- 1Division of Developmental Higher Brain Functions, United Graduate School of Child Development, The University of Osaka, Kanazawa University, Hamamatsu University School of Medicine, Chiba University, University of Fukui, Osaka, Japan
- 2Research Center for Child Mental Development, University of Fukui, Fukui, Japan
- 3Life Science Innovation Center, University of Fukui, Fukui, Japan
- 4Department of Child and Adolescent Psychological Medicine, University of Fukui Hospital, Fukui, Japan
Introduction: Childhood maltreatment (CM) has broad and severe adverse effects in later life, but there are not enough studies conducted during childhood close to the time of maltreatment. Most studies have focused only on a single symptom and have not attempted to capture the global picture of CM.
Methods: We used the Child Behavior Checklist (CBCL) to assess children's behavioral/emotional problems more comprehensively. This study leveraged 32 CM children and 29 typically developing (TD) children who have been assessed using the CBCL 4–18 from our dataset. Group comparisons of the eight subscales were conducted to characterize each behavioral/emotional problem. Receiver Operating Characteristic (ROC) curve analysis was conducted to assess the classification performance. Finally, sensitive period and type analyses were performed based on the children's maltreatment history.
Results: The CM group showed significantly higher behavioral/emotional problems in seven out of the eight subscales. Logistic regression analysis was performed using all combinations of CBCL subscale T-scores and age, sex, and IQ. We created 2047 models and performed ROC analysis for each. Three models were generated: the most accurate model (comprising CBCL T-score, age, sex, and IQ; sensitivity: 0.906, specificity: 0.966), a model excluding IQ (sensitivity: 0.875, specificity: 0.931), and a model consisting only of CBCL (sensitivity: 0.906, specificity: 0.862). The CBCL demonstrated robust predictive capacity for CM by utilizing information provided by caregivers, without directly inquiring about trauma. The sensitive period analysis revealed that the temporal predictor of severity for “withdrawn” and “thought problems” were exposure to CM at age five. Similarly, exposure to CM between the ages of five and seven predicted “somatic complaints”. In the case of type, physical abuse was the predictor for “somatic complaints” and “delinquent behavior”, and emotional abuse was the predictor for “anxious/depressed” and “thought problems”.
Conclusion: Maltreated children present a wider range of behavioral/emotional problems, which must be considered when supporting them. Perspectives gained from sensitive analyses of maltreatment history will help clinicians provide more appropriate interventions.
1 Introduction
Childhood maltreatment (CM) survivors have been shown to present with extensive and severe psychosocial problems in childhood as well as in adulthood (1). CM increases the risk of developing depression in adulthood that is less likely to remit (2, 3). It is also associated with a wide range of psychopathologies, including an increased prevalence of eating disorders (4) and personality disorders (5). The adverse impact of CM on later life is related not only to mental health but also to lifestyle-related diseases, such as obesity (6) and hypertension in sexually abused women (7). According to a large epidemiological study conducted by the Centers for Disease Control and Prevention (CDC) in the United States, a higher number of adverse childhood experiences leads to increased premature mortality risk in later life (8). In the context of social life, CM survivors also have fewer years of education, employment, assets, and income than those without CM exposure, highlighting how CM can negatively impact their quality of life later (9).
The majority of studies are retrospective studies of adults, and with exceptions such as the Bucharest Early Intervention Project (10), which examines the long-term brain effects of receiving institutional care vs. foster care, there are not enough studies on CM effects on childhood. The few existing studies involving children have reported that maltreated children showed physical and mental vulnerabilities, including asthma in physically and sexually abused children (11), deterioration of sleep (12), reduced social interaction, such as emotional recognition from the eyes (13). However, these are separate studies that have focused on each feature observed in maltreated children. In addition to clarifying the vulnerability of maltreated children to individual symptoms through individual hypotheses, research that takes a comprehensive approach to the overall picture of their vulnerability is also necessary.
Psychological scales that measure traumatic symptoms in children, including a short form of the Childhood Trauma Questionnaire (14) and Trauma Symptom Checklist for Children (15), have been used in clinical circumstances. However, the administration of these scales involves directly asking children about their maltreatment and traumatic experiences, which places a high psychological burden on them. The Child Behavior Checklist 4–18 (CBCL) is a non–self-rating questionnaire that parents and surrogate parents, in “problem items”, use to comprehensively rate behavioral/emotional problems in their children (16, 17). It has been used to characterize children with social anxiety (18), and the subscales have also been used in clinical trials of medications for children with conduct disorder (19).
Therefore, this study aimed to characterize the behavioral/emotional problems of maltreated children using the CBCL. The influence of maltreatment history, such as type of maltreatment and length, on behavioral/emotional problems was also compared. Among the various traits that were comprehensively captured, those that were particularly relevant to CM were extracted and their feasibility as predictors for CM was also examined.
