- 1Unit of Urological Robotic Surgery and Renal Transplantation, University of Florence, Careggi Hospital, Florence, Italy
- 2Department of Experimental and Clinical Medicine, University of Florence, Florence, Italy
- 3Unit of Oncologic Minimally Invasive Urology and Andrology, University of Florence, Careggi Hospital, Florence, Italy
Objective: To date, several ultra-minimally-invasive surgical techniques are available for the treatment of male LUTS due to benign prostatic obstruction (BPO). Herein we report our preliminary experience with SoracteLite™ TPLA for the treatment of carefully selected patients with LUTS due to BPO.
Methods: Data from all consecutive patients undergoing TPLA at our institution between April 2021 and February 2022 were prospectively collected in a specific database. Data regarding functional and sexual outcomes evaluated by validated questionnaires and uroflowmetry were analyzed. All the procedure were performed in an outpatient setting, under local anesthesia and conscious sedation, using EchoLaser device, a multisource diode laser generator.
Results: Overall, 38 patients underwent TPLA at our institution during the study period. The median prostate volume was 46 ml (IQR 38-71). The median time to complete the procedure was 31 min (IQR 28-37). All patients but one were discharged within 8 hours of hospital stay. No perioperative Clavien-Dindo grade ≥2 complications were recorded. Median improvement in Qmax was 17%, 24% and 32% at 1 month, 3 months and last follow-up after surgery; as a result, the median postoperative IPSS at 1 month, 3 months and at last follow-up decreased by -14%, -36% and -35%, respectively. All patients preserved ejaculatory and sexual function. Two patients (5%), catheter carriers before the procedure, experienced acute urinary retention after TPLA treatment and required replacement of an indwelling catheter.
Conclusions: TPLA can be a feasible, safe and effective ultra-minimally-invasive procedure for carefully selected patients with LUTS due to BPO.
Introduction
Benign Prostatic Obstruction (BPO) is one of the most common causes of lower urinary tract symptoms (LUTS) in adult men resulting in a non-negligible impact on the quality of life (QoL). The latest european guidelines on Non-Neurogenic Male LUTS recommend change in the lifestyle and pharmacological therapy as first line of treatment, followed by surgery in case of failure or intolerance (1).
Surgical treatment of patients with male LUTS due to BPO is a field in constant evolution. The advent of endoscopy and the development of less invasive techniques has brought about an epochal change in surgery for BPO, reducing complication rates and operative times and ensuring rapid recovery. Moreover, the evolution of laser technologies (Holmium, Greenlight and Thulium lasers) and related enucleative techniques (HoLEP, GreenLEP, ThuLEP) has made it possible to endoscopically treat patients with almost any prostate volume, becoming the first choice for the larger ones (1).
Of note, in the last 5 years, several ultra-minimally invasive surgical techniques (uMISTs) have been added to the armamentarium of the urologist to personalize treatment of patients with LUTS due to BPO (2–5).
Several factors might explain this constant evolution. Firstly, the desire to meet the patient’s wishes on maintaining ejaculation and to offer a treatment that might be as tailored as possible to the individual clinical scenario. In particular, a recent systematic review evaluated the available evidence regarding the values, preferences, and expectations of men towards the investigation and treatment of LUTS and found out that men prefer lower-risk management options that have fewer sexual side effects and are primarily effective at improving urgency incontinence and nocturia, with variable preferences depending on baseline symptom severity and the risk/benefit characteristics of the treatment (6).
Although uMISTs generally provide inferior improvements in functional outcomes as compared to gold standard procedures as transurethral resection of prostate (TURP) or laser enucleative techniques, they allow in most cases to maintain ejaculation while still guaranteeing favourable functional outcomes. Moreover, they can be performed under local anaesthesia and even in an outpatient setting, ensuring short recovery times and reducing hospital loads (1–4).
In this scenario, transperineal interstitial laser ablation of the prostate (TPLA) represents a novel option for minimally invasive treatment of BPO; although it is still not recommended by the latest European Association of Urology (EAU) Guidelines, it has shown promising results in terms of feasibility and safety (7–12). Nevertheless, data in literature are still scarce regarding the best indications, functional outcomes and patient-reported outcomes after TPLA.
Herein we report our preliminary experience with TPLA for the treatment of carefully selected patients with LUTS due to BPO, focusing on technical feasibility and on early functional and sexual outcomes.
Methods
Study cohort, inclusion and exclusion criteria, data collection
After Institutional Review Board approval and obtained patients’ written informed consent, data from all consecutive patients undergoing TPLA at our institution between April 2021 and February 2022 were prospectively collected in a specific database.
Inclusion criteria were age ≥ 45 years; moderate to severe LUTS due to BPO with an International Prostate Symptom Score, (IPSS) score ≥ 12; prostate volume ≥ 30 mL and ≤ 100mL; ineffectiveness of medical therapies due to lack of efficacy, intolerance, or poor compliance. Patients with clinical suspicion of prostate cancer or prostate cancer history, neurogenic bladder disfunctions, urethral strictures, bladder stones were excluded. Patients with an indwelling catheter were considered eligible for TPLA after performing an invasive urodynamic assessment that excluded severe detrusor hypo-contractility.
All patients underwent a standardized preoperative diagnostic work-up including transrectal ultrasound (TRUS), serum PSA and potentially multiparametric magnetic resonance imaging (mpMRI) in case of suspected prostate cancer. Patients with ultrasound- and/or mpMRI-detected large median lobe were not considered candidates for TPLA.
