- 1Rehabilitation Services, Yishun Community Hospital, Singapore, Singapore
- 2Health and Social Sciences Cluster, Singapore Institute of Technology, Singapore, Singapore
- 3Public Health and Sport Sciences, University of Exeter, Exeter, United Kingdom
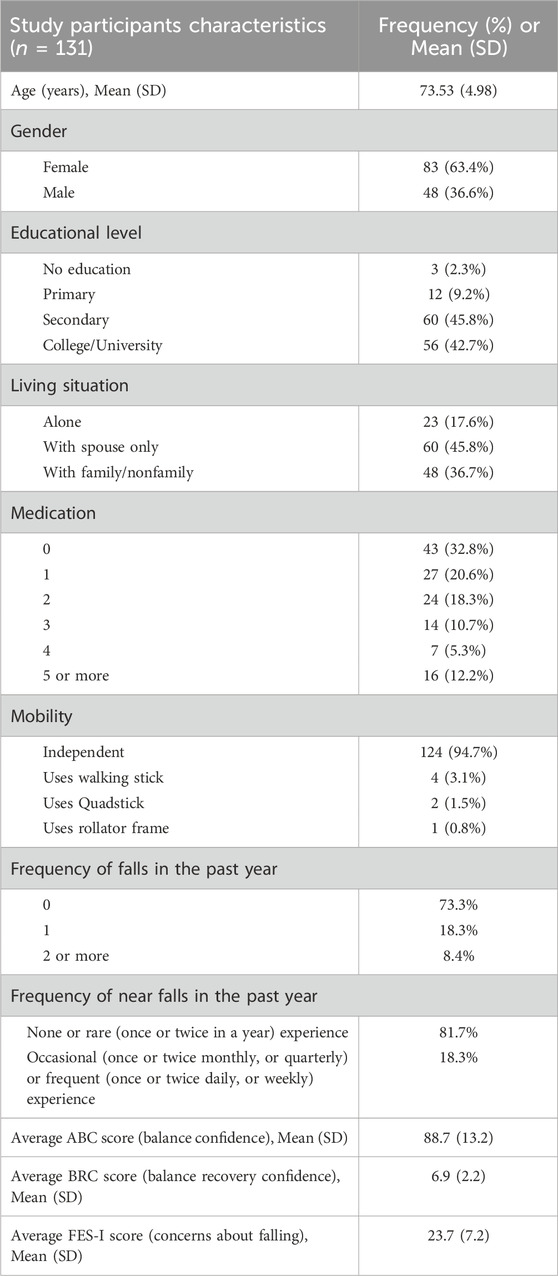
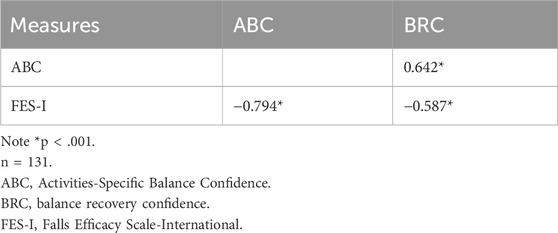
The purpose of this study was to determine the convergent validity between the Activities-specific Balance Confidence (ABC) Scale, Balance Recovery Confidence (BRC) Scale and Falls Efficacy Scale-International (FES-I), which are assessment tools used to measure the constructs of falls efficacy and concerns about falling. The study also investigated the predictive validity of ABC and BRC on concerns about falling. One hundred and thirty-one older adults (mean age of 73.5 years, SD 4.98) completed the three scales and self-reported their demographic data. 63.4% were female. The convergent validity between the ABC, BRC, and FES-I scales was investigated using Pearson correlation coefficients. Predictive validity was investigated using regression models. Findings indicated strong correlation between ABC and FES-I (r = −0.794, p < 0.001), and moderate correlation between BRC and FES-I (r = −0.587, p < 0.001) and ABC and BRC (r = 0.642, p < 0.001). ABC (R2 = 0.6279) was found to be a stronger predictor of FES-I than BRC (R2 = 0.3398). In conclusion, assessment tools for balance confidence, balance recovery confidence, and concerns about falling should be appropriately selected when studying the various constructs of interest, instead of using them interchangeably. Concerns about falling can also be further understood by exploring balance confidence and balance recovery confidence.