2 Materials and methods
2.1 Participants
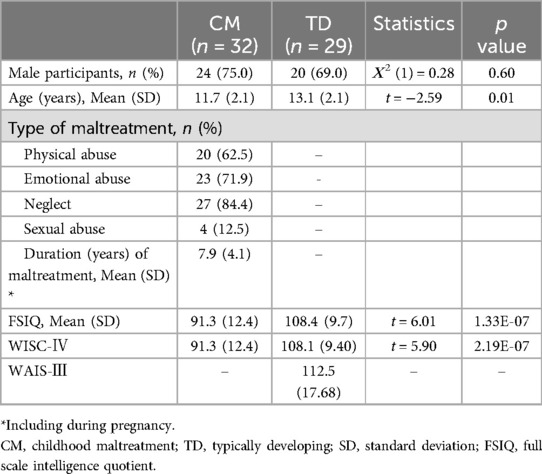
Thirty-two children with maltreatment experiences (CM group) aged 8–16, and 29 typically developing children with no history of maltreatment (TD group) aged 10–17 participated in the study. Many children from the CM group were separated from their biological parents by the Child Protection Service or its equivalent and placed in residential childcare facilities. At the time of this study, the children participating in the study and receiving social care were in residential institutional care. Most of them were in small groups, with two children in large-scale group. All children were in a protected environment (20). All children in the CM group experienced either physical, emotional, or sexual abuse or neglect (ICD-10-CM Code T74). The Child Protection Service's records are based on objective observations and assessments, with the provision of a safe environment. This is important for reliability and accuracy in maltreatment diagnoses and interventions. Individual records were continuously collected and updated over time by various professionals (e.g., behavioral evaluations by temporary shelter staff, medical evaluations by child mental health specialists and pediatric nurses, social evaluations by Child Protection Service staff, and psychological evaluations by licensed psychologists). Detailed demographic characteristics are shown in Table 1. Participants' intelligence quotient (IQ) was measured with the Wechsler Intelligence Scale for Children-Fourth Edition (WISC-IV) or Wechsler Adult Intelligence Scale-Third Edition (WAIS-III). One participant in the CM group had a specific learning disorder with no IQ problem (IQ = 81). Our study included this participant because it was confirmed that they had experienced maltreatment. The clinical diagnostics for neurodevelopmental disorders were assessed by a pediatric psychiatry clinician.
The protocol of this study was approved by The Research Ethics Committee of University of Fukui (Assurance no. 20220039) and was conducted in accordance with the Declaration of Helsinki. This study made secondary use of data obtained from previous studies (21, 22). The study was conducted using an opt-out method in lieu of obtaining written consent, and opt-out information was published on the website of the University of Fukui Hospital in Japan.
2.2 Child behavior checklist (CBCL) 4–18
The parent-rated version of the CBCL has been used to measure children's behavioral/emotional problems (16). In the case of CM, the staff in charge of the child welfare facility, foster parents, or their parents not involved in maltreatment conducted the ratings. The checklist has subscales, including “withdrawn”, “somatic complaints”, “anxious/depressed”, “social problems”, “thought problems”, “attention problems”, “delinquent behavior”, and “aggressive behavior” (16). These eight subscale scores represent the severity of the problem in each domain. Standardized T-scores were used in each domain. In contrast to the original version, the Japanese version of the CBCL was designed to make it applicable for 4–15-year-old children (23). The T-score for the five participants (CM: 1, TD: 4) older than 15 years was calculated as if they were 15 years old since there was no conversion table for that age.
2.3 Receiver operating characteristic (ROC) curve analysis for classification model
Both stepwise regression and Lasso regression were examined to create a model for predicting CM. Stepwise regression uses the statistical information criterion for selecting a regression model. However, this model may not consistently exhibit a high area under the curve (AUC) or Youden index in receiver operating characteristic (ROC) analysis. Similarly, Lasso regression has the same consistency problem. Additionally, Lasso regression is concerned about reproducibility because it uses random numbers in its calculations. Therefore, we chose to perform logistic regression analysis for all combinations of CBCL subscale T-scores and age, sex, and IQ. Using the predicted probabilities from each regression analysis, ROC analysis was performed to calculate the AUC and Youden index; models with high AUC and high Youden index were considered to determine the most suitable model for adoption. For practical reasons, models without IQ and with CBCL only were also created; the model with the highest Youden index was selected. If there were multiple models, the one with the highest AUC was chosen.
2.4 Sensitive period and type analyses for maltreatment history
As in our previous study (24), the sensitive period in which CM exposure may be more strongly associated with behavioral/emotional problems was explored using random forest regression with conditional inference trees (“cforest” in R package party) (25). Two separate analyses were conducted to assess the importance of potential predictors for behavioral/emotional problems. In the first analysis, we evaluated the importance of specific periods of exposure, such as maternal domestic violence during pregnancy and exposure to neglect or physical, emotional, or sexual abuse from birth to age 18. Exposure to each type of maltreatment was coded as 0 (no exposure) or 1 (exposure). The second analysis assessed the importance of exposure to different forms of abuse (physical, emotional, sexual) and neglect, as well as the cumulative number of maltreatment types experienced. This cumulative maltreatment variable was treated as a continuous variable, representing the total number of maltreatment types each participant experienced. Each random forest model consisted of 200 trees, with 4 variables randomly selected at each node. These parameters were guided by theoretical considerations (26, 27) and follow common practices in similar prior research (24) and not optimized through model tuning by grid search. We used permutation testing to assess model performance, comparing the results from the original and permuted data to evaluate statistical significance. Variable importance was assessed using mean decrease in accuracy, where each variable's importance is based on the reduction in prediction accuracy when its values are permuted. This approach highlights the most influential variables in the model.
2.5 Statistical analysis
To compare the behavioral/emotional problems of the CM and TD groups, a multiple linear regression analysis was used for each of the eight domains. The explanatory variables were group (CM group was set to 1 and TD group was set to 0), age, sex, and full-scale IQ. The maximum likelihood with robust standard errors was employed as the estimator since the Breusch-Pagan test failed to assume homoscedasticity for some of the subscales. The Benjamini–Hochberg method was used to correct for false discovery rate (FDR) for multiple testing. All statistical analyses were performed using R software (version 4.4.1) (28) and packages eeptools (29), lmtest (30), lavaan (31), Epi (32), leaps (33), pROC (34), ggplot2 (35), and party (25, 36–39).
