- 1School of Medicine, Guilan University of Medical Sciences, Rasht, Iran
- 2School of Medicine, Iran University of Medical Sciences, Tehran, Iran
- 3School of Medicine, Islamic Azad University of Medical Sciences, Tehran, Iran
- 4School of Medicine, Zahedan University of Medical Sciences, Zahedan, Iran
- 5School of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
- 6Avicennet, Tehran, Iran
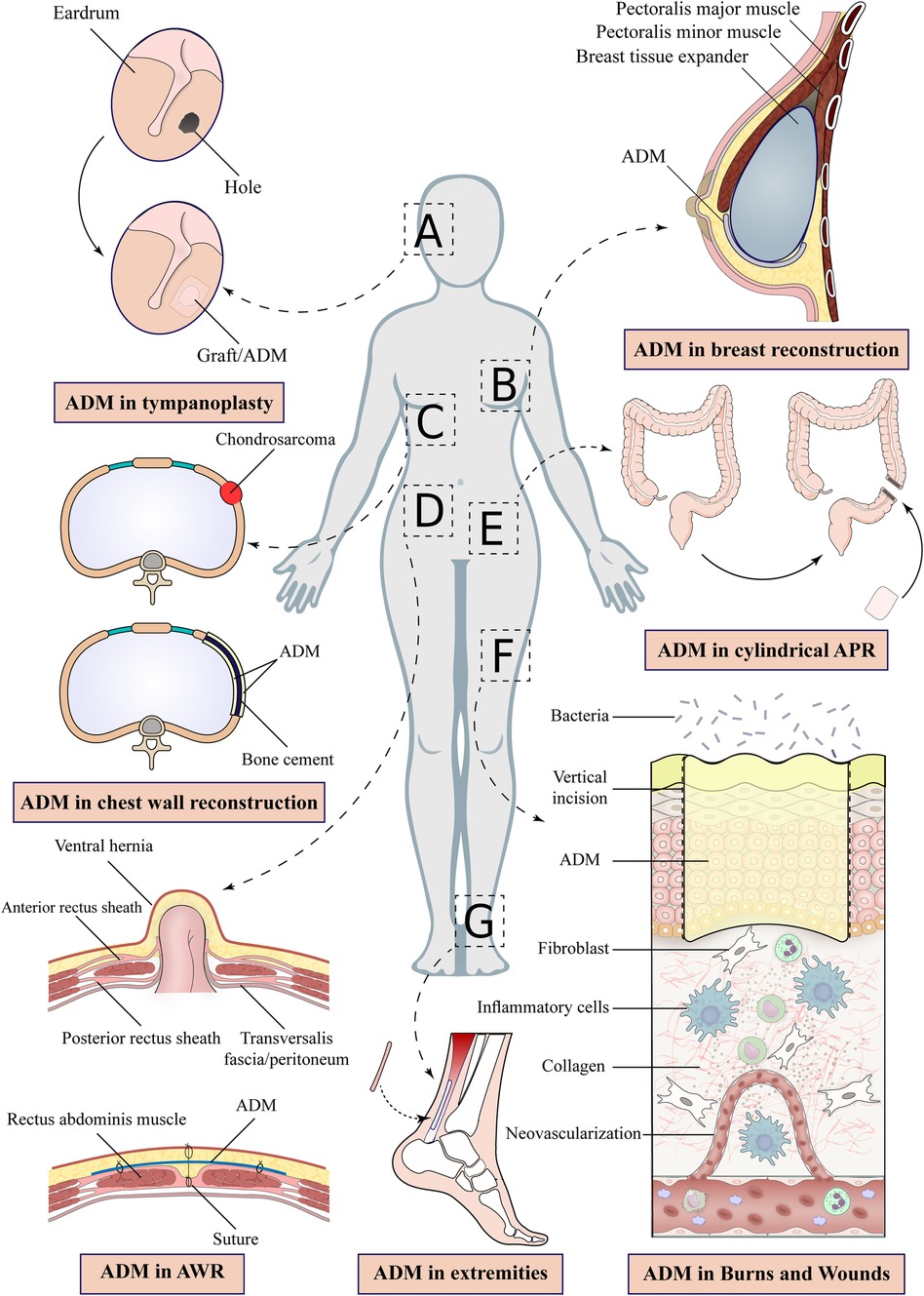
Modern tissue engineering has made substantial advancements that have revolutionized plastic surgery. Acellular dermal matrix (ADM) is an example that has gained considerable attention recently. ADM can be made from humans, bovines, or porcine tissues. ADM acts as a scaffold that incorporates into the recipient tissue. It is gradually infiltrated by fibroblasts and vascularized. Fortunately, many techniques have been used to remove cellular and antigenic components from ADM to minimize immune system rejection. ADM is made of collagen, fibronectin, elastin, laminin, glycosaminoglycans, and hyaluronic acid. It is used in critical wounds (e.g., diabetic wounds) to protect soft tissue and accelerate wound healing. It is also used in implant-based breast reconstruction surgery to improve aesthetic outcomes and reduce capsule contracture risk. ADM has also gained attention in abdominal and chest wall defects. Some studies have shown that ADM is associated with less erosion and infection in abdominal hernias than synthetic meshes. However, its higher cost prevents it from being commonly used in hernia repair. Also, using ADM in tendon repair (e.g., Achilles tendon) has been associated with increased stability and reduced rejection rate. Despite its advantages, ADM might result in complications such as hematoma, seroma, necrosis, and infection. Moreover, ADM is expensive, making it an unsuitable option for many patients. Finally, the literature on ADM is insufficient, and more research on the results of ADM usage in surgeries is needed. This article aims to review the literature regarding the application, Benefits, and costs of ADM in reconstructive surgery.
1. Introduction
Traditionally, autologous tissue grafts and synthetic materials have been used in reconstruction surgery, but each has its disadvantages (1). With autologous tissue graft, the morbidity of the second (donor) surgical site and the patients' more painful recovery period were significant problems (1). While with Synthetic materials, infection is always a risk (2). Thus, reconstructive surgery still needs a suitable material (2).
Acellular dermal matrix (ADM) is a biological graft that contains neither cellular nor antigenic components to avoid immunogenicity (3). Therefore, it has been recognized as a good substitute material for plastic and reconstructive surgeries (4). ADM can be obtained from humans, bovine, and porcine tissues (2). ADM comprises collagen fibers, fibronectin, elastin, laminin, glycosaminoglycans, and hyaluronic acid (2, 5, 7, 8). It serves as a scaffold that is gradually vascularized and cellularized by the host (2, 6, 8–10). ADM is utilized in aesthetic and reconstructive surgeries of nasal and oral cavities, breast, and abdominal walls (2, 4, 10, 11). It is also used in burn and diabetic wounds (4, 6, 9).
It should be noted that ADM is not supposed to substitute a full layer of skin tissue due to its lack of epidermis (2). By using ADM, instead of a full-thickness skin graft, only a thin layer of skin graft is needed leading to less scar formation at the donor site (2).
Many studies have shown favorable results of ADM in implant-based breast reconstructions with low complication rates (2). Also, some research showed faster healing of diabetic foot ulcers with ADM than standard treatment (12). Several studies have also evaluated the outcomes of biological mesh (i.e., ADM) vs. synthetic mesh in abdominal hernia repair, but the results are contradictory, and more research is warranted (13).
Despite its advantages, ADM is still a foreign material, and infection, necrosis, and seroma are possible complications (14). Also, ADM is expensive and can only be a reasonable choice for some patients (2).
Unfortunately, the data on the clinical outcome of ADM usage in many surgeries is still insufficient (8). Research on the cost-effectiveness of ADM is also inadequate, and more work is warranted to clarify these matters (8). This review highlights ADM applications in reconstructive surgery and its costs and benefits.
2. Head & neck
ADM is increasingly used in cosmetic and reconstructive head and neck surgeries. It is applied in periorbital soft tissue, dura mater, extraoral and intraoral, and oropharyngeal defects. It also has applications in skeletal support, nasal soft tissue, and tympanic membrane repair (1, 15–23).
Many studies have worked on using ADM in cleft palate repair (1, 10, 17, 18, 20, 21, 23–54). Achieving a tension-free, water-tight closure has always been a challenge in palatoplasty because otherwise, the patient may predispose to a fistula formation (55–57). The use of ADM in palatoplasty has been associated with better repair and less fistula formation (55–57). In palatoplasty, a thin (nearly 0.5 mm) 2 × 4-cm piece of ADM is sutured to the nasal lining (58). These measures change due to the availability of ADMs at different surgical facilities (28, 55, 58). This technique results in a more robust repair with a lower chance of fistula formation (28). Helling et al. (58) found that in a case series of 31 ADM palatoplasties, the rate of fistula formation was lower (3.2%) compared to historical cohorts (about 8%) (58). To support these findings, additional research with bigger sample sizes is necessary (56).
The disadvantage of ADM is its high price of approximately $135. Fortunately, the significant financial burden of fistula repair surgery makes this price seem acceptable (55, 58). Aside from the cost, ADM is an avascular graft, which means that necrosis and infection are its potential consequences (28).
Skull base tumor excision has always been challenging (1, 10, 17, 18, 20, 21, 23–54). Even with the endoscopic excision, the risk of complications (e.g., rhinorrhea) remains high (59, 60). As a result, identifying an appropriate material for CSF rhinorrhea repair following tumor excision is critical (10, 18–20, 22–24, 26–28, 30–54, 61–70). In a randomized control trial study, Zhong et al. (59) compared the clinical outcome of CSF leakage repair using ADM with Turbinate Flap. They used a fascia lata graft to repair the defect in the dura mater. Then they covered the fascia lata with ADM and adhered the ADM to the nasal mucosa. Eventually, Vaseline gauze is inserted into the nasal cavity (59). They found that both ADM and the turbinate flap had corresponding clinical outcomes. Thus, ADM might be a safe alternative for CSF rhinorrhea repair following skull base tumor excision (59).
Youngerman et al. (71) also compared the ADM and autologous fascia lata graft in CSF leakage repair. They opted to use ADM or fascia lata to repair the dural lesions with substantial CSF leakage. The ADM or fascia lata was then covered with a polyethylene implant.
They discovered similar clinical outcomes in the two groups. Accordingly, ADM is a viable option for this operation since it eliminates the requirement to obtain an autologous fascia lata graft from the patient's tissue (71). Also, Mericli et al. (72), in a case report, used a 4 × 1 cm piece of ADM with a thickness of 1–2.3 mm for CSF repair and found a successful result (72). These measures depend on the patient's needs and the surgical approach (72).
To confirm these findings, more research on the efficacy and cost-effectiveness of ADM in CSF rhinorrhea repair is needed (71).
