- 1Department of Neurology, Affiliated Yixing Hospital of Jiangsu University, Yixing, China
- 2Department of Neurology, Jinling Hospital, Medical School of Nanjing University, Nanjing, China
- 3Department of Neurology, The Fourth Affiliated Hospital of Nanjing Medical University, Nanjing Pukou Hospital, Nanjing, China
- 4Department of Neurology, First Affiliated Hospital, College of Clinical Medicine, Henan University of Science and Technology, Luoyang, China
- 5Department of Neurology, Affiliated Hospital of Yangzhou University, Yangzhou, China
- 6Department of Neurology, No. 984 Hospital of PLA, Beijing, China
Background: Preventive strategies implemented during the COVID-19 pandemic may negatively influence the management of patients with acute ischemic stroke (AIS). Nowadays, studies have demonstrated that the pandemic has led to a delay in treatment among patients with AIS. Whether this delay contributes to meaningful short-term outcome differences warranted further exploration.
Objective: The objective of this study was to evaluate the impacts of the COVID-19 pandemic on treatment delay and short-term outcomes of patients with AIS treated with IVT and MT.
Methods: Patients admitted before (from 11/1/2019 to 1/31/2020) and during the COVID-19 pandemic (from 2/1/2020 to 3/31/2020) were screened for collecting sociodemographic data, medical history information, and symptom onset status, and comparing the effect of treatment delay. The patients treated with IVT or MT were compared for delay time and neurological outcomes. Multivariable logistic regression was used to estimate the effect of treatment delay on short-term neurological prognosis.
Results: In this study, 358 patients receiving IVT were included. DTN time increased from 50 min (IQR 40–75) before to 65 min (IQR 48–84), p = 0.048. 266 patients receiving MT were included. The DTP was 120 (112–148) min vs. 160 (125-199) min before and during the pandemic, p = 0.002. Patients with stroke during the pandemic had delays in treatment due to the need for additional PPE (p < 0.001), COVID-19 screening processes (p < 0.001), multidisciplinary consultation (p < 0.001), and chest CT scans (p < 0.001). Compared with pre-COVID-19, during the pandemic, patients had a higher likelihood of spontaneous intracranial hemorrhage after IVT (OR: 1.10; 95% CI, 1.03–1.30) and a lower likelihood of mRS scores 0–2 at discharge (OR: 0.90; 95% CI, 0.78–0.99). In logistic regression analysis, high NIHSS score at admission, increasing age, worse pre-admission mRS, large vessel occlusion, admission during the lockdown period, and low mTICI grade after MT were associated with an mRS ≥ 3.
Conclusion: The COVID-19 pandemic has had remarkable impacts on the management of AIS. The pandemic might exacerbate certain time delays and play a significant role in early adverse outcomes in patients with AIS.
Introduction
The likelihood of acute ischemic stroke (AIS) patients with large vessel occlusion (LVO) to receive emergency care, such as endovascular mechanical thrombectomy (MT) or intravenous thrombolysis (IVT), is extremely time-dependent (1). This is partially influenced by the effectiveness of pre-hospital care and the sufficiency of hospital resources. However, the impact of the pandemic is perhaps inevitable. Since the pandemic breakout, there has been a noticeably lower rate of thrombolysis and thrombectomy in patients with AIS, as documented by various facilities (2–5). Meanwhile, several articles have reported that the COVID-19 outbreak was linked to delays in the treatment of patients with AIS (6–8). Speculative explanations for these delays include the disruption of medical services cause by the pandemic, the anxiety of patients over contracting SARS-CoV-2, psychological stress brought on by the pandemic, and associated lockdowns (8, 9).
Hospitals must take the required precautions due to the outbreak escalation to prevent the simultaneous spread of the SARS-CoV-2 virus to patients and medical staff (10). According to reports, some medical facilities increased their precautionary procedures in responding to the pandemic, thus leading to longer delays in diagnosis and treatment (11), resulting in poor outcomes. Even during the pandemic, thrombolysis and thrombectomy should be administered to patients with AIS without any delay to reduce mortality and morbidity (12). With the escalation of the pandemic, the preventive measures around the world have also been upgraded accordingly. During the pandemic, China had launched several control measures to gradually reduce COVID-19 transmission. Recent studies have also shown a decrease in stroke admissions during the pandemic, but data on emergency stroke management and treatment outcomes are still limited (13). Therefore, we performed a multicenter retrospective study to compare treatment processes and clinical outcomes of patients with AIS who underwent IVT and MT before and after the pandemic outbreak to evaluate the impact of the pandemic on the processes and outcomes of IVT and MT performed in patients with AIS.
