- 1Department of Molecular, Cellular & Biomedical Sciences, CUNY School of Medicine, New York, NY, United States
- 2Movement Disorders Division, Department of Neurology, Northwell Health, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Long Island, NY, United States
- 3Parkinson's Foundation, New York, NY, United States
- 4Department of Neurology, Baylor College of Medicine, Houston, TX, United States
- 5Dallas Fort Worth Community Health Worker Association, Dallas, TX, United States
- 6Department of Neurology, Feinberg School of Medicine, Northwestern University, Chicago, IL, United States
Parkinson's disease (PD), a progressive neurodegenerative disorder, manifests with motor and non-motor symptoms. Despite similar incidence, in the US, disease management of Hispanic patients with PD is poorer than that of White non-Hispanics, and their participation in clinical trials does not reflect expected values (well below 5% vs. expected values around 20%). Together with other evidence, these observations are expressions of poor healthcare in Hispanic patients with PD, suggesting underutilization of proper healthcare, social and economic disadvantage, and other factors. The scant participation of Hispanic patients in clinical trials further exacerbates care inadequacy. In this paper, after reviewing evidence of healthcare gaps in Hispanic patients with PD and their low participation in research, we present a comprehensive model for reaching these patients and their caregivers, educating them on PD, and engaging them in research. This model is based on the work and experience of the Parkinson's Foundation, which over the years, has worked to increase PD awareness in Hispanic communities. This model is based on the training of promotores de salud (community health workers) inside Hispanic communities, the identification of needs and priorities of patients and caregivers with surveys and focus groups within Hispanic communities, and the patients' feedback about their participation in research. The development of this model could achieve sustainable partnerships with community-based organizations to promote better care and enhance participation in research of Hispanic patients. In turn, this could lead to a better quality of life for all patients with PD and their caregivers.
1 Introduction
Parkinson's disease (PD), the world's fastest-growing neurodegenerative disease, is a progressive condition characterized by motor and non-motor manifestations. The incidence of PD in the US appears to be similar amongst White and Hispanic/Latino peoples (for simplicity, we will use “Hispanic”; De Lau and Breteler, 2006; Aamodt et al., 2023), defined as Spanish-speaking people of Central and South American origin. Nevertheless, the best predictors for optimal care are high social and economic level, marital status, urban living, and being White (Ojukwu et al., 2021). Within the US Hispanic community, which often has incomes below the national median, management of motor and non-motor PD symptoms lags behind that of White non-Hispanic patients. In addition, the participation of Hispanic patients with PD in clinical trials is disproportionately low, with percentages varying from 1.6 to 5.4% (Schneider et al., 2009; Kurlawala et al., 2021), despite Hispanics representing at least 18% of the US population (De Lau and Breteler, 2006). This discrepancy may reflect limited healthcare access or underutilization of healthcare services, social and economic disadvantages, and cultural perception of PD manifestations (Duarte Folle et al., 2023). Unless we address this critical gap, the generalizability and validity of trial results in PD will remain limited, and Hispanic patients with PD will remain caught in a vicious cycle of inadequate care. This is rather crucial, as the Hispanic population is one of the fastest-growing demographic groups, fueled by factors such as immigration, higher birth rates, and a youthful population. A notable increase in life expectancy parallels this demographic trend, thus increasing the urgency to devise ways for greater access to care and participation in clinical trials of Hispanic patients with PD. Here, we first review the evidence of healthcare gaps in Hispanic patients with PD, studies underlying their low participation in research, and the attempts to foster their engagement in clinical trials. We then describe a possible model to address these problems based on the experience of recent initiatives by the Parkinson's Foundation.
