- 1Department of Pathology and Biomedical Science, University of Otago, Christchurch, New Zealand
- 2Christchurch Heart Institute, Department of Medicine, University of Otago, Christchurch, New Zealand
- 3Biochemistry Department, University of Otago, Dunedin, New Zealand
- 4Division of Clinical Immunology and Rheumatology, University of Alabama at Birmingham, Birmingham, AL, United States
- 5Pacific Trust Canterbury, Montreal Street, Christchurch, New Zealand
- 6Department of Pathology, Center for Personalized Medicine, Children’s Hospital Los Angeles, Los Angeles, CA, United States
The enzyme cytochrome P450 2D6 (CYP2D6) metabolises approximately 25% of commonly prescribed drugs, including analgesics, anti-hypertensives, and anti-depressants, among many others. Genetic variation in drug metabolising genes can alter how an individual responds to prescribed drugs, including predisposing to adverse drug reactions. The majority of research on the CYP2D6 gene has been carried out in European and East Asian populations, with many Indigenous and minority populations, such as those from Oceania, greatly underrepresented. However, genetic variation is often population specific and analysis of diverse ethnic groups can reveal differences in alleles that may be of clinical significance. For this reason, we set out to examine the range and frequency of CYP2D6 variants in a sample of 202 Māori and Pacific people living in Aotearoa (New Zealand). We carried out long PCR to isolate the CYP2D6 region before performing nanopore sequencing to identify all variants and alleles in these samples. We identified twelve variants which have previously not been reported in the PharmVar CYP2D6 database, three of which were exonic missense variations. Six of these occurred in single samples and one was found in 19 samples (9.4% of the cohort). The remaining five variants were identified in two samples each. Identified variants formed twelve new CYP2D6 suballeles and four new star alleles, now recorded in the PharmVar database. One striking finding was that CYP2D6*71, an allele of uncertain functional status which has been rarely observed in previous studies, occurs at a relatively high frequency (8.9%) within this cohort. These data will help to ensure that CYP2D6 genetic analysis for pharmacogenetic purposes can be carried out accurately and effectively in this population group.
Introduction
Pharmacogenetics is the study of genetic variants which impact on an individual’s response to drugs, with the aim of guiding prescription practices to improve healthcare quality and outcomes (Bank et al., 2018; Cacabelos et al., 2019). CYP2D6 is one of the most studied pharmacogenes. This gene encodes an enzyme (CYP2D6) which is expressed in the liver and responsible for metabolising approximately 25% of commonly prescribed drugs or prodrugs (Nofziger et al., 2020).
The CYP2D6 gene is highly polymorphic, with many recorded single nucleotide variants (SNVs), small insertions/deletions, larger copy number variants including whole gene deletions or duplications, as well as hybrid genes formed by recombination with the closely related pseudogene (CYP2D7) that is in close proximity (Nofziger et al., 2020). Over 150 CYP2D6 alleles have so far been identified, each of which is allocated a name using a “star” nomenclature scheme, and tracked within the PharmVar database. Minor variations are often allocated a “suballele” designation (Gaedigk et al., 2020; Nofziger et al., 2020).
Variants of the gene may impact CYP2D6 function, ranging from completely inactivating the enzyme through to elevating its activity, although the impact of many variants is yet to be quantified. Where the functional impact of alleles is known or can be inferred, individuals can be categorised into one of four metaboliser phenotypes—ultrarapid metaboliser (UM), normal metaboliser (NM), intermediate metaboliser (IM), and poor metaboliser (PM), each of which describes activity of the CYP2D6 enzyme (Gaedigk et al., 2008). Depending on the type of medication, individuals defined as poor or ultrarapid metabolisers are at particular risk of experiencing drug toxicity or poor drug response (Cacabelos et al., 2019).
Interethnic differences in allele distribution or frequencies are evident for CYP2D6 (Gaedigk et al., 2017; Zhou et al., 2017; Koopmans et al., 2021). For example, CYP2D6*10 is reported with a frequency of 45% in East Asian populations, compared to only 1.6% in Europeans (Zhou et al., 2017). Furthermore, the PharmGKB database of CYP2D6 variants (Whirl-Carrillo et al., 2021) includes data from over 64,000 Europeans compared to less than 800 individuals from the Oceanian biogeographic grouping, defined as pre-colonial populations of the Pacific, including Hawaii, Australia, New Zealand and Papua New Guinea (Huddart et al., 2019). Many of the existing ‘Oceania’ studies focus on individuals from Papua New Guinea and Melanesia, which will not fully represent genetic diversity of Oceanian populations. Aotearoa (New Zealand) was the last major landmass to be inhabited, with Māori settlers arriving about 730 years before present (BP) (Gosling and Matisoo-Smith, 2018). Māori and Pacific Island populations have origins in South-East Asia, before migrations brought them to remote Oceania around 3000 BP (Helsby 2016; Gosling and Matisoo-Smith, 2018). There have been very few studies specifically examining pharmacogenetic variability in Māori and Pacific Island people (Wanwimolruk et al., 1995; Wanwimolruk et al., 1998; Lea et al., 2008). To ensure equitable application of pharmacogenetic tests that detect clinically relevant alleles in people of all ancestries, it is important that such pharmacogenetic variants are identified and quantified by analysis of appropriate population samples.
