- 1Behavioral Health Services, Denver Health and Hospital Authority, Denver, CO, United States
- 2Department of Psychiatry, University of Colorado School of Medicine, Aurora, CO, United States
Background: Despite known risks of substance use, mortality following adolescent substance treatment has not been examined. Knowing which youth have greatest risk and how youth die may inform future interventions.
Methods: This retrospective chart review combined records from a single adolescent substance treatment program at an urban, safety-net health system (n = 2,957, ages 10–19 years) with a public health registry of deaths from 2003 to 2024. Records from the child mental health treatment program at the same health system (n = 4,400, ages 10–19 years) were used for comparison. The crude mortality rate per 100 person years was calculated for both samples for all 21 years. The standard mortality rate using death within one year of intake was also calculated. Finally, a logistic regression model was used to test the project hypotheses that self-identification as a person of color, no engagement in care, male sex at birth, and involvement in substance treatment would predict mortality.
Results: Overall, 92 (2.1%) adolescents in mental health treatment had a death record compared to 119 (4.0%) of adolescents in substance treatment. The crude mortality rate per 100 person years for adolescents in mental health treatment was 0.19 (CI: 0.18–0.20) compared to 0.37 (CI: 0.36–0.38) for adolescents in substance treatment. The standard mortality rate was 120 (32.7–308) for adolescents in mental health treatment compared to the standardized mortality rate of 944 (CI: 599–1,420) for adolescents in substance treatment. Accidental death, which includes overdose, was the most common cause of death in both groups. Results of the logistic regression showed male sex at birth (p = 0.0434, OR = 2.10, CI 1.06–4.53) and substance treatment (p = 0.0035, OR = 3.02, CI 1.47–6.55) as predictors of death within 5 years of treatment intake.
Conclusions: Adolescents in substance treatment compared to those in mental health treatment are more likely to die within 5 years of intake. Males compared to females are also more likely to die. Interventions to prevent overdose and other causes of mortality may be indicated.
Introduction
Substance use disorders (SUD) and psychiatric disorders are the 18th and 22nd leading causes of global death, respectively (1). In the European Union, the mortality rate due to overdose alone is 22.5 deaths per million population aged 15–64 (2). In the United States, three different substances (tobacco, alcohol, and illegal) account for three of the top 10 leading causes of death (3). As a result, death due to these disorders is common and widespread. Consistent with these findings, adolescents seeking psychiatric treatment have elevated risk of mortality. For instance, a study of almost 60,000 adolescents with an inpatient psychiatric admission in the United Kingdom shows a standard mortality rate of 642 (CI: 532–767), with 100 being a reference standard mortality rate (4). Standard mortality is typically defined as the observed number of deaths in a sample divided by the expected number of deaths in a population of similar age and sex multiplied by 100 (4). Therefore, rates greater than 100 indicate greater than average risk of death, and rates less than 100 indicate a lower risk of death compared to the general population. Another sample in Sweden shows that adolescents with either an inpatient or outpatient mental health encounter had a standard mortality rate of 221 (CI: 156–303) (5). Mortality risk factors for adolescents entering mental health treatment include affective disorders, co-occurring substance use, eating disorders, history of psychosis, older age at intake, and school problems (4, 6, 7). Conversely, having an outpatient appointment within 7 days of discharge from an adolescent psychiatric hospital is a protective factor against mortality (8).
Among adolescents, substance use is associated with the leading causes of death, which include accidents and injuries, self-harm, and interpersonal violence (9). Adolescent substance use is also complicated by a high prevalence of co-occurring psychiatric disorders (Dennis et al., 2004) (10). Furthermore, substances such as cannabis are strongly associated with psychiatric symptoms such as psychosis (11–13). Despite the devastating outcomes of adolescent substance use and the known risk of mortality for adolescents in psychiatric treatment more generally, mortality following adolescent substance treatment remains understudied. Most studies focus on adults seeking substance treatment and show an elevated risk of mortality compared to the general population (14, 15). Mortality risk factors for adults in substance treatment include chronic medical illness, homelessness, older age at intake, past suicide attempt, male sex, and alcohol or heroin as a primary substance use disorder diagnosis (16–19). Moreover, for adults in behavioral health treatment, substance use disorders are associated with increased mortality compared to other psychiatric disorders (20). Additionally, in the United States age adjusted mortality from substance use disorders increased significantly from 2000 to 2019, especially for African American and American Indian/Alaska Native populations (14). These groups now experience the highest mortality rates from substance use disorders compared to other racial and ethnic groups (14).