Patient age, body mass index (BMI), Charlson Comorbidity Index (CCI), anticoagulant/antiplatelet medication, BPH medical history, symptoms index scores including international index of erectile function (IIEF-5), Quality of life (QoL) preoperative International Prostate Symptom Score (IPSS), Male Sexual Health Questionnaire-Ejaculatory Dysfunction (MSHQ-EjD) 3-items and bother as well as clinical data like maximum flow at uroflowmetry (Qmax), prostate-specific antigen (PSA) level, prostate volume, and post-void residual (PVR) were recorded prospectively and included in the database.
Technical equipment
SoracteLite™ TPLA is an ultrasound (US) guided minimally invasive procedure requiring a biplanar TRUS (in our practice, BK 5000) and EchoLaser system consisted of a multisource diode laser with four independent laser sources, operating at 1064 nm wavelength (EchoLaser, El.En. S.p.A, Calenzano, Italy) and a dedicated planning tool (Echolaser Smart Interface, Elesta S.p.A, Calenzano, Italy) with a simulation software that allows the user to plan the treatment and to place applicators in the prostate in a safe manner. The laser light is conveyed by the source to the tissues through 300µm quartz optical fibers with a flat tip (Fiber Optic for PLA, Elesta S.p.A., Calenzano, Italy), which are inserted percutaneously within 21G Chiba needles (Introducer, Elesta S.p.A., Calenzano, Italy). The laser light produces an ellipsoidal shape area of coagulative necrosis around the tip of the fiber (2/3 extended beyond the fiber tip and 1/3 behind it).
Preliminary steps
Routine blood testing, overmentioned functional questionnaires and non-invasive urodynamics data were collected for all patients. Intravenous antibiotic prophylaxis with 2g cephazolin was administered within one hour before the procedure. Medical thromboprophylaxis and suspension of antiplatelet agents were generally not required, except for highly selected high-risk patients; new oral anticoagulants (NOACs) were discontinued 48 hours before the procedure and reintroduced after 24 hours. A three-way 18-Fr Foley catheter was placed with continuous irrigation, to ensure cooling of the urethral wall during lasing time, avoiding possible thermal damages.
A superficial local anaesthesia of perineum skin and subcutaneous tissue was provided using lidocaine-prilocaine 5% cream and 10 ml of lidocaine 2%. Benzodiazepine oral solution was used for conscious sedation. Therefore, after biplanar transrectal ultrasound probe introduction, 2% lidocaine (10mL) periprostatic anaesthesia at each lobe of the prostate and gland measurements were performed.
Transperineal laser ablation procedure
Our technique for TPLA followed the technical principles previously described by other experiences (8, 13).
The procedure has been performed in an outpatient setting equipped with a surgical table with legs support. Although only a surgeon is needed, the technical support of a clinical specialist is advisable, especially for the first cases. After local disinfection, one 21G needle was introduced transperineally and located in the middle of each lobe, under ultrasound guidance, with its orientation parallel to the longitudinal axis of the gland.
Before starting the treatment security distances from the urethra (8 mm, thus preventing possible damages resulting in hematuria, storage LUTS and lumen stenosis) and from the bladder neck (around 15 mm, critical to avoid ejaculatory dysfunction) were checked. The procedure was then planned thanks to the Echolaser Smart Interface (ESI), a dedicated device with a planning software connected with the video output of the US system, for real-time user assistance in performing the procedure, helping to establish the correct position of applicators showing an ellipsoidal shape area that takes into account safety distances to maintain from critical structures.
The stopper devices were applied to fix the needle in the desired position, preventing their intraprocedural misplacement; the 300 micrometers disposable optical fibers were then introduced. After the insertion of the applicators, a check of their safe position was performed with ESI.
The starting power energy was 5 W, reduced in about 2 minutes to 3,5 W, when a cavity starts to grow with vapor formation resulting in bubbles hyperechoic images at US. In our experience, we used a fixed protocol to deliver laser energy, consisting in 1400 J per fiber. In case of large prostates, a pull back, retraction of the applicator of 10 mm along its trajectory,was performed allowing the ablation of another part of the prostatic tissue, delivering additional laser energy up to 1800 J per fiber.
Postoperative management and follow-up
At the end of the treatment 20 mg of Metilprednisolone iv was administered for anti-edema and anti-inflammatory purposes. An antibiotic (cefixime 400mg daily), pain relief (ibuprofen 600mg twice a day) and gastroprotective therapy (pantoprazole 20mg daily) was given for 1 week. After an observation period of a few hours in the outpatient clinic, patients were discharged from the hospital with the urinary catheter in place, to be removed 7 days after procedure in absence of complications. We removed the catheter 1 week after the treatment according to our internal postoperative management, but there is the potential to remove the catheter before. At 1 and 3 months after TPLA, patients underwent uroflowmetry and symptoms evaluation through validated questionnaires. A further evaluation was subsequently performed for all patients with variable timing, collecting the same information of the first two. Complications were recorded and classified according to the modified Clavien-Dindo classification (14).
Statistical analysis
Descriptive statistics were obtained reporting medians (and interquartile ranges, IQR) for continuous variables, and frequencies and proportions for categorical variables, as appropriate.
The main outcome measures evaluated in this study included both urodynamic measures (Qmax, PRV) and clinical parameters related to urinary, sexual and ejaculatory function.
Statistical analyses were performed using SPSS v. 24 (IBM SPSS Statistics for Mac, Armonk, NY, IBM Corp).
Results
Overall, 38 patients underwent TPLA at our institution during the study period.