The choice of technology employed for studies of interethnic diversity in CYP2D6 is critical. Many prior studies have used targeted genotyping arrays or allele-specific polymerase chain reaction (PCR) methods, targeting only known alleles of interest, often derived from analysis of Europeans (Carvalho Henriques et al., 2021). These analyses are relatively cheap and straightforward to carry out, but unknown or rare alleles will not be detected (and will be potentially reported as *1 if not positive for another allele of interest). A more effective approach to identify all variants and determine haplotypes is to employ long-read, single molecule nanopore DNA sequencing on a PCR product encompassing the entire CYP2D6 region (Liau et al., 2019). In this paper, we applied these methods to characterise the allelic landscape of CYP2D6 in two cohorts of New Zealand Māori and Pacific Island people.
Materials and methods
Study cohorts
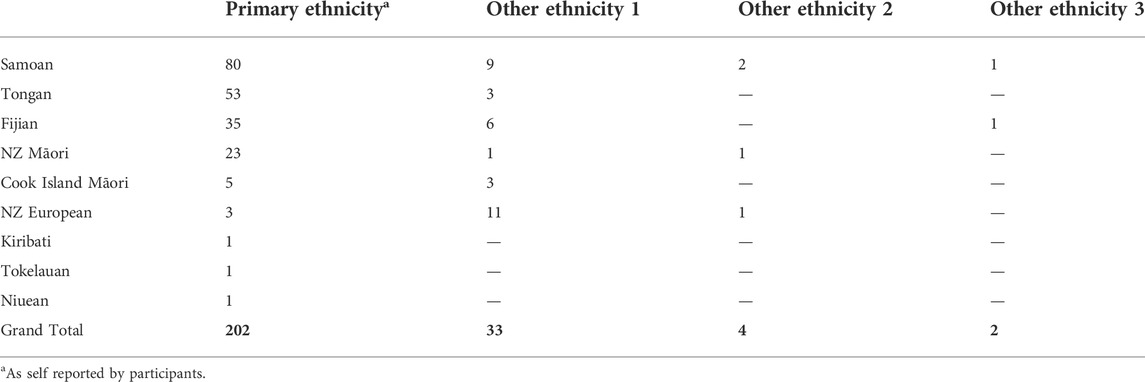
A total of 202 samples were drawn from two existing studies. Thirty-five of these samples were from a study called Genetics of Gout, Diabetes, and Kidney Disease in Aotearoa New Zealand, which recruited individuals aged ≥16 years primarily from the Auckland, Waikato and Christchurch regions of Aotearoa (New Zealand) (Krishnan et al., 2018). The remaining 167 samples were from the Pasifika Heart Study (Faatoese et al., manuscript in preparation). This study involved 200 Pacific participants aged 20–64 years, selected from the patient register of a Pacific-led primary healthcare clinic (Pacific Trust Canterbury, Christchurch, NZ), a low-cost health provider largely serving Pacific residents of Christchurch. Screening clinics for the Pasifika Heart Study were held from May 2015—June 2016 at the Pacific Trust Health Clinic and the Nicholls Research Centre, University of Otago, Christchurch. In both studies, ethnicity was self-reported and the ethnicities of each participant’s four grandparents were also documented. The majority of samples were Polynesian, self-reporting as Samoan, Tongan, or Māori. Other included ethnicities were Cook Island Māori, Fijian (Melanesian), Tokelauan, Kiribati, and Niuean (Table 1).
Ethical approval for the study Genetics of Gout, Diabetes, and Kidney Disease in Aotearoa New Zealand was given by the NZ Multi-Region Ethics Committee (MEC/05/10/130; MEC/10/09/092; MEC/11/04/036). The Pasifika Heart Study was approved by the New Zealand Health and Disability Ethics Committee (14/CEN/72/AM04). Participants in both studies gave written, informed consent.
CYP2D6 long PCR
CYP2D6 was amplified by PCR as a 6.6 kb product, including the whole gene as well as upstream and downstream non-coding regions. Duplication and deletion primers were used to identify the presence of a CYP2D6 duplication or deletion via amplification of a secondary 3.5 kb fragment if present (Gaedigk et al., 2007; Maggo S. D. S. et al., 2019; Liau et al., 2019). Primer sequences are provided in Supplementary Table S1.
Barcoding of PCR amplicons
Oxford Nanopore Technologies (ONT) PCR Barcoding Expansion 1–96 kit was used to add specific barcodes onto the CYP2D6 amplicons. This allowed sample pooling in later steps. For a 50 μL reaction, 0.5 nM CYP2D6 6.6 kb tailed amplicon was amplified in the presence of 1x LongAMP buffer, 0.3 mM Kapa dNTPs, 5 units of LongAMP Hot Start Taq DNA polymerase, 0.2 μM barcode and ultra-pure H2O to make up the final volume. This followed the ONT protocol SQK- LSK109, (version PBAC96_9069_v109_revO_14August 2019). The PCR began with an incubation at 95°C for 3 min, followed by 15 cycles of 95°C for 15 s, 62°C for 15 s, 65°C for 7 min, and finally 65°C for 7 min, as recommended by ONT.
