- 1Department of Public Health and Hygiene, Faculty of Health Sciences, University of Buea, Buea, Cameroon
- 2Department of Biomedical Sciences, Faculty of Health Sciences, University of Buea, Buea, Cameroon
- 3DigiCare Cameroon Consortium, University of Buea, South West Region, Cameroon
- 4Department of Computer Sciences, Faculty of Sciences, University of Buea, Buea, Cameroon
- 5Department of Women and Gender Studies, Faculty of Social and Management Sciences, University of Buea, Buea, Cameroon
- 6Department of Microbiology and Infectious Diseases, School of Veterinary Medicine and Sciences, University of Ngaoundéré, Ngaoundéré, Cameroon
- 7Department of Genetics and Biostatistics, School of Veterinary Medicine and Sciences, University of Ngaoundéré, Ngaoundéré, Cameroon
- 8Department of Obstetrics and Gynaecology, Faculty of Health Sciences, University of Buea, Buea, Cameroon
- 9Department of Mathematics & Statistics, York University, Toronto, ON, Canada
Background: Artificial Intelligence (AI) in healthcare is rapidly growing in recent years, and has substantially improved the quality of care and health outcomes of patients. Understanding healthcare providers' perception and knowledge of AI in healthcare is crucial for its effective adoption, and its use. This study aimed to determine healthcare providers' awareness, assess their knowledge of healthcare AI, assess their perceived benefits, readiness to adopt AI in healthcare in Limbe and Buea Health Districts.
Methods: A hospital-based cross-sectional study was conducted using a multi-staged sampling technique that recruited participants from seven hospitals in Limbe and Buea Health Districts. A questionnaire designed on koboCollect was used for data collection through face-to-face interviews from 494 participants recruited through a multi-stage sampling technique. The data was analyzed using SPSS version 26 where descriptive statistics and logistic regressions were done to determine the factors associated with readiness to adopt AI in healthcare. A P-value of <0.05 at 95% CI was considered statistically significant.
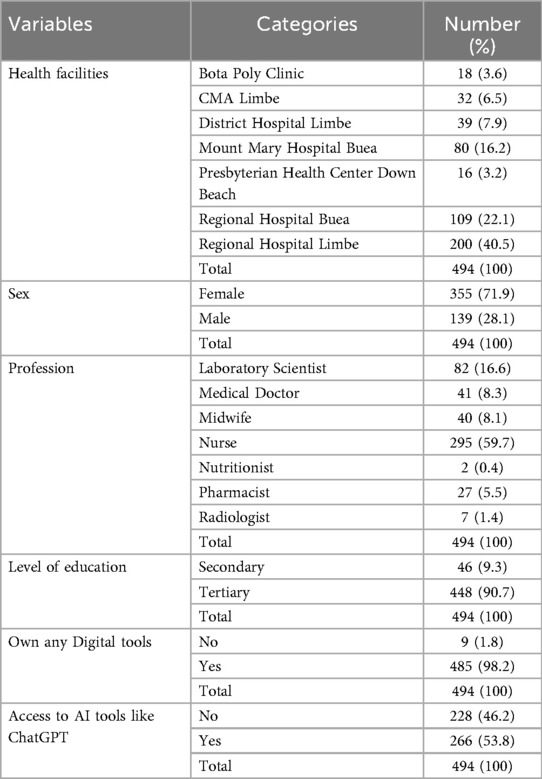
