disease. Biochim. Biophys. Acta 1862, 688–695. doi: 10.1016/j.bbadis.2016.01.005
Liu, Z., Geng, L., Li, R., He, X., Zheng, J. Q., and Xie, Z. (2003). Frequency modulation of synchronized Ca2+ spikes in cultured hippocampal networks through G-protein-coupled receptors. J. Neurosci. 23, 4156–4163. doi: 10.1523/jneurosci.23-10-04156.2003
Macdonald, D. S., Weerapura, M., Beazely, M. A., Martin, L., Czerwinski, W., Roder, J. C., et al. (2005). Modulation of NMDA receptors by pituitary adenylate cyclase activating peptide in CA1 neurons requires G alpha q, protein kinase C, and activation of Src. J. Neurosci. 25, 11374–11384. doi: 10.1523/jneurosci.3871-05.2005
Martin, B. S., Corbin, J. G., and Huntsman, M. M. (2014). Deficient tonic GABAergic conductance and synaptic balance in the fragile X syndrome amygdala. J. Neurophysiol. 112, 890–902. doi: 10.1152/jn.00597.2013
Marzagalli, R., Leggio, G. M., Bucolo, C., Pricoco, E., Keay, K. A., Cardile, V., et al. (2016). Genetic blockade of the dopamine D3 receptor enhances hippocampal expression of PACAP and receptors and alters their cortical distribution. Neuroscience 316, 279–295. doi: 10.1016/j.neuroscience.2015.12.034
Masuo, Y., Matsumoto, Y., Tokito, F., Tsuda, M., and Fujino, M. (1993). Effects of vasoactive intestinal polypeptide (VIP) and pituitary adenylate cyclase activating polypeptide (PACAP) on the spontaneous release of acetylcholine from the rat hippocampus by brain microdialysis. Brain Res. 611, 207–215. doi: 10.1016/0006-8993(93)90504-g
Matsuyama, S., Matsumoto, A., Hashimoto, H., Shintani, N., and Baba, A. (2003). Impaired long-term potentiation in vivo in the dentate gyrus of pituitary adenylate cyclase-activating polypeptide (PACAP) or PACAP type 1 receptor-mutant mice. Neuroreport 14, 2095–2098. doi: 10.1097/00001756-200311140-00017
Maurin, T., Lebrigand, K., Castagnola, S., Paquet, A., Jarjat, M., Popa, A., et al. (2018a). HITS-CLIP in various brain areas reveals new targets and new modalities of RNA binding by fragile X mental retardation protein. Nucleic Acids Res. 46, 6344–6355. doi: 10.1093/nar/gky267
Maurin, T., Melancia, F., Jarjat, M., Castro, L., Costa, L., Delhaye, S., et al. (2018b). Involvement of phosphodiesterase 2A activity in the pathophysiology of fragile X syndrome. Cereb. Cortex [Epub ahead of print].
Maurin, T., Zongaro, S., and Bardoni, B. (2014). Fragile X syndrome: from molecular pathology to therapy. Neurosci. Biobehav. Rev. 46(Pt 2), 242–255. doi: 10.1016/j.neubiorev.2014.01.006
Meloni, E. G., Kaye, K. T., Venkataraman, A., and Carlezon, W. A. Jr. (2018). PACAP increases Arc/Arg 3.1 expression within the extended amygdala after fear conditioning in rats. Neurobiol. Learn Mem. 157, 24–34. doi: 10.1016/j.nlm.2018.11.011
Meloni, E. G., Venkataraman, A., Donahue, R. J., and Carlezon, W. A. Jr. (2016). Bi-directional effects of pituitary adenylate cyclase-activating polypeptide (PACAP) on fear-related behavior and c-Fos expression after fear conditioning in rats. Psychoneuroendocrinology 64, 12–21. doi: 10.1016/j.psyneuen.2015.11.003
Min, W. W., Yuskaitis, C. J., Yan, Q., Sikorski, C., Chen, S., Jope, R. S., et al. (2009). Elevated glycogen synthase kinase-3 activity in Fragile X mice: key metabolic regulator with evidence for treatment potential. Neuropharmacology 56, 463–472. doi: 10.1016/j.neuropharm.2008.09.017
