- 1Department of Nursing, The Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou, China
- 2Department of Orthopedic Surgery, The Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China
- 3Orthopedics Research Institute of Zhejiang University, Hangzhou, China
- 4Key Laboratory of Motor System Disease Research and Precision Therapy of Zhejiang Province, Hangzhou, China
- 5Zhejiang Provincial Clinical Medical Research Center for Motor System Diseases, Hangzhou, China
Purpose: To assess the knowledge, attitudes, and practices (KAP) regarding osteoporosis prevention among older adult patients following lumbar fusion surgery and identify associated factors.
Patients and methods: A cross-sectional study was conducted with participants aged ≥50 years. Data on demographic characteristics, KAP related to osteoporosis prevention, and lifestyle behaviors were collected using structured questionnaires. Chi-square tests were performed to explore associations between demographic variables and knowledge levels.
Results: A total of 217 participants were included in the study. Participants demonstrated varying levels of knowledge, with 28.6% scoring high on the OPAAT. Female gender, higher educational attainment, urban residence, and diabetes were significantly associated with higher knowledge levels. Positive lifestyle practices, such as calcium and vitamin D supplementation, were observed in 64.5% and 41.0% of participants, respectively, while regular outdoor exercise and dairy product consumption were less common.
Conclusion: The findings highlight gaps in osteoporosis prevention KAP among older adult patients following lumbar fusion surgery. Tailored educational programs and interventions are necessary to enhance awareness and promote healthier behaviors.
Introduction
Osteoporosis is a prevalent condition among older adults, characterized by reduced bone density and increased fracture risk (Cosman et al., 2024; Quek et al., 2024; Wang et al., 2024). Notably, many patients remain untreated for osteoporosis before undergoing lumbar fusion surgery, particularly men. Untreated patients typically exhibit lower bone mineral density (BMD) and elevated bone resorption markers compared to those receiving treatment (Köhli et al., 2025). Furthermore, osteoporosis is a significant risk factor for mechanical complications of lumbar fusion (Filley et al., 2024) and anti-osteoporosis therapy could reduce bone resorption and thus facilitate fusion (S et al., 2024). Thus, adequate knowledge, positive attitudes, and appropriate practices (KAP) regarding osteoporosis prevention are essential to mitigating these risks. However, studies on osteoporosis-related KAP in this specific patient population are limited.
Postoperative recovery following lumbar fusion surgery often involves prolonged periods of reduced activity (Devin and McGirt, 2015; Wang et al., 2020), which can further compromise bone health. Additionally, the aging process itself, along with common comorbidities such as diabetes and cardiovascular disease, may exacerbate the risk of osteoporosis (Ross et al., 2022; Azeez, 2023). Despite the critical importance of osteoporosis prevention, there is a lack of targeted educational programs addressing this issue in the context of surgical recovery. Investigating the knowledge gaps and lifestyle behaviors of these patients can help identify specific barriers to effective osteoporosis prevention and guide the development of tailored interventions.
This study aims to evaluate the levels of knowledge, attitudes, and practices concerning osteoporosis prevention among older adult patients following lumbar fusion surgery. The findings can inform the development of targeted educational strategies and interventions to promote bone health in this high-risk group.
Materials and methods
Study participants
A cross-sectional study was conducted on older adult patients (aged ≥50 years) who underwent lumbar fusion surgery from April 2024 to July 2024. Participants were recruited from a tertiary hospital. Only patients with no previous diagnosis of osteoporosis were included in the study.
Ethics statement
This study was reviewed and approved by the local Ethics Committee (IRB-2024–1492). Written consent was obtained from all participants. Informed consent was submitted by all subjects when they were enrolled.
Sampling method
This study utilized a convenience sampling method, selecting eligible patients consecutively from those admitted for spinal surgery during the study period. While this approach enables efficient data collection within a specific population, it may introduce selection bias, which should be taken into account when interpreting the results.
Questionnaire
Data on KAP related to osteoporosis prevention, along with lifestyle habits, were collected using structured questionnaires. The Osteoporosis Prevention and Awareness Test (OPAAT) was employed to evaluate knowledge levels (Toh et al., 2015; Ahmed et al., 2023). This instrument includes 30 questions covering topics such as the pathophysiology of osteoporosis, preventive strategies, and the consequences of untreated disease. Scores were assigned based on participant responses: 1 point for each correct answer and 0 points for incorrect answers or “do not know” responses. Knowledge levels were categorized as high (≥24/30), average (19–23), or low (<19).