Nasal septal perforation management remains a serious issue in otorhinolaryngology (18, 23, 25, 28, 30, 31, 33, 36, 38–54, 60, 64, 68–70, 73). Several treatment strategies have been presented so far, but their success rate is debatable (25). Prosthetic nasal buttons are a non-invasive form of treatment, although they are often poorly tolerated by patients (25). Conrad et al. (25) employed an ADM graft as a substitute material for septal perforations (25). They demonstrated that ADM administration is an effective approach for minimizing postoperative symptoms (nasal obstruction, sleep issues) (25). Nevertheless, there is insufficient data to support this finding (25, 41).
The use of ADM in the treatment of rhinophyma has recently attracted interest (74, 75). Torresetti et al. (74), in a case report, described the use of an ADM with the size of 5 × 5-cm on a severe rhinophyma. Postoperatively, the nasal shape and functions had improved, but the aesthetic results were unsatisfactory, and the patient still needed cosmetic procedures (74). They suggest that despite ADM's efficacy in rhinophyma surgery, more aesthetic procedures may be needed (74). Another factor that physicians should consider is the higher expense of ADM compared to other surgical procedures (74).
On the contrary, Ozkan et al. (75) used ADM in another severe rhinophyma case and found a successful aesthetic and functional result (75). As the results are inconclusive, additional research is required to shed light on this topic (75).
Recent studies have shown favorable results regarding the use of ADM in Tympanic membrane reconstruction (10, 18–20, 22–24, 26–28, 30–54, 61–70).
Lee et al. (76), in a clinical trial, compared the results of tympanoplasty using ADM to the standard approach (using tragal perichondrium) (Figure 1A) (76). For the ADM group, they used an ADM graft with a size of 1.5 × 2-cm and a thickness of 0.3–0.5 mm (76). They demonstrated that ADM yielded similar hearing outcomes and a shorter surgical duration than conventional methods (76).
Research has suggested that ADM is a suitable material for rhinoplasty (18, 22, 23, 25, 28, 30, 31, 33, 36, 38–54, 60, 62, 64, 68–70, 73). Previous studies have shown a low rate of extrusion and infection in ADM-used rhinoplasties (77). Park et al. (78) have studied the use of ADM in primary and revision dorsal augmentation rhinoplasties. They showed that ADM can be used in both situations and has a low complication rate (78). Other studies have shown that ADM is a biocompatible material that gives a natural appearance to the nose, long-term integrity, and low infection and extrusion risk (77).
In a retrospective study, Yang et al. (79) assessed the utility of ADM in dorsal augmentation rhinoplasties (79). They stated that ADM is an ideal substitute for autologous tissue due to the reduction of donor site morbidity. They showed successful results of ADM with the patient satisfaction score of 81.02 out of 100. Moreover, none of the patients experienced any major complications (79).
In a case series, Sherries et al. (80) investigated the complications of ADM in rhinoplasty. They found no infection, skin discoloration, seroma, septal perforation, and extrusion (80). According to their study, ADM is a safe and effective substitute for traditional methods (80).
3. Chest
Chest wall defects are frequently caused by tumor herniation and resection (1, 2, 21, 29, 30, 81–91). Defects in the chest wall impair the strong framework that supports breathing and safeguards the viscera (92). Loss of chest wall integrity leads to devastating complications such as lung hernia, hemithorax shrinkage, and paradoxical chest wall motion (50). Consequently, it is essential to repair the chest wall properly (50). The material typically employed in chest wall repair is synthetic mesh (1, 2, 21, 29, 30, 81–91). It does, however, have drawbacks (for example, infection) (93). ADM has so been the subject of investigations to replace the mesh in these operations (Figure 1D) (1, 2, 21, 29, 30, 33, 36, 68, 81–91, 94–101).
In a study, Heo et al. (29) did chest wall repair with ADM on six patients following tumor resection. This technique employed two layers of ADM and bone cement (29). They discovered positive outcomes, and none of the patients experienced postoperative complications or soft tissue defects (29). They demonstrated the safety of ADM and its substitutability in chest wall repair after tumor removal (Supplementary Table S1) (29).
Also, Giordano et al. (93), in a study, compared the postoperative complications of mesh vs. ADM in chest wall reconstruction. They discovered a lower rate of surgical site infection in the ADM group, demonstrating ADM's suitability for patients at higher risk of infection (93).
Yoon et al. (102) also used ADM to repair a chest wall defect caused by a sternal metastatic tumor excision (102). To repair the defect, a 12 cm × 12 cm piece of ADM was used in this technique. The patient had a successful clinical outcome, and no complications emerged (102).
Rigid prosthetics were previously used for large chest wall defects (89). These prosthetics were inflexible, resulting in reduced lung capacity and even pain. As foreign bodies, they also increased the likelihood of infection (89). Following chondrosarcoma resection, Ely et al. (89) decided to repair a sternal defect with an ADM and soft tissue flap. The patient had excellent clinical outcomes with no complications over a two-year follow-up (89). They showed that ADM as a biological mesh could repair large sternal defects (Figure 1C) (89).
Stanizzi et al. (103) used ADM in a lung hernia and severe pectoralis major muscle retraction following a mini-thoracotomy for mitral valve surgery (103). The lung hernia was reduced following surgery, and it did not recur during a six-year follow-up (103). They discovered excessive serum production after surgery, so the patient had a drain for 15 days to avoid seroma. As a disadvantage, ADM is more expensive than synthetic meshes or autologous tissues, which keeps it from being a popular repair method (103).
4. Breast
Breast cancer is the most common cancer in women worldwide, causing numerous social and psychological issues (104–106). Several surgical options are being employed for breast reconstruction surgery. The use of ADM in implant-based breast reconstruction following mastectomy has received a lot of attention recently (2, 83, 91, 94, 104, 107–112). The advantages of ADM in implant-based breast surgery include implant stabilization, improved aesthetic outcomes, and reduced capsular contracture risks, donor site morbidity, and postoperative pain (34, 83, 86, 109, 112–114).
Following a mastectomy, implant-based breast reconstruction is a popular option (Figure 1B) (83). Yet, one of the risks of this technique is capsular contracture (115). Previous research has suggested that ADM-covered breast implants are less prone to capsular contracture (115). Stump et al. (115) decided to compare the capsular contracture rate in breast implants with and without ADM in primates (115). They found that ADM-covered breast implants significantly reduce the rate of capsule contracture. Enclosing the implant in ADM prevents the immune system from recognizing it and forming a fibrous capsule around it (115). More research is needed to determine whether this result is repeatable in humans (115).
As previously stated, ADM is a costly option compared to other reconstructive materials (116). In a cost analysis study, Jensen et al. (116) compared the cost of implant-based breast reconstruction with and without ADM. Surprisingly, they discovered that implant-based breast reconstruction with ADM is less expensive ($10,240 vs. $10,584 for a 6 cm × 16 cm ADM sheet). With a more miniature ADM sheet (6 cm × 12 cm), the cost drops to $9673 (116). These estimates were derived from a university-based hospital in Canada, and more research on different medical centers is needed to prove this cost-effectiveness (116).
Nevertheless, the use of ADM in implant-based breast reconstruction has disadvantages (114, 117).
The most frequently mentioned ADM complications in the literature are necrosis, seroma, hematomas, and infection (2, 104, 118). In a randomized control trial, Hansson et al. (119) compared the first-year complication rate of a biological mesh (ADM) with that of a synthetic mesh in implant-based breast surgeries (119). They found a higher implant loss rate due to infection in ADM cases than in synthetic mesh cases (12.5% vs. 0%). They hypothesized that this increased infection rate was due to higher seroma formation in ADM patients (38% vs. 3.8%) (119).
Also, Dikmans et al. (120), in a randomized control trial, investigated the rate of adverse events of implant-based breast reconstructions with and without ADM. They showed that skin necrosis (11% vs. 1%), Hematoma formation (3% vs. 2%), and wound infection (8% vs. 2%) were all higher in the ADM group. According to their findings, the ADM group had a lower rate of seroma formation (3% vs. 2%), which contradicts previous research (120).
Lohmander et al. (99) also compared the complications of implant-based breast surgeries with and without ADM. They discovered that the ADM group has a higher rate of skin blisters (9% vs. 0%) and infection rates (14% vs. 6%). In another study, Kumar et al. (96) also suggested that ADM is associated with a higher rate of postoperative complications, especially in overweight women (96).
Some patients develop erythema following ADM breast reconstruction surgery (118). This condition is known as red breast syndrome (118). Danino et al. (118) investigated red breast syndrome cases and found bacterial biofilms on all the ADMs, hypothesizing that these biofilms could be linked to the syndrome (118).
5. Abdomen
Despite numerous options for abdominal wall reconstruction, surgeons have long struggled to find an ideal mesh (1, 16, 21, 29, 83, 87, 89, 121–126).
In the past, abdominal hernias were treated with synthetic meshes such as polypropylene (82). Despite their strength, their complications, like erosion into the bowel wall, adhesion, infection, and fistula formation, have limited their use in abdominal wall reconstruction (81). So, biological meshes such as ADM have recently gained attention (1, 16, 21, 29, 33, 34, 38, 45, 83, 87, 89, 101, 121–126, 127). ADM is biocompatible, integrates into the surrounding tissue, and allows vascularization (1, 16, 21, 29, 33, 34, 38, 45, 83, 87, 89, 101, 121–126, 127). The revascularization of ADM by the host makes it resistant to infection (1, 10, 16, 21, 29, 33, 34, 38, 45, 52, 83, 87, 89, 101, 121–126, 127–129).
Cevasco et al. (130) reviewed the pros, cons, and indications of using different meshes (130). They showed that propylene meshes are long-lasting and suitable for use in extra-peritoneal clean hernias (130). Due to their high rate of erosion into the bowel wall, they are not recommended for intraperitoneal placement (130). Still, their low cost and easy application make them a good choice for many surgeries.
Cevasco et al. (130) also showed that ADM is a suitable substitute in contamination where other synthetic meshes are not recommended (130). Unfortunately, ADM costs more than synthetic mesh, preventing its widespread use (131).
In a systematic review, Fischer et al. (132) investigated the cost-effectiveness of different meshes in clean-contaminated hernias (132). Their study showed that synthetic mesh costs $15,776, while biological mesh costs $23,844 (132). In clean-contaminated hernia repair, synthetic mesh is still a cost-effective material (132). This view has been corroborated by other studies (133).
The data on the recurrence rate of hernia repair using ADM is scarce. Brewer et al. (134) showed that biologic mesh (ADM) has a lower recurrence rate than non-biologic mesh (24% vs. 77%) (134). In contrast, Darehzereshki et al. (135) found no significant difference between biologic and non-biologic mesh recurrence rates (135).
Garvey et al. (136) found that using ADM for abdominal wall reconstruction resulted in 11.5% and 14.6% hernia recurrence rates after 3 and 5 years of follow-up, respectively (136).
More research is needed to determine the precise contribution of ADM to abdominal wall reconstruction (137).