Methods
Study design and patient population
This study was part of an ongoing program for analyzing the COVID-19 pandemic in managing patients with stroke. The current study was a retrospective analysis of prospectively collected data. A total of six tertiary hospitals with comprehensive stroke centers were included in this study, four of which are in Jiangsu Province, namely, Jinling Clinical College of Nanjing Medical University, Affiliated Yixing Hospital of Jiangsu University, The Fourth Affiliated Hospital of Nanjing Medical University, and The Affiliated Hospital of Yangzhou University. The First Affiliated Hospital and College of Clinical Medicine of Henan University of Science and Technology is located in Henan Province, and NO 984 Hospital of PLA is in Beijing. On 31 January 2020, the Chinese government announced several nationwide strategies for preventing the COVID-19 pandemic. Patients with AIS diagnosed from 1 December 2019 to 31 January 2020 (pre-COVID-19), and those diagnosed from 1 February 2020 to 31 March 2020 (post-COVID-19) were compared in this study. AIS was diagnosed based on clinical symptoms and computed tomography or magnetic resonance imaging. Patients who reached the hospitals within 7 days after stroke onset were included. Socioeconomic status, medical history, stroke symptoms, National Institutes of Health Stroke Scale (NIHSS) score, Alberta Stroke Program Early CT Score (ASPECTS), modified thrombolysis in cerebral infarction (mTICI) score before discharge, onset-to-door (OTD) time defined as the time from onset to hospital arrival, door-to-needle (DTN) time defined as the time from hospital arrival to initiation of thrombolysis, door-to-puncture (DTP) time defined as the time from hospital arrival to groin puncture, and post-treatment NIHSS scores were reviewed and analyzed. All participants and their relatives provided written informed consent, and the study was approved by the ethics committees of the participating hospitals. The reporting of this study conformed to the STROBE statement (14). The emergency department staff were equipped with adequate personal protective equipment (PPE). Nucleic acid tests, body temperature measurements, inquiries about recent travel, complete blood count checks, and chest CT scans were all part of the COVID-19 screening process. Patients with definite fever or respiratory symptoms, as well as those whose routine chest CT scans suggested COVID-19 imaging, would need to undergo in-hospital multidisciplinary consultation. According to an expert consensus on the stroke emergency map during the epidemic of coronavirus disease 2019 (15), hospitals involved in the study had a 24/7 on-call COVID-19 expert group (associate chief physician and above), including respiratory physicians, infection physicians, critical care physicians, imaging physicians, emergency medicine physicians, respiratory nurses, and critical care nurses, to closely coordinate with the stroke green channel, responsible for the consultation of patients with suspected COVID-19. We would consult patients with suspected COVID-19 acute stroke (mainly by video consultation) to clarify the diagnosis and guide the clinical treatment and protection strategy. Patients were triaged by multidisciplinary consultation based on the results of these screenings. In brief, COVID-19 nucleic acid-negative patients requiring MT were treated in routine standard operating procedures. Suspected positive patients were treated in a specialized operating room with the highest level of protection and transferred to a specialized isolation ward after surgery. Patients with AIS undergoing MT procedures were generally recommended to undergo local anesthesia, unless the patients were irritable and uncooperative.
The primary outcome of this trial was the mRS score at discharge after IVT or MT. Safety outcomes included intracerebral hemorrhage (ICH), arterial perforation, subarachnoid hemorrhage (SAH), and arterial entrapment (a complication of entrapment of the internal carotid artery, the vertebrobasilar artery entrapment, and the large intracranial vessels).
All variables with a p < 0.1 were then entered into the multivariable logistic regression model—influencing factors for short-term clinical poor outcomes. For patients treated with IVT, variables such as age, sex, stroke etiology, pre-admission mRS, NIHSS at admission, stroke history, hypertension, diabetes, hyperlipidemia, atrial fibrillation, and coronary heart disease were included in the full model. For patients with MT treatment, mTICI 2b-3 was also included in the model. In this study, variables such as smoking, alcohol drinking, anterior circulation, solitary, daytime onset, and residence were removed from the full to final models.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation or median and interquartile range (IQR), as appropriate. Categorical variables were presented as frequency and percentage. Continuous variables with normal distribution were compared using Student's t-test. The χ2 and Fisher's exact tests were used for comparing categorical values. Multivariable stepwise logistic regression was used to determine influencing factors for short-term clinical poor outcomes (mRS ≥ 3) among all the patients with AIS enrolled in this study. A two-sided p-value of < 0.05 was deemed statistically significant. All statistical analyses were performed using SPSS 25.