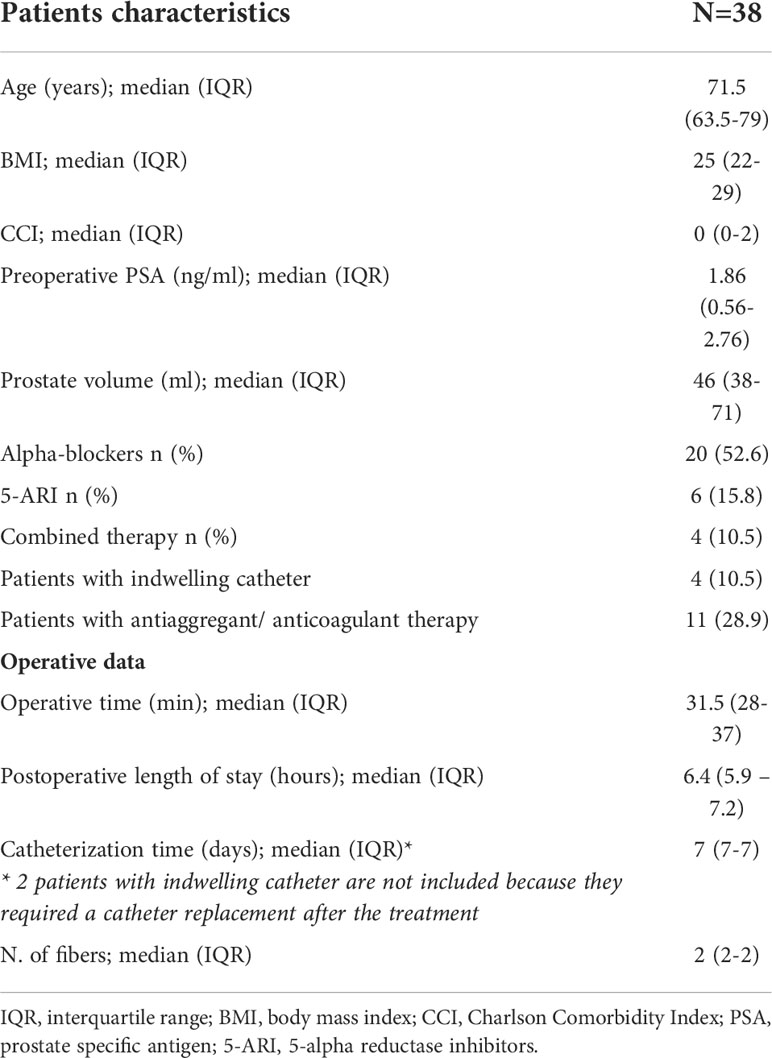
The characteristics of the patients included in the analytic cohort are shown in Table 1. Median age, BMI and CCI were 71.5 years (IQR 63.5-79), 25 (IQR 22-29) and 0 (IQR 0-2), respectively. The median preoperative PSA level was 1.86 ng/mL (IQR 0.56-2.76) while the median prostate volume at TRUS was 46 ml (IQR 38-71). Overall, 24 patients (63%) had a prostate between 30 and 50 mL, 9 patients (24%) between 50 and 80 ml and 5 patients (13%) between 80 and 100 ml. Four (10.5%) patients had an indwelling catheter before the procedure; data about these patients were excluded from the preoperative and postoperative analysis, since data on uroflowmetry or questionnaires on urinary symptoms and sexual function were not available due to the presence of the catheter. A more specific view on the anamnestic, urological characteristics and functional outcomes of the four patients with indwelling catheter, as well as their actual status are depicted in Supplementary Table 1.
The median time to complete the procedure was 31 min (IQR 28-37), using 2 laser fibers in all cases. All but one patient were discharged within 8 hours of hospital stay (median 6.4h; IQR 5.9-7.2). One patient required hospitalization for pelvic discomfort and was discharged on postoperative day 1. The median catheterization time was 7 (IQR 7-7) days. Two patients (5%) experienced acute urinary retention after TPLA and required placement of an indwelling catheter; of note, these patients had an indwelling catheter also before the procedure.