6. Pelvis
There are various surgical methods for treating urogynaecological disorders, each with its own set of advantages and disadvantages (138). Synthetic materials can cause erosion, infection, hematoma, and dyspareunia (34, 46, 60, 121, 123, 129, 139–141). ADM is a biocompatible material that may be linked to a lower risk of complications, increased durability, and improved efficacy (34, 46, 60, 121, 123, 129, 138–141). The host vascularizes ADM sheets, lowering the risk of infection and making it an ideal choice for infected surgical sites (142).
Many studies have confirmed the benefits of ADM in vaginal reconstruction surgery (34, 46, 53, 54, 60, 121, 123, 129, 139–141, 143, 144). Gualtieri et al. (145) compared the effect of propylene mesh with porcine ADM on vaginal smooth muscle cells. They showed that vaginal smooth muscle cell proliferation is higher on ADM compared to synthetic mesh. This could explain why ADM produces better results and has a lower erosion rate than synthetic mesh (145).
ADM has also been used in the treatment of abdominoperineal resection, urogynaecological issues, and perineal wound complications (146, 147).
In a study, Han et al. (146) investigated the surgical complications in pelvic reconstruction using ADM following cylindrical abdominoperineal resection (Figure 1E) (146). In 11 patients, the perineal wounds healed two weeks after the operation. After a median follow-up of eight months, they concluded that ADM is a safe and suitable alternative for reconstructing large pelvic defects in patients after cylindrical abdominoperineal resection (146).
Tognetti et al. (147) concluded that synthetic materials are not recommended after some cases of pelvic exenteration and radical vulvectomy and that ADM is a suitable alternative in these cases (147).
ADM can have some negative side effects, such as hernia bulging, infection, seroma, and chronic pain (148–150). Various studies have found that the rate of seroma production ranges from 6% to 26% (146) (146). Unfortunately, there is insufficient data on the complications of ADM in pelvic reconstruction (151). According to Han et al. (146), despite the successful use of ADM in pelvic reconstruction, nearly 33% of patients experienced chronic pain and discomfort (146). This pain could also be attributed to the surgical procedure and wide excision (146, 151). The presence of chronic pain following biologic mesh has been echoed by other studies (151, 152).
Butler et al. (153) studied the use of ADM in pelvic reconstruction in cancer patients. They used an average of 4.5 (2 to 10) ADM sheets per defect (defect size approximately 435 cm2). They discovered that ADM had positive results for pelvic reconstruction, but its high cost prevents it from being used in many cases (153). Another potential disadvantage of ADM is its limited size. The largest available ADM is 8 × 12-cm, and for larger defects, ADM sheets need to be joined together (153). More research is required to elucidate the benefits of employing ADM over synthetic mesh (153).
ADM can manage complex pelvic defects by forming a barrier between the intra-abdominal contents and external flaps, preventing intestinal adhesion, obstruction, and fistula (50). There need to be more extensive trials comparing synthetic mesh to biological mesh and more studies on the cost-analysis of the ADM (151).
7. Extremities
In recent years, the use of ADM in extremity reconstructive surgery has increased (1, 10, 16, 19, 26, 30, 40, 46, 47, 62, 73, 97, 124, 139, 140, 154–158). ADM's applications in the extremities include soft tissue and tendon regeneration, heel and nail bed reconstruction, and burn and diabetic wound management (Figure 1G) (50).
Despite its thickness, the Achilles tendon can be torn and damaged (159, 160). To repair an Achilles tendon rupture, various augmentations such as autografts, xenografts, and allografts are used. Autografts are associated with complexity, donor site morbidity, and longer surgery time. Xenografts are associated with rejection risk. These issues have prompted some surgeons to abandon their use in favor of alternative materials such as ADM (159, 160).
Tendon repair has been successful with the use of ADM (1, 10, 16, 19, 26, 30, 40, 46, 47, 52, 54, 62, 73, 97, 124, 139, 140, 154–158, 161–163). ADM is an ideal scaffold for native cells and is ready to be vascularized by the host (40, 159). In a case series, Cole et al. (160) used a 5 cm × 5 cm piece of ADM for tendon augmentation and found successful results, with no complications or rerupture (160).
In the upper limb, lee et al. (163) conducted a randomized trial on the use of ADM in the repair of the flexor tendons of the III, IV, and V sections of the hand (163). They applied an ADM sheet over the repaired tendon and found good functional results with no peritendinous adhesions postoperatively (163). This study shows that ADM might act as an anti-adhesive physical barrier in hand tendon repair. They calculated that using ADM increases the cost of surgery by 15%, but since it cuts down on the need for reoperation (due to postoperative adhesions), this may be a fair trade-off (163). More studies with larger sample sizes are needed to corroborate this data (163).
In lower limb reconstruction, heel reconstruction is one of the most challenging procedures. Many studies have found ADM to be effective in heel reconstruction (1, 10, 16, 19, 20, 26, 30, 40, 46, 47, 52, 54, 62, 73, 97, 124, 139, 140, 154–158, 161). A case report of heel reconstruction using ADM and skin graft showed optimal gait function recovery and social participation (157). According to gait analysis, measured gait and posture were essentially normal with ADM (157). Nonetheless, the pressure distribution study revealed a slight imbalance, which could be attributed to the new morphology and sensitivity of the feet (157).
Fingertip injuries are common and can result in nail trauma; however, nail bed repair is challenging due to the exposed bone (164). ADM and subsequent skin graft can be utilized to repair nail bed injuries and loss of germinal matrix. Unfortunately, patients with complex crush trauma may not be good candidates for this method (164). In a study, Fiedler et al. (165) successfully used a monolayer bovine ADM to reconstruct a sterile nail bed (165). Still, they did not recommend this technique for nail beds with germinal matrix injuries (165). The cost of the specific ADM used in this study (single layer, 5.08 cm × 5.08 cm) is $2,266, making it impractical to use widely (165).
Management of extremity burn wounds is critical due to the risk of systemic infections and death (166–168). ADM can be utilized effectively in extremity burn repairs by minimizing wound contractions, lowering the risk of recurrence, and improving function (166–168). Additionally, it can be underlined that ADM grafts can be used on nerves, arteries, and tendons where skin grafts cannot integrate and result in contractures (167). It should be noted that ADM is not recommended in cases of compromised tissue vasculature or infection (167). In addition, Diabetic foot ulcers must be managed due to the risk of infection, amputation, and death (12, 169–172). Numerous articles have discussed the use of ADM in these types of wounds, and it has been shown to be effective in closing Diabetic foot ulcers (12, 169–172).
8. Burns and wounds
Severe burns can cause serious skin damage, and managing the aesthetic outcomes and potential infections of these injuries is critical (16, 21, 24, 31, 33, 44, 62, 64, 66–68, 99, 123, 139, 140, 147, 154, 162, 173–176). Full-thickness and some deep partial-thickness burns require skin transplantation (177–180). Split-thickness skin grafts, local flap coverage, and skin substitutes are materials used in transplantation. The disadvantages of these materials include morbidity of the donor site, risk of flap and graft complication, and failure.
As an acellular skin substitute, ADM incorporates into the wound and is gradually vascularized by the wound bed allowing infiltration of fibroblasts (16, 21, 24, 31, 33, 44, 62, 64, 66–68, 99, 123, 139, 140, 147, 154, 162, 173–176). These events protect the wound and prevent granulation tissue and scar formation (Figure 1F) (181).
Recently, self-assembled skin substitutes have been used to manage severe burn wounds. A Self-assembled skin substitute is a dermal substitute underlying an epidermis (182). Producing these materials is troublesome and takes nearly four weeks (182). According to Cloutier et al. (182), the addition of ADM to self-assembled skin substitutes reduces production time, increases cell proliferation, and reduces the possibility of rejection (182).
In a randomized control trial, Heimbach et al. (183) compared the result of ADM graft vs. conventional skin graft material (183). In the intervention group, they sutured the artificial dermis (ADM) to the wound, and 14 days later, when it was revascularized, they grafted it with a thin epidermis. They showed that the functional and aesthetic results were comparable (183). They found that the ADM group had a less hypertrophic scar, and the patients were more satisfied with the ADM (183). When compared to other methods, ADM requires a thinner layer of the epidermis, resulting in faster donor site healing (183).
Moreover, Demircan et al. (184) conducted a study on multiple burn wounds to confirm the positive outcomes of ADM and showed a successful graft outcome (184). They stated that the graft was comparable to normal skin regarding vascularization, elasticity, plasticity, texture, and color (184). They also came to promising results in terms of aesthetic and practical dimensions. This result confirms the influential role of ADM in dermal replacement (184). ADM is associated with rapid healing and satisfactory aesthetic and functional outcomes (184, 185). There is also the possibility of favorable outcomes following the closure of facial burn wounds in children (184).
Other studies on the effects of ADM on deep burns have yielded promising results (16, 21, 24, 31, 33, 44, 62, 64, 66–68, 99, 123, 139, 140, 147, 154, 162, 173–176).
Zhi-Qian Guo et al. (186) reported a combination of early dermabrasion and porcine ADM coverage could facilitate the healing of the wounds. It also reduces hospitalization time and improves the aesthetic and functional outcomes of extensive deep dermal burns (186).
Yet, there needs to be more information concerning the contribution of ADM in burn wound management (187). Given the high price of ADM sheet, more study on the cost-effectiveness of ADM in burn wounds needs to be done (187).
9. Conclusion and future perspective
Using ADM in various surgical procedures can yield favorable results in function, aesthetics, and fewer complications. ADM is an acellular graft that protects it against immunogenicity. It also spares the need for extracting the autologous graft, reducing the morbidity of donor-site surgery. ADM is rapidly vascularized and cellularized by the host. This mechanism protects it against infection and makes it ideal for contaminated sites.
Previous literature results have shown successful results of ADM use in palatoplasty, implant-based breast surgery, tendon repair, and wound management. However, the results of ADM use in rhinophyma and hernia repair have been contradictory.
Despite all the ADM benefits, complications such as hematoma, seroma, necrosis, and infection must be considered. Moreover, ADM is an expensive material and cannot be used ubiquitously. More work should be done to achieve cheaper ADM to make it a cost-effective choice. Overall, the number of reports on ADM is limited, and more extensive research on ADM use, especially in plastic and reconstructive surgery is expected.
Author contributions
Study concept and design: FM. Acquisition of data: FM, SO-T. Drafting of the manuscript: MK, AA, SP, AB, RH, and FK. Critical revision of the manuscript for important intellectual content: FM, SP. Study supervision: FM. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frtra.2023.1133806/full#supplementary-material.