Magnetic bead purification
Magnetic beads were used to purify the PCR products both prior to and following the barcoding step. This removed DNA fragments shorter than 3–4 kb (to avoid off-target amplification) and other impurities. Magbio beads (MagBio Genomics Inc., Gaithersburg, Maryland, USA) were pelleted and re-dissolved in a buffer with 10 mM Tris-HCl, 1.6M NaCl, 1 mM EDTA pH 8, 11% (w/v) PEG 8000, 0.20% (v/v) Tween-20, and ultra-pure water to make a 10 ml bead solution (Nagar and Schwessinger, 2018). DNA samples were purified as described previously (Liau et al., 2019).
Nanopore sequencing library preparation
DNA libraries of barcoded amplicons were prepared according to the 1D PCR barcoding (96) amplicons ONT protocol, SQK-LSK109. Briefly, after pooling the barcoded amplicons, about 200 fmoles of the DNA pool was subjected to end-repair and ONT adapter ligation. After purification, approximately 210 ng (∼ 50 fmoles) of the library was introduced to the MinION flowcell (R9.4.1) and sequenced for up to 48 h on the GridION X5 nanopore sequencer (ONT, UK). Some sequencing was also completed on a FLO-FLG-001 Flongle (R9.4.1) loaded with approximately 90 ng (∼ 20 fmoles) of library.
Nanopore sequencing data analysis
A previously designed pipeline was used to analyse the data generated (Graham et al., 2020). The GridION platform conducted real-time filtering, basecalling, and demultiplexing (separating and binning each sample per barcode) using Guppy version 5.0.12 (ONT, UK). A quality threshold for sequencing was set, specifying reads between 6 and 8 kb in length and a Qscore of >9. An end-to-end pipeline for data management was designed in a conda environment using a snakemake workflow (Mölder et al., 2021). The process included utilising the output of the GridION to initially map the FASTQ files generated against a reference sequence (CYP2D6_NG008376.4) using MiniMap2 version 2.20-r1061 (Li, 2018). SAMtools (version 1.7) (Li et al., 2009) was employed to perform indexing at various stages of this pipeline. Nanopolish (version 0.13.2) (Quick et al., 2016) was used to analyse variant calls. Whatshap (version 0.17) (Martin et al., 2016) was used to phase the VCF files generated by Nanopolish. Variants were then matched to CYP2D6 star alleles using the PharmVar database (Pharmacogene Variation Consortium, 2021) and unmatched variants were identified and marked as potentially novel to be taken forward for later validation. Finally, Stargazer v1.0.8 (Lee et al., 2019), an automated tool for pharmacogenetic star allele assignment, was used to confirm the CYP2D6 star allele assigned to each sample. Star allele frequencies between studies were compared with two sided Fisher’s exact test and considered significant at p = 0.05.
Sanger sequencing
To validate potential novel alleles, Sanger sequencing was performed following a nested PCR on the relevant CYP2D6 gene locations, using the long amplicon as a template as described (Maggo et al., 2019a; Maggo et al., 2019b). Primer sequences are provided in Supplementary Table S2.
Results
From an initial 282 samples, 202 were successfully sequenced and analysed at all steps. Excluded samples included those that failed to amplify the 6.6 kb CYP2D6 PCR product (n = 52), or samples with a low read depth (less than 50 reads; n = 28). Genomic DNA samples which failed to amplify were checked on a TapeStation platform (Agilent, Santa Clara, USA) and were usually found to be fragmented, with this fragmentation being the likely cause of long-PCR failure. 120 of the samples were sequenced with an R9.4.1 flow cell, and the remaining 82 were sequenced with a FLG-001 Flongle, with both flow cell types run on the GridION X5.
CYP2D6 genotypes
Unlike short-read sequencing technologies, nanopore sequencing gives long single molecule reads that allow sample haplotypes to be discerned.
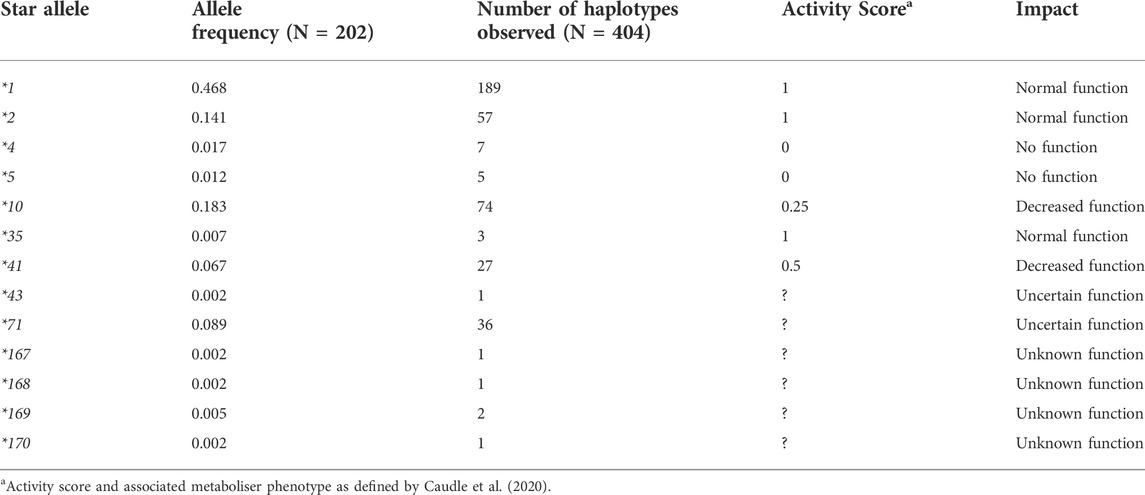
Thirteen different CYP2D6 star alleles were identified amongst 202 individuals, including the *5 gene deletion and novel star alleles (Table 2). No CYP2D6 gene duplications were observed. The most common allele was *1 with an allele frequency of 0.48. Following this, in order of frequency, were *10, *2, and *71. Four of the identified star alleles, *4, *5, *10, and *41, are known to decrease or completely inactivate the function of the CYP2D6 enzyme, while *1, *2, and *35 have no impact. *43 and *71 have uncertain functional effects on CYP2D6. *167, *168, *169, and *170 were discovered during this study and have been named by the PharmVar CYP2D6 committee, designated as novel and of unknown function.