Introduction
Falls has been identified as a major health issue among older adults and is ranked as the second most common reason for unintentional injury deaths worldwide (World Helath Organization, 2021). In addition to physical and social consequences, falls also result in psychological consequences such as reduction in activity due to decreased confidence in mobility, leading to physiological and functional declines (Moore and Ellis, 2008). The 2022 World Guidelines for Falls Prevention and Management for Older Adults has recommended a holistic approach to the assessment of older adults, by including concerns about falling on top of balance and gait assessment (Montero-Odasso et al., 2022). In the literature of falls prevention practice, falls efficacy and fear of falling are key psychological factors that have been given much attention. Distinguishing falls efficacy and fear of falling is important because these two concepts are distinct even though they are closely related. Falls efficacy, rooted in Bandura’s self-efficacy theory, is a cognitive element referring to the perceived ability to prevent and manage falls (Soh, 2022a). Falls efficacy has been posited as a multidimensional construct encompassing four domains: balance confidence, balance recovery confidence, safe-landing confidence, and post fall recovery confidence (Soh, 2022a). Previously, falls efficacy has been considered to be synonymous to balance confidence (Hadjistavropoulos et al., 2011). Since then, the focus has largely been on balance confidence when targeting falls efficacy both in research and in practice (Soh et al., 2022a). However, a broader concept of falls efficacy allows different self-efficacies to be reflected and attended to when older adults need to develop their agencies to deal with falls (Soh et al., 2021a). The knowledge about the relationships between the different falls-related self-efficacies, for example, how closely balance recovery confidence is related to balance confidence, is currently limited. There is a need for a greater understanding of balance recovery confidence to advance fall prevention and management practice.
Falls efficacy has often been conflated with fear of falling (Soh, 2022a). The construct of fear of falling is generally considered to represent an emotional state that can have clear impacts on behaviour (e.g., activity avoidance) (Hughes et al., 2015). Fear of falling has been postulated to serve either as a protective or maladaptive mechanism for older adults to guard against falls (Ellmers et al., 2022). Rather than “fear of falling”, some researchers and the recent World Falls Guidelines have proposed that the term “concerns about falling” should be used instead (Ellmers et al., 2023). Concerns appear to be a less intense emotion than fear, as fear could imply analogy to phobias (Tinetti et al., 1990). Thus, older adults may find concerns about falling more relatable, more accurate in describing what they experience, and more socially acceptable to reveal (Yardley et al., 2005). Concerns about falling is prevalent in both older adults who have fallen before and those who have not yet fallen (Hadjistavropoulos et al., 2011). Having high concerns raises the risk of frailty (de Souza et al., 2022), decreased activity participation (Greenberg et al., 2016), and poorer quality of life (Schoene et al., 2019). Given the complexity of understanding the different concepts, there is a need for more evidence surrounding various falls efficacy and concerns about falling assessment tools for one to consider in their decision-making process when selecting the most appropriate tool for use (Hughes et al., 2015).
Several assessment tools, such as the Activities-specific Balance Confidence (ABC) Scale, Balance Recovery Confidence (BRC) Scale, and Falls Efficacy Scale-International (FES-I) have been developed to measure falls efficacy or concerns about falling. The 16-item ABC was constructed to assess how confident individuals were to perform various activities without losing balance or experiencing a sense of unsteadiness (Powell and Myers, 1995). Since its development in 1995, several studies have demonstrated good psychometric properties of the ABC to determine balance confidence in older adults (Soh et al., 2021b) (Stasny et al., 2011). Another tool, the newly-developed 19-item BRC, was constructed to assess how confident individuals were able to arrest falls in response to different perturbations such as a slip, a trip or a loss of balance from volitional movement (Soh, 2022b). This balance recovery confidence measure was developed in 2022 after a systematic review of falls efficacy instruments identified an absence of a suitable instrument to measure balance recovery confidence (Soh et al., 2021b). The psychometric study of BRC scale has demonstrated excellent test-retest reliability when the assessment was administered to community-dwelling older adults during a 1-week time frame (ICC3,1 = 0.944, 95% CI of 0.891 and 0.969) and high internal consistency (α = 0.975) (Soh, 2022b). Finally, the 16-item FES-I, is a widely used tool to assess how concerned individuals were about falling when performing different activities of daily living (Yardley et al., 2005; McGarrigle et al., 2023). This measure of concerns about falling was developed in 2005 after a series of meetings between members of the Prevention of Falls Network Europe (ProFaNE) (Yardley et al., 2005). The FES-I and its translated versions have been validated by numerous international studies to have excellent psychometric properties (Healthy Ageing Research Group).