References
1. Dadlani S. Porcine acellular dermal matrix: an alternative to connective tissue graft-A narrative review. Int J Dent. (2021) 2021:1652032. doi: 10.1155/2021/1652032
2. Gravina PR, Pettit RW, Davis MJ, Winocour SJ, Selber JC. Evidence for the use of acellular dermal matrix in implant-based breast reconstruction. Semin Plast Surg. (2019) 33(4):229–35. doi: 10.1055/s-0039-1696986
3. Gierek M, Labus W, Kitala D, Lorek A, Ochala-Gierek G, Zagorska KM, et al. Human acellular dermal matrix in reconstructive surgery-A review. Biomedicines. (2022) 10(11):2–3. doi: 10.3390/biomedicines10112870
4. Haney NM, Huang MM, Liu JL, Hawksworth DJ, Burnett AL. Acellular dermal matrix tissues in genitourinary reconstructive surgery: a review of the literature and case discussions. Sex Med Rev. (2021) 9(3):488–97. doi: 10.1016/j.sxmr.2020.07.003
5. Chung AM, Stein MJ, Ghumman A, Zhang J. The effect of post mastectomy radiation therapy on breast reconstruction with and without acellular dermal matrix: a systematic review and meta-analysis protocol. Syst Rev. (2019) 8(1):58. doi: 10.1186/s13643-019-0958-z
6. Lee M, Jun D, Choi H, Kim J, Shin D. Clinical efficacy of acellular dermal matrix paste in treating diabetic foot ulcers. Wounds. (2020) 32(1):50–6. PMID: 31876513.31876513
7. Lin W, Qi X, Guo W, Liang D, Chen H, Lin B, et al. A barrier against reactive oxygen species: chitosan/acellular dermal matrix scaffold enhances stem cell retention and improves cutaneous wound healing. Stem Cell Res Ther. (2020) 11(1):383. doi: 10.1186/s13287-020-01901-6
8. Daar DA, Gandy JR, Clark EG, Mowlds DS, Paydar KZ, Wirth GA. Plastic surgery and acellular dermal matrix: highlighting trends from 1999 to 2013. World J Plast Surg. (2016) 5(2):97–108. PMID: 27579264.27579264
9. Omranifard M, Rasti Ardakani M, Abdali H, Mortazavi P, Hoseini S, Hoghoughi MA. Comparative experimental study of dermal stability: acellular dermal matrix versus crayopreserved dermis. World J Plast Surg. (2021) 10(2):82–8. doi: 10.52547/wjps.10.2.82
10. Petrie K, Cox CT, Becker BC, MacKay BJ. Clinical applications of acellular dermal matrices: a review. Scars Burn Heal. (2022) 8:20595131211038313. doi: 10.1177/20595131211038313
11. Wu S, He R, Sun J, Zhao H. Acellular dermal matrix graft for ventral corporal lengthening orthoplasty in 2-stage proximal hypospadias repair. Transl Pediatr. (2021) 10(12):3151–8. doi: 10.21037/tp-21-372
12. Guo X, Mu D, Gao F. Efficacy and safety of acellular dermal matrix in diabetic foot ulcer treatment: a systematic review and meta-analysis. Int J Surg. (2017) 40:1–7. doi: 10.1016/j.ijsu.2017.02.008
13. Liang MK, Berger RL, Nguyen MT, Hicks SC, Li LT, Leong M. Outcomes with porcine acellular dermal matrix versus synthetic mesh and suture in complicated open ventral hernia repair. Surg Infect (Larchmt). (2014) 15(5):506–12. doi: 10.1089/sur.2013.090
15. Allen EP. Soft tissue grafting with the tunnel technique in the mandibular anterior: myths and realities. J Esthet Restor Dent. (2021) 33(1):152–7. doi: 10.1111/jerd.12712
16. Babaki D, Khoshsimaybargard M, Yaghoubi S, Gholami M. Comparison of vestibular depth relapse and wound healing after reconstructive preprosthetic surgery using cryopreserved amniotic membrane and acellular dermal matrix - A comparative study. Ann Maxillofac Surg. (2021) 11(1):12–6. doi: 10.4103/ams.ams_322_20
17. Bing Z, Feng L, Wu CS, Du JT, Liu YF, Liu SX. Acellular dermal matrix contributes to epithelialization in patients with chronic sinusitis. J Biomater Appl. (2019) 33(8):1053–9. doi: 10.1177/0885328218822636
18. Chambrone L, Pinto R, Chambrone LA. The concepts of evidence-based periodontal plastic surgery: application of the principles of evidence-based dentistry for the treatment of recession-type defects. Periodontol 2000. (2019) 79(1):81–106. doi: 10.1111/prd.12248
19. Changi KK, Greenstein G, Tarnow D, Royzman D, Kang P. Creeping clinical attachment after acellular dermal matrix augmentation to attain root coverage. Clin Adv Periodontics. (2020) 10(2):75–80. doi: 10.1002/cap.10078
20. Cigerim L. Treatment of exposed bone with acellular dermal matrix in a smoker patient after dental implant surgery: a case report. J Oral Implantol. (2020) 46(3):245–9. doi: 10.1563/aaid-joi-D-19-00221
21. Cohen LE, Bogue JT, Jin J, Disa JJ. Explantation in tissue expander and direct-to-implant reconstruction with acellular dermal matrix: how to avoid early reconstructive failures. Plast Reconstr Surg. (2021) 147(4):579e–86e. doi: 10.1097/PRS.0000000000007702
22. Custer PL, Maamari RN. Porcine dermal matrix sandwich graft for lower eyelid reconstruction. Orbit. (2021) 40(2):138–44. doi: 10.1080/01676830.2020.1755316
23. Emodi O, Ginini JG, van Aalst JA, Shilo D, Naddaf R, Aizenbud D, et al. Cleft palate Fistula closure utilizing acellular dermal matrix. Plast Reconstr Surg Glob Open. (2018) 6(3):e1682. doi: 10.1097/GOX.0000000000001682
24. Aronson S, Ellis MF. Hostile scalp wound reconstruction using acellular dermal matrix for soft tissue augmentation. J Craniofac Surg. (2020) 31(3):e309–12. doi: 10.1097/SCS.0000000000006170
25. Conrad DJ, Zhang H, Côté DWJ. Acellular human dermal allograft as a graft for nasal septal perforation reconstruction. Plast Reconstr Surg. (2018) 141(6):1517–24. doi: 10.1097/PRS.0000000000004410
26. Ferrari B, Reggiani C, Francomano M, Bellini P, Ferrari F, Giacomelli L, et al. Clinical factors influencing the outcomes of an acellular dermal matrix for skin cancer treatment: a retrospective study. Adv Skin Wound Care. (2020) 33(7):367–74. doi: 10.1097/01.ASW.0000666900.03111.c3
27. Fisher M, Alba B, Ahmad J, Robotti E, Cerkes N, Gruber RP, et al. Current practices in dorsal augmentation rhinoplasty. Plast Reconstr Surg. (2022) 149(5):1088–102. doi: 10.1097/PRS.0000000000009057
28. Goh BKL, Chia HL. The use of acellular dermal matrix in combination with pedicled buccal fat pad in wide cleft palate repair: a case report and literature review. Cleft Palate Craniofac J. (2019) 56(10):1381–5. doi: 10.1177/1055665619851915
29. Heo CY, Kang B, Jeong JH, Kim K, Myung Y. Acellular dermal matrix and bone cement sandwich technique for chest wall reconstruction. Arch Plast Surg. (2022) 49(1):25–8. doi: 10.5999/aps.2021.01067
30. Jansen LA, De Caigny P, Guay NA, Lineaweaver WC, Shokrollahi K. The evidence base for the acellular dermal matrix AlloDerm: a systematic review. Ann Plast Surg. (2013) 70(5):587–94. doi: 10.1097/SAP.0b013e31827a2d23
31. Kiely AL, Cooper LRL, Greig A. Acellular dermal matrix reconstruction of a nail bed avulsion in a 13-year-old child. BMJ Case Rep. (2020) 13:e236253. doi: 10.1136/bcr-2020-236253
32. Kim JH, Kim SE, Kim YJ, Kim YW, Cheon YW. Comparison of volume retention and biocompatibility of acellular dermal matrix/hyaluronic acid filler to autologous fat grafts in a mouse model. Aesthetic Plast Surg. (2020) 44(3):986–92. doi: 10.1007/s00266-020-01680-8
33. Kim YS, Na YC, Yoon HS, Huh WH, Kim JM. Short-term changes of human acellular dermal matrix (megaderm) in a mouse model. Arch Craniofac Surg. (2019) 20(1):10–6. doi: 10.7181/acfs.2018.02243
34. Lee JS, Lee JH, Ryu JY, Park SH, Park JY, Han MH, et al. Influence of irradiation on capsules of silicone implants covered with acellular dermal matrix in mice. Aesthetic Plast Surg. (2022) 46(2):937–46. doi: 10.1007/s00266-021-02618-4
35. Lembo F, Cecchino LR, Parisi D, Portincasa A. Utility of a new artificial dermis as a successful tool in face and scalp reconstruction for skin cancer: analysis of the efficacy, safety, and aesthetic outcomes. Dermatol Res Pract. (2020) 2020:4874035. doi: 10.1155/2020/4874035
36. Lisa AVE, Galtelli L, Vinci V, Veronesi A, Cozzaglio L, Cananzi FCM, et al. Adoption of a newly introduced dermal matrix: preliminary experience and future directions. Biomed Res Int. (2020) 2020:3261318. doi: 10.1155/2020/3261318
37. Losco L, Sereni S, Aksoyler D, Spadoni D, Bolletta A, Cigna E. Perforator-based adipofascial flaps and ADM: a novel combined approach to distal lower extremity defects. Plast Reconstr Surg Glob Open. (2022) 10(2):e4131. doi: 10.1097/GOX.0000000000004131
38. Ludolph I, Gruener JS, Kengelbach-Weigand A, Fiessler C, Horch RE, Schmitz M. Long-term studies on the integration of acellular porcine dermis as an implant shell and the effect on capsular fibrosis around silicone implants in a rat model. J Plast Reconstr Aesthet Surg. (2019) 72(9):1555–63. doi: 10.1016/j.bjps.2019.04.015
39. Madaree A. Use of acellular dermal matrix in craniosynostosis. J Craniofac Surg. (2018) 29(1):126–9. doi: 10.1097/SCS.0000000000004123
40. Melandri D, Marongiu F, Carboni A, Rubino C, Razzano S, Purpura V, et al. A new human-derived acellular dermal matrix for 1-stage coverage of exposed tendons in the foot. Int J Low Extrem Wounds. (2020) 19(1):78–85. doi: 10.1177/1534734619884422
41. Mirzai S, Lee AH, Chi JJ. Nasal septal perforation repair with an Inferior turbinate flap and acellular dermal matrix. Surg J (N Y). (2021) 7(1):e26–e9. doi: 10.1055/s-0040-1713418
42. Patel MH, Kim RY, Aronovich S, Skouteris CA. Clinical assessment of acellular dermal matrix (AlloDerm (c)) as an option in the replacement of the temporomandibular joint disc: a pilot study. J Stomatol Oral Maxillofac Surg. (2020) 121(5):496–500. doi: 10.1016/j.jormas.2019.12.018
43. Patel S, Ziai K, Lighthall JG, Walen SG. Biologics and acellular dermal matrices in head and neck reconstruction: a comprehensive review. Am J Otolaryngol. (2022) 43(1):103233. doi: 10.1016/j.amjoto.2021.103233
44. Pereira CM, Barra ID, Badaró KA. Bilateral eyelid necrosis with dermal matrix reconstruction and skin grafting. Rev Bras Cir Plast. (2021) 36(2):217–21.