3 Results
3.1 Between-group comparisons
As shown in Table 2, the CM group showed significantly higher behavioral/emotional problems compared to the TD group in seven of the eight subscales (0.004 < FDR < 0.009), except for somatic complaints (FDR = 0.456).
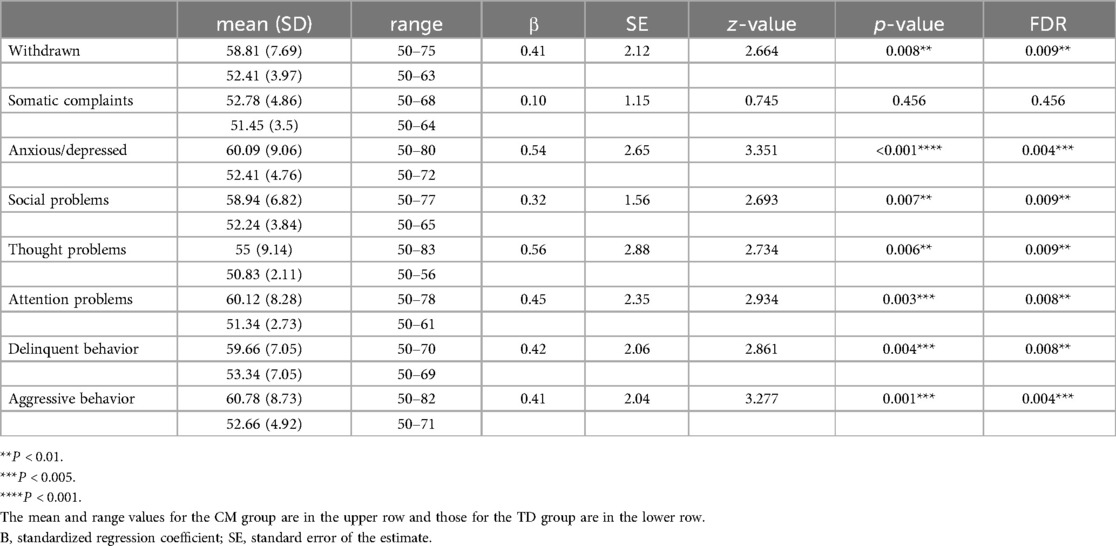
Table 2. Effects of CM or TD group on each behavioral/emotional problem using multiple regression analysis.
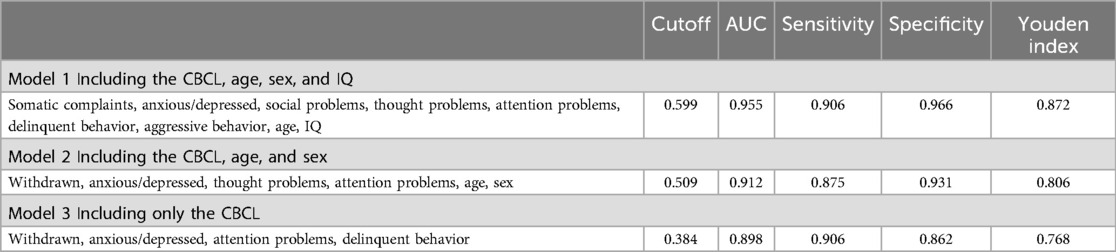
3.2 ROC analysis for classification model
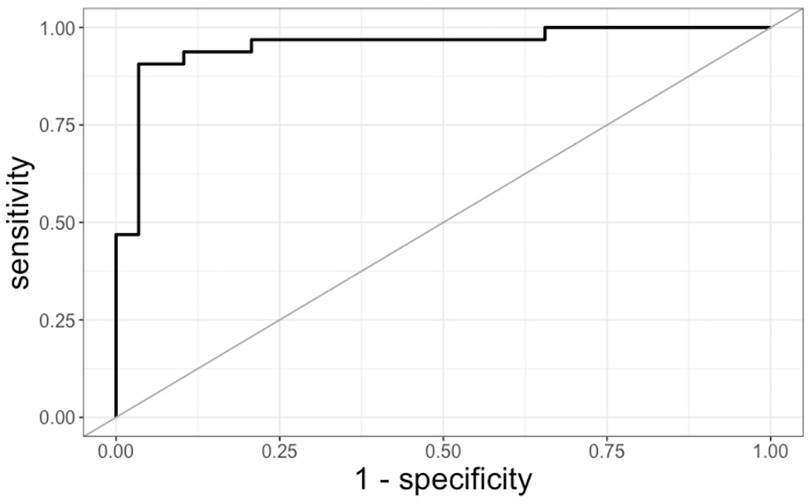
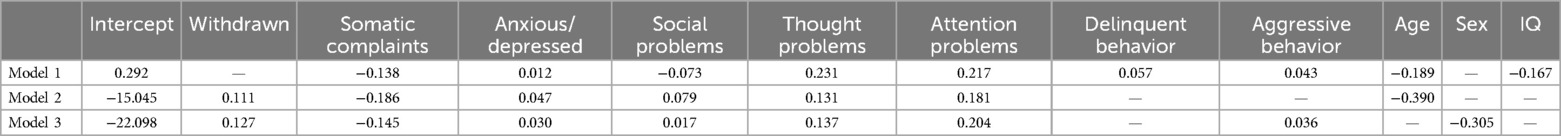
Model 1 in Table 3 displays the top model out of 2,047 total combinations, having high AUC and Youden index. Since the model with the highest AUC also had the highest Youden Index, it was chosen as the most accurate. This model had an AUC of 0.955 with a 95% CI of [0.901–1], a Youden index of 0.872, a sensitivity of 0.906, a specificity of 0.966, and a cutoff point of 0.599. The ROC curve is shown in Figure 1. Models without IQ, and only with CBCL, are also shown in Table 3. The coefficients for the three models are listed in Table 4. The T-scores for each CBCL subscale are multiplied by the coefficients, summed, and logit transformed. The resulting score was evaluated using the cutoff points outlined in Table 3.