Miyata, A., Arimura, A., Dahl, R. R., Minamino, N., Uehara, A., Jiang, L., et al. (1989). Isolation of a novel 38 residue-hypothalamic polypeptide which stimulates adenylate cyclase in pituitary cells. Biochem. Biophys. Res. Commun. 164, 567–574. doi: 10.1016/0006-291x(89)91757-9
Nonaka, N., Banks, W. A., Mizushima, H., Shioda, S., and Morley, J. E. (2002). Regional differences in PACAP transport across the blood-brain barrier in mice: a possible influence of strain, amyloid beta protein, and age. Peptides 23, 2197–2202. doi: 10.1016/s0196-9781(02)00248-6
Nonaka, N., Farr, S. A., Nakamachi, T., Morley, J. E., Nakamura, M., Shioda, S., et al. (2012). Intranasal administration of PACAP: uptake by brain and regional brain targeting with cyclodextrins. Peptides 36, 168–175. doi: 10.1016/j.peptides.2012.05.021
Ogata, K., Shintani, N., Hayata-Takano, A., Kamo, T., Higashi, S., Seiriki, K., et al. (2015). PACAP enhances axon outgrowth in cultured hippocampal neurons to a comparable extent as BDNF. PLoS One 10:e0120526. doi: 10.1371/journal.pone.0120526
Osterweil, E. K., Krueger, D. D., Reinhold, K., and Bear, M. F. (2010). Hypersensitivity to mGluR5 and ERK1/2 leads to excessive protein synthesis in the hippocampus of a mouse model of fragile X syndrome. J. Neurosci. 30, 15616–15627. doi: 10.1523/JNEUROSCI.3888-10.2010
Otto, C., Kovalchuk, Y., Wolfer, D. P., Gass, P., Martin, M., Zuschratter, W., et al. (2001). Impairment of mossy fiber long-term potentiation and associative learning in pituitary adenylate cyclase activating polypeptide type I receptor-deficient mice. J. Neurosci. 21, 5520–5527. doi: 10.1523/jneurosci.21-15-05520.2001
Pecoraro, V., Sardone, L. M., Chisari, M., Licata, F., Li Volsi, G., Perciavalle, V., et al. (2017). A subnanomolar concentration of pituitary adenylate cyclase-activating polypeptide (PACAP) pre-synaptically modulates glutamatergic transmission in the rat hippocampus acting through acetylcholine. Neuroscience 340, 551–562. doi: 10.1016/j.neuroscience.2016.10.061
Pirger, Z., Naskar, S., Laszlo, Z., Kemenes, G., Reglodi, D., and Kemenes, I. (2014). Reversal of age-related learning deficiency by the vertebrate PACAP and IGF-1 in a novel invertebrate model of aging: the pond snail (Lymnaea stagnalis). J. Gerontol. A Biol. Sci. Med. Sci. 69, 1331–1338. doi: 10.1093/gerona/glu068
Prickaerts, J., Heckman, P. R. A., and Blokland, A. (2017). Investigational phosphodiesterase inhibitors in phase I and phase II clinical trials for Alzheimer’s disease. Exp. Opin. Invest. Drugs 26, 1033–1048. doi: 10.1080/13543784.2017.1364360
Rat, D., Schmitt, U., Tippmann, F., Dewachter, I., Theunis, C., Wieczerzak, E., et al. (2011). Neuropeptide pituitary adenylate cyclase-activating polypeptide (PACAP) slows down Alzheimer’s disease-like pathology in amyloid precursor protein-transgenic mice. FASEB J. 25, 3208–3218. doi: 10.1096/fj.10-180133
Reglodi, D., Atlasz, T., Jungling, A., Szabo, E., Kovari, P., Manavalan, S., et al. (2018a). Alternative routes of administration of the neuroprotective pituitary adenylate cyclase activating polypeptide. Curr. Pharm Des. 24, 3892–3904. doi: 10.2174/1381612824666181112110934