While adolescents in mental health treatment and adults in substance treatment both face elevated risks of mortality, there is a lack of research documenting mortality for adolescents engaging in substance treatment. Investigating this area is important, as it could inform interventions to prevent mortality in this population. Extrapolating from the literature reviewed above, we hypothesize that adolescents in substance treatment have elevated risk of mortality compared to adolescents in mental health treatment and that risk factors for mortality include older age at intake, male sex, and having an ethnic or racial identity with a history of marginalization. We also hypothesize that successful treatment engagement is protective. The objective of this project is to evaluate these hypotheses using data from an adolescent substance treatment program with a 21-year follow-up.
Materials and methods
Overview
This project is a retrospective chart review, which explores mortality following referral to adolescent mental health and substance treatment.
Procedure
All adolescent patients (10–19 years of age) presenting to an urban, safety-net health system in Denver, Colorado, for either mental health or substance treatment between January 2, 2003, and July 8, 2024, were included in the analysis. Data were extracted from the electronic health record for analysis. These data were cross-referenced with a public health database of mortality. The Revised Standards for Quality Improvement Reporting Excellence (SQUIRE 2.0) are used to carry out the project and report its findings (21). The project was reviewed by the Colorado Multiple Institutional Review Board and was determined to be non-human subjects research.
Intervention
All adolescents had at least one appointment in either a state-licensed mental health or substance treatment program. Adolescents who received treatment in both programs were placed in the adolescent substance treatment program to avoid duplication. Treatment included outpatient psychotherapy and/or medication management depending on clinical indication and patient preference.
Measures
Baseline demographic variables were extracted from the electronic health record. These include age at intake, ethnicity, race, sex at birth, and whether adolescents had successful treatment engagement, which is defined by the Healthcare Effectiveness Data and Information Set (HEDIS) as having two or more treatment sessions within 34 days of intake (22). Mortality data included death as a binary variable (yes/no), date of death, and manner of death. Manner of death included the six categories of accidental, homicide, natural, pending, and undetermined. Of note, unintentional overdose is typically categorized as accidental.
Data analysis
Data were analyzed using RStudio (V.2024.04.01) and tidyverse (23). Descriptive statistics are used to characterize the sample. To compare to previous research, a crude mortality rate per 100 person years was calculated for each sample (16). Crude mortality rate is calculated by dividing the number of deaths in the sample by the sum of the years each person in the sample was followed and multiplying by 100 (16). Assuming a Poisson distribution for crude mortality rate, a 95% Confidence Interval (CI) was also calculated. A standardized mortality rate was calculated by dividing observed deaths by expected deaths and multiplying by 100. Expected deaths were calculated by age group (10–14-year-olds, 15–19-year-olds) and sex using published mortality rates for the United States (24). Confidence intervals were calculated assuming Poisson distributions for standard mortality. For formal analyses, ethnicity and race were categorized dichotomously as Black, Indigenous, or Person of Color (BIPOC) or Non-Hispanic White. This dichotomization was done because of shifting standards in the collection of data related to ethnicity and race since 2003 and because of a small sample size of some races. Similarly, sex at birth was categorized as a binary variable (female, male) because of changing standards of reporting sex and gender since 2003. A logistic regression model was used to test the project hypotheses identification as a person of color, no engagement in care, male sex at birth, and involvement in substance treatment would predict mortality. For the logistic regression, the binary outcome of death within 5 years of intake (yes, no) was used as the dependent variable. Therefore, this model used a sub-sample of individuals who sought treatment at least five years before the dataset was created (July 8, 2024). This standardization was chosen to provide meaningful comparison between adolescents in the two programs and to assess outcomes temporally related to treatment.