Stargazer 1.0.8 (Lee et al., 2019) was used to call star alleles for the first 120 samples, using variants aligned to hg19. Of these 120, eleven were called incorrectly. Five of the incorrect haplotype assignments were due to the presence of a *5 allele, while the remaining six carried *71 variants.
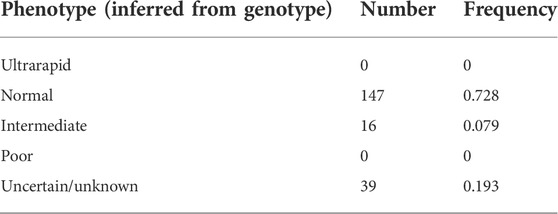
Predicted metaboliser phenotypes
Metaboliser status was inferred from the genotype of each sample using the diplotype activity score as previously defined (Caudle et al., 2020). In this classification, diplotypes with an activity score of 0 are classified as poor metabolisers, 0.25–1 are intermediate metabolisers, 1.25–2 are normal metabolisers, and scores above 2 are ultrarapid metabolisers. Using this definition, the majority (73%) of individuals within the cohort were classified as normal metabolisers. No individuals were identified as being ultrarapid or poor metabolisers, and a small subset (8%) of our study cohort were intermediate metabolisers. Almost 20% of the characterised samples had a metaboliser status that could not be assigned due to the presence of one or more *71, *43, or novel alleles (Table 3).
Variants previously not reported in PharmVar CYP2D6 database
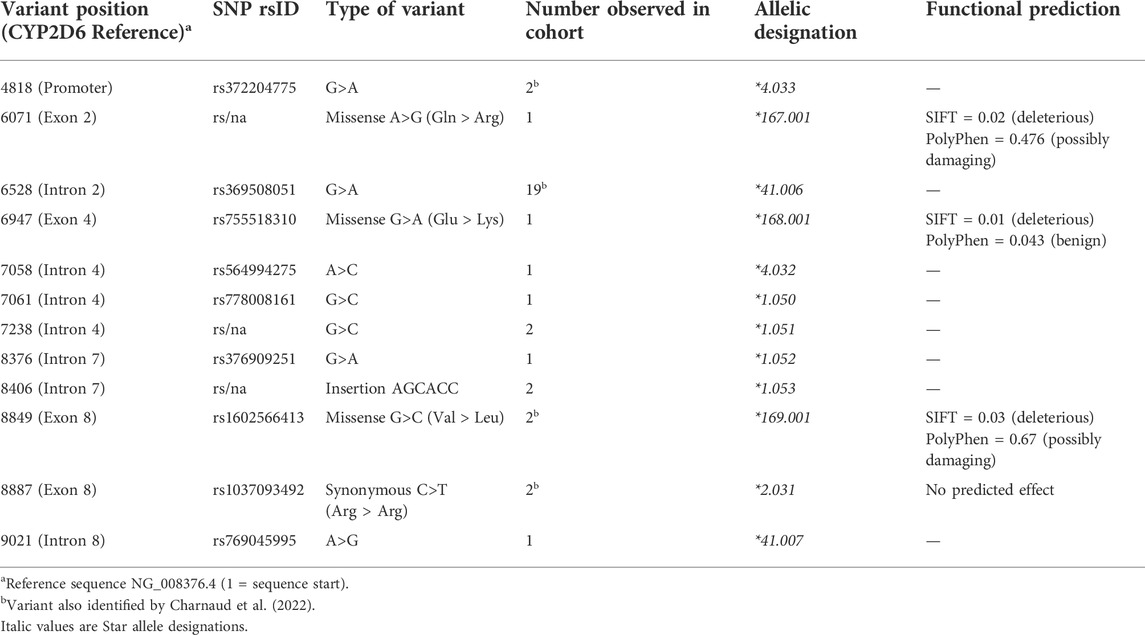
We identified twelve variants that have not previously been reported as PharmVar CYP2D6 alleles, however nine of these are recorded in dbSNP and have been assigned reference SNP numbers (rsIDs). These variants were validated in our samples using Sanger sequencing (Table 4). Seven variants occurred within an intron of the gene, one in the promoter region, and four were exonic variants, three of which are non-synonymous. These were submitted to the PharmVar committee and assigned as new CYP2D6 star alleles and suballeles.
