- 1National University of Singapore Graduate School for Integrative Sciences and Engineering, National University of Singapore, Singapore, Singapore
- 2Saw Swee Hock School of Public Health, National University of Singapore and National University Health System, Singapore, Singapore
- 3Division of Advanced Internal Medicine, National University Hospital, Singapore, Singapore
- 4Group Chief Technology Office, National University Health System Singapore, Singapore, Singapore
Introduction
Singapore's healthcare system is in the process of transformation. From country-wide vaccination programmes started during Singapore's independence focusing on infectious diseases (1), to the establishment of polyclinics, general hospitals, and specialist centers to address chronic disease management, to the current COVID-19 pandemic (2), healthcare challenges are constantly evolving. Although Singapore has excellent healthcare outcomes with an average life expectancy increased over the years (3), we face the combined challenge of rising healthcare costs, aging population with an increasing burden of chronic diseases and shortage of healthcare professionals. Diabetes alone is projected to affect more than 1 million people by 2050, more than double compared to 2014 (4).
To overcome these challenges, Singapore needs to transform the way it delivers care. The Ministry of Health Singapore (MOH) has framed the healthcare transformation using the “3 Beyonds” strategy—“Beyond Healthcare to Health, Beyond Hospital to Community, Beyond Quality to Value” (5). “Beyond Healthcare to Health” involves strategies to promote the early detection of chronic diseases and prevent diseases with healthy lifestyles. “Beyond Hospital to Community” drives a shift in care from the hospital to primary care and then to the home, enabling aging in place at home. “Beyond Quality to Value” strives for improved efficiency to achieve better outcomes while lowering costs and reducing waste. The explosive increase in the amounts of healthcare data, along with the improved performance of Artificial Intelligence (AI) is poised as a transformational force in healthcare.
First of all, AI tools have demonstrated the capability to enable the creation and delivery of better management services to deal with chronic diseases. Many research groups have investigated the application of AI to control blood glucose for diabetes mellitus (DM) (6–9). Many of them have been tested using virtual patients or simulations. For example, Mauseth et al. (6) designed an AI-based controller, namely fuzzy logic controller (FLC) to personalize glycemic control by determining the dosing of insulin on artificial pancreas. Daskalaki et al. (7) presented an adaptive, patient-specific blood glucose control strategy based on the another AI approach called reinforcement learning, and tested their approach on 28 virtual type-1 DM patients. Their results suggested that the AI approach could improve nocturnal blood glucose control without increasing the risk of hypoglycaemia.
Secondly, AI could also be used as a digital health coaching tool that help patients to manage their conditions at home. AI has empowered chatbots to provide virtual assistance to patients and answer simple questions about their condition. For example, Stein et al. (10) developed a pure AI-driven fully automated conversational health coaching mobile application for obese adults. Their results showed that the AI application could help the participants to achieve weight loss comparable to in-person lifestyle interventions. Other researchers have developed “AI doctors” that provide health advice directly to patients with common symptoms, freeing up primary care access for more complex care (11). A survey conducted on 800 European and American patients with atrial fibrillation, Type 2 diabetes or breast cancer found that while many patients did not want their doctors replaced by AI, most of them were happy with a round-the-clock virtual assistance from an AI agent (12).
Last but not least, AI could help to improve accuracy and efficiency of disease diagnosis. The AI-powered algorithms for diagnosing disease is now outperforming physicians in detecting skin cancer (12), breast cancer (13), and brain tumors (14). Besides, AI can also help to quickly process large volumes of both unstructured and structured data including past medical history, continuous physiologic signals (such as vital signs), laboratory results, genomics data, imaging reports, and many others. As a result, the physicians can better focus on more complex cases and improve the efficiency of diagnosis.
AI-based approaches could empower individuals to take charge of their health as well as enhance the quality and accessibility of care. It would be a powerful force for the healthcare transformation if it is implemented wisely. Poorly implemented AI applications in healthcare would lead to extra burdens and increased risks for both patients and physicians. Therefore, it is extremely important to make sure all the AI-based approaches are validated by clinical proof-of-concepts (POC) before entering large clinical trials and implementing to clinical workspaces. Hence, we propose “healthcare datathon” as a testbed for clinical POC and a pilot for the development of strategies to deal with real clinical problems.
Healthcare Datathon
The word datathon is a portmanteau for a data hackathon, which is originated from technology companies as internal events for engineers and computer scientists to collaborate, brainstorm, and build innovative solutions to challenging, company-wide problems in a concentrated period of time (15). Thereafter, the datathon model has been adapted to other domains to address problems with broader interests rather than company-exclusive problems. In particular, a healthcare datathon bring together interdisciplinary teams of students and professionals from both technical and healthcare domain to collaborate, brainstorm, and build solutions to unmet clinical needs.