In addition to knowledge assessment, sociodemographic and behavioral data were gathered. Variables included age, gender, body mass index (BMI), education level, residence, marital status, and the presence of comorbidities such as hypertension, diabetes, and heart disease. Lifestyle practices were also evaluated, distinguishing between positive behaviors (e.g., regular exercise, calcium and vitamin K2 consumption, sun exposure) and negative behaviors (e.g., smoking, alcohol use, and sedentary habits).
A self-administered questionnaire was distributed to patients upon admission in a paper-based format or electronically via WeChat, prior to receiving any education or information from their doctor. To ensure consistency, ward nurses received standardized training to guide patients in completing the survey. Incomplete responses were deemed invalid to maintain data integrity.
Statistical analysis
Categorical variables were reported as frequencies and percentages. Chi-square tests were employed for categorical variables. A p-value of less than 0.05 was considered statistically significant. All statistical and descriptive analysis were performed by using SPSS 22.0 software (SPSS Inc., Chicago, IL, United States). A p-value <0.05 was considered statistically significant.
Results
Demographic characteristics
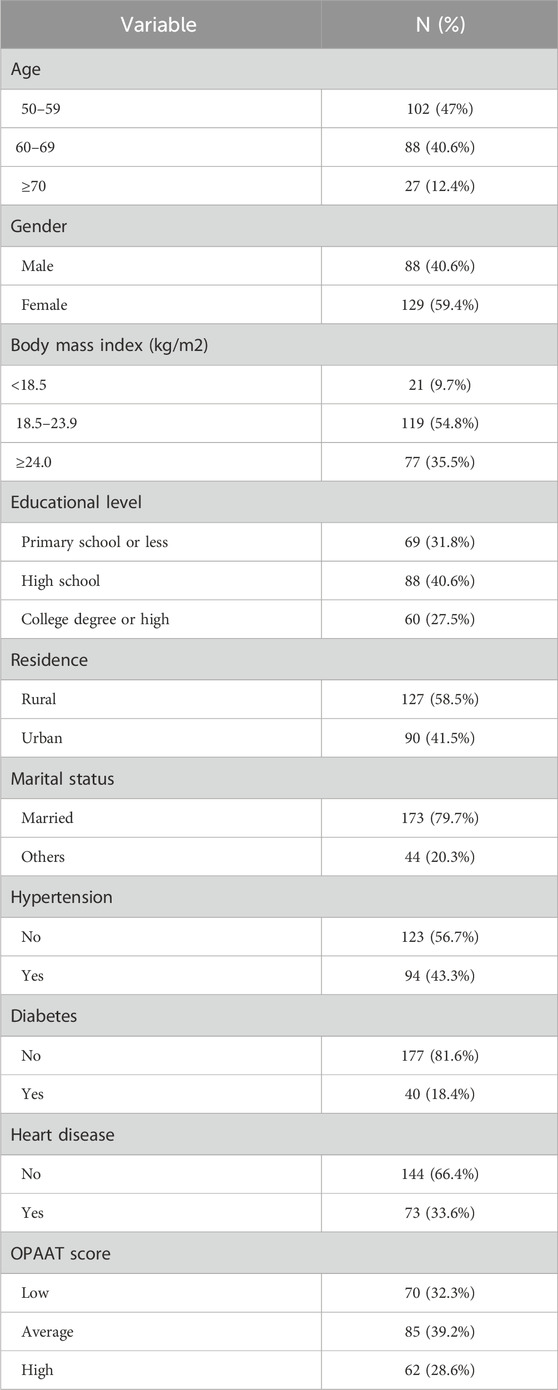
A total of 217 participants were included in the study. The majority were aged between 50 and 59 years (47%), followed by 60–69 years (40.6%), and ≥70 years (12.4%). Females accounted for 59.4% of the participants, while 40.6% were male. Most participants had a BMI within the range of 18.5–23.9 (54.8%), while 35.5% were classified as ≥24.0 kg/m2, and 9.7% had a BMI of <18.5. Educational levels varied, with 31.8% having a primary school education or less, 40.6% completing high school, and 27.5% attaining a college degree or higher. A larger proportion of participants resided in rural areas (58.5%) compared to urban areas (41.5%). The majority were married (79.7%). Regarding comorbidities, 43.3% had hypertension, 18.4% had diabetes, and 33.6% had heart disease (Table 1).