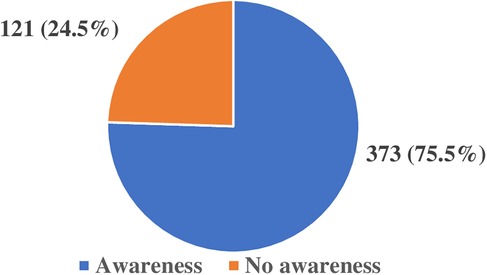
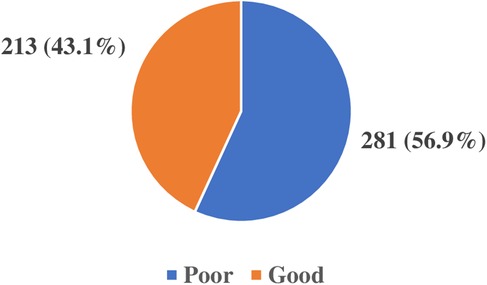
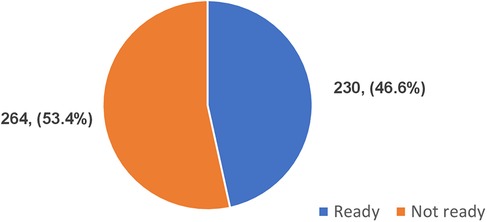
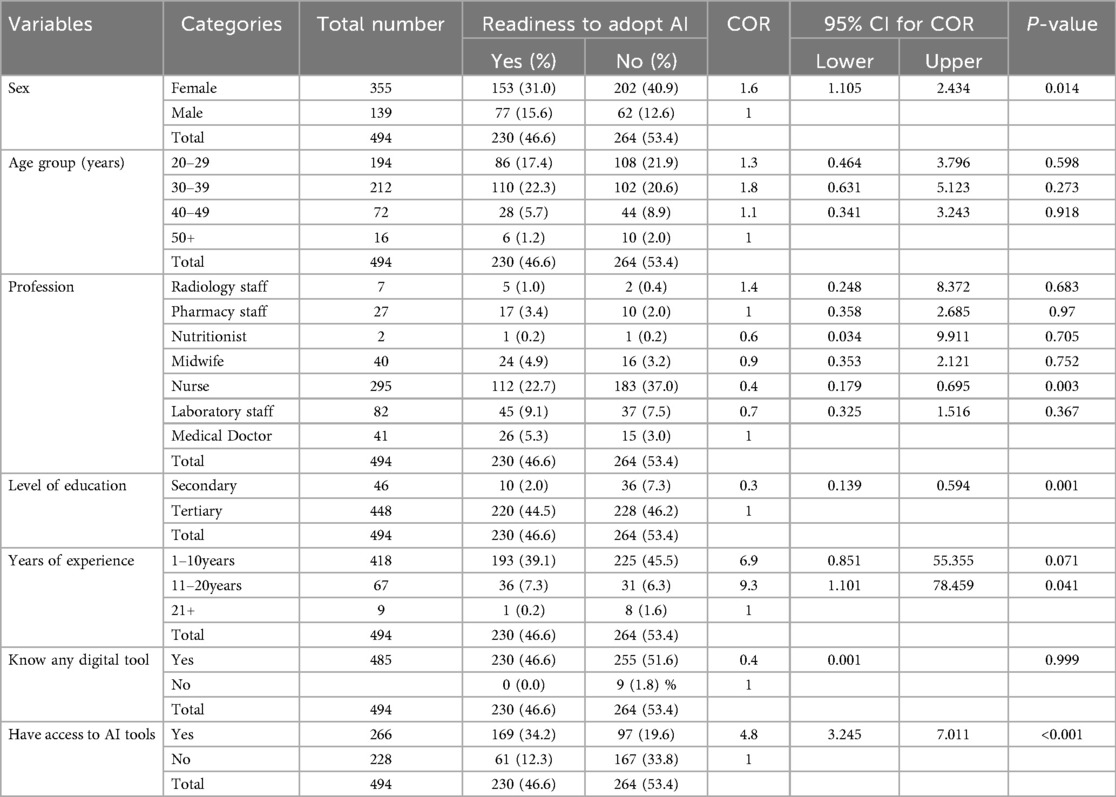
Results: A total of 494 participants were recruited into the study with a mean age of 32.6 ± 7.5 years, the majority 355 (71.9%) were females, 448 (90.7%) had attained tertiary education and the highest proportion 295 (59.7%) were Nurses. The study revealed that 373 (75.5%) were aware of the use of AI in healthcare, 261 (52.8%) had used AI tools, 213 (43.1%) had good knowledge of healthcare AI, 283 (57.3%) had good perception of its benefits and 230 (46.6%) were ready to adopt its use. Those who had access to AI tools were about 5 times more ready to adopt AI use (AOR: 4.5, CI: 3.05–6.72, p: <0.001). The main challenges reported were job displacement, lack of understanding of AI, and limited access to quality health data. A majority of 465 (94.1%) believed training is important to effectively use AI in healthcare.
Conclusion: Healthcare providers' awareness and perceived benefits of AI use in healthcare were good, the knowledge was below average, and an average of the population were ready to adopt AI. Despite the benefits of AI, most of them fear AI will replace their jobs and believe training is important for the effective adoption of AI in healthcare.
1 Introduction
Artificial intelligence (AI) started in early 1950s when Alan Turing developed the Turing test whereby he asked that, “can machines think?” (1) and considered that machines can learn like a child. AI has evolved from the fundamental AI algorithms to machine learning and deep learning algorithms over the years (2). Many definitions of AI exist, but Aiken and Epstein defined AI as a branch of science and technology that allows intelligent computers and computer programs to perform tasks that would typically need human intelligence (3). It is therefore, the imitation of human intellect in computers to carry out tasks like learning, reasoning, problem solving, speech recognition, and decision-making that normally need human intelligence due to its ability to access and analyse large input data (4, 5).