There have been limited studies investigating the construct validity between ABC, BRC, and the FES-I scale and the predictive validity of the BRC scale on concerns about falling as the BRC scale has been recently developed. Previous studies had reported moderate-strong convergent validity between ABC and FES-I in various populations such as Iranian older adults (r = −0.48) (Taheri-Kharameh et al., 2022), Portuguese older adults (r = −0.85) (Figueiredo and Santos, 2017), Japanese post-stroke individuals (r = −0.77) (Ishige et al., 2020), and persons with balance and vestibular dysfunction (r = −0.84) (Morgan et al., 2013). Further, there are no studies reporting the relationships of these measures in the Singapore community-dwelling older adult population, despite Singapore being the second fastest ageing country (Luk, 2023). In Singapore, one in three community-dwelling older adults aged 65 years and above will have at least one fall (World Health Organization, 2007), and the ratio increases to one in two for adults aged 80 years and above (Stalenhoef et al., 1997). Falls is a leading cause of injury among older adults in Singapore, accounting for 85% of elderly patients with trauma seen at hospitals’ emergency department (Matchar et al., 2017). More psychometric studies relating to the BRC scale are also needed to provide a greater level of confidence for its use. This study aims to determine the convergent validity of the ABC, BRC and FES-I to establish the relationship between these tools measuring similar constructs, and the predictive validity of ABC and BRC scales on concerns about falling in Singapore community-dwelling older adults.
Methods
Design and participants
A cross-sectional study with a convenience sample of community-dwelling older adults in Singapore was conducted between February 2021 and May 2023. Ethical approval was obtained from the Singapore Institute of Technology Institutional Review Board (Ref. 2020098). Participants were recruited from word-of-mouth recommendation and poster circulation through contact networks of the study team members. Participants were included if they were ≥65 years old and living independently in the community with or without the use of a walking aid. Participants were excluded if they required any physical assistance from another person to walk within home, presented with clinical observable severe cognitive impairment, and were unable to provide written consent to participate in the study.
Assessment tools
The Activities-Specific Balance Confidence (ABC) Scale (Powell and Myers, 1995): The ABC aims to assess individuals’ confidence in performing several progressively challenging balance and mobility tasks. Participants rated how confident he or she would be in maintaining balance if asked to perform a variety of activities, expressed as 0% = no confidence; 100% = total confidence. Confidence was ranked for 16 different activities such as getting into or out of a car, bending over to pick up a slipper, and walking in a crowded mall. The sum of the ratings (possible range = 0 to 1,600) was divided by 16 to get each participant’s ABC score. A higher score denoted a higher level of balance confidence.
The Balance Recovery Confidence (BRC) Scale (Soh et al., 2022b): The BRC aims to assess individuals’ confidence to recover balance across several progressively challenging near-fall scenarios depicting different perturbations, e.g., a slip, a trip, or from volitional movements. Participants rated how confident he or she would be to arrest a fall if faced with the different scenarios, expressed as 0 = cannot do at all; 10 = highly certain can do. Confidence was ranked for 19 different activities such as recover from a loss of balance while walking down a flight of steps without railings, recover from a trip while carrying groceries with both hands, and recover from a minor slip on a puddle of water. The sum of the ratings (possible range = 0–190) was divided by 19 to get each participant’s BRC score. A higher score denoted a higher level of balance recovery confidence.
The Falls Efficacy Scale-International (FES-I) (Yardley et al., 2005): The FES-I aims to assess individuals’ concerns about falling relating to basic and more demanding activities. Participants rated how concerned he or she would be if asked to perform a variety of activities, expressed as 1 = not at all concerned; 2 = somewhat concerned; 3 = fairly concerned; 4 = very concerned. The level of concern was ranked for 16 different activities such as cleaning the house, taking a bath or shower, going to the shop, and walking on an uneven surface. The sum of the ratings (possible range = 16–64) was obtained to get each participant’s FES-I score. A higher score denoted a higher level of concerns about falling.
A self-reported demographic characteristics form was used to record participant’s age, gender, level of education, living situation, number of medications consumed on a regular basis, functional mobility status, previous falls in the past year, and frequency of near falls in the past year.
Statistical analysis
Statistical analyses were conducted using R version 4.3.1 (Beagle Scouts) (R Core Team, 2023). Descriptive statistics were used to summarise the characteristics of the sample.
Convergent validity refers to correlations between two measures believed to be reflecting similar constructs (Portney and Watkins, 2015). Pearson correlation coefficients were calculated to determine the association between the ABC, BRC and FES-I. The hypotheses regarding correlations between the measures constructed were:
1. The correlation between the ABC and BRC was predicted to be moderate and positive (r = 0.3–0.59).
2. The correlation between the ABC and FES-I was predicted to be strong and negative (r ≥ 0.6).
3. The correlation between the BRC and FES-I was predicted to be moderate and negative (r = −0.3 to −0.59).
Linear regression analyses were conducted to further explore the relationships between ABC, BRC and FES-I. The scores of ABC and BRC were individually correlated to FES-I score to analyse if ABC and BRC were able to explain individuals with high concerns about falling reflected on their FES-I score. Multiple regression analysis was then conducted to explore how the combination of ABC and BRC scores could explain FES-I. In both analyses, ABC and BRC scores were modeled as continuous variables, while FES-I score was inserted as a continuous outcome. These analyses provided insight into how the ABC and BRC scores (the independent variables) could predict the dependent outcomes of “concerns about falling”.