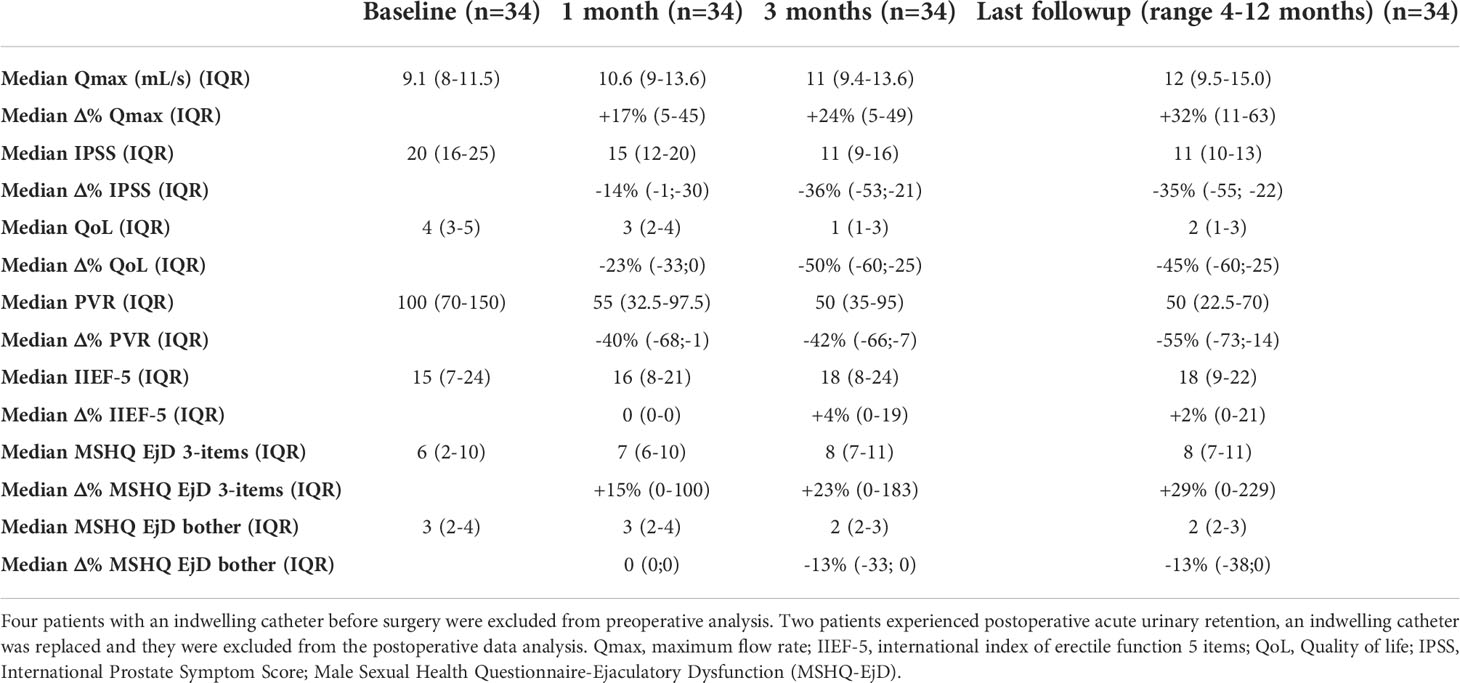
Pre- and postoperative functional and sexual outcomes are depicted in Table 2: a substantial improvement in flowmetry indexes as well as in quality-of-life measures and questionnaires was observed at all time-points.
The median follow-up for patients included in the analysis was 6 months (IQR 4.75-7), ranging from 3 to 12 months.
In particular, the median % improvement in Qmax was 17% at 1 month, 24% at 3 months and 32% at last follow-up. Similarly, a progressive % decrease in PVRs values was noted, namely by 40% after 1 month, by 42% after 3 months and by 52% at last follow-up. These results led to a significant improvement in both IPSS and QoL.
Regarding sexual function, ejaculation was preserved in all patients or even improved according to the results of the MSHQ questionnaires. Erectile function, assessed by the IIEF-5 questionnaire, remained substantially stable.
No perioperative complications were recorded. All patient discontinued medical therapy.
Discussion
In this manuscript we present our preliminary experience with TPLA for the treatment of carefully selected patients with LUTS due to BOO, focusing on its feasibility, safety and early perioperative and functional/sexual outcomes.
The contemporary therapeutic algorithm for patients with LUTS due to BPO currently includes medical therapy (i.e., alpha-blockers alone or in combination with 5-alpha-reductase inhibitors [5-ARI)) as first line treatment in symptomatic patients (1). Nonetheless, alpha-blockers do not affect the clinical evolution of BPH, acting only on patients’ symptomatic burden. On the other hand, 5-ARIs have an impact on clinical progression but a late-onset symptoms relief. Furthermore, these drugs have a non-negligible impact on the sexual sphere, in particular on the ejaculatory function, leading many patients to have low adherence rates or to discontinue the therapy (15, 16).
The latest EAU Guidelines on the management of non-neurogenic male LUTS recommend TURP as first choice option for surgical treatment in patients with LUTS due to BPO and prostate size between 30 and 80 mL while enucleative techniques for larger volumes (>80 mL) (1). Although major strides towards less invasive surgery have been made, these techniques are not devoid of side effects (i.e., the rate of ejaculatory disfunction ranges from 11 to 70%) and require general or spinal anesthesia as well as hospitalization (17, 18). Notably, a recent systematic review evaluating the available evidence regarding the values, preferences, and expectations of men towards the investigation and treatment of LUTS found that men prefer lower-risk management options that have fewer sexual side effects and are primarily effective at improving urgency incontinence and nocturia, with their variable preferences depending on baseline symptom severity and the risk/benefit characteristics of the treatment (6).
As such, the treatment landscape of LUTS due to BPO represents an area of increasing interest for both patients and clinicians, with increasing focus on patients’ quality of life and expectations regarding postoperative sexual and functional outcomes (19, 20). In particular, an increasing body of evidence is showing how surgical approaches and techniques can be tailored to the individual patient’s characteristics and preferences, beyond the anatomical features characterizing BPO itself (21). In this regard, Miernik and Roehrborn in a recent editorial underline in a very timely manner how BPO therapy should not be a ‘‘one-fits-all’’ solution, because treating BPO is not all about the prostate, but “about a man in a social network” (22).