Its application in healthcare, known as healthcare AI has experienced rapid growth in the past decades due to the promising benefits it has offered to the healthcare industry that generates vast amount of health data (6) which can be used to train these machines. This rapid growth has led to patients accessing healthcare from the comfort of their homes (7). The emergence of the coronavirus disease greatly transformed the fundamental building blocks of global health system forcing healthcare stakeholders to adopt digital technologies in healthcare (8). AI has revolutionized the health sector and has substantially improved the quality of services rendered to patients from disease prevention, early detection of diseases, diagnosis, treatment, adherence to treatment, and follow-up of care (9–11). AI can be more cost-effective, accurate, and precise when compared with humans due to its ability to analyse large input data and make evidence-based decision (12–14) as such can reduce patients waiting time, medical errors and length of stay in hospitals. AI has played a crucial role in healthcare through big data analysis, diagnosis, precision medicine, electronic health records, virtual patient care, administrative duties, and research and drug development (15) as well as patient monitoring using wearable sensor devices that have allowed for prompt treatment when need arises (16).
Khosla in 2012, reported that AI will be incorporated into about 80% of hospitals by 2025 and will perform about 90% of tasks that physicians were currently doing (17). Despite the benefits of AI, its application in healthcare especially in Low and Middle Income Countries is still very lacking (18) due to a number of factors such as the absence of regulatory guidelines, unavailability of easy to use AI tools, inappropriate infrastructure and poor internet connections. There exist a lot of obstacles to the use of AI in healthcare. including standardization gaps, unclear legal liability, and ethical concerns (19) as well as misconception about how it will affect the health sector, the patient and the government especially in low- and middle-income countries where data generated are usually disorganized, fragmented, and dispersed making it difficult to be used in real time situations (20, 21). The health sector which is very heavily regulated (22) needs strict rules and guidelines to validate the use of AI tools in healthcare. This requires that the personnel have the knowledge and skills to use and interpret results generated by AI tools (23) which is a major shortcoming in the context of LMICs. The fear that AI will replace jobs (24) has resulted to resistance to the adoption of AI. The difficulty and complexity in understanding how AI tools operate (25) have compromised its trust and validity. AI can breech patient-provider relationship, lacks empathy, emotion and cannot be appropriate in complex health conditions where the inputs from many disciplines are required to come out with a solution (26). It is therefore important to understand that to effectively adopt AI in healthcare, its benefits must be tangible followed by appropriate ethical and legal regulatory standards (27) and healthcare leaders have a role to play when it concerns setting up the standards of health practices in the health system.
The readiness to adopt AI in healthcare can be influenced by the willingness and optimism of healthcare providers about its use as well as the technological, organisational, and environmental (TOE) factors. The TOE framework (28) that was established by Tornatsky and Fleischer in 1990 was considered appropriate and adapted for the study and was used to assess healthcare providers' readiness to adopt AI in healthcare.
The aim of this study was to determine the proportion of awareness and knowledge of the use of AI, perceived benefits, readiness to adopt AI, and perceived challenges in the implementation of AI in healthcare service delivery among healthcare workers in the Limbe and Buea Health Districts of Cameroon.
2 Materials and methods
2.1 Study design and population
A hospital based cross-sectional study, targeting healthcare providers, was conducted in the Limbe and Buea Health Districts of Cameroon from February 2024 to June 2024.
2.2 Selection criteria
The inclusion criteria were healthcare providers aged 18 years and above, and who have at least six months of working experience while healthcare providers who were sick and mentally unstable were excluded from the study. The different categories of healthcare providers who participated in the study were medical doctors, nurses, laboratory scientists, radiologists, pharmacists, midwives and nutritionists.
2.3 Sample size determination and sampling
From the personnel registry of the Limbe Health District, the estimated number of personnel (1,139) was used to calculate the sample size of 296 while for Buea, 391 health personnel gave 198 using the Yamane's (1967) formula (29). The two were summed up to 494 participants as minimum for the study. A multi-staged sampling technique was used to randomly selected the 296 participants from five health facilities in Limbe Health District (Regional Hospital Limbe, District Hospital Limbe, Sub-Divisional Hospital Limbe, Bota Polyclinic, and PCC Health Centre Limbe) and the 198 participants from two health facilities in Buea Health District (Regional Hospital Buea, and Mount Mary Hospital Buea) to participate in the study.
2.4 Ethical consideration
Ethical clearance was obtained from the Institutional Review Board (IRB) of the Faculty of Health Sciences (FHS) No 2024/2331-01 of the University of Buea followed by administrative authorizations to carry out the research from the seven selected health facilities.