2 Healthcare gaps in Hispanic patients with PD
Several analyses of available data sets have now provided evidence that Hispanic patients with PD may receive inadequate quality of health care compared to White non-Hispanic patients. As an example, a recent review of discharge data (from 2012 to 2018) of the National Inpatient Sample, Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality showed that, among many healthcare inequities, Hispanic patients with PD are less likely to be treated with deep brain stimulation than White patients (Dorritie et al., 2023), confirming earlier findings (Willis et al., 2014). Also, there are only a few clinical studies or trials focused on Hispanic patients with PD, and only in one of them, which combined two cohorts followed for a few years in two different periods in California, Hispanic patients were present in representative proportion (18%, corresponding to N = 138; Duarte Folle et al., 2023). That longitudinal study showed that in Hispanic patients, PD symptoms and signs appear at a younger age, progress faster in terms of the Hoehn & Yahr scale, and are, on average, more severe compared to their non-Hispanic counterparts (Duarte Folle et al., 2023). Moreover, studies indicate that in a large proportion of Hispanic patients, little or no drug adjustment occurs with the progression of the symptoms (Duarte Folle et al., 2023), even though changes in pharmacological treatment can improve life quality, prevent comorbidities and delay disability. This suboptimal therapeutical management may stem from a lack of financial resources, language and cultural obstacles, and difficulty in accessing adequate medical facilities, prescriptions, and medications. Indeed, studies have found that Hispanic patients with PD are 40% less likely to seek neurological care (Saadi et al., 2017) and in particular, to be cared for by a movement disorders specialist (Willis et al., 2011). This population also has lower access to nursing facilities than White non-Hispanic patients (Kumar et al., 2024). Altogether, these care differences may account for faster time to disability and earlier age at death in Hispanic patients with PD (Duarte Folle et al., 2023). Since the Hispanic population is the fastest growing in the U.S., as per the 2020 Census, finding strategies to improve quality and access to movement disorder care is imperative.
The impact of PD extends beyond motor symptoms. Depression is a frequent non-motor symptom of PD that may precede the appearance of motor symptoms. Notably, depression is more frequent and severe in Hispanic than in White non-Hispanic patients with PD (Duarte Folle et al., 2023; Jones et al., 2023), a finding in line with the fact that people of Hispanic origin display the highest rates of depression compared to non-Hispanic populations (Hooker et al., 2019). The higher depression rate in Hispanic PD patients can be accounted for by the lower use of antidepressant drugs (Cheng et al., 2008; Duarte Folle et al., 2023), thus pointing to underutilization of medical services of Hispanic people, another potential gap in their healthcare quality. Importantly, reduced care for depression significantly increases the risk of developing other non-motor signs of PD, such as cognitive impairment (Babulal et al., 2022). Indeed, a study following for some years a substantial number of Hispanics with PD, reported that Hispanic patients with PD had lower scores in cognitive tests (Duarte Folle et al., 2023). These gaps in healthcare quality likely have significant negative impacts on the Hispanic patient population.
In summary, Hispanic patients with PD, on average, experience lower quality of clinical care, including delayed diagnosis, poorer care, and inadequate treatment for both motor and non-motor symptoms. Limited access to proper healthcare, social and economic disadvantage, language barrier, and perception of both the disease's clinical manifestations and the healthcare environment may be the major contributors to healthcare problems in PD. These observations highlight the inadequate care of Hispanic patients with PD and the critical need to develop strategies to improve their use of the healthcare system.
3 Healthcare gaps in Hispanic patients with PD parallel low participation in clinical trials
According to the 2020 Census, Hispanic people living in the US were about 62 million (18.9% of the population), the second largest racial or ethnic group after White non-Hispanic people. The Hispanic group includes persons of Mexican, Puerto Rican, Central or South American, Cuban, or other Spanish culture or origin, regardless of race. Mexicans are highly represented with 61.6%, followed by Puerto Ricans (9.6%), Central Americans (9.3%), South Americans (6.4%), other Hispanics (including Spanish; 5.8%), and Cubans (3.9%). New York State, our base of work, has the fourth largest Hispanic population in the United States, with more than 2.4 million in New York City (more than 25%) and 4.8 million in the metro area. Considering areas that are part of the larger New York region up the Connecticut coastline, the number increases to 5.3 million, representing 22% of the region's population. The distribution of the Hispanic population in New York City includes, in decreasing order, Puerto Ricans and Dominicans, followed by Mexicans, Guatemalans, Salvadorians, Ecuadorians, and other origin, with no group reaching a clear majority. Importantly, according to the population estimate of the US Census of July 2022, Hispanic people represented more than 56% of the total population.