3.3 Sensitive period and type analyses for maltreatment history
The most important temporal predictor of the severity of the somatic complaints domain was CM exposure at ages 5–7 years (peak at 5 years old) (Figure 2A, MSE = 82.56, r = 0.41, Ps < 0.05). Similarly, the withdrawn and thought problems domains were predicted by CM exposure at 5 years old (Figure 2A, MSE = 86.55, r = 0.35, P = 0.02 and MSE = 87.56, r = 0.34, P = 0.04). Symptom severity could be predicted with reasonable accuracy from the type of CM. One specific maltreatment, physical abuse (PA), was the most demanding predictor of somatic complaints and delinquent behavior (Figure 2B, MSE = 83.40, r = 0.38, P = 0.007, and MSE = 86.84, r = 0.33, P = 0.046, respectively). Emotional abuse (EA) emerged as the most important predictor of the anxious/depressed and thought problems domains (Figure 2B, MSE = 88.72, r = 0.32, P = 0.03 and MSE = 88.72, r = 0.32, P = 0.04, respectively).
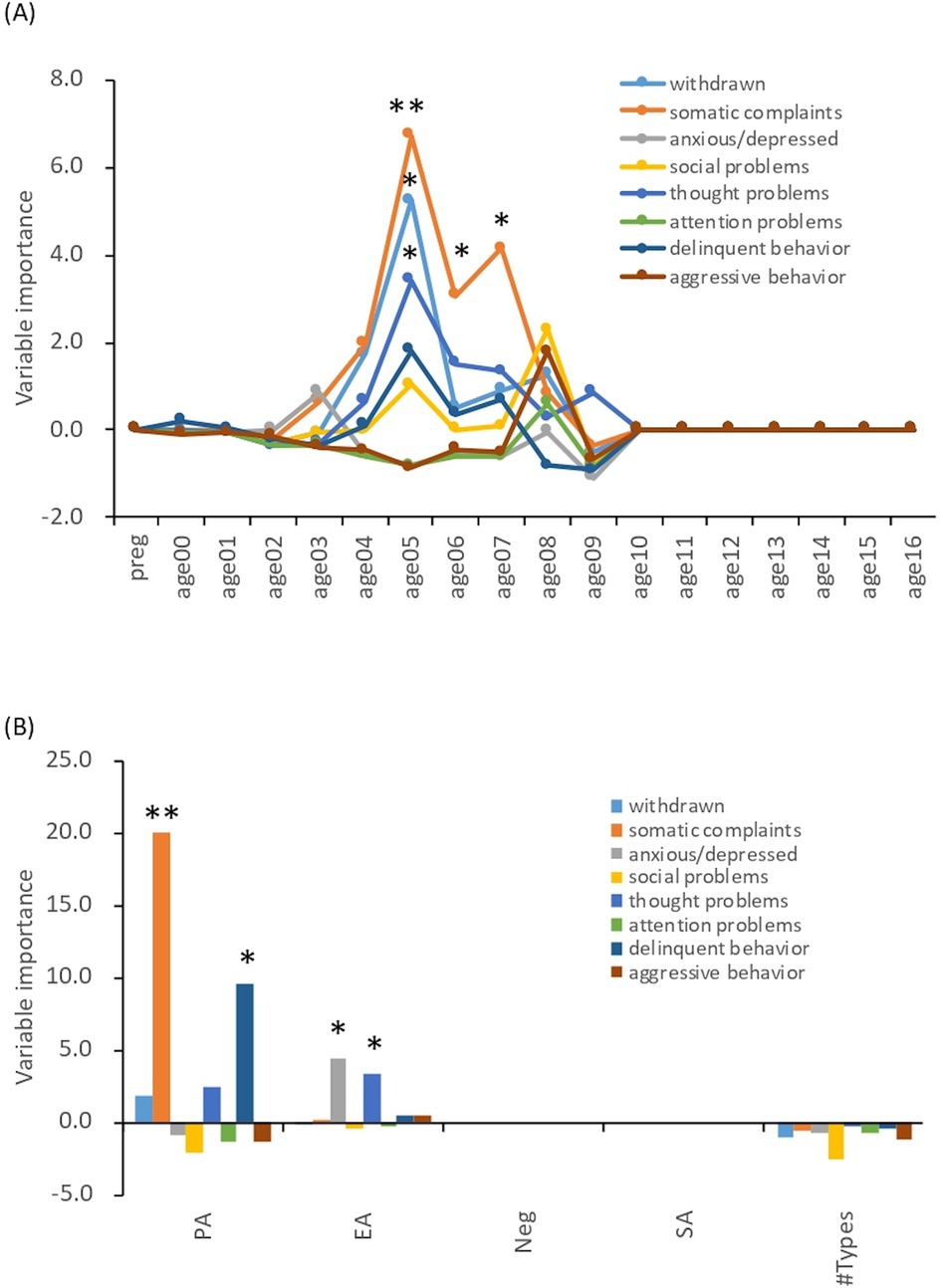
Figure 2. Sensitive period and type analyses. The data are based on historical records from the Child Protection Service or its equivalent agency up to the time of the CBCL evaluation. Of the CM group participants, 17 had experienced maltreatment since during pregnancy. Exposure to maltreatment was coded as 0 (no exposure) or 1 (exposure). (A) Sensitive period analyses. Preg: during pregnancy. *: P < 0.05, **: P < 0.01. (B) Sensitive type analyses. PA, physical abuse; EA, emotional abuse; Neg, neglect; SA, sexual abuse. *: P < 0.05, **: P < 0.01.