Results
Descriptive statistics
One hundred and thirty-one older adults with a mean age of 73.5 years (SD 4.98) participated in the study (Table 1). Over half (63.4%) were female. Just under half were educated up to secondary school level. Most participants do not stay alone, and 17.5% reported taking 4 or more medications a day. Almost all the participants could walk independently without aid. In the past year, almost three-quarter of participants did not experience a fall, whereas slightly more than three-quarter do not or rarely experience near fall.
Convergent validity
The correlations between the different measures are reported in Table 2A strong negative correlation was found between the ABC and FES-I. (r = −0.794, p < 0.001), and a moderate negative correlation between the BRC and FES-I (r = −0.587, p < 0.001). Between ABC and BRC (r = 0.642, p < 0.001), there was a moderate positive correlation.
Predictive validity of ABC and BRC on FES-I
Linear regression analysis of ABC and BRC on FES-I showed that both ABC and BRC contribute to FES-I, as reported in Table 3. ABC (R2 = 0.6279) was a stronger predictor of FES-I than BRC (R2 = 0.3398). Combining ABC and BRC scores only marginally increased the R2 to 0.6353 (Table 4).
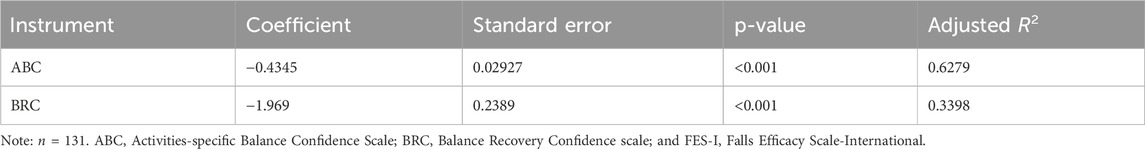
Table 3. Linear regression analysis including ABC and BRC scores with FES-I score as dependent variable.
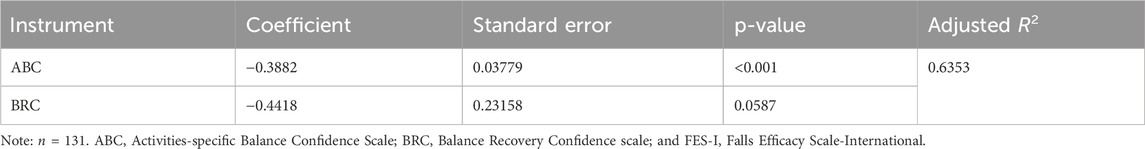
Table 4. Multiple regression analysis including a combination of ABC and BRC scores with FES-I score as dependent variable.
Discussion
The convergent and predictive validity of ABC, BRC, and FES-I have been evaluated in this study using a sample of high functioning older adults living independently in the community. Findings indicated that ABC and BRC as well as BRC and FES-I measured distinct constructs, even though the constructs may appear to be similar in nature and have often been used interchangeably. The correlations between ABC and FES-I demonstrated a higher level of congruency than between FES-I and BRC. Results also found that ABC and BRC were able to predict concerns about falling to varying degree. When compared against BRC, ABC was a stronger predictor of concerns about falling in individuals.
A mean ABC score of 88.7 in this population is generally higher than that of other populations in other studies. The mean ABC score of populations from previous studies was 86.9 in Taiwanese (Hwang et al., 2023), 85.74 in Portuguese (Figueiredo and Santos, 2017) and 70.1 in American (Cleary and Skornyakov, 2017) community dwelling older adults. The mean FES-I score of 23.7 in this study is comparable to a mean FES-I score of 23.5 in a Taiwanese study conducted in similar population (Kuo et al., 2021). However, it is generally lower than other population e.g., Turkish community-dwelling older adults (mean FES-I of 34.88) (Ulus et al., 2012) and Portuguese community-dwelling older adults (mean FES-I of 27.74) (Figueiredo and Santos, 2017). As BRC has not yet been used in other populations, no comparison of the population’s mean BRC score can be done. Future studies can look at investigating if these differences are due to cultural differences, or differences in characteristics within the population e.g., education and falls history.