Six of the twelve variants were singletons (detected in only one individual each), five were identified in two individuals each, while a variant at position 6528 was found in nineteen individuals. In addition, four novel suballeles were also identified (data not shown). These variants occur within the PharmVar CYP2D6 database but as part of different star alleles to those observed in this study. The majority exist on the haplotype without any core variants belonging to star alleles, so are by default *1. One known variant (position 8934) formed a new star allele (*170.001), due to its predicted deleterious effect and prior existence as a core variant for another star allele (*136). Two variants at position 9414 and 9464 are new *10 suballeles as all samples have the *10 core variants.
Discussion
Of the nine broad ethnic groups defined by Huddart et al., and reported by PharmGKB, 2021, Oceania is by far the least represented (PharmGKB, 2021) (Huddart et al., 2019). We have successfully used nanopore sequencing to analyse the entire CYP2D6 gene (including important upstream and downstream regions) of 202 Māori and Pacific Island individuals, coupled with analyses to call the star allele diplotypes of each participant.
Nine previously reported star alleles were identified amongst this cohort. CYP2D6*71, a previously identified rare allele with an uncertain function was identified at a relatively high frequency within this cohort (8.9%). Twelve variants not previously reported in the PharmVar CYP2D6 database were also discovered, four of which are exonic. Five known variants were found within star alleles in which they have not been reported previously. From these variants, four new star alleles have been assigned (*167-*170), in addition to thirteen novel suballeles (Table 4).
From each individual’s diplotype, we were able to categorise the majority of the cohort into metaboliser phenotypes. We did not find any ultrarapid or poor metabolisers. A large percentage of participants (73%) were normal metabolisers and 8% had a predicted activity score within the range of intermediate metabolisers (Caudle et al., 2020). The remaining 19% were unable to be assigned to a metaboliser status due to carrying one or more copies of a *43, *71, or a novel star allele.
We did not identify any poor metabolisers in the present study, as all non-functional alleles were found in diplotypes with a fully functional or partially functional allele. Non-functional alleles (*4 and *5 gene deletion) were present in ∼3% of the cohort, so they do exist at a low frequency within the population and therefore could give rise to poor metaboliser phenotypes. In this regard, it is interesting to note that a pharmacological study using the probe drug debrisoquine in 101 Māori participants identified 5% as poor metabolisers (Wanwimolruk et al., 1995), and a similar study in 100 Polynesian participants found no poor metabolisers (Wanwimolruk et al., 1998). Therefore, our genetic findings are reasonably congruent with these earlier studies.
However, CYP2D6 allele frequencies observed in our study do not match allele frequencies previously reported by PharmGKB, 2021 for the Oceanian region (PharmGKB, 2021). This is almost certainly because the Oceanian definition encompasses populations with diverse, complex migration and ancestral histories (Gosling and Matisoo-Smith, 2018). The Oceanian CYP2D6 data currently available comes from studies that in total include less than 800 individuals. The largest study (Gutiérrez Rico et al., 2020) focused on 278 Ni-Vanuatu (Micronesian) subjects, and found the majority of individuals to carry at least one *1 allele (allele frequency of 0.804), significantly greater than our identified frequency of 0.468 (p = 3.8 × 10–19). In total, they identified nine different star alleles amongst their cohort, the majority of which had allelic frequencies of <0.01. *2 and *10 existed above this frequency (0.068 and 0.029, respectively) as well as a duplication of *1 at 0.025 (Gutiérrez Rico et al., 2020). Our study found no duplications and only two non-novel alleles had observed frequencies below 0.01 (*35, *43). Prior reports describing high rates of CYP2D6 duplications in Oceania have been entirely based on Papua New Guinea samples (Sistonen et al., 2007; von Ahsen et al., 2010).
The relatively high frequency of the *71 allele we observed is one of the most striking findings from this study, for several reasons. Because *71 has thus far been considered a rare allele, it would not be routinely included in most CYP2D6 genotyping panels. The functional impact of *71 is uncertain, so we were unable to predict the metaboliser status for 19% of our cohort. The first study to identify *71 was performed in a Han Chinese population (Zhou et al., 2009). This group suggested the allele could be non-functional due to the p. Gly42 > Glu substitution in the protein N- terminus, a region which is involved in membrane anchoring of the enzyme (Zhou et al., 2009). However, this is speculative and has yet to be tested. Other reports, in Micronesian populations, have described allele frequencies of 0.009 in a Ni-Vanuatu sample (Gutiérrez Rico et al., 2020), significantly less than our 0.089 (p = 2.0 × 10–7) and 0.058 in a large sample of Solomon Islanders (Charnaud et al., 2022), comparable but significantly less than our 0.089 (p = 0.043).
Conclusion
In conclusion, we have used a nanopore sequencing approach to identify CYP2D6 star alleles and respective frequencies from 202 individuals of Māori and Pacific Island ethnicity. We identified nine known star alleles in this cohort, including CYP2D6*71, a previously identified rare allele of uncertain function, which comprised ∼9% of the alleles detected. The frequency of this allele prevented us from inferring metabolic function for nearly 20% of this cohort, and clearly, understanding the functional impact of *71 using clinical phenotyping approaches or in vitro analyses is a priority area for future research. Should this allele have an altered function, it would be important to ensure it is included in pharmacogenetic testing panels, particularly if to be used in the Oceania region.