Knowledge, attitude, and awareness of osteoporosis prevention
Participants were categorized into low (32.3%), average (39.2%), and high (28.6%) knowledge levels based on their OPAAT scores (Table 1). Gender was significantly associated with knowledge levels (P = 0.012), with females more likely to have higher knowledge scores. Educational level also had a significant impact (P = 0.022); participants with a college degree or higher demonstrated higher knowledge. Rural residents were less knowledgeable compared to their urban counterparts (P = 0.009). Diabetes status was another significant factor (P = 0.011), as participants with diabetes tended to have higher knowledge scores (Table 2).
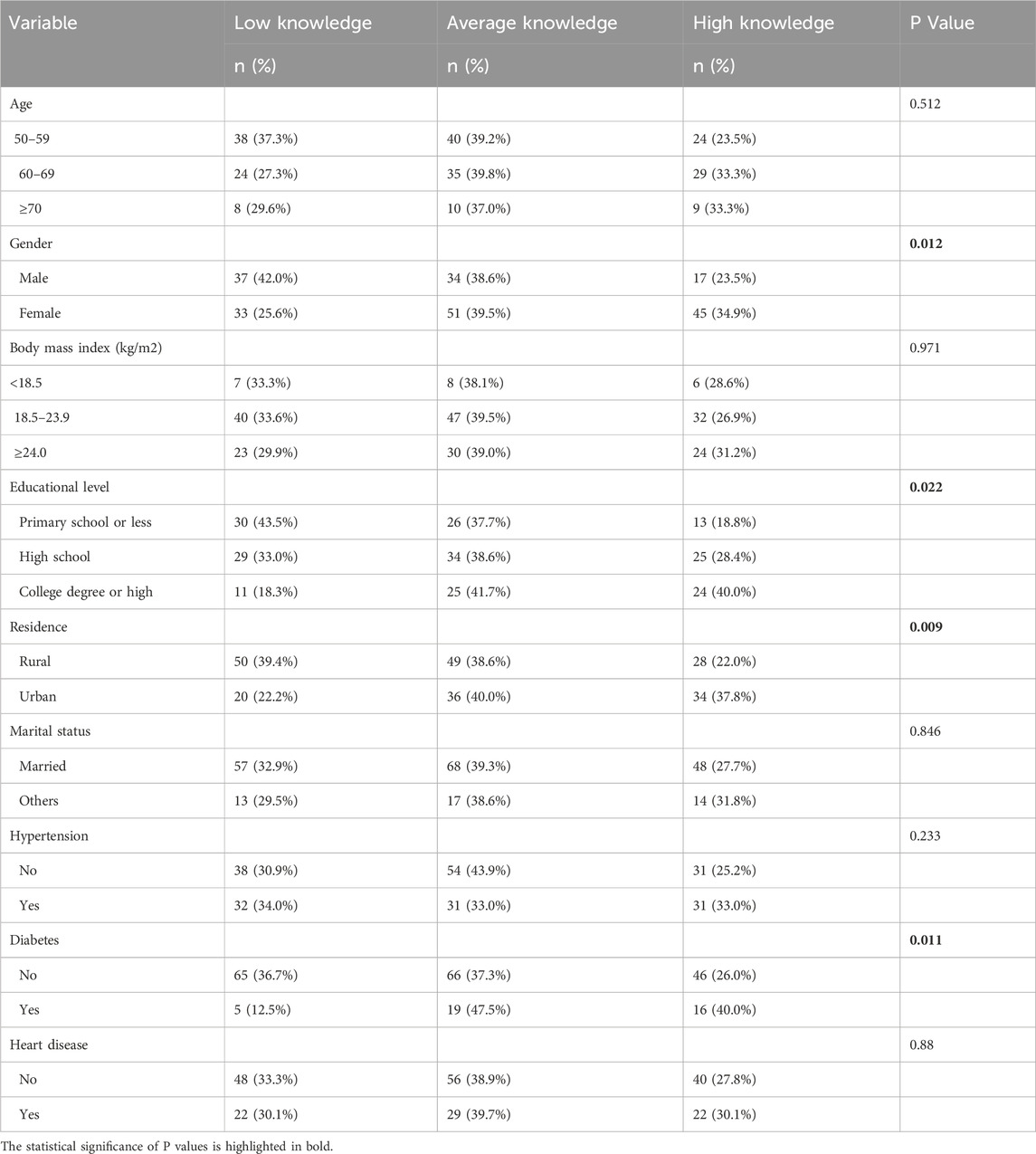
Table 2. Association of demographic characteristics with participants’ knowledge of osteoporosis prevention and awareness.