This study has generated insights of the different constructs of ABC, BRC and FES-I by examining the relationship between these three scales. Previous systematic reviews on tools measuring fall-related psychological constructs have stressed that greater clarity in their psychometric properties is needed to help researchers and clinicians determine which tool is most suitable for measuring falls efficacy and concerns about falling as part of the holistic approach recommended by the World Guidelines (Montero-Odasso et al., 2022; Soh et al., 2022a; Jørstad et al., 2005). This study’s finding of ABC and FES-I demonstrating a high level of congruency was supported in previous studies conducted in community-dwelling older adults. Moore et al. (2004) as well as Figueiredo and Santos (2019) found ABC and FES-I to be highly correlated (r = −0.68 and r = −0.85 respectively) (Figueiredo and Santos, 2017; Moore et al., 2011). This suggested that the constructs measured in ABC and FES-I are more similar in nature compared to BRC. This may be because BRC relates to recovery from instability while ABC relates to maintenance of stability. While confidence of balance and balance recovery stems on the perceived ability surrounding balance control, the mechanisms to maintain balance and to recover balance when a loss of balance occur are different (Soh, 2022b). Change-in-support balance recovery strategies that involve rapid stepping and reaching movement are posited to be the only recourse in responding to large perturbations, even though they are also prevalent in relatively small perturbations (Maki et al., 2008). Given age-related physiological declines in these balance recovery strategies in older adults (Pijnappels et al., 2008; Pijnappels et al., 2010), it is imperative to account for their balance recovery confidence as many would underestimate or overestimate their risk of falling (Delbaere et al., 2010).
As falls efficacy and concerns about falling are similar in nature, researchers have been using falls efficacy and concerns about falling assessment tools interchangeably (Moore and Ellis, 2008). It is therefore important to reiterate that falls efficacy and concerns about fallings are distinct constructs (Soh et al., 2022a). Falls efficacy refers to the cognitive element and confidence in one’s perceived ability to perform activities without falling, whereas concerns about falling refer to an emotional state that results in activity avoidance (Moore and Ellis, 2008). While perceived abilities are likely to mediate concerns, other factors could also influence this relationship, e.g., the perceived safety of one’s environment and the vicarious experience of observing others suffering from falls-related injuries (Ellmers et al., 2022). For a case in point about balance recovery confidence, we postulate that near-falls experienced by individuals could potentially increase an older adult’s confidence in recovering their balance in response to different perturbations, such as trips or slips. Our previous studies have shown that near falls can be common among seniors, and compensatory stepping and reach-to-grasp strategies are frequently used to recover their balance (Soh et al., 2021c). Recognising that the perceived ability to recover from loss of balance is dissimilar to the perceived ability to perform activities steadily, researchers and clinicians should ensure using the most appropriate measurement instruments for the construct they want to study For example, balance confidence should be measured by a balance confidence-related scale, such as the ABC scale, and the BRC scale should be used to measure the balance recovery confidence for interventions, such as perturbation training.
Concerns about falling will be best measured by FES-I because of the strong evidence of its psychometric properties. However, clinicians will also need to work with their patients regarding potential factors such as balance or balance recovery confidence that could give rise to the concerns about falling. Without addressing the root causes, patients are likely to avoid or excessively limit the activities (Greenberg et al., 2016; Lach, 2002) as a strategy to overcome their concerns about falling. To measure balance confidence, ABC scale is of choice because of the strong evidence of its psychometric properties (Powell and Myers, 1995). BRC scale will be suitably used to measure balance recovery confidence as there are no other scales measuring this construct ((Soh et al., 2022b)). Based on the findings, ABC explained 62.8% of variance for concerns about falling, whereas BRC explained 34.0% of variance. When the combination of ABC and BRC scores was compared to FES-I score, ABC and BRC together explained 63.5% of FES-I score. Previous studies have also found that strategies adopted by an individual to maintain balance when engaging in activities can affect the development of concerns about falling (Ellmers et al., 2022). Balance confidence and balance recovery confidence could thus be useful psychological factors to inform clinicians how they could intervene behavioural responses to concerns about falling and measure the outcome of interventions. Literature has also shown that balance training exercises can improve balance confidence as reflected in improvements in ABC score (Myers et al., 1998). As BRC is a relatively new assessment tool, future studies can explore how exercises or other clinical interventions can improve balance recovery.
There are some limitations of this study. First, study participants are high functioning level older adults living in the community. The findings may not be representative of other populations such as frail older adults and people with stroke or Parkinson’s. Second, this study has only used falls efficacy tools targeting balance confidence and balance recovery confidence. The tools to measure other domains of falls efficacy such as safe falling confidence and post fall recovery confidence have not been assessed. However, we view that the convergent and predictive validity of these falls efficacy tools compared against ABC, BRC and FES-I should provide similar findings considering the nature of the constructs targeted.