4 Discussion
The aim of this study was to comprehensively evaluate the mental and physical features of maltreated children using the CBCL. The CM group scored higher than the TD group on seven subscales except for that of somatic complaints. Comparing the standardized regression coefficients, the subscales of thought problems, anxious/depressed, and attention problems were higher, in that order. CBCL thought problems consist of items screening obsessive-compulsive disorder (40) and/or psychotic symptoms (41), the raw scores on thought problems in CM revealed higher scores for items indicating obsessive thoughts and compulsive behavior. A previous study examined adult patients with obsessive-compulsive disorder who had CM experiences (42), and our results indicated that obsessive thoughts and compulsive behaviors are preceded during childhood. Our previous study using the DSRS-C, which measures depressive symptoms in children, showed that maltreated children presented significantly higher depressive symptom scores than the children in the TD group (21). The higher anxious/depressed scores in this study may be an analog for the higher depressive symptoms seen in the CM group. It has been repeatedly verified that CM causes sleep disturbances (43). Sleep disturbances, such as insomnia, are a major risk factor for daytime inattention (44); however, the CBCL does not have a subscale for sleep disturbances, but seven sleep-related items were used in previous study (45). The results of a group comparison by multiple linear regression analysis of the overall scores on these seven items showed that the CM group has a trend toward significant higher scores (P = 0.017). Thus, the inattention problems that were prominent in the CM children may have resulted partially from sleep disturbances. Regarding the assessment of sleep disturbance in children, CBCL did not cover it sufficiently and it would need to be measured more accurately with more specialized scales and objective methods such as actigraphs. For somatic complaints, there was no significant difference. Adolescents are prone to physical complaints such as headaches and abdominal pain even in normal circumstances (46), which may have made it difficult to detect differences. Therefore, the CBCL results appear to capture the characteristics of CM, yielding outcomes that do not dissociate from the practical clinical picture.
A model using the T-scores of the CBCL subscale, age, and IQ was found to predict CM with a high probability of AUC 0.955, sensitivity of 0.906, and specificity of 0.966 (47). This model may have the potential to capture features of maltreated children and be used for screening, even though it is not a questionnaire that directly asks about traumatic or maltreatment experiences. To the extent that CM features can even be captured from only a combination of comprehensive questions, in contrast to questionnaires that explicitly ask about traumatic or abusive experiences, CBCL may be useful and less psychologically invasive for screening for CM.
The different maltreatment histories in CM and their impact on the behavioral/emotional problems of maltreatment children were examined through a sensitive period analysis (24). The severity of being withdrawn and having thought problems were associated with maltreatment exposure at 5 years of age. This is a period of language development (48) and social development, when social skills gradually increase as children interact with others based on attachments (49). Maltreatment during this period may impede social development and the child may become withdrawn and develop thought problems in the future due to social isolation. Somatic complaints were significantly associated with whether the children had been exposed to maltreatment at ages 5–7, although somatic complaints comprised the only subscale that did not differ between the CM and TD groups. A possible explanation, although the exact reason is not known, is that the tendency for somatic complaints is due to immature language development (50, 51). In the CM group, the delay in language development due to CM may contribute to somatic complaints at the age of 5 to 7 years. Even in the TD group, nonverbal distress may have manifested as physical symptoms due to underdeveloped language. However, the factors influencing their language development remain unclear.
Analysis by type of abuse showed that PA was a predictor of somatic complaints and delinquent behavior. The importance of PA in the severity of somatic complaints may suggest that physical punishment, such as punching and kicking, can affect the development of brain regions involved in the control of somatic symptoms in children. Indeed, harsh corporal punishment during childhood reduced the prefrontal cortex gray matter volume in young adults, as reported by our group (52). Furthermore, increased delinquent behavior when subjected to active maltreatment, such as PA, was observed in previous studies (53). In addition, EA was important concerning the severity of being anxious/depressed and having thought problems. EA has been reported to increase anxiety and depressed symptoms (54). The EA group showed high scores for obsessive-compulsive symptoms (40), while scores for items measuring other psychotic symptoms were lower than that. According to previous studies (55), EA is associated with more severe obsessive-compulsive disorder symptoms in adult patients, and this finding may be consistent with previous ones.