In recent years, the range of options for BPO surgery has undergone a rapid evolution, and a variety of ultra-minimally invasive techniques have been proposed by different groups (2, 4, 5). A recent systematic review including parallel-group randomized controlled trials assessing the effects of several minimally-invasive techniques, including convective radiofrequency water vapor therapy, prostatic arteries embolization (PAE), prostatic urethral lift, temporary implantable nitinol device (TIND) and transurethral microwave thermotherapy, compared to TURP, found low to very-low quality evidence of similar or worse effects concerning urinary symptoms and quality of life at short-term follow-up (4). Another recent systematic review evaluating the perioperative and functional outcomes of uMISTs, concluded that uMISTs can yield fast and effective relief of LUTS without affecting patient quality of life and that only Rezūm, UroLift, and PAE had a minimal impact on patients’ sexual function with respect to baseline, especially regarding preservation of ejaculation (2). All these techniques, including TPLA, can be safely performed in an outpatient setting and may be an option for both patients with higher anesthesiologic risks and those who prefer to avoid a more invasive procedure and/or prefer to avoid sexual dysfunction after treatment. It is important to note that in our series no patient experienced loss of anterograde ejaculation: on the contrary, an improvement in the results of MSHQ questionnaire was noted, probably due to the suspension of alpha-blocker drugs.
Of note, none of the available systematic reviews in this field included data from TPLA, though different authors have already described its feasibility and safety in real-life settings (7–12).
De Rienzo et al. reported the results of TPLA in their prospective cohort of patients with moderate-to-severe LUTS due to BPO and a prostate volume <100 ml (8). The authors found that TPLA achieved good functional outcomes in these carefully selected patients, with ejaculatory function preserved in all patients. The only complication recorded by the authors was a prostatic abscess treated with transperineal drainage and antibiotic. A similar study by Frego et al. in a cohort of patients with slightly higher prostate volumes and including three-lobes prostates confirmed the promising role of TPLA for carefully selected patients with LUTS due to BPO (9). The favorable outcomes obtained by TPLA were reported by similar previous experiences (10–12). While some surgeons did not consider the presence of a prostatic median lobe as a formal contraindication to TPLA (8, 9, 11, 12), in our cohort we selected only patients with BPO without a median lobe, mainly due to learning curve issues. Yet, after proper expertise in the technique is reached, the presence of a median lobe could theoretically not be an absolute contraindication for TPLA, despite the additional challenges of reaching it form a transperineal approach. Further research is needed to assess the feasibility, safety and outcomes of TPLA in this specific patient cohort. Another debated theme is also the potential contraindication for TPLA represented by patients with BPO and an indwelling catheter, which was considered an exclusion criterion by some authors (8, 10). As reported above, we included 4 patients with indwelling catheter in our analysis, obtaining resumption of micturition after treatment in two (50%) of them. In all these patients, preoperative invasive urodynamic evaluation ruled out an impaired bladder contractility before TPLA.
Although TPLA represents a promising ultra-minimally-invasive option for selected patients with BPO, it is still not currently recommended by EAU Guidelines (1) due to lack of robust high-quality studies comparing its efficacy with the current gold standard treatments. In particular, the clinical improvements reported with this technique might theoretically be still inferior to those obtained by recommended techniques such as TURP and enucleative procedures, especially from a pure urodynamic standpoint. On the other side, TPLA has several potential advantages over traditional techniques, including avoidance of general anesthesia, performance in an outpatient setting, the low risk of intra- and perioperative adverse events and the virtually absent risk of ejaculatory disfunction (3, 7–12). In this regard, the right placement of the applicators and the use of the planning software of Echolaser Smart Interface during TPLA is crucial to maintain a safe distance from the bladder neck and the urethral lumen (Figure 1). In fact, precise needle placement is a critical factor to optimize patient outcomes. The number of the needle to place per lobe and the energy settings are also debated topics with different approaches according to each author (7–12). In this study we used one fiber per lobe in all cases to ensure the best safety outcomes respecting all safety landmarks, preferring the pull-back technique to a second fiber placement in case of large prostates.
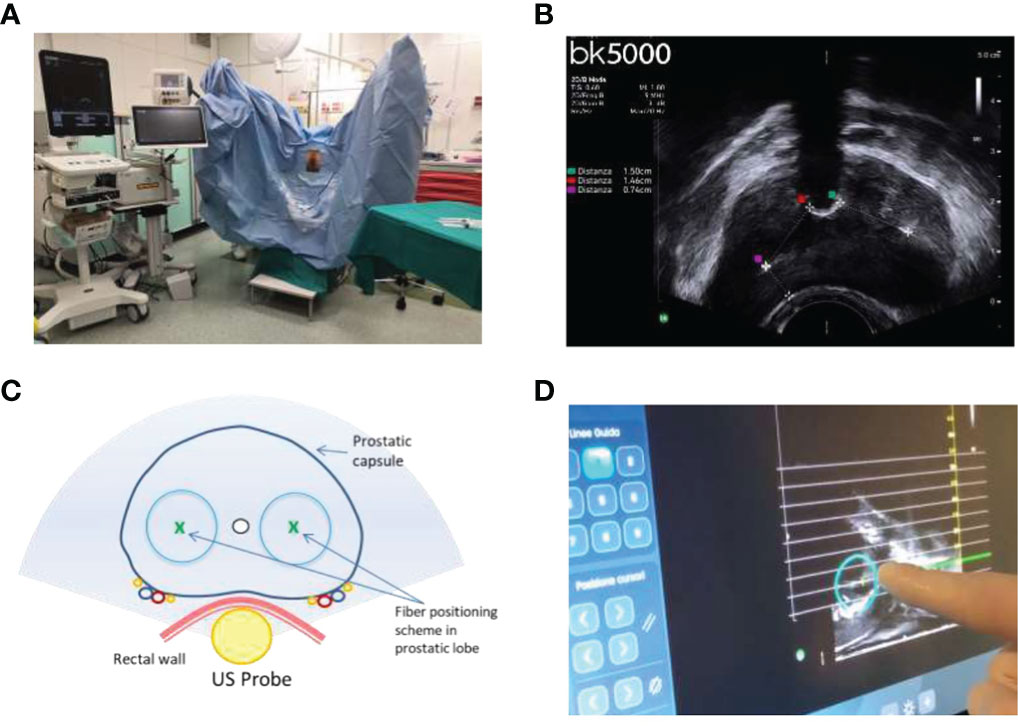
Figure 1 (A) Outpatient clinic setting. (B) Ultrasound security distances evaluation between needle/laser optic fiber tip complex and safety landmarks (urethral lumen wall, bladder neck, prostate capsule). (C) Schematic representation of treatment procedure with anatomical landmarks. (D) Before delivering the energy, Echolaser Smart Interface (ESI) software enables an optimal pre procedural planning. Once set the desired treatment parameters (needle insertion angle, fibers number, pullback etc.), an ellipsoidal shaped area will simulate the treatment zone where critical structures should not be contained in, aiming to preserve them from the effect of thermal damage.