The goal of a healthcare datathon is to enhance collaboration among participants from various backgrounds to produce clinically relevant research that relies on sound statistical rigor and adequate data samples. It features an iterative process of idea elaboration and group learning among individuals with different types and levels of expertise in a mutually supportive environment.
Healthcare datathon is usually an annual event which spans 2–3 days and follows a 6-stage process illustrated in Figure 1. (1) Problem identification: clinical needs/questions are presented to participants by healthcare professionals. (2) Team formation: interdisciplinary teams are formed around the clinical question by healthcare professionals, computer scientists, statisticians, and other data enthusiasts. (3) Working with data: data extraction, cleaning, and processing are performed by team members from technical background. All teams share a common clinical database. (4) Analysis and hypothesis testing: teams brainstorm the solutions to the clinical question and conduct analysis to verify their hypothesis. (5) Result presentation: teams present their ideas and results to judges and the all the participants. (6) Research project formalization: if a clinical solution or a hypothesis is validated through stage (1)–(5), teams can formalize the clinical question to a research project, and continue to work on the project after the healthcare datathon.
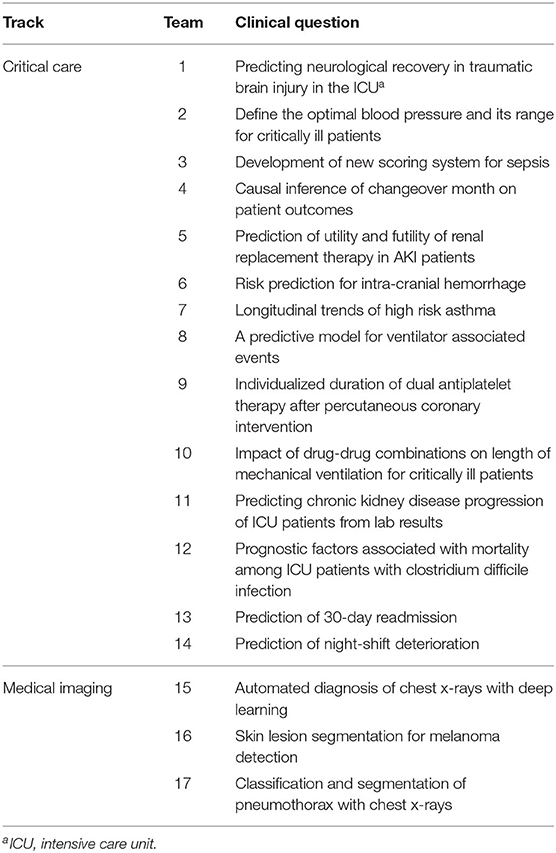
A real practice of healthcare datathon, named, “Healthcare AI Datathon and Expo,” was organized in Singapore on July 6–8, 2019 (event videos and the participants information and can be referenced in the Supplementary Material). The clinical questions were proposed by physicians in a local hospital and were later revised by clinical researchers to verify their relevance and feasibility of developing a solution. In total, 17 questions were selected and categorized into two tracks: Critical Care and Medical Imaging (Table 1). Following the 6-stage process of datathon, clinical leads first pitched their clinical questions to rest of the participants and then were instructed to form teams on their own. All participating teams were then given 2 days to solve their clinical questions and were mentored by data experts and clinical professionals. At the end of the event, all 17 projects were completed within the event timeline. Teams presented their results to a judging panel of data scientists and clinical experts, who selected the champion projects and provided feedbacks and suggestions for future work to individual teams. In the last stage, teams with promising results would continue their project, and transform it into academic research.
Discussion
The healthcare datathon that organized in Singapore in 2019 brought together a diverse group of participants with wide-ranging domains of expertise. The event attracted more than 200 participants from over 8 countries, including healthcare workers from local hospitals, academic researchers and students from local and overseas universities, and various data scientists from industry. The majority of participants (56%) had backgrounds in data science, others were healthcare professionals (28%), and graduates (5%) and undergraduate (11%) students from science and engineering faculties in local universities. With media exposure and industry-wise collaborations, we observed an increased number of participants with a diversity of backgrounds compared to the past events. The clinical questions in datathon can be roughly classified into 4 types: the prediction of disease progressions (n = 9, 53%); analysis of the treatments' impact on patient outcomes (n = 3, 18%); training of automated AI tool for disease diagnosis (n = 3, 18%); and development of new clinical definition/guideline for disease management (n = 2, 12%). Among all the teams in healthcare datathon over the years, we found that on average, 10% of teams remained active after the event. They were able to formalize their clinical problems into research projects and produce impactful publications (16–19). For example, van den Boom et al. (16) were a group of researchers who participated in healthcare datathon 2018 in Singapore and formed a research team to study the optimal oxygen saturation target for critically ill patients. Upon the completion of datathon, they identified a potential optimal ranges of SpO2 among patients requiring oxygenation therapy. Working collaboratively among the health professionals and data scientists in the group, van den Boom et al. managed to validate their proposed optimal range in two large public electronic medical records databases (20, 21) and published their findings. Their research project were successfully conducted and translated into clinical knowledge. Later, their findings were studied and referenced by many other researchers in the field (22–24), and had potential to impact real clinical practice during the pandemic by guiding the respiratory support for critically ill patients with COVID-19 (22, 24).