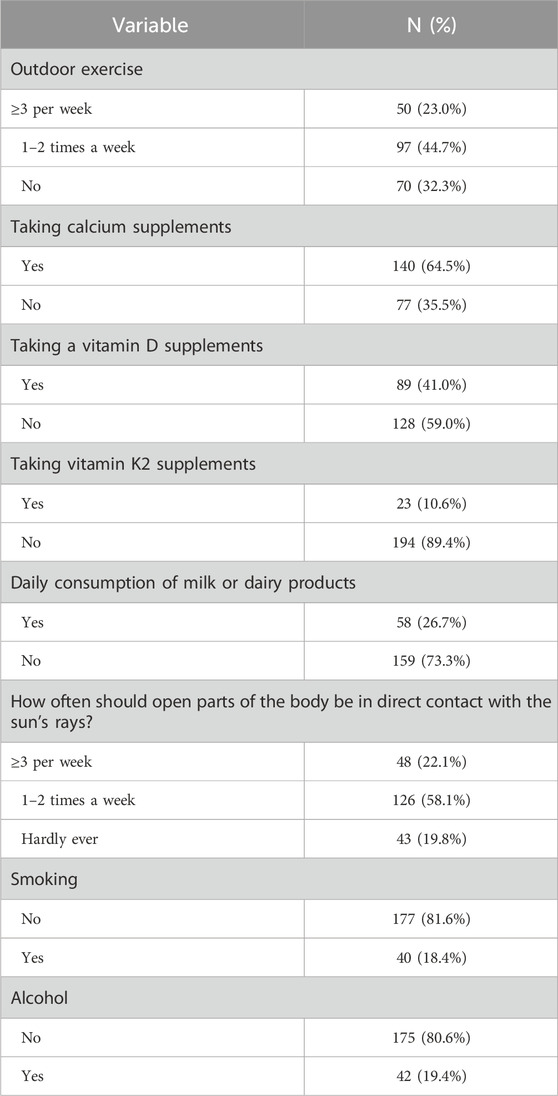
Healthy lifestyle behaviors
Regarding osteoporosis prevention practices, only 23% of participants engaged in outdoor exercise ≥3 times per week, 44.7% exercised 1–2 times weekly, and 32.3% reported no outdoor exercise. Calcium supplementation was reported by 64.5% of participants, while 41.0% used vitamin D supplements; however, only 10.6% included vitamin K2 in their regimen. Daily consumption of milk or dairy products was low, with only 26.7% reporting regular intake. Sun exposure habits revealed that 22.1% exposed their skin to sunlight ≥3 times weekly, 58.1% did so 1–2 times weekly, and 19.8% rarely had sun exposure. Smoking and alcohol consumption rates were relatively low, at 18.4% and 19.4%, respectively (Table 3).
Discussion
The study revealed that gender, educational level, residence, and diabetes status significantly influenced osteoporosis prevention knowledge. Female participants demonstrated higher awareness, possibly due to greater health-related information-seeking behavior. Similarly, participants with college education or higher displayed better knowledge, underscoring the impact of educational attainment, which was in line with many previous studies (Tabor et al., 2022; Elgzar et al., 2023; Oumer et al., 2020). However, Alhouri et al. (2022) reported no significant association between educational level and osteoporosis knowledge, suggesting variability in results across different populations and contexts. Urban residents displayed higher levels of awareness compared to their rural counterparts, possibly due to better access to healthcare resources. This aligns with Alhouri et al. (2022), who also reported greater osteoporosis awareness among urban participants. Beyond healthcare access, additional factors may contribute to this disparity, including cultural perceptions of aging and bone health, lower literacy rates, and economic constraints (Oumer et al., 2020). Rural populations often have limited exposure to formal health education and may rely more on traditional beliefs, which can shape their health behaviors. To narrow this knowledge gap, targeted interventions such as community-based health programs, mobile health education initiatives, and expanded osteoporosis screening services in rural areas could be effective in improving awareness and preventive practices.