Most publications suggest that Hispanic and White non-Hispanic peoples have a similar incidence of PD (i.e., 1% of people older than 60 years; Van Den Eeden, 2003; De Lau and Breteler, 2006). Thus, based on the demographics outlined above, 20% of the participants in clinical trials for PD should be Hispanic patients. Yet, Hispanic research engagement is much lower, with most studies not defining all populations' characteristics. Indeed, a meta-analysis of 239 clinical trials in PD found that only 33 studies—for a total of almost 7,500 participants—specified all populations' characteristics (Schneider et al., 2009). Notably, only eight of the 33 studies included Hispanics/Latinos, for a total of 27 patients, with percentages varying from 1.6 to 5.4% (Schneider et al., 2009), in line with the 2.8% rate of Hispanic participants recruitment observed in the large-scale Parkinson's Progression Markers Initiative (PPMI) multisite study (Kurlawala et al., 2021). Most recently, two clinical trials, the Steady-PD III and the SURE-PD3, were not more successful in recruiting Hispanic participants despite the explicit use of direct or indirect incentives for enrolment: in both studies, only 2.9% of the participants were Hispanics (12 out of 413 and 17 out of 585, respectively; Di Luca et al., 2023). These findings show that, based on ethnic/racial population composition, the recruitment rate of Hispanics in the US is far below expectations, thus lessening the generalizability and validity of the results for persons with PD.
Why is fostering Hispanic patients' enrollment in clinical trials so difficult? While translating study and recruitment materials into Spanish overcomes the language barrier, other factors, such as different views about aging, family involvement, and perception of disease, are in play. The low involvement of Hispanic patients in clinical trials is likely linked to healthcare gaps and their possible causes, as illustrated above. Several studies have used strategies to address social barriers, such as language problems, yet with scant results. To effectively increase the involvement of Hispanic patients in clinical trials, other factors beyond language barriers need to be addressed, such as low healthcare literacy, mistrust in the healthcare system, investigators, and sponsors, lack of clinical trial awareness, poor communication; ineffective recruitment tools, and the concerns associated with disease (Adrissi and Fleisher, 2022; Vaswani et al., 2020; Picillo et al., 2015; Fleisher et al., 2014; George et al., 2014). The picture is further complicated by the patient's difficulty in accessing specialized movement disorders centers, together with a growing paucity of neurologists and movement disorders experts. Therefore, there is an urgent need to develop strategies for effective recruitment and retention of Hispanic patients with PD.
Recent studies have assessed strategies to increase and diversify recruitment for PD clinical studies. For example, Fox Insight used web-based digital marketing campaigns to increase Hispanic participation and the participation of people of lower educational and social and economic levels (Dobkin et al., 2020). It has been suggested that the continuous use of newsletters, social media, and PD-related websites—methods defined as “passive recruitment” tools—must be coupled with the so-called “active recruitment” methods that include networking with local clinicians or other health providers, outreach during PD support groups, and partnerships with community organizations (Picillo et al., 2015). Indeed, changing the environment of the recruitment from the clinic/hospital to more familiar surroundings (Nwabuobi et al., 2019; Fleisher et al., 2018), and directly involving the family with appropriate approaches and language settings (Damron et al., 2021), create a better foundation for building relationship, facilitating trust, and addressing most concerns. Also, engaging community stakeholders, such as those in religious centers, barbershops, beauty parlors, and community centers, can foster recruitment and retention in all communities (Jones and Wells, 2007; Levkoff and Sanchez, 2003; Mensah et al., 2018). In addition to the utilization of community opinion leaders and patient advocates during recruitment and, if possible, early in the study design (Feeney et al., 2020), community physicians, such as internists, primary care physicians, and neurologists, undoubtedly can play an important role. Thus, strategies for effective recruitment and retention of Hispanic patients with PD must be designed to involve community physicians and consider their time, resources, as well as patient concerns (Ison et al., 2024). Such strategies may include supporting research coordinators and implementing local training and educational events for physicians (Tilley et al., 2012).
Together, these studies and observations support the development of strategies that integrate clinical research within the patients' local community and milieu to increase the possibility of recruiting and retaining more Hispanic patients with PD in clinical trials and improve their access to optimal PD care.
4 The Parkinson's Foundation model
People with PD who identify as Hispanic or Latino have been under-resourced not only in Spanish-language education on PD but also in Spanish-speaking providers and support services. The Parkinson's Foundation has been serving Spanish-speaking people with PD for more than 20 years, establishing a variety of programs and resources to better reach people of the Hispanic community, remove obstacles to care, open research participation, and ensure that information and resources are easy to find for all (for example, see: https://www.parkinson.org/espanol). The proposed model (see Figure 1) is based on three main activities: the training of the promotores de salud; the identification of needs and priorities of patients and caregivers with surveys and focus groups within the Hispanic communities, and feedback from Hispanic patients about their participation in research.