Healthcare datathon can benefit AI-based clinical research in several ways. First of all, healthcare datathon is served as a testbed and a clinical POC to validate ideas and hypothesis. By analyzing the real-world clinical data, healthcare datathon encourages effective discussion between healthcare professionals and data scientists to validate and prototype clinical problems with solutions over the course of the event. Secondly, healthcare datathon is a collaborative event that assemble interdisciplinary teams of experts with medical, engineering, business background, so that the team could develop interdisciplinary solution to the unmet clinical needs while drawing upon best practices from the technology industry. Thirdly, healthcare datathon provides a great opportunity for participants to exchange ideas and gain valuable research experience. Some participants may also find datathon beneficial for their own research by getting inspiration from projects presented by other teams. Last but not the least, healthcare datathon is an effective platform to build teams with common research interest and diverse expertise. Therefore, clinical problems can be smoothly formalized to research projects, and translate to clinical knowledge.
Summary Findings and Conclusion
• Singapore's healthcare landscape is evolving toward holistic, longitudinal, preventive, and individualized care.
• Artificial Intelligence (AI) has the potential to help in individualizing and improving prevention, diagnosis, and treatment for healthcare transformation.
• In particular, the “healthcare datathon” can be used as an effective model to testbed clinical POC with real clinical problems.
The healthcare datathon was an effective platform to bring together people with various backgrounds and expertise. For data scientists, the event provided them with an opportunity to work with clinicians, understand the clinical questions in-depth and apply their skills on real health data. For physicians, the datathon afforded them access to both data and analytic expertise. The event demonstrated an effective method of promoting the cross-discipline collaboration that is needed to transform the healthcare culture in Singapore.
Author Contributions
SL, KN, and MF contributed to the initiation and the discussion of the research topic. SL, QK, KH, KN, and MF contributed to the analysis of the contents and to the writing of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
SL was funded by the National University of Singapore Graduate School for Integrative Sciences and Engineering Scholarship. This research was supported by the National University Health System joint grant (WBS R-608-000-199-733) and the National Medical Research Council health service research grant (HSRG-OC17nov004).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fdgth.2020.592121/full#supplementary-material
References
1. Bai Y, Shi C, Li X, Liu F. Healthcare System in Singapore. New York, NY: Columbia University (2012).
2. Lee VJ, Chiew CJ, Khong WX. Interrupting transmission of COVID-19: lessons from containment efforts in Singapore. J Travel Med. (2020) 27:taaa039. doi: 10.1093/jtm/taaa039
3. Ong HL, Abdin E, Chua BY, Zhang Y, Seow E, Vaingankar JA, et al. Hand-grip strength among older adults in Singapore: a comparison with international norms and associative factors. BMC Geriatr. (2017) 17:176. doi: 10.1186/s12877-017-0565-6
4. Phan TP, Alkema L, Tai ES, Tan KH, Yang Q, Lim W-Y, et al. Forecasting the burden of type 2 diabetes in Singapore using a demographic epidemiological model of Singapore. BMJ Open Diabetes Res Care. (2014) 2:e000012. doi: 10.1136/bmjdrc-2013-000012
5. Khalik S. The'3 Beyonds': Singapore's strategy to sustain quality healthcare as demand rises. The Straits Times (2017). p. 30.
6. Mauseth R, Wang Y, Dassau E, Kircher R Jr, Matheson D, Zisser H, et al. Proposed clinical application for tuning fuzzy logic controller of artificial pancreas utilizing a personalization factor. J Diabetes Sci Technol. (2010) 4:913–22. doi: 10.1177/193229681000400422
7. Daskalaki E, Diem P, Mougiakakou SG. An actor–critic based controller for glucose regulation in type 1 diabetes. Comput Methods Programs Biomed. (2013) 109:116–25. doi: 10.1016/j.cmpb.2012.03.002
8. Nimri R, Atlas E, Ajzensztejn M, Miller S, Oron T, Phillip M. Feasibility study of automated overnight closed-loop glucose control under MD-logic artificial pancreas in patients with type 1 diabetes: the DREAM Project. Diabetes Technol Therapeutics. (2012) 14:728–35. doi: 10.1089/dia.2012.0004
9. Dinani ST, Zekri M, Kamali M. Regulation of blood glucose concentration in type 1 diabetics using single order sliding mode control combined with fuzzy on-line tunable gain, a simulation study. J Med Signals Sens. (2015) 5:131. doi: 10.4103/2228-7477.161463
10. Stein N, Brooks K. A fully automated conversational artificial intelligence for weight loss: longitudinal observational study among overweight and obese adults. JMIR Diabetes. (2017) 2:e28. doi: 10.2196/diabetes.8590
11. Razzaki S, Baker A, Perov Y, Middleton K, Baxter J, Mullarkey D, et al. A comparative study of artificial intelligence and human doctors for the purpose of triage and diagnosis. arXiv [Preprint] arXiv:1806.10698 (2018).