Results
In this study, a total of 1,286 patients with AIS were enrolled, among which 928 were ultimately not treated with thrombolysis due to contraindications, out-of-time window, personal preferences, and either too high or too low NIHSS ratings (Figure 1). Finally, 358 patients receiving IVT were included (Table 1), with 230 (64.2%) in the pre-COVID-19 group and 128 (35.7%) in the post-COVID-19 group. No discernible baseline differences were found between the two groups. All the post-COVID-19 group patients underwent additional screening, such as a chest CT scan and a multidisciplinary evaluation. In the pre-COVID-19 group, the median admission NIHSS score (IQR) was 9 (6–13), but in the post-COVID-19 group, it was 11 (7–15). According to expectations, the patients admitted during the COVID-19 period exhibited more severe symptoms (p = 0.020). OTD time increased from 68 min (interquartile range [IQR] 40–111) before to 85 min (IQR 45–127) after the COVID-19 pandemic (p = 0.001). DTN time increased from 50 min (IQR 40–75) before to 65 min (IQR 48–84) after the COVID-19 pandemic (p = 0.048). Compared with the pre-COVID-19 group, post-COVID-19 patients with IVT treatment had a higher rate of symptomatic intracranial hemorrhage (sICH) (p = 0.043). No significant differences were found in early neurological improvement, in-hospital mortality, mRS score (0-2) pre-admission, and at discharge between the two groups (Table 1).
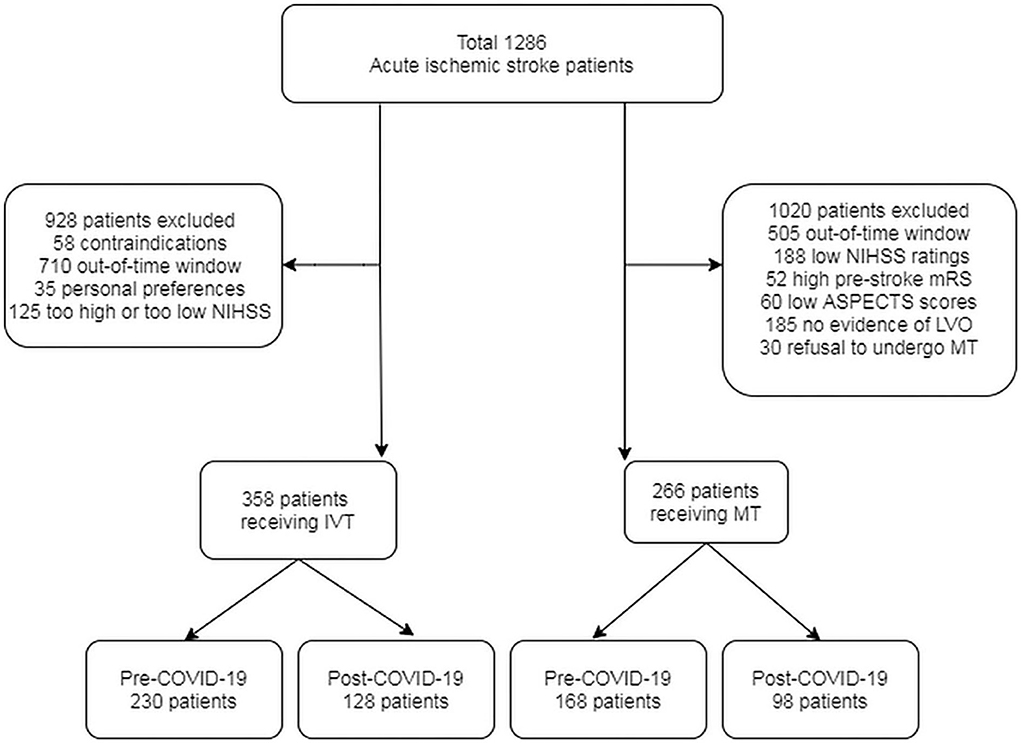
Figure 1. The flow chart of acute stroke patients receiving IVT or MT treatment during pre- and post-COVID-19 period.