Our analysis did not reveal any CYP2D6 duplications in this cohort, and overall our findings highlight the significant limitations of the Oceania biogeographic grouping for pharmacogenetic research, given the wide allele frequency differences we observe relative to studies on other Oceanian ancestral groups.
Finally, this study has further demonstrated the utility of nanopore sequencing for highly variable genes like CYP2D6, with long-read sequencing providing the advantage of analysing the entire gene, including intronic regions, at high throughput and relatively low cost. In addition, this method allows direct observation of haplotypes, without the need for allele-specific long PCR or other approaches which are often applied to resolve haplotypes detected in short read sequencing data. It is to be hoped this research will contribute to a more equitable uptake of CYP2D6 pharmacogenetics in people of Māori and Pacific ancestry.
Data availability statement
The datasets presented in this article are not readily available because ethical approval for the underlying studies prohibit public sharing of data. Requests to access the datasets should be directed to Dr Kennedy (bWFydGluLmtlbm5lZHlAb3RhZ28uYWMubno=) or Dr Faatoese (YWxsYW1hbmRhLmZhYXRvZXNlQG90YWdvLmFjLm56).
Ethics statement
The studies involving human participants were reviewed and approved by NZ Multi-Region Ethics Committee (MEC/05/10/130; MEC/10/09/092; MEC/11/04/036) (Genetics of Gout, Diabetes and Kidney Disease in Aotearoa New Zealand cohort). New Zealand Health and Disability Ethics Committee (14/CEN/72/AM04) (Pasifika Heart Study cohort). The patients/participants provided their written informed consent to participate in this study.
Author contributions
LH carried out the lab work and contributed greatly to the manuscript. AF and TM provided the DNA samples and provided advice on the manuscript. AM supported and advised on laboratory work. YL set up workflow and helped troubleshoot issues. OG established bioinformatic workflow. PK performed Sanger sequencing. JP helped with bioinformatics and statistical analyses. TF contributed to establishing the Pasifika Heart Study. VC advised on manuscript and contributed to establishing and maintaining Pasifika Heart Study. MK and SM supervised LH during study and contributed significantly to manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgene.2022.1016416/full#supplementary-material
Supplementary Table S1 | Primer Sequences for CYP2D6 amplification.
Supplementary Table S2 | Primer Sequences for novel variant confirmation.
References
Bank, P. C. D., Swen, J. J., and Guchelaar, H. J. (2018). Implementation of pharmacogenomics in everyday clinical settings. Adv. Pharmacol. 83, 219–246. doi:10.1016/bs.apha.2018.04.003
Cacabelos, R., Cacabelos, N., and Carril, J. C. (2019). The role of pharmacogenomics in adverse drug reactions. Expert Rev. Clin. Pharmacol. 12, 407–442. doi:10.1080/17512433.2019.1597706
Carvalho Henriques, B., Buchner, A., Hu, X., Wang, Y., Yavorskyy, V., Wallace, K., et al. (2021). Methodology for clinical genotyping of CYP2D6 and CYP2C19. Transl. Psychiatry 11, 596. doi:10.1038/s41398-021-01717-9
Caudle, K. E., Sangkuhl, K., Whirl-Carrillo, M., Swen, J. J., Haidar, C. E., Klein, T. E., et al. (2020). Standardizing CYP2D6 genotype to phenotype translation: Consensus recommendations from the clinical pharmacogenetics implementation Consortium and Dutch pharmacogenetics working group. Clin. Transl. Sci. 13, 116–124. doi:10.1111/cts.12692
Charnaud, S., Munro, J. E., Semenec, L., Mazhari, R., Brewster, J., Bourke, C., et al. (2022). PacBio long-read amplicon sequencing enables scalable high-resolution population allele typing of the complex CYP2D6 locus. Commun. Biol. 5, 168. doi:10.1038/s42003-022-03102-8
Gaedigk, A., Ndjountche, L., Divakaran, K., Dianne Bradford, L., Zineh, I., Oberlander, T., et al. (2007). Cytochrome P4502D6 (CYP2D6) gene locus heterogeneity: Characterization of gene duplication events. Clin. Pharmacol. Ther. 81, 242–251. doi:10.1038/sj.clpt.6100033
Gaedigk, A., Sangkuhl, K., Whirl-Carrillo, M., Klein, T., and Leeder, J. S. (2017). Prediction of CYP2D6 phenotype from genotype across world populations. Genet. Med. 19, 69–76. doi:10.1038/gim.2016.80
Gaedigk, A., Simon, S. D., Pearce, R. E., Bradford, L. D., Kennedy, M. J., and Leeder, J. S. (2008). The CYP2D6 activity score: Translating genotype information into a qualitative measure of phenotype. Clin. Pharmacol. Ther. 83, 234–242. doi:10.1038/sj.clpt.6100406