In conclusion, this study has highlighted some key points advocating a proper selection of the commonly used tools measuring falls efficacy and concerns about falling. First, ABC, BRC, and FES-I are measuring similar, but distinct constructs. The conceptual nature of the constructs measured by the different instruments are reportedly different and this is demonstrated by moderate-strong levels of correlation found between the instruments. Second, ABC and BRC scores contribute to FES-I scores, suggesting that balance confidence and balance recovery confidence can be examined when targeting concerns about falling. This would provide a deeper understanding of the interventional mechanisms in a way whether concerns about falling was addressed due to changes in perceived balance control abilities or influences in other potential variables, such as a greater perceptual control towards reducing falls-related consequences (Soh, 2022a).
Data availability statement
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Ethics statement
The studies involving humans were approved by Singapore Institute of Technology Institutional Review Board (Ref. 2020098). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
HT: Writing – original draft, Writing – review and editing. JH: Writing – review and editing. PO: Writing – review and editing. WY: Writing – review and editing. SS: Writing – review and editing, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The opinions given in this article are those of the authors and do not necessarily represent the official position of the organisations and universities listed.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Cleary, K., and Skornyakov, E. (2017). Predicting falls in community dwelling older adults using the Activities-specific Balance Confidence Scale. Arch. Gerontol. Geriatr. 72, 142–145. doi:10.1016/j.archger.2017.06.007
Delbaere, K., Close, J. C. T., Brodaty, H., Sachdev, P., and Lord, S. R. (2010). Determinants of disparities between perceived and physiological risk of falling among elderly people: cohort study. Br. Med. J. 341 (4), c4165. doi:10.1136/bmj
de Souza, L. F., Canever, J. B., Moreira, B. de S., Danielewicz, A. L., and de Avelar, N. C. P. (2022). Association between fear of falling and frailty in community-dwelling older adults: a systematic review. Clin. Interv. Aging 17, 129–140. doi:10.2147/CIA.S328423
Ellmers, T. J., Freiberger, E., Hauer, K., Hogan, D. B., McGarrigle, L., Lim, M. L., et al. (2023). Why should clinical practitioners ask about their patients’ concerns about falling? Age Ageing 52 (4), afad057. doi:10.1093/ageing/afad057
Ellmers, T. J., Wilson, M. R., Norris, M., and Young, W. R. (2022). Protective or harmful? A qualitative exploration of older people’s perceptions of worries about falling. Age Ageing 51 (4), afac067. doi:10.1093/ageing/afac067
Figueiredo, D., and Santos, S. (2017). Cross-cultural validation of the Falls Efficacy Scale-International (FES-I) in Portuguese community-dwelling older adults. Arch. Gerontol. Geriatr. 68, 168–173. doi:10.1016/j.archger.2016.10.010
Greenberg, S. A., Sullivan-Marx, E., Sommers, M., Lynn, S., Chittams, J., and Cacchione, P. Z. (2016). Measuring fear of falling among high-risk, urban, community-dwelling older adults. Geriatr. Nur (Lond). 37 (6), 489–495. doi:10.1016/j.gerinurse.2016.08.018
Hadjistavropoulos, T., Delbaere, K., and Fitzgerald, T. D. (2011). Reconceptualizing the role of fear of falling and balance confidence in fall risk. J. Aging Health 23 (1), 3–23. doi:10.1177/0898264310378039
Healthy ageing research Group. The University of Manchester. Available online at: https://sites.manchester.ac.uk/fes-i/. (Accessed 08, July, 2023)
Hughes, C. C., Kneebone, I. I., Jones, F., and Brady, B. (2015). A theoretical and empirical review of psychological factors associated with falls-related psychological concerns in community-dwelling older people. Int. Psychogeriatr. 27 (7), 1071–1087. doi:10.1017/S1041610214002701
Hwang, H. F., Suprawesta, L., Chen, S. J., Yu, W. Y., and Lin, M. R. (2023). Predictors of incident reversible and potentially reversible cognitive frailty among Taiwanese older adults. BMC Geriatr. 23 (1), 24. doi:10.1186/s12877-023-03741-4
Ishige, S., Wakui, S., Miyazawa, Y., and Naito, H. (2020). Reliability and validity of the Activities-specific Balance Confidence scale-Japanese (ABC-J) in community-dwelling stroke survivors. Phys. Ther. Res. 23 (1), 15–22. doi:10.1298/ptr.E9982
Jørstad, E. C., Hauer, K., Becker, C., and Lamb, S. E.ProFaNE Group (2005). Measuring the psychological outcomes of falling: a systematic review. J. Am. Geriatr. Soc. 53 (3), 501–510. doi:10.1111/j.1532-5415.2005.53172.x
Kuo, C. T., Chen, D. R., Chen, Y. M., and Chen, P. Y. (2021). Validation of the short falls efficacy scale-international for Taiwanese community-dwelling older adults: associations with fall history, physical frailty, and quality of life. Geriatr. Nur (Lond). 42 (5), 1012–1018. doi:10.1016/j.gerinurse.2021.06.006
Lach, H. W. (2002). Fear of falling: an emerging public health problem. J. Am. Soc. Aging 26 (4), 33–37.