Our study is not devoid of limitations. First, this is a preliminary, single-Centre experience with a relatively low sample size, short follow-up and lack of a control group. Second, our findings might not be generalizable to other healthcare and clinical contexts. Lastly, we did not perform any analysis on the cost-effectiveness of TPLA vs TURP or other gold-standard enucleative techniques.
Acknowledged these limitations, our experience provides additional evidence supporting the feasibility and safety of TPLA for the treatment of carefully selected patients with LUTS due to BPH.
Larger prospective (ideally randomized) comparative studies with longer follow-up are needed to assess the benefits, cost-effectiveness and limits of TPLA for the treatment of patients with LUTS due to BPO, as compared to both gold standard techniques as well as new emerging procedures (2). Several clinical trials evaluating TPLA are ongoing (Table 3) (23–27).
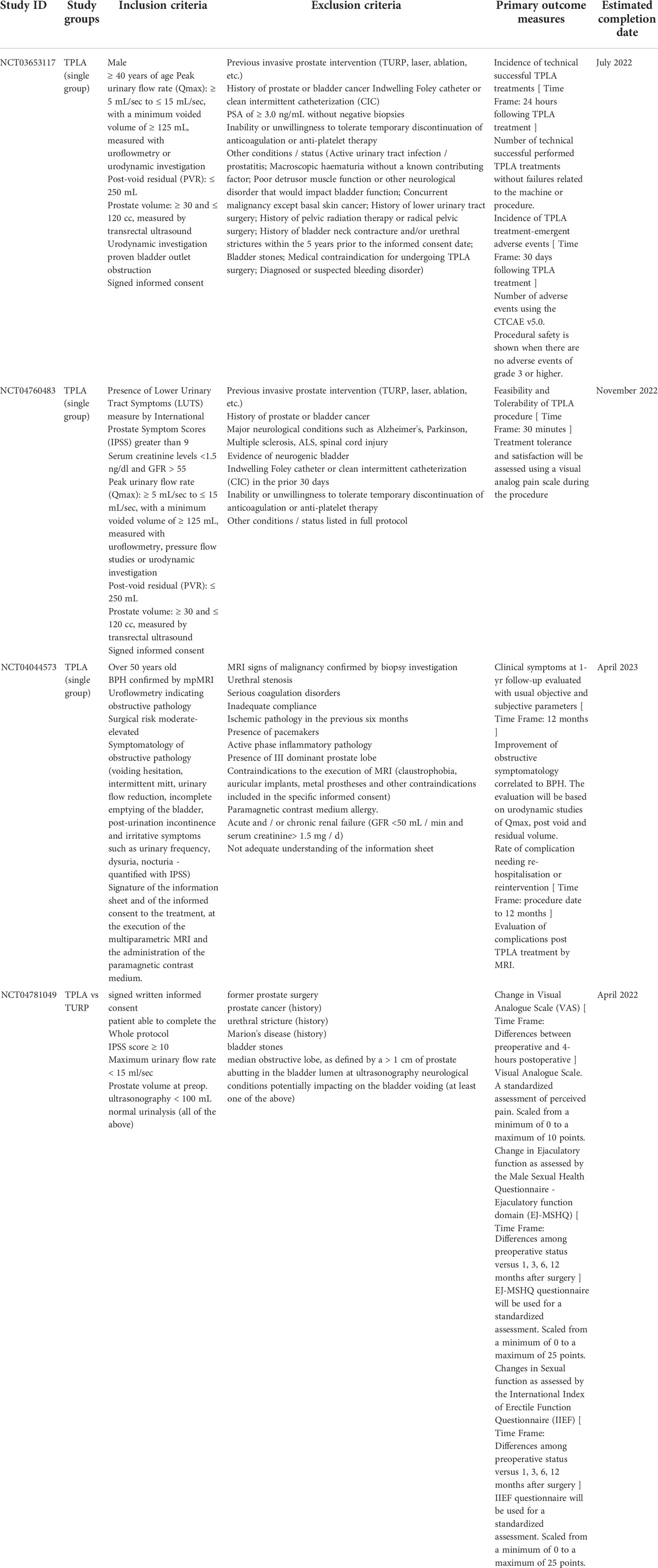
Table 3 Ongoing trials on TPLA (source: clinicaltrials.gov).
Of note, integration of TPLA into the therapeutic armamentarium for BPO will require careful patient selection and judicious decision-making to tailor the techniques to the most suitable candidates (and not vice versa), aiming to achieve the best postoperative outcomes according to patients’ characteristics and expectations. This strategy will hopefully provide insights for profiling the ideal candidates for each therapeutic option among the wide panorama of microinvasive treatments (2, 5).