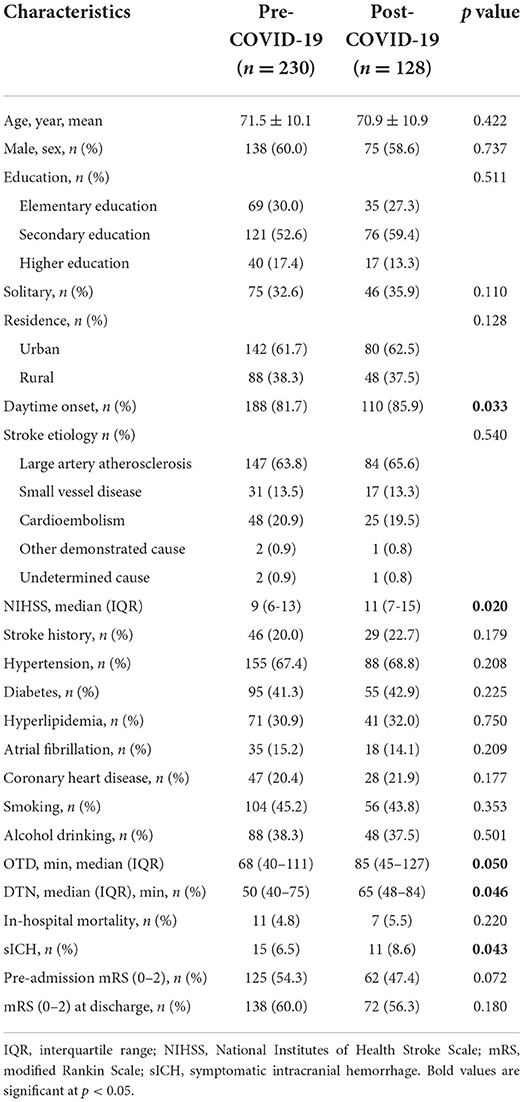
Table 1. Characteristics of acute ischemic stroke patients with intravenous thrombolysis treatment before and during the COVID-19 pandemic.
Of the patients enrolled, 1020 of them were excluded for out-of-time window, low NIHSS scores, high pre-stroke mRS scores, low ASPECTS, no evidence of large artery occlusion, or refusal to undergo MT (Figure 1). A total of 266 patients with intracranial large artery occlusion were finally included (Table 2); of these, 168 (63.2%) were in the pre-COVID-19 group and 98 (36.8%) in the post-COVID-19 group. Compared with the pre-COVID-19 group, post-COVID-19 group patients had a higher NIHSS score [12 (9–17) vs. 10 (7–15), p = 0.042], and a lower percentage of pre-admission mRS (0–2) [68 (37.5%) vs. 29 (29.6%), p = 0.011], but no significant differences were found in the remaining baseline characteristics, including ASPECTS and the percentage of anterior circulation. The OTD time was 72 (38–118) min vs. 87 (41–136) min in the pre- and post-COVID-19 groups, p = 0.012. The DTP time was 120 (112–148) min vs. 160 (125–199) min before and after the pandemic, p = 0.002. No significant difference was found in the mTICI 2b-3 scores of the two groups (86.2 vs. 82.4 %, p = 0.088). Adverse events, including sICH, were not significantly different between the two groups (Table 2).
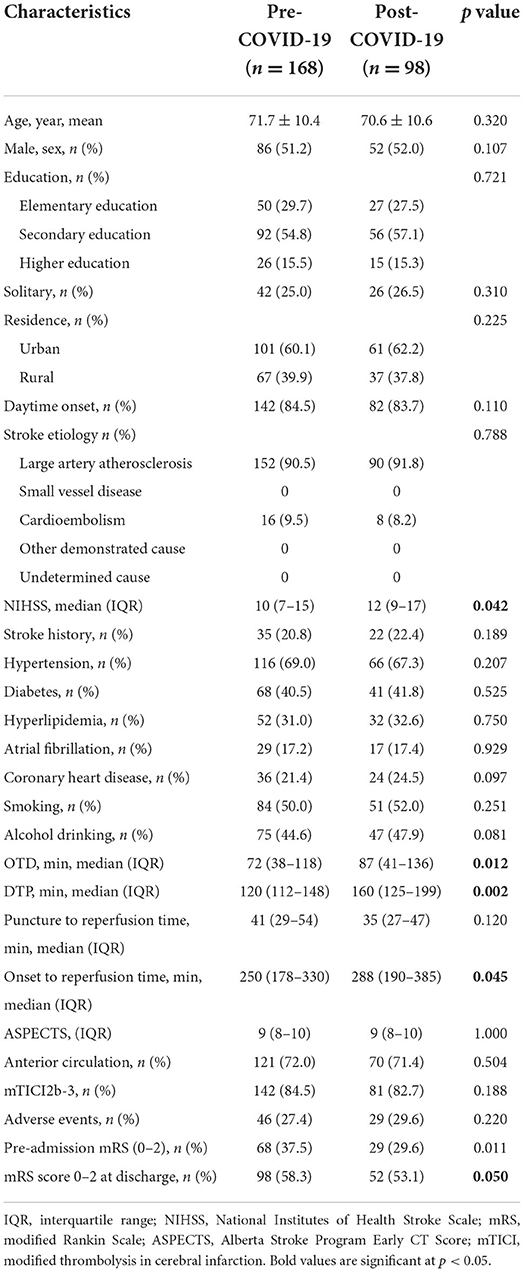
Table 2. Characteristics of acute ischemic stroke patients with mechanical thrombectomy treatment before and after the COVID-19 pandemic.