Reglodi, D., Atlasz, T., Szabo, E., Jungling, A., Tamas, A., Juhasz, T., et al. (2018b). PACAP deficiency as a model of aging. Geroscience 40, 437–452. doi: 10.1007/s11357-018-0045-8
Reglodi, D., Vaczy, A., Rubio-Beltran, E., and MaassenVanDenBrink, A. (2018c). Protective effects of PACAP in ischemia. J. Headache Pain 19:19. doi: 10.1186/s10194-018-0845-3
Reglodi, D., Lubics, A., Tamas, A., Szalontay, L., and Lengvari, I. (2004). Pituitary adenylate cyclase activating polypeptide protects dopaminergic neurons and improves behavioral deficits in a rat model of Parkinson’s disease. Behav. Brain Res. 151, 303–312. doi: 10.1016/j.bbr.2003.09.007
Reglodi, D., Renaud, J., Tamas, A., Tizabi, Y., Socias, S. B., Del-Bel, E., et al. (2017). Novel tactics for neuroprotection in Parkinson’s disease: role of antibiotics, polyphenols and neuropeptides. Prog. Neurobiol. 155, 120–148. doi: 10.1016/j.pneurobio.2015.10.004
Reglodi, D., Tamas, A., Lengvari, I., Toth, G., Szalontay, L., and Lubics, A. (2006). Comparative study of the effects of PACAP in young, aging, and castrated males in a rat model of Parkinson’s disease. Ann. N. Y. Acad. Sci. 1070, 518–524. doi: 10.1196/annals.1317.072
Rhea, E. M., Bullock, K. M., and Banks, W. A. (2018). Effect of controlled cortical impact on the passage of pituitary adenylate cyclase activating polypeptide (PACAP) across the blood-brain barrier. Peptides 99, 8–13. doi: 10.1016/j.peptides.2017.10.013
Roberto, M., and Brunelli, M. (2000). PACAP-38 enhances excitatory synaptic transmission in the rat hippocampal CA1 region. Learn Mem. 7, 303–311. doi: 10.1101/lm.34200
Roberto, M., Scuri, R., and Brunelli, M. (2001). Differential effects of PACAP-38 on synaptic responses in rat hippocampal CA1 region. Learn Mem. 8, 265–271. doi: 10.1101/lm.40501
Runcie, M. J., Ulman, L. G., and Potter, E. K. (1995). Effects of pituitary adenylate cyclase-activating polypeptide on cardiovascular and respiratory responses in anaesthetised dogs. Regul. Pept. 60, 193–200. doi: 10.1016/0167-0115(95)00131-x
Saavedra, A., Giralt, A., Arumi, H., Alberch, J., and Perez-Navarro, E. (2013). Regulation of hippocampal cGMP levels as a candidate to treat cognitive deficits in Huntington’s disease. PloS One 8:e73664. doi: 10.1371/journal.pone.0073664
Sacchetti, B., Lorenzini, C. A., Baldi, E., Bucherelli, C., Roberto, M., Tassoni, G., et al. (2001). Pituitary adenylate cyclase-activating polypeptide hormone (PACAP) at very low dosages improves memory in the rat. Neurobiol. Learn. Mem. 76, 1–6. doi: 10.1006/nlme.2001.4014
Santoro, M. R., Bray, S. M., and Warren, S. T. (2012). Molecular mechanisms of fragile X syndrome: a twenty-year perspective. Annu. Rev. Pathol. 7, 219–245. doi: 10.1146/annurev-pathol-011811-132457
Sauvage, M., Brabet, P., Holsboer, F., Bockaert, J., and Steckler, T. (2000). Mild deficits in mice lacking pituitary adenylate cyclase-activating polypeptide receptor type 1 (PAC1) performing on memory tasks. Brain Res. Mol. Brain Res. 84, 79–89. doi: 10.1016/s0169-328x(00)00219-9
Schmidt, S. D., Myskiw, J. C., Furini, C. R., Schmidt, B. E., Cavalcante, L. E., and Izquierdo, I. (2015). PACAP modulates the consolidation and extinction of the contextual fear conditioning through NMDA receptors. Neurobiol. Learn. Mem. 118, 120–124. doi: 10.1016/j.nlm.2014.11.014