Results
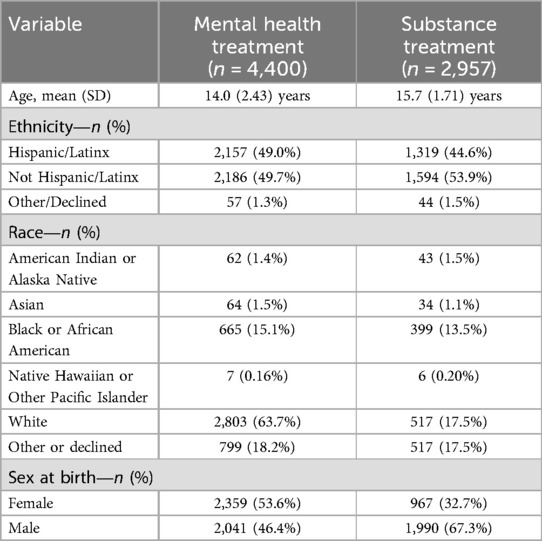
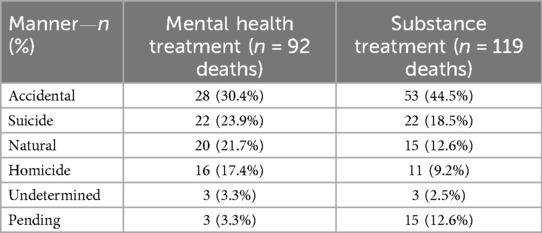
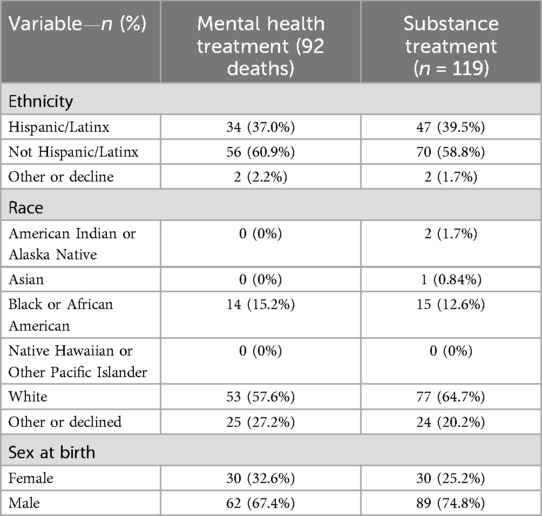
The sample included 4,400 adolescents in mental health treatment and 2,957 adolescents in substance treatment. Table 1 displays the baseline characteristics of the sample. Generally, adolescents in substance treatment were slightly older and were more likely to have male sex at birth compared to adolescents in mental health treatment. The most common substance use disorder diagnoses were cannabis use disorder (n = 2,096, 70.9%, alcohol use disorder (n = −665, 22.5%), stimulant use disorder (n = 424, 14.3%), and opioid use disorder (n = 366, 12.4%). Overall, 92 (2.1%) adolescents in mental health treatment had a death record compared to 119 (4.0%) of adolescents in substance treatment. The crude mortality rate for adolescents in mental health treatment was 0.19 (CI: 0.18–0.20) per 100 person years compared to 0.37 (CI: 0.36–0.38) per 100 person years for adolescents in substance treatment. The standardized mortality rate for adolescents in substance treatment was 120 (32.7–308) for adolescents in mental health treatment compared to 944 (CI: 599–1,420) for adolescents in substance treatment. The manner of death is displayed in Table 2. Accidental death was the most common cause of death in both groups but appears to be slightly more prevalent among adolescents in substance treatment. Table 3 compares deaths by ethnicity, race, and sex at birth. For both groups, death appears to be more common among males.
The project hypotheses were tested with a logistic regression using the independent variables of age, engagement in care, dichotomization of race and ethnicity as BIPOC or Non-Hispanic/White, sex at birth, and whether the adolescent was in mental health or substance treatment. This analysis included a sub-sample for whom 5-year follow-up data were available (n = 3,188 in mental health treatment and n = 2,331 in substance treatment). Twelve adolescents (0.38%) in mental health treatment died within 5 years of intake, and 32 adolescents in substance treatment died within 5 years of intake. Results of the logistic regression showed male sex at birth (p = 0.0434, OR = 2.10, CI 1.06–4.53) and substance treatment (p = 0.0035, OR = 3.02, CI 1.47–6.55) as predictors of death within 5 years of treatment intake. Age at intake, engagement in care, and race/ethnicity were not statistically associated with death within 5 years.
Discussion
This retrospective review finds that 0.38% of adolescents in mental health treatment and 1.4% of adolescents in substance treatment died within 5 years of intake. Having male sex and enrollment in substance treatment were significant predictors of mortality. This project did not find ethnicity, race, or treatment engagement as significant predictors of death. The most common cause of death was accidental, including unintentional overdose, followed by suicide.
The study has several limitations. First, its use of a single site limits the generalizability of the findings. Future research is needed to evaluate our findings in other geographical locations. Second, as a retrospective review, the study is susceptible to potential confounds. Finally, standards for collecting demographic variables, such as ethnicity, race, and sex have evolved since the data collection began in 2003.