There are several limitations to this study. First, because the CBCL is a questionnaire designed to be answered by parents and surrogate parents, the results may be inaccurate due to bias depending on the raters or information they did not have access to. Second, the study included two participants with IQs below 70. In addition, the CM group had significantly lower IQs than the TD group; it has been repeatedly shown (56) that children who have experienced CM have lower IQs than TD children, and the participants in this study may reflect these assumptions. Third, the Japanese version of the CBCL is standardized for ages 4 to 15. However, this study included participants aged 16 to 17, who were converted to T-scores as though they were 15 years old. This may affect the validity of the analysis. Fourth, the model to predict CM using T-scores of the CBCL subscale, age, and IQ showed very high predictive power, but has not been validated with other data. Thus, the model will need to be validated with larger sample sizes and cross-validation. Fifth, we did not perform any parameter optimization of the model, such as grid search, which could affect its performance and the accuracy of the results. We also used permutation testing to assess model performance and did not perform cross-validation; nevertheless, we acknowledge the potential value of such model optimization and performance assessments and plan to incorporate them in future work. Finally, a larger sample size might have made it possible to observe sex differences (e.g., somatic symptoms are likely to be more prevalent in girls).
5 Conclusion
Maltreated children exhibited various behavioral/emotional problems compared to TD children. Therefore, when providing supportive interventions, it is necessary to pay attention not only to their traumatic symptoms but also to existing behavioral/emotional problems. The CBCL is a useful questionnaire to comprehensively measure those underlying issues. Furthermore, we believe that the perspectives gained from a sensitive analysis of maltreatment history contribute to the establishment of more precise interventions.
Data availability statement
The datasets presented in this article are not readily available because ethical considerations. Requests to access the datasets should be directed to corresponding author. Data may be provided to interested researchers upon reasonable request to the corresponding authors, after clearance from The Research Ethics Committee of University of Fukui and consent of all authors.
Ethics statement
The studies involving humans were approved by The Research Ethics Committee of University of Fukui. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin because The study was conducted using an opt-out method in lieu of obtaining written consent, and opt-out information was published on the website of the University of Fukui Hospital in Japan.
Author contributions
TM: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing. SN: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing, Funding acquisition. ST: Data curation, Writing – review & editing, Funding acquisition. AY: Formal analysis, Writing – review & editing. TF: Data curation, Formal analysis, Writing – review & editing, Funding acquisition. AT: Data curation, Writing – review & editing, Funding acquisition.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. All phases of this study were supported by AMED under Grant Number JP20gk0110052 (AT and SN), JSPS KAKENHI Scientific Research (A) (19H00617 and 22H00492 to AT), Scientific Research (C) (20K02700 to SN, 18K02480 to TXF), Young Scientists, and Early-Career Scientists (15K21026 and 18K13109 to ST), Grant-in-Aid for “Creating a Safe and Secure Living Environment in the Changing Public and Private Spheres” from the Japan Science and Technology Agency (JST)/Research Institute of Science and Technology for Society (RISTEX) (AT and TXF), a research grant from Japan-United States Brain Research Cooperative Program (AT), research grant from the Strategic Budget to Realize University Missions (AT), research grants from the University of Fukui (FY 2019 and 2020 to SN), Grant-in-Aid for Translational Research from the Life Science Innovation Center, University of Fukui (LSI20305 and LSI22202 to SN), and Grant for Life Cycle Medicine from Faculty of Medical Sciences, University of Fukui (SN).
Acknowledgments
We thank all the participants and the staff of the Research Center for Child Mental Development.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Tomoda A, Nishitani S, Takiguchi S, Fujisawa TX, Sugiyama T, Teicher MH. The neurobiological effects of childhood maltreatment on brain structure, function, and attachment. Eur Arch Psychiatry Clin Neurosci. (2024). doi: 10.1007/s00406-024-01779-y
2. Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: a meta-analysis. Am J Psychiatry. (2012) 169:141–51. doi: 10.1176/appi.ajp.2011.11020335
3. Nelson J, Klumparendt A, Doebler P, Ehring T. Childhood maltreatment and characteristics of adult depression: meta-analysis. Br J Psychiatry. (2017) 210:96–104. doi: 10.1192/bjp.bp.115.180752
4. Afifi TO, Sareen J, Fortier J, Taillieu T, Turner S, Cheung K, et al. Child maltreatment and eating disorders among men and women in adulthood: results from a nationally representative United States sample. Int J Eat Disord. (2017) 50:1281–96. doi: 10.1002/eat.22783
5. Johnson JG, Cohen P, Brown J, Smailes EM, Bernstein DP. Childhood maltreatment increases risk for personality disorders during early adulthood. Arch Gen Psychiatry. (1999) 56:600–6. doi: 10.1001/archpsyc.56.7.600
6. Hemmingsson E, Johansson K, Reynisdottir S. Effects of childhood abuse on adult obesity: a systematic review and meta-analysis. Obes Rev. (2014) 15:882–93. doi: 10.1111/obr.12216
7. Suglia SF, Clark CJ, Boynton-Jarrett R, Kressin NR, Koenen KC. Child maltreatment and hypertension in young adulthood. BMC Public Health. (2014) 14:1149. doi: 10.1186/1471-2458-14-1149
8. Brown DW, Anda RF, Tiemeier H, Felitti VJ, Edwards VJ, Croft JB, et al. Adverse childhood experiences and the risk of premature mortality. Am J Prev Med. (2009) 37:389–96. doi: 10.1016/j.amepre.2009.06.021
9. Currie J, Widom CS. Long-term consequences of child abuse and neglect on adult economic well-being. Child Maltreat. (2010) 15:111–20. doi: 10.1177/1077559509355316
10. Bick J, Zhu T, Stamoulis C, Fox NA, Zeanah C, Nelson CA. Effect of early institutionalization and foster care on long-term white matter development: a randomized clinical trial. JAMA Pediatr. (2015) 169:211–9. doi: 10.1001/jamapediatrics.2014.3212
11. Cohen RT, Canino GJ, Bird HR, Celedón JC. Violence, abuse, and asthma in Puerto Rican children. Am J Respir Crit Care Med. (2008) 178:453–9. doi: 10.1164/rccm.200711-1629OC
12. Chae W, Jang J, Park EC, Jang SI. Changes in child abuse experience associated to sleep quality: results of the Korean children & youth panel survey. BMC Public Health. (2021) 21:1210. doi: 10.1186/s12889-021-11309-3
13. Koizumi M, Takagishi H. The relationship between child maltreatment and emotion recognition. PLoS One. (2014) 9:e86093. doi: 10.1371/journal.pone.0086093
14. Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse Negl. (2003) 27:169–90. doi: 10.1016/s0145-2134(02)00541-0
15. Brier J. Trauma Symptom Checklist for Children (TSCC), Professional Manual. Odessa: Psychological Assessment Resources (1996).