Schytz, H. W., Birk, S., Wienecke, T., Kruuse, C., Olesen, J., and Ashina, M. (2009). PACAP38 induces migraine-like attacks in patients with migraine without aura. Brain 132, 16–25. doi: 10.1093/brain/awn307
Sekar, R., Wang, L., and Chow, B. K. (2017). Central control of feeding behavior by the secretin, PACAP, and glucagon family of peptides. Front. Endocrinol. 8:18. doi: 10.3389/fendo.2017.00018
Sethna, F., Moon, C., and Wang, H. (2014). From FMRP function to potential therapies for fragile X syndrome. Neurochem. Res. 39, 1016–1031. doi: 10.1007/s11064-013-1229-3
Sharma, A., Hoeffer, C. A., Takayasu, Y., Miyawaki, T., McBride, S. M., Klann, E., et al. (2010). Dysregulation of mTOR signaling in fragile X syndrome. J. Neurosci. 30, 694–702. doi: 10.1523/JNEUROSCI.3696-09.2010
Shioda, S., and Nakamachi, T. (2015). PACAP as a neuroprotective factor in ischemic neuronal injuries. Peptides 72, 202–207. doi: 10.1016/j.peptides.2015.08.006
Shioda, S., Shuto, Y., Somogyvari-Vigh, A., Legradi, G., Onda, H., Coy, D. H., et al. (1997). Localization and gene expression of the receptor for pituitary adenylate cyclase-activating polypeptide in the rat brain. Neurosci. Res. 28, 345–354.
Shivers, K. Y., Nikolopoulou, A., Machlovi, S. I., Vallabhajosula, S., and Figueiredo-Pereira, M. E. (2014). PACAP27 prevents Parkinson-like neuronal loss and motor deficits but not microglia activation induced by prostaglandin J2. Biochim. Biophys. Acta 1842, 1707–1719. doi: 10.1016/j.bbadis.2014.06.020
Ster, J., de Bock, F., Bertaso, F., Abitbol, K., Daniel, H., Bockaert, J., et al. (2009). Epac mediates PACAP-dependent long-term depression in the hippocampus. J. Physiol. 587, 101–113. doi: 10.1113/jphysiol.2008.157461
Takuma, K., Maeda, Y., Ago, Y., Ishihama, T., Takemoto, K., Nakagawa, A., et al. (2014). An enriched environment ameliorates memory impairments in PACAP-deficient mice. Behav. Brain Res. 272, 269–278. doi: 10.1016/j.bbr.2014.07.005
Tan, C. L., Cooke, E. K., Leib, D. E., Lin, Y. C., Daly, G. E., Zimmerman, C. A., et al. (2016). Warm-sensitive neurons that control body temperature. Cell 167:e15. doi: 10.1016/j.cell.2016.08.028
Taylor, R. D., Madsen, M. G., Krause, M., Sampedro-Castaneda, M., Stocker, M., and Pedarzani, P. (2014). Pituitary adenylate cyclase-activating polypeptide (PACAP) inhibits the slow afterhyperpolarizing current sIAHP in CA1 pyramidal neurons by activating multiple signaling pathways. Hippocampus 24, 32–43. doi: 10.1002/hipo.22201
Toda, A. M., and Huganir, R. L. (2015). Regulation of AMPA receptor phosphorylation by the neuropeptide PACAP38. Proc. Natl. Acad. Sci. U.S.A. 112, 6712–6717. doi: 10.1073/pnas.1507229112
Tsutsumi, M., Claus, T. H., Liang, Y., Li, Y., Yang, L., Zhu, J., et al. (2002). A potent and highly selective VPAC2 agonist enhances glucose-induced insulin release and glucose disposal: a potential therapy for type 2 diabetes. Diabetes 51, 1453–1460. doi: 10.2337/diabetes.51.5.1453
Uzunova, G., Hollander, E., and Shepherd, J. (2014). The role of ionotropic glutamate receptors in childhood neurodevelopmental disorders: autism spectrum disorders and fragile x syndrome. Curr. Neuropharmacol. 12, 71–98. doi: 10.2174/1570159X113116660046