12. Winkler JK, Fink C, Toberer F, Enk A, Deinlein T, Hofmann-Wellenhof R, et al. Association between surgical skin markings in dermoscopic images and diagnostic performance of a deep learning convolutional neural network for melanoma recognition. JAMA Dermatol. (2019) 155:1135–41. doi: 10.1001/jamadermatol.2019.1735
13. Liu Y, Kohlberger T, Norouzi M, Dahl GE, Smith JL, Mohtashamian A, et al. Artificial intelligence–based breast cancer nodal metastasis detection: insights into the black box for pathologists. Arch pathol Lab Med. (2019) 143:859–68. doi: 10.5858/arpa.2018-0147-OA
15. Wang JK, Roy SK, Barry M, Chang RT, Bhatt AS. Institutionalizing healthcare hackathons to promote diversity in collaboration in medicine. BMC Med Educ. (2018) 18:269. doi: 10.1186/s12909-018-1385-x
16. van den Boom W, Hoy M, Sankaran J, Liu M, Chahed H, Feng M, et al. The search for optimal oxygen saturation targets in critically ill patients: observational data from large ICU databases. Chest. (2020) 157:566–73. doi: 10.1016/j.chest.2019.09.015
17. Du H, Markus C, Metz M, Feng M, Loh TP. Derivation of outcome-based pediatric critical values. Am J Clin Pathol. (2018) 149:324–31. doi: 10.1093/ajcp/aqx165
18. Zhang VRY, Woo ASJ, Scaduto C, Cruz MTK, Tan YY, Du H, et al. Systematic review on the definition and predictors of severe Clostridiodes difficile infection. J Gastroenterol Hepatol. (2020). doi: 10.1111/jgh.15102
19. Tyler PD, Du H, Feng M, Bai R, Xu Z, Horowitz GL, et al. Assessment of intensive care unit laboratory values that differ from reference ranges and association with patient mortality and length of stay. JAMA Netw Open. (2018) 1:e184521. doi: 10.1001/jamanetworkopen.2018.4521
20. Johnson AE, Pollard TJ, Shen L, Li-Wei HL, Feng M, Ghassemi M, et al. MIMIC-III, a freely accessible critical care database. Sci Data. (2016) 3:1–9. doi: 10.1038/sdata.2016.35
21. Pollard TJ, Johnson AE, Raffa JD, Celi LA, Mark RG, Badawi O. The eICU Collaborative Research Database, a freely available multi-center database for critical care research. Sci Data. (2018) 5:180178. doi: 10.1038/sdata.2018.178
22. Dondorp AM, Hayat M, Aryal D, Beane A, Schultz MJ. Respiratory support in COVID-19 patients, with a focus on resource-limited settings. Am J Trop Med Hyg. (2020) 102:1191–7. doi: 10.4269/ajtmh.20-0283
23. da Silva CM, do Nascimento Andrade A, Nepomuceno B, Xavier DS, Lima E, Gonzalez I, et al. Evidence-based physiotherapy and functionality in adult and pediatric patients with COVID-19. J Hum Growth Dev. (2020) 30:148–55. doi: 10.7322/jhgd.v30.10086
Keywords: healthcare datathon, datathon model, healthcare transformation, artificial intelligence, machine learning
Citation: Liu S, Ko QS, Heng KQA, Ngiam KY and Feng M (2020) Healthcare Transformation in Singapore With Artificial Intelligence. Front. Digit. Health 2:592121. doi: 10.3389/fdgth.2020.592121
Received: 06 August 2020; Accepted: 20 October 2020;
Published: 17 November 2020.
Edited by:
Xi Long, Eindhoven University of Technology, NetherlandsReviewed by:
Xiaorong Ding, University of Oxford, United KingdomCopyright © 2020 Liu, Ko, Heng, Ngiam and Feng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mengling Feng, ZXBoZm1AbnVzLmVkdS5zZw==
 Siqi Liu
Siqi Liu Qianwen Stephanie Ko3
Qianwen Stephanie Ko3 Kee Yuan Ngiam
Kee Yuan Ngiam Mengling Feng
Mengling Feng