Conclusions
Our preliminary experience confirms that in experienced hands TPLA can be a feasible, safe and effective ultra-minimally-invasive procedure for carefully selected patients with LUTS due to BPO.
Larger prospective and comparative studies are needed to provide further evidence on the long-term outcomes of TPLA and to select the best candidates for this procedure.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
Author contributions
FS, PP, and RC contributed to conception and design of the study. CB, GS and MLR organized the database. AP and PS performed the statistical analysis. PP wrote the first draft of the manuscript. AR, FLC and AC wrote sections of the manuscript. DV, AM, MG, VLM and SS supervised the draft of the manuscript and revised the final version. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fruro.2022.969208/full#supplementary-material
Supplementary Table 1 | Preoperative characteristics and postoperative outcomes of the four patients with indwelling catheter. ASA, American Society of Anesthesiologists; CCI: CCI, Charlson Comorbidity Index; Qmax, maximum flow rate; HoLEP, Holmium Laser Enucleation of Prostate.
References
1. Gravas S, Cornu JN, Gacci M, et al. EAU guidelines on management of non-neurogenic Male lower urinary tract symptoms (LUTS), incl. benign prostatic obstruction (BPO). version 2021. edn. presented at the EAU annual congress Milan (2021). Available at: https://uroweb.org/guideline/treatment-of-non-neurogenic-male-luts/.
2. Checcucci E, Veccia A, De Cillis S, Piramide F, Volpi G, Amparore D, et al. New ultra-minimally invasive surgical treatment for benign prostatic hyperplasia: A systematic review and analysis of comparative outcomes. Eur Urol Open Sci (2021) 33:28–41. doi: 10.1016/j.euros.2021.08.009
3. De Rienzo G, Minafra P, Ditonno P. Reply to davide rosati, riccardo lombardo, cosimo de nunzio, constantino Leonardo, and Andrea tubaro's words of wisdom re: Transperineal interstitial laser ablation of the prostate, a novel option for minimally invasive treatment of benign prostatic obstruction. eur urol 2021;80:673-4. Eur Urol (2022) 81(4):e100-1. doi: 10.1016/j.eururo.2021.12.037
4. Franco JV, Jung JH, Imamura M, Borofsky M, Omar MI, Escobar Liquitay CM, et al. Minimally invasive treatments for lower urinary tract symptoms in men with benign prostatic hyperplasia: a network meta-analysis. Cochrane Database Syst Rev (2021) 7(7):CD013656. doi: 10.1002/14651858.CD013656.pub2
5. Manfredi C, Arcaniolo D, Spatafora P, Crocerossa F, Fusco F, Verze P, et al. Emerging minimally invasive transurethral treatments for benign prostatic hyperplasia: a systematic review with meta-analysis of functional outcomes and description of complications. Minerva Urol Nephrol (2022) 4(4):389–99. doi: 10.23736/S2724-6051.21.04530-4
6. Malde S, Umbach R, Wheeler JR, Lytvyn L, Cornu JN, Gacci M, et al. A systematic review of patients' values, preferences, and expectations for the diagnosis and treatment of Male lower urinary tract symptoms. Eur Urol (2021) 79(6):796–809. doi: 10.1016/j.eururo.2020.12.019
7. Cai HJ, Fang JH, Kong FL, Xu CK, Chen CH, Wang W, et al. Ultrasound-guided transperineal laser ablation for percutaneous treatment of benign prostatic hyperplasia: a new minimally invasive interventional therapy. Acta Radiol (2022) 63(4):553–8. doi: 10.1177/02841851211003289
8. de Rienzo G, Lorusso A, Minafra P, Zingarelli M, Papapicco G, Lucarelli G, et al. Transperineal interstitial laser ablation of the prostate, a novel option for minimally invasive treatment of benign prostatic obstruction. Eur Urol (2021) 80(1):95–103. doi: 10.1016/j.eururo.2020.08.018
9. Frego N, Saita A, Casale P, Diana P, Contieri R, Avolio PP, et al. Feasibility, safety, and efficacy of ultrasound-guided transperineal laser ablation for the treatment of benign prostatic hyperplasia: a single institutional experience. World J Urol (2021) 39(10):3867–73. doi: 10.1007/s00345-021-03685-7
10. Manenti G, Perretta T, Calcagni A, Ferrari D, Ryan CP, Fraioli F, et al. 3-T MRI and clinical validation of ultrasound-guided transperineal laser ablation of benign prostatic hyperplasia. Eur Radiol Exp (2021) 5(1):41. doi: 10.1186/s41747-021-00239-9
11. Pacella CM, Patelli G, Iapicca G, Manenti G, Perretta T, Ryan CP, et al. Transperineal laser ablation for percutaneous treatment of benign prostatic hyperplasia: a feasibility study. results at 6 and 12 months from a retrospective multi-centric study. Prostate Cancer Prostatic Dis (2020) 23(2):356–63. doi: 10.1038/s41391-019-0196-4
12. Patelli G, Ranieri A, Paganelli A, Mauri G, Pacella CM. Transperineal laser ablation for percutaneous treatment of benign prostatic hyperplasia: A feasibility study. Cardiovasc Intervent Radiol (2017) 40(9):1440–6. doi: 10.1007/s00270-017-1662-9