Vaudry, D., Falluel-Morel, A., Bourgault, S., Basille, M., Burel, D., Wurtz, O., et al. (2009). Pituitary adenylate cyclase-activating polypeptide and its receptors: 20 years after the discovery. Pharmacol. Rev. 61, 283–357. doi: 10.1124/pr.109.001370
Verkerk, A. J., Pieretti, M., Sutcliffe, J. S., Fu, Y. H., Kuhl, D. P., Pizzuti, A., et al. (1991). Identification of a gene (FMR-1) containing a CGG repeat coincident with a breakpoint cluster region exhibiting length variation in fragile X syndrome. Cell 65, 905–914. doi: 10.1016/0092-8674(91)90397-h
Wang, G., Pan, J., Tan, Y. Y., Sun, X. K., Zhang, Y. F., Zhou, H. Y., et al. (2008). Neuroprotective effects of PACAP27 in mice model of Parkinson’s disease involved in the modulation of K(ATP) subunits and D2 receptors in the striatum. Neuropeptides 42, 267–276. doi: 10.1016/j.npep.2008.03.002
Weinstein, J. J., Chohan, M. O., Slifstein, M., Kegeles, L. S., Moore, H., and Abi-Dargham, A. (2017). Pathway-specific dopamine abnormalities in schizophrenia. Biol. Psychiatry 81, 31–42. doi: 10.1016/j.biopsych.2016.03.2104
Wu, Z. L., Ciallella, J. R., Flood, D. G., O’Kane, T. M., Bozyczko-Coyne, D., and Savage, M. J. (2006). Comparative analysis of cortical gene expression in mouse models of Alzheimer’s disease. Neurobiol. Aging 27, 377–386. doi: 10.1016/j.neurobiolaging.2005.02.010
Yaka, R., He, D. Y., Phamluong, K., and Ron, D. (2003). Pituitary adenylate cyclase-activating polypeptide (PACAP(1-38)) enhances N-methyl-D-aspartate receptor function and brain-derived neurotrophic factor expression via RACK1. J. Biol. Chem. 278, 9630–9638. doi: 10.1074/jbc.m209141200
Yang, K., Lei, G., Jackson, M. F., and Macdonald, J. F. (2010). The involvement of PACAP/VIP system in the synaptic transmission in the hippocampus. J. Mol. Neurosci. 42, 319–326. doi: 10.1007/s12031-010-9372-7
Yu, R., Guo, X., Huang, L., Zeng, Z., and Zhang, H. (2012a). The novel peptide PACAP-TAT with enhanced traversing ability attenuates the severe lung injury induced by repeated smoke inhalation. Peptides 38, 142–149. doi: 10.1016/j.peptides.2012.09.005
Yu, R., Zeng, Z., Guo, X., Zhang, H., Liu, X., Ding, Y., et al. (2012b). The TAT peptide endows PACAP with an enhanced ability to traverse bio-barriers. Neurosci. Lett. 527, 1–5. doi: 10.1016/j.neulet.2012.08.005
Keywords: pituitary adenylate cyclase-activating polypeptide, fragile X syndrome, cyclic adenosine monophosphate, long-term depression induced by metabotropic glutamate receptor, hippocampus, learning
Citation: Ciranna L and Costa L (2019) Pituitary Adenylate Cyclase-Activating Polypeptide Modulates Hippocampal Synaptic Transmission and Plasticity: New Therapeutic Suggestions for Fragile X Syndrome. Front. Cell. Neurosci. 13:524. doi: 10.3389/fncel.2019.00524
Received: 03 September 2019; Accepted: 08 November 2019;
Published: 27 November 2019.
Edited by:
Annalisa Scimemi, University at Albany, United StatesReviewed by:
Andrea Tamas, University of Pécs, HungaryCarmelo Sgobio, German Center for Neurodegenerative Diseases (DZNE), Germany
Copyright © 2019 Ciranna and Costa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lucia Ciranna, Y2lyYW5uYUB1bmljdC5pdA==
 Lucia Ciranna
Lucia Ciranna Lara Costa
Lara Costa