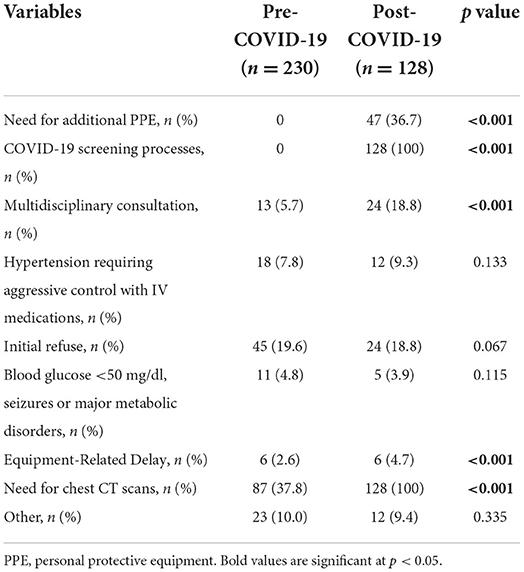
The post-COVID-19 group underwent a substantial delay for patients receiving IVT or MT due to the need for additional PPE (p < 0.001), COVID-19 screening processes (p < 0.001), multidisciplinary consultation (p < 0.001), and chest CT scans (p < 0.001). No significant differences were found in the proportion of patients receiving intravenous antihypertensive medication, family hesitancy about therapy, or hypoglycemia between the two groups before IVT or MT (Tables 3, 4).
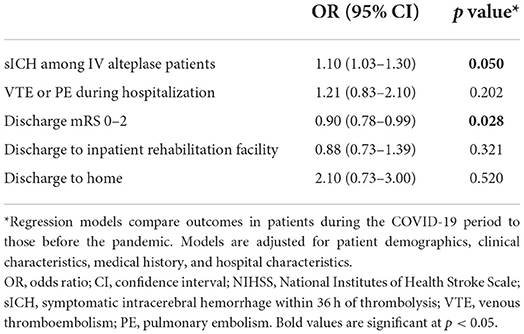
Table 5 presents the potential influencing factors for the prognosis of AIS by multivariate logistic regression analysis. Compared with the patients before the pandemic, the patients during the COVID-19 lockdown period had an odds ratio (OR) of 1.10 (95% confidence interval [CI], 1.03–1.30) for spontaneous intracranial hemorrhage, and an OR of 0.90 (95% CI, 0.78–0.99) for mRS scores 0–2 at discharge, whereas no significant differences were found in the proportion of lower extremity venous thromboembolism (VTE) or pulmonary embolism (PE) during hospitalization and discharge disposition (home, inpatient rehabilitation).
In the current study, we found increasing age, OR: 1.81 (1.18–2.92), p = 0.005; worse pre-admission mRS, OR: 1.30 (1.15–1.48), p = 0.010; higher NIHSS score at admission, OR: 2.84 (1.45–4.8), p < 0.001; large vessel occlusion, OR: 2.02 (1.32–3.05), p < 0.001; admission during the lockdown period, OR: 1.22 (1.02–1.34), p = 0.050; mTICI grade 2b-3 after MT, OR: 0.44 (0.25–0.67), p < 0.001, to be significantly associated with poor outcomes in AIS (mRS ≥ 3) by logistic regression, whereas sex, history of stroke, hypertension, diabetes, hyperlipidemia, atrial fibrillation, and coronary artery disease were not (Table 6).