13. Sessa F, Bisegna C, Polverino P, Gacci M, Siena G, Cocci A, et al. Transperineal laser ablation of the prostate (TPLA) for selected patients with lower urinary tract symptoms due to benign prostatic obstruction: a step-by-step guide. Urol Video J (2022). doi: 10.1016/j.urolvj.2022.100167
14. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg (2004) 240:205–13. doi: 10.1097/01.sla.0000133083.54934.ae
15. Cindolo L, Pirozzi L, Sountoulides P, Fanizza C, Romero M, Castellan P, et al. Patient’s adherence on pharmacological therapy for benign prostatic hyperplasia (BPH)-associated lower urinary tract symptoms (LUTS) is different: is combination therapy better than monotherapy? BMC Urol (2015) 15:96. doi: 10.1186/s12894-015-0090-x
16. Gacci M, Ficarra V, Sebastianelli A, Corona G, Serni S, Shariat SF, et al. Impact of medical treatments for male lower urinary tract symptoms due to benign prostatic hyperplasia on ejaculatory function: a systematic review and meta-analysis. J Sex Med (2014) 11(6):1554–66. doi: 10.1111/jsm.12525
17. Couteau N, Duquesne I, Frédéric P, Thiounn N, Timsit MO, Mejean A, et al. Ejaculations and benign prostatic hyperplasia: An impossible compromise? a comprehensive review. J Clin Med (2021) 10(24):5788. doi: 10.3390/jcm10245788
18. De Nunzio C, Tabatabaei S, Tubaro A. Ejaculation disorders in prostate surgery. Minerva Urol Nefrol (2019) 71(5):549–50. doi: 10.23736/S0393-2249.19.03638-5
19. Gravas S. Hot topics in the clinical practice guidelines for treatment of Male lower urinary tract symptoms due to benign prostatic obstruction. Eur Urol Focus (2022) 8(2):396–8. doi: 10.1016/j.euf.2022.03.006
20. Sokolakis I, Pyrgidis N, Russo GI, Sountoulides P, Hatzichristodoulou G. Preserving ejaculation: A guide through the landscape of interventional and surgical options for benign prostatic obstruction. Eur Urol Focus (2022) 8(2):380–3. doi: 10.1016/j.euf.2022.03.008
21. Gross AJ, Netsch C. Does a 55-year-old Male with lower urinary tract symptoms and a 50-ml gland have to decide between ejaculation and voiding function? Eur Urol Focus (2022) 8(2):375–6. doi: 10.1016/j.euf.2022.03.016
22. Miernik A, Roehrborn CG. Benign prostatic hyperplasia treatment on its way to precision medicine: Dream or reality? Eur Urol Focus (2022) 8(2):363–4. doi: 10.1016/j.euf.2022.03.023
23. ClinicalTrials.gov. Transperineal laser ablation vs transurethral resection for benign prostatic obstruction: A randomized clinical trial . Available at: https://clinicaltrials.gov/ct2/show/NCT04781049.
24. ClinicalTrials.gov. Office based transperineal laser ablation for benign prostatic hyperplasia HYPERPLASIA . Available at: https://clinicaltrials.gov/ct2/show/NCT04760483.
25. ClinicalTrials.gov. Registry: TPLA for LUTS . Available at: https://clinicaltrials.gov/ct2/show/NCT04044573.
26. ClinicalTrials.gov. Transperineal laser ablation for treatment of benign prostatic obstruction . Available at: https://clinicaltrials.gov/ct2/show/NCT03653117.
27. Zhang W, Zhang W, Guo Q, Chen L, Meng Z, Xu Y, et al. The design and rationale of a multicentre randomised controlled trial comparing transperineal percutaneous laser ablation with transurethral resection of the prostate for treating benign prostatic hyperplasia. Front Surg (2021) 8:755957. doi: 10.3389/fsurg.2021.755957
Keywords: benign prostatic hyperplasia, minimally invasive surgical techniques, interstitial laser, transperineal, lower urinary tract symptoms, ejaculation sparing
Citation: Sessa F, Polverino P, Bisegna C, Siena G, Lo Re M, Spatafora P, Pecoraro A, Rivetti A, Conte FL, Cocci A, Villari D, Minervini A, Gacci M, Li Marzi V, Serni S and Campi R (2022) Transperineal laser ablation of the prostate with EchoLaser™ system: perioperative and short-term functional and sexual outcomes. Front. Urol. 2:969208. doi: 10.3389/fruro.2022.969208
Received: 14 June 2022; Accepted: 08 July 2022;
Published: 04 August 2022.
Edited by:
Gian Maria Busetto, University of Foggia, ItalyReviewed by:
Matteo Ferro, European Institute of Oncology (IEO), ItalyDaniele Amparore, San Luigi Gonzaga University Hospital, Italy
Angelo Porreca, Veneto Institute of Oncology (IRCCS), Italy
Cristian Fiori, University of Turin, Italy
Copyright © 2022 Sessa, Polverino, Bisegna, Siena, Lo Re, Spatafora, Pecoraro, Rivetti, Conte, Cocci, Villari, Minervini, Gacci, Li Marzi, Serni and Campi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Francesco Sessa, ZnJhbmNlc2NvX3Nlc3NhQGhvdG1haWwuaXQ=
†These authors have contributed equally to this work and share first authorship
‡These authors share senior authorship
 Francesco Sessa
Francesco Sessa Paolo Polverino
Paolo Polverino Claudio Bisegna1
Claudio Bisegna1 Donata Villari
Donata Villari Andrea Minervini
Andrea Minervini Sergio Serni
Sergio Serni Riccardo Campi
Riccardo Campi