45. Pourtaheri N, Wang D, Calva D, Chopra K, Kumar AR. Adipofascial flaps with acellular dermal matrix compared with myocutaneous flap reconstruction in lumbar myelomeningocele defects. J Craniofac Surg. (2018) 29(5):1137–42. doi: 10.1097/SCS.0000000000004598
46. Sarkozyova N, Dragunova J, Bukovcan P, Ferancikova N, Breza J, Zilinska Z, et al. Preparation and processing of human allogenic dermal matrix for utilization in reconstructive surgical procedures. Bratisl Lek Listy. (2020) 121(6):386–94. doi: 10.4149/BLL_2020_063
47. Stefanini M, Rendon A, Zucchelli G. Porcine-Derived acellular dermal matrix for buccal soft tissue augmentation at single implant sites: a 1-year follow-up case series. Int J Periodontics Restorative Dent. (2020) 40(1):121–8. doi: 10.11607/prd.4477
48. Sun J, Liu X, Zhang Y, Huang Y, Zhong S, Fang S, et al. Bovine acellular dermal matrix for levator lengthening in thyroid-related upper-eyelid retraction. Med Sci Monit. (2018) 24:2728–34. doi: 10.12659/MSM.909306
49. Tavelli L, McGuire MK, Zucchelli G, Rasperini G, Feinberg SE, Wang HL, et al. Extracellular matrix-based scaffolding technologies for periodontal and peri-implant soft tissue regeneration. J Periodontol. (2020) 91(1):17–25. doi: 10.1002/JPER.19-0351
50. Tork S, Jefferson RC, Janis JE. Acellular dermal matrices: applications in plastic surgery. Semin Plast Surg. (2019) 33(3):173–84. doi: 10.1055/s-0039-1693019
51. Vincent-Bugnas S, Laurent J, Naman E, Charbit M, Borie G. Treatment of multiple gingival recessions with xenogeneic acellular dermal matrix compared to connective tissue graft: a randomized split-mouth clinical trial. J Periodontal Implant Sci. (2021) 51(2):77–87. doi: 10.5051/jpis.2002400120
52. Wells HC, Sizeland KH, Kirby N, Hawley A, Mudie S, Haverkamp RG. Acellular dermal matrix collagen responds to strain by intermolecular spacing contraction with fibril extension and rearrangement. J Mech Behav Biomed Mater. (2018) 79:1–8. doi: 10.1016/j.jmbbm.2017.12.009
53. Zhan YL, Wang MZ, Cao XJ, Liu F. Effectiveness of acellular dermal matrix graft with a coronally advanced flap for the treatment of miller class I/II single gingival recession with thin gingival phenotype: study protocol for a split-mouth randomised controlled trial. BMJ Open. (2022) 12(1):8. doi: 10.1136/bmjopen-2020-047703
54. Zhu Z, Yuan ZQ, Huang C, Jin R, Sun D, Yang J, et al. Construction of a dermis-fat composite in vivo: optimizing heterogeneous acellular dermal matrix with in vitro pretreatment. J Tissue Eng Regen Med. (2020) 14(2):215–28. doi: 10.1002/term.2986
55. Losee JE, Smith DM. Acellular dermal matrix in palatoplasty. Aesthet Surg J. (2011) 31(7 Suppl):108s–15s. doi: 10.1177/1090820X11418216
56. Kattan AE, Abdulghafour M, Ahmed BA, Gelidan AG, Alhumsi TR. The use of acellular dermal matrix in palatoplasty to decrease the rate of postoperative oronasal fistula. J Pak Med Assoc. (2022) 72(2):337–41. doi: 10.47391/JPMA.20-581
57. Gilardino MS, Aldekhayel S, Govshievich A. A prospective study investigating Fistula rate following primary palatoplasty using acellular dermal matrix. Plast Reconstr Surg Glob Open. (2018) 6(6):e1826. doi: 10.1097/GOX.0000000000001826
58. Helling ER, Dev VR, Garza J, Barone C, Nelluri P, Wang PT. Low fistula rate in palatal clefts closed with the furlow technique using decellularized dermis. Plast Reconstr Surg. (2006) 117(7):2361–5. doi: 10.1097/01.prs.0000218788.44591.f0
59. Zhong B, Song NY, Deng D, Li LK, Du JT, Liu F, et al. Intraoperative repair of cerebrospinal fluid rhinorrhea in skull base tumor resection: a retrospective study of acellular dermal matrix versus turbinate flap. World Neurosurg. (2020) 133:e275–80. doi: 10.1016/j.wneu.2019.08.245
60. Lee H, Eom YS, Pyon JK. A method to prevent cerebrospinal fluid leakage: reinforcing acellular dermal matrix. Arch Craniofac Surg. (2020) 21(1):45–8. doi: 10.7181/acfs.2019.00535
61. Caputo GG, Vigato E, Cordaro ER, Parodi PC, Governa M. Comparative study of patient outcomes between direct to implant and two-stage implant-based breast reconstruction after mastectomy. J Plast Reconstr Aesthet Surg. (2021) 74(10):2573–9. doi: 10.1016/j.bjps.2021.03.058
62. Couto SR, Luan X, Rossmann JA, Stenberg WV, Yen K, Atwi S, et al. An in vivo comparison of wound healing characteristics of two commercial acellular dermal matrices. Clin Exp Dent Res. (2021) 7(5):679–91. doi: 10.1002/cre2.412
63. Dee DT, Hung VT, Schamblin CJ, Lupica GM, Hitchens HR, McGarry MH, et al. Radiocapitellar contact characteristics after osteochondral defect repair using a novel hybrid reconstructive procedure. Orthop J Sports Med. (2022) 10(3):23259671221083582. doi: 10.1177/23259671221083582
64. Hahn HM, Lee DH, Lee IJ. Ready-to-Use micronized human acellular dermal matrix to accelerate wound healing in diabetic foot ulcers: a prospective randomized pilot study. Adv Skin Wound Care. (2021) 34(5):1–6. doi: 10.1097/01.ASW.0000741512.57300.6d
65. Heidemann LN, Gunnarsson GL, Salzberg CA, Sørensen JA, Thomsen JB. Complications following nipple-sparing mastectomy and immediate acellular dermal matrix implant-based breast reconstruction-A systematic review and meta-analysis. Plast Reconstr Surg Glob Open. (2018) 6(1):e1625. doi: 10.1097/GOX.0000000000001625
66. Jackson SR, Roman S. Matriderm and split skin grafting for full-thickness pediatric facial burns. J Burn Care Res. (2019) 40(2):251–4. doi: 10.1093/jbcr/irz006
67. Jankau J, Blazynska-Spychalska A, Kubiak K, Jedrzejczak-Krzepkowska M, Pankiewicz T, Ludwicka K, et al. Bacterial cellulose properties fulfilling requirements for a biomaterial of choice in reconstructive surgery and wound healing. Front Bioeng Biotechnol. (2022) 9:21. doi: 10.3389/fbioe.2021.805053
68. Leypold T, Schäfer B, Boos AM, Beier JP. Plastic surgery reconstruction of chronic/non-healing wounds. Surg Technol Int. (2020) 38:65–71. doi: 10.52198/21.STI.38.WH1371
69. Lu W, Qi G, Ding Z, Li X, Qi W, He F. Clinical efficacy of acellular dermal matrix for plastic periodontal and implant surgery: a systematic review. Int J Oral Maxillofac Surg. (2020) 49(8):1057–66. doi: 10.1016/j.ijom.2019.12.005
70. Shi Y, Segelnick SL, El Chaar ES. A modified technique of tacking acellular dermal matrix to increase keratinized Mucosa around dental implants as an alternative to a free gingival graft: a case report. Clin Adv Periodontics. (2020) 10(4):175–80. doi: 10.1002/cap.10113
71. Youngerman BE, Kosty JA, Gerges MM, Tabaee A, Kacker A, Anand VK, et al. Acellular dermal matrix as an alternative to autologous fascia lata for skull base repair following extended endoscopic endonasal approaches. Acta Neurochir (Wien). (2020) 162(4):863–73. doi: 10.1007/s00701-019-04200-z
72. Mericli AF, Gampper TJ. The use of an acellular dermal matrix “sandwich” for the successful treatment of a persistent cranial cerebrospinal fluid fistula. J Craniofac Surg. (2013) 24(4):1314–6. doi: 10.1097/SCS.0b013e3182953a39
73. Salinas F, Robla D, Meana Á, Pevida M, Martinez Magide G, Sánchez Nuño C, et al. Novel technique of development of human derived acellular dermal matrix. Cell Tissue Bank. (2021) 23:1. doi: 10.1007/s10561-021-09954-4
74. Torresetti M, Scalise A, Di Benedetto G. Acellular dermal matrix for rhinophyma: is it worth it? A new case report and review of literature. Int J Surg Case Rep. (2019) 59:120–3. doi: 10.1016/j.ijscr.2019.05.013
75. Özkan A, Topkara A, Özcan RH, Şentürk S. The use of the PlasmaBlade and acellular dermal matrix in rhinophyma surgery: a case report. J Cutan Med Surg. (2016) 20(2):155–8. doi: 10.1177/1203475415612422
76. Lee JM, Seo YJ, Shim DB, Lee HJ, Kim SH. Surgical outcomes of tympanoplasty using a sterile acellular dermal allograft: a prospective randomised controlled study. Acta Otorhinolaryngol Ital. (2018) 38(6):554–62. doi: 10.14639/0392-100X-1839
77. Kim CH, Park SC. Homologous tissue for dorsal augmentation. Facial Plast Surg Clin North Am. (2018) 26(3):311–21. doi: 10.1016/j.fsc.2018.03.005
78. Park SC, Nam JS, Lee KI, Lee YW, Park JJ, Ha JG, et al. Effectiveness of cross-linked human acellular dermal matrix in primary and revision augmentation rhinoplasty. J Plast Reconstr Aesthet Surg. (2022) 75(4):1447–54. doi: 10.1016/j.bjps.2021.09.062
79. Yang CE, Kim SJ, Kim JH, Lee JH, Roh TS, Lee WJ. Usefulness of cross-linked human acellular dermal matrix as an implant for dorsal augmentation in rhinoplasty. Aesthetic Plast Surg. (2018) 42(1):288–94. doi: 10.1007/s00266-017-0996-7
80. Sherris DA, Oriel BS. Human acellular dermal matrix grafts for rhinoplasty. Aesthet Surg J. (2011) 31(7 Suppl):95s–100s. doi: 10.1177/1090820X11418200
81. Adams WP, Baxter R, Glicksman C, Mast BA, Tantillo M, Van Natta BW. The use of poly-4-hydroxybutyrate (P4HB) scaffold in the ptotic breast: a multicenter clinical study. Aesthetic Surg J. (2018) 38(5):502–18. doi: 10.1093/asj/sjy022
82. Al Jammal OM, Wali AR, Lewis CS, Zaldana MV, Suliman AS, Pham MH. Management of giant sacral pseudomeningocele in revision spine surgery. Int J Spine Surg. (2020) 14(5):778–84. doi: 10.14444/7111