Notably, the study revealed a significant association between diabetes and increased osteoporosis awareness. A possible explanation is that individuals with diabetes have more frequent interactions with healthcare professionals for regular monitoring and treatment, which exposes them to more health education, including information on bone health. Moreover, diabetes management often incorporates lifestyle interventions—such as dietary modifications and physical activity—that overlap with osteoporosis prevention strategies. To address these disparities, targeted interventions, such as community health programs and educational initiatives in rural areas, should be implemented. These efforts could help bridge knowledge gaps and ensure equitable access to osteoporosis-related information and preventive resources. Further research exploring the role of chronic disease education in osteoporosis awareness could provide deeper insights into effective public health strategies.
The rates of calcium and vitamin D supplementation among participants were relatively high, at 64.5% and 41.0%, respectively. However, only 10.6% reported using vitamin K2 supplements, reflecting a limited understanding of comprehensive bone health practices. This aligns with findings in prior studies, which have highlighted the underutilization of vitamin K2 in osteoporosis prevention regimens, despite its role in regulating calcium metabolism and enhancing bone mineralization (Shiraki et al., 2010; Elahmer et al., 2024). The low prevalence of vitamin K2 supplementation in our study population may stem from a general lack of awareness, as most osteoporosis prevention efforts primarily emphasize calcium and vitamin D. Additionally, dietary sources of vitamin K2, such as fermented foods (Bonaldo et al., 2024), are not widely consumed in certain regions, further contributing to inadequate intake. To enhance awareness, targeted educational initiatives should emphasize the complementary role of vitamin K2 in bone health. Healthcare providers can integrate this information into routine patient counseling and postoperative care plans to ensure a more holistic approach to osteoporosis prevention. Furthermore, the low daily consumption of dairy products (26.7%) and inconsistent sun exposure observed in this study may result from factors such as limited dietary diversity, misconceptions about bone health, and lifestyle constraints. These behaviors could significantly affect vitamin D and calcium intake, highlighting the need for tailored interventions to promote healthier habits and improve osteoporosis prevention efforts.
Furthermore, only 23% of participants engaged in regular outdoor exercise, a crucial factor for maintaining bone density and overall health. This low participation rate aligns with findings from similar studies, such as a Korean cohort where approximately 80% of older adults aged 60–70 years did not engage in moderate physical activity, and inactivity increased to 90% in those over 71 years (Park et al., 2014). In contrast, Western populations often report slightly higher physical activity rates, attributed to better access to community fitness programs and culturally ingrained exercise habits (Zhang and Warner, 2023). These differences highlight the importance of infrastructure and cultural influences in promoting physical activity. To address the low participation in outdoor exercise, targeted interventions are needed. Healthcare providers can offer personalized counseling on the benefits of physical activity, while community-based and home exercise programs can provide accessible options for patients. Leveraging technology, such as mobile health apps and virtual classes, can further support engagement, especially for those with mobility limitations. Additionally, educational campaigns highlighting the role of weight-bearing exercises in osteoporosis prevention can help raise awareness and encourage behavior change. These strategies can bridge the gap and promote healthier lifestyles in this patient population.
Healthcare providers play a pivotal role in osteoporosis prevention. Integrating bone health education into routine postoperative care for lumbar fusion patients could enhance knowledge and attitudes. Additionally, implementing policy-level initiatives, such as subsidized calcium and vitamin supplements for at-risk populations, could improve accessibility. Leveraging technology, such as mobile health applications, can also facilitate the dissemination of targeted educational materials and monitor patient compliance with prevention strategies.
This study has several limitations. First, our study was conducted in a tertiary hospital, which may introduce some selection bias, as patients from different socioeconomic backgrounds and healthcare access levels may have varying knowledge and attitudes toward osteoporosis prevention. However, we aimed to include a diverse sample by recruiting both urban and rural residents and patients with different education levels. Future studies with multi-center data collection would help improve the generalizability of our findings. Second, the self-reported nature of the questionnaires may introduce response bias, as participants may overestimate positive behaviors. Lastly, the cross-sectional design precludes causal inferences about the relationships between demographic factors and knowledge levels. Future research should incorporate longitudinal follow-up studies to assess changes in knowledge, attitudes, and practices over time. Evaluating the effectiveness of targeted educational interventions on osteoporosis prevention behaviors would be a valuable extension of our current work.