In context, these data show a crude mortality rate of 0.37 per 100 person years for adolescents in substance treatment compared to crude mortality rates ranging from 0.30 to 1.48 per 100 person years (depending on primary substance diagnosis) for a national sample of all patients entering substance treatment in New Zealand (16). Our data show a standardized mortality rate of 944 for adolescents in substance treatment compared to previous findings of a standard mortality rate of 642 for adolescents with an inpatient psychiatric admission and 221 for adolescents with either an inpatient or outpatient mental health encounter (4). Our finding that males compared to females have greater mortality risk is also consistent with previous findings in other populations in substance treatment (17). Therefore, our data are generally consistent with previous reports and suggest that adolescents in substance treatment carry increased mortality risk compared to adolescents in treatment for other psychiatric disorders. However, our finding that ethnicity and race did not predict mortality is not consistent with previously documented disparities (14). Perhaps, the shifting effects by ethnicity and race of the different waves of the opioid overdose epidemic account for this inconsistency (25).
These data are important because they suggest that adolescents in substance treatment may benefit from interventions to reduce their mortality. Given that the leading cause of death was accidental, which includes overdose, harm reduction approaches such as encouraging adolescents to use designated drivers, carry naloxone, use fentanyl testing strips, and avoid using substances alone may be beneficial. Since suicide and homicide were also significant contributors to death, interventions that address gun violence could be helpful. Using Learning Health System approaches to implement and sustain evidence-based suicide interventions into substance treatment such as the Collaborative Assessment and Management of Suicidality (CAMS) could also be an important future direction (26). Finally, adolescent males in substance treatment may benefit from targeted screening and interventions aimed at reducing mortality. Future directions could include an evaluation of our findings in different locations and with different populations to inform future population-based prevention efforts.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Colorado Multiple Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
CT: Funding acquisition, Methodology, Writing – original draft, Supervision, Conceptualization, Formal analysis, Writing – review & editing. CE: Writing – review & editing, Data curation. EC: Data curation, Validation, Writing – review & editing. HS: Writing – review & editing, Validation, Data curation. RL: Formal analysis, Validation, Conceptualization, Data curation, Supervision, Methodology, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This project was funded by the Denver Health Foundation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Correction Note
A correction has been made to this article. Details can be found at: 10.3389/frcha.2025.1656174.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Institute for Health Metrics and Evaluation (IHME). Global burden of disease 2021: findings from the GBD 2021 Study (2024).
2. European Monitoring Centre for Drugs and Drug Addiction. European drug report 2024: trends and Developments (2024).
3. Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. J Am Med Assoc. (2004) 291:1238–45. doi: 10.1001/jama.291.10.1238
4. James A, Clacey J, Seagroatt V, Goldacre M. Adolescent inpatient psychiatric admission rates and subsequent one-year mortality in England: 1998–2004. J Child Psychol Psychiatry. (2010) 51(12):1395–404. doi: 10.1111/j.1469-7610.2010.02293.x
5. Engqvist U, Rydelius PA. Death and suicide among former child and adolescent psychiatric patients. BMC Psychiatry. (2006) 6:1–11. doi: 10.1186/1471-244X-6-51
6. Astrup H, Myhre M, Kildahl AT, Walby FA. Suicide after contact with child and adolescent mental health services—a national registry study. Front Psychiatry. (2022) 13:886070. doi: 10.3389/fpsyt.2022.886070
7. Simon GE, Stewart C, Yarborough BJ, Lynch F, Coleman KJ, Beck A, et al. Mortality rates after the first diagnosis of psychotic disorder in adolescents and young adults. JAMA Psychiatry. (2018) 75(3):254–60. doi: 10.1001/jamapsychiatry.2017.4437
8. Fontanella CA, Warner LA, Steelesmith DL, Brock G, Bridge JA, Campo JV. Association of timely outpatient mental health services for youths after psychiatric hospitalization with risk of death by suicide. JAMA Netw Open. (2020) 3(8):e2012887. doi: 10.1001/jamanetworkopen.2020.12887
9. World Health Organization. Adolescent and young adult health (2024). Available at: https://www.who.int/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions (Accessed March 21, 2025).
