- 1Grado Department of Industrial and Systems Engineering, Virginia Polytechnic Institute and State University, Blacksburg, VA, United States
- 2Department of Mechanical & Industrial Engineering, The University of Illinois Chicago, Chicago, IL, United States
- 3Division of Emergency Medicine, Children’s National Hospital, Washington, DC, United States
- 4School of Medicine and Health Sciences, Geroge Washington University, Washington, DC, United States
- 5Department of Neonatology, Children’s National Hospital, Washington, DC, United States
Remote Measurement Technologies (RMTs) have the potential to become widely used tools for monitoring and treating mental health. However, their adoption faces multiple barriers. We conducted a focused literature review to identify commonly used devices and assessment surveys, synthesize barriers to their use, and explore proposed solutions. Our review highlighted several challenges in implementing RMTs, including technological limitations, user-related factors, legal and ethical concerns, research constraints, and difficulties integrating these technologies into clinical practice. While studies have examined barriers through user interviews, empirical analyses of success factors remain limited, highlighting a need for further research in this area.
1 Background
Remote Measurement Technologies (RMTs) are increasingly utilized for screening, monitoring, and treatment of mental health conditions. Remote Measurement Technologies (RMTs) are digital tools—such as smartphones, wearables, and associated apps—that collect data in real time either passively or actively (1). Passive data collection involves gathering information through embedded sensors or user interactions with the device, such as tracking steps via an accelerometer or measuring heart rate using photoplethysmography—a technique that uses light, typically green LEDs, to detect changes in blood volume beneath the skin. Active data collection, on the other hand, requires direct input from individuals, such as completing mood surveys or logging medication use through a smartphone app or web link.
Clinicians are increasingly seeking ways to access hard to reach populations such as rural areas, low-income communities, and postpartum caregivers. RMT provides clinicians with further reach than traditional means. For example, at Children's National in Washington DC, a Level IV Neonatal Intensive Care Unit (NICU), caregivers of children are often not present at the bedside. The infants are transported to the hospital from over 40 area NICUs and parents often return to work during their infant's long length of stay. Screening and treatment of these postpartum caregivers is hampered by absence from the bedside. Therefore, we are frequently looking for RMT solutions to overcome this problem.
Although the clinical utility of RMTs in improving depression symptoms and outcomes is yet to be determined (1–3), these technologies provide multiple other benefits. First, RMT can increase access to healthcare (4) and overall capacity of mental healthcare. Many individuals experience barriers to traditional in-person care, due to geographic distance, limited mobility, or the stigma associated with seeking help for mental health (5). By using RMTs, healthcare providers can reach patients who might otherwise be excluded from timely, quality mental health support. However, health inequalities can persist if individuals with limited access, experience, or capacity are not equipped to benefit from these technologies (6). Second, continuous data collection from RMTs enables healthcare professionals to gather more accurate and detailed information about a patient's condition, rather than relying solely on episodic visits or self-reports (7). Thus, it helps to create a clearer picture of the patient's health at various points in time, enhancing the overall understanding of their condition without creating a large burden on the patient (7). Third, RMTs can assist in personalized detection of mental health symptoms. For example, data collected from mobile phones and sensors such as movement patterns and communication behaviors improve prediction of depressive symptoms (8). Finally, RMTs provide cost savings for both patients (i.e., transportation costs) and providers (i.e., facilities, and staffing) (5, 9, 10) and lead to reduced stress for patients (9).
Past systematic literature reviews of RMTs examined the impact of these technologies on depression outcomes. Goldberg and colleagues identified 13 randomized controlled trials, but only three specifically isolated the clinical impact of RMTs (2). One of these trials found that adding a monthly remote measurement-based care via secure messaging to treatment as usual (TAU) in primary care led to significantly greater symptom improvement compared to TAU alone. This systematic review concluded that while RMTs are feasible, further research is needed to assess their impact on depression outcomes (2). Another systematic review found that data derived from remote measurement technologies can be used to construct digital phenotypes that facilitate clinical assessment and may serve as predictors of relapse or symptom worsening (11). Walsh and colleagues conducted a realist review of RMTs for depression in individuals aged 14–24 years. They found that RMTs were useful for detecting changes in sleep, mobility, smartphone use, social communication, and mood, which supported screening, self-monitoring, and feedback to healthcare providers. However, RMTs were less effective for relapse prevention and delivering personalized interventions (1). Although past reviews investigated the context in which RMTs are useful, they have not synthesized the barriers of implementing RMTs for mental health problems and the proposed solutions. This study reviews the literature on RMTs to explore common devices and assessment surveys, identify barriers to their use, and examine solutions proposed to address these challenges.