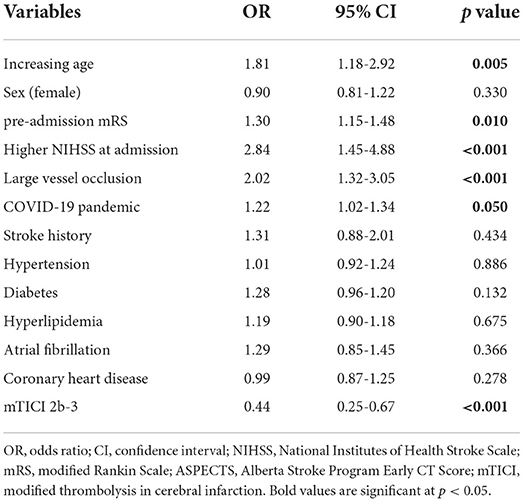
Table 6. Multivariate logistic regression analysis of influencing factors for short-term clinical poor outcomes (mRS ≥ 3).
Discussion
In this retrospective study with focus on the COVID-19 lockdown period, we evaluated the impact of the pandemic on treatment delays and short-term clinical outcomes in patients with AIS. In this study, DTN time and DTP time were significantly longer during the COVID-19 period than during the pre-COVID-19 period. In our previous study, we found that the onset-to-door time was significantly prolonged during the COVID-19 pandemic compared with that in the pre-pandemic period (16). In this study, the need for additional PPE, viral nucleic acid testing, and chest CT scans were the main causes of in-hospital delay during the pandemic. PPE contributed to the delay in treatment times mainly due to the shortage or unavailability including the filtering facepiece respirators and gowns in the early lockdown period. In addition, the pandemic in itself was an independent risk factor for treatment delay and short-term unfavorable outcomes in patients with treated stroke. A large registry study involving 55,296 patients with AIS showed that in-hospital mortality was higher in patients with delayed thrombolytic therapy and that treatment delay was associated with poor clinical outcomes (17). According to a previous study, patients admitted during the COVID-19 pandemic experienced pre- and in-hospital treatment delays to varying extents (16).
Recent research has shown that even minor delays might have a negative impact on clinical outcomes in the short term (18). In the current study, the COVID-19 pandemic played a significant role in early adverse outcomes in patients with AIS. This effect is mainly attributed to the pandemic, which exacerbated certain time delays. The proportion of VTE or PE during hospitalization was not significantly associated with the COVID-19 pandemic partly due to the relatively short hospital stay in this study. In addition, a marginal increase in in-hospital mortality was noted among patients with AIS during the pandemic, which may have been due to the greater severity of stroke (19). Many patients with mild to moderate stroke avoided hospital admissions during the lockdown period, as indicated by the reports from some countries, which showed a 50–80% reduction in acute stroke admissions (20). The increased NIHSS score in the post-COVID-19 period partially supports this proposition. A similar pattern of delay in seeking medical care due to the fear of being infected within the hospital was observed during the Ebola epidemic in West Africa (21).
Our study also indicated that admission during the pandemic was an independent risk factor for short-term mortality and other adverse outcomes. It is crucial to identify and examine specific stroke workflows to improve stroke reperfusion rates and clinical outcomes. According to a previous study, inadequate imaging techniques may result in delays (22). However, this finding was unnoticed in our study and some other studies (23, 24). Kansagra et al. (25) reported a 39% decrease in the use of stroke imaging during the early COVID-19 pandemic period. Among these phases, delays from imaging to thrombolysis were the main factor responsible for the overall delay. Therefore, future research concentrating on imaging flow may be crucial to achieving a reduction in treatment delays in the ongoing pandemic. The findings of the current investigation (26) indicate that the prolongation of DTN time and DTP time can have a negative impact on short-term outcomes.
The strength of this study was that it included a large number of patients with non-COVID strokes based on real-world data. While previous studies from China for the most part focused on Wuhan, which was the initial area of the COVID-19 outbreak, we collected data from three provinces away from Wuhan, which could reflect the impact of the pandemic on stroke management outside the epicenter. Another strength of our study was that we examined how the pandemic affected treatment delays and clinical outcomes in patients with treated strokes and also identified the pandemic as an independent risk factor for poor short-term prognosis in AIS.
Limitation
A main limitation of this study was its retrospective, observational design, which made it prone to selection bias. Second, because COVID-19 -infected patients were not included in this study, we could not analyze any potential detrimental effects of the virus on patient prognosis. Third was the lack of data on the other changes that could have contributed to the delay such as adjustments made to triage protocols and availability of staff due to extremely busy emergency personnel during the earliest stages of the pandemic. Furthermore, the time of treatment delay in bridging therapy, which means patients received both thrombolysis and MT treatment, was not specifically collected by some centers, so the potential detrimental effects on the bridging therapy were not analyzed. In addition, the long-term effects of treatment delay on the 90-day functional outcomes of patients with AIS were not examined in the current study. Therefore, prospective multicenter studies with sizable sample numbers are needed to clarify the aforementioned findings.