83. Berna G, Cagli B, Persichetti P, Cogliandro A, Silan F, Maritan M, et al. Feasibility study on equine acellular pericardium matrix (APM): a new tool for breast reconstruction. J Plast Reconstr Aesthet Surg. (2020) 73(12):2150–5. doi: 10.1016/j.bjps.2020.05.013
84. Broyles JM, Liao EC, Kim J, Heistein J, Sisco M, Karp N, et al. Acellular dermal matrix-associated complications in implant-based breast reconstruction: a multicenter, prospective, randomized controlled clinical trial comparing two human tissues. Plast Reconstr Surg. (2021) 148(3):493–500. doi: 10.1097/PRS.0000000000008194
85. Brunbjerg ME, Jensen TB, Overgaard J, Christiansen P, Damsgaard TE. Comparison of one-stage direct-to-implant with acellular dermal matrix and two-stage immediate implant-based breast reconstruction-a cohort study. Gland Surg. (2021) 10(1):207–18. doi: 10.21037/gs-20-581
86. Cattelani L, Polotto S, Arcuri MF, Pedrazzi G, Linguadoca C, Bonati E. One-Step prepectoral breast reconstruction with dermal matrix-covered implant compared to submuscular implantation: functional and cost evaluation. Clin Breast Cancer. (2018) 18(4):e703–11. doi: 10.1016/j.clbc.2017.11.015
87. Chan YHY, Yue IKH, Ho CM, Cheung PSY. The use of Serratus anterior fascial flap in integrated mastectomy and implant reconstruction. World J Surg. (2020) 44(3):825–30. doi: 10.1007/s00268-019-05275-6
88. DeLong MR, Tandon VJ, Bertrand AA, MacEachern M, Goldberg M, Salibian A, et al. Review of outcomes in prepectoral prosthetic breast reconstruction with and without surgical mesh assistance. Plast Reconstr Surg. (2021) 147(2):305–15. doi: 10.1097/PRS.0000000000007586
89. Ely S, Gologorsky RC, Hornik BM, Velotta JB. Sternal reconstruction with non-rigid biologic mesh overlay. Ann Thorac Surg. (2020) 109(5):e357–e9. doi: 10.1016/j.athoracsur.2019.08.072
90. Heine N, Hoesl V, Seitz S, Prantl L, Brebant V. Implant-based immediate reconstruction in prophylactic mastectomy: is the caudal dermis flap a reliable alternative to synthetic mesh or acellular dermal matrix? Arch Gynecol Obstet. (2022) 305(4):937–43. doi: 10.1007/s00404-021-06244-y
91. Khan A, Tasoulis MK, Teoh V, Tanska A, Edmonds R, Gui G. Pre-pectoral one-stage breast reconstruction with anterior biological acellular dermal matrix coverage. Gland Surg. (2021) 10(3):1002–9. doi: 10.21037/gs-20-652
92. Chen Y, Liu X, Zheng X, Huang X, Dan W, Li Z, et al. Advances on the modification and biomedical applications of acellular dermal matrices. Journal of Leather Science and Engineering. (2022) 4(1):13–14. doi: 10.1186/s42825-022-00093-4
93. Giordano S, Garvey PB, Clemens MW, Baumann DP, Selber JC, Rice DC, et al. Synthetic mesh versus acellular dermal matrix for oncologic chest wall reconstruction: a comparative analysis. Ann Surg Oncol. (2020) 27(8):3009–17. doi: 10.1245/s10434-019-08168-z
94. Bojanic C, Lawrence A, Mitrasinovic S, Samaras S, Fopp LJ, Forouhi P, et al. Indications and pitfalls of prepectoral breast reconstruction with braxonⓇ acellular dermal matrix (ADM): a preliminary plastic surgical experience. J Plast Reconstr Aesthet Surg. (2021) 74(8):1931–71. doi: 10.1016/j.bjps.2021.03.124
95. Kim A, Jung JH, Choi YL, Pyon JK. Capsule biopsy of acellular dermal matrix (ADM) to predict future capsular contracture in two-stage prosthetic breast reconstruction. J Plast Reconstr Aesthet Surg. (2019) 72(9):1576–606. doi: 10.1016/j.bjps.2019.05.021
96. Kumar NG, Berlin NL, Kim HM, Hamill JB, Kozlow JH, Wilkins EG. Development of an evidence-based approach to the use of acellular dermal matrix in immediate expander-implant-based breast reconstruction. J Plast Reconstr Aesthet Surg. (2021) 74(1):30–40. doi: 10.1016/j.bjps.2020.10.005
97. Lee CB, Kim YS, Lee SE. Imaging features of volume replacement using an acellular dermal matrix in oncoplastic breast conserving surgery: a case report. Radiol Case Rep. (2022) 17(6):2146–9. doi: 10.1016/j.radcr.2022.03.003
98. Liu J, Hou JF, Li ZP, Wang B, Sun JM. Efficacy of acellular dermal matrix in capsular contracture of implant-based breast reconstruction: a single-arm meta-analysis. Aesthetic Plast Surg. (2020) 44(3):735–42. doi: 10.1007/s00266-019-01603-2
99. Lohmander F, Lagergren J, Roy PG, Johansson H, Brandberg Y, Eriksen C, et al. Implant based breast reconstruction with acellular dermal matrix: safety data from an open-label, multicenter, randomized, controlled trial in the setting of breast cancer treatment. Ann Surg. (2019) 269(5):836–41. doi: 10.1097/SLA.0000000000003054
100. Luan AN, Patel AA, Martin SA, Nazerali RS. Single-Unit technique for the use of acellular dermal matrix in immediate expander-based breast reconstruction. J Plast Reconstr Aesthet Surg. (2021) 74(5):981–6. doi: 10.1016/j.bjps.2020.10.048
101. Maliska CM III, Archer RL, Tarpley SK, Miller AS III. Complex sternal and rib reconstruction with allogeneic material. Arch Plast Surg. (2018) 45(6):593–7. doi: 10.5999/aps.2017.00122
102. Yoon YC, Lee J, Jeong JY. Radical resection and reconstruction of the sternum for metastasis of hepatocellular carcinoma. J Cardiothorac Surg. (2020) 15(1):202. doi: 10.1186/s13019-020-01247-3
103. Stanizzi A, Torresetti M, Salati M, Benedetto GD. Use of porcine acellular dermal matrix to repair lung hernia after minithoracotomy: a case report with 6-year follow-up. JPRAS Open. (2021) 28:56–60. doi: 10.1016/j.jpra.2021.01.012
104. Stein MJ, Chung A, Arnaout A, Ghaedi B, Ghumman A, Zhang TH, et al. Complication rates of acellular dermal matrix in immediate breast reconstruction with radiation: a single-institution retrospective comparison study. J Plast Reconstr Aesthet Surg. (2020) 73(12):2156–63. doi: 10.1016/j.bjps.2020.05.065
105. Antony AK, Poirier J, Madrigrano A, Kopkash KA, Robinson EC. Evolution of the surgical technique for “breast in a day” direct-to-implant breast reconstruction: transitioning from dual-plane to prepectoral implant placement. Plast Reconstr Surg. (2019) 143(6):1547–56. doi: 10.1097/PRS.0000000000005627
106. Fakim B, Highton L, Gandhi A, Johnson R, Murphy J. Implant-based breast reconstruction with Artia (TM) tissue matrix. J Plast Reconstr Aesthet Surg. (2019) 72(9):1548–54. doi: 10.1016/j.bjps.2019.05.024
107. Onesti MG, Di Taranto G, Ribuffo D, Scuderi N. ADM-assisted prepectoral breast reconstruction and skin reduction mastectomy: expanding the indications for subcutaneous reconstruction. J Plast Reconstr Aesthet Surg. (2020) 73(4):673–80. doi: 10.1016/j.bjps.2019.11.004
108. Tierney BP, De La Garza M, Jennings GR, Weinfeld AB. Clinical outcomes of acellular dermal matrix (SimpliDerm and AlloDerm ready-to-use) in immediate breast reconstruction. Cureus. (2022) 14(2):e22371. doi: 10.7759/cureus.22371
109. Stein MJ, Arnaout A, Lichtenstein JB, Frank SG, Cordeiro E, Roberts A, et al. A comparison of patient-reported outcomes between alloderm and dermacell in immediate alloplastic breast reconstruction: a randomized control trial. J Plast Reconstr Aesthet Surg. (2021) 74(1):41–7. doi: 10.1016/j.bjps.2020.08.018
110. Kalstrup J, Balslev Willert C, Brinch-Møller Weitemeyer M, Hougaard Chakera A, Hölmich LR. Immediate direct-to-implant breast reconstruction with acellular dermal matrix: evaluation of complications and safety. Breast. (2021) 60:192–8. doi: 10.1016/j.breast.2021.10.006
111. Negenborn VL, Smit JM, Dikmans REG, Winters HAH, Twisk JWR, Ruhé PQ, et al. Short-term cost-effectiveness of one-stage implant-based breast reconstruction with an acellular dermal matrix versus two-stage expander-implant reconstruction from a multicentre randomized clinical trial. Br J Surg. (2019) 106(5):586–95. doi: 10.1002/bjs.11102
112. Jones G, Antony AK. Single stage, direct to implant pre-pectoral breast reconstruction. Gland Surg. (2019) 8(1):53–60. doi: 10.21037/gs.2018.10.08
113. Franceschini G, Masetti R. Acellular dermal matrix as filler in breast-conserving surgery: warnings for a careful use. World J Surg Oncol. (2021) 19(1):1. doi: 10.1186/s12957-020-02109-x
114. Powell-Brett S, Goh S. Clinical and patient reported outcomes in breast reconstruction using acellular dermal matrix. JPRAS Open. (2018) 17:31–8. doi: 10.1016/j.jpra.2018.06.006
115. Stump A, Holton LH 3rd, Connor J, Harper JR, Slezak S, Silverman RP. The use of acellular dermal matrix to prevent capsule formation around implants in a primate model. Plast Reconstr Surg. (2009) 124(1):82–91. doi: 10.1097/PRS.0b013e3181ab112d
116. Jansen LA, Macadam SA. The use of AlloDerm in postmastectomy alloplastic breast reconstruction: part II. A cost analysis. Plast Reconstr Surg. (2011) 127(6):2245–54. doi: 10.1097/PRS.0b013e3182131c6b
117. Levy AS, Bernstein JL, Xia JJ, Otterburn DM. Poly-4-Hydroxybutyric acid mesh compares favorably with acellular dermal matrix in tissue expander-based breast reconstruction. Ann Plast Surg. (2020) 85(S1 Suppl 1):S2–7. doi: 10.1097/SAP.0000000000002339