2.4 Data collection
A questionnaire, adapted from the Shinners artificial intelligence perception tool (30) and from the existing reviewed literature was designed and deployed on KoboCollect v2023.2.4 for data collection through face-to-face based interview with the use of smart phones. Pretesting of fifteen questionnaires was done in the Sub-Divisional Hospital Bonadikombo and PCC eye clinic Limbe to assess the feasibility and correctness of the data collection tool in responses to obtaining relevant data for the attainment of the specific objectives of the study. The questionnaire advised potential respondents that consent was implied by completing the survey and submitting the questionnaire into the online KoboCollect application while anonymity and confidentiality of the respondents were respected throughout the interview.
The scoring was done based on a set of questions each pertaining to knowledge, perception, and readiness. The correct/appropriate response was scored as “1” and incorrect/inappropriate response score as “0” which were summed up and a cut-off for each was determined. Scores greater than the cut-off score were considered good/ready and scores less than or equal to the cut-off score were considered poor/not ready.
2.5 Data management and analysis
Completely filled questionnaires submitted online into Kobo Collect were later downloaded onto MS Excel, then cleansed and stored in a safe external storage device. The data were then exported to IBM SPSS statistics v26 for analysis. Descriptive statistics was done for discrete variables and presented as means and standard deviations while categorical variables were presented as frequency tables and charts and logistic regression was used to analyse the association of socio-demographic characteristics of the participants with their readiness to adopt AI in healthcare service delivery. Variables with that from the binary analysis with a P-value of <0.02 at 95% confidence interval were imported into the logistic regression model. A P-value of <0.05 at 95% confidence interval was considered statistically significant.
3 Results
3.1 Socio-demographic characteristics of the participants
A total of 494 healthcare providers were recruited in the study whose mean age was 32.6 ± 7.5 years and mean duration of working experience was 6.0 ± 5.1 years. The highest proportion of the participants of the study as shown in Table 1 was recorded from Regional Hospital Limbe being 200 (40.5%) followed by Regional Hospital Buea 109 (22.1%) and the lowest was from Presbyterian Health Center Down Beach Limbe. The majority of the respondents were made up of females 355 (71.9%), Nurses 295 (59.7%), those who had attained a tertiary level of education 488 (90.7%), and owned smart phones 485 (98.2%). However, only a few 266 (53.8%) of them have had access to an AI tool.
3.2 Awareness of artificial intelligence use in healthcare among healthcare providers
From the results of the study a total of 409 (82.8%) participants reported having heard of AI before and out of this number, 373 (75.5%) were aware that AI can be used in healthcare service delivery and only 261 (52.8%) of them had used one or more AI tools in their practices. Figure 1 shows the proportion of healthcare providers' awareness of AI use in healthcare.
3.3 Assessment of healthcare provider's knowledge of healthcare artificial intelligence
The healthcare providers' knowledge of the use of AI in healthcare was assessed from a set of four questions which had a total score of 11points, with a cut-off of 6/11 points and above considered as having good knowledge while from 5/11 and below poor knowledge. The results as shown in Figure 2 revealed 213 (43.1%) had good knowledge on AI use in healthcare and 281 (56.9%) had poor knowledge.
3.4 Healthcare providers' perception of the benefits of artificial intelligence in healthcare
The perception of the benefits of AI in healthcare of the participants was categorized as good or poor following a scoring of 10 pts from a set of three questions. A cut-off of 6 was categorized as good perception of the benefits of AI in healthcare while from 5 and below was categorized as poor and summarized in Figure 3.
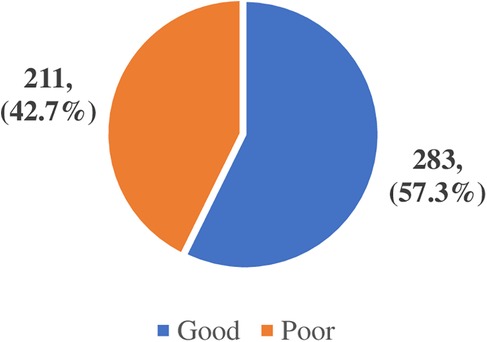
Figure 3. Healthcare providers' perception of the benefits of artificial intelligence in healthcare.
3.5 Healthcare providers' readiness to adopt artificial intelligence in healthcare
With respect to adopting AI in healthcare, a set of three questions were scored, based on their willingness, optimism and the TOE framework and on a scale of 13 with a cut-off score of 7/13. Scores greater than 7 were categorized as ready and from 7 and below were considered not ready. The study revealed 230 (46.6%) readiness to adopt AI in healthcare while 264 (53.4%) not ready as shown in Figure 4.
3.6 Factors associated with the readiness to adopt AI
Tables 2, 3 shows the factors that were significantly associated with the readiness to adopt AI in healthcare at multivariate analysis using the multiple logistic regression model. The odds of those with tertiary education being ready to adopt AI in healthcare service delivery were 0.1 (95% CI: 1.027–4.888, P = 0.043) times lower than the odds of those of secondary education. The odds of those who had access to AI tools were 4.5 times (95% CI: 3.053–6.715, P ≤ 0.001) ready to adopt AI tools in healthcare.
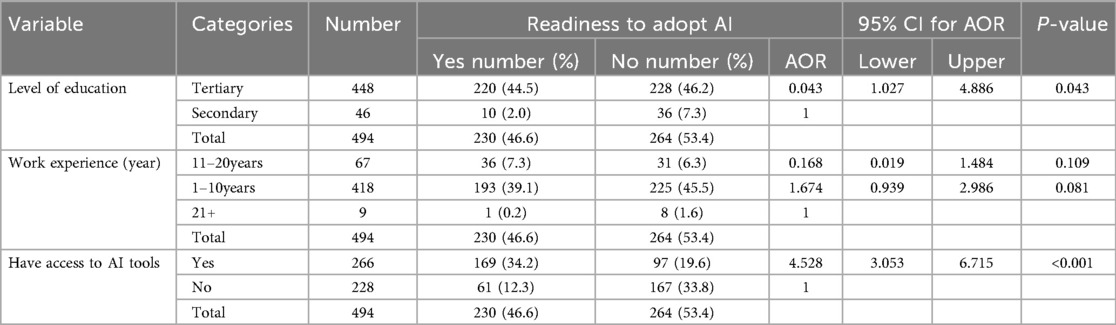
Table 3. Multivariate analysis of factors associated with readiness to adopt artificial intelligence in healthcare.
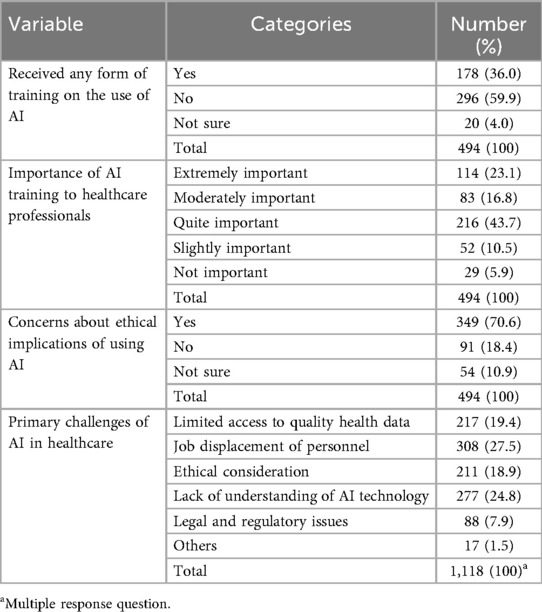
3.7 Healthcare providers' perceived challenges with the use of artificial intelligence in healthcare
The results in Table 4 showed that a good proportion of the participants 296 (59.9%) had never had any formal or informal form of training in AI while 178 (36.0%) have had informal training. The majority 349 (70.6%) were very concerned about the ethical implications of the use of AI in health as issues of confidentiality, patient's privacy and lack of empathy in AI tools while the primary challenges were fear of job displacement 308 (27.5%), lack of knowledge of the functionality of AI tools 277 (24.8%), and limited access to quality health data 217 (19.4%).
4 Discussions
The use of artificial intelligence in healthcare which is in its initial phase in this region is very much exiting and promising owing to the many benefits it has in the health sector. The findings of this study have provided insights into healthcare providers' perception and knowledge of the use of artificial intelligence in healthcare service delivery which is relevant for developing future strategies in Public health to facilitate the adoption and use of AI in healthcare.
Most of the participants had heard about artificial intelligence before and fewer of them had actually used either AI tools from the application on their smart phones, or wearable sensor devices. A study by Samyuktha et al. (31) carried out in India in 2020 on awareness and knowledge about artificial intelligence in healthcare among doctors showed an awareness of about 55% of artificial intelligence in healthcare. The results also revealed that only 43.1% of them had good knowledge and understanding of AI use in healthcare though many did not understand the full applicability of AI in their practices. This higher awareness and knowledge can be attributed to the rapidly growing technology, and information and communication tools like smart phones with the stable internet connection, allowing more healthcare workers to be informed about AI at anytime and anywhere. This is supported by the fact that 98.2% of the participants owned at least a smart phone giving them access to vast information around the world. The highest proportion of the respondents were of the age group 30–39 years accounting for the younger generation being more aware and engaged with technologies and their uses than the older generation. Due to the fact that a vast majority of the respondents had attained tertiary education which when combined with the use of smart phones they can easily get access to information and gain more knowledge on AI use in healthcare. A study carried out by Catalina et al. (32) on knowledge and perception of primary care healthcare professionals on the use of artificial intelligence as a healthcare tool in 2023, revealed an awareness of 85.7% which is higher compared with that of this study. This can be due to the fact that the use of artificial intelligence is more integrated into their healthcare system than in the Health Districts of Limbe and Buea. The healthcare providers' perception of the benefits of AI in healthcare from the study showed that a good proportion of the respondents had good perception about AI's benefits in healthcare as it can enhance patient management, assist in evidence-based decision making, diagnostic precision and accuracy, reduction in patient waiting time and medical errors and as such reduction in health cost both to the patient and the personnel and reduced length of stay in the hospital.
With respect to the readiness to adopt AI, few of the respondents were ready to adopt AI in their practices. A study by Ogolodom et al. (33) in Nigeria, reported that most of the respondents agreed that AI can be incorporated into medical specialties and were ready to use it. Nonetheless, its adoption in healthcare has to be strictly regulated and validated to ensure compliance and to avoid unnecessary bias.
This study's results revealed that the perceived fear that AI will replace healthcare providers in their jobs, lack of knowledge of how AI functions and limited access to quality health data were the major challenges in the implementation of AI in healthcare among others. A similar report done in Saudi Arabia by Serbaya et al. (34) revealed that 58% of healthcare workers expressed fear about job displacement. Ogolodom et al. (33) in Nigeria, agreed that healthcare workers are at risks of being replaced in their jobs which is consistent with this study. Quite a good number of the respondents are very concerned about the ethical issues of using machines to perform tasks of care to patients as they think the relationship between the patient and the health care providers may be breeched as machines can never provide emotional support, empathy and have no feelings as such AI may dehumanize healthcare service delivery (35) and only a few of the respondents trusted AI driven decision-making. WHO has developed six ethical principles to guide the development of AI tools. Ethical principles guiding AI in healthcare research are deeply rooted in the foundational principles of medical research ethics.
Training was an important facilitator mentioned by the health care provider to adopt AI in health care service. According to Catalina et al. (32), 65.8% of healthcare professionals also indicated that they had not received any training and 91.4% would like to receive training on AI which is similar with the results obtained in this study.
5 Limitations of the study
Limited scope of the study: The study was focused on two Health Districts of Cameroon and mainly in the urban areas which may limit the generalizability of the findings to other Regions or beyond Cameroon. Studies from rural or primary healthcare settings are required for a more representative view. Furthermore, the study relies on self-reported awareness and use of AI, which may be influenced by social desirability and participant might have overreported on their digital skills.
6 Conclusions
This study found out that healthcare providers were aware that artificial intelligence can be used in healthcare, though their knowledge of the functionality of AI in healthcare is slightly below average. They were very optimistic and willing to adopt AI in their practices. This result will guide the implementation of AI taking into consideration the challenges and concern of the health care providers. Training and sensitisation is necessary to facilitate the use of AI in health care.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Faculty of Health Sciences Institutional Review Board of the University of Buea, Cameroon. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
OI: Conceptualization, Data curation, Formal analysis, Writing – original draft. FT: Conceptualization, Writing – review & editing. OK: Writing – review & editing. IK: Methodology, Writing – review & editing. ET: Conceptualization, Data curation, Formal analysis, Writing – original draft. DNk: Investigation, Methodology, Writing – review & editing. MN: Investigation, Methodology, Writing – review & editing. PA: Data curation, Investigation, Methodology, Writing – review & editing. CT: Data curation, Investigation, Methodology, Writing – review & editing. JA: Writing – review & editing. MO: Writing – review & editing. PN: Investigation, Writing – review & editing. MS: Data curation, Writing – review & editing. GH-E: Supervision, Writing – review & editing. JK: Supervision, Writing – review & editing. DNs: Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by the International Development Research Center (IDRC) Canada through partnership with the York University (Grant number: 09981-001) to AI4PEP (Artificial Intelligence for Pandemic and Epidemic Preparedness) and the Common Wealth Foreign and Development Office of the United Kingdom.
Acknowledgments
The authors would like to thank all the healthcare providers in the different hospitals of the Limbe and Buea Health Districts who participated in the survey and all the heads of health facilities who facilitated access to the participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Muggleton S. Alan turing and the development of artificial intelligence. AI Commun. (2014) 27(1):3–10. doi: 10.3233/AIC-130579
2. Delipetrev B, Tsinaraki C, Kostic U. Historical Evolution of Artificial Intelligence Publications Office of the European Union. (2020). (Accessed December 28, 2023, 10:45pm).
3. Ali O, Abdelbaki W, Shrestha A, Elbasi E, Alryalat MAA, Dwivedi YK. A systematic literature review of artificial intelligence in the healthcare sector: benefits, challenges, methodologies, and functionalities. J Innov Knowl. (2023) 8(1):100333. doi: 10.1016/j.jik.2023.100333
4. Martinez-Ortigosa A, Martinez-Granados A, Gil-Hernández E, Rodriguez-Arrastia M, Ropero-Padilla C, Roman P. Applications of artificial intelligence in nursing care: a systematic review. J Nurs Manag. (2023) 20(23):1–12. doi: 10.1155/2023/3219127
5. Shabbir J, Anwer T. Artificial Intelligence and its role in the near Future. arXiv Preprint. (2018) 18(4):01396.
6. Kayyali B, Knott D, Kuiken SV. The big-data revolution in US health care: accelerating value and innovation. MC Kinsey Co. (2013) 2(8):1–3.
7. Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. (2017) 7(8):e016242. doi: 10.1136/bmjopen-2017-016242
8. Siriwardhana Y, Gur G, Ylianttila M, Liyanage M. The role of 5G for digital healthcare against COVID-19 pandemic: opportunities and challenges. ICT Express. (2021) 7(2):244–52. doi: 10.1016/j.icte.2020.10.002
9. Ahmed MI, Spooner B, Isherwood J, Lane M, Orrock E, Dennison A. A systematic review of the barriers to the implementation of artificial intelligence in healthcare. Cureus. (2023) 15(10):46454.
10. Kaushik P. Artificial intelligence accelerated transformation in the healthcare industry. Amity J Prof Pract. (2023) 3(1). doi: 10.55054/ajpp.v3i01.630
11. Singareddy S, Sn VP, Jaramillo AP, Yasir M, Iyer N, Hussein S, et al. Artificial intelligence and its role in the management of chronic medical conditions: a systematic review. Cureus. (2023) 15(9). doi: 10.7759/cureus.46066
12. Khanna NN, Maindarkar MA, Viswanathan V, Fernandes JF, Paul S, Bhagawati M, et al. Economics of artificial intelligence in healthcare: diagnosis vs treatment. InHealthcare. (2022) 10(12):2493. doi: 10.3390/healthcare10122493
13. Hendrix N, Veenstra DL, Cheng M, Anderson NC, Verguet S. Assessing the economic value of clinical artificial intelligence: challenges and opportunities. Value Health. (2022) 25(3):331–9. doi: 10.1016/j.jval.2021.08.015
14. Xu Q, Xie W, Liao B, Hu C, Qin L, Yang Z, et al. Interpretability of clinical decision support systems based on artificial intelligence from technological and medical perspective: a systematic review. J Healthc Eng. (2023) 9(9):192–69.
15. Kuwaiti A, Nazer K, Reedy A, Shehri S, Muhanna A, Subbarayalu AV, et al. A review of the role of artificial intelligence in healthcare. JPM (2023) 13(6):951. doi: 10.3390/jpm13060951
16. Udeghe FC, Ebulue OR, Ebulue CC, Ekesiobi CS. The role of artificial intelligence in healthcare: a systematic review of applications and challenges. Int Med Sci Res J. (2024) 4(4):500–8. doi: 10.51594/imsrj.v4i4.1052
17. Uzir MUH, Al Halbusi H, Lim R, Jerin I, Abdul Hamid AB, Ramayah T, et al. Applied artificial intelligence and user satisfaction: smartwatch usage for healthcare in Bangladesh during COVID-19. Technol Soc. (2021) 67:101780. doi: 10.1016/j.techsoc.2021.101780
18. Saif-Ur-Rahman K, Islam MS, Alaboson J, Ola O, Hasan I, Islam N, et al. Artificial intelligence and digital health in improving primary health care service delivery in LMICs. A systematic review. J Evid Based Med. (2023) 16(3):303–20. doi: 10.1111/jebm.12547
19. Maskara R, Bhootra V, Thakkar D, Nishkalank N. A study on the perception of medical professionals towards artificial intelligence. Int J Multidiscip Res Dev. (2017) 4(4):34–9.
20. Beltempo L, Zerrer J, Härting R-C, Hoppe N. Barriers of artificial intelligence in the health sector. In: Lim CP, Vaidya A, Chen Y-W, Jain V, Jain LC, editors. Artificial Intelligence and Machine Learning for Healthcare. Cham: Springer International Publishing (2023). p. 251–73.
21. Tachkov K, Zemplenyi A, Kamusheva M, Dimitrova M, Siirtola P, Pontén J, et al. Barriers to use artificial intelligence methodologies in health technology assessment in central and East European countries. Front Public Health. (2022) 10:127–33. doi: 10.3389/fpubh.2022.921226
22. Schonberger D. Artificial intelligence in healthcare: a critical analysis of the legal and ethical implications. Int J Law Inform Technol. (2019) 27(2):171–203. doi: 10.1093/ijlit/eaz004
23. Singh RP, Hom GL, Abramoff MD, Campbell JP, Chiang MF. Current challenges and barriers to real-world artificial intelligence adoption for the healthcare system, provider, and the patient. Transl Vis Sci Technol. (2020) 9(2):45. doi: 10.1167/tvst.9.2.45
24. Qadri HM, Bashir M, Khan M, Amir A, Khan AYY, Safdar Z, et al. Knowledge, awareness and practice of artificial intelligence and types of realities among healthcare professionals: a nationwide survey from Pakistan. Cureus. (2024) 16(4):23–36.
25. Hazarika I. Artificial intelligence: opportunities and implications for the health workforce. Int Health. (2020) 12(4):241–5. doi: 10.1093/inthealth/ihaa007
26. Petersson L, Larsson I, Nygren JM, Nilsen P, Neher M, Reed JE, et al. Challenges to implementing artificial intelligence in healthcare: a qualitative interview study with healthcare leaders in Sweden. BMC Health Serv Res. (2022) 22(1):850. doi: 10.1186/s12913-022-08215-8
27. Manson EN, Hasford F, Trauernicht C, Ige TA, Inkoom S, Inyang S, et al. Africa’s readiness for artificial intelligence in clinical radiotherapy delivery: medical physicists to lead the way. Phys Med. (2023) 11(3):1026–53.
28. Hoosen KF. Factors Influencing Artificial Intelligence Adoption in South African Organisations: A Technology, Organisation, Environment (TOE) Framework. Johanesberg: University of the Witwatersrand (2023).
29. Adam AM. Sample size determination in survey research. J Sci Res Rep. (2020) 26(5):90–7. doi: 10.9734/jsrr/2020/v26i530263
30. Shinners L, Grace S, Smith S, Stephens A, Aggar C. Exploring healthcare professionals' perceptions of artificial intelligence: piloting the shinners artificial intelligence perception tool. Digital Health. (2022) 8:1–8.
31. Samyuktha PS, Geetha RV, Jayalakshmi S. Awareness and knowledge about artificial intelligence among doctors-a survey. Eur J Mol Clin Med. (2020) 7(1):697–708.
32. Catalina QM, Fuster-Casanovas A, Vidal-Alaball J, Escalé-Besa A, Marin-Gomez FX, Femenia J, et al. Knowledge and perception of primary care healthcare professionals on the use of artificial intelligence as a healthcare tool. Digital Health. (2023) 9(20):55–11. doi: 10.1177/20552076231180511
33. Ogolodom MP, Mbaba AN, Johnson J, Chiegwu HU, Ordu KS, Okej MC, et al. Knowledge and perception of healthcare workers towards the adoption of artificial intelligence in healthcare service delivery in Nigeria. AG Salud. (2023) 3(1):1–16.
34. Serbaya SH, Khan AA, Surbaya SH, Alzahrani SM. Knowledge, attitude and practice toward artificial intelligence among healthcare workers in private polyclinics in Jeddah, Saudi Arabia. Adv Med Educ Pract. (2024) 15:269–280. doi: 10.2147/AMEP.S448422
Keywords: artificial intelligence, healthcare, healthcare provider, perception, Cameroon
Citation: Itoe O, Tatsinkou Bomba FD, Kibu OD, Kwalar IG, Tanue EA, Nkweteyim D, Nyamsi ML, Achankeng PL, Tchapga C, Ayuk J, Ondua M, Ngono Ema PJ, Sandeu MM, Halle-Ekane GE, Kong JD and Nsagha DS (2025) Healthcare providers' perception and knowledge of the use of artificial intelligence in healthcare service delivery in the Limbe and Buea Health Districts: a cross-sectional study. Front. Digit. Health 7:1575633. doi: 10.3389/fdgth.2025.1575633
Received: 13 February 2025; Accepted: 4 September 2025;
Published: 1 October 2025.
Edited by:
Shikha Kukreti, National Cheng Kung University, TaiwanReviewed by:
Mukaila Rahman, Lagos State University, NigeriaSwati Jain, National Cheng Kung University, Taiwan
Copyright: © 2025 Itoe, Tatsinkou Bomba, Kibu, Kwalar, Tanue, Nkweteyim, Nyamsi, Achankeng, Tchapga, Ayuk, Ondua, Ngono Ema, Sandeu, Halle-Ekane, Kong and Nsagha. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dickson Shey Nsagha, bnNhbmdoYS5kaWNrc29uQHVidWVhLmNt
 Oliver Itoe1
Oliver Itoe1 Innocentia Ginyu Kwalar
Innocentia Ginyu Kwalar Elvis Asangbeng Tanue
Elvis Asangbeng Tanue Denis Nkweteyim
Denis Nkweteyim Moise Ondua
Moise Ondua Jude Dzevela Kong
Jude Dzevela Kong Dickson Shey Nsagha
Dickson Shey Nsagha