10. Dennis M, Godley SH, Diamond G, Tims FM, Babor T, Donaldson J, et al. The Cannabis youth treatment (CYT) study: main findings from two randomized trials. J Subst Abuse Treat. (2004) 27(3):197–213. doi: 10.1016/j.jsat.2003.09.005
11. Ricci V, Ciavarella M, Marrangone C, Messas G, Maina G, Martinottie G. Modern perspectives on psychoses: dissociation, automatism, and temporality across exogenous and endogenous dimensions. Front Psychiatry. (2025) 16:1543673. doi: 10.3389/fpsyt.2025.1543673
12. Sarni A, Martinotti G, Maina G, Ricci V. Lysergic psychoma and mental automatism: a clinical exploration of synthetic psychosis. Riv Psychiatr. (2025) 16:4487. doi: 10.1708/4487.44875
13. Ricci V, Chiappini S, Martinotti G, Maina G. Cannabis use and psychotic-like experiences: a systematic review of biological vulnerability, potency effects, and clinical trajectories. Psychiatry Res. (2025) 348:116496. doi: 10.1016/j.psychres.2025.116496
14. Bhagavathula AS, Daglis T, Nishimura Y. Trends in racial/ethnic and geographic disparities in substance use disorders mortality in the United States, 2000–2019. Am J Addict. (2024) 34:93–100. doi: 10.1111/ajad.13654
15. Formánek T, Krupchanka D, Mladá K, Winkler P, Jones PB. Mortality and life-years lost following subsequent physical comorbidity in people with pre-existing substance use disorders: a national registry-based retrospective cohort study of hospitalised individuals in Czechia. Lancet Psychiatry. (2022) 9(12):957–68. doi: 10.1016/S2215-0366(22)00335-2
16. Havard A, Jones N, Bharat C, Gisev N, Pearson SA, Shakeshaft A, et al. Mortality during and after specialist alcohol and other drug treatment: variation in rates according to principal drug of concern and treatment modality. Drug Alcohol Rev. (2023) 42(6):1461–71. doi: 10.1111/dar.13669
17. Ledberg A, Reitan T. Increased risk of death immediately after discharge from compulsory care for substance abuse. Drug Alcohol Depend. (2022) 236:109492. doi: 10.1016/j.drugalcdep.2022.109492
18. Saitz R, Gaeta J, Cheng DM, Richardson JM, Larson MJ, Samet JH. Risk of mortality during four years after substance detoxification in urban adults. J Urban Health. (2007) 84(2):272–82. doi: 10.1007/s11524-006-9149-z
19. Satre DD, Mertens JR, Areán PA, Weisner C. Five-year alcohol and drug treatment outcomes of older adults versus middle-aged and younger adults in a managed care program. Addiction. (2004) 99(10):1286–97. doi: 10.1111/j.1360-0443.2004.00831.x
20. Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. (2014) 13(2):153–60. doi: 10.1002/wps.20128
21. Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. SQUIRE 2.0 (standards for quality improvement reporting excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf. (2016) 25(12):501–7. doi: 10.1136/bmjqs-2015-004411
22. National Committee for Quality Assurance. HEDIS my measure descriptions (2024). Available at: https://wpcdn.ncqa.org/www-prod/wp-content/uploads/HEDIS-MY-2025-Measure-Description.pdf (Accessed June 16, 2025).
25. Alexander MJ, Kiang MV, Barbieri M. Trends in black and white opioid mortality in the United States, 1979–2015. Epidemiology. (2018) 29(5):707–15. doi: 10.1097/EDE.0000000000000858
Keywords: adolescent, mental health, mortality, substance misuse, treatment
Citation: Thurstone C, Etzig C, Chen E, Seely HD and Loh R (2025) Mortality following adolescent substance treatment: 21-year follow-up from a single clinical site. Front. Child Adolesc. Psychiatry 4:1600101. doi: 10.3389/frcha.2025.1600101
Received: 25 March 2025; Accepted: 11 June 2025;
Published: 20 June 2025;
Corrected: 14 July 2025.
Edited by:
Valerio Ricci, San Luigi Gonzaga University Hospital, ItalyReviewed by:
Stefania Chiappini, Saint Camillus International University of Health and Medical Sciences, ItalyAngel Puig-Lagunes, Universidad Veracruzana, Mexico
Copyright: © 2025 Thurstone, Etzig, Chen, Seely and Loh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christian Thurstone, Y2hyaXN0aWFuLnRodXJzdG9uZUBkaGhhLm9yZw==
 Christian Thurstone
Christian Thurstone Cassandra Etzig1
Cassandra Etzig1 Eileen Chen
Eileen Chen