16. Achenbach TM. Integrative Guide for the 1991 CBCL/4-18, YSR, and TRF Profiles. Burlington, VT: Department of Psychiatry, University of Vermont (1991).
17. Achenbach TM, Ruffle TM. The child behavior checklist and related forms for assessing behavioral/emotional problems and competencies. Pediatrics. (2000) 21:265–71. doi: 10.1542/pir.21-8-265
18. Sackl-Pammer P, Özlü-Erkilic Z, Jahn R, Karwautz A, Pollak E, Ohmann S, et al. Somatic complaints in children and adolescents with social anxiety disorder. Neuropsychiatr. (2018) 32:187–95. doi: 10.1007/s40211-018-0288-8
19. Ercan ES, Kutlu A, Cıkoğlu S, Veznedaroğlu B, Erermiş S, Varan A. Risperidone in children and adolescents with conduct disorder: a single-center, open-label study. Curr Ther Res Clin Exp. (2003) 64:55–64. doi: 10.1016/S0011-393X(03)00006-7
20. Suzuki H, Tomoda A. Roles of attachment and self-esteem: impact of early life stress on depressive symptoms among Japanese institutionalized children. BMC Psychiatry. (2015) 15:8. doi: 10.1186/s12888-015-0385-1
21. Fujisawa TX, Nishitani S, Takiguchi S, Shimada K, Smith AK, Tomoda A. Oxytocin receptor DNA methylation and alterations of brain volumes in maltreated children. Neuropsychopharmacol. (2019) 44:2045–53. doi: 10.1038/s41386-019-0414-8
22. Nishitani S, Fujisawa TX, Hiraoka D, Makita K, Takiguchi S, Hamamura S, et al. A multi-modal MRI analysis of brain structure and function in relation to OXT methylation in maltreated children and adolescents. Transl Psychiatry. (2021) 11:589. doi: 10.1038/s41398-021-01714-y
23. Itani T, Kanbayashi Y, Nakata Y, Kita M, Fujii H, Kuramoto H. Standardization of the Japanese version of the child behavior checklist/4–18. Psychiatr Neurol Paediatr Jpn. (2001) 41:243–52.
24. Fujisawa TX, Shimada K, Takiguchi S, Mizushima S, Kosaka H, Teicher MH, et al. Type and timing of childhood maltreatment and reduced visual cortex volume in children and adolescents with reactive attachment disorder. NeuroImage Clin. (2018) 20:216–21. doi: 10.1016/j.nicl.2018.07.018
25. Strobl C, Boulesteix AL, Zeileis A, Hothorn T. Bias in random forest variable importance measures: illustrations, sources and a solution. BMC Bioinformatics. (2007) 8:25. doi: 10.1186/1471-2105-8-25
28. R Core Team. R: A Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing (2024). https://www.R-project.org/ (accessed August 13, 2024).
29. Knowles JE. eeptools: Convenience Functions for Education Data. (2023). Available at: https://CRAN.R-project.org/package=eeptools (accessed August 13, 2024).
30. Zeileis A, Hothorn T. Diagnostic checking in regression relationships. R News. (2002). Available at: https://CRAN.R-project.org/doc/Rnews/ (accessed August 13, 2024).
31. Rosseel Y. Iavaan: an R package for structural equation modeling. J Stat Softw. (2012) 48:1–36. doi: 10.18637/jss.v048.i02
32. Carstensen B, Plummer M, Laara E, Hills M. Epi: A Package for Statistical Analysis in Epidemiology. (2024). Available at: https://CRAN.R-project.org/package=Epi (Accessed August 13, 2024).
33. Lumley T, Miller A. leaps: Regression Subset Selection. (2024). Available at: https://CRAN.R-project.org/package=leaps (Accessed February 14, 2025).
34. Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez JC, et al. pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinform. (2011) 12:77. doi: 10.1186/1471-2105-12-77
36. Hothorn T, Bühlmann P, Dudoit S, Molinaro A, van der Laan MJ. Survival ensembles. Biostatistics. (2006) 7:355–73. doi: 10.1093/biostatistics/kxj011
37. Hothorn T, Hornik K, Zeileis A. Unbiased recursive partitioning: a conditional inference framework. J Comput Graph Stat. (2006) 15:651–74. doi: 10.1198/106186006X133933
38. Strobl C, Boulesteix AL, Kneib T, Augustin T, Zeileis A. Conditional variable importance for random forests. BMC Bioinform. (2008) 9:307. doi: 10.1186/1471-2105-9-307
39. Zeileis A, Hothorn T, Hornik K. Model-based recursive partitioning. J Comput Graph Stat. (2008) 17:492–514. doi: 10.1198/106186008X319331
40. Ivarsson T, Larsson B. The obsessive-compulsive symptom (OCS) scale of the child behavior checklist: a comparison between Swedish children with obsessive-compulsive disorder from a specialized unit, regular outpatients and a school sample. J Anxiety Disord. (2008) 22:1172–9. doi: 10.1016/j.janxdis.2007.12.004
41. Simeonova DI, Nguyen T, Walker EF. Psychosis risk screening in clinical high-risk adolescents: a longitudinal investigation using the child behavior checklist. Schizophr Res. (2014) 159:7–13. doi: 10.1016/j.schres.2014.07.046
42. Ou W, Li Z, Zheng Q, Chen W, Liu J, Liu B, et al. Association between childhood maltreatment and symptoms of obsessive-compulsive disorder: a meta-analysis. Front Psychiatry. (2020) 11:612586. doi: 10.3389/fpsyt.2020.612586
43. Brown SM, Rodriguez KE, Smith AD, Ricker A, Williamson AA. Associations between childhood maltreatment and behavioral sleep disturbances across the lifespan: a systematic review. Sleep Med Rev. (2022) 64:101621. doi: 10.1016/j.smrv.2022.101621
44. Gruber R, Michaelsen S, Bergmame L, Frenette S, Bruni O, Fontil L, et al. Short sleep duration is associated with teacher-reported inattention and cognitive problems in healthy school-aged children. Nat Sci Sleep. (2012) 4:33–40. doi: 10.2147/NSS.S24607
45. Alfano CA, Zakem AH, Costa NM, Taylor LK, Weems CF. Sleep problems and their relation to cognitive factors, anxiety, and depressive symptoms in children and adolescents. Depress Anxiety. (2009) 26:503–12. doi: 10.1002/da.20443
46. Swain MS, Henschke N, Kamper SJ, Gobina I, Ottová-Jordan V, Maher CG. An international survey of pain in adolescents. BMC Public Health. (2014) 14:447. doi: 10.1186/1471-2458-14-447
47. Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd ed. New York: Wiley (2000). doi: 10.1002/0471722146
48. Feldman HM. How young children learn language and speech. Pediatr Rev. (2019) 40:398–411. doi: 10.1542/pir.2017-0325
49. Manuela V, Santos AJ, Fernandes C, Shin N, Vaughn BE, Nio JS. Associations between attachment security and social competence in preschool children. Merrill Palmer Q. (2014) 60:80–99. doi: 10.1353/mpq.2014.a538697
50. Lu HH, Tsao FM, Tsai JD. Behavioral problems of mandarin-speaking late-talking toddlers and preschool aged children: a prospective case-control study in Taiwan. Medicine. (2020) 99: e23341. doi: 10.1097/MD.0000000000023341
51. Nitin R, Shaw DM, Rocha DB, Walters CE Jr, Chabris CF, Camarata SM, et al. Association of developmental language disorder with comorbid developmental conditions using algorithmic phenotyping. JAMA Netw Open. (2022) 5:e2248060. doi: 10.1001/jamanetworkopen.2022.48060
52. Tomoda A, Suzuki H, Rabi K, Sheu YS, Polcari A, Teicher MH. Reduced prefrontal cortical gray matter volume in young adults exposed to harsh corporal punishment. Neuroimage. (2009) 47(2):T66–71. doi: 10.1016/j.neuroimage.2009.03.005
53. Lansford JE, Miller-Johnson S, Berlin LJ, Dodge KA, Bates JE, Pettit GS. Early physical abuse and later violent delinquency: a prospective longitudinal study. Child Maltreat. (2007) 12:233–25. doi: 10.1177/1077559507301841
54. Dye HL. Is emotional abuse as harmful as physical and/or sexual abuse? J Child Adolesc Trauma. (2020) 13:399–407. doi: 10.1007/s40653-019-00292-y
55. Boger S, Ehring T, Berberich G, Werner GG. Impact of childhood maltreatment on obsessive-compulsive disorder symptom severity and treatment outcome. Eur J Psychotraumatol. (2020) 11:1753942. doi: 10.1080/20008198.2020.1753942
Keywords: child abuse, child behavior checklist, childhood maltreatment, ROC curve analysis, sensitive analyses
Citation: Makino T, Nishitani S, Takiguchi S, Yao A, Fujisawa TX and Tomoda A (2025) Assessing childhood maltreatment exposure using the child behavior checklist. Front. Child Adolesc. Psychiatry 4:1493432. doi: 10.3389/frcha.2025.1493432
Received: 9 September 2024; Accepted: 21 April 2025;
Published: 8 May 2025.
Edited by:
Paolo Meneguzzo, University of Padua, ItalyReviewed by:
Sonia S. Sousa, University of Minho, PortugalAlberta Mereu, Maggiore Carlo Alberto Pizzardi Hospital, Italy
Copyright: © 2025 Makino, Nishitani, Takiguchi, Yao, Fujisawa and Tomoda. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shota Nishitani, bnNob3RhQHUtZnVrdWkuYWMuanA=; Akemi Tomoda, YXRvbW9kYUB1LWZ1a3VpLmFjLmpw
 Takuya Makino
Takuya Makino Shota Nishitani
Shota Nishitani Shinichiro Takiguchi
Shinichiro Takiguchi Akiko Yao
Akiko Yao Takashi X. Fujisawa
Takashi X. Fujisawa Akemi Tomoda
Akemi Tomoda