2 Method
2.1 Search strategy
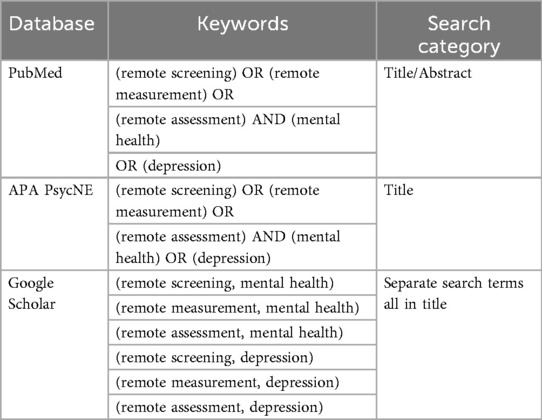
We conducted a literature review to identify journal publications about remote screening of mental health. The search was performed across three databases—PubMed, APA PsycNET, and Google Scholar—covering publications from 2004 to 2024. The table below outlines the keywords and search categories used for each database (Table 1).
2.2 Inclusion criteria
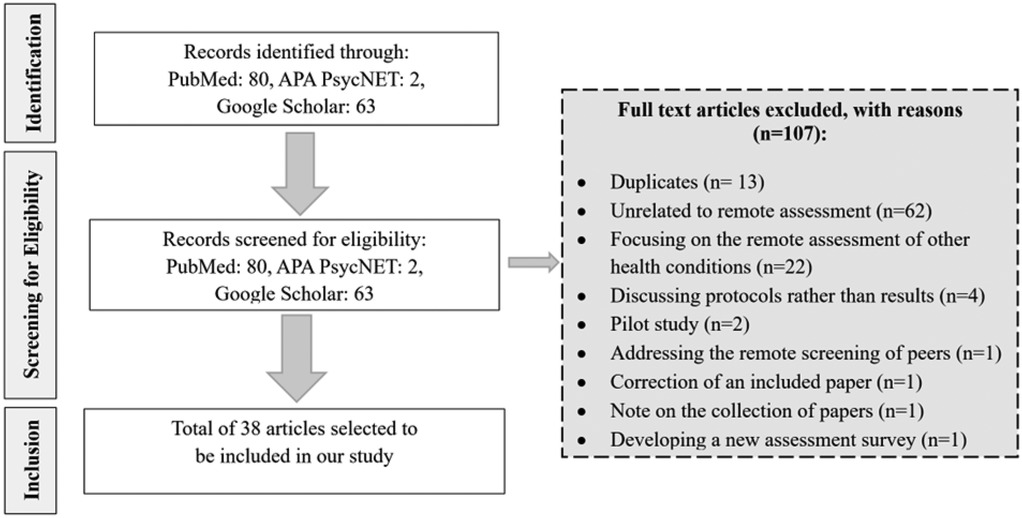
After conducting an initial search across three databases, we identified 80 papers in PubMed, 2 in APA PsycNET, and 63 in Google Scholar. The titles and abstracts of these 145 articles were screened, and duplicates and studies unrelated to remote screening for mental health and depression were excluded from further review. The exclusion criteria included the following: duplicates (n = 13), studies unrelated to remote assessment (n = 62), studies focusing on the remote assessment of other health conditions (n = 22), studies discussing protocols rather than results (n = 4), pilot studies (n = 2), studies addressing the remote screening of peers instead of individuals with mental health concerns (n = 1), a correction of an included paper (n = 1), a note on the collection of papers about mental health remote screening (n = 1), and developing a new assessment survey (n = 1) (Figure 1).
2.3 Study selection
After screening the abstracts retrieved from PubMed, APA PsycNET, and Google Scholar, we selected 38 studies for inclusion in our analysis. Through a detailed review of these papers, we identified the tools and assessment surveys used in remote screening, the barriers and success factors in implementing remote screening systems, and the pathways for connecting at-risk individuals to providers. A summary of the key steps and findings from this process is provided below.
3 Results
Results from the articles were grouped into 4 categories: (a) devices used, (b) assessment surveys utilized, (c) Strategies to connect patients to services, and (d) Barriers and Facilitators of RMT.
3.1 Devices used
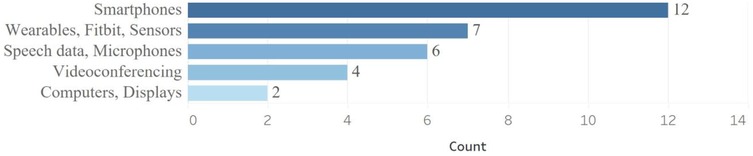
Multiple devices have been used to collect data, including smartphones (12–23), wearables (15, 17, 18, 21–24), computers/displays (10, 13, 19), videoconferencing (21, 25–27), and microphone of computers, phones, or tablet to record patients' speech (15, 18, 20, 24, 28, 29). As shown in Figure 2, the most common device used was smartphones.
Studies' objectives determine what device to use (1). Wearable devices offer continuous and often more accurate data; however, they rely on users remembering to charge and wear them, which can lead to decreased usage over time compared to active monitoring. In contrast, active monitoring—based on direct user input—may improve adherence, but the frequency, timing, and content of prompts must be carefully tailored to sustain engagement.