Conclusion
Older adult patients recovering from lumbar fusion surgery exhibit varied levels of knowledge, attitudes, and practices regarding osteoporosis prevention. Gender, education, residence, and comorbidities such as diabetes are significant determinants of awareness. While some positive behaviors, such as supplement use, were observed, gaps in exercise and dietary habits remain. This study emphasizes the importance of personalized educational interventions to improve bone health and prevent osteoporosis-related complications in this vulnerable group.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The Second Affiliated Hospital of Zhejiang University School of Medicine Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SS: Data curation, Formal Analysis, Investigation, Methodology, Project administration, Software, Writing – original draft. MW: Formal Analysis, Investigation, Methodology, Writing – review and editing. CY: Data curation, Formal Analysis, Methodology, Writing – review and editing. QL: Investigation, Methodology, Writing – review and editing. ZW: Conceptualization, Formal Analysis, Investigation, Methodology, Supervision, Writing – review and editing. YM: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Writing – review and editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by Zhejiang Provincial Medical and Health Science and Technology Plan (2025KY867).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Ahmed, S., Farooqui, A. J., Pradhan, N. A., Zehra, N., Majid, H., Jafri, L., et al. (2023). Assessing the knowledge, attitude and practice of osteoporosis among Pakistani women: a national social-media based survey. PLoS One 18 (11), e0288057. doi:10.1371/journal.pone.0288057
Alhouri, A., Zahrawi, H., Alasaad, S., Alhayek, S. M., Al Houri, H. N., Jomaa, S., et al. (2022). Assessing the knowledge and attitude towards osteoporosis among Syrian women: a cross-sectional study. Int. J. rheumatology. 2022, 6431151. doi:10.1155/2022/6431151
Azeez, T. A. (2023). Osteoporosis and cardiovascular disease: a review. Mol. Biol. Rep. 50 (2), 1753–1763. doi:10.1007/s11033-022-08088-4
Bonaldo, F. (2024). Leroy FJTiFS, Technology. Bacterially produced vitamin K2 and its potential to generate health benefits in humans.
Cosman, F., Lewiecki, E. M., Eastell, R., Ebeling, P. R., Jan De Beur, S., Langdahl, B., et al. (2024). Goal-directed osteoporosis treatment: ASBMR/BHOF task force position statement 2024. J. bone mineral Res. official J. Am. Soc. Bone Mineral Res. 39 (10), 1393–1405. doi:10.1093/jbmr/zjae119
Devin, C. J., and McGirt, M. J. (2015). Best evidence in multimodal pain management in spine surgery and means of assessing postoperative pain and functional outcomes. J. Clin. Neurosci. official J. Neurosurg. Soc. Australasia 22 (6), 930–938. doi:10.1016/j.jocn.2015.01.003
Elahmer, N. R., Wong, S. K., Mohamed, N., Alias, E., Chin, K. Y., and Muhammad, N. (2024). Mechanistic insights and therapeutic strategies in osteoporosis: a comprehensive review. Biomedicines 12 (8), 1635. doi:10.3390/biomedicines12081635
Elgzar, W. T., Nahari, M. H., Sayed, S. H., and Ibrahim, H. A. (2023). Determinant of osteoporosis preventive behaviors among perimenopausal women: a cross-sectional study to explore the role of knowledge and health beliefs. Nutrients 15 (13), 3052. doi:10.3390/nu15133052
Filley, A., Baldwin, A., Ben-Natan, A. R., Hansen, K., Arora, A., Xiao, A., et al. (2024). The influence of osteoporosis on mechanical complications in lumbar fusion surgery: a systematic review. North Am. Spine Soc. J. 18, 100327. doi:10.1016/j.xnsj.2024.100327