118. Danino MA, El Khatib AM, Doucet O, Dao L, Efanov JI, Bou-Merhi JS, et al. Preliminary results supporting the bacterial hypothesis in red breast syndrome following postmastectomy acellular dermal matrix- and implant-based reconstructions. Plast Reconstr Surg. (2019) 144(6):988e–92e. doi: 10.1097/PRS.0000000000006227
119. Hansson E, Edvinsson AC, Elander A, Kölby L, Hallberg H. First-year complications after immediate breast reconstruction with a biological and a synthetic mesh in the same patient: a randomized controlled study. J Surg Oncol. (2021) 123(1):80–8. doi: 10.1002/jso.26227
120. Dikmans RE, Negenborn VL, Bouman MB, Winters HA, Twisk JW, Ruhé PQ, et al. Two-stage implant-based breast reconstruction compared with immediate one-stage implant-based breast reconstruction augmented with an acellular dermal matrix: an open-label, phase 4, multicentre, randomised, controlled trial. Lancet Oncol. (2017) 18(2):251–8. doi: 10.1016/S1470-2045(16)30668-4
121. Bonitz RP, Hanna MK. Use of human acellular dermal matrix during classic bladder exstrophy repair. J Pediatr Urol. (2016) 12(2):114.e1–5. doi: 10.1016/j.jpurol.2015.10.005
122. Brunbjerg ME, Jensen TB, Christiansen P, Overgaard J, Damsgaard TE. Reinforcement of the abdominal wall with acellular dermal matrix or synthetic mesh after breast reconstruction with the pedicled transverse rectus abdominis musculocutaneous flap. A prospective double-blind randomized study. J Plast Surg Hand Surg. (2021) 55(4):202–9. doi: 10.1080/2000656X.2020.1856673
123. Gogna S, Latifi R, Policastro A, Prabhakaran K, Anderson P, Con J, et al. Complex abdominal wall hernia repair with biologic mesh in elderly: a propensity matched analysis. Hernia. (2020) 24(3):495–502. doi: 10.1007/s10029-019-02068-7
124. Hackenberger PN, Poteet SJ, Janis JE. Bridging acellular dermal matrix in abdominal wall repair following radical resection of recurrent endometrioma. Plast Reconstr Surg Glob Open. (2020) 8(1):e2603. doi: 10.1097/GOX.0000000000002603
125. Hohn EA, Gillette BP, Burns JP. Outcomes of arthroscopic revision rotator cuff repair with acellular human dermal matrix allograft augmentation. J Shoulder Elbow Surg. (2018) 27(5):816–23. doi: 10.1016/j.jse.2017.09.026
126. Kalaiselvan R, Carlson GL, Hayes S, Lees NP, Anderson ID, Slade DAJ. Recurrent intestinal fistulation after porcine acellular dermal matrix reinforcement in enteric fistula takedown and simultaneous abdominal wall reconstruction. Hernia. (2020) 24(3):537–43. doi: 10.1007/s10029-019-02097-2
127. Lembo F, Cecchino LR, Parisi D, Portincasa A. Role of a new acellular dermal matrix in a multistep combined treatment of dermatofibrosarcoma protuberans of the lumbar region: a case report. J Med Case Rep. (2021) 15(1):180. doi: 10.1186/s13256-021-02787-5
128. Razavi SA, Desai KA, Hart AM, Thompson PW, Losken A. The impact of mesh reinforcement with components separation for abdominal wall reconstruction. Am Surg. (2018) 84(6):959–62. doi: 10.1177/000313481808400648
129. Tang X, Zhang XW, Wu YY, Yin HQ, Du YQ, Zhang XP, et al. The clinical effects of utilizing allogeneic acellular dermal matrix in the surgical therapy of anterior urethral stricture. Urol Int. (2020) 104(11-12):933–8. doi: 10.1159/000510317
130. Cevasco M, Itani KM. Ventral hernia repair with synthetic, composite, and biologic mesh: characteristics, indications, and infection profile. Surg Infect (Larchmt). (2012) 13(4):209–15. doi: 10.1089/sur.2012.123
131. Bhanot P, King KS, Albino FP. Biologic mesh for abdominal wall reconstruction. Chronic Wound Care Manag Res. (2014) 2014:1. doi: 10.2147/CWCMR.S58816
132. Fischer JP, Basta MN, Krishnan NM, Wink JD, Kovach SJ. A cost-utility assessment of mesh selection in clean-contaminated ventral hernia repair. Plast Reconstr Surg. (2016) 137(2):647–59. doi: 10.1097/01.prs.0000475775.44891.56
133. Fischer JP, Basta MN, Mirzabeigi MN, Kovach SJ 3rd. A comparison of outcomes and cost in VHWG grade II hernias between rives-stoppa synthetic mesh hernia repair versus underlay biologic mesh repair. Hernia. (2014) 18(6):781–9. doi: 10.1007/s10029-014-1309-6
134. Brewer MB, Rada EM, Milburn ML, Goldberg NH, Singh DP, Cooper M, et al. Human acellular dermal matrix for ventral hernia repair reduces morbidity in transplant patients. Hernia. (2011) 15(2):141–5. doi: 10.1007/s10029-010-0748-y
135. Darehzereshki A, Goldfarb M, Zehetner J, Moazzez A, Lipham JC, Mason RJ, et al. Biologic versus nonbiologic mesh in ventral hernia repair: a systematic review and meta-analysis. World J Surg. (2014) 38(1):40–50. doi: 10.1007/s00268-013-2232-1
136. Garvey PB, Giordano SA, Baumann DP, Liu J, Butler CE. Long-Term outcomes after abdominal wall reconstruction with acellular dermal matrix. J Am Coll Surg. (2017) 224(3):341–50. doi: 10.1016/j.jamcollsurg.2016.11.017
137. Janis JE, O'Neill AC, Ahmad J, Zhong T, Hofer SOP. Acellular dermal matrices in abdominal wall reconstruction: a systematic review of the current evidence. Plast Reconstr Surg. (2012) 130(5 Suppl 2):183s–93s. doi: 10.1097/PRS.0b013e3182605cfc
138. Skowronek K, Łabuś W, Stojko R, Kitala D, Sadłocha M, Drosdzol-Cop A. Application of acellular dermal matrix in gynaecology-A current review. J Clin Med. (2022) 11(14):2. doi: 10.3390/jcm11144030
139. Ji H, Sukarto A, Deegan D, Fan F. Characterization of inflammatory and fibrotic aspects of tissue remodeling of acellular dermal matrix in a nonhuman primate model. Plast Reconstr Surg Glob Open. (2021) 9(2):e3420. doi: 10.1097/GOX.0000000000003420
140. Maruccia M, Marannino PC, Elia R, Ribatti D, Tamma R, Nacchiero E, et al. Treatment of finger degloving injury with acellular dermal matrices: functional and aesthetic results. J Plast Reconstr Aesthet Surg. (2019) 72(9):1509–17. doi: 10.1016/j.bjps.2019.05.029
141. Morgante D, Radford A, Abbas SK, Ingham E, Subramaniam R, Southgate J. Augmentation of the insufficient tissue bed for surgical repair of hypospadias using acellular matrix grafts: a proof of concept study. J Tissue Eng. (2021) 12:12. doi: 10.1177/2041731421998840
142. Gupta A, Zahriya K, Mullens PL, Salmassi S, Keshishian A. Ventral herniorrhaphy: experience with two different biosynthetic mesh materials, surgisis and alloderm. Hernia. (2006) 10(5):419–25. doi: 10.1007/s10029-006-0130-2
143. Xin ZC, Yang BC, Li M, Yuan YM, Cui WS, Tang Y, et al. Appllication of human acellular dermal matrix in surgical treatment of genitourinary disease. Beijing Da Xue Xue Bao Yi Xue Ban. (2019) 51(4):778–82. doi: 10.19723/j.issn.1671-167X.2019.04.033
144. Yang F, Liu Y, Xiao H, Ma JY, Cun HY, Wu CD. A novel technique combining human acellular dermal matrix (HADM) and enriched platelet therapy (EPT) for the treatment of vaginal laxity: a single-arm, observational study. Aesthetic Plast Surg. (2022) 9:3. doi: 10.1007/s00266-022-02805-x
145. Gualtieri M, Zhang Y, Candiotti K, Yavagal S, Medina CA, Takacs P. The effect of biological and synthetic meshes on vaginal smooth muscle cell proliferation. Neurourol Urodyn. (2011) 30(3):435–7. doi: 10.1002/nau.21064
146. Han JG, Wang ZJ, Gao ZG, Xu HM, Yang ZH, Jin ML. Pelvic floor reconstruction using human acellular dermal matrix after cylindrical abdominoperineal resection. Dis Colon Rectum. (2010) 53(2):219–23. doi: 10.1007/DCR.0b013e3181b715b5
147. Tognetti L, Pianigiani E, Ierardi F, Lorenzini G, Casella D, Liso FG, et al. The use of human acellular dermal matrices in advanced wound healing and surgical procedures: state of the art. Dermatol Ther. (2021) 34(4):e14987. doi: 10.1111/dth.14987
148. Coon D, Calotta NA, Broyles JM, Sacks JM. Use of biological tissue matrix in postneurosurgical posterior trunk reconstruction is associated with higher wound complication rates. Plast Reconstr Surg. (2016) 138(1):104e–10e. doi: 10.1097/PRS.0000000000002244
149. Musters GD, Lapid O, Stoker J, Musters BF, Bemelman WA, Tanis PJ. Is there a place for a biological mesh in perineal hernia repair? Hernia. (2016) 20(5):747–54. doi: 10.1007/s10029-016-1504-8
150. Yurteri-Kaplan LA, Gutman RE. The use of biological materials in urogynecologic reconstruction: a systematic review. Plast Reconstr Surg. (2012) 130(5 Suppl 2):242s–53s. doi: 10.1097/PRS.0b013e31826154e4
151. Jensen KK, Rashid L, Pilsgaard B, Møller P, Wille-Jørgensen P. Pelvic floor reconstruction with a biological mesh after extralevator abdominoperineal excision leads to few perineal hernias and acceptable wound complication rates with minor movement limitations: single-centre experience including clinical examination and interview. Colorectal Dis. (2014) 16(3):192–7. doi: 10.1111/codi.12492
152. Peacock O, Pandya H, Sharp T, Hurst NG, Speake WJ, Tierney GM, et al. Biological mesh reconstruction of perineal wounds following enhanced abdominoperineal excision of rectum (APER). Int J Colorectal Dis. (2012) 27(4):475–82. doi: 10.1007/s00384-011-1325-2
153. Butler CE, Langstein HN, Kronowitz SJ. Pelvic, abdominal, and chest wall reconstruction with AlloDerm in patients at increased risk for mesh-related complications. Plast Reconstr Surg. (2005) 116(5):1263–75; discussion 76–7. doi: 10.1097/01.prs.0000181692.71901.bd