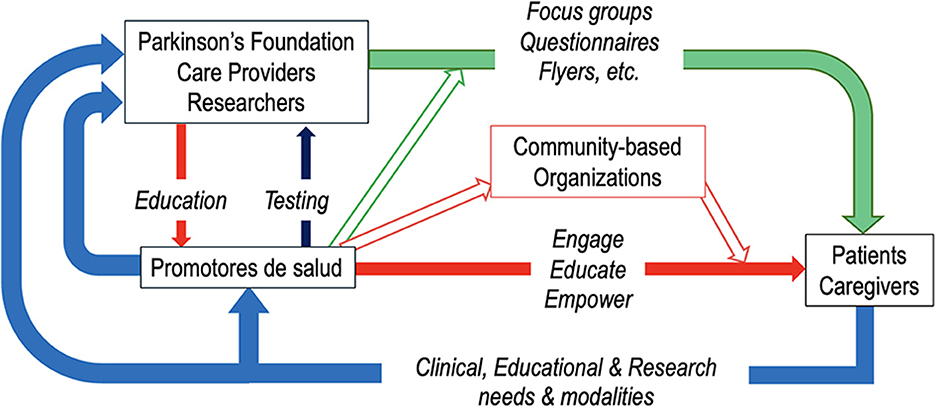
Figure 1. The model of the Parkinson's Foundation to address gaps in care and research participation of Hispanic patients with PD. This model is based on three lines of intervention. The first line is about the training and activities of the promotores de salud (in red). The promotores receive training from the Parkinson's Foundation, care providers, and researchers; provide feedback about the achieved knowledge; establish links with community-based organizations and build an infrastructure to engage, educate, and empower patients and caregivers in the Hispanic community. A second line (in green) exploits all contacts of the Parkinson's Foundation and other sources and uses different means to identify the needs and priorities of patients and caregivers. The third line (in light blue) is based on the collection of direct feedback from patients and caregivers to guide research objectives, modalities of patient participation in research, and clinical and social interventions.
4.1 Training the “promotores de salud”
Leveraging partnerships with different local organizations, the Parkinson's Foundation has used the promotores de salud to engage health educators already embedded in the Hispanic community. Community health worker models have been utilized in communities across the country and internationally to effectively reach various communities in different fields of medicine (Cosgrove et al., 2014). In the Hispanic community, promotores de salud are recognized as lay health workers who work in Spanish-speaking communities and are community leaders, motivators, health educators, champions for health literacy, and community advocates. Like other community health worker models, the promotores de salud program is based on the tested concept that trusted individuals from targeted communities can be the best conduit for outreach, communication, and education (Sapienza et al., 2007).
Since early 2022, the Parkinson's Foundation has provided peer-to-peer education and continuous support on PD education and care in Texas, Arizona, and Illinois, educating and training more than 350 promotores de salud in collaboration with local community organizations. During training sessions conducted in Spanish (see an example in Table 1), participants acquired basic knowledge of PD, identified resources available, and established talking points enabling them to deliver PD education to their community. Faculty included researchers, clinicians, and community health workers who have successfully partnered with Hispanic communities to increase knowledge about PD and engagement in research and care. After the training, promotores were provided with educational materials and resources to return to their communities and build on their outreach programs. Some preliminary results (Aranda et al., 2024) demonstrated the success of this initiative: following the training, analyses of the promotores' questionnaires revealed an increase in PD knowledge and symptom awareness. Moreover, the number of accesses to resources and educational materials of the Parkinson's Foundation (among others: Recursos webpage, Helpline, and Parkinson.org/10 Signos) also increased. By educating trusted individuals within the Hispanic community, this training program can engage and inform about PD Hispanic patients and their families.
