- 1Shanghai Key Laboratory of Birth Defects, Pediatric Heart Center, Children’s Hospital of Fudan University, Shanghai, China
- 2BengBu First People’s Hospital, BengBu, China
- 3Obstetrics and Gynecology Hospital, Institute of Reproduction and Development, Fudan University, Shanghai, China
- 4Fujian Key Laboratory of Neonatal Diseases, Children’s Hospital of Fudan University at Xiamen (Xiamen Children’s Hospital), Fujian, China
- 5Research Unit of Early Intervention of Genetically Related Childhood Cardiovascular Diseases (2018RU002), Chinese Academy of Medical Sciences, Shanghai, China
Introduction: The genetic factors underlying congenital heart disease and heterotaxy (CHD/HTX) are complex, including copy number variants, loss-of-function mutations, and missense variants, many of which can be detected by high-throughput sequencing. The screening for chromosomal structural variations (SVs) is another important strategy to understand the genetic etiology of CHD/HTX.
Methods: We employed optical genome mapping (OGM), an innovative technique capable of capturing SVs often missed by traditional cytogenetic methods, to screen for SVs in 12 patients with complex CHD/HTX. Several patients had previously undergone chromosomal microarray analysis (CMA) or whole exome sequencing (WES), but their genetic diagnoses remained inconclusive.
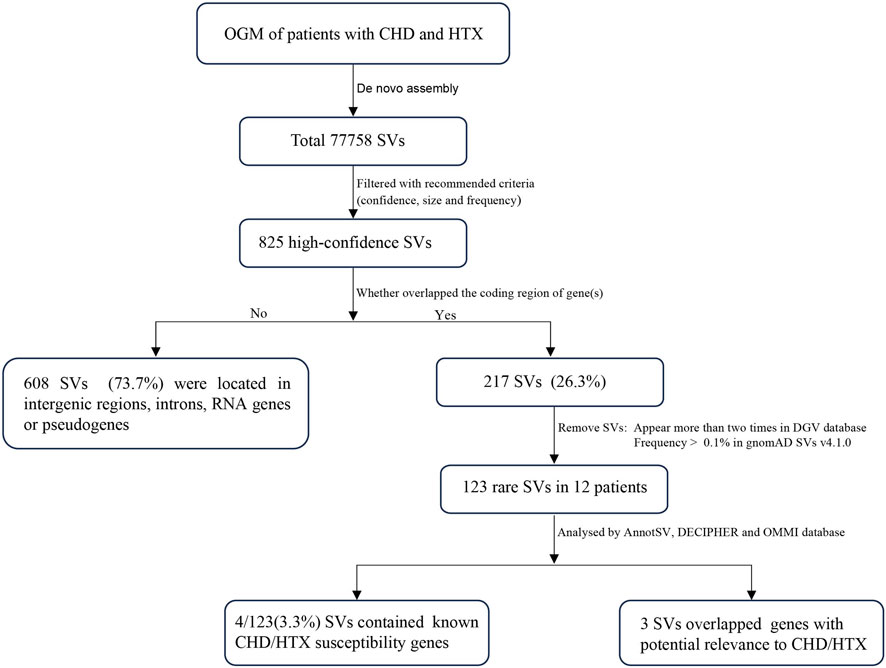
Results: By integrating data from CMA or WES, we analyzed potentially pathogenic SVs in patients with CHD/HTX. In total, we identified 825 high-confidence SVs, including 609 SVs (73.7%) located in intergenic regions or containing introns, pseudogenes, or RNA genes, while 217 (26.3%) overlapped the coding regions of genes. Analyzed through AnnotSV, DECIPHER and OMIM databases, 7 SVs of interest were identified, including: one previously reported pathogenic SV, three SVs overlapping established CHD/HTX associated genes (NOTCH2, KDM6A and CBL), and three SVs located in SMARCA2 and CEP164, which are proposed as candidate susceptibility genes pending further validation.
Conclusion: Our findings highlight the utility of OGM in analyzing the genetic etiology of CHD/HTX and contribute to broadening of the complex genetic landscape underlying these diseases.
1 Introduction
Congenital heart disease (CHD) is the most common birth defect affecting approximately 8.98‰ of live births in China (Zhao et al., 2019). Heterotaxy (HTX) is a rare disorder characterized by the abnormal arrangement of visceral organs along the left-right (L-R) body axis and is strongly associated with complex CHD. Approximately 83% of HTX patients present with complex CHD, including double outlet right ventricle (DORV), transposition of the great arteries (TGA) and atrioventricular septal defects. Conversely, about 2.3% of patients with CHD are diagnosed with HTX, a condition associated with poor prognosis and high mortality (Lin et al., 2014; Huang et al., 2023).
The etiology and underlying mechanisms of the co-occurrence of CHD and HTX remain incompletely understood despite decades of research. Bilateral symmetry in the embryo is first broken at the ventral node (also referred to as the left–right organizer, LRO), where motile cilia generate a leftward directional flow (nodal flow) through their posteriorly tilted rotational motion. In turn, immotile cilia sense this flow and transmit asymmetric signals to the lateral plate mesoderm (LPM), leading to asymmetric gene expression (Hirokawa et al., 2006; Yoshiba et al., 2012). To date, causative genetic mutations identified in CHD/HTX patients often involve genes related to L-R asymmetric development (e.g., NODAL (Dardas et al., 2024), ZIC3 (Ware et al., 2004)) and ciliary assembly and function (e.g., DNAH11 (Liu et al., 2019), DNAH5 (Bolkier et al., 2022), DNAI1 (Kennedy et al., 2007)). Additional clinically significant genes have also been reported, including PKD1L1 (Vetrini et al., 2016), SHROOM3 (Tariq et al., 2011), MMP21 (Guimier et al., 2015), PNPLA4 (Gao et al., 2024). However, these mutations explain only a small fraction of CHD/HTX cases, leaving the genetic etiology of the majority of patients unresolved.
Structural variations (SVs) are genomic rearrangements of at least 50 bp in length, including deletions, duplications, insertions, translocations and copy number variations (CNVs) (Sudmant et al., 2015). SVs have long been recognized as major contributors to human diseases, particularly genetic disorders (Weischenfeldt et al., 2013). Numerous studies have demonstrated a substantial burden of CNVs in CHD/HTX. For example, Glessner JT et al. analyzed a cohort of 538 CHD trios and found that the frequency of de novo CNVs among patients with heterotaxy was as high as 21% (Glessner et al., 2014). Similarly, another study identified clinically relevant CNVs in approximately 20% of patients with CHD/HTX (Cowan et al., 2016). However, these studies primarily employed chromosomal microarray analysis (CMA), which has limitations in the detection of balanced SVs and resolution. Therefore, the true burden of SVs in CHD/HTX patients remains significantly underexplored.
Optical genome mapping (OGM) is a novel, high-resolution (>500 bp) and genome-wide technique that does not rely on DNA amplification. It enables the detection of all classes of SVs, including CNVs, balanced translocations and inversions in a single test. An increasing number of studies have confirmed that OGM shows high concordance with traditional detection techniques for detecting SVs, while also revealing additional clinically relevant SVs, thereby advancing the field of precision medicine. However, the clinical application of OGM in birth defects remains limited. In this study, genomic SVs in CHD/HTX samples were analyzed by OGM.
2 Materials and methods
2.1 Patient sample collection
A total of 12 peripheral blood samples were collected from patients with CHD/HTX and stored at −80 °C in accordance with the Helsinki Declaration. All participants were of Chinese origin. Optical genome mapping analysis was performed on all de-identified samples by two independent operators. Some cases had previously undergone WES (n = 2) and CMA (n = 1). This study was approved by the Ethics Committee of Children’s Hospital of Fudan University.
2.2 De novo assembly and structural variant calling and filtering
OGM was performed as previously described (Neveling et al., 2021). Briefly, ultra-high-molecular-weight (HMW) DNA was extracted from frozen peripheral blood using Bionano SP Blood & Cell Culture DNA Isolation Kit, and then HMW DNA was labelled at the specific sequence CTTAAG with the Direct Label and Stain (DLS) Kit according to the manufacturer’s protocol. The labelled HMW-DNA was loaded onto Bionano Genomics Saphyr Chip for electrophoretic linearization and imaging.
De novo assembly pipeline was executed using Bionano Solve (version 3.7) with the human reference genome GRCh38 as the reference. For SV calls filtering, the following criteria were applied: (1) recommended confidence with values: insertions and deletions >0, inversions >0.7, duplications = 1, intrachromosomal fusions >0.05, CNV > 0.99; (2) recommended sizes: insertions and deletions >500 bp, CNV > 500 Kbp, AOH/LOH >25,000 Kbp; (3) SVs occurring in ≤1% of Bionano control samples (n > 300). All data were visualized using Bionano Access (version 1.7 or version 1.7.2). To identify clinically relevant SVs, only those overlapping the coding regions of genes were selected. The remaining SVs were analyzed by AnnotSV and interpreted by OMIM (https://omim.org/), gnomAD (https://gnomad.broadinstitute.org/), DGV (http://dgv.tcag.ca/dgv/app/home) and DECIPHER (https://www.deciphergenomics.org/) databases.
2.3 Whole exome sequencing and chromosomal microarray analysis
Genomic DNA was extracted from peripheral blood samples using the QIAamp DNA Blood Mini Kit (Qiagen) following the manufacturer’s instructions. Whole exome sequencing (WES) was performed on an Illumina HiSeq X Ten platform. Detailed methodologies for exome library preparation, sequencing and variant calling were performed as previously described (Wang et al., 2025). We screened for known pathogenic variants or rare deleterious coding variants (MAF < 0.0001 in gnomAD_exome_EAS and CADD score >20). Additionally, patient 2247 underwent chromosomal microarray analysis (CMA) following previously published protocols (Gao et al., 2024).
2.4 Literature review
A literature review was conducted through PubMed search using the keywords “Optical Genome Mapping OR OGM” and “Structural variation OR Structural variant OR SV”. Only studies focusing on the clinical application of OGM in human samples and comparing OGM with standard cytogenetic techniques were systematically reviewed. Detailed information is summarized in Table 1.
3 Results
3.1 Patient characteristics
Our study enrolled 12 patients with complex CHD and heterotaxy, including 6 females and 6 males. Levocardia was observed in 58% (7/12), dextrocardia in 42% (5/12). The mean age at diagnosis was 3.3 years (range 0–9.3 years), and all complex cardiac defects were diagnosed by echocardiogram. Patient 2962 died of respiratory failure at the age of 4 months and 8 days. In addition to cardiovascular malformations, four patients presented with other structural anomalies, such as asplenia and polydactyly. Case 2247 underwent CMA, which did not identify any pathogenic, likely pathogenic CNVs or variants of uncertain significance (VUS). WES was also performed for this patient, but the result was inconclusive; therefore, no further analysis was conducted. Case 2582 also underwent WES, which did not reveal any clinically relevant variations. Detailed clinical characteristics of all patients are summarized in Table 1.
3.2 Raw data quality and SVs detected by OGM
Bionano optical genome imaging generated an average of 570.9 Gb of raw data per sample. The 12 samples achieved an average effective coverage of 124.74X (range: 92.58-232.21X) and a map rate of 89.31% (±3.05%). The label density ranged from 14.45–16.56 per 100 kb, and the range of N50 molecular length (≥150 kb) was 260.63–367.39 kb. Thus, all samples passed the quality control (QC) metrics. Detailed QC parameters for each sample are listed in Supplementary Table S1.
In total, 77758 SVs were detected in 12 samples (Figure 1). After filtering out low-confidence and common SVs, 825 SVs (1.1%) remained, with an average of 68.8 SVs per sample (including 39.2 deletions, 24.4 insertions, 1.3 inversions and 3.8 duplications). SVs were detected in all chromosomes, with the highest SV burden observed on chromosomes 1 (Supplementary Figure S1). The majority of SVs did not overlap any coding gene, and only 26.3% of SVs overlapped one or more exons of protein coding gene(s), potentially affecting coding sequences (Figures 1, 2). Among all SV types, deletions were the most frequent (median = 39, range: 3–44), followed by insertions (median = 24, range: 2–20) (Figure 2B). Most deletions and insertions were less than 50 kb (Figure 2C), which is consistent with recent findings from OGM-based SV detection in cancer samples (Wagener et al., 2024).

Figure 2. Distribution of high confidence SVs in 12 patients with complex CHD and HTX (A) Summary of proportion of SVs located in intergenic regions, RNA genes or pseudogenes, exons and introns. (B) The distribution of detected SVs (deletions, insertions, inversions, duplications). (C) The scatter plot illustrates the length distribution of the identified SVs. Each dot represents one SV. The dashed line marks the 50 kb threshold. The red vertical lines represent the median values. (D) The distribution of 123 rare SVs on chromosomes. Colored boxes on the right side of the chromosome represent the SV types, including deletion, insertion, duplication, inversion and duplication_inverted respectively.
3.3 Detection of SVs encompassing clinically relevant genes in CHD/HTX patients by OGM
Among all high confidence SVs, we identified 216 SVs involving coding regions of genes in 12 patients. To further filter out common SVs, we removed SVs that appear more than twice in DGV (overlapping more than 50%) and frequency >0.1% in gnomAD, leaving only 123 rare SVs for further clinical significance assessment. The chromosomal distribution of these rare SVs is shown in Figure 2D. Among them, seven SVs of interest were identified (Supplementary Table S2): one with previously established clinical significance, three involving known CHD/HTX susceptibility genes, and three affecting novel candidate genes.
3.3.1 Known pathogenic SVs and SVs harboring known CHD/HTX susceptibility genes
A 1.85 Mb heterozygous deletion in 2q13 region was identified in patient 1809 (Figure 3). The deletion encompasses 11 protein-coding genes, including RGPD6, BUB1, ACOXL, BCL2L11, ANAPC1, MERTK, TMEM87B, FBLN7, ZC3H8, ZC3H6 and RGPD8. The cardiovascular phenotype associated with 2q13 deletion syndrome has been reported as highly variable (Digilio et al., 2022). In our study, the proband 1809 presented with L-transposition of the great arteries (L-TGA), a condition not previously reported in 2q13 deletion cases. According to ACMG guidelines, this variant was classified as pathogenic.

Figure 3. Identification of a chromosome 2q deletion in sample 1809 by OGM (A) Left panel shows a circos plot illustrating SVs in the sample and the blue box on chromosome 2 highlights the pathogenic deletion. Right panel representing the genome browser view provides the detail of the structural variation. The sample’s map (blue bar) alignment to the reference map of chromosomes 2 reveals a large ∼1.85 Mbp deletion (light red) and mapping genes in GRCh38/hg38. (B) Copy number profile of chromosomes 2 indicates a loss in chromosome 2q.
In addition to the above pathogenic SVs, we identified three SVs encompassing three known syndromic CHD-associated genes (Figures 4A–C): NOTCH2 (#MIM 610205), KDM6A (#MIM 300867), and CBL (#MIM 613563). These included a 3.3 kb deletion of 1p12 region overlapping exon3 and exon4 of the NOTCH2 gene in patient 2247, who had previously undergone CMA but no clinical CNVs were found; a deletion of Xp11.3 region potentially disrupting exon4 of KDM6A gene in case 3861; and a 6.6 kb heterozygous deletion of 11q23.3 in case 3617, partially deleting the CBL gene. Both patients 3861 and 3617 presented with syndromic CHD.

Figure 4. Genome browser view of three SVs overlapping CHD/HTX susceptibility genes: (A) NOTCH2. (B) KDM6A. (C) CBL. The green bar represents the reference map, while patient maps are shown in blue. Deletions are highlighted in light red, and insertions are marked in light blue.
3.3.2 OGM unveiled rare SVs involving candidate susceptibility genes
Through a comprehensive analysis of the remaining rare SVs, we identified three SVs of interest that potentially overlap novel candidate genes of CHD/HTX in three patients, including CEP164 and SMARCA2. Patient 2247 carried a unique 1.4 kb deletion, ogm [GRCh38] 11q23.3 (117312178_117342581)x1 (Figure 5A). This deletion partially affects the 5′UTR and exon 1-3 of CEP164 gene and is predicted to result in loss of function. In two unrelated patients 2765 and 4066, we found 1035 bp and 2049 bp insertions respectively in 9p24.3 (Figure 5B), which may disrupt SMARCA2 function. Both patients presented with complex CHD, including DORV, pulmonary stenosis, ASD, single atrium and single ventricle.

Figure 5. Genome browser view of SVs overlapping potential CHD/HTX candidate genes (CEP164 and SMARCA2) (A) A 1.4 kb deletion of CEP164 on 11q13.3. (B) Heterozygous insertions in the SMARCA2 gene in two patients (case 2765 and 4066).
The expression patterns of the two candidate genes in the developing human heart were analyzed by publicly available single cell RNA-seq data (Speir et al., 2021). As shown in Supplementary Figure S2A–C, both CEP164 and SMARCA2 are widely expressed in the human embryonic heart, with SMARCA2 exhibiting particularly high expression levels. Although their expression is relatively low in cardiomyocytes, they exhibit higher expression levels in non-cardiomyocyte cells, such as fibroblasts and smooth muscle cells. Consistent with these observations, in situ hybridization data obtained from the GenePaint database (https://www.genepaint.org) revealed similar expression patterns in E14.5 mouse embryos, with both Cep164 and Smarca2 being expressed in the developing heart and surrounding tissues (Supplementary Figure S2D,E). In addition, a previous study employing wholemount β-galactosidase (LacZ) staining demonstrated broad Cep164 expression during early murine embryogenesis (E9.5, E10.5, and E12.5), including the central ventricle, bulbus cordis, and outflow tract of the developing heart (Devlin et al., 2020). Taken together, these findings provide converging evidence that CEP164 and SMARCA2 may represent plausible contributors to CHD/HTX pathogenesis and warrant further functional investigation.
4 Discussion
SVs play a critical role in a variety of diseases, including CHD/HTX. Current methods for detecting SVs mainly include karyotype (KT), FISH and CMA. However, each technique has its own limitations. KT requires cell culture and has a low resolution of approximately 5–10 Mb. FISH is a targeted approach limited to the detection of known variations. CMA is unable to detect balanced chromosomal aberrations (e.g., inversions, translocations) and determine the precise location/orientation of insertions. Given these limitations, the true burden of SVs may be significantly underestimated in CHD/HTX, highlighting the need for higher-resolution genome-wide approaches to elucidate its genetic architecture.
OGM represents a genome-wide, high-resolution platform for SV detection that bridges the gap between cytogenetic and sequencing approaches. Recent studies have evaluated the performance of OGM across diverse clinical settings, including hematologic malignancies, solid tumors, prenatal diagnosis, reproductive disorders, and neurodevelopmental diseases (Xiao et al., 2024; Schrauwen et al., 2024; Cheng et al., 2024; Shim et al., 2022; Dai et al., 2022; Loghavi et al., 2024). These studies have consistently demonstrated high concordance (frequently approaching 100%) with conventional cytogenetic methods, while revealing additional clinically relevant SVs that were undetectable by CMA or short-read sequencing (Supplementary Table S3). Although these findings firmly establish OGM as a next-generation cytogenomic tool, its utility in congenital heart disease, particularly in CHD/HTX, remains largely unexplored.
Building upon previous validations of OGM, we applied this technology to investigate the cryptic SV burden in CHD/HTX. In this study, most SVs identified by OGM were less than 50 kb in size, which were frequently elusive to conventional cytogenetic methods. The smaller size of these SVs facilitates the prioritization of potential candidate genes. Additionally, most SVs were located in non-coding regions, requiring integrative analyses with complementary approaches to assess their clinical relevance. OGM revealed a total of 7 SVs potentially associated with the patients’ phenotypes, including one microdeletion of known pathogenicity, three overlapping known CHD susceptibility genes, and three overlapping candidate susceptibility genes. Among them, the SVs involving CEP164 and SMARCA2 are currently lacking established clinical significance, but these findings may provide valuable information for future research.
The recurrent 2q13 deletion syndrome is associated with developmental delay and multiple deformities, including cranial dysmorphism, CHD and urogenital malformations (Yu et al., 2012; Riley et al., 2015; Wolfe et al., 2018). CHD has been reported in approximately 30%–60% of affected individuals, including diverse manifestations such as heterotaxy, tetralogy of Fallot (TOF), and septal defects (Digilio et al., 2022). Zebrafish models have implicated FBLN7 and TMEM87B as candidate genes for cardiac defects and craniofacial abnormalities (Russell et al., 2014). However, the specific molecular mechanisms underlying their roles in cardiogenesis remain unclear. Notably, a potentially deleterious TMEM87B variant was identified in a patient with a hemizygous 2q13 microdeletion, suggesting a recessive condition characterized by CHD and restrictive cardiomyopathy (Yu et al., 2016). In our cohort, a patient carrying a 2q13 microdeletion was diagnosed with isolated CHD-L/TGA. This finding is consistent with a previous study describing a patient with 2q13 deletion syndrome who also exhibited CHD and heterotaxy, further supporting a role for this region in left-right patterning (Rudd et al., 2009).
Several studies have demonstrated that OGM can achieve molecular diagnosis in cases unresolved by conventional cytogenetic techniques and short-read sequencing. In this study, we applied OGM to investigate SVs in two unexplained CHD/HTX cases. Case 2247 had previously undergone CMA, which did not reveal any clinically relevant SVs. However, OGM identified two SVs in this patient: a likely pathogenic 3.3 kb deletion in the 1p12 region overlapping the CHD-associated gene NOTCH2, and a 1.4 kb heterozygous deletion of uncertain significance affecting part of the 5′UTR and exons 1-3 of CEP164, which encodes a protein required for primary cilia assembly. Consistent with previous functional studies, zebrafish experiments have shown that CEP164 deficiency results in ciliopathy phenotypes, including abnormal heart looping (Chaki et al., 2012). Additional parental genotyping and RNA-seq analyses are necessary to clarify the pathogenic role of these SVs. In another WES-negative patient (ID 2582), 16 rare SVs were identified; however, none were classified as pathogenic or likely pathogenic, suggesting that SVs may not represent the primary causative factor in this case.
In addition, two insertions within the SMARCA2 gene at 9p24.3 were identified in two unrelated patients and were absent in the OGM control database. SMARCA2 encodes a subunit of the ATP-dependent chromatin remodeling complex SWI/SNF, which regulates chromatin structure and transcription and plays a crucial role in cardiac development. Mutations in SMARCA2 were reported in developmental syndromes that involved CHD, including Nicolaides–Baraitser syndrome (#MIM 601358) and blepharophimosis intellectual disability syndrome (Cappuccio et al., 2020). Moreover, the 9p24.2 locus (rs7863990, close to SMARCA2) has been identified as CHD risk loci in Chinese populations (Lin et al., 2015). Homozygous ablation of Smarca2 in mouse embryonic stem cells resulted in impaired cardiac differentiation, and instead, cells acquired a neuronal identity (Hota et al., 2022). To our knowledge, this is the first report of SVs involving SMARCA2 in CHD/HTX patients, providing new insights into its role in cardiac development.
5 Limitation
Although OGM is a comprehensive technique for detecting SVs, it has some limitations. OGM relies on fluorescent labels at specific sequences rather than DNA sequencing, making it unable to detect single nucleotide variants or poorly labeled regions, such as centric fusions, centromeres and telomeres. Moreover, a reliable control database for interpreting SVs, especially those <50 kb in size, is currently lacking, which poses a challenge for interpreting novel or rare SVs.
This study also has some limitations. First, the sample size was relatively small, and further larger cohorts are needed to clarify the correlation between candidate SVs and CHD/HTX. Second, due to insufficient blood samples from probands’ parents, we were unable to determine the inheritance pattern of the identified SVs (inherited or de novo). Moreover, because only a few patients had undergone CMA or WES prior to OGM analysis, systematic comparison across methods was not feasible. Once additional samples become available, future studies will aim to validate the identified SVs and clarify their pathogenic relevance. Third, we did not validate the SVs by another assay such as CMA or long-read sequencing techniques. Nevertheless, the clinical utility of OGM has been well established, and it may serve as a first-tier test, replacing traditional cytogenetic tools in both prenatal and postnatal settings (Valkama et al., 2023; Sahajpal et al., 2023; Iqbal et al., 2023). Although long-read sequencing was not employed in our study, a previous study combining OGM and long-read sequencing technologies for pathogenic SVs detection in Parkinson’s disease-related iPSC has shown that triplication, duplication and large deletion were missed by long-read sequencing technologies (Trinh et al., 2024).
6 Conclusion
To our knowledge, this is the first study to evaluate the burden of SVs using OGM in patients with CHD/HTX. OGM detected additional SVs not captured by CMA or WES, thereby expanding the spectrum of detectable genomic alterations and providing preliminary evidence for candidate loci that may contribute to CHD/HTX. These results enhance our understanding of the genetic architecture of CHD/HTX and highlight OGM as a powerful and promising tool in rare disease genomics.
Data availability statement
The datasets presented in this article are not publicly available due to privacy and ethical restrictions involving human participants. Processed data supporting the conclusions of this study are included in the article and Supplementary Material. Requests for access to additional data can be directed to the corresponding author and will be considered in accordance with institutional ethical guidelines.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Children’s Hospital of Fudan University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
SM: Conceptualization, Data curation, Writing – review and editing, Writing – original draft, Formal Analysis. JS: Formal Analysis, Data curation, Writing – review and editing, Investigation. WC: Writing – review and editing, Formal Analysis, Data curation. ZF: Writing – review and editing, Formal Analysis, Data curation. QZ: Data curation, Writing – review and editing, Formal Analysis. YG: Data curation, Formal Analysis, Writing – review and editing. SiL: Writing – review and editing, Formal Analysis, Data curation. SS: Formal Analysis, Data curation, Writing – review and editing. YL: Formal Analysis, Data curation, Writing – review and editing. ShL: Data curation, Formal Analysis, Writing – review and editing. XT: Methodology, Writing – review and editing, Funding acquisition, Data curation. GH: Methodology, Data curation, Funding acquisition, Writing – review and editing. WS: Supervision, Writing – review and editing, Funding acquisition, Methodology, Conceptualization. XH: Supervision, Methodology, Writing – review and editing, Conceptualization, Funding acquisition.
Funding
The authors declare that financial support was received for the research and/or publication of this article. This work was supported by the National Key Research and Development Program of China (Nos. 2021YFC2701000, 2023YFC2705704), National Natural Science Foundation of China (Nos. 82270312, 82200264, 82370309), Science and Technology Projects of Xizang Autonomous Region, China (No.XZ202401ZY0042), Major Special Project of Xiamen Health High Quality Development Science and Technology Plan (No.2024GZL-ZD06), Xiamen Natural Science Foundation Project (No.3502Z202373137), Fujian Provincial Health and Health Technology Program (No.2024GGB26), Anhui Provincial Health Commission Key Project (AHWJ2022a04) and the CAMS Innovation Fund for Medical Sciences (No. 2019-I2M-5-002).
Acknowledgements
We sincerely thank all patients and their families for participation in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgene.2025.1673539/full#supplementary-material
References
Bolkier, Y., Barel, O., Marek-Yagel, D., Atias-Varon, D., Kagan, M., Vardi, A., et al. (2022). Whole-exome sequencing reveals a monogenic cause in 56% of individuals with laterality disorders and associated congenital heart defects. J. Med. Genet. 59 (7), 691–696. doi:10.1136/jmedgenet-2021-107775
Cappuccio, G., Sayou, C., Tanno, P. L., Tisserant, E., Bruel, A.-L., Kennani, S. E., et al. (2020). De novo SMARCA2 variants clustered outside the helicase domain cause a new recognizable syndrome with intellectual disability and blepharophimosis distinct from Nicolaides-Baraitser syndrome. Genet. Med. 22 (11), 1838–1850. doi:10.1038/s41436-020-0898-y
Chaki, M., Airik, R., Ghosh, A. K., Giles, R. H., Chen, R., Slaats, G. G., et al. (2012). Exome capture reveals ZNF423 and CEP164 mutations, linking renal ciliopathies to DNA damage response signaling. Cell 150 (3), 533–548. doi:10.1016/j.cell.2012.06.028
Cheng, Y., Dong, L., Bu, D., Han, L., Zhao, Y., Liu, J., et al. (2024). Optical genome mapping reveals the landscape of structural variations and their clinical significance in HBOC-related breast cancer. Front. Biosci. 29 (1), 2. doi:10.31083/j.fbl2901002
Cowan, J. R., Tariq, M., Shaw, C., Rao, M., Belmont, J. W., Lalani, S. R., et al. (2016). Copy number variation as a genetic basis for heterotaxy and heterotaxy-spectrum congenital heart defects. Philos. Trans. R. Soc. Lond. B. Biol. Sci. 371 (1710), 20150406. doi:10.1098/rstb.2015.0406
Dai, P., Zhu, X., Pei, Y., Chen, P., Li, J., Gao, Z., et al. (2022). Evaluation of optical genome mapping for detecting chromosomal translocation in clinical cytogenetics. Mol. Genet. Genomic Med. 10 (6), e1936. doi:10.1002/mgg3.1936
Dardas, Z., Fatih, J. M., Jolly, A., Dawood, M., Du, H., Grochowski, C. M., et al. (2024). NODAL variants are associated with a continuum of laterality defects from simple D-transposition of the great arteries to heterotaxy. Genome Med. 16 (1), 53. doi:10.1186/s13073-024-01312-9
Devlin, L. A., Ramsbottom, S. A., Overman, L. M., Lisgo, S. N., Clowry, G., Molinari, E., et al. (2020). Embryonic and foetal expression patterns of the ciliopathy gene CEP164. PloS One 15 (1), e0221914. doi:10.1371/journal.pone.0221914
Digilio, M. C., Dentici, M. L., Loddo, S., Laino, L., Calcagni, G., Genovese, S., et al. (2022). Congenital heart defects in the recurrent 2q13 deletion syndrome. Eur. J. Med. Genet. 65 (1), 104381. doi:10.1016/j.ejmg.2021.104381
Gao, H., Huang, X., Chen, W., Feng, Z., Zhao, Z., Li, P., et al. (2024). Association of copy number variation in X chromosome-linked PNPLA4 with heterotaxy and congenital heart disease. Chin. Med. J. 137 (15), 1823–1834. doi:10.1097/CM9.0000000000003192
Glessner, J. T., Bick, A. G., Ito, K., Homsy, J., Rodriguez-Murillo, L., Fromer, M., et al. (2014). Increased frequency of de novo copy number variants in congenital heart disease by integrative analysis of single nucleotide polymorphism array and exome sequence data. Circulation Res. 115 (10), 884–896. doi:10.1161/CIRCRESAHA.115.304458
Guimier, A., Gabriel, G. C., Bajolle, F., Tsang, M., Liu, H., Noll, A., et al. (2015). MMP21 is mutated in human heterotaxy and is required for normal left-right asymmetry in vertebrates. Nat. Genet. 47 (11), 1260–1263. doi:10.1038/ng.3376
Hirokawa, N., Tanaka, Y., Okada, Y., and Takeda, S. (2006). Nodal flow and the generation of left-right asymmetry. Cell 125 (1), 33–45. doi:10.1016/j.cell.2006.03.002
Hota, S. K., Rao, K. S., Blair, A. P., Khalilimeybodi, A., Hu, K. M., Thomas, R., et al. (2022). Brahma safeguards canalization of cardiac mesoderm differentiation. Nature 602 (7895), 129–134. doi:10.1038/s41586-021-04336-y
Huang, X., Gao, Y., Chen, W., Sheng, W., and Huang, G. (2023). Noncardiac anomalies in children with congenital heart disease. Front. Cardiovasc. Med. 10, 1293210. doi:10.3389/fcvm.2023.1293210
Iqbal, M. A., Broeckel, U., Levy, B., Skinner, S., Sahajpal, N. S., Rodriguez, V., et al. (2023). Multisite assessment of optical genome mapping for analysis of structural variants in constitutional postnatal cases. J. Mol. Diagn. 25 (3), 175–188. doi:10.1016/j.jmoldx.2022.12.005
Kennedy, M. P., Omran, H., Leigh, M. W., Dell, S., Morgan, L., Molina, P. L., et al. (2007). Congenital heart disease and other heterotaxic defects in a large cohort of patients with primary ciliary dyskinesia. Circulation 115 (22), 2814–2821. doi:10.1161/CIRCULATIONAHA.106.649038
Lin, A. E., Krikov, S., Riehle-Colarusso, T., Frías, J. L., Belmont, J., Anderka, M., et al. (2014). Laterality defects in the national birth defects prevention study (1998-2007): birth prevalence and descriptive epidemiology. Am. J. Med. Genet. Part A 164A (10), 2581–2591. doi:10.1002/ajmg.a.36695
Lin, Y., Guo, X., Zhao, B., Liu, J., Da, M., Wen, Y., et al. (2015). Association analysis identifies new risk loci for congenital heart disease in Chinese populations. Nat. Commun. 6, 8082. doi:10.1038/ncomms9082
Liu, S., Chen, W., Zhan, Y., Li, S., Ma, X., Ma, D., et al. (2019). DNAH11 variants and its association with congenital heart disease and heterotaxy syndrome. Sci. Rep. 9 (1), 6683. doi:10.1038/s41598-019-43109-6
Loghavi, S., Wei, Q., Ravandi, F., Quesada, A. E., Routbort, M. J., Hu, S., et al. (2024). Optical genome mapping improves the accuracy of classification, risk stratification, and personalized treatment strategies for patients with acute myeloid leukemia. Am. J. Hematol. 99 (10), 1959–1968. doi:10.1002/ajh.27435
Neveling, K., Mantere, T., Vermeulen, S., Oorsprong, M., van Beek, R., Kater-Baats, E., et al. (2021). Next-generation cytogenetics: comprehensive assessment of 52 hematological malignancy genomes by optical genome mapping. Am. J. Hum. Genet. 108 (8), 1423–1435. doi:10.1016/j.ajhg.2021.06.001
Riley, K. N., Catalano, L. M., Bernat, J. A., Adams, S. D., Martin, D. M., Lalani, S. R., et al. (2015). Recurrent deletions and duplications of chromosome 2q11.2 and 2q13 are associated with variable outcomes. Am. J. Med. Genet. Part A 167A (11), 2664–2673. doi:10.1002/ajmg.a.37269
Rudd, M. K., Keene, J., Bunke, B., Kaminsky, E. B., Adam, M. P., Mulle, J. G., et al. (2009). Segmental duplications mediate novel, clinically relevant chromosome rearrangements. Hum. Mol. Genet. 18 (16), 2957–2962. doi:10.1093/hmg/ddp233
Russell, M. W., Raeker, M. O., Geisler, S. B., Thomas, P. E., Simmons, T. A., Bernat, J. A., et al. (2014). Functional analysis of candidate genes in 2q13 deletion syndrome implicates FBLN7 and TMEM87B deficiency in congenital heart defects and FBLN7 in craniofacial malformations. Hum. Mol. Genet. 23 (16), 4272–4284. doi:10.1093/hmg/ddu144
Sahajpal, N. S., Mondal, A. K., Fee, T., Hilton, B., Layman, L., Hastie, A. R., et al. (2023). Clinical validation and diagnostic utility of optical genome mapping in prenatal diagnostic testing. J. Mol. Diagn. 25 (4), 234–246. doi:10.1016/j.jmoldx.2023.01.006
Schrauwen, I., Rajendran, Y., Acharya, A., Öhman, S., Arvio, M., Paetau, R., et al. (2024). Optical genome mapping unveils hidden structural variants in neurodevelopmental disorders. Sci. Rep. 14 (1