Köhli, P., Hambrecht, J., Wang, S. H., Zhu, J., Chiapparelli, E., Schönnagel, L., et al. (2025). Untreated osteoporosis in lumbar fusion surgery patients: prevalence, risk-factors, and effect on bone metabolism. Spine (Phila Pa 1976). 50 (6), 420–428. doi:10.1097/BRS.0000000000005231
Oumer, K. S., Liu, Y., Yu, Q., Wu, F., and Yang, S. (2020). Awareness of osteoporosis among 368 residents in China: a cross-sectional study. BMC Musculoskelet. Disord. 21 (1), 197. doi:10.1186/s12891-020-03217-1
Park, C. H., Elavsky, S., and Koo, K. M. (2014). Factors influencing physical activity in older adults. J. Exerc. rehabilitation. 10 (1), 45–52. doi:10.12965/jer.140089
Quek, Y. Y., Cheng, L. J., Ng, Y. X., Hey, H. W. D., and Wu, X. V. (2024). Effectiveness of anthocyanin-rich foods on bone remodeling biomarkers of middle-aged and older adults at risk of osteoporosis: a systematic review, meta-analysis, and meta-regression. Nutr. Rev. 82 (9), 1187–1207. doi:10.1093/nutrit/nuad121
Ross, B. J., Lee, O. C., Harris, M. B., Dowd, T. C., Savoie, F. H., and Sherman, W. F. (2022). The impact of diabetes on osteoporosis management and secondary fracture risk after primary fragility fractures: a propensity score-matched cohort study. J. Am. Acad. Orthop. Surg. 30 (2), e204–e212. doi:10.5435/jaaos-d-21-00185
Shi, T., Shou, F., Xia, Q., Zhang, T., Teng, D., Jing, W., et al. (2024). Effects of anti-osteoporosis treatment in older adult patients with osteoporosis and lumbar discectomy and fusion. J. back Musculoskelet. rehabilitation 37 (5), 1277–1287. doi:10.3233/bmr-230381
Shiraki, M., Yamazaki, Y., Shiraki, Y., Hosoi, T., Tsugawa, N., and Okano, T. (2010). High level of serum undercarboxylated osteocalcin in patients with incident fractures during bisphosphonate treatment. J. bone mineral metabolism 28 (5), 578–584. doi:10.1007/s00774-010-0167-2
Tabor, E., Grodzki, A., and Pluskiewicz, W. (2022). Higher education and better knowledge of osteoporosis improve bone health in Polish postmenopausal women. Endokrynol. Pol. 73 (5), 831–836. doi:10.5603/EP.a2022.0055
Toh, L. S., Lai, P. S., Wu, D. B., Wong, K. T., Low, B. Y., and Anderson, C. (2015). The development and validation of the osteoporosis prevention and awareness Tool (OPAAT) in Malaysia. PLoS One 10 (5), e0124553. doi:10.1371/journal.pone.0124553
Wang, P., Wang, Q., Kong, C., Teng, Z., Li, Z., Zhang, S., et al. (2020). Enhanced recovery after surgery (ERAS) program for older adult patients with short-level lumbar fusion. J. Orthop. Surg. Res. 15 (1), 299. doi:10.1186/s13018-020-01814-3
Wang, Z., Li, Z., Shen, Y., Qian, S., Tang, M., He, J., et al. (2024). Long-term effects of COVID-19 infection on bone mineral density. J. Glob. health 14, 05029. doi:10.7189/jogh.14.05029
Keywords: osteoporosis, older adult female patients, lumbar fusion surgery, osteoporosis prevention and awareness tool (OPAAT), education programs
Citation: Sheng S, Wang M, Yu C, Li Q, Wang Z and Ma Y (2025) Knowledge, attitude, and practice of osteoporosis prevention in elder patients following lumbar fusion surgery: a cross-sectional study. Front. Aging 6:1543839. doi: 10.3389/fragi.2025.1543839
Received: 18 December 2024; Accepted: 03 June 2025;
Published: 10 June 2025.
Edited by:
Xun Sun, Tianjin Hospital, ChinaReviewed by:
Wen Yu, Fourth Medical Center of PLA General Hospital, ChinaZhenjiang Ma, Shanghai Jiao Tong University School of Medicine, China
Copyright © 2025 Sheng, Wang, Yu, Li, Wang and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhan Wang, d2FuZ3poYW5oekB6anUuZWR1LmNu; Yaojing Ma, MjUwNDAyOUB6anUuZWR1LmNu
†These authors have contributed equally to this work
 Shaoying Sheng1
Shaoying Sheng1 Zhan Wang
Zhan Wang