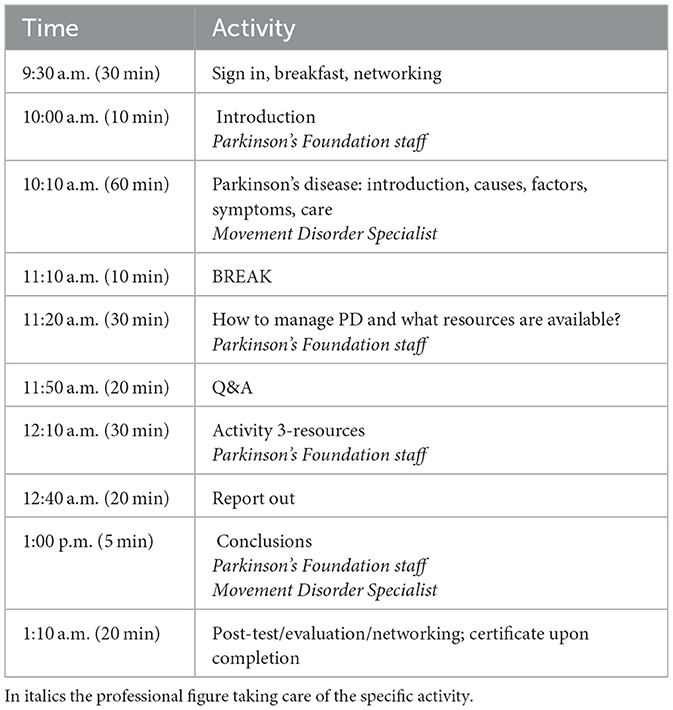
Table 1. An example of schedule and agenda “La enfermedad de Parkinson 101: cómo hablar sobre el Parkinson en su comunidad.”
Based on these results, the promotores de salud could be employed to educate and could be involved in research on Hispanic patients with PD. Specifically, they could help design, explain, and disseminate information for research trials and, most importantly, build a local and permanent infrastructure to be used as a community resource for education and involvement in research.
4.2 Identification of needs and priorities with focus groups and surveys
In addition to the promotores de salud, the Parkinson's Foundation directly engages patients through the Parkinson's Foundation Survey and semi-structured focus groups. These instruments can provide better insights into the unique experiences, needs, and priorities of those affected by PD who identify as Hispanic. In particular, the Parkinson's Foundation Survey initiative invites people with PD, care partners, and medical professionals to share more about living with and treating PD. Surveys can be developed and launched to understand the needs, priorities, knowledge, and attitudes toward research in a specific community and to inform the development of a recruitment model for research. Surveys may be launched in a variety of ways to extend reach or define a target audience (i.e., Hispanic community), using the contacts established by the promotores as well as mailing lists of Hispanic organizations and those of the Parkinson's Foundation that include participants in PD GENEration (Cook et al., 2023), attendees of local, regional, and national Hispanic education as well as outreach events and constituents that identify as Hispanic that have contacted the Parkinson's Foundation helpline.
4.3 Gathering patients' feedback about their participation in research
Another important benefit to improving research participation is facilitating focus groups of Hispanic patients with PD participating in research studies to gather feedback about their experience. Work in this specific area is still in progress, and results are not yet available. Nevertheless, it is plausible that, in this respect, findings from the Parkinson's Foundation Survey and focus groups can provide a framework for improving recruitment models. Contributions to these models include the development of specific recruitment content for dissemination through many platforms, including the Parkinson's Foundation Spanish Facebook groups, targeted recruitment emails, personalized emails to coordinators of the Parkinson's Foundation Centers of Excellence, and scripts about the study for the Parkinson's Foundation Helpline Staff.
In summary, the training of promotores de salud can provide educational programs for Hispanic communities and can be used to monitor patients' feedback on their research experience. This, in turn, can give essential support for the recruitment and participation maintenance of Hispanic patients in research and clinical trials and, thus, more importantly, can lead to better care and access to care for Hispanic patients with PD.