154. Becker H, Lind Ii JG. The use of synthetic mesh in reconstructive, revision, and cosmetic breast surgery. Aesthetic Plast Surg. (2020) 44(4):1120–7. doi: 10.1007/s00266-020-01822-y
155. Cook LJ, Kovacs T. Novel devices for implant-based breast reconstruction: is the use of meshes to support the lower pole justified in terms of benefits? A review of the evidence. Ecancermedicalscience. (2018) 12:796. doi: 10.3332/ecancer.2018.796
156. Mangialardi ML, Salgarello M, Cacciatore P, Baldelli I, Raposio E. Complication rate of prepectoral implant-based breast reconstruction using human acellular dermal matrices. Plast Reconstr Surg Glob Open. (2020) 8(12):e3235. doi: 10.1097/GOX.0000000000003235
157. Scalise A, Torresetti M, Verdini F, Capecci M, Andrenelli E, Mengarelli A, et al. Acellular dermal matrix and heel reconstruction: a new prospective. J Appl Biomater Funct Mater. (2017) 15(4):e376–e81. doi: 10.5301/jabfm.5000357
158. Shim HS, Park KS, Kim SW. Preventing postoperative adhesions after hand tendon repair using acellular dermal matrix. J Wound Care. (2021) 30(11):890–5. doi: 10.12968/jowc.2021.30.11.890
159. Blum BE, Burgess AV. Special segment: soft tissue matrices–one form of acellular human dermis for use in tendon and ligament repairs in the foot and ankle. Foot Ankle Spec. (2009) 2(5):235–9. doi: 10.1177/1938640009347455
160. Cole W, Samsell B, Moore MA. Achilles tendon augmented repair using human acellular dermal matrix: a case series. J Foot Ankle Surg. (2018) 57(6):1225–9. doi: 10.1053/j.jfas.2018.03.006
161. Susarla SM, Hauptman J, Ettinger R, Sittler B, Ellenbogen RG. Acellular dermal matrix as a definitive reconstructive option for management of a large myelomeningocele defect in the setting of severe lumbar kyphosis. World Neurosurg. (2019) 129:363–6. doi: 10.1016/j.wneu.2019.06.116
162. Watts V, Attie MD, McClure S. Reconstruction of Complex full-thickness scalp defects after dog-bite injuries using dermal regeneration template (Integra): case report and literature review. J Oral Maxillofac Surg. (2019) 77(2):338–51. doi: 10.1016/j.joms.2018.08.022
163. Lee YJ, Ryoo HJ, Shim HS. Prevention of postoperative adhesions after flexor tendon repair with acellular dermal matrix in zones III, IV, and V of the hand: a randomized controlled (CONSORT-compliant) trial. Medicine (Baltimore). (2022) 101(3):e28630. doi: 10.1097/MD.0000000000028630
164. Liu TH, Hsieh MC, Chou PR, Huang SH. Reconstruction for defects of total nail bed and germinal matrix loss with acellular dermal matrix coverage and subsequently skin graft. Medicina (Kaunas). (2020) 56(1):7. doi: 10.3390/medicina56010017
165. Fiedler DK, Barrett JE, Lourie GM. Nail bed reconstruction using single-layer bovine acellular dermal matrix. J Hand Surg Am. (2017) 42(1):e67–74. doi: 10.1016/j.jhsa.2016.10.010
166. Askari M, Cohen MJ, Grossman PH, Kulber DA. The use of acellular dermal matrix in release of burn contracture scars in the hand. Plast Reconstr Surg. (2011) 127(4):1593–9. doi: 10.1097/PRS.0b013e31820a6511
167. Ellis CV, Kulber DA. Acellular dermal matrices in hand reconstruction. Plast Reconstr Surg. (2012) 130(5 Suppl 2):256s–69s. doi: 10.1097/PRS.0b013e318265a5cf
168. Shang F, Hou Q. Effects of allogenic acellular dermal matrix combined with autologous razor-thin graft on hand appearance and function of patients with extensive burn combined with deep hand burn. Int Wound J. (2021) 18(3):279–86. doi: 10.1111/iwj.13532
169. Brigido SA. The use of an acellular dermal regenerative tissue matrix in the treatment of lower extremity wounds: a prospective 16-week pilot study. Int Wound J. (2006) 3(3):181–7. doi: 10.1111/j.1742-481X.2006.00209.x
170. Brigido SA, Schwartz E, McCarroll R, Hardin-Young J. Use of an acellular flowable dermal replacement scaffold on lower extremity sinus tract wounds: a retrospective series. Foot Ankle Spec. (2009) 2(2):67–72. doi: 10.1177/1938640009333474
171. Cazzell S, Moyer PM, Samsell B, Dorsch K, McLean J, Moore MA. A prospective, multicenter, single-arm clinical trial for treatment of Complex diabetic foot ulcers with deep exposure using acellular dermal matrix. Adv Skin Wound Care. (2019) 32(9):409–15. doi: 10.1097/01.ASW.0000569132.38449.c0
172. Kavros SJ, Dutra T, Gonzalez-Cruz R, Liden B, Marcus B, McGuire J, et al. The use of PriMatrix, a fetal bovine acellular dermal matrix, in healing chronic diabetic foot ulcers: a prospective multicenter study. Adv Skin Wound Care. (2014) 27(8):356–62. doi: 10.1097/01.ASW.0000451891.87020.69
173. Barrett TF, Rasouli JJ, Taub P, Kopell BH. Technical note: preemptive surgical revision of impending deep brain stimulation hardware erosion. World Neurosurg. (2018) 111:41–6. doi: 10.1016/j.wneu.2017.12.045
174. Bondioli E, Purpura V, Orlandi C, Carboni A, Minghetti P, Cenacchi G, et al. The use of an acellular matrix derived from human dermis for the treatment of full-thickness skin wounds. Cell Tissue Bank. (2019) 20(2):183–92. doi: 10.1007/s10561-019-09755-w
175. Chang EI. Latest advancements in autologous breast reconstruction. Plast Reconstr Surg. (2021) 147(1):111e–22e. doi: 10.1097/PRS.0000000000007480
176. Powers JM, Munoz KDR, Parkerson J, Nigro LC, Blanchet NP. From salvage to prevention: a single-surgeon experience with acellular dermal matrix and infection in prepectoral breast reconstruction. Plast Reconstr Surg. (2021) 148(6):1201–8. doi: 10.1097/PRS.0000000000008519
177. Hur GY, Seo DK, Lee JW. Contracture of skin graft in human burns: effect of artificial dermis. Burns. (2014) 40(8):1497–503. doi: 10.1016/j.burns.2014.08.007
178. Guo HL, Ling XW, Liu ZJ, Xu JJ, Lin C, Lu CJ. [Split-thickness scalp and allogenic acellular dermal matrix in repairing deep wounds of hands in patients with extremely extensive burns]. Zhonghua Shao Shang Za Zhi. (2019) 35(12):876–8. doi: 10.3760/cma.j.issn.1009-2587.2019.12.009
179. Tang B, Zhu B, Liang YY, Bi LK, Chen B, Hu ZC, et al. Early escharectomy and concurrent composite skin grafting over human acellular dermal matrix scaffold for covering deep facial burns. Plast Reconstr Surg. (2011) 127(4):1533–8. doi: 10.1097/PRS.0b013e31820a63e8
180. Chen SG, Tzeng YS, Wang CH. Treatment of severe burn with DermACELL(®), an acellular dermal matrix. Int J Burns Trauma. (2012) 2(2):105–9. PMID: 23071908.23071908
181. Janis JE, Nahabedian MY. Acellular dermal matrices in surgery. Plast Reconstr Surg. (2012) 130(5 Suppl 2):7s–8s. doi: 10.1097/PRS.0b013e31825f2d20
182. Beaudoin Cloutier C, Guignard R, Bernard G, Gauvin R, Larouche D, Lavoie A, et al. Production of a bilayered self-assembled skin substitute using a tissue-engineered acellular dermal matrix. Tissue Eng Part C Methods. (2015) 21(12):1297–305. doi: 10.1089/ten.tec.2015.0258
183. Heimbach D, Luterman A, Burke J, Cram A, Herndon D, Hunt J, et al. Artificial dermis for major burns. A multi-center randomized clinical trial. Ann Surg. (1988) 208(3):313–20. doi: 10.1097/00000658-198809000-00008
184. Demircan M, Cicek T, Yetis MI. Preliminary results in single-step wound closure procedure of full-thickness facial burns in children by using the collagen-elastin matrix and review of pediatric facial burns. Burns. (2015) 41(6):1268–74. doi: 10.1016/j.burns.2015.01.007
185. Bloemen MCT, van Leeuwen MCE, van Vucht NE, van Zuijlen PPM, Middelkoop E. Dermal substitution in acute burns and reconstructive surgery: a 12-year follow-up. Plast Reconstr Surg. (2010) 125(5):1450–9. doi: 10.1097/PRS.0b013e3181d62b08
186. Guo ZQ, Qiu L, Gao Y, Li JH, Zhang XH, Yang XL, et al. Use of porcine acellular dermal matrix following early dermabrasion reduces length of stay in extensive deep dermal burns. Burns. (2016) 42(3):598–604. doi: 10.1016/j.burns.2015.10.018
Keywords: acellular dermal matrix, ADM, plastic surgery, wound healing, tissue engineering
Citation: Mohammadyari F, Parvin S, Khorvash M, Amini A, Behzadi A, HajEbrahimi R, Kasaei F and Olangian-Tehrani S (2023) Acellular dermal matrix in reconstructive surgery: Applications, benefits, and cost. Front. Transplant. 2:1133806. doi: 10.3389/frtra.2023.1133806
Received: 29 December 2022; Accepted: 13 February 2023;
Published: 10 March 2023.
Edited by:
Bibo Ke, University of California, Los Angeles, United StatesReviewed by:
Seokchan Eun, Seoul National University Bundang Hospital, Republic of KoreaYanis Berkane, Harvard Medical School, United States
© 2023 Mohammadyari, Parvin, Khorvash, Amini, Behzadi, HajEbrahimi, Kasaei and Olangian-Tehrani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sepehr Olangian-Tehrani b2xhbmdpYW5AeWFob28uY29t
Specialty Section: This article was submitted to Tissue Injury, Repair, Inflammation and Aging, a section of the journal Frontiers in Transplantation
 Fatemeh Mohammadyari
Fatemeh Mohammadyari Sadaf Parvin2
Sadaf Parvin2 Amirhasan Amini
Amirhasan Amini Reyhaneh HajEbrahimi
Reyhaneh HajEbrahimi