Luk, S. C. Y. (2023). Healthy ageing in Singapore: opportunities, challenges and the way forward. Singapore: Palgrave Macmillan.
Maki, B. E., Cheng, K. C., Mansfield, A., Scovil, C. Y., Perry, S. D., Peters, A. L., et al. (2008). Preventing falls in older adults: new interventions to promote more effective change-in-support balance reactions. J. Electromyogr. Kinesiol 18 (2), 243–254. doi:10.1016/j.jelekin.2007.06.005
Matchar, D. B., Duncan, P. W., Lien, C. T., Ong, M. E. H., Lee, M., Gao, F., et al. (2017). Randomized controlled trial of screening, risk modification, and physical therapy to prevent falls among the elderly recently discharged from the emergency department to the community: the steps to avoid falls in the elderly study. Arch. Phys. Med. Rehabil. 98 (6), 1086–1096. doi:10.1016/j.apmr.2017.01.014
McGarrigle, L., Yang, L. R., Gittins, M., and Todd, C. (2023). A systematic review and meta-analysis of the measurement properties of concerns-about-falling instruments in older people and people at increased risk of falls. Age Ageing 52 (5), afad055. doi:10.1093/ageing/afad055
Montero-Odasso, M., van der Velde, N., Martin, F., Petrovic, M., Tan, M. P., Ryg, J., et al. (2022). World guidelines for falls prevention and management for older adults: a global initiative. Age Ageing 51 (9), 1–36. doi:10.1093/ageing/afac205
Moore, D. S., and Ellis, R. (2008). Measurement of fall-related psychological constructs among independent-living older adults: a review of the research literature. Aging Ment. Health 12 (6), 684–699. doi:10.1080/13607860802148855
Moore, D. S., Ellis, R., Kosma, M., Fabre, J. M., McCarter, K. S., and Wood, R. H. (2011). Comparison of the validity of four fall-related psychological measures in a community-based falls risk screening. Res. Q. Exerc Sport 82 (3), 545–554. doi:10.1080/02701367.2011.10599787
Morgan, M. T., Friscia, L. A., Whitney, S. L., Furman, J. M., and Sparto, P. J. (2013). Reliability and validity of the Falls Efficacy Scale-International (FES-I) in individuals with dizziness and imbalance. Otol. Neurotol. 34 (6), 1104–1108. doi:10.1097/MAO.0b013e318281df5d
Myers, A. M., Fletcher, P. C., Myers, A. H., and Sherk, W. (1998). Discriminative and evaluative properties of the activities-specific balance confidence (ABC) scale. J. Gerontol. 53A (4), M287–M294. doi:10.1093/gerona/53a.4.m287
Pijnappels, M., Kingma, I., Wezenberg, D., Reurink, G., and van Dieën, J. H. (2010). Armed against falls: the contribution of arm movements to balance recovery after tripping. Exp. Brain Res. 201 (4), 689–699. doi:10.1007/s00221-009-2088-7
Pijnappels, M., Reeves, N. D., Maganaris, C. N., and van Dieën, J. H. (2008). Tripping without falling; lower limb strength, a limitation for balance recovery and a target for training in the elderly. J. Electromyogr. Kinesiol 18 (2), 188–196. doi:10.1016/j.jelekin.2007.06.004
Portney, L. G., and Watkins, M. P. (2015). Foundations of clinical research: applications to practice. Philadelphia, PA: Pearson/Prentice Hall, 912.
Powell, L. E., and Myers, A. M. (1995). The activities-specific balance confidence (ABC) scale. J. Gerontol. A Biol. Sci. Med. Sci. 50A (1), M28–M34. doi:10.1093/gerona/50a.1.m28
R Core Team (2023). R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. Available online at: https://www.R-project.org/.
Schoene, D., Heller, C., Aung, Y. N., Sieber, C. C., Kemmler, W., and Freiberger, E. (2019). A systematic review on the influence of fear of falling on quality of life in older people: is there a role for falls? Clin. Interv. Aging 14, 701–719. doi:10.2147/CIA.S197857
Soh, S. L. H. (2022a). Falls efficacy: the self-efficacy concept for falls prevention and management. Front. Psychol. 13, 1011285. doi:10.3389/fpsyg.2022.1011285
Soh, S. L. H. (2022b). Development of a balance recovery confidence scale for community-dwelling older adults. UK: Queen Margaret University.