Gaedigk, A., Whirl-Carrillo, M., Pratt, V. M., Miller, N. A., and Klein, T. E. (2020). PharmVar and the landscape of pharmacogenetic resources. Clin. Pharmacol. Ther. 107, 43–46. doi:10.1002/cpt.1654
Gosling, A. L., and Matisoo-Smith, E. A. (2018). The evolutionary history and human settlement of Australia and the Pacific. Curr. Opin. Genet. Dev. 53, 53–59. doi:10.1016/j.gde.2018.06.015
Graham, O. E. E., Pitcher, T. L., Liau, Y., Miller, A. L., Dalrymple-Alford, J. C., Anderson, T. J., et al. (2020). Nanopore sequencing of the glucocerebrosidase (GBA) gene in a New Zealand Parkinson's disease cohort. Park. Relat. Disord. 70, 36–41. doi:10.1016/j.parkreldis.2019.11.022
Gutiérrez Rico, E. M., Kikuchi, A., Saito, T., Kumondai, M., Hishinuma, E., Kaneko, A., et al. (2020). CYP2D6 genotyping analysis and functional characterization of novel allelic variants in a Ni-Vanuatu and Kenyan population by assessing dextromethorphan O-demethylation activity. Drug Metab. Pharmacokinet. 35, 89–101. doi:10.1016/j.dmpk.2019.07.003
Helsby, N. A. (2016). CYP2C19 and CYP2D6 genotypes in Pacific peoples. Br. J. Clin. Pharmacol. 82, 1303–1307. doi:10.1111/bcp.13045
Huddart, R., Fohner, A. E., Whirl-Carrillo, M., Wojcik, G. L., Gignoux, C. R., Popejoy, A. B., et al. (2019). Standardized biogeographic grouping system for annotating populations in pharmacogenetic research. Clin. Pharmacol. Ther. 105, 1256–1262. doi:10.1002/cpt.1322
Koopmans, A. B., Braakman, M. H., Vinkers, D. J., Hoek, H. W., and Van Harten, P. N. (2021). Meta-analysis of probability estimates of worldwide variation of CYP2D6 and CYP2C19. Transl. Psychiatry 11, 141. doi:10.1038/s41398-020-01129-1
Krishnan, M., Major, T. J., Topless, R. K., Dewes, O., Yu, L., Thompson, J. M. D., et al. (2018). Discordant association of the CREBRF rs373863828 A allele with increased BMI and protection from type 2 diabetes in Maori and Pacific (Polynesian) people living in Aotearoa/New Zealand. Diabetologia 61, 1603–1613. doi:10.1007/s00125-018-4623-1
Lea, R., Roberts, R., Green, M., Kennedy, M., and Chambers, G. (2008). Allele frequency differences of cytochrome P450 polymorphisms in a sample of New Zealand Maori. N. Z. Med. J. 121, 33–37.
Lee, S.-B., Wheeler, M. M., Thummel, K. E., and Nickerson, D. A. (2019). Calling star alleles with stargazer in 28 pharmacogenes with whole genome sequences. Clin. Pharmacol. Ther. 106, 1328–1337. doi:10.1002/cpt.1552
Li, H., Handsaker, B., Wysoker, A., Fennell, T., Ruan, J., Homer, N., et al. (2009). The sequence alignment/map format and SAMtools. Bioinformatics 25, 2078–2079. doi:10.1093/bioinformatics/btp352
Li, H. (2018). Minimap2: Pairwise alignment for nucleotide sequences. Bioinformatics 34, 3094–3100. doi:10.1093/bioinformatics/bty191
Liau, Y., Maggo, S., Miller, A. L., Pearson, J. F., Kennedy, M. A., and Cree, S. L. (2019). Nanopore sequencing of the pharmacogene CYP2D6 allows simultaneous haplotyping and detection of duplications. Pharmacogenomics 20, 1033–1047. doi:10.2217/pgs-2019-0080
Maggo, S. D. S., Sycamore, K. L. V., Miller, A. L., and Kennedy, M. A. (2019b). The three ps: Psychiatry, pharmacy, and pharmacogenomics, a brief report from New Zealand. Front. Psychiatry 10, 690. doi:10.3389/fpsyt.2019.00690
Maggo, S., Kennedy, M. A., Barczyk, Z. A., Miller, A. L., Rucklidge, J. J., Mulder, R. T., et al. (2019a). Common CYP2D6, CYP2C9, and CYP2C19 gene variants, health anxiety, and neuroticism are not associated with self-reported antidepressant side effects. Front. Genet. 10, 1199. doi:10.3389/fgene.2019.01199
Martin, M., Patterson, M., Garg, S., Fischer, S., Pisanti, N., Klau, G., et al. (2016). WhatsHap: Fast and accurate read-based phasing. bioRxiv. doi:10.1101/085050
Mölder, F., Jablonski, K., Letcher, B., Hall, M., Tomkins-Tinch, C., Sochat, V., et al. (2021). Sustainable data analysis with snakemake. F1000Research 10, 33. doi:10.12688/f1000research.29032.2
Nagar, R., and Schwessinger, B. (2018). DNA size selection (> 3–4 kb) and purification of DNA using an improved homemade SPRI beads solution. Protoc. io 110, 6. doi:10.17504/protocols.io.n7hdhj6
Nofziger, C., Turner, A. J., Sangkuhl, K., Whirl-Carrillo, M., Agundez, J. a. G., Black, J. L., et al. (2020). PharmVar GeneFocus: CYP2D6. Clin. Pharmacol. Ther. 107, 154–170. doi:10.1002/cpt.1643
Pharmacogene Variation Consortium (2021). CYP2D6 [online]. Available at: https://www.pharmvar.org/gene/CYP2D6 (Accessed 6 October 2021).