3.2 Assessment surveys used
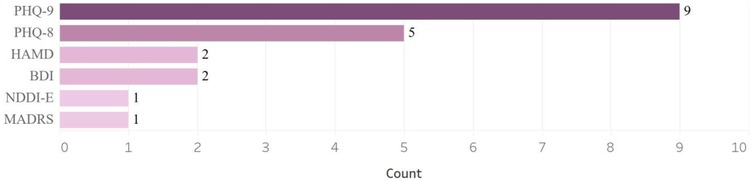
The Patient Health Questionnaire-9 (PHQ-9) is one of the most frequently self-administered-questionnaires used to screen for and assess the severity of depression. Our search identified nine studies that used PHQ-9 (14, 15, 19, 21, 28, 30–33) and five studies that utilized PHQ-8 (17, 18, 22, 24, 29). Other questionnaires that were used included the Hamilton Depression Rating Scale (HAMD) (21, 26), the Beck Depression Inventory-II (BDI) (20, 21), the Neurological Disorders Depression Inventory in Epilepsy (NDDI-E) (34), and the Montgomery-Asberg Depression Rating Scale (MADRS) (27, 35) (Figure 3).
3.3 Strategies to connect suicidal people to providers
Few studies discussed how suicidal people are connected to the healthcare system. One study describes a national service in Australia, MindSpot, that offers remote mental health screening, assessment, and treatment for adults (32). The questionnaire sent by this program includes questions about suicidal thoughts, with those answering “yes” receiving an immediate on-screen alert that promotes personal safety and provides crisis and emergency service contact details. Additionally, a MindSpot therapist promptly reaches out to conduct a “structured risk assessment” to gather more details on risk factors and, if necessary, refer the individual to emergency services. The questions are sourced from an on-screen form visible only to therapists, ensuring adherence to the risk assessment protocol. As part of the procedure, therapists complete a crisis summary report, which outlines risk and protective factors, documents referrals or other actions taken in response to the assessed risk, and records the outcomes of those actions (32). Another study reported the discussion of a panel on suicide prevention and management (36). The panel was part of a one-day workshop to enhance mental health services for veterans. The panel emphasized the importance of combining call services with onsite follow-ups for building trust and rapport. While call services provide initial contact and support, onsite follow-ups reinforce credibility and strengthen relationships, both on a personal level and within the broader community (36). Another study noted that patients with suicidal intent were referred to appropriate care but did not provide detailed information about the referral process or follow-up outcomes (30).
3.4 Barriers of remote mental health screening and proposed solutions
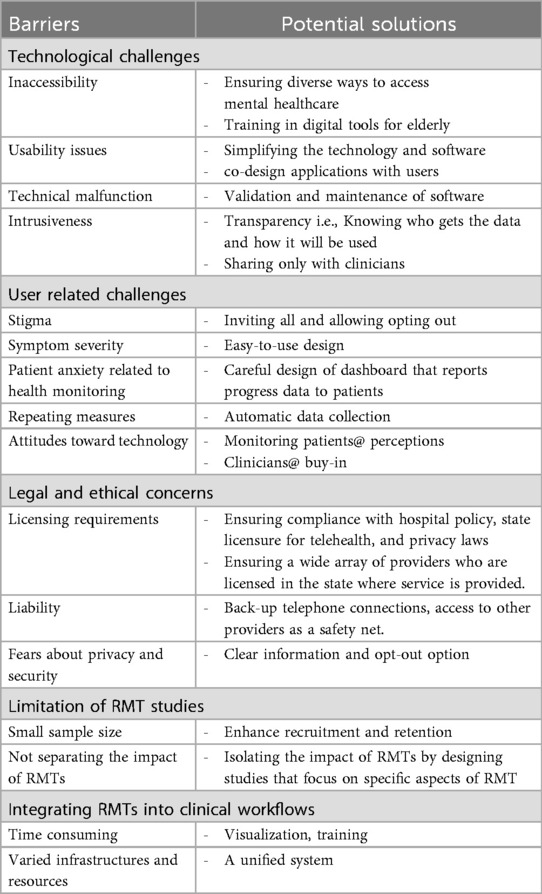
The adoption of RMTs in healthcare has faced several barriers, including technological challenges, user-related factors, legal and ethical concerns, research-related limitations, and difficulties in integrating these technologies into clinical practices. The identified barriers and their subcategories, along with the proposed solutions, are presented in Table 2. More details follow.
Technological challenges include inaccessibility, usability issues, technical malfunction, and intrusiveness (1, 6, 23, 37, 38). Studies reported concerns about the price of the technology and access to reliable wi-fi which affect accessibility of the RMTs (6, 38). If accessibility is not addressed, the use of RMT may widen the mental health disparity (1). Ensuring RMTs are not the only entrance level to mental healthcare, and training in digital tools for elderly are essential to minimize inaccessibility (39). Complex technology, regular software updates, “relearning a new operating system,” and technological literacy affect usability (6, 23). Solutions range from simplifying technology and software to codesigning software with users (6, 37). Users reported technical malfunctions such as apps crashing, apps logging out, and difficulties with rescanning QR codes (23). Validation and iterative testing of digital tools ensure they function across different types of devices and settings. Some users were concerned about data sharing and perceived the technology to be intrusive (38). Knowing with whom the data is shared and sharing data only with clinicians might address this issue (38). Wearables were perceived as less intrusive in some studies (23) while others reported invasion of privacy when passive data is reported (15).
User-related barriers include stigma (6, 36, 40), symptom severity (38), “patient anxiety related to health monitoring” (21, 41), not willing to complete repeated measurement surveys (6, 23), and attitudes toward technology (6, 38). To reduce stigma in one study, the invitation to participate in a self-report screening was sent to all personnel in a fire department, and they were allowed to participate or opt out (40). To enhance the adherence of patients with depressive symptoms who may not be able to engage with RMTs, studies suggested easy-to-use-design (38, 39). In addition, training in digital tools for those with low digital literacy has been recommended (39). Careful design of dashboards that report back the collected information to patients is suggested for reducing anxiety generated due to health monitoring (41). Additionally, visualizing patients' health and progress over time facilitates reflection and provides an objective basis for validating improvements in mental health (21). Patients disliked repeating surveys, and they prefer automatic data collections (6). Attitudes toward technology affect the RMT use for all users including providers (38). Some users were concerned about the quality of remote monitoring. As a result, frequent surveys of patients' perception about acceptability of the technology and outcomes are necessary (39). Buy-in by clinicians promotes patients' use of RMTs (6).
Remote assessment of mental health involves legal issues including licensing requirements (i.e., clinicians need to be licensed in the state of the patient), liability (e.g., liability for remote suicide evaluations when technical issues interrupt patient interview) (25), and data security and privacy (6, 39). Proposed solutions for liability related to the interruption include having back-up telephone connections, access to other providers, or other resources (25). Fear about privacy and security are the major barriers of implementing (6, 38, 39). Proposed solutions include ensuring that apps provide clear information on data handling and allowing patients to opt out of data sharing (6, 39).
Small sample size in RMT studies (median sample size = 58) reduce their statistical power and subsequently clinical implementations (38). Lessons learned from large studies, such as the Remote Assessment of Disease and Relapse-Major Depressive Disorder (RADAR-MDD) study, can guide others to enhance recruitments (37) and retention of participants (17). These lessons include co-design with users, ensuring a competent recruitment team with patience and awareness of potential technological barriers, and minimizing participant burden by creating a standardized pathway that guides participants from initial contact to enrolment. In addition, few studies have isolated the impact of RMTs from other factors examined in research projects. Isolating the impact of RMTs is essential for drawing reliable conclusions.
Integrating RMTs into clinical workflows is challenging due to the time-intensive nature of data review and the limited training available for healthcare providers. The sheer volume of data generated by RMTs often exceeds the capacity of clinicians to interpret effectively (6, 41). Automated data visualization tools have emerged as a solution, enabling healthcare providers to quickly interpret trends and anomalies in patient data, reducing mental load and improving efficiency in decision-making (6, 25, 40). Continuous feedback from clinicians has further refined these tools, making sure they align with clinical workflows and complement existing care practices (1, 2, 35). Addressing these challenges involves conducting usability and feasibility studies to identify potential integration issues and adapt tools accordingly. Another barrier for integrating RMT in the clinical setting is the variation in infrastructures and resources across sites (42). A potential solution is a unified clinical informatics system, which has been successfully implemented to streamline screening, assessment, and data integration across pediatric and mental health settings. By incorporating EHR data and patient-reported outcomes, this system has enhanced care coordination for adolescent depression and underscored the need for expanded capabilities, such as patient-facing tools for automated and customized assessments (42).
4 Discussion
We conducted a focused literature review about RMTs to identify the most prevalent devices and questionnaires used for measuring mental health factors. Consistent with past studies (1), we found that smartphones were the most popular device for collecting data. Devices were used based on the objective of the studies. Wearable devices provide continuous and more accurate information; however, users need to remember to charge and wear them which may lead to lower use over time relative to active monitoring (1). Active monitoring through direct input from users may increase adherence, but the frequency, timing, and content of prompts should be selected carefully to enhance engagement (1).
The most used questionnaire was the PHQ-9. Many depression questionnaires are available for both the general population and specific subgroups. The choice of questionnaires is guided by the study population. For example, in maternal mental health, the Edinburgh Postnatal Depression Scale (EPDS) and PHQ-9 are frequently used. Additionally, some questionnaires include items on suicidality, which make remote screening challenging—especially if a patient is in acute crisis and requires immediate intervention. On the other hand, not screening for suicidal ideation risks missing critical information and valuable opportunities to intervene. We have successfully used remote screeners that include questions on suicidal ideation and have implemented systems and safety protocols to manage such situations. These include obtaining emergency contact information and the patient's location prior to screening.
We also synthesized barriers to implementing the technologies and the proposed solutions. Our study identified multiple barriers for implementing RMTs including technological challenges, user-related factors, legal and ethical concerns, research-related limitations, and difficulties in integrating these technologies into clinical practices (Table 2). Not all barriers have clear or practical solutions. For example, the repetitive nature of standard mental health questionnaires is a major challenge in maintaining patient engagement. While passive data collection could address this issue (6), it may not be feasible due to patient reluctance, high costs, and the lack of necessity for continuous data collection. Additionally, the data collected from surveys often provide different or additional insight than what is collected from passive devices.
Some hospitals are testing ways to make the user experience more seamless (43–45). For example, partnerships with human factors engineers have been established to study workflow and user interaction with screening tools. This process is iterative and involves qualitative interviews with both staff and patients. The goal is to improve engagement with the tools and reduce the time required to complete questionnaires based on user feedback. In some cases, local hospital teams have been actively involved in developing the software. By leveraging resources already available within the hospital, these efforts aim to ensure the sustainability of software maintenance. This approach also keeps the data within the hospital's systems, making it accessible to patients and protected under HIPAA regulations, rather than becoming the property of external vendors. While this model requires upfront investment from the hospital, it avoids the ongoing maintenance fees associated with commercial products—particularly beneficial in settings with lower patient volumes. Additional efforts include the development of clinician dashboards to monitor patient progress, as well as mobile apps that allow patients to track their own progress. However, adding an app may introduce another step in the process and may not always be perceived as useful by patients. Still, it could provide a secure channel for communication between clinicians and patients. Surveys can also be integrated into the app to assess patient perceptions and gather feedback on the clinical services received.
Most studies identifying barriers relied on interviews with users, including patients and practitioners, and some proposed potential solutions (1, 6, 23, 39). However, no empirical studies have examined the impact of success factors on the effective implementation of RMTs. While the implementation of RMTs in healthcare presents several challenges, the adoption of codesign with users, easy-to-use design, training, the monitoring of patients' perception, clinicians' buy-in, the enhancement of security and privacy measures, multi-method data collection, and automated data analysis can be effective in addressing these barriers, making RMTs a more viable option for remote healthcare, ultimately improving patient engagement and health outcomes. Specifically, security is one of the major challenges in digital mental health, and recent studies are proposing novel frameworks to address it (46).
Although RMTs can enhance access, save costs, collect continuous and detailed data that can be used for self-monitoring and feedback to the healthcare providers (1), and assists in personalized interventions (8, 47–49), it does not replace face-to-face care (41). This review and our experience have shown that patients engage better with RMT if they have been introduced to it by a trusted provider (39). It is also possible that retention and continued engagement would increase if there is a mix of RMT and in person contact including messaging and phone calls. Personal contact prior to use of RMT could influence attitude and increase perceived control thus improving adherence based on the theory of planned behavior (50).
5 Limitations
This study has multiple limitations. First, this focused review is designed to answer specific questions we encountered when developing a remote screening system in our hospital which focuses only on screening. For example, our keywords do not include telemedicine, which encompasses a wide range of services such as treatment and care management. Studies that used alternative terms such as e-screening may have been missed due to our limited keywords. Second, unlike systematic literature review, this study does not assess potential biases or the quality of the papers included. The selection of studies was guided by their scope rather than their methodological quality. Future work could benefit from evaluating both scope and quality. Third, we used only three databases to identify relevant papers, and including additional databases could reduce the likelihood of missing relevant papers. Multiple recent systematic literature reviews exist that have addressed these limitations (1, 2, 11, 41).
6 Conclusion
Remote Measurement Technologies (RMTs) offer promising avenues for enhancing mental health assessment and care, but their implementation remains complex and context-dependent. Our review identified commonly used devices and questionnaires, as well as multifaceted barriers including technological, user-related, legal, ethical, and integration challenges. While some healthcare settings are actively testing innovative, user-centered solutions—such as incorporating human factors design, building internal systems, and developing mobile apps—widespread adoption still faces hurdles. Our findings underscore the importance of aligning RMT design with patient needs, clinical workflows, and privacy standards. Crucially, successful implementation may depend on hybrid approaches that combine RMTs with trusted human interaction. Future empirical research is needed to evaluate which strategies most effectively support engagement and long-term use, helping realize the full potential of RMTs in mental healthcare.
Author's note
The authors are solely responsible for this document’s contents, findings, and conclusions, which do not necessarily represent the views of AHRQ. Readers should not interpret any statement in this report as an official position of AHRQ.
Author contributions
NQ: Data curation, Investigation, Writing – original draft, Writing – review & editing. TS: Data curation, Investigation, Writing – original draft, Writing – review & editing. FS: Methodology, Project administration, Visualization, Writing – original draft, Writing – review & editing. NH: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. LJ: Conceptualization, Writing – review & editing. LS: Conceptualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was funded under grant number R18HS029458 from the Agency for Healthcare Research and Quality (AHRQ), U.S. Department of Health and Human Services (HHS).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Walsh AE, Naughton G, Sharpe T, Zajkowska Z, Malys M, Van Heerden A, et al. A collaborative realist review of remote measurement technologies for depression in young people. Nat Hum Behav. (2024) 8(3):480–92. doi: 10.1038/s41562-023-01793-5
2. Goldberg SB, Buck B, Raphaely S, Fortney JC. Measuring psychiatric symptoms remotely: a systematic review of remote measurement-based care. Curr Psychiatry Rep. (2018) 20:1–12. doi: 10.1007/s11920-018-0958-z
3. Wies B, Landers C, Ienca M. Digital mental health for young people: a scoping review of ethical promises and challenges. Front Digit Health. (2021) 3:697072. doi: 10.3389/fdgth.2021.697072
4. Banbury A, Roots A, Nancarrow S. Rapid review of applications of e-health and remote monitoring for rural residents. Aust J Rural Health. (2014) 22(5):211–22. doi: 10.1111/ajr.12127
5. Bardram JE. Remote assessment in healthcare—technologies, methods, benefits, and challenges. PLoS One. (2023) 18(4):e0283945. doi: 10.1371/journal.pone.0283945
6. De Angel V, Lewis S, White KM, Matcham F, Hotopf M. Clinical targets and attitudes toward implementing digital health tools for remote measurement in treatment for depression: focus groups with patients and clinicians. JMIR Ment Health. (2022) 9(8):e38934. doi: 10.2196/38934
7. De Angel V, Lewis S, Munir S, Matcham F, Dobson R, Hotopf M. Using digital health tools for the remote assessment of treatment prognosis in depression (RAPID): a study protocol for a feasibility study. BMJ Open. (2022) 12(5):e059258. doi: 10.1136/bmjopen-2021-059258
8. Kathan A, Harrer M, Küster L, Triantafyllopoulos A, He X, Milling M, et al. Personalised depression forecasting using mobile sensor data and ecological momentary assessment. Front Digit Health. (2022) 4:964582. doi: 10.3389/fdgth.2022.964582
9. Beldjerd MH, Lafouge A, Giorgi R, Le Corroller-Soriano A-G, Quarello E. Asynchronous tele-expertise (ASTE) for prenatal diagnosis is feasible and cost saving: results of a French case study. PLoS One. (2022) 17(8):e0269477. doi: 10.1371/journal.pone.0269477
10. You JH, Luk SW, Chow DY, Jiang X, Mak AD, Mak WW. Cost-effectiveness of internet-supported cognitive behavioral therapy for university students with anxiety symptoms: a Markov-model analysis. PLoS One. (2022) 17(5):e0268061. doi: 10.1371/journal.pone.0268061
11. Bufano P, Laurino M, Said S, Tognetti A, Menicucci D. Digital phenotyping for monitoring mental disorders: systematic review. J Med Internet Res. (2023) 25:e46778. doi: 10.2196/46778
12. Adler DA, Wang F, Mohr DC, Choudhury T. Machine learning for passive mental health symptom prediction: generalization across different longitudinal mobile sensing studies. PLoS One. (2022) 17(4):e0266516. doi: 10.1371/journal.pone.0266516
13. Baumel A, Edan S, Kane JM. Is there a trial bias impacting user engagement with unguided e-mental health interventions? A systematic comparison of published reports and real-world usage of the same programs. Transl Behav Med. (2019) 9:1020–33. doi: 10.1093/tbm/ibz147
14. Choudhary S, Thomas N, Ellenberger J, Srinivasan G, Cohen R. A machine learning approach for detecting digital behavioral patterns of depression using nonintrusive smartphone data (complementary path to patient health questionnaire-9 assessment): prospective observational study. JMIR Form Res. (2022) 6(5):e37736. doi: 10.2196/37736
15. De Angel V, Adeleye F, Zhang Y, Cummins N, Munir S, Lewis S, et al. The feasibility of implementing remote measurement technologies in psychological treatment for depression: mixed methods study on engagement. JMIR Ment Health. (2023) 10:e42866. doi: 10.2196/42866
16. Klein A, Clucas J, Krishnakumar A, Ghosh SS, Van Auken W, Thonet B, et al. Remote digital psychiatry for mobile mental health assessment and therapy: MindLogger platform development study. J Med Internet Res. (2021) 23(11):e22369. doi: 10.2196/22369
17. Matcham F, Carr E, White KM, Leightley D, Lamers F, Siddi S, et al. Predictors of engagement with remote sensing technologies for symptom measurement in Major depressive disorder. J Affect Disord. (2022) 310:106–15. doi: 10.1016/j.jad.2022.05.005
18. Matcham F, Leightley D, Siddi S, Lamers F, White KM, Annas P, et al. Remote assessment of disease and relapse in Major depressive disorder (RADAR-MDD): recruitment, retention, and data availability in a longitudinal remote measurement study. BMC Psychiatry. (2022) 22:136. doi: 10.1186/s12888-022-03753-1
19. Pardes A, Lynch W, Miclette M, Mcgeoch E, Daly BP. Use of a mobile health (mHealth) platform for remote assessment of suicidal ideation, depression, and anxiety: a longitudinal retrospective study. Innov Digit Health Diagn Biomark. (2022) 2:8–15. doi: 10.36401/IDDB-21-03
20. Edward Thomas J, Richardson-Vejlgaard R. Remote behavioral sampling for psychological assessment: using interactive technologies to detect depression. Grad Stud J Psychol. (2023) 17:45–55. doi: 10.52214/gsjp.v17i.10919
21. Thompson A, Naidoo D, Becker E, Trentino KM, Rooprai D, Lee K. Remote monitoring and virtual appointments for the assessment and management of depression via the Co-HIVE model of care: a qualitative descriptive study of patient experiences. Healthcare. (2024) 12:2084. doi: 10.3390/healthcare12202084
22. White KM, Carr E, Leightley D, Matcham F, Conde P, Ranjan Y, et al. Engagement with a remote symptom-tracking platform among participants with major depressive disorder: randomized controlled trial. JMIR Mhealth Uhealth. (2024) 12:e44214. doi: 10.2196/44214
23. White KM, Dawe-Lane E, Siddi S, Lamers F, Simblett S, Alacid GR, et al. Understanding the subjective experience of long-term remote measurement technology use for symptom tracking in people with depression: multisite longitudinal qualitative analysis. JMIR Hum Factors. (2023) 10:e39479. doi: 10.2196/39479
24. Zhang Y, Folarin AA, Dineley J, Conde P, De Angel V, Sun S, et al. Identifying depression-related topics in smartphone-collected free-response speech recordings using an automatic speech recognition system and a deep learning topic model. J Affect Disord. (2024) 355:40–9. doi: 10.1016/j.jad.2024.03.106
25. Godleski L, Nieves JE, Darkins A, Lehmann L. VA Telemental health: suicide assessment. Behav Sci Law. (2008) 26(3):271–86. doi: 10.1002/bsl.811
26. Kobak KA, Williams JB, Engelhardt N. A comparison of face-to-face and remote assessment of inter-rater reliability on the Hamilton depression rating scale via videoconferencing. Psychiatry Res. (2008) 158(1):99–103. doi: 10.1016/j.psychres.2007.06.025
27. Kobak KA, Williams JB, Jeglic E, Salvucci D, Sharp IR. Face-to-face versus remote administration of the montgomery–asberg depression rating scale using videoconference and telephone. Depress Anxiety. (2008) 25:913–9. doi: 10.1002/da.20392
28. Jiang Z, Seyedi S, Griner E, Abbasi A, Bahrami Rad A, Kwon H, et al. Multimodal mental health assessment with remote interviews using facial, vocal, linguistic, and cardiovascular patterns. medRxiv, 2023.09.11.23295212. (2023).
29. Olah J, Diederen K, Gibbs-Dean T, Kempton MJ, Dobson R, Spencer T, et al. Online speech assessment of the psychotic spectrum: exploring the relationship between overlapping acoustic markers of schizotypy, depression and anxiety. Schizophr Res. (2023) 259:11–9. doi: 10.1016/j.schres.2023.03.044
30. Contreras C, Santa Cruz J, Galea JT, Chu AL, Puma D, Ramos L, et al. Programmatic implementation of depression screening and remote mental health support sessions for persons recently diagnosed with TB in Lima, Peru during the COVID-19 pandemic. Glob Ment Health (Camb). (2024) 11:e59. doi: 10.1017/gmh.2024.21
31. Mandryk RL, Birk MV, Vedress S, Wiley K, Reid E, Berger P, et al. Remote assessment of depression using digital biomarkers from cognitive tasks. Front Psychol. (2021) 12:767507. doi: 10.3389/fpsyg.2021.767507
32. Nielssen O, Dear BF, Staples LG, Dear R, Ryan K, Purtell C, et al. Procedures for risk management and a review of crisis referrals from the MindSpot Clinic, a national service for the remote assessment and treatment of anxiety and depression. BMC Psychiatry. (2015) 15:1–6. doi: 10.1186/s12888-015-0676-6
33. White KM, Williamson C, Bergou N, Oetzmann C, De Angel V, Matcham F, et al. Exploring the definition, measurement, and reporting of engagement in remote measurement studies for physical and mental health symptom tracking: a systematic review (2022).
34. Munger Clary HM, Snively BM, Kumi-Ansu Y, Alexander HB, Kimball J, Duncan P, et al. Quality of life during usual epilepsy care for anxiety or depression symptoms: secondary patient-reported outcomes in a randomized trial of remote assessment methods. Epilepsy Res. (2024) 204:107396. doi: 10.1016/j.eplepsyres.2024.107396
35. Giansanti D, Siotto M, Maccioni G, Aprile I. A remote assessment of anxiety on young people: towards their views and their different pet interaction. Healthcare. (2022) 10(7):1242. doi: 10.3390/healthcare10071242
36. Doarn CR, Shore J, Ferguson S, Jordan PJ, Saiki S, Poropatich RK. Challenges, Solutions, and Best Practices in Telemental Health Service Delivery Across the Pacific Rim—a Summary. New Rochelle, NY USA: Mary Ann Liebert, Inc (2012).
37. Oetzmann C, White KM, Ivan A, Julie J, Leightley D, Lavelle G, et al. Lessons learned from recruiting into a longitudinal remote measurement study in major depressive disorder. NPJ Digit Med. (2022) 5:133. doi: 10.1038/s41746-022-00680-z
38. Simblett S, Matcham F, Siddi S, Bulgari V, Di San Pietro CB, López JH, et al. Barriers to and facilitators of engagement with mHealth technology for remote measurement and management of depression: qualitative analysis. JMIR Mhealth Uhealth. (2019) 7(1):e11325. doi: 10.2196/11325
39. Funnell EL, Spadaro B, Martin-Key NA, Benacek J, Bahn S. Perception of apps for mental health assessment with recommendations for future design: United Kingdom semistructured interview study. JMIR Form Res. (2024) 8:e48881. doi: 10.2196/48881
40. Wright HM, Fuessel-Hermann D, Pazdera M, Lee S, Ridge B, Kim JU, et al. Preventative care in first responder mental health: focusing on access and utilization via stepped telehealth care. Front Health Serv. (2022) 2:848138. doi: 10.3389/frhs.2022.848138
41. Andrews JA, Craven MP, Lang AR, Guo B, Morriss R, Hollis C, et al. Making remote measurement technology work in multiple sclerosis, epilepsy and depression: survey of healthcare professionals. BMC Med Inform Decis Mak. (2022) 22:125. doi: 10.1186/s12911-022-01856-z
42. Verduin TL. 8.4 Development of an integrated clinical informatics system to support a unified system of care for adolescent depression. J Am Acad Child Adolesc Psychiatry. (2018) 57:S13.
43. Lagoski M, Soghier L, Lagata J, Shivers M, Sadler E, Fischer E, et al. Mental health support and screening for mood disorders for caregivers in the neonatal intensive care unit: is the call to arms being answered? Am J Perinatol. (2025) 42(03):320–6. doi: 10.1055/a-2353-0993
44. Sadjadpour F, Hosseinichimeh N, Jarvis L, Perazzo S, Soghier L. A participatory approach to enhance screening system for perinatal mood and anxiety disorder in critical care settings. Syst Res Behav Sci. (2025). doi: 10.1002/sres.3173
45. Sadler EM, Okito O, Soghier L. Addressing caregiver mental health in the neonatal ICU. Curr Opin Pediatr. (2023) 35(3):390–7. doi: 10.1097/MOP.0000000000001242
46. Georgiou D, Katsaounis S, Tsanakas P, Maglogiannis I, Gallos P. Towards a secure cloud repository architecture for the continuous monitoring of patients with mental disorders. Front Digit Health. (2025) 7:1567702. doi: 10.3389/fdgth.2025.1567702
47. Abbas A, Sauder C, Yadav V, Koesmahargyo V, Aghjayan A, Marecki S, et al. Remote digital measurement of facial and vocal markers of Major depressive disorder severity and treatment response: a pilot study. Front Digit Health. (2021) 3:610006. doi: 10.3389/fdgth.2021.610006
48. Hornstein S, Zantvoort K, Lueken U, Funk B, Hilbert K. Personalization strategies in digital mental health interventions: a systematic review and conceptual framework for depressive symptoms. Front Digit Health. (2023) 5:1170002. doi: 10.3389/fdgth.2023.1170002
49. Wanniarachchi VU, Greenhalgh C, Choi A, Warren JR. Personalization variables in digital mental health interventions for depression and anxiety in adolescents and youth: a scoping review. Front Digit Health. (2025) 7:1500220. doi: 10.3389/fdgth.2025.1500220
Keywords: remote measurement technologies (RMTs), barriers of implementing RMTs, solutions to enhance use of RMTs, assessment surveys, mental health
Citation: Quiram N, Salam T, Sadjadpour F, Hosseinichimeh N, Jarvis L and Soghier L (2025) A literature review of remote mental health screening: barriers, potential solutions, and tools. Front. Digit. Health 7:1670691. doi: 10.3389/fdgth.2025.1670691
Received: 22 July 2025; Accepted: 26 September 2025;
Published: 13 October 2025.
Edited by:
Luca Steardo Jr, University Magna Graecia of Catanzaro, ItalyReviewed by:
Pasquale Bufano, Institute of Clinical Physiology, National Research Council (CNR), ItalyJames Pittman, United States Department of Veterans Affairs, United States
Copyright: © 2025 Quiram, Salam, Sadjadpour, Hosseinichimeh, Jarvis and Soghier. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nicole Quiram, bnF1aXJhbUB2dC5lZHU=
 Nicole Quiram
Nicole Quiram Tamjid Salam1,2
Tamjid Salam1,2 Fatima Sadjadpour
Fatima Sadjadpour Niyousha Hosseinichimeh
Niyousha Hosseinichimeh Lamia Soghier
Lamia Soghier