Soh, S. L. H., Lane, J., Lim, A. Y. H., Mujtaba, M. S., and Tan, C. W. (2022a). Interventions and measurement instruments used for falls efficacy in community-dwelling older adults: a systematic review. J. Frailty Sarcopenia Falls 7 (3), 151–164. doi:10.22540/JFSF-07-151
Soh, S. L. H., Lane, J., Xu, T., Gleeson, N., and Tan, C. W. (2021b). Falls efficacy instruments for community-dwelling older adults: a COSMIN-based systematic review. BMC Geriatr. 21 (21), 21–10. doi:10.1186/s12877-020-01960-7
Soh, S. L. H., Tan, C. W., Lane, J., Yeh, T. T., and Soon, B. (2021c). Near-falls in Singapore community-dwelling older adults: a feasibility study. Pilot Feasibility Stud. 7 (1), 25. doi:10.1186/s40814-020-00748-1
Soh, S. L. H., Tan, C. W., Thomas, J. I., Tan, G., Xu, T., Ng, Y. L., et al. (2021a). Falls efficacy: extending the understanding of self-efficacy in older adults towards managing falls. J. Frailty Sarcopenia Falls 6 (3), 131–138. doi:10.22540/JFSF-06-131
Soh, S. L. H., Tan, C. W., Xu, T., Yeh, T. T., Bte Abdul Rahman, F., Soon, B., et al. (2022b). The balance recovery confidence (BRC) scale. Physiother. Theory Pract. 40, 658–669. doi:10.1080/09593985.2022.2135420
Stalenhoef, P. A., Crebolder, HFJM, Knottnerus, J. A., and van der Horst, F. (1997). Incidence, risk factors and consequences of falls among elderly subjects living in the community. Eur. J. Public Health 7 (3), 328–334.
Stasny, B. M., Newton, R. A., LoCascio, L. V., Bedio, N., Lauke, C., Conroy, M., et al. (2011). The ABC scale and fall risk: a systematic review. Phys. Occup. Ther. Geriatr. 29 (3), 233–242. doi:10.3109/02703181.2011.572249
World Helath Organization (2021). Step safely: strategies for preventing and managing falls across the life-course. Geneva: World Health Organization.
Taheri-Kharameh, Z., Barati, M., Bashirian, S., Heidarimoghadam, R., and Poorolajal, J. (2022). Psychometric properties of the Persian version of the falls behavioral scale in seniors. J. Educ. Community Health 9 (2), 118–122. doi:10.34172/jech.2022.18
Tinetti, M. E., Richman, D., and Powell, L. (1990). Falls efficacy as a measure of fear of falling. J. Gerontol. 45 (6), 239–243. doi:10.1093/geronj/45.6.p239
Ulus, Y., Durmus, D., Akyol, Y., Terzi, Y., Bilgici, A., and Kuru, O. (2012). Reliability and validity of the Turkish version of the Falls Efficacy Scale International (FES-I) in community-dwelling older persons. Arch. Gerontol. Geriatr. 54 (3), 429–433. doi:10.1016/j.archger.2011.06.010
World Health Organization (2007). WHO global report on falls prevention in older age. Geneva: World Health Organization. Available online at: https://extranet.who.int/agefriendlyworld/wp-content/uploads/2014/06/WHo-Global-report-on-falls-prevention-in-older-age.pdf.
Keywords: falls efficacy, balance confidence, balance recovery confidence, concerns about falling, psychological constructs, psychometric, community-dwelling, older adults, fall prevention
Citation: Ting HXT, Ho J, Ong PH, Young WR and Soh SLH (2025) Convergent and predictive validity of the activities-specific balance confidence scales and balance recovery confidence scale, with regard to the falls efficacy scale-international: a cross-sectional study. Front. Aging 6:1330612. doi: 10.3389/fragi.2025.1330612
Received: 31 October 2023; Accepted: 05 May 2025;
Published: 30 May 2025.
Edited by:
Roberto Tedeschi, University of Bologna, ItalyReviewed by:
Morten Scheibye-Knudsen, University of Copenhagen, DenmarkEllen Freiberger, University of Erlangen Nuremberg, Germany
Copyright © 2025 Ting, Ho, Ong, Young and Soh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hazel Xu Teng Ting, dGluZy5oYXplbC54dEB5aXNodW5ob3NwaXRhbC5jb20uc2c=
 Hazel Xu Teng Ting
Hazel Xu Teng Ting Jiaying Ho
Jiaying Ho Peck Hoon Ong
Peck Hoon Ong William R. Young
William R. Young Shawn Leng Hsien Soh
Shawn Leng Hsien Soh