5 Conclusions
The proposed approach will provide a greater understanding of the challenges associated with fostering Hispanic patient participation in clinical trials for PD and a working model for outreach, awareness, education, and recruitment for clinical PD studies in the Hispanic communities. Importantly, this approach could also be adapted for reaching other communities. Those in the Hispanic community suffering from PD are disproportionately impacted by the disease symptoms while at the same time being inadequately represented in clinical research. The development of this research engagement model in the Hispanic population will not only provide local infrastructure for outreach and clinical studies, such as the genetic studies proposed in the PD GENEration (Cook et al., 2023), but, most importantly, has the potential to become the means to educate patients and implement better clinical care for all communities and groups. Furthermore, this program can establish sustainable partnerships with community-based organizations to empower patients, promote research efforts, and disseminate knowledge about PD. Altogether, these strategies may become essential tools for improving Hispanic patients' health, enhancing their quality of life, and promoting initial steps toward universal PD care.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
MFG: Conceptualization, Funding acquisition, Project administration, Resources, Writing – original draft, Writing – review & editing. AD: Writing – review & editing. JF: Writing – review & editing. DS: Writing – review & editing. ML: Writing – review & editing. NV-A: Writing – review & editing. ET: Writing – review & editing. MA: Writing – review & editing. ES: Writing – review & editing. DH: Writing – review & editing. PL-G: Writing – review & editing. M-MD: Writing – review & editing. CE: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work has been supported by the NIH grant U54MD017979 (PI: MFG). This work was also funded by the Parkinson's Foundation.
Acknowledgments
The authors gratefully acknowledge the contributions of people with Parkinson's, promotores de salud, Dr. Katherline Longardner, Dr. Juan Ramirez-Castaneda, and Dr. Charenya Anandan for developing the research engagement model.
Conflict of interest
The authors declare that the research was conducted without any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aamodt, W. W., Willis, A. W., and Dahodwala, N. (2023). Racial and ethnic disparities in Parkinson disease. a call to action. Neurol. Clin. Pract. 13:e200138. doi: 10.1212/CPJ.0000000000200138
Adrissi, J., and Fleisher, J. (2022). Moving the dial toward equity in Parkinson's disease clinical research: a review of current literature and future directions in diversifying PD clinical trial participation. Curr. Neurol. Neurosci. Rep. 22, 475–483. doi: 10.1007/s11910-022-01212-8
Aranda, C., Gonzalez-Latapi, P., and Fearday, J. (2024). Community-academic initiative to improve knowledge of Parkinson's disease in Hispanic/Latino community health workers. Neurology 102(7suppl):1. doi: 10.1212/WNL.0000000000206541
Babulal, G. M., Zhu, Y., Roe, C. M., Hudson, D. L., Williams, M. M., Murphy, S. A., et al. (2022). The complex relationship between depression and progression to incident cognitive impairment across race and ethnicity. Alzheimer. Dement. 18, 2593–2602. doi: 10.1002/alz.12631
Cheng, E. M., Siderowf, A. D., Swarztrauber, K., Lee, M., Vassar, S., Jacob, E., et al. (2008). Disparities of care in veterans with Parkinson's disease. Parkinsonism Relat. Disord. 14, 8–14. doi: 10.1016/j.parkreldis.2007.05.001
Cook, L., Verbrugge, J., Schwantes-An, T.-H., Schulze, J., Beck, J. C., Naito, A., et al. (2023). Providing genetic testing and genetic counseling for Parkinson's disease to the community. Genet. Med. 25:100907. doi: 10.1016/j.gim.2023.100907
Cosgrove, S., Monroy, M., Jenkins, C., Castillo, S. R., Williams, C., Parris, E., et al. (2014). Community health workers as an integral strategy in the REACH U.S. Program to eliminate health inequities. Health Promot Pract. 15, 795–802. doi: 10.1177/1524839914541442
Damron, L., Litvan, I., Bayram, E., Berk, S., Siddiqi, B., and Shill, H. (2021). Hispanic perspectives on Parkinson's disease care and research participation. J. Alzheimer. Dis. 81, 809–819. doi: 10.3233/JAD-210231
De Lau, L. M., and Breteler, M. M. (2006). Epidemiology of Parkinson's disease. Lancet Neurology 5, 525–535. doi: 10.1016/S1474-4422(06)70471-9
Di Luca, D. G., Macklin, E. A., Hodgeman, K., Lopez, G., Pothier, L., Callahan, K. F., et al. (2023). Enrollment of participants from marginalized racial and ethnic groups: a comparative assessment of the STEADY-PD III and SURE-PD3 trials. Neurol. Clin. Pract. 13:e200113. doi: 10.1212/CPJ.0000000000200113
Dobkin, R. D., Amondikar, N., Kopil, C., Caspell-Garcia, C., Brown, E., Chahine, L. M., et al. (2020). Fox Insight study, innovative recruitment strategies to increase diversity of participation in Parkinson's disease research: the fox insight cohort experience. J. Parkinsons. Dis. 10, 665–675. doi: 10.3233/JPD-191901
Dorritie, A., Faysel, M., Gruessner, A., and Robakis, D. (2023). Black and hispanic patients with movement disorders less likely to undergo deep brain stimulation. Parkinsonism Relat. Disord. 115:105811. doi: 10.1016/j.parkreldis.2023.105811
Duarte Folle, A., Flores, M. E. S., Kusters, C., Paul, K. C., Del Rosario, I., Zhang, K., et al. (2023). Ethnicity and Parkinson's disease: motor and nonmotor features and disease progression in Latino patients living in rural California. J. Gerontol. Ser. A 78, 1258–1268. doi: 10.1093/gerona/glad016
Feeney, M., Evers, C., Agpalo, D., Cone, L., Fleisher, J., and Schroeder, K. (2020). Utilizing patient advocates in Parkinson's disease: a proposed framework for patient engagement and the modern metrics that can determine its success. Health Expect. 23, 722–730. doi: 10.1111/hex.13064
Fleisher, J., Barbosa, W., Sweeney, M. M., Oyler, S. E., Lemen, A. C., Fazl, A., et al. (2018). Interdisciplinary home visits for individuals with advanced Parkinson's disease and related disorders. J. Am. Geriatr. Soc. 66, 1226–1232. doi: 10.1111/jgs.15337
Fleisher, J., Bhatia, R., Margus, C., Pruitt, A., and Dahodwala, N. (2014). Health literacy and medication awareness in outpatient neurology. Neurol. Clin. Pract. 4, 71–81. doi: 10.1212/01.CPJ.0000436211.73013.ab
George, S., Duran, N., and Norris, K. (2014). A systematic review of barriers and facilitators to minority research participation among African Americans, Asian Americans, and Pacific Islanders. Am. J. Public Health 104, e16–e31. doi: 10.2105/AJPH.2013.301706
Hooker, K., Phibbs, S., Irvin, V. L., Mendez-Luck, C. A., Doan, L. N., Li, T., et al. (2019). Depression among older adults in the United States by disaggregated race and ethnicity. Gerontologist 59, 886–891. doi: 10.1093/geront/gny159
Ison, J. M., Jackson, J. D., Hemley, H., Willis, A., Siddiqi, B., Macklin, E. A., et al. (2024). Fostering inclusivity in research engagement for underrepresented populations in Parkinson's disease: the FIRE-UP PD study. Contemp. Clin. Trials 144:107619. doi: 10.1016/j.cct.2024.107619
Jones, J. D., Uribe-Kirby, R., Rivas, R., Cuellar-Rocha, P., Valenzuela, Y., Luna, K., et al. (2023). Mental health disparities and the role of perceived discrimination among Latinx individuals living with Parkinson's disease. Parkinsonism Relat. Disord. 116:105867. doi: 10.1016/j.parkreldis.2023.105867
Jones, L., and Wells, K. (2007). Strategies for academic and clinician engagement in community-participatory partnered research. JAMA 297, 407–410. doi: 10.1001/jama.297.4.407
Kumar, P., Yasmin, F., Khan, M. S., Shahid, I., Diwan, M. N., Leiter, R. E., et al. (2024). Place of death in Parkinson's disease: trends in the USA. BMJ Support Palliat Care. 14, e1060–e1066. doi: 10.1136/bmjspcare-2021-003016
Kurlawala, Z., Shadowen, P. H., McMillan, J. D., Beverly, L. J., and Friedland, R. P. (2021). Progression of nonmotor symptoms in Parkinson's disease by sex and motor laterality. Parkinson. Dis. 2021, 1–12. doi: 10.1155/2021/8898887
Levkoff, S., and Sanchez, H. (2003). Lessons learned about minority recruitment and retention from the Centers on Minority Aging and Health Promotion. Gerontologist 43, 18–26. doi: 10.1093/geront/43.1.18
Mensah, G. A., Cooper, R. S., Siega-Riz, A. M., Cooper, L. A., Smith, J. D., Brown, C. H., et al. (2018). Reducing cardiovascular disparities through community-engaged implementation research: A National Heart, Lung, and Blood Institute workshop report. Circ. Res. 122, 213–230. doi: 10.1161/CIRCRESAHA.117.312243
Nwabuobi, L., Barbosa, W., Sweeney, M., Oyler, S., Meisel, T., Di Rocco, A., et al. (2019). Sex-related differences in homebound advanced Parkinson's disease patients. Clin. Interv. Aging 14, 1371–1377. doi: 10.2147/CIA.S203690
Ojukwu, D. I., Andruska, K. M., and Halpern, C. H. (2021). Lessons from George Floyd: racial inequalities in the treatment of Parkinson's disease. Movement Disord. 36, 599–603. doi: 10.1002/mds.28388
Picillo, M., Kou, N., Barone, P., and Fasano, A. (2015). Recruitment strategies and patient selection in clinical trials for Parkinson's disease: going viral and keeping science and ethics at the highest standards. Parkinsonism Relat. Disord. 21, 1041–1048. doi: 10.1016/j.parkreldis.2015.07.018
Saadi, A., Himmelstein, D. U., Woolhandler, S., and Mejia, N. I. (2017). Racial disparities in neurologic health care access and utilization in the United States. Neurology 88, 2268–2275. doi: 10.1212/WNL.0000000000004025
Sapienza, J. N., Corbie-Smith, G., Keim, S., and Fleischman, A. R. (2007). Community engagement in epidemiological research. Ambulatory Pediatrics 7, 247–252. doi: 10.1016/j.ambp.2007.01.004
Schneider, M. G., Swearingen, C. J., Shulman, L. M., Ye, J., Baumgarten, M., and Tilley, B. C. (2009). Minority enrollment in Parkinson's disease clinical trials. Parkinsonism Relat. Disord. 15, 258–262. doi: 10.1016/j.parkreldis.2008.06.005
Tilley, B. C., Mainous, A. G., Elm, J. J., Pickelsimer, E., Soderstrom, L. H., Ford, M. E., et al. (2012). A randomized recruitment intervention trial in Parkinson's disease to increase participant diversity: early stopping for lack of efficacy. Clin. Trials 9, 188–197. doi: 10.1177/1740774512436881
Van Den Eeden, S. K. (2003). Incidence of Parkinson's disease: variation by age, gender, and race/ethnicity. Am. J. Epidemiol. 157, 1015–1022. doi: 10.1093/aje/kwg068
Vaswani, P. A., Tropea, T. F., and Dahodwala, N. (2020). Overcoming barriers to Parkinson disease trial participation: increasing diversity and novel designs for recruitment and retention. Neurotherapeutics 17, 1724–1735. doi: 10.1007/s13311-020-00960-0
Willis, A. W., Schootman, M., Evanoff, B. A., Perlmutter, J. S., and Racette, B. A. (2011). Neurologist care in Parkinson disease: a utilization, outcomes, and survival study. Neurology 77, 851–857. doi: 10.1212/WNL.0b013e31822c9123
Keywords: promotores de salud, Latino, Hispanic/Latino, healthcare improvement, Parkinson disease, research participation, community intervention, community health worker
Citation: Ghilardi MF, Di Rocco A, Fearday J, Sperlakis D, Lima M, Vanegas-Arroyave N, Tatti E, Arroyave M, Stevens E, Hernandez D, Latapi-Gonzalez P, Deoudes M-M and Evers C (2025) A model to address healthcare gaps and poor research participation in Hispanic patients with Parkinson's disease. Front. Aging Neurosci. 17:1610448. doi: 10.3389/fnagi.2025.1610448
Received: 12 April 2025; Accepted: 25 July 2025;
Published: 12 August 2025.
Edited by:
Liane Kaufmann, Ernst von Bergmann Clinic, GermanyReviewed by:
Ece Bayram, University of Colorado, United StatesJanice C. Wong, Janssen Pharmaceuticals, Inc., United States
Jori Fleisher, Rush University, United States
Copyright © 2025 Ghilardi, Di Rocco, Fearday, Sperlakis, Lima, Vanegas-Arroyave, Tatti, Arroyave, Stevens, Hernandez, Latapi-Gonzalez, Deoudes and Evers. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: M. Felice Ghilardi, bGljZS5tZzc5QGdtYWlsLmNvbQ==
 M. Felice Ghilardi
M. Felice Ghilardi Alessandro Di Rocco2
Alessandro Di Rocco2 Maria Lima
Maria Lima Elisa Tatti
Elisa Tatti Evelyn Stevens
Evelyn Stevens Christiana Evers
Christiana Evers