Conclusion
In-hospital delays during the COVID-19 pandemic negatively impacted the treatment of non-COVID strokes in China. Given that anti-COVID-19 measures are evolving into medical norms, stroke centers need to evaluate local practice patterns to optimize the management processes and lessen the impact of the pandemic on clinical outcomes in patients with AIS.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
SG, JL, and ZD: study design, interpretation of results, and manuscript drafting. SG, YB, JL, HZ, and HS: study design and interpretation of results. YY, ZD, YB, JL, HS, HZ, and SZ: data collection. WT, YY, SZ, JL, YB, ZD, HS, and SG: study design, statistical analysis, and critical revision of the manuscript. SG and WT: interpretation of results, critical revision of the manuscript, has full access to all of the data in the study, took responsibility for the integrity of the data, and the accuracy of the data analysis. All authors contributed to the article and approved the submitted version.
Funding
The work was supported by the Foundation of Jiangsu Province of China (Z2021001), the Health Institute of Wuxi (M202157), and Top Talent Support Program for young and middle-aged people of Wuxi (Yixing) Health Committee (BJ2020108).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW, et al. Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA. (2016) 316:1279–88. doi: 10.1001/jama.2016.13647
2. Pandey AS, Daou BJ, Tsai JP, Zaidi SF, Salahuddin H, Gemmete JJ, et al. Letter: COVID-19 pandemic: the bystander effect on stroke care in Michigan. Neurosurgery. (2020) 87:E397–9. doi: 10.1093/neuros/nyaa252
3. Pop R, Quenardelle V, Hasiu A, Mihoc D, Sellal F, Dugay MH, et al. Impact of the Covid-19 outbreak on acute stroke pathways: insights from the Alsace region in France. Eur J Neurol. (2020) 19:1–5. doi: 10.1111/ene.14316
4. Hoyer C, Ebert A, Huttner HB, Puetz V, Kallmünzer B, Barlinn K, et al. Acute stroke in times of the COVID-19 pandemic: a multicenter study. Stroke. (2020) 51:2224–7. doi: 10.1161/STROKEAHA.120.030395
5. Zhao J, Li H, Kung D, Fisher M, Shen Y, Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. (2020) 51:1996–2001. doi: 10.1161/STROKEAHA.120.030225
6. Teo KC, Leung WC, Wong YK, Liu RK, Chan AH, Choi OM, et al. Delays in stroke onset to hospital arrival time during COVID-19. Stroke. (2020) 51:2228–31. doi: 10.1161/STROKEAHA.120.030105
7. Tejada Meza H, Lambea Gil Á, Sancho Saldaña A, Villar Yus C, Pardiñas Barón B, Sagarra Mur D, et al. Ischemic stroke in the time of coronavirus disease 2019. Eur J Neurol. (2020) 27:1788–92. doi: 10.1111/ene.14327
8. Yang B, Wang T, Chen J, Chen Y, Wang Y, Gao P, et al. Impact of the COVID-19 pandemic on the process and outcome of thrombectomy for acute ischemic stroke. J Neurointerv Surg. (2020) 12:664–8. doi: 10.1136/neurintsurg-2020-016177
9. Schirmer CM, Ringer AJ, Arthur AS, Binning MJ, Fox WC, James RF, et al. Delayed presentation of acute ischemic strokes during the COVID-19 crisis. J Neurointerv Surg. (2020) 12:639–42. doi: 10.1136/neurintsurg-2020-016299
10. Gagliano A, Villani PG, Manelli A, Paglia S, Bisagni PA, Perotti GM, et al. COVID-19 epidemic in the middle province of Northern Italy: impact, logistics, and strategy in the first line hospital. Disaster Med Public Health Prep. (2020) 24:1–5. doi: 10.1017/dmp.2020.51
11. Tam CF, Cheung KS, Lam S, Wong A, Yung A, Sze M, et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. (2020) 13:e006631. doi: 10.1161/CIRCOUTCOMES.120.006631
12. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. (2019) 50:e344–418. doi: 10.1161/STR.0000000000000211
13. Ortega-Gutierrez S, Farooqui M, Zha A, Czap A, Sebaugh J, Desai S, et al. Decline in mild stroke presentations and intravenous thrombolysis during the COVID-19 pandemic: The society of vascular and interventional neurology multicenter collaboration. Clin Neurol Neurosurg. (2021) 10:64–36. doi: 10.1016/j.clineuro.2020.106436
14. Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann Intern Med. (2007) 147:573–7. doi: 10.7326/0003-4819-147-8-200710160-00010
15. National Stroke Prevention Committee National National Health Commission of the People's Republic of China the the Writing Group of the Expert Consensus on National Stroke Emergency Map. Expert consensus on stroke emergency map during the epidemic of corona virus disease 2019 (first edition). Int J Cerebrovasc Dis. (2020) 28:321–5. doi: 10.3760/cma.j.issn.16734165.2020.05.001
16. Gu S, Dai Z, Shen H, Bai Y, Zhang X, Liu X, et al. Delayed Stroke Treatment during COVID-19 Pandemic in China. Cerebrovascular diseases (Basel, Switzerland). (2021) 50:715–21. doi: 10.1159/000517075
17. Kamal N, Sheng S, Xian Y, Matsouaka R, Hill MD, Bhatt DL, et al. Delays in door-to-needle times and their impact on treatment time and outcomes in get with the guidelines-stroke. Stroke. 48:946–954. doi: 10.1161/STROKEAHA.116.015712
18. Siegler JE, Zha AM, Czap AL, Ortega-Gutierrez S, Farooqui M, Liebeskind DS, et al. Influence of the COVID-19 pandemic on treatment times for acute ischemic stroke: The Society of Vascular and Interventional Neurology Multicenter Collaboration. Stroke. 52:40–47. doi: 10.1161/STROKEAHA.120.032789
19. Siegler JE, Heslin ME, Thau L, Smith A, Jovin TG. Falling stroke rates during COVID-19 pandemic at a comprehensive stroke center. J Stroke Cerebrovasc Dis. (2020) 29:104953. doi: 10.1016/j.jstrokecerebrovasdis.2020.104953
20. Wu Y, Chen F, Wang Z, Feng W, Liu Y, Wang Y, et al. Reductions in hospital admissions and delays in acute stroke care during the pandemic of COVID-19. Front Neurol. (2020) 11:584734. doi: 10.3389/fneur.2020.584734
21. McQuilkin PA, Udhayashankar K, Niescierenko M, Maranda L. Health-care access during the ebola virus epidemic in Liberia. Am J Trop Med Hyg. (2017) 97:931–6. doi: 10.4269/ajtmh.16-0702
22. Markus HS, Brainin M. COVID-19 and stroke- A global World Stroke Organization perspective. Int J Stroke. (2020) 15:361–4. doi: 10.1177/1747493020923472
23. Briard JN, Ducroux C, Jacquin G, Alesefir W, Boisseau W, Daneault N, et al. Early impact of the COVID-19 pandemic on acute stroke treatment delays. Can J Neurol Sci. (2021) 48:122–6. doi: 10.1017/cjn.2020.160
24. Padmanabhan N, Natarajan I, Gunston R, Raseta M, Roffe C. Impact of COVID-19 on stroke admissions, treatments, and outcomes at a comprehensive stroke centre in the United Kingdom. Neurol Sci. (2020) 42:15–20. doi: 10.1007/s10072-020-04775-x
25. Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of Covid-19 on stroke evaluation in the United States. N Engl J Med. (2020) 383:400-1. doi: 10.1056/NEJMc2014816
26. Jillella D, Nahab F, Nguyen T, Abdalkader M, Liebeskind D, Vora N, et al. Delays in thrombolysis during COVID-19 are associated with worse neurological outcomes: the Society of Vascular and Interventional Neurology Multicenter Collaboration. J. Neurol. (2022) 269:603–8. doi: 10.1007/s00415-021-10734-z
Keywords: acute stroke, COVID-19, intravenous thrombolysis, mechanical thrombectomy, treatment delay
Citation: Gu S, Li J, Shen H, Dai Z, Bai Y, Zhang S, Zhao H, Zhou S, Yu Y and Tang W (2022) The impact of COVID-19 pandemic on treatment delay and short-term neurological functional prognosis for acute ischemic stroke during the lockdown period. Front. Neurol. 13:998758. doi: 10.3389/fneur.2022.998758
Received: 20 July 2022; Accepted: 26 September 2022;
Published: 20 October 2022.
Edited by:
Bin Qiu, Yale University, United StatesReviewed by:
Fadi Nahab, Emory University, United StatesAlicia Zha, The Ohio State University, United States
Amy Starosciak, Baptist Health South Florida, United States
Copyright © 2022 Gu, Li, Shen, Dai, Bai, Zhang, Zhao, Zhou, Yu and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wuzhuang Tang, staff1987@yxph.com
 Shiyuan Gu
Shiyuan Gu Jie Li1
Jie Li1