PharmGKB (2021). Pharmgkb CYP2D6 Frequency Table [online]. Available at: https://api.pharmgkb.org/v1/download/file/attachment/CYP2D6_frequency_table.xlsx (Accessed 30 Sept 2021).
Quick, J., Loman, N. J., Duraffour, S., Simpson, J. T., Severi, E., Cowley, L., et al. (2016). Real-time, portable genome sequencing for Ebola surveillance. Nature 530, 228–232. doi:10.1038/nature16996
Sistonen, J., Sajantila, A., Lao, O., Corander, J., Barbujani, G., and Fuselli, S. (2007). CYP2D6 worldwide genetic variation shows high frequency of altered activity variants and no continental structure. Pharmacogenet. Genomics 17, 93–101. doi:10.1097/01.fpc.0000239974.69464.f2
Steen, V., Andreassen, O., Daly, A., Tefre, T., Borresen, A., Idl, E. J., et al. (1995). Detection of the poor metabolizer-associated CYP2D6(D) gene deletion allele by long-PCR technology. Pharmacogenetics 5, 215–223. doi:10.1097/00008571-199508000-00005
Von Ahsen, N., Tzvetkov, M., Karunajeewa, H. A., Gomorrai, S., Ura, A., Brockmöller, J., et al. (2010). CYP2D6 and CYP2C19 in Papua New Guinea: High frequency of previously uncharacterized CYP2D6 alleles and heterozygote excess. Int. J. Mol. Epidemiol. Genet. 1, 310–319.
Wanwimolruk, S., Bhawan, S., Coville, P. F., and Chalcroft, S. C. (1998). Genetic polymorphism of debrisoquine (CYP2D6) and proguanil (CYP2C19) in South Pacific Polynesian populations. Eur. J. Clin. Pharmacol. 54, 431–435. doi:10.1007/s002280050488
Wanwimolruk, S., Pratt, E. L., Denton, J. R., Chalcroft, S. C., Barron, P. A., and Broughton, J. R. (1995). Evidence for the polymorphic oxidation of debrisoquine and proguanil in a New Zealand Maori population. Pharmacogenetics 5, 193–198. doi:10.1097/00008571-199508000-00002
Whirl-Carrillo, M., Huddart, R., Gong, L., Sangkuhl, K., Thorn, C. F., Whaley, R., et al. (2021). An evidence-based framework for evaluating pharmacogenomics knowledge for personalized medicine. Clin. Pharmacol. Ther. 110, 563–572. doi:10.1002/cpt.2350
Wright, G. E. B., Niehaus, D. J. H., Drögemöller, B. I., Koen, L., Gaedigk, A., and Warnich, L. (2010). Elucidation of CYP2D6 genetic diversity in a unique african population: Implications for the future application of pharmacogenetics in the Xhosa population. Ann. Hum. Genet. 74, 340–350. doi:10.1111/j.1469-1809.2010.00585.x
Zhou, Q., Yu, X. M., Lin, H. B., Wang, L., Yun, Q. Z., Hu, S. N., et al. (2009). Genetic polymorphism, linkage disequilibrium, haplotype structure and novel allele analysis of CYP2C19 and CYP2D6 in Han Chinese. Pharmacogenomics J. 9, 380–394. doi:10.1038/tpj.2009.31
Keywords: CYP2D6, pharmacogenetics, Polynesian, Māori, Pasifika, drug response, nanopore sequencing, ancestry
Citation: Hitchman LM, Faatoese A, Merriman TR, Miller AL, Liau Y, Graham OEE, Kee PS, Pearson JF, Fakahau T, Cameron VA, Kennedy MA and Maggo SDS (2022) Allelic diversity of the pharmacogene CYP2D6 in New Zealand Māori and Pacific peoples. Front. Genet. 13:1016416. doi: 10.3389/fgene.2022.1016416
Received: 10 August 2022; Accepted: 26 September 2022;
Published: 13 October 2022.
Edited by:
Luis Abel Quiñones, University of Chile, ChileReviewed by:
Maria Ana Redal, University of Buenos Aires, ArgentinaYitian Zhou, Karolinska Institutet (KI), Sweden
Copyright © 2022 Hitchman, Faatoese, Merriman, Miller, Liau, Graham, Kee, Pearson, Fakahau, Cameron, Kennedy and Maggo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Martin A. Kennedy, bWFydGluLmtlbm5lZHlAb3RhZ28uYWMubno=; Simran D. S. Maggo, c21hZ2dvQGNobGEudXNjLmVkdQ==
†Present address: Yusmiati Liau, Auckland District Health Board, LabPLUS, Auckland City Hospital, Auckland, New Zealand
 Leonie M. Hitchman
Leonie M. Hitchman Allamanda Faatoese
Allamanda Faatoese Tony R. Merriman
Tony R. Merriman Allison L. Miller
Allison L. Miller Yusmiati Liau1†
Yusmiati Liau1† Ping Siu Kee
Ping Siu Kee John F. Pearson
John F. Pearson Martin A. Kennedy
Martin A. Kennedy Simran D. S. Maggo
Simran D. S. Maggo