- 1Division of General Medicine and Geriatrics, Washington University in St. Louis, St. Louis, MO, United States
- 2Rosemead School of Psychology, Biola University, La Mirada, CA, United States
- 3Brown School, Washington University in St. Louis, St. Louis, MO, United States
Background: Religious affiliation and attendance at services is associated with lower levels of support for some genomic activities, such as genetic testing. However, little is known about why or how religion shapes attitudes toward genomics.
Materials and methods: We conducted a cross-sectional survey with 4,939 participants representative of nine religious groups in the US (including atheist and agnostic). The survey examined (a) attitudes toward diverse activities associated with genomic medicine, (b) religious beliefs and practices, (c) control variables including trust in the healthcare system and knowledge of genetics, and (d) demographics. We examined differences between groups using an Analysis of Covariance (ANCOVA), and developed a regression model to identify significant predictors of support for genetic medicine.
Results: When controlling for demographic variables, only small attitudinal differences existed between religious groups, though substantial variability existed within groups. Only seven variables uniquely predicted attitudes toward genomic medicine: acceptance of evolution, support for promoting community health within their spiritual community, knowledge of genetics, more permissive attitudes toward reproduction and end of life care within their spiritual community, distrust in the healthcare system, political orientation, and frequency of volunteering (in descending order).
Discussion: Our findings suggest that stereotyping based on religious affiliation is seriously misguided, and engagement with religious groups on genomic medicine must go beyond education and address moral issues and worldviews.
Introduction
Religion is observed throughout all of human history and across cultures (Smith, 1981; Kim-Prieto, 2014). Despite declining rates of attendance at services (Pew Research Center, 2021), approximately 75% of people in the US still identify with a religion, and 45% say religion is very important in their lives (Gallup, 2024). Among those who are highly religious, their faith is the most important thing they consider when making major decisions or deciding what is right or wrong (Pew Research Center, 2018).
A growing consensus has developed that patient acceptance of genomics, novel vaccines, and public health measures will increase when healthcare professionals engage with patient’s perspectives (Wagner et al., 2016; Glasgow et al., 2018). Within the world of patient-centered outcomes research, “patient-centeredness is at its heart a question of including the worldview of patients” (Frank et al., 2014, p. 1513). From its inception, genomics has included investigation into its ethical, social, and legal implications (ELSI) (McEwen et al., 2014). The ELSI literature has grown significantly since that time, and has generate a body of empirical and policy literature that explores how adult and prenatal genetic testing is understood and used, and what unintended consequences it might have (Henneman et al., 2013; Jarvik et al., 2014; DuBois and Antes, 2015; Schneider et al., 2016; Cousens et al., 2017; Lazaro-Munoz et al., 2017; Sanderson et al., 2022; Iltis et al., 2023); whether genetic counseling is genuinely non-directive and how it is used by patients (Cadigan et al., 2011; Natoli et al., 2012; Jarvik et al., 2014; Stenehjem et al., 2018; Mayo-Gamble et al., 2019); ethical issues in gene editing (Allyse et al., 2015; Sankar and Cho, 2015; Michie and Allyse, 2019; Snure Beckman et al., 2019); and informed consent and privacy protections for biobanking and environmental data storage and use (Kaufman et al., 2008; Sanderson et al., 2017; Platt et al., 2018; Schwab et al., 2018; Lee et al., 2019; Staunton et al., 2019).
Nevertheless, the field of bioethics has been criticized for attempting to represent the interests of the public in health policy while losing touch with the actual views of the public, which are often deeply influenced by religious convictions (Evans, 2014).
Failure to engage patients and the public on matters of religion risks exacerbating health disparities through lower rates of engagement with genomic medicine and public health genomics. Specifically, it may increase disparities between religious and non-religious people but also disparities across races and the urban-rural divide: People belonging to several medically underserved communities—Black, Hispanic, and rural—are more likely to fall into the highly religious group which seeks to make major decisions informed by their faith (Pew Research Center, 2018; Association of Religion Data Archives, 2021).
Past studies indicate that religion is a strong predictor of concerns with genomic medicine and related technologies (Evans, 2006; Evans, 2014; Sayres et al., 2014; Allum et al., 2017; Scheufele et al., 2017; Critchley et al., 2019). However, these studies have generally focused only on religious affiliation and attendance at services; they do not indicate why religious affiliation is generally associated with lower support for genomic medicine. Moreover, most of these studies have focused on one technology or issue in genomic medicine—such as genetic testing—rather than the full array of activities associated with genomic medicine (Etchegary et al., 2010; Sayres et al., 2014; Allum et al., 2017; Scheufele et al., 2017; Critchley et al., 2019).
Because so little is known about why religion is associated with attitudes toward genomic medicine, we proposed a large sample exploratory study with two main research questions:
1. Are there significant differences between religious groups, including atheist and agnostic, regarding support for genomic medicine?
2. While taking into account demographic variables and other known predictors of attitudes, what specific features of religious or spiritual life uniquely predict support for genomic medicine?
Based on prior work in this area, in the present study we adopted a very broad concept of genomic medicine and public health genomics, one that includes six activities: (a) post-natal genetic testing, (b) storing and sharing biospecimens and health data, (c) genome editing, (d) stem cell therapy and research, (f) prenatal genetic testing, and (e) mRNA vaccines (Collins and Varmus, 2015; Jameson and Longo, 2015; Wagner et al., 2016; Sankar and Parker, 2017; Molster et al., 2018; DuBois et al., 2021). Together, these activities have contributed to significant health benefits, reducing infection rates, fostering innovative research, identifying health disorders, and more recently, even correcting genetic disorders (Manolio et al., 2024).
In selecting religious variables to examine, we drew upon several resources: (a) the project’s National Research Advisory Board, which is comprised of nine leaders working at the intersection of health and diverse religious traditions; (b) the guidance of a consultant who served as an editor of the encyclopedic work, Measures of Religiosity and Spirituality (Hill et al., 2026); and (c) a review of existing measures of variables of interest, including integration of faith with daily living, religious fundamentalism, views toward evolution and the theology of the body, religious discrimination, view toward God’s role in determining health, and Pew survey items on religious affiliation and practice (Hoge, 1972; Rutledge and Warden, 1999; Wallston et al., 1999; Altemeyer and Hunsberger, 2004; Mahoney et al., 2005; Pew Research Center, 2014; Kawika Allen et al., 2020).
Materials and methods
Study design
This study used a non-experimental, cross-sectional design, which is appropriate for exploratory studies aimed at testing differences between groups and building predictive models (Vogt et al., 2012). Participants completed a battery of measures in an online survey.
Because some of our analytical decisions were necessarily data-driven, we share some data in our Methods section, while reserving primary findings for the Results section.
Data collection methods
The online survey battery consisted of measures assessing participants’ religious and spiritual beliefs and practices, which we have named the Spiritual Portrait Questionnaire. They also completed the Attitudes toward Genomics and Precision Medicine measure, measures of genetic knowledge, healthcare system distrust, and religious discrimination, and items pertaining to participant demographics. Further details of these measure are described in Supplementary Material.
Sample characteristics
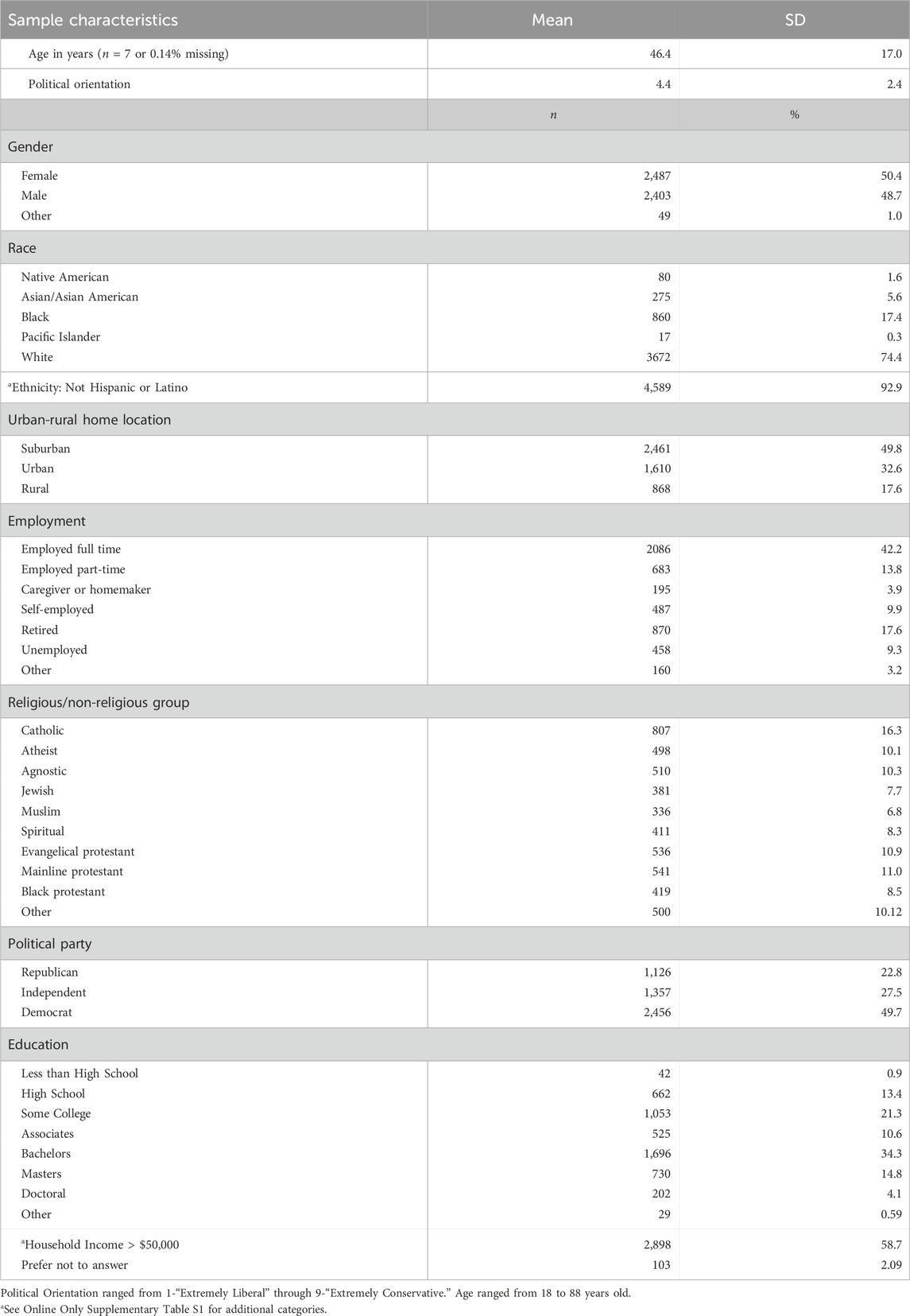
Participants were recruited using two panel service companies, Prolific and Cloud Research. From Prolific, we recruited participants who were representative of the US population in terms of age, gender, and race (n = 2,999). From Cloud Research, we recruited stratified samples of at least 300 participants from each of six religious groups: Black Protestant (e.g., African Methodist Episcopalian and National Baptist Convention), Catholic, Evangelical Protestant (e.g., Assemblies of God, Church of Christ, and Southern Baptist), Jewish (e.g., Conservative, Orthodox, and Reform), Mainline Protestant (e.g., Methodist, Episcopal, and Lutheran), and Muslim (e.g., Shi’a and Sunni) (n = 1,940) (Pew Research Center, 2025). To qualify for the study, participants needed to be 18 years or older and located in the United States. After removing participants who did not pass preliminary quality checks, our total sample size was N = 4,939 participants. Table 1 lists demographic details and composition of religious groups.
Survey administration
Participants completed the survey in Qualtrics, an online survey platform, in February, March, and April 2023. The survey took 30–45 min to complete. Within the survey, participants needed to correctly respond to two of three total attention check items presented (e.g., “If you are reading this item, please select the option strongly agree as your answer”).
Ethical considerations
The study was approved (IRB #202201153) by the Institutional Review Board (IRB) at Washington University in St. Louis. Surveys were anonymous, using unique participant IDs provided by the survey panel companies. All data were stored in a password protected Box cloud storage folder.
Statistical analysis
To answer the two main research questions, this study was divided into two major analytical sections. The first analytical section is comprised of an Analysis of Covariance (ANCOVA) model predicting general attitudinal support of genetic precision medicine. The second analytical section was comprised of a backward chunkwise elimination model building procedure (Kleinbaum et al., 2008) predicting general attitudinal support of genetic precision medicine. Supplementary Material provides further details on all variables that were included in the ANCOVA and backward chunkwise elimination model building procedure. Both analyses were conducted using IBM SPSS Statistics (Version 29).
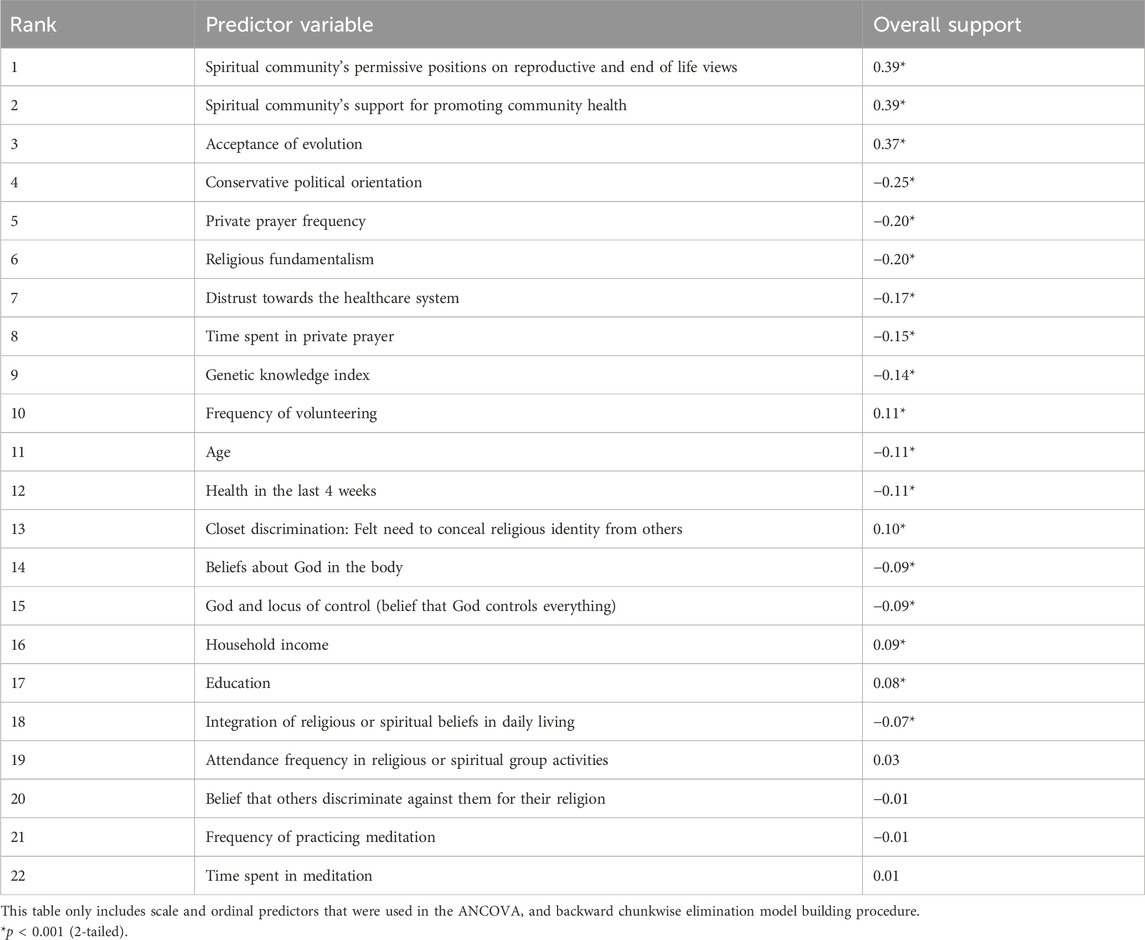
Table 2 depicts the bivariate correlations between predictor variables used in the ANCOVA and backward chunkwise elimination model building procedures with overall attitudinal support for genomic medicine, which was calculated as the mean score of responses to the statements of general support for each of the six genomic medicine activities described in the AGPM. Scores thus ranged from 1 (strongly disagree) to 7 (strongly agree).
Analysis 1: Analysis of covariance (ANCOVA)
The ANCOVA compared means of general attitudinal support for genetic precision medicine across the nine religious and non-religious groups while accounting for six demographic covariates. The religious and non-religious groups were Agnostic, Atheist, Black Protestant, Catholic, Evangelical Protestant, Jewish, Mainline Protestant, Muslim, and Spiritual but not religious. The demographic covariates were age in years, education, household income, urban/suburban/rural status, political orientation, and employment. The covariates were selected a priori based on the research team’s evaluation of previous related literature. Five hundred participants were excluded because they did not belong to one of the nine religious/non-religious groups—e.g., they reported being Orthodox Christian, no denominational affiliation, Mormon, Jehovah’s witness, Buddhist, Hindu—as these subgroup samples were too small to analyze. Consistent with safe harbor privacy rules, we excluded respondents who reported age ≥89 (n = 7). Additionally, 167 participants were excluded when responses could not be used in statistical analyses, such as “other,” “prefer not to answer,” or “more than one” on education, income, and race respectively. Because the exclusionary criteria were not mutually exclusive for the ANCOVA subsample (e.g., a participant may be age >89 and education listed as “other”), the total number of number of participants removed was only 623; and our total sample size for the ANCOVA was thus 4,316.
Analysis 2: Backward chunkwise elimination regression model building
The backward chunkwise elimination procedure was conducted to build a regression model for predicting attitudinal support for genetic precision medicine based on religious or spiritual variables, accounting for (1) demographic variables, (2) religious group, and (3) other general covariates known to predict attitudes in the literature. The research team identified 28 prospective predictor variables to include in the maximum model, which could be broadly divided into four categories (demographic variables, religious group, religious or spiritual predictors, or general covariates; Supplementary Material, pp. 5–10).
Because the model building procedure involved religious or spiritual variables, participants who reported being atheistic or agnostic (n = 1,008) were excluded from the model building procedure because they did not complete questionnaires related to religious or spiritual predictors. Additionally, participants who could not be categorized into any of the religious or non-religious categories (n = 500) were excluded from the model building procedures–leaving us with N = 3,431 participants. Subsequently, this subset of participants was randomly divided into a training group (n = 1,715) and holdout group (n = 1,716). Further details about model reliability indices can be found in Supplementary Material (p. 12). A backward chunkwise elimination model building procedure was conducted in the training group sample (Kleinbaum et al., 2008). More details about the backward chunkwise elimination procedure are described in the Supplementary Material (p. 13).
Results
Dispersion of mean support scores
Figure 1 presents the distribution of participants’ mean level of support across all six genomic and precision medicine activities (1 strongly disagree – seven strongly agree) with higher scores indicating higher levels of support. The mean score of 5.37 roughly corresponds to a response of “somewhat agree” (a score of 5) to the statement “I generally support [the activity]”. Only 12% of respondents had mean ratings at or below neutral. Supplementary Figure S1 shows the distribution of support across all six genomic and precision medicine activities.
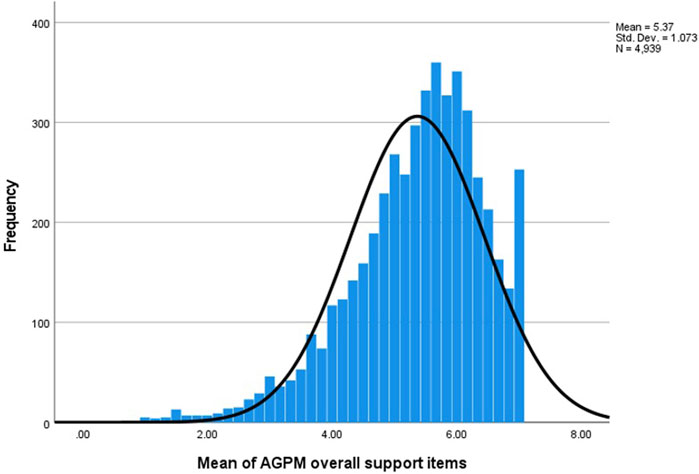
Figure 1. Dispersion of participants’ overall support (1–7) for genomic and medicine activities (Supplementary Figure S1 illustrates the distribution of “support” responses at the level of specific activities).
Analysis 1: Are there significant differences between religious groups, including atheist and agnostic, regarding support for genomic medicine?
Prior to building the ANCOVA model, we assessed collinearity among the predictors by conducting preliminary pairwise correlations and ANOVA tests between demographic variables (i.e., age, education, household income, employment, urban/suburban/rural status, and political orientation). The relationship between age and employment had a large effect size (
The ANCOVA results suggested statistically significant, but very small mean differences (partial
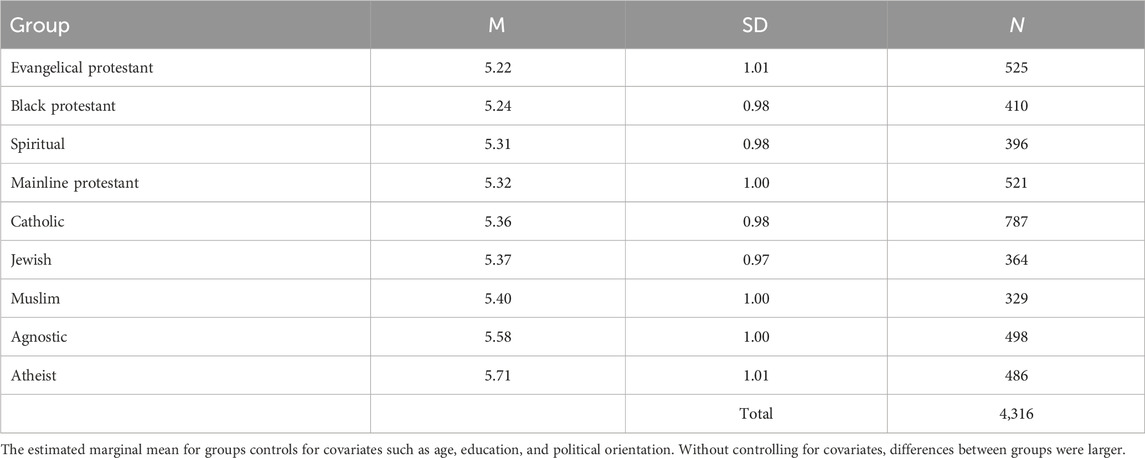
Table 3. Estimated marginal means for attitudinal support among religious and non-religious groups in 4,316 survey participants in 2023.
Analysis 2: What specific features of religious or spiritual life uniquely predict support for genomic medicine?
Prior to the backward chunkwise elimination procedure, a total of 28 predictors were considered for inclusion in the maximum model (Supplementary Material, pp. 5–10). Based on the training sample (n = 1,715), we conducted preliminary correlations and ANOVAs between each predictor and attitudinal support to exclude predictors that were (1) not statistically significant (p < 0.05) and (2) had a small effect size (r < 0.1;
Next, we sequentially removed 15 grouped predictors that produced a minimum test statistic Fp that was smaller than FCRIT, where α = 0.002) (Šidák, 1967) until the minimum test statistic Fp in the model was larger than FCRIT, leaving us with six grouped predictors. The seven variables contained in these six groups were then subjected to a single variable backward elimination procedure using the same inclusion criterion (α = 0.002). All seven variables met the criterion for inclusion. Thus, these seven predictors were entered into a hierarchical regression (Table 4), arranged according to previously mentioned conceptual categories (see Supplementary Material pp. 5–10 for variable categories).
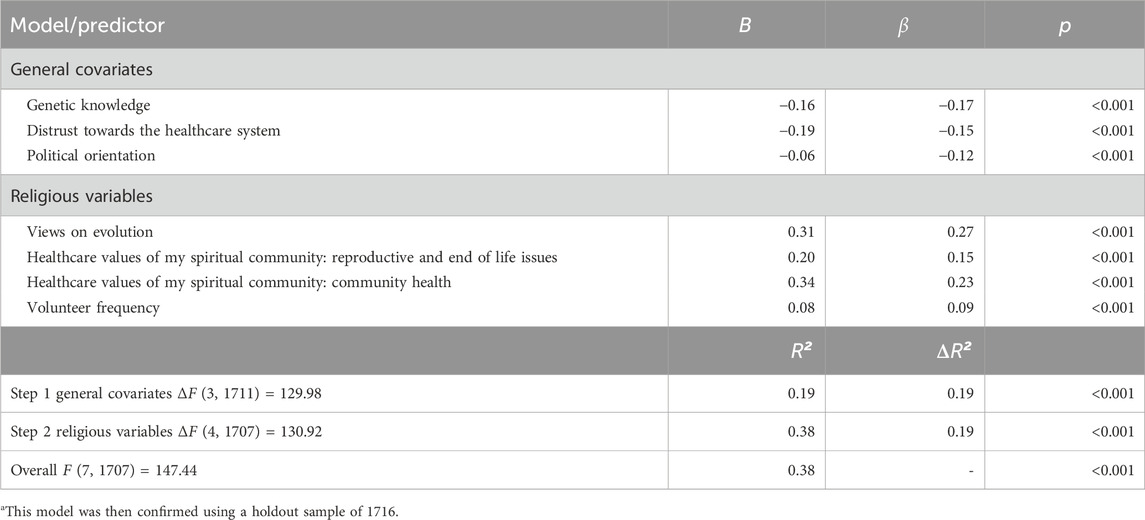
Table 4. Model for predicting support for the six genomic and precision medicine activities in a sample of n = 1,715.a
Next, we evaluated the reliability of the model in the holdout sample (n = 1,716). We used the estimated prediction equation from the training sample (n = 1,715) to compute predicted values of the outcome in the holdout sample and determine the percentage relative shrinkage (Supplementary Material, p. 12). The shrinkage on cross-validation was 0.054, which was smaller than 0.10 suggested threshold (Kleinbaum et al., 2008), supporting the conclusion that this was a reliable model.
In summary, only four religious/spiritual variables remained as statistically significant predictors (p < 0.001) of support for genomic medicine after accounting for statistically significant general covariate variables, with a moderate effect size (ΔR2 = 0.19) (Cohen, 2013) when all four variables were entered into the regression model (Table 4). Acceptance of evolution (B = 0.31, p < 0.001), permissive attitudes among their spiritual community regarding to reproductive (e.g., abortion) and end-of-life issues (e.g., euthanasia) (B = 0.20, p < 0.001), more favorable attitudes among their spiritual community regarding community health (B = 0.34, p < 0.001), and higher frequency of volunteer experience within their religious or spiritual group (e.g., help with food drives) (B = 0.08, p < 0.001) predicted stronger support for genetic precision medicine.
Discussion
In a large sample that was nearly representative of the US in terms of age, gender, and race, with more than 300 participants representing each of the largest religious and non-religious groups in the US, we identified the variables that most strongly predicted support for genomic medicine. In descending order, these were: acceptance of evolution, support for promoting community health within their spiritual community, knowledge of genetics, and more permissive attitudes toward reproduction and end of life care within their spiritual community, distrust in the healthcare system, political orientation, and frequency of volunteering (Table 4). Many variables were examined but had no independent explanatory power such as level of education, income, age, gender, and race.
These findings are striking considering that the issues examined in this survey included elements of genomic healthcare that have been highly politicized (such as mRNA vaccines, stem cell research, and prenatal genetic testing). Despite being highly politicized, the influence of political orientation was weak when compared to several religious variables. Previous research has focused heavily on race, trust in the healthcare system, and level of education as possible predictors (Sayres et al., 2014; Critchley et al., 2019; Fisher et al., 2020); and indeed, we found that many of these variables were significantly correlated with attitudes toward genomic medicine (Table 2). However, by examining religious variables in more depth than is common and by using a rigorous regression design with a large sample, we found that these commonly examined factors generally paled in comparison with religiously-influenced variables. This aligns with the notion that faith is the most important consideration when making major decisions or deciding right or wrong among the highly religious (Pew Research Center, 2018).
At the same time, after controlling for covariates, the differences between religious and non-religious groups were very modest in terms of support for genomic medicine. That is, there were differences between religious groups, but they are not best explained in terms of group membership. In his post-mortem of the 2024 US Presidential election, David Brooks suggests that many people forecasted the results badly due to poor mental models. Specifically, he claims that the 2024 election results challenge a mental model in which “individual cognition is de-emphasized while collective consciousness is emphasized,” which views people “as members of a group before they are seen as individuals,” and where “groups are assumed to be relatively homogeneous” (Brooks, 2024). This study suggests that his intuition is correct: Most variation observed in this study was not across groups but within groups. The biggest difference in group mean support for genomic medicine that we observed—between atheists and Evangelical Protestants—was only 0.49, while the smallest standard deviation within a group was twice that size (0.97). This is an important finding: When it comes to attitudes toward genomic medicine, we must not make assumptions about people based on religious group membership.
How can this be reconciled with the finding that the strongest predictors of attitudes were religious—not political, educational, or racial? Specifically, how can this be reconciled with the fact that some of the strongest predictors of attitudes were precisely the values of their spiritual community? The groups that matter may be smaller, local, faith communities, which may not be homogenous within larger families of faith (e.g., Evangelical Protestant or Jewish). Further, within these groups there exist very different attitudes toward matters such as evolution and creation, and people may interpret their own traditions very differently.
On the matter of evolution, one might expect attitudes to be related to level of education. However, education level had no explanatory value in our models. Recent work by the sociologist, John Evans, may offer a key to understanding these findings. He suggests that the science-religion divide has less to do with methods of knowing the world and more to do with morality. His review of data indicates that “no religious group differs from the nonreligious comparison group in its propensity to seek out scientific knowledge,” but those who are religious may reject some claims that appear to contradict religious teachings, and above all, they have concerns about the moral agenda of researchers, or in our case, genomic medicine (e.g., regarding embryonic stem cell research, vaccine mandates, or prenatal genetic testing) (Evans, 2011, p. 707). It is possible that Evans’ findings also help explain how it is possible that religious fundamentalism and views about God and the body were not significant predictors of support for genomic medicine in our model: Fundamentalism and related beliefs do not diminish support unless they are accompanied by a rejection of scientific claims that appear to contradict religious beliefs. While scientists may not think fundamentalist beliefs and scientific beliefs can coexist, it appears that they can in fact (Evans, 2018).
Our study, combined with these insights from Evans, suggests that engaging the public with information only—that is educating the public on the nature and benefits of various genomic medicine activities—may be radically insufficient to increase acceptance of these activities within religious circles. Differences in how individuals evaluate these activities and technologies may rest more heavily on worldviews and morals than on factual knowledge. Effective engagement with religious communities—or individuals with religious convictions—may require two-way listening. Further, we may need to accept that some activities—despite their personal health or public health benefits—may never be acceptable to some segments of society.
As the United States and the international community observe rapid and radical changes in healthcare and health research policies with the start of President Trump’s second term, it is clear that we are in the midst of a so-called culture war (Messerly, 2025). But in healthcare, there is no room for cultural combat against patients or research participants. Peaceful and constructive engagement begins with understanding. We believe the current study greatly advances understanding by uncovering a lack of major attitudinal differences due to religious affiliation, and a diversity of views within groups. This is not to say that religious convictions do not matter–some religious convictions matter more than political and educational differences. Increasing awareness of these convictions and social dynamics within groups will be crucial to effective engagement with religious communities and individuals.
Limitations of the current study include the following: The sample was somewhat skewed toward more educated and more liberal individuals, which affects the generalizability of our descriptive statistics, though our sample size and statistical approach make it unlikely any inferential conclusions would change. Our sample sizes of specific racial and ethnic groups make it impossible to examine them as religious subgroups. Future research would benefit from stratified or purposive sampling by race and religion (Critchley et al., 2019). It might also examine how loyalty (or in-group vs. out-group thinking) moderates the effects of the values of one’s spiritual community regarding genomic medicine, which was a strong predictor in this study. Finally, our study’s measurement of certain predictor variables were brief when they were not the primary area of focus. For example, our measure of genetic knowledge focused on genetics, rather than, for example, the logistics of genetic testing and biobanking; our measures of political orientation included party affiliation and self-described liberal-conservative orientation, but did not assess group loyalty, which characterizes many people’s style of political engagement (Graham et al., 2009). Other variables, such as whether participants themselves or their families members have a genetic disorder, were not explored in this paper given the need to control the length of the survey, which required 30–45 min to complete.
In a follow up qualitative interview project, we are examining to what extent faith leaders (N = ∼160) from the six religious groups examined in this survey believe that religious teachings on prenatal genetic testing and vaccines are central and unchanging or rather might change with new information. We are also asking faith leaders what would constitute constructive and respectful public health engagement with their faith communities. Respecting the worldview of patients is important for reasons of ethics and effective engagement (Frank et al., 2014), yet one hopes that if beliefs are based on misinformation rather than core values or religious beliefs, then they might be subject to revision.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Human Research Protection Office at Washington University in St. Louis. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because this was a minimal risk survey and participants agreed to participate by clicking on a button.
Author contributions
JD: Conceptualization, Methodology, Supervision, Writing – original draft, Funding acquisition. EC: Data curation, Formal Analysis, Methodology, Writing – review and editing. ES: Data curation, Formal Analysis, Writing – review and editing. JH: Data curation, Formal Analysis, Writing – review and editing. PH: Conceptualization, Writing – review and editing. KB: Project administration, Writing – review and editing. LB: Writing – review and editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Research reported in this publication was supported by the National Human Genome Research Institute (NHGRI) of the National Institutes of Health under award 5R01HG012830.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgene.2025.1587774/full#supplementary-material
References
Allum, N., Allansdottir, A., Gaskell, G., Hampel, J., Jackson, J., Moldovan, A., et al. (2017). Religion and the public ethics of stem-cell research: attitudes in Europe, Canada and the United States. PLoS One 12 (4), e0176274. doi:10.1371/journal.pone.0176274
Allyse, M., Michie, M., Mozersky, J., and Rapp, R. (2015). Cherchez la Femme: reproductive CRISPR and women's choices. Am. J. Bioeth. 15 (12), 47–49. doi:10.1080/15265161.2015.1103808
Altemeyer, B., and Hunsberger, B. (2004). RESEARCH: a revised religious fundamentalism scale: the short and sweet of it. Int. J. Psychol. Relig. 14 (1), 47–54. doi:10.1207/s15327582ijpr1401_4
Association of Religion Data Archives (2021). Religious service attendance by race (2014 data). Available online at: https://www.thearda.com/quickStats/qs_105_p.asp.
Cadigan, R. J., Michie, M., Henderson, G., Davis, A. M., and Beskow, L. M. (2011). The meaning of genetic research results: reflections from individuals with and without a known genetic disorder. J. Empir. Res. Hum. Res. Ethics 6 (4), 30–40. doi:10.1525/jer.2011.6.4.30
Collins, F. S., and Varmus, H. (2015). A new initiative on precision medicine. N. Engl. J. Med. 372 (9), 793–795. doi:10.1056/NEJMp1500523
Cousens, N., Kaur, R., Meiser, B., and Andrews, L. (2017). Community attitudes towards a Jewish community BRCA1/2 testing program. Fam. Cancer 16 (1), 17–28. doi:10.1007/s10689-016-9918-0
Critchley, C., Nicol, D., Bruce, G., Walshe, J., Treleaven, T., and Tuch, B. (2019). Predicting public attitudes toward gene editing of germlines: the impact of moral and hereditary concern in human and animal applications. Front. Genet. 9, 704. doi:10.3389/fgene.2018.00704
DuBois, J. M., and Antes, A. L. (2015). In guanine we trust: genetic testing and the sense of coherence. Narrat. Inq. Bioeth. 5 (3), 237–244. doi:10.1353/nib.2015.0063
DuBois, J. M., Mozersky, J., Antes, A., English, T., Parsons, M. V., and Baldwin, K. (2021). Attitudes toward genomics and precision medicine. J. Clin. Transl. Sci. 5 (1), e120. doi:10.1017/cts.2021.774
Etchegary, H., Cappelli, M., Potter, B., Vloet, M., Graham, I., Walker, M., et al. (2010). Attitude and knowledge about genetics and genetic testing. Public Health Genomics 13 (2), 80–88. doi:10.1159/000220034
Evans, J. H. (2006). Religious belief, perceptions of human suffering, and support for reproductive genetic technology. J. Health Polit. Policy Law 31 (6), 1047–1074. doi:10.1215/03616878-2006-019
Evans, J. H. (2011). Epistemological and moral conflict between religion and science. J. Sci. Study Relig. 50 (4), 707–727. doi:10.1111/j.1468-5906.2011.01603.x
Evans, J. H. (2014). The history and future of bioethics: a sociological view. New York, NY: Oxford.
Evans, J. H. (2018). Morals not knowledge: recasting the contemporary U.S. conflict between religion and science. Berkeley, CA: University of California Press.
Fisher, E. R., Pratt, R., Esch, R., Kocher, M., Wilson, K., Lee, W., et al. (2020). The role of race and ethnicity in views toward and participation in genetic studies and precision medicine research in the United States: a systematic review of qualitative and quantitative studies. Mol. Genet. Genomic Med. 8 (2), e1099. doi:10.1002/mgg3.1099
Frank, L., Basch, E., and Selby, J. V.Patient-Centered Outcomes Research Institute (2014). The PCORI perspective on patient-centered outcomes research. JAMA 312 (15), 1513–1514. doi:10.1001/jama.2014.11100
Gallup (2024). How religious are Americans? Available online at: https://news.gallup.com/poll/358364/religious-americans.aspx (Accessed 17 October 2024).
Glasgow, R. E., Kwan, B. M., and Matlock, D. D. (2018). Realizing the full potential of precision health: the need to include patient-reported health behavior, mental health, social determinants, and patient preferences data. J. Clin. Transl. Sci. 2 (3), 183–185. doi:10.1017/cts.2018.31
Graham, J., Haidt, J., and Nosek, B. A. (2009). Liberals and conservatives rely on different sets of moral foundations. J. Personality Soc. Psychol. 96 (5), 1029–1046. doi:10.1037/a0015141
Henneman, L., Vermeulen, E., van El, C. G., Claassen, L., Timmermans, D. R. M., and Cornel, M. C. (2013). Public attitudes towards genetic testing revisited: comparing opinions between 2002 and 2010. Eur. J. Hum. Genet. 21 (8), 793–799. doi:10.1038/ejhg.2012.271
Hill, P. C., Hood Jr, R. W., Jong, J., and Harris, K. A. (2026). Measures of religiosity and spirituality. New York, NY: Springer.
Hoge, R. (1972). A validated intrinsic religious motivation scale. J. Sci. Study Relig. 11, 369–376. doi:10.2307/1384677
Iltis, A. S., Rolf, L., Yaeger, L., Goodman, M. S., and DuBois, J. M. (2023). Attitudes and beliefs regarding race-targeted genetic testing of Black people: a systematic review. J. Genet. Couns. 32 (2), 435–461. doi:10.1002/jgc4.1653
Jameson, J. L., and Longo, D. L. (2015). Precision medicine--personalized, problematic, and promising. N. Engl. J. Med. 372 (23), 2229–2234. doi:10.1056/NEJMsb1503104
Jarvik, G. P., Amendola, L. M., Berg, J. S., Brothers, K., Clayton, E. W., Chung, W. K., et al. (2014). Return of genomic results to research participants: the floor, the ceiling, and the choices in between. Am. J. Hum. Genet. 94 (6), 818–826. doi:10.1016/j.ajhg.2014.04.009
Kaufman, D., Geller, G., Leroy, L., Murphy, J., Scott, J., and Hudson, K. (2008). Ethical implications of including children in a large biobank for genetic-epidemiologic research: a qualitative study of public opinion. Am. J. Med. Genet. Part C 148C (1), 31–39. doi:10.1002/ajmg.c.30159
Kawika Allen, G. E., Wang, K. T., Richards, P. S., Ming, M., and Suh, H. N. (2020). Religious discrimination scale: development and initial psychometric evaluation. J. Relig. Health 59 (2), 700–713. doi:10.1007/s10943-018-0617-z
Kleinbaum, D. G., Kupper, L. L., Nizam, A., and Muller, K. E. (2008). Applied regression Analysis and other multivariable methods. Belmont, CA: Duxbury Press.
Lazaro-Munoz, G., Conley, J. M., Davis, A. M., Prince, A. E., and Cadigan, R. J. (2017). Which results to return: subjective judgments in selecting medically actionable genes. Genet. Test. 21 (3), 184–194. doi:10.1089/gtmb.2016.0397
Lee, S. S., Cho, M. K., Kraft, S. A., Varsava, N., Gillespie, K., Ormond, K. E., et al. (2019). I don't want to be Henrietta Lacks: diverse patient perspectives on donating biospecimens for precision medicine research. Genet. Med. 21 (1), 107–113. doi:10.1038/s41436-018-0032-6
Mahoney, A., Carels, R. A., Pargament, K. I., Wachholtz, A., Edwards Leeper, L., Kaplar, M., et al. (2005). RESEARCH: the sanctification of the body and behavioral health patterns of college students. Int. J. Psychol. Relig. 15 (3), 221–238. doi:10.1207/s15327582ijpr1503_3
Manolio, T. A., Narula, J., Rupert, A., Bult, C. J., Chisholm, R. L., Ginsburg, G. S., et al. (2024). Genomic medicine year in review: 2024. Am. J. Hum. Genet. 111 (12), 2585–2588. doi:10.1016/j.ajhg.2024.11.002
Mayo-Gamble, T. L., Schlundt, D., Cunningham-Erves, J., Murry, V. M., Bonnet, K., Quasie-Woode, D., et al. (2019). Sickle cell carriers' unmet information needs: beyond knowing trait status. J. Genet. Couns. 28 (4), 812–821. doi:10.1002/jgc4.1124
McEwen, J. E., Boyer, J. T., Sun, K. Y., Rothenberg, K. H., Lockhart, N. C., and Guyer, M. S. (2014). The ethical, legal, and social implications program of the national human genome research Institute: reflections on an ongoing experiment. Annu. Rev. Genom Hum. Genet. 15, 481–505. doi:10.1146/annurev-genom-090413-025327
Michie, M., and Allyse, M. (2019). Gene modification therapies: views of parents of people with Down syndrome. Genet. Med. 21 (2), 487–492. doi:10.1038/s41436-018-0077-6
Molster, C. M., Bowman, F. L., Bilkey, G. A., Cho, A. S., Burns, B. L., Nowak, K. J., et al. (2018). The evolution of public health genomics: exploring its past, present, and future. Front. Public Health 6, 247. doi:10.3389/fpubh.2018.00247
Natoli, J. L., Ackerman, D. L., McDermott, S., and Edwards, J. G. (2012). Prenatal diagnosis of Down syndrome: a systematic review of termination rates (1995-2011). Prenat. Diagn 32 (2), 142–153. doi:10.1002/pd.2910
Pew Research Center (2014). 2014 religious landscape study (RLS-II) main survey of nationally representative sample of adults. Washington, DC: Pew Research Center. Available online at: https://www.pewforum.org/wp-content/uploads/sites/7/2015/11/201.11.03_rls_ii_questionnaire.pdf.
Pew Research Center (2025). Decline of christianity in the U.S. Has slowed, maybe have leveled off. Pew Research Center.
Platt, J. E., Jacobson, P. D., and Kardia, S. L. R. (2018). Public trust in health information sharing: a measure of system trust. Health Serv. Res. 53 (2), 824–845. doi:10.1111/1475-6773.12654
Rutledge, M. L., and Warden, M. A. (1999). The development and validation of the measure of acceptance of the theory of evolution instrument. Sch. Sci. Math. 99 (1), 13–18. doi:10.1111/j.1949-8594.1999.tb17441.x
Sanderson, S. C., Brothers, K. B., Mercaldo, N. D., Clayton, E. W., Antommaria, A. H. M., Aufox, S. A., et al. (2017). Public attitudes toward consent and data sharing in biobank research: a large multi-site experimental survey in the us. Am. J. Hum. Genet. 100 (3), 414–427. doi:10.1016/j.ajhg.2017.01.021
Sanderson, S. C., Lewis, C., Hill, M., Peter, M., McEntagart, M., Gale, D., et al. (2022). Decision-making, attitudes, and understanding among patients and relatives invited to undergo genome sequencing in the 100,000 Genomes Project: a multisite survey study. Genet. Med. 24 (1), 61–74. doi:10.1016/j.gim.2021.08.010
Sankar, P. L., and Cho, M. K. (2015). Engineering values into genetic engineering: a proposed analytic framework for scientific social responsibility. Am. J. Bioeth. 15 (12), 18–24. doi:10.1080/15265161.2015.1104169
Sankar, P. L., and Parker, L. S. (2017). The Precision Medicine Initiative's All of Us Research Program: an agenda for research on its ethical, legal, and social issues. Genet. Med. 19 (7), 743–750. doi:10.1038/gim.2016.183
Sayres, L. C., Allyse, M., Goodspeed, T. A., and Cho, M. K. (2014). Demographic and experiential correlates of public attitudes towards cell-free fetal DNA screening. J. Genet. Couns. 23 (6), 957–967. doi:10.1007/s10897-014-9704-9
Scheufele, D. A., Xenos, M. A., Howell, E. L., Rose, K. M., Brossard, D., and Hardy, B. W. (2017). US attitudes on human genome editing. Science 357 (6351), 553–554. doi:10.1126/science.aan3708
Schneider, J. L., Goddard, K. A., Davis, J., Wilfond, B. S., Kauffman, T. L., Reiss, J. A., et al. (2016). Is it worth knowing? Focus group participants' perceived utility of genomic preconception carrier screening. J. Genet. Couns. 25 (1), 135–145. doi:10.1007/s10897-015-9851-7
Schwab, A. P., Luu, H. S., Wang, J., and Park, J. Y. (2018). Genomic privacy. Clin. Chem. 64 (12), 1696–1703. doi:10.1373/clinchem.2018.289512
Šidák, Z. (1967). Rectangular confidence regions for the means of multivariate normal distributions. J. Am. Stat. Assoc. 62 (318), 626–633. doi:10.1080/01621459.1967.10482935
Smith, W. C. (1981). Towards a world theology: faith and the comparative history of religion. Springer.
Snure Beckman, E., Deuitch, N., Michie, M., Allyse, M. A., Riggan, K. A., and Ormond, K. E. (2019). Attitudes toward hypothetical uses of gene-editing technologies in parents of people with autosomal aneuploidies. Crispr J. 2 (5), 324–330. doi:10.1089/crispr.2019.0021
Staunton, C., Adams, R., Dove, E. S., Harriman, N., Horn, L., Labuschaigne, M., et al. (2019). Ethical and practical issues to consider in the governance of genomic and human research data and data sharing in South Africa: a meeting report. AAS Open Res. 2, 15. doi:10.12688/aasopenres.12968.1
Stenehjem, D. D., Au, T., Sainski, A. M., Bauer, H., Brown, K., Lancaster, J., et al. (2018). Impact of a genetic counseling requirement prior to genetic testing. BMC Health Serv. Res. 18 (1), 165. doi:10.1186/s12913-018-2957-5
Vogt, W. P., Gardner, D. C., and Haeffele, L. M. (2012). When to use what research design. New York, NY: Guilford.
Wagner, J. K., Peltz-Rauchman, C., Rahm, A. K., and Johnson, C. C. (2016). Precision engagement: the PMI's success will depend on more than genomes and big data. Genet. Med. 19, 620–624. doi:10.1038/gim.2016.165
Keywords: ELSI, genomics, survey research, ethics, religion & public life
Citation: DuBois JM, Chin EG, Solomon ED, Harris JK, Hill P, Baldwin K and Baker LL (2025) Religious factors predict support for genomic medicine more strongly than politics, education, or trust: A survey of 4,939 adults in the United States. Front. Genet. 16:1587774. doi: 10.3389/fgene.2025.1587774
Received: 04 March 2025; Accepted: 16 May 2025;
Published: 04 June 2025.
Edited by:
Hannah Kim, Yonsei University, Republic of KoreaReviewed by:
Joseph L. Graves Jr, North Carolina Agricultural and Technical State University, United StatesGarbiñe Saruwatari, National Institute of Genomic Medicine (INMEGEN), Mexico
Copyright © 2025 DuBois, Chin, Solomon, Harris, Hill, Baldwin and Baker. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: James M. DuBois, ZHVib2lzam1Ad3VzdGwuZWR1
†ORCID: James M. DuBois, orcid.org/0000-0002-3712-7051; Eu Gene Chin, orcid.org/0000-0003-2615-9223; Erin D. Solomon, orcid.org/0000-0002-3295-0698; Jenine K. Harris, orcid.org/0000-0002-3576-5906; Peter Hill, orcid.org/0000-002-3423-5719; Lauren L. Baker, orcid.org/0009-0009-6627-9079
 James M. DuBois
James M. DuBois Eu Gene Chin
Eu Gene Chin Erin D. Solomon
Erin D. Solomon Jenine K. Harris
Jenine K. Harris Peter Hill
Peter Hill Kari Baldwin
Kari Baldwin Lauren L. Baker
Lauren L. Baker