Abstract
Background:
Sierra Leone has advanced its digital health agenda. However, digital literacy among frontline health workers remains low, with over 82% reporting limited confidence in using digital tools. The health workforce also recorded the lowest digital health maturity score among all enablers in the WHO Global Digital Health Monitor, underscoring the need for workforce upskilling as a foundation for digital transformation.
Objective:
This paper describes the design, implementation, and outcomes of a foundational digital literacy training program for frontline health workers under the Digital Innovation in Pandemic Control (DIPC) project, aimed at improving readiness for digital tool adoption.
Methods:
A training needs analysis (TNA) aligned skill gaps with the competencies required for using the electronic Stock Management Tool (eSMT). Training modules were adapted from the European Commission's DigComp framework, contextualized for Sierra Leone, and delivered through a blended learning model. Post-training competency gains were assessed to determine effectiveness.
Results (Implementation):
Among 150 trained health workers, “high understanding” in basic computer literacy increased from 7.1% to 72.2%, while “low understanding” dropped from 65.9% to 9.2%. For computer troubleshooting skills, “high understanding” rose from 4.4% to 73.8%. Both courses showed large effect sizes (Cohen's d = 1.3–2.1), indicating substantial learning gains.
Conclusions:
Systematic digital literacy training, grounded in competency frameworks and contextual design, can substantially improve digital readiness among frontline health workers. Such interventions are essential foundations for sustainable digital transformation in health systems.
Introduction
Overview
Adoption of digital technologies in the health sector has witnessed rapid increase in recent years (1). The global COVID-19 pandemic threat has significantly contributed to this trend (2, 59). Though not without challenges, many LMICs continue to adopt these technologies to advance healthcare (3, 4). Digital technologies have no doubt shown promise in effectively addressing health systems challenges (5) informing their recommended scale-up to achieve greater impact (6, 7).
Table 1
| Level | Points | Description |
|---|---|---|
| L1 | 0–5 | No understanding |
| L2 | 6–10 | Very low understanding |
| L3 | 11–15 | Low understanding |
| L4 | 16–20 | Average understanding |
| L5 | 21–25 | High understanding |
| L6 | 26–30 | Very high understanding |
Digital literacy scale.
However, implementation outcomes in digital health initiatives are influenced not only by infrastructure, but also by factors such as institutional readiness, user confidence, and behavioral responses to new technologies (8). This underscores the need to consider human and organizational factors when assessing digital transformation. Successful adoption of digital health solutions depends on the systematic understanding of these dimensions and the integration of relevant theoretical frameworks throughout the design and implementation phases.
Theoretical framework: technology acceptance, self-efficacy and e-readiness
Digital health adoption is shaped by complex interactions between individual, organizational, and contextual determinants. The Technology Acceptance Model (TAM) (9) posits that users' adoption decisions are influenced by perceived usefulness and perceived ease of use, which in turn affect behavioral intention and system use. In healthcare, these perceptions are strongly mediated by self-efficacy, the belief in one's ability to successfully perform technology-related tasks (10). Low self-efficacy has been linked to low confidence and resistance to digital innovation, while training interventions that improve competence and confidence strengthen both perceived ease of use and perceived usefulness (11).
Furthermore, the degree of e-readiness—the preparedness of individuals, institutions, and systems to adopt and sustain digital technologies (12), moderates these relationships. E-readiness encompasses access to digital infrastructure, leadership commitment, policies, and skills alignment. Integrating these theories provides a more holistic understanding of how workforce training can translate into actual technology use and institutional transformation, particularly in low-resource settings.
Digital transformation
Efforts to unlock digital transformation gains are often hampered by digital literacy gaps among health workforce as evident during the COVID-19 pandemic (2, 11). Addressing these gaps through computer skills training alone are incapable of advancing digital transformation (13). For digital transformation to occur, a wide range of competencies must be applied to create new knowledge, innovate and communicate (14, 15). Healthcare professionals need digital readiness by acquiring these competencies (16). This differentiates digital literacy from computer literacy. Digital literacy involves the mastery of simple and practical skills required to be digitally intelligent and creative (60), and to effectively compete in the 21st century (17). This is critical in protecting against the associated risk of digital investments (18).
Training needs analysis
Training Needs Analysis (TNA) is an essential first step in designing and developing effective training programmes (19). It aligns training goals with potential constraints faced by health workers and relevant competencies required to perform a specific task (20, 21). Many studies have demonstrated the positive linkages between TNA and achievement of training program goals (22, 23). This correlation stems from leveraging gaps identified from TNA, guided by the training goals for developing a contextual competency framework (24).
Digital health competency framework development
Competency framework outlines the specific knowledge, skills and attitude required by job roles to successfully complete assigned tasks (25). Global digital literacy competency frameworks are well documented in literature. Each framework provides a reference targeting specific objectives – to achieve SDG Indicator 4.4.2 (26), foster emerging digital economies (27) and understand child-related digital literacy needs (60). The European Commission's Digital literacy framework (DigCom) provides 5 adaptable conceptual learning models for citizens and non-IT professionals (25). However, the Global Digital Health Literacy competency framework is currently under development (28).
Novelty and research gap
While several studies have explored digital health literacy, they have largely focused on non-professional populations and academic or adolescent cohorts rather than on frontline health workers operating in real health system contexts. For example (29), assessed digital health literacy among students in Iran using a cross-sectional design but did not evaluate structured training interventions. Similarly (30),co-designed an educational resource for adolescents but did not assess its operational utility in healthcare delivery (31). Examined the relationship between digital literacy, trust, and health anxiety, yet their scope remained limited to non-clinical environments (10). Demonstrated that self-efficacy mediates the relationship between digital literacy and self-management behaviors, but their work was restricted to college students and lacked application to professional healthcare roles. Other related studies have similarly concentrated on general populations outside formal health system operations.
In contrast, this study is the first to document an applied digital literacy intervention targeted at frontline immunization officers in low-resource settings, integrating a competency-based training framework with operational digital tools deployed for pandemic control. Unlike previous works, it combines pre-deployment readiness assessment, context-specific skills training, and evaluation of post-training knowledge gains within a live national health project. This approach addresses the critical implementation gap between digital literacy theory and operational practice, contributing new empirical evidence on how structured training interventions can strengthen workforce preparedness and digital transformation in LMIC health systems.
Blended learning
Appropriate training delivery approach is crucial to ensuring timeliness and addressing diverse learning needs (32, 33). Blended learning involves a combination of face-to-face direct facilitation, and self-paced online learning (34, 35). Previous studies have shown its ability to compensate the disadvantages of traditional learning and online learning (36), improve performance and critical thinking (37), promote skill development (38), enhance self-management in learning and motivation (39), and provide a satisfactory learning experience (40).
Knowledge evaluation
Knowledge evaluation measures how well frontline health workers' skills match the tasks required to effectively operate a digital health application (41). This is crucial to determining the effectiveness of the training programme. However, post training knowledge gains were shown to depreciate significantly over time justifying the need for continuous training (42). Moreso, the availability of lifelong learning opportunities significantly contributes to the effectiveness of any digital literacy training program (43).
Change management
Change management is a system of providing continuous end user support to address potential risks associated with adoption and use of new technologies (44). Adoption risks include unintended consequences arising from new digital culture and resulting in resistance (45). Many studies have linked unsatisfactory end user experience with resistance to change (46–49).
Digital innovation in pandemic control (DIPC) project
The Sierra Leone Digital Innovation in Pandemic Control (DIPC) commenced in 2023 as part of post COVID-19 resilience building. It aimed to improve vaccine stock management and prevent stock-outs and wastages from expiry (50). Consequently, the electronic Stock Management Tool (eSMT) application was deployed across 96 CHCs in 4 selected Districts.
This project faced potential threats from observed digital literacy gaps among intended end users - frontline immunization officers. Prior to DIPC, workforce had the lowest digital health maturity score amongst all digital health enablers (61). This was attributed to gaps in both pre-service and in-service digital literacy training (51). Existing trainings were often ad hoc, lecture-styled, and one-off without continuous support. This approach has limited impact on learning and performance (62). With increasing digitalization, health workers needed new skills to adopt digital technologies and improve health program performance.
Considering the importance of ensuring workforce readiness prior to deployment of digital technology (43), a national digital literacy gap assessment was conducted in 2022. This assessment revealed 82% of frontline health workers rated themselves as having low confidence level to effectively operate a computer device and utilize ICT applications without technical assistance (51). The same report revealed that minor troubleshooting issues significantly contributed to over 12.4% of computer devices found to be non-functional. Addressing this situation required an effective approach to building the critical mass of digitally skilled health workforce required to facilitate the DIPC project and support the digital transformation drive. This informed the design and implementation of the digital literacy skills training programme.
This paper elaborates the processes and lessons learned from implementing digital literacy skills intervention program in Sierra Leone as part of enhancing vaccine logistics, real-time data management, and digital transformation in healthcare in the post COVID-19 era.
Objectives
Motivated by the opportunity to share lessons learned in addressing challenges of low digital skilling of health workforce, this paper highlights the processes and lessons learned in implementing a competency-based foundational digital literacy skills intervention program to support achievement of the DIPC project goals and overarching digital health vision in Sierra Leone (62).
Methods
Overview
The goal of our training program was to empower 150 frontline immunization officers at the 96 Comprehensive Health Centres (CHC) selected for the DIPC project with the minimum competency required to effectively use the eSMT application. A TNA was conducted to define required competencies, develop training modules and design the training approach.
Training needs analysis
TNA involved a hierarchical approach utilized to analyze the competencies required for the DIPC training goals (21, 52). Current competency gaps were identified using a self-reporting technology confidence tool and responses from 338 frontline health workers. This tool has been effectively applied in multiple studies to align digital literacy requirements with operational tasks (41, 53). Assessment gaps were adapted to training needs and aligned with the DigCom 2.2 framework to define the necessary skills and proficiency levels, which informed the development of training modules validated by a digital literacy work group.
Training module development
A multi-stakeholder digital literacy work group was set up at the Ministry of Health (MoH) to develop contextualized training modules. The group membership included technical officers from the Ministry of Communications, Technology and Information (MoCTI), the Directorate of Science, Technology and Innovation (DSTI) and development partners. Existing digital literacy training modules from these organizations were consolidated and enhanced using locally relevant content, interactive videos with local language narration, and self-paced sub-modules in alignment with multimedia principles (54).
Training cascade
Seventeen National and District levels immunization supervisors and ICT officers were trained on both digital literacy skills training facilitation and coaching skills. They were then supported to cascade the training to 150 immunization officers across 96 PHC facilities and 20 district level immunization officers and supervisors across the four DIPC districts. A face-to-face, direct hands-on training was conducted over a 4-day period. Each trainee was provided with a laptop device and internet connectivity. Instructional materials were competency focused and interactive with in-course test questions, direct simulations and individual skills practice sessions. The basic computer literacy and internet skills training course was delivered first to lay the foundation for the basic troubleshooting course which followed thereafter.
Competency gain evaluation
A self-evaluating, identical pre and post-test questionnaire comprising 30 objective questions adapted from both training modules was administered to each of the 150 trainees. Only 139 and 142 trainees successfully completed both pre and post-test evaluation assessments for both courses respectively. Each correct answer was assigned 1 point while a wrong answer was assigned 0 point. The minimum and maximum possible scores for each participant ranged from 0 to 30 points respectively. A tool for measuring competency gain, based on the Digital Literacy Scale (DLS) shown in Table 1 and proven effective in assessing digital competency improvements, was adapted for use (11, 18, 55). To ensure cultural relevance and measurement accuracy, the adapted tool was reviewed and validated by the Ministry of Health and key national stakeholders before implementation. The adapted DLS was then used to grade the scores into six levels of understanding ranging from “no understanding” to “very high understanding”. The changes in the level of understanding between pre- and post-tests were compared to determine the competency gain for both courses. Post-course evaluation feedback survey was conducted at the end of both modules to measure training relevance and satisfaction.
Change management
Continuous onsite coaching and mentoring support was provided to end users in addition to the blended learning approach adopted. We trained National and District levels coaches and supported them to conduct monthly on-the-job skills reinforcement coaching after the initial hands-on training. This aimed to facilitate the shift to a digital culture and shorten the learning curve for the eSMT application. Performance coaching technique was adopted due to its effectiveness in addressing both end-users learning barriers and meeting program performance goals (56). Additionally, lessons learned in previous coaching sessions were reflected upon and end users were actively involved in deciding the dates, duration and discussion for each coaching visit. This is crucial to achieving successful coaching (57). A virtual help desk platform was also created on WhatsApp to provide offsite remote support after the training and in between coaching visits.
Results
Training needs analysis
Confidence level assessment for identified tasks
A total of 338 healthcare professionals from 14 primary and secondary healthcare facilities completed the self-reported confidence level assessment tool regarding their ability to perform basic computer tasks. Participants indicated their comfort level with tasks such as basic device management, application navigation, document management, internet browsing, and email communication. The respondent demographics included Nurses (51.2%), Community Health Officers/Assistants (26.9%), Laboratory Scientists/Technicians (6.5%), Administrative Staff (4.1%), Doctors (11%), Pharmacists (2.1%), and Data Clerks/Monitoring and Evaluation Officers (5.9%). Analysis of the results revealed that a significant majority, 82.8% of healthcare workers reported feeling unconfident in performing basic computer tasks (Figure 1). Meanwhile, 13% expressed confidence, and only 4.2% felt very confident in their abilities. These findings highlighted a substantial need for targeted training programs to enhance digital competency among healthcare workers.
Figure 1
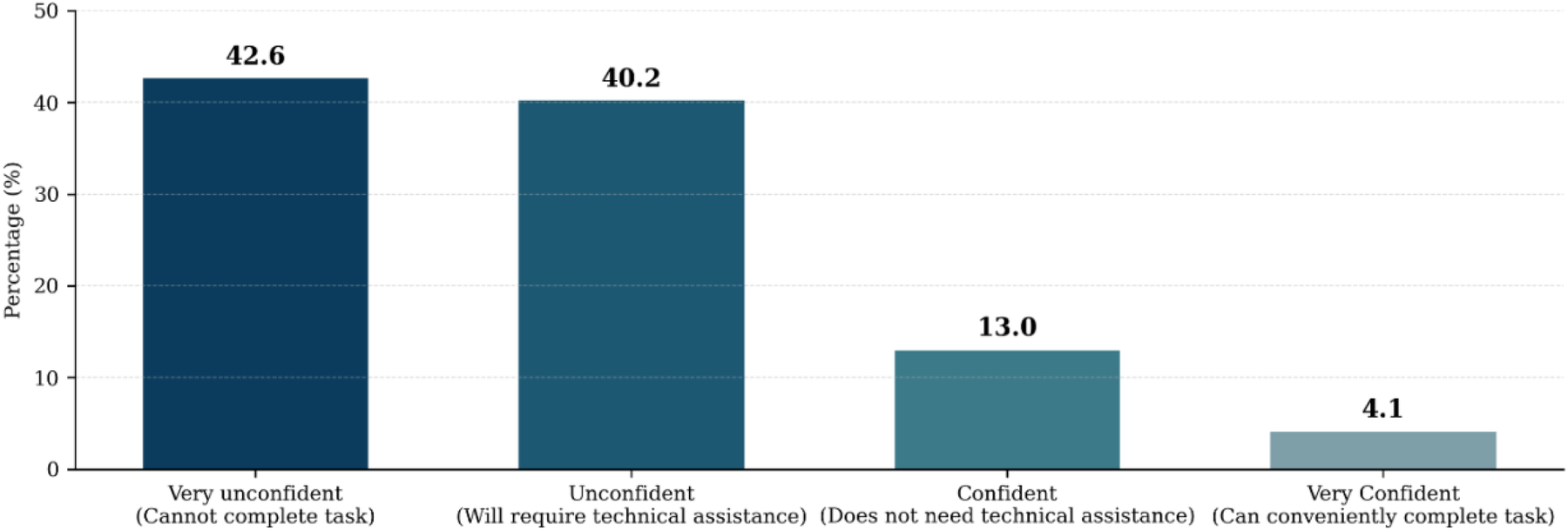
Self-reported pre-training digital competency confidence levels among healthcare workers.
Training module development
The training modules were developed by aligning training requirements identified from the TNA with the DigCom 2.2 digital competency framework (Table 2). This informed the proficiency level and content for the seventeen training modules developed for both Basic Computer Literacy and Internet Skills (BCLIS) and Basic Computer Troubleshooting Skills (BCTS). The foundational proficiency level was selected for the courses given the need to build foundational abilities before advancing to specialized skills (58). The module content informed by the corresponding DigCom 2.2 competence was collaboratively created using resources from the Ministry of Health (MoH), implementing partners, the Ministry of Communications, Technology, and Innovations (MoCTI), and credible online sources. To address linguistic diversity among the health workers, language and multimedia enhancements in the widely spoken Krio language were incorporated into the modules (25).
Table 2
| Training needs based on TNA | DigCom 2.2 competence area | Proficiency level | Competence | Corresponding Training Module |
|---|---|---|---|---|
| Identify computer parts, desktop icons and how to use them. | Information and Data Literacy | Foundational | Managing data, information, and digital content | BCLIS Module 1 (A–E), 2 |
| Learning simple methods to organize, store, and retrieve data and digital content using the home screen, desktop icons, and task bar | ||||
| Creating a digital identity, setting up and using email, composing and sending messages, and understanding common email terminology | Communication and Collaboration | Foundational | Managing digital identities | 5, 6, 7 |
| Creating and editing simple documents, including typing, saving, locating, and opening files | Digital Content Creation | Foundational | Developing digital content | 3, 6 |
| Securing devices and data, practicing safe online behaviors, identifying security threats, and knowing appropriate actions to protect digital content | Safety | Foundational | Protecting devices, personal data and privacy | 4 |
| Addressing basic computer hardware and software problems effectively | Problem solving | Foundational | Solving technical problems while operating device | BCTS Modules 1–10 |
Mapping identified training needs to DigCom 2.2 digital competence framework.
Training outcomes
Pre and Post-Test questionnaires were administered to the trainees for both BCLIS (n = 139) and BCTS (n = 142). Test scores for each trainee were recorded and categorized into the six level of understanding or competency (L1-L6) using the class interval method. Each level of understanding was then allocated corresponding points as follows: “No understanding – 1”, “ Very Low understanding – 2”, “Low Understanding = 3”, “Average understanding = 4”, “High level of understanding = 5”, “ Very high (Advanced) level of understanding = 6”. Therefore, the maximum point allocated for each level is 6 and the minimum point is 1. The percentage of scores for “No”, “Low”, “Average” and “High” levels of understanding for each course was calculated and compared between pre and post tests to determine competency gain (Table 3).
Table 3
| Competency Level | Score Interval | Description | No of trainees (Pre-Test) | Maximum Score (Pre-Test) | Score % (Pre-Test) | Pre-test Mean (SD) | No of trainees (Post-Test) | Maximum Score (Post-Test) | Score % (Post-Test) | Post-test Mean (SD) | Statistics |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Basic Computer Literacy and Internet Skills Course | |||||||||||
| L1 | 0–5 | No understanding | 0 | 0 | 0 | 3.1 (0.8) | 0 | 0 | 0 | 4.9 (0.9) | t = −47.10, p < 0.001, d = 2.1, CI [1.8, 2.4]. |
| L2 | 6–10 | Very low understanding | 26 | 52 | 12 | 1 | 2 | 0.3 | |||
| L3 | 11–15 | Low understanding | 78 | 234 | 53.9 | 11 | 33 | 4.8 | |||
| L4 | 16–20 | Average understanding | 27 | 108 | 24.9 | 24 | 96 | 14.1 | |||
| L5 | 21–25 | High understanding | 8 | 40 | 9.2 | 67 | 335 | 49.1 | |||
| L6 | 26–30 | Very high understanding | 0 | 0 | 0 | 36 | 216 | 31.7 | |||
| Total | 139 | 434 | 100 | 139 | 682 | 100 | |||||
| Basic computer troubleshooting skills course | |||||||||||
| L1 | 0–5 | No understanding | 1 | 6 | 1.2 | 3.6 (0.9) | 0 | 0 | 0 | 4.8 (0.8) | t = −24.32, p < 0.001, d = 1.3, CI [1.1, 1.6]. |
| L2 | 6–10 | Very low understanding | 12 | 24 | 4.7 | 0 | 0 | 0 | |||
| L3 | 11–15 | Low understanding | 59 | 177 | 34.9 | 10 | 30 | 4.4 | |||
| L4 | 16–20 | Average understanding | 53 | 212 | 41.8 | 37 | 148 | 21.8 | |||
| L5 | 21–25 | High understanding | 14 | 70 | 13.8 | 69 | 345 | 50.8 | |||
| L6 | 26–30 | Very high understanding | 3 | 18 | 3.6 | 26 | 156 | 23 | |||
| Total | 142 | 507 | 100 | 142 | 679 | 100 | |||||
Pre-and post-training competency levels of frontline health workers in digital literacy courses.
Our comparative analysis of pre and post-tests shows a significant shift in the level of understanding between across both training courses (Figure 2). In the BCLIS course, “High or Very high level of understanding” (levels L5–L6, scores 21–30) significantly rose from 9.3% to 80.8%, while “Low or Very low level of understanding” (levels L2–L3,scores 6–15) also significantly declined from 65.9% to 9.2% between pre and post-test scores. Similarly, in the BCTS course, “High or Very high level of understanding” increased from 17.6% to 73.8%, with “Low or Very low level of understanding” dropping from 39.6% to 4.4%. Mean scores (SD 0.9) improved from 3.1 to 4.9 and 3.6 to 4.8 for both BCLIS and BCTS courses respectively. Post-training satisfaction was high (95%).
Figure 2
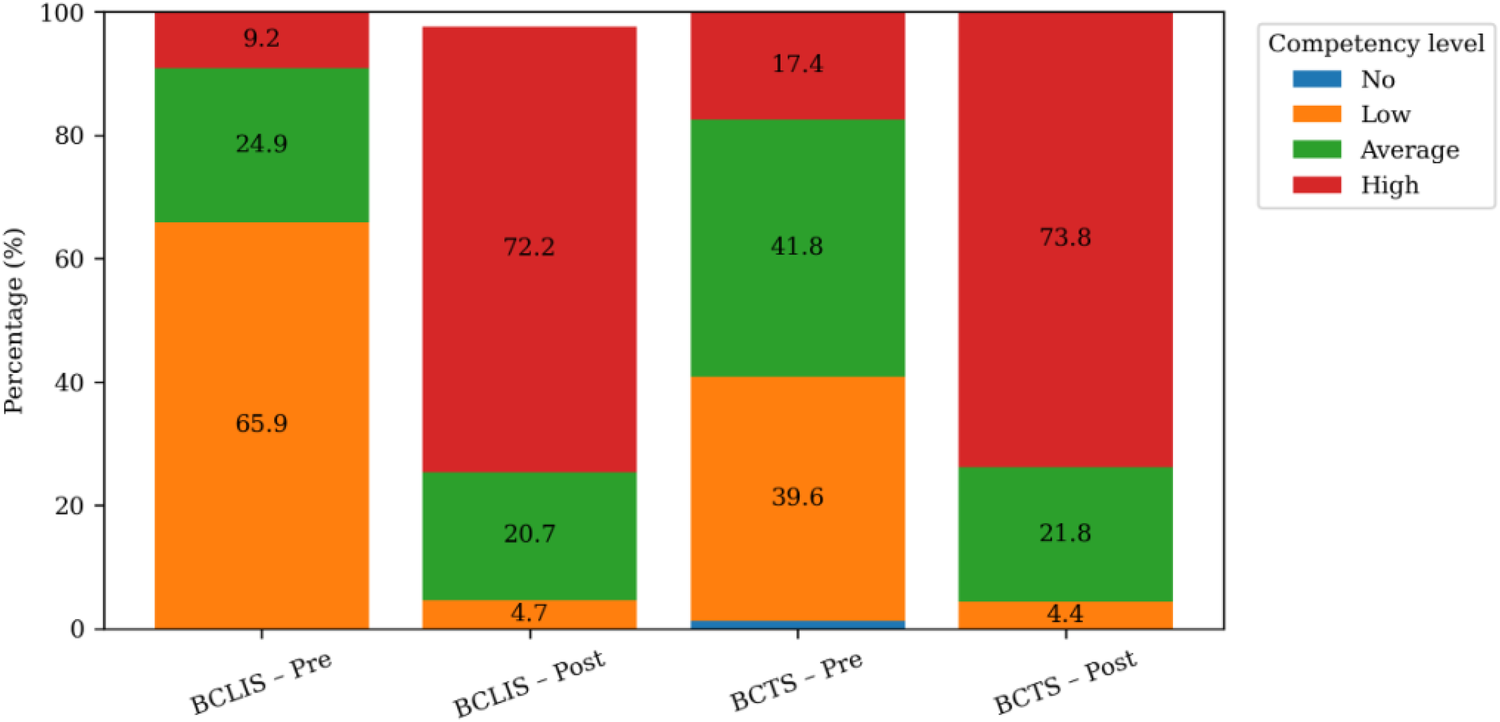
Improvement in digital literacy competency levels among health workers before and after BCLIS and BCTS training.
Statistical analysis of the training scores demonstrated significant and practically meaningful gains. Paired t-tests confirmed strong evidence of improvement in both BCLIS (t = 47.10, p < 0.001) and BCTS (t = 24.32, p < 0.001). Large effect sizes for BCLIS (Cohen's d = 2.1) and BCTS (Cohen's d = 1.3) reinforce the practical impact, with narrow confidence intervals indicating robust findings. These results underscore the effectiveness of targeted, context-appropriate digital literacy interventions for enhancing health workforce capacity in resource-limited settings.
Change management
Coaching was conducted onsite and was performance-based, with a focus on using the eSMT application to address key digital literacy challenges identified during the visits. Coaches reported satisfaction with the overall performance in 70% of the facilities visited. Following two rounds of coaching, self-assessment confidence levels among participants (n = 71) were 23.5% unconfident, 2.4% confident, and 57.7% very confident (Figure 3). This reflects a substantial reduction in the proportion of unconfident staff, dropping from 82.8% pre-training to 23.5% post-training.
Figure 3
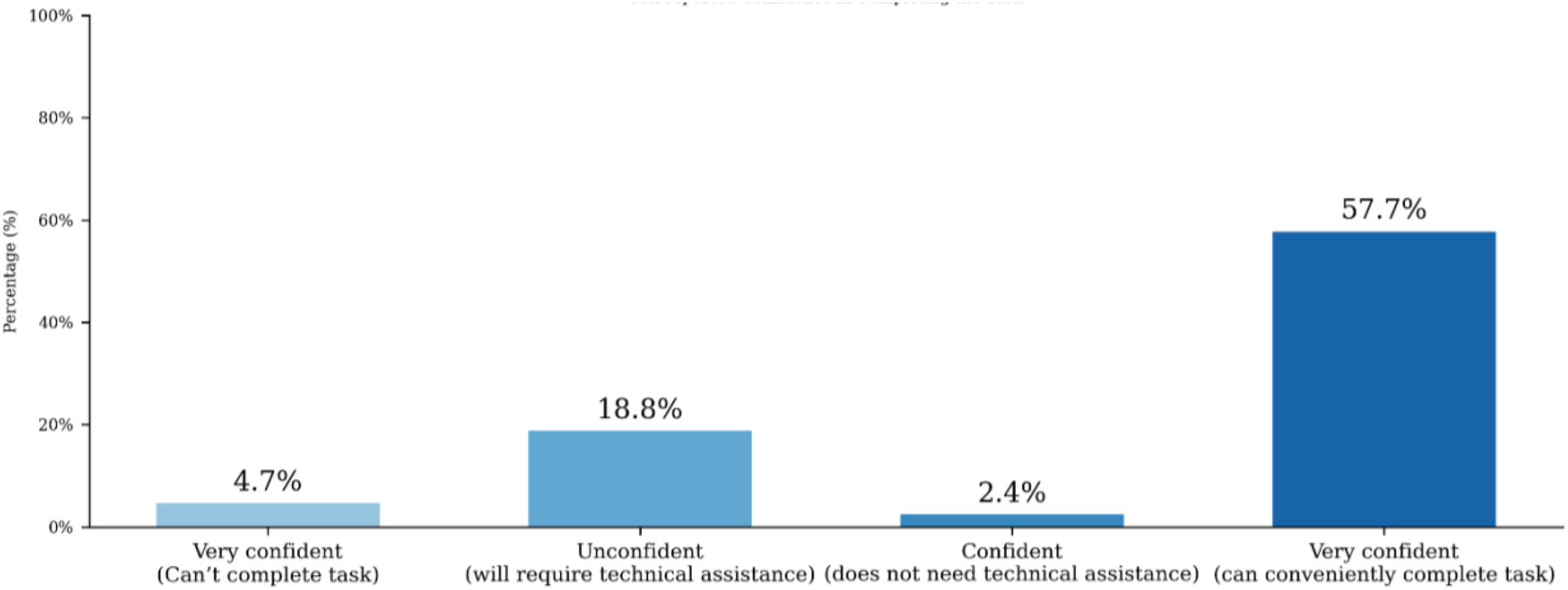
Change in self-reported confidence levels of health workers following digital literacy coaching.
Despite this improvement, the remaining 23.5% of participants who still felt unconfident likely reflect residual skill gaps and contextual barriers such as limited prior digital experience. Also, coaches reported inconsistent access to functioning devices in some health facilities. These findings suggest that continuous mentoring, peer learning, and periodic refresher sessions are essential to consolidate digital competence and ensure long-term behavioral change.
Discussion (lessons learned)
Digital health transformation and the need for early assessment of workforce readiness
A new digital culture is emerging in the health sector, compelling health workers to transition rapidly from manual, paper-based systems to digital platforms and data-driven workflows. This transition, however, is often constrained by limited e-Readiness, a key determinant of organizational and individual capacity to adopt new technologies. Previous studies identified inadequate readiness as a major factor behind failed digital health implementations (12). Our findings revealed that 82% of frontline health workers had low confidence levels in using digital technologies.
From the lens of the Technology Acceptance Model (TAM), such low self-efficacy negatively influences both perceived ease of use and perceived usefulness, two fundamental predictors of adoption behavior. The observed gaps therefore highlight the mediating role of digital readiness and self-efficacy in determining successful technology uptake. To address these factors, we employed a Training Needs Analysis (TNA) approach to align competencies with expected job tasks (21) and to build readiness prior to system deployment, consistent with capacity-building frameworks that emphasize pre-implementation user preparedness (43).
Localizing relevant content for effective digital literacy capacity building
The design of digital literacy interventions must transcend generic computer training to embed local realities and learning contexts. Aligning training programs solely with institutional goals is insufficient for meaningful behavioral change. Capacity building theory suggests, contextual relevance and experiential learning drive sustained knowledge retention and confidence (25, 32, 38). In our study, locally adapted content, multimedia learning in the Krio language, and blended delivery methods significantly enhanced competence gains.
Drawing on TAM and self-efficacy theory, the incorporation of interactive and accessible learning modalities increased users' perceived ease of use and sense of mastery, both of which function as mediators between training exposure and sustained digital application. Low-cadre health workers, previously constrained by anxiety or unfamiliarity, reported improved confidence and autonomy in operating digital tools, reinforcing the importance of designing interventions that build both technical skill and psychological readiness (10).
From digital competence to digital use: sustaining transformational change
True digital transformation extends beyond competency acquisition to consistent, confident digital use supported by enabling environments. Within the TAM framework, transformation occurs when perceived usefulness translates into actual behavioral intention and habitual usage. Our findings, where 60% of participants had their first computer experience during training, underscore the necessity of coupling skill acquisition with institutional support mechanisms such as device provision, connectivity, and peer mentorship.
Here, institutional support operates as a moderating factor that strengthens the link between digital literacy and technology adoption. Without such supportive conditions, even well-trained users may fail to translate competence into regular use. This reinforces the multidimensional nature of digital transformation, requiring synergy between individual capabilities and systemic enablers within the broader e-Readiness ecosystem (2).
Digital literacy coaching a mechanism for change management
Beyond formal instruction, the project integrated continuous coaching and virtual mentorship, reflecting principles of change management theory that emphasize iterative support during technology adoption. Simulation-based learning and individualized coaching promoted adaptive learning and helped overcome resistance, a common barrier in digital transitions (45).
From a theoretical standpoint, ongoing coaching acts as a reinforcement mechanism that sustains self-efficacy and mitigates the decay of perceived behavioral control over time. This aligns with capacity-building models emphasizing cyclical learning, reflection, and reinforcement to consolidate digital transformation.
Collaborative approaches for scaling and sustaining digital adoption
Collaboration with Ministry of Health partners facilitated the institutionalization of foundational digital literacy training as a prerequisite for deployment of specialized digital health applications. This systemic integration supports organizational e-Readiness by embedding human capacity development within national digital transformation strategies.
By situating these findings within the TAM and capacity-building frameworks, the study demonstrates that digital literacy training alone is insufficient. Sustainable adoption requires reinforcing mediating factors (self-efficacy, digital readiness) and moderating supports (institutional commitment, infrastructure). The intervention thus contributes new knowledge to the field by illustrating how a theoretically grounded, context-specific digital literacy program can accelerate workforce-level adoption and system-wide digital transformation in LMICs.
Theoretical and practical implications for digital health adoption
This study shows that a competency-based, contextually adapted, and blended digital literacy intervention effectively improved technical and behavioral adoption of technology. Unlike traditional lectures, this approach increased participants' self-efficacy and perceived relevance, core aspects of the Technology Acceptance Model (TAM). Digital literacy emerged as a key mediator between workforce readiness and technology adoption, shaping perceived usefulness, ease of use, and intent to adopt. The research also highlights the moderating roles of e-readiness, institutional support, and self-efficacy. Although promising, long-term impact remain unclear since the project is still ongoing as well as limitations in the study design. Nonetheless, the approach offers a scalable model for LMICs, underscoring the need for integrating ongoing learning, mentorship, and monitoring into national digital transformation strategies.
However, caution should be exercised in generalizing these findings to settings outside Sierra Leone. Cultural differences, such as language preferences, attitudes towards technology, and workplace norms, may influence the effectiveness of digital literacy interventions in other countries. Moreso, the geographic coverage is limited to only the 4 Districts involved in the DIPC project. Additionally, variations in technological infrastructure—such as internet connectivity, device availability, and IT support—and differences in the baseline educational levels of health workers could affect both the implementation and outcomes of similar programs elsewhere. Addressing these contextual factors may require adapting training content, delivery methods, and support mechanisms to local needs. Future research should focus on evaluating the transferability of this model across diverse environments, systematically exploring how cultural, infrastructural, and educational variables mediate or moderate the impact of digital literacy capacity-building interventions.
Limitations and constraints
This paper is formative and does not cover long-term training outcomes and impacts of the adopted approaches since coaching and mentorship activities are still ongoing. It highlights potential bottlenecks and proposes mitigation strategies to enhance the adoption of digital skills and prevent unsuccessful digital health implementations in a typical low- and middle-income country (LMIC). Moreover, the lack of a comparison group, reliance on self-reported competence, and absence of longitudinal follow-up limit the ability to draw strong causal inferences or predict sustained impact.
Recognizing these limitations, a follow-up evaluation has been planned to assess the retention of digital competencies and sustained application of learned skills over time. This will determine knowledge retention, continued system use, and factors influencing long-term digital adoption. Further summative evaluation will therefore be required to measure knowledge gain trajectories, learning curves, and the overall outcome of eSMT application in vaccine logistics management.
Conclusion
This formative study underscores the critical importance of contextually adapted, competency-based digital literacy interventions for advancing digital health adoption in LMICs. While initial findings indicate positive impacts on workforce readiness and technology uptake, the absence of long-term outcome data and a comparison group limits the strength of causal inferences. Ongoing coaching and mentorship, as well as planned follow-up evaluations, are essential for assessing knowledge retention and sustained digital competency. The lessons learned highlight the need for flexible, scalable strategies that consider local cultural, infrastructural, and educational factors, in line with global best practices. Future research should focus on rigorous, longitudinal evaluations to establish generalizability and inform evidence-based policy and practice in diverse settings.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
IE: Writing – original draft, Writing – review & editing, Conceptualization, Methodology, Supervision. TS: Writing – review & editing, Project administration. RS: Project administration, Writing – review & editing, Supervision. EF: Writing – review & editing. FS: Writing – review & editing. DK: Project administration, Writing – review & editing. AA: Writing – review & editing, Funding acquisition. VJ: Writing – review & editing, Funding acquisition. AM: Writing – review & editing, Formal analysis. TL: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. UNICEF is funding the publication fee.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1673085/full#supplementary-material
References
1.
Cuff A . The evolution of digital health and its continuing challenges. BMC Digit Health. (2023) 1(1):1–2. 10.1186/s44247-022-00004-x
2.
Jeilani A Hussein A . Impact of digital health technologies adoption on healthcare workers’ performance and workload: perspective with DOI and TOE models. BMC Health Serv Res. (2025) 25(1):1–17. 10.1186/s12913-025-12414-4
3.
Oke GI Sibomana O . Adoption of digital health technology in Nigeria: a scoping review of current trends and future directions. Adv Public Health. (2025) 2025(1):4246285. 10.1155/adph/4246285
4.
Kasaye MD Getahun AG Tessema AM Yimer N Kalayou MH Alhur AA . The national determinants of digital health: health professionals’ electronic health literacy from a cross-sectional perspective in Ethiopia: an umbrella review. Digit Health. (2025) 11:20552076251362396. 10.1177/20552076251362396
5.
Nafees A Khan M Chow R Fazelzad R Hope A Liu G et al Evaluation of clinical decision support systems in oncology: an updated systematic review. Crit Rev Oncol Hematol. (2023) 192:104143. 10.1016/j.critrevonc.2023.104143
6.
World Bank. Digital-in-health: Unlocking the value for everyone. (2023). Available online at:https://www.worldbank.org/en/topic/health/publication/digital-in-health-unlocking-value-for-everyone (Accessed July 13, 2025).
7.
World Health Organization. Global strategy on digital health 2020–2025. (2021). Available online at:https://www.who.int/publication/i/item/9789240020924
8.
Kasaye MD Kebede N Kalayou MH Kebede SD Molla A . Digital health literacy and associated factors among health professionals during the outbreak of corona virus pandemic in Ethiopia: a systematic review and meta-analysis. Digital Health. (2024) 10:1–14. 10.1177/20552076241271799
9.
Davis FD . Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. (1989) 13(3):319–40. 10.2307/249008
10.
Zhou Y Xu J Wang R Guan X . Understanding how digital health literacy affects health self-management behaviors: the mediating role of self-efficacy in college students. Sci Rep. (2025) 15(1):1–11. 10.1038/s41598-025-12726-9
11.
Reddy P Chaudhary K Hussein S . A digital literacy model to narrow the digital literacy skills gap. Heliyon. (2023) 9(4):e14878. 10.1016/j.heliyon.2023.e14878
12.
Mauco KL Scott RE Mars M . Validation of an e-health readiness assessment framework for developing countries. BMC Health Serv Res. (2020) 20(1):456–64. 10.1186/s12913-020-05448-3
13.
Tinmaz H Lee YT Fanea-Ivanovici M Baber H . A systematic review on digital literacy. Smart Learn Environ. (2022) 9(1):22–35. 10.1186/s40561-022-00204-y
14.
Reddy P Sharma B Chaudhary K . Digital literacy: a review of literature. Int J Technoethics. (2020) 11(2):65–94. 10.4018/ijt.20200701.oa1
15.
Borges do Nascimento IJ Abdulazeem H Vasanthan LT Martinez EZ Zucoloto ML Østengaard L et al Barriers and facilitators to utilizing digital health technologies by healthcare professionals. NPJ Digit Med. (2023) 6(1):1–28. 10.1038/s41746-023-00899-4
16.
Alotaibi N Wilson CB Traynor M . Enhancing digital readiness and capability in healthcare: a systematic review of interventions, barriers, and facilitators. BMC Health Serv Res. (2025) 25(1):1–15. 10.1186/s12913-025-12663-3
17.
Martin A Grudziecki J . Digeulit: concepts and tools for digital literacy development. Innov Teach Learn Inform Comput Sci. (2006) 5(4):249–67. 10.11120/ital.2006.05040249
18.
Rodríguez-De-dios I Igartua JJ González-Vázquez A . Development and validation of a digital literacy scale for teenagers. ACM International Conference Proceeding Series (2016). p. 1067–72. 10.1145/3012430.3012648
19.
Holloway K Arcus K Orsborn G . Training needs analysis—the essential first step for continuing professional development design. Nurse Educ Pract. (2018) 28:7–12. 10.1016/j.nepr.2017.09.001
20.
UNICEF. Designing digital interventions for lasting impact: A human-centred guide to digital health deployments. (2018). Available online at:https://www.unicef.org/innovation/media/511/file (Accessed July 13, 2025).
21.
Merriman SE Plant KL Revell KMA Stanton NA . A new approach for training needs analysis: a case study using an automated vehicle. Appl Ergon. (2023) 111:104014. 10.1016/j.apergo.2023.104014
22.
Perfect P Jump M White MD . Towards the development of a flight training programme for future personal aerial vehicle users. CEAS Aeronaut J. (2017) 8(3):541–60. 10.1007/s13272-017-0255-2
23.
Huddlestone J Pike J . Team and Collective Training Needs Analysis: Defining Requirements and Specifying Training Systems. Boca Raton: CRC Press (2016). 10.1201/9781315563275
24.
UNICEF. Digital literacy for children: Exploring definitions and frameworks. (2018). Available online at:https://www.unicef.org (Accessed July 13, 2025).
25.
Vuorikari R Kluzer S Punie Y . DigComp 2.2: The Digital Competence Framework for Citizens—with New Examples of Knowledge, Skills and Attitudes EUR 31006 EN. Luxembourg: Publications Office of the European Union (2022). 10.2760/115376
26.
UNESCO. A global framework of reference on digital literacy skills for indicator 4.4.2. (2018). Available online at:http://www.uis.unesco.org (Accessed July 14, 2025).
27.
World Bank. Digital skills: Frameworks and programs. (2020). Available online at:https://www.worldbank.org (Accessed July 14, 2025).
28.
World Health Organization. Invitation to participate in virtual workshops on the global digital health competency framework. (2025). Available online at:https://www.who.int/news-room/events/detail/2025/03/03/default-calendar/invitation-to-participate-in-virtual-workshops-on-the-global-digital-health-competency-framework (Accessed July 14, 2025).
29.
Darabi F Ziapour A Ahmadinia H . Digital health literacy and sociodemographic factors among students in western Iran: a cross-sectional study. BMC Med Educ. (2025) 25(1):1–12. 10.1186/s12909-025-06774-y
30.
Aloi MA Caldwell PHY Taba M Kang M Skinner SR Bray L et al Co-designing an online educational resource to help adolescents improve their digital health literacy. BMC Public Health. (2025) 25(1):1–10. 10.1186/s12889-025-22949-0
31.
Dağ E Demir Y Kayar Z Nal M . Relationship between digital health literacy, distrust in the health system, and health anxiety in health sciences students. BMC Med Educ. (2025) 25(1):1–8. 10.1186/s12909-025-06903-7
32.
Jowsey T Foster G Cooper-Ioelu P Jacobs S . Blended learning via distance in pre-registration nursing education: a scoping review. Nurse Educ Pract. (2020) 44:102775. 10.1016/j.nepr.2020.102775
33.
Li M Hong Y Wu A Ou W Yang J Lin G et al The effectiveness of blended learning in nursing and medical education: an umbrella review. Nurse Educ Pract. (2025) 86:104421. 10.1016/j.nepr.2025.104421
34.
Bruggeman B Tondeur J Struyven K Pynoo B Garone A Vanslambrouck S . Experts speaking: crucial teacher attributes for implementing blended learning in higher education. Internet High Educ. (2021) 48:100772. 10.1016/j.iheduc.2020.100772
35.
Ladur AN Egere U Ravit M Mgawadere F Murray C White SA et al A blended learning approach for capacity strengthening to improve the quality of integrated HIV, TB, and malaria services during antenatal and postnatal care in LMICs: a feasibility study. BMC Med Educ. (2025) 25(1):1–11. 10.1186/s12909-024-06633-2
36.
Niu Y Xi H Liu J Sui X Li F Xu H et al Effects of blended learning on undergraduate nursing students’ knowledge, skills, critical thinking ability and mental health: a systematic review and meta-analysis. Nurse Educ Pract. (2023) 72:103786. 10.1016/j.nepr.2023.103786
37.
Jiang L Wang D Yan J Yang M . Effect of a blended learning design in an undergraduate nursing electrocardiogram course: a quasi-experimental study. Nurs Open. (2023) 10(7):4461–70. 10.1002/nop2.1688
38.
Wang R Raman A . Systematic literature review on the effects of blended learning in nursing education. Nurse Educ Pract. (2025) 82:104238. 10.1016/j.nepr.2024.104238
39.
Duan A Jiang F Li L Li Q Chen W . Design and practice of blended teaching of internal medicine nursing based on O-AMAS effective teaching model. BMC Med Educ. (2024) 24(1):78–89. 10.1186/s12909-024-05588-8
40.
Wang L Liao B Yang H Yang C . Exploring nursing undergraduates’ experiences with a redesigned blended learning course: a descriptive qualitative study. Nurs Open. (2023) 10(4):2689–95. 10.1002/nop2.1478
41.
Karnoe A Furstrand D Christensen KC . Assessing competencies needed to engage with digital health services: development of the eHealth literacy assessment toolkit. J Med Internet Res. (2018) 20(5):e178. 10.2196/jmir.8347
42.
Nelissen E Ersdal H Mduma E Evjen-Olsen B Broerse J van Roosmalen J et al Helping mothers survive bleeding after birth: retention of knowledge, skills, and confidence nine months after obstetric simulation-based training. BMC Pregnancy Childbirth. (2015) 15(1):1–7. 10.1186/s12884-015-0612-2
43.
World Health Organization. Digital education for building health workforce capacity. (2020). Available online at:https://www.who.int/publication/i/item/978924000 (Accessed July 15, 2025).
44.
Marle F Jankovic M Maurer M Schmidt D Lindemann U . Risk and Change Management in complex Systems. Munich: Hanser Publishers (2014). 10.3139/9781569904923
45.
Lientz BP Rea KP . Breakthrough IT Change Management: How to get Enduring Change Results. Burlington: Elsevier Butterworth-Heinemann (2004). 10.1016/b978-0-7506-7686-1.x5000-2
46.
Scholl J Syed-Abdul S Ahmed LA . A case study of an EMR system at a large hospital in India: challenges and strategies for successful adoption. J Biomed Inform. (2011) 44(6):958–67. 10.1016/j.jbi.2011.07.008
47.
Lennon MR Bouamrane MM Devlin AM O’Connor S O’Donnell C Chetty U et al Readiness for delivering digital health at scale: lessons from a longitudinal qualitative evaluation of a national digital health innovation program in the United Kingdom. J Med Internet Res. (2017) 19(2):e42. 10.2196/jmir.6900
48.
Ekong I Esan O Chukwu E Kawu M . Ehealth adoption on patients’ pre-consultation waiting time: a comparative assessment of two district hospitals in Abuja, Nigeria. Int J Inform Technol Web Eng. (2020) 15(2):102–13. 10.4018/ijitwe.2020040105
49.
Gyee KM Mroueh L Bruand PE Min S Kleinebreil L Ohmmar T et al Empowering health workers and leveraging digital technology to improve access to mental health and epilepsy care: a longitudinal quasi-experimental study in hlaing thar Yar township. Lancet Reg Health Southeast Asia. (2022) 5:100052. 10.1016/j.lansea.2022.100052
50.
Giz. Digital Innovation in Pandemic Control Project Report. GIZ Sierra Leone (2024). Available online at:https://www.bmz-digital.global/en/overview-of-initiatives/digital-innovation (Accessed July 15, 2025).
51.
Ministry of Health, Sierra Leone. Sierra Leone National Digital Health Roadmap. (2024). Available online at:https://www.mohsl.gov.sl/digital-health/ (Accessed July 15, 2025).
52.
Navas de Maya B Komianos A Wood B de Wolff L Kurt RE Turan O . A practical application of the hierarchical task analysis (HTA) and human error assessment and reduction technique (HEART) to identify the major errors with mitigating actions taken after fire detection onboard passenger vessels. Ocean Eng. (2022) 253:111339. 10.1016/j.oceaneng.2022.111339
53.
Cho AH Arar NH Edelman DE Hartwell PH Oddone EZ Yancy WS . Do diabetic veterans use the internet? Self-reported usage, skills, and interest in using my HealtheVet web portal. Telemed e-Health. (2010) 16(2):245–50. 10.1089/tmj.2009.0164
54.
Mayer RE . Using multimedia for e-learning. J Comput Assist Learn. (2017) 33(5):403–23. 10.1111/jcal.12197
55.
Yusoff R Mohd Janor R . Generation of an interval metric scale to measure attitude. SAGE Open. (2014) 4(1). 10.1177/2158244013516768
56.
Lancer N Clutterbuck D Megginson D . Techniques for Coaching and Mentoring. Abingdon: Routledge (2016). 10.4324/9781315691251
57.
Clutterbuck D Whitaker C Lucas M . Coaching Supervision: A Practical Guide for Supervisees. Abingdon: Routledge (2016). 10.4324/9781315687070
58.
Hovenga E . Health workforce competencies needed for a digital world. Stud Health Technol Inform. (2013) 192:33–47. 10.3233/978-1-61499-289-9-33
59.
Zarekar M Al-Shehabi H Dörner R Weishaar H Lennemann T El Bcheraoui C et al The impact of information and communication technology on immunisation and immunisation programmes in low-income and middle-income countries: A systematic review and meta-analysis. eBioMedicine. (2025) 111:105520. 10.1016/j.ebiom.2024.105520
60.
Nascimbeni F Vosloo S . Digital literacy for children: Exploring definitions and frameworks.UNICEF Office of Global Insight and Policy (2019).
61.
World Health Organization. Country Profile: Sierra Leone. (2023). Available online at:https://monitor.digitalhealthmonitor.org/country_profile/SLE(Accessed July 13, 2025).
62.
Johns Hopkins Program for International Education in Gynecology and Obstetrics. Low Dose, High Frequency: A Learning Approach to Improve Health Workforce Competence, Confidence, and Performance. (2016). Available online at:https://hms.jhpiego.org/wp-content/uploads/2016/08/LDHF_briefer.pdf
Summary
Keywords
digital literacy, training needs analysis, competency framework, digitalization, e-readiness, digital transformation
Citation
Ekong I, Sesay T, Samuels R, Foday E, Smart F, Kangbai D, Ameha A, Joshi V, Mayei A and Lennemann T (2025) Foundational digital literacy training for frontline immunization officers: lessons from implementing the electronic stock management tool across selected comprehensive health centers in Sierra Leone. Front. Digit. Health 7:1673085. doi: 10.3389/fdgth.2025.1673085
Received
25 July 2025
Accepted
27 October 2025
Published
19 December 2025
Volume
7 - 2025
Edited by
Björn Wolfgang Schuller, Imperial College London, United Kingdom
Reviewed by
Unik Hanifah Salsabila, Islamic Religious Education, Indonesia
Eti Rimawati, Universitas Dian Nuswantoro, Indonesia
Updates
Copyright
© 2025 Ekong, Sesay, Samuels, Foday, Smart, Kangbai, Ameha, Joshi, Mayei and Lennemann.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
* Correspondence: Iniobong Ekong inijust@yahoo.co.uk
†Present Address: Iniobong Ekong, Ministry of Health, Directorate of Policy, Planning and Information, Government of Sierra Leone, Freetown, Sierra Leone
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.