- 1Interdisciplinary School of Health Sciences and AGE-WELL Network of Centres of Excellence, University of Ottawa, Ottawa, ON, Canada
- 2School of Epidemiology and Public Health, University of Ottawa, Ottawa, ON, Canada
- 3School of Electrical Engineering and Computer Science, University of Ottawa, Ottawa, ON, Canada
- 4School of Rehabilitation Sciences and AGE-WELL Network of Centres of Excellence, University of Ottawa, Ottawa, ON, Canada
The critical importance of technological innovation in home care for older adults is indisputable. Less well understood is the question of how to measure its performance and impact on the delivery of healthcare to older adults who are living with chronic illness and disability. Knowing how well digital technologies, such as smartphones, tablets, wearable devices, and Ambient Assisted Living Technologies (AAL) systems “work” should certainly include assessing their impact on older adults’ health and ability to function in daily living but that will not guarantee that it will necessarily be adopted by the user or implemented by a healthcare facility or the healthcare system. Technology implementation is a process of planned and guided activities to launch, introduce and support technologies in a certain context to innovate or improve healthcare, which delivers the evidence for adoption and upscaling a technology in healthcare practices. Factors in addition to user acceptance and clinical effectiveness require investigation. Failure to appreciate these factors can result in increased likelihood of technology rejection or protracted procurement decision at the “adoption decision” stage or delayed or incomplete implementation or discontinuance (following initial adoption) during implementation. The aim of our research to analyze research studies on the effectiveness of digital health technologies for older adults to answer the question, “How well do these studies address factors that affect the implementation of technology?” We found common problems with the conceptualization, design, and methodology in studies of digital technology that have contributed to the slow pace of implementation in home care and long-term care. We recommend a framework for improving the quality of research in this critical area.
Systematic Review Registration: https://archive.org/details/osf-registrations-f56rb-v1, identifier osf-registrations-f56rb-v1.
Introduction
The critical importance of technological innovation in home care for older adults is indisputable (Rogers and Mitzner, 2017; Linskell et al., 2019; Rajer and Bogataj, 2022). Less well understood is the question of how to measure its performance and impact on the delivery of healthcare to older adults who are living with chronic illness and disability (Matthew-et al., 2016). Knowing how well digital technologies, such as smartphones, tablets, wearable devices, and Ambient Assisted Living Technologies (AAL) systems “work” should certainly include assessing their impact on older adults’ health and ability to function in daily living. However, it should not be assumed that, because a technology produces clinical benefits and is acceptable to the user, it will necessarily work in the sense that it provides solutions for the needs of users and healthcare facilities that will be adopted and implemented.
Technology implementation has been defined as a process of several planned and guided activities to launch, introduce and maintain technologies in a certain context to innovate or improve healthcare, which delivers the evidence for adoption and upscaling a technology in healthcare practices (van Gemert-Pijnen, 2022). For digital technologies to be successfully implemented in delivery of healthcare and social services to older people, factors in addition to their user acceptance and clinical effectiveness require investigation. Failure to appreciate these factors can result in increased likelihood of technology rejection or protracted procurement decision at the ‘adoption decision’ stage or delayed or incomplete implementation or discontinuance (following initial adoption) during implementation (Kyratsis et al., 2012).
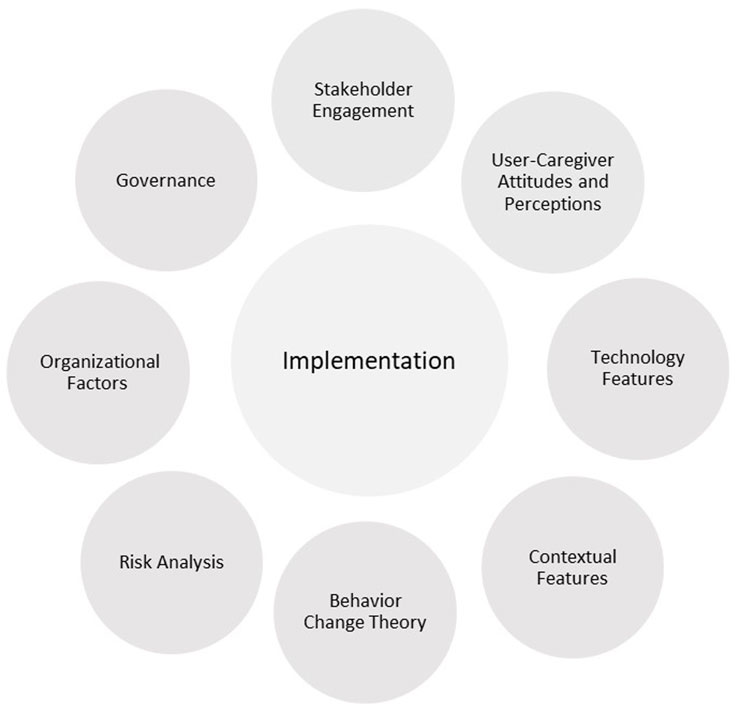
Categories of factors that are proposed to affect the implementation of healthcare technologies have been identified in the literature (Kyratsis et al., 2012; Keyworth et al., 2018; van Gemert-Pijnen, 2022) and are depicted in Figure 1. Some categories, such as Governance, Organizational Factors, and Risk analysis, may be more applicable to some residential settings (e.g., long-term care facilities or retirement communities) than others (e.g., community-dwelling older adults). For example, issues of governance and care facility management would have lesser importance for older adults who consume technologies in their private homes and apartments but significant importance for agencies that purchase and maintain technologies for older adults who are under their care.
Stakeholder engagement is regarded as crucial for ensuring that a technology realizes the values of end users and other stakeholders and identifying issues for implementation (van Gemert-Pijnen, 2022). Behavior change theory is recognized as an important ingredient (Keyworth et al., 2018). Types of technology interventions that have been shown to be effective include reminders and alerts and computer-generated feedback. The most targeted behavior is adherence to clinical prescriptions and prescribing behaviors. Behavior change techniques include instruction on how to perform the behavior, feedback on behavior, prompts and cues, demonstration of the behavior, reducing negative emotions, social comparison, and problem solving. Contextual features include practice and workload considerations. Features of the technology include pilot testing before wide-scale usage, an iterative modification approach, and the ease of use of the technology. The attitudes and perceptions of older adult users and their caregivers, who include healthcare providers, are important for adoption and use. Organizational factors are also critical for successful implementation (Kyratsis et al., 2012). Technology researchers and developers should recognize that the key motivator for adoption decisions by healthcare organizations is finding solutions to problems. Among types of knowledge, scientifically produced research evidence has the highest priority for judging technology effectiveness. It is often combined with experiential (“how-to”) knowledge to evaluate the appropriateness of technology for a particular setting. Governance, by way of establishing vision, leadership, policy, and accountability, is essential for sustaining implementation through appropriate planning, commitment of staff, manageable workload, and positive attitudes (van Gemert-Pijnen, 2022).
There will necessarily be variation in implementation performance since different agencies, whether they be households, healthcare facilities, or healthcare systems, will not respond in these categories in the same way (Goggin, 1986). Technology researchers and developers should be aware of this variation and consider how they might assist potential adopters to do implementation planning within their areas of competence and expertise.
A final set of factors pertains to risk analysis, which helps us understand and prepare responses for the potential risks associated with adopting and implementing the new technologies. Brown and Osborne (Brown and Osborne, 2013) identified the key elements for analysis and classified risks as follows. The locus for consequential risk is the individual and refers to direct risk to the user of the digital health service. For example, deviation from established approaches to home care for older adults may introduce emotional distress and risks to physical health. The locus for organizational risk is the service agency and its staff. The risk here involves vulnerable individuals remaining living independently for longer than they might have been able to and the implications for the organizational or professional reputation and/or legitimacy and sustainability of the service agency. For example, managers and staff tend to be risk averse and may tend toward concealing errors instead of identifying and learning from them. The locus for behavioral risk is the community of interest and involves risk to the stakeholders surrounding a service and/or the wider community. For example, digital health technologies, while offering a more appropriate response to the needs of community-dwelling older adults, can lead to risks to other people in the community, such as distress to uncomprehending relatives and neighbors. Implementation is undermined by failure to acknowledge and discuss these risks.
As an important first step toward understanding the state of knowledge on this topic, we performed a scoping review. The aim was to characterize the research available to address the question, “How well have research studies on the effectiveness of digital health technologies for older adults addressed factors that affect the implementation of these technologies?” In our analysis, we looked for evidence that researchers considered the implementation factor categories described above in their studies.
Methods
Study design
We conducted a scoping review of the peer-reviewed literature with an unlimited publishing time limit. As described by Arksey and O’Malley (Arksey and O’Malley, 2005) and Levac et al. (Levac et al., 2010), the use of scoping reviews was determined to be the most appropriate approach to collate a wide range of evidence and identify research gaps in the literature. The findings can be used for mapping a complex area of investigation and informing future research. The population of interest is older adults living with chronic health conditions and disabilities. In this review, we did not restrict the range of digital health technologies and settings for their application, as we were interested to learn if studies addressed factors for digital health technology implementation, whether an older adult was living at home in the community or in long-term care or similar facility. The potential range of devices includes ambient assisted living (AAL) systems, wearable sensors, smart everyday objects, environmental sensors, and social assistive robots that are intended to be used by older adults, their caregivers, and healthcare providers (Cicirelli et al., 2021).
The research question was composed based on a lack of consensus in the research literature on the most appropriate set of indicators for the successful implementation of digital health systems in all settings that matter. It should be noted that we did not evaluate methodological quality of included studies, in accordance with the convention for scoping reviews. A detailed search strategy for peer-reviewed literature was developed prior to conducting any searches. The review protocol was designed and conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) (RRID:SCR_018721) guidelines and was registered with Open Science Framework (RRID:SCR_003238) to increase research transparency and prevent any duplication efforts as per best practice guidelines.
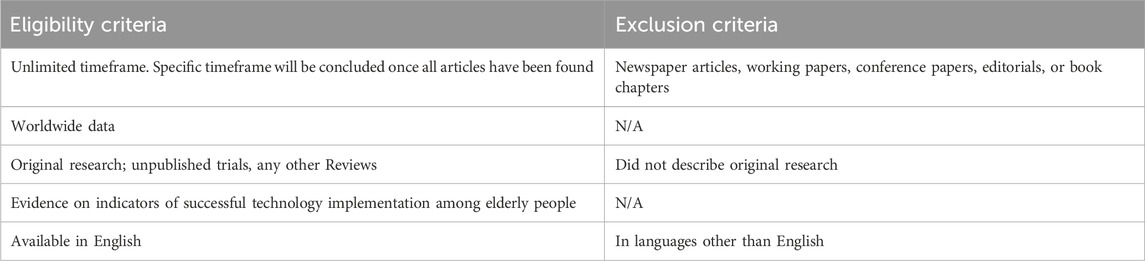
Eligibility criteria
We considered all peer-reviewed journal articles related to technologies for assisted living for older adults (aged 60+ years) and published in English. This age group was selected as the definition of ‘older adults’ because in most contemporary Western countries, 60 or 65 is the age of eligibility for retirement and old-age social programs (OECD, 2021). We did not consider any grey literature reports. A complete list of the eligibility criteria is shown in Table 1. To be included in this review, the authors of the original papers did not have to explicitly name “implementation” as an outcome or objective of the study. The reviewers included all studies that reported outcome measures relevant to the effectiveness, feasibility, and implementation of digital technologies as noted in the introduction to this article.
Search strategy
The technical information about the search strategy is presented in Appendix. A systematic search of the following five academic databases was conducted to identify relevant peer-reviewed results: Ovid MEDLINE/PubMed, Scopus, Ovid Embase, Ovid PsycINFO and Ovid Cochrane Library (Cochrane Central Register of Trials). The search strings used for the academic databases (available on request from the authors) were developed with guidance from a university librarian with expertise in the health sciences. This search of electronic databases was conducted using only English search terms. All results retrieved by the search were imported into Covidence (RRID:SCR_016484; Veritas Health Innovation, Melbourne, AU, 2020) a web-based software for systematic reviews, and duplicates were automatically removed.
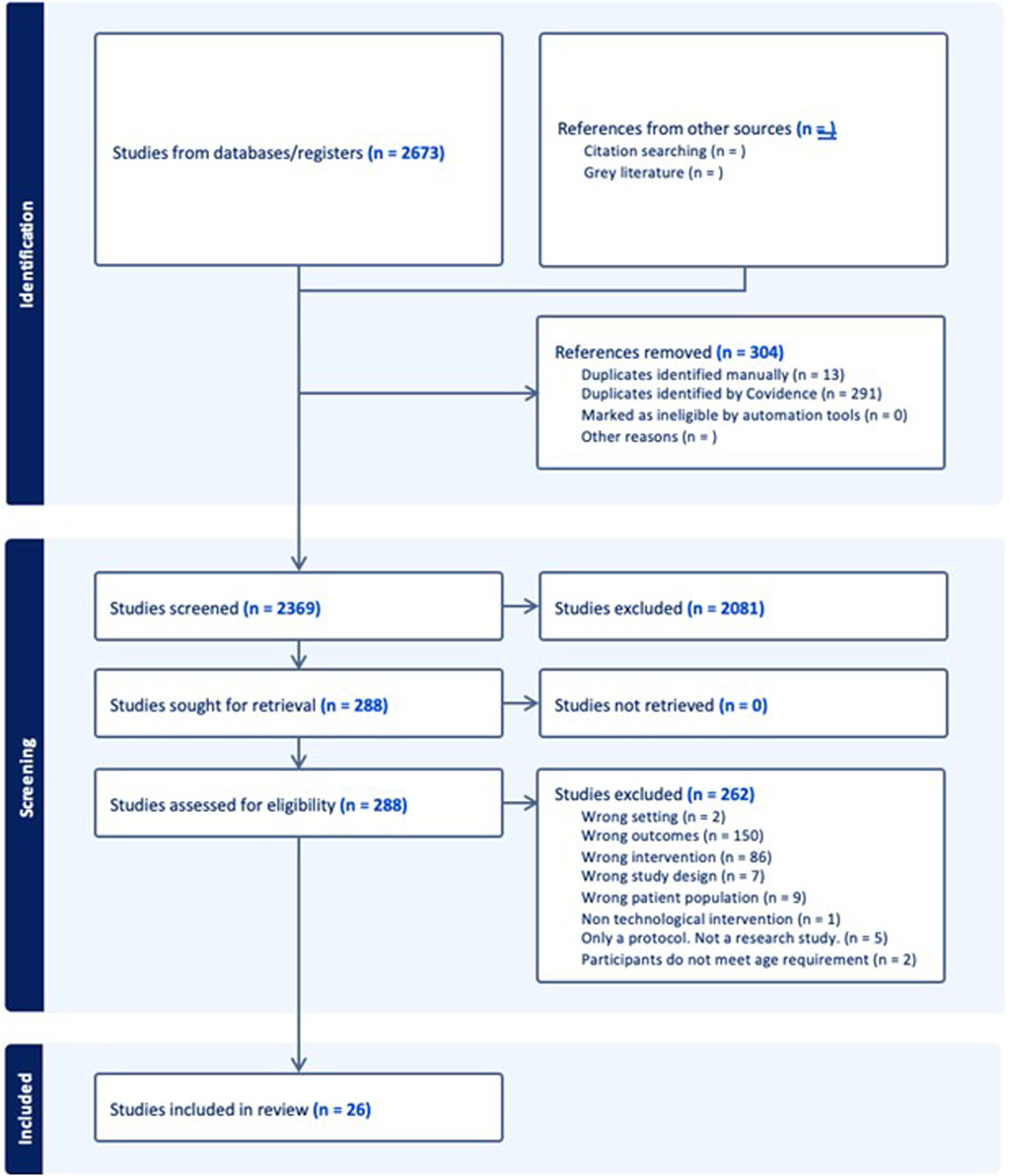
Selection of articles for review
Two reviewers (FH and DB) screened all peer-reviewed results using Covidence. The screening of search results from the electronic academic databases occurred in two phases. First, two reviewers (FH and DW) independently screened the title and abstract of each article using the predefined eligibility criteria; any disagreements were resolved via consensus. Next, both reviewers screened the full texts of potential articles for eligibility by both reviewers. Disagreements were also resolved by discussion and/or consultation with a third reviewer (JJ) when necessary. All articles that remained after full text screening were included in the study. Figure 2 summarizes study selection process for peer-reviewed and grey literature, based on the PRISMA-ScR reporting guidelines.
A total of 150 studies were dropped at the full-text screening phase as “wrong outcomes” and 86 as “wrong intervention”. Our selection criteria did not exclude outcome measures and digital health technology interventions based upon lists of examples because we did not want to risk overlooking any promising studies. Studies that were screened out for the reasons listed above included those that described outcome measures and interventions that were irrelevant for implementation, such as bio-signal characteristics and electronic medical records, respectively.
Data extraction and charting
Following the screening of results, three reviewers (FH, DB, MH) extracted from each article. The extracted data included author and publication year, publication type, data collection period, population and key results related to the research question. Four reviewers (FH, DB, MH, JJ) completed validation of the extracted data. We subsequently grouped the results by outcome measure and relevancy.
Data analysis
As scoping reviews typically do not include an assessment of methodological limitations or the potential for evidence bias (Munn et al., 2018), we elected to focus our analysis on the implications for future research design, rather than the practical applications of our findings.
Results
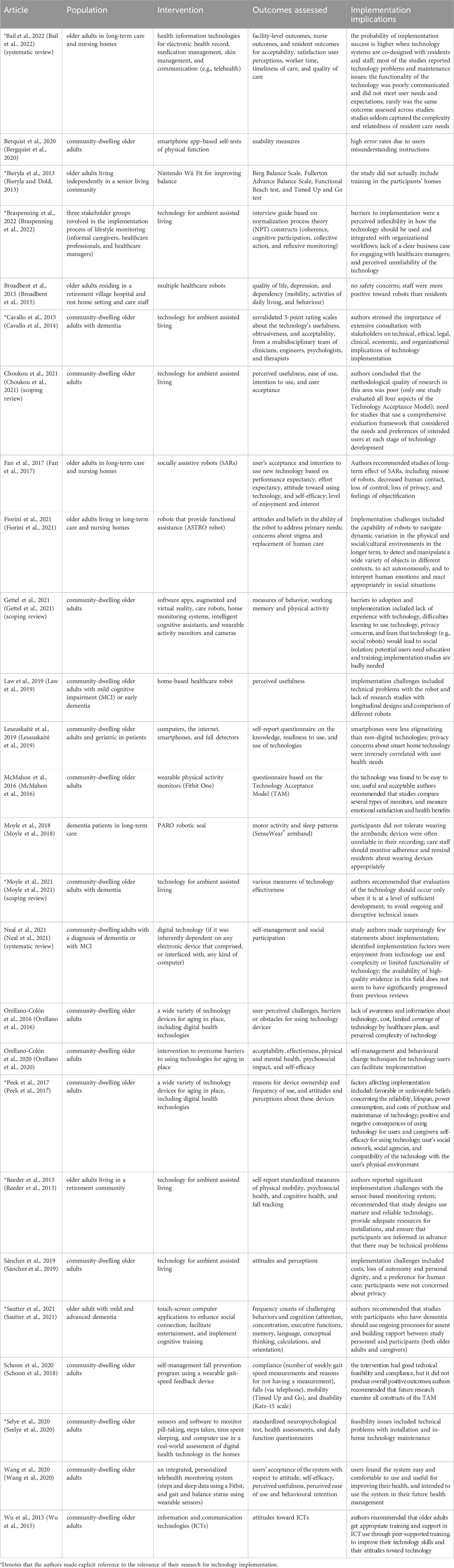
Table 2 presents essential information from the 26 selected articles, which includes the study population, nature of the technology intervention, the outcomes that were assessed, and implications of the study findings for technology implementation. Five of the articles were reviews (scoping or systematic). The populations researched in these articles were overwhelmingly community-dwelling older adults (n = 17), but also long-term care and nursing homes (n = 4), retirement community or village (n = 3), setting not specified (n = 1), and implementation stakeholders (n = 1). The categories of interventions were information and communication technologies (n = 7), wearable sensors (n = 2), ambient assisted living technologies (n = 6), assistive robots (n = 5), interventions to overcome barriers to using technologies for aging in place (n = 1). Some articles discussed several different categories (n = 5). The domains in which outcomes were assessed spanned a wide range at the levels of users (or residents), healthcare providers, and healthcare facilities. Most of the studies used measures of user acceptance and intention to use technology (derived from the Technology Acceptance Model and its variants) (n = 9). Note that only nine of these studies explicitly discussed the relevance of the findings for implementation.
From the list of implementation issues identified in the selected studies, we detected the following themes:
1. Communication (technology utilization and functionality poorly communicated to users).
2. Context sensitivity (e.g., need to train users in their homes; need to investigate workflow compatibility).
3. Design (importance of co-design with users and caregivers).
4. Economic analysis (e.g., cost-benefit analysis).
5. Ethical considerations (e.g., need for ongoing processes for assent for users with dementia).
6. Outcome assessment (inconsistent across studies; not comprehensive with respect to user and caregiver needs, emotional satisfaction, and health benefits).
7. Quality of research (weak evidence basis; poor methodology; lack of theoretical grounding; lack of cross-product comparisons; lack of longitudinal studies to analyze dynamic variations in physical, social, and cultural environments).
8. Technology maturity and readiness (unreliability; malfunction and maintenance concerns).
9. Unmet user needs and expectations.
10. User education and training (e.g., peer-supported training).
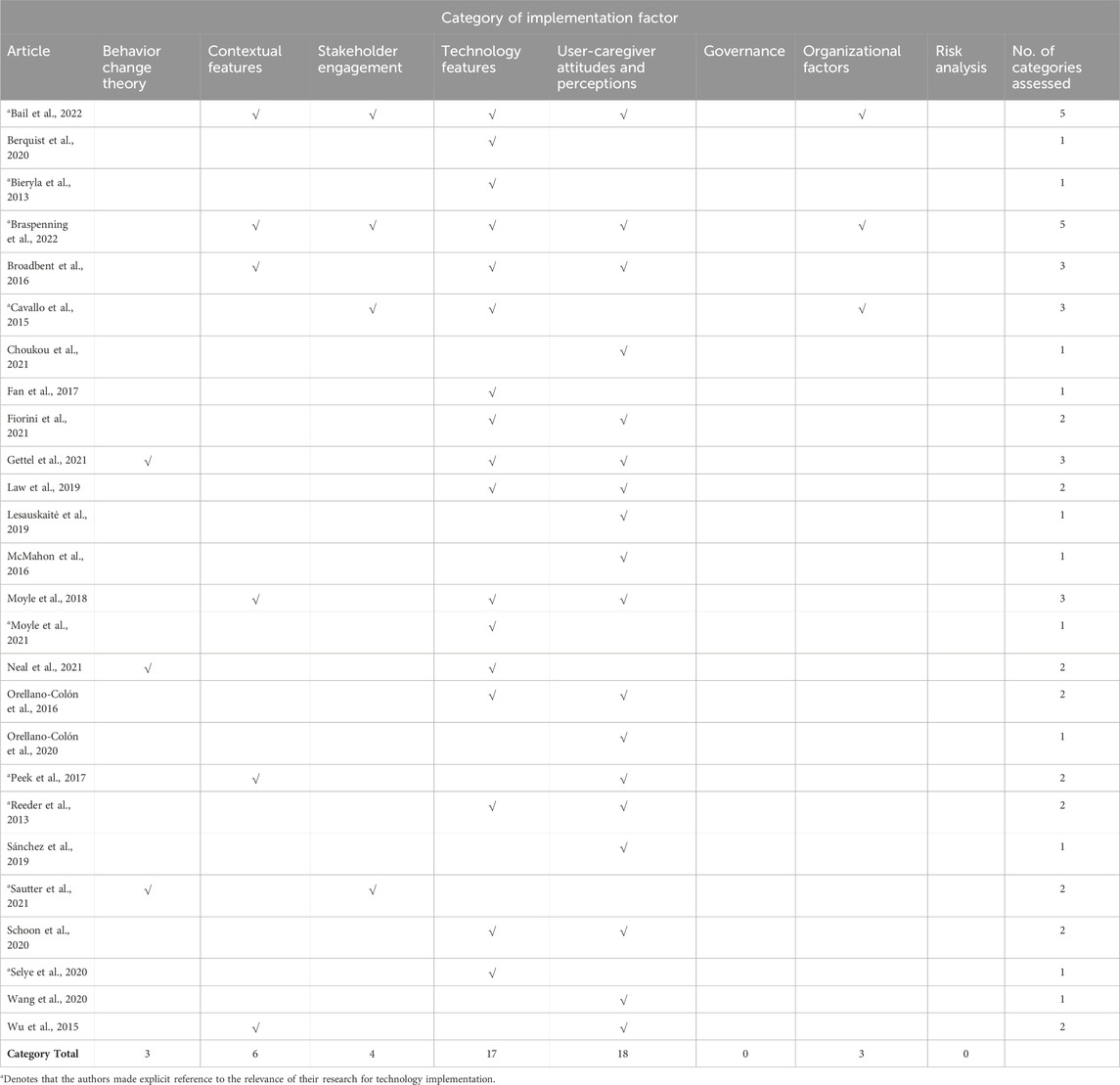
Table 3 presents an analysis of whether the selected articles referred to implementation factors presented in Figure 1. Those marked with an asterisk (*) made explicit reference to the relevance of their research for technology implementation. Most of the articles reviewed made only indirect references to implementation. The overwhelming focus of studies has been on implementation issues related to features of the technology under investigation and the attitudes and perceptions of technology users and caregivers. As previously noted the methodological rigour of these studies was weak. Very few studies used a theory-driven approach and validated methods for assessing attitudes and perceptions. We were unable to find any studies of the impact of governance and risk analysis on the implementation of digital health technologies for older adults.
Discussion
We found that understandings about factors affecting implementation across research studies of digital health technologies for older adults varied significantly and was reflected by a wide variety of methods for technology evaluation and uneven quality of research. Most of the research studies were either focused on the smart home technology development phase or were laboratory-based evaluation studies that narrowly defined implementation in terms of technical feasibility, clinical effectiveness, and user acceptance. None of these articles examined the full range of implementation factors depicted in Figure 1 for either community-dwelling older adults or those residing in long-term care facilities.
Areas where high-quality research is particularly needed include managing risks of discontinuous, potentially disruptive innovations by health and social services (Brown and Osborne, 2013), developing culturally and linguistically appropriate technology-delivered interventions for ethnic minority older adults (Chung et al., 2016), evaluating the impacts of technology implementation on service delivery (Cucciniello and Nasi, 2013), and adoption and long-term use of technologies for health self-management (Courtney, 2008; Lee and Coughlin, 2015). In each setting in which digital health technologies may be deployed, we need to understand how they should be developed alongside the networked social relations that make them ‘work’ and pragmatically customized to meet older adults’ unique and changing medical, personal, social, and cultural needs” (Greenhalgh et al., 2015; Sánchez et al., 2015; Jutai et al., 2022).
It is unreasonable to expect that a single research study should investigate in all eight of the categories of implementation factors that we identified. We argue, though, that the quality of research in this area would be markedly improved if researchers would subscribe to a more comprehensive program logic for their studies. For example, investigations of the technical feasibility, clinical effectiveness, or user acceptance of a new technology should show how they have anticipated the most pressing concerns that might arise from the domains of behavior change, governance, organizational factors, risk analysis, and stakeholder engagement. Adherence to an accepted conceptual framework should improve the likelihood of successful technology implementation. Several published frameworks, such as NASSS (Greenhalgh and Abimbola, 2019), CeHREs (van et al., 2011), and SCIROCCO (Grooten et al., 2020) offer excellent, detailed guidance, and we encourage researchers to consider them. We recommend their use because they can inform the design of a new technology, identify technological solutions that have a limited chance of achieving large-scale, sustained adoption, help to plan the implementation of technology, and help explain and learn from implementation failures (Greenhalgh et al., 2017). These frameworks are underutilized at present, due in part to their recent development, but probably also due to a need for them to be adequately contextualized for individual technologies (Abell et al., 2023).
Limitations
Our study did not include stakeholder consultation on the scoping review but we plan to conduct stakeholder evaluations of the provisional framework, to identify opportunities for its application across the broadest possible range of digital health technologies for older adults.
Future directions
Our findings reinforce the view that implementation is often planned and executed only after the design of a technology has been completed. Future studies of technology development should include consideration of the eight categories of factors that can affect implementation. They should acknowledge the implications of the technology not only for individual users, but the healthcare system and society at large (van Gemert-Pijnen, 2022). We recognize that it is challenging for a single study to address all these factors, but if indeed the goal for the research is to achieve successful implementation of the technology, then researchers should be expected at least to demonstrate their awareness of the issues.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
JJ: Conceptualization, Funding acquisition, Project administration, Writing–original draft, Writing–review and editing. FH: Data curation, Methodology, Software, Writing–review and editing. DB: Data curation, Formal Analysis, Methodology, Writing–review and editing. MH: Data curation, Formal Analysis, Methodology, Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Mitacs Accelerate funding program (Award # IT27530) as part of the project, Developing and Implementing Governance and Algorithms for the PATH (Program to Accelerate Technologies for Homecare) Platform of the AGE-WELL Network.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fragi.2024.1349520/full#supplementary-material
References
Abell, B., Naicker, S., Rodwell, D., Donovan, T., Tariq, A., Baysari, M., et al. (2023). Identifying barriers and facilitators to successful implementation of computerized clinical decision support systems in hospitals: a NASSS framework-informed scoping review. Implement. Sci. 18, 32. doi:10.1186/s13012-023-01287-y
Arksey, H., and O’Malley, L. (2005). Scoping studies: towards a methodological framework. Int. J. Soc. Res. Methodol. 8 (1), 19–32. doi:10.1080/1364557032000119616
Bail, K., Gibson, D., Acharya, P., Blackburn, J., Kaak, V., Kozlovskaia, M., et al. (2022). Using health information technology in residential aged care homes: an integrative review to identify service and quality outcomes. Int. J. Med. Inf. 165, 104824. doi:10.1016/j.ijmedinf.2022.104824
Bergquist, R., Vereijken, B., Mellone, S., Corzani, M., Helbostad, J. L., and Taraldsen, K. (2020). App-based self-administrable clinical tests of physical function: development and usability study. JMIR mHealth uHealth 8 (4), e16507. doi:10.2196/16507
Bieryla, K., and Dold, N. (2013). Feasibility of Wii Fit training to improve clinical measures of balance in older adults. Clin. Interventions Aging 775, 775. doi:10.2147/cia.s46164
Braspenning, A. M., Cranen, K., Snaphaan, LJAE, and Wouters, E. J. M. (2022). A multiple stakeholder perspective on the drivers and barriers for the implementation of lifestyle monitoring using infrared sensors to record movements for vulnerable older adults living alone at home: a qualitative study. Int. J. Environ. Res. Public Health 19 (1), 570. doi:10.3390/ijerph19010570
Broadbent, E., Kerse, N., Peri, K., Robinson, H., Jayawardena, C., Kuo, T., et al. (2015). Benefits and problems of health-care robots in aged care settings: a comparison trial. Australas. J. Ageing 35 (1), 23–29. doi:10.1111/ajag.12190
Brown, L., and Osborne, S. P. (2013). Risk and innovation. Public Manag. Rev. 15 (2), 186–208. doi:10.1080/14719037.2012.707681
Cavallo, F., Aquilano, M., and Arvati, M. (2014). An ambient assisted living approach in designing domiciliary services combined with innovative technologies for patients with Alzheimer's disease: a case study. Am. J. Alzheimer’s Dis. Other Dementiasr 30 (1), 69–77. doi:10.1177/1533317514539724
Choukou, M. A., Shortly, T., Leclerc, N., Freier, D., Lessard, G., Demers, L., et al. (2021). Evaluating the acceptance of ambient assisted living technology (AALT) in rehabilitation: a scoping review. Int. J. Med. Inf. 150, 104461. doi:10.1016/j.ijmedinf.2021.104461
Chung, J., Demiris, G., Thompson, H. J., Chen, K., Burr, R., Patel, S., et al. (2016). Feasibility testing of a home-based sensor system to monitor mobility and daily activities in Korean American older adults. Int. J. Older People Nurs. 12 (1). doi:10.1111/opn.12127
Cicirelli, G., Marani, R., Petitti, A., Milella, A., and D’Orazio, T. (2021). Ambient assisted living: a review of technologies, methodologies and future perspectives for healthy aging of population. Sensors 21 (10), 3549. doi:10.3390/s21103549
Courtney, K. L. (2008). Privacy and senior willingness to adopt smart home information technology in residential care facilities. Methods Inf. Med. 47 (01), 76–81. doi:10.3414/me9104
Cucciniello, M., and Nasi, G. (2013). Evaluation of the impacts of innovation in the health care sector: a comparative analysis. Public Manag. Rev. 16 (1), 90–116. doi:10.1080/14719037.2013.798026
Fan, J., Bian, D., Zheng, Z., Beuscher, L., Newhouse, P., Mion, L. C., et al. (2017). A robotic coach architecture for elder care (ROCARE) based on multi-user engagement models. IEEE Trans. Neural Syst. Rehabil. Eng. 25 (8), 1153–1163. doi:10.1109/TNSRE.2016.2608791
Fiorini, L., De Mul, M., Fabbricotti, I., Limosani, R., Vitanza, A., D’Onofrio, G., et al. (2021). Assistive robots to improve the independent living of older persons: results from a needs study. Disability and Rehabilitation. Assist. Technol. 16 (1), 1–11. doi:10.1080/17483107.2019.1642392
Gettel, C. J., Chen, K., and Goldberg, E. M. (2021). Dementia care, fall detection, and ambient-assisted living technologies help older adults age in place: a scoping review. J. Appl. Gerontology 14, 073346482110058. doi:10.1177/07334648211005868
Goggin, M. L. (1986). The “too few cases/too many variables” problem in implementation research. Political Res. Q. 39 (2), 328–347. doi:10.2307/448302
Greenhalgh, T., and Abimbola, S. (2019). The NASSS framework - a synthesis of multiple theories of technology implementation. Stud. health Technol. Inf. 263, 193–204. doi:10.3233/SHTI190123
Greenhalgh, T., Procter, R., Wherton, J., Sugarhood, P., Hinder, S., and Rouncefield, M. (2015). What is quality in assisted living technology? The ARCHIE framework for effective telehealth and telecare services. BMC Med. 13 (1), 91. doi:10.1186/s12916-015-0279-6
Greenhalgh, T., Wherton, J., Papoutsi, C., Lynch, J., Hughes, G., A'Court, C., et al. (2017). Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the scale-up, spread, and sustainability of health and care technologies. J. Med. Internet Res. 19 (11), e367. doi:10.2196/jmir.8775
Grooten, L., Vrijhoef, H. J. M., Alhambra-Borrás, T., Whitehouse, D., and Devroey, D. (2020). The transfer of knowledge on integrated care among five European regions: a qualitative multi-method study. BMC health Serv. Res. 20 (1), 11. doi:10.1186/s12913-019-4865-8
Jutai, J. W. (2022). “Technology and connected autonomy,” in Well-being in later life: the notion of connected autonomy. Editors L. J. Garcia, L. Bélanger-Hardy, J. W. Jutai, and M. Łuszczyńska (London: Routledge eBooks), 99–107.
Keyworth, C., Hart, J., Armitage, C. J., and Tully, M. P. (2018). What maximizes the effectiveness and implementation of technology-based interventions to support healthcare professional practice? A systematic literature review. BMC Med. Inf. Decis. Mak. 18 (1), 93. doi:10.1186/s12911-018-0661-3
Kyratsis, Y., Ahmad, R., and Holmes, A. (2012). Technology adoption and implementation in organisations: comparative case studies of 12 English NHS Trusts. BMJ Open 2 (2), e000872. doi:10.1136/bmjopen-2012-000872
Law, M., Sutherland, C., Ahn, H. S., MacDonald, B. A., Peri, K., Johanson, D. L., et al. (2019). Developing assistive robots for people with mild cognitive impairment and mild dementia: a qualitative study with older adults and experts in aged care. BMJ Open 9 (9), e031937. doi:10.1136/bmjopen-2019-031937
Lee, C., and Coughlin, J. F. (2015). PERSPECTIVE: older adults' adoption of technology: an integrated approach to identifying determinants and barriers. J. Prod. Innovation Manag. 32 (5), 747–759. doi:10.1111/jpim.12176
Lesauskaitė, V., Damulevičienė, G., Knašienė, J., Kazanavičius, E., Liutkevičius, A., and Janavičiūtė, A. (2019). Older adults-potential users of technologies. Med. Kaunas. Lith. 55 (6), 253. doi:10.3390/medicina55060253
Levac, D., Colquhoun, H., and O’Brien, K. K. (2010). Scoping studies: advancing the methodology. Implement. Sci. 5 (1), 69–9. doi:10.1186/1748-5908-5-69
Linskell, J., and Dewsbury, G. (2019). “Assisted living,” in Handbook of electronic assistive technology. Editors D. Cowan,, and L. Najafi (Amsterdam: Elsevier), 215–258.
Matthew-Maich, N., Harris, L., Ploeg, J., Markle-Reid, M., Valaitis, R., Ibrahim, S., et al. (2016). Designing, implementing, and evaluating mobile health technologies for managing chronic conditions in older adults: a scoping review. JMIR mHealth uHealth 4 (2), e29. doi:10.2196/mhealth.5127
McMahon, S. K., Lewis, B., Oakes, M., Guan, W., Wyman, J. F., and Rothman, A. J. (2016). Older adults’ experiences using a commercially available monitor to self-track their physical activity. JMIR mHealth uHealth 4 (2), e35. doi:10.2196/mhealth.5120
Moyle, W., Jones, C., Murfield, J., Thalib, L., Beattie, E., Shum, D., et al. (2018). Effect of a robotic seal on the motor activity and sleep patterns of older people with dementia, as measured by wearable technology: a cluster-randomised controlled trial. Maturitas 110, 10–17. doi:10.1016/j.maturitas.2018.01.007
Moyle, W., Murfield, J., and Lion, K. (2021). The effectiveness of smart home technologies to support the health outcomes of community-dwelling older adults living with dementia: a scoping review. Int. J. Med. Inf. 153, 104513. doi:10.1016/j.ijmedinf.2021.104513
Munn, Z., Peters, M. D. J., Stern, C., Tufanaru, C., McArthur, A., and Aromataris, E. (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 18 (1), 143. doi:10.1186/s12874-018-0611-x
Neal, D., van den Berg, F., Planting, C., Ettema, T., Dijkstra, K., Finnema, E., et al. (2021). Can use of digital technologies by people with dementia improve self-management and social participation? A systematic review of effect studies. J. Clin. Med. 10 (4), 604. doi:10.3390/jcm10040604
OECD (2021). Pensions at a glance 2021: OECD and G20 indicators. Paris: OECD. doi:10.1787/ca401ebd-en
Orellano-Colón, E. M., Harrison-Cruz, S., López-Lugo, E., Ramos-Peraza, S., Meléndez-Ortiz, A., Ortiz-Torres, J., et al. (2020). Assistive technology self-management intervention for older Hispanics: a feasibility study. Disabil. Rehabilitation Assistive Technol. 15 (8), 862–870. doi:10.1080/17483107.2019.1621954
Orellano-Colón, E. M., Mann, W. C., Rivero, M., Torres, M., Jutai, J., Santiago, A., et al. (2016). Hispanic older adult’s perceptions of personal, contextual and technology-related barriers for using assistive technology devices. J. Racial Ethn. Health Disparities 3 (4), 676–686. doi:10.1007/s40615-015-0186-8
Peek, S. T. M., Luijkx, K. G., Vrijhoef, H. J. M., Nieboer, M. E., Aarts, S., van der Voort, C. S., et al. (2017). Origins and consequences of technology acquirement by independent-living seniors: towards an integrative model. BMC Geriatr. 17 (1), 189. doi:10.1186/s12877-017-0582-5
Rajer, C., and Bogataj, D. (2022). Digital transformation of home care: literature review and research agenda. IFAC-PapersOnLine 55 (39), 229–234. doi:10.1016/j.ifacol.2022.12.070
Reeder, B., Chung, J., Lazar, A., Joe, J., Demiris, G., and Thompson, H. J. (2013). Testing a theory-based mobility monitoring protocol using in-home sensors: a feasibility study. Res. Gerontological Nurs. 6 (4), 253–263. doi:10.3928/19404921-20130729-02
Rogers, W. A., and Mitzner, T. L. (2017). Envisioning the future for older adults: autonomy, health, well-being, and social connectedness with technology support. Futures 87, 133–139. doi:10.1016/j.futures.2016.07.002
Sánchez, V. G., Anker-Hansen, C., Taylor, I., and Eilertsen, G. (2019). Older people’s attitudes and perspectives of welfare technology in Norway. J. Multidiscip. Healthc. 12, 841–853. doi:10.2147/JMDH.S219458
Sánchez Criado, T., and Domènech, M. (2015). Older people in a connected autonomy? Promises and challenges in the technologisation of care. Rev. Esp. Investig. Sociol. 152, 105–120.
Sautter, S. W., Ord, A. S., Azher, A., Chidester, A., and Aravich, P. F. (2021). Benefits of computer engagement in older adults with dementia. Gerontology Geriatric Med. 7, 2333721421992996. doi:10.1177/2333721421992996
Schoon, Y., Bongers, K. T. J., and Olde Rikkert, M. G. M. (2018). Feasibility study by a single-blind randomized controlled trial of self-management of mobility with a gait-speed feedback device by older persons at risk for falling. Assist. Technol. 32 (4), 222–228. doi:10.1080/10400435.2018.1529004
Seelye, A., Leese, M. I., Dorociak, K., Bouranis, N., Mattek, N., Sharma, N., et al. (2020). Feasibility of in-home sensor monitoring to detect mild cognitive impairment in aging military veterans: prospective observational study. JMIR Form. Res. 4 (6), e16371. doi:10.2196/16371
van Gemert-Pijnen, J. L. (2022). Implementation of health technology: directions for research and practice. Front. Digital Health 4, 1030194. doi:10.3389/fdgth.2022.1030194
van Gemert-Pijnen, J. E., Nijland, N., van Limburg, M., Ossebaard, H. C., Kelders, S. M., Eysenbach, G., et al. (2011). A holistic framework to improve the uptake and impact of eHealth technologies. J. Med. Internet Res. 13 (4), e111. doi:10.2196/jmir.1672
Wang, H., Zhao, Y., Yu, L., Liu, J., Zwetsloot, I. M., Cabrera, J., et al. (2020). A personalized health monitoring system for community-dwelling elderly people in Hong Kong: design, implementation, and evaluation study. J. Med. Internet Res. 22 (9), e19223. doi:10.2196/19223
Keywords: ambient assisted living, aging, digital health, gerontechnology, technology implementation, scoping review
Citation: Jutai JW, Hatoum F, Bhardwaj D and Hosseini M (2024) Implementation of digital health technologies for older adults: a scoping review. Front. Aging 5:1349520. doi: 10.3389/fragi.2024.1349520
Received: 08 December 2023; Accepted: 17 April 2024;
Published: 07 May 2024.
Edited by:
Alexander Moreno, University of Montreal, CanadaCopyright © 2024 Jutai, Hatoum, Bhardwaj and Hosseini. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jeffrey W. Jutai, amp1dGFpQHVvdHRhd2EuY2E=
 Jeffrey W. Jutai
Jeffrey W. Jutai Farah Hatoum2
Farah Hatoum2 Devvrat Bhardwaj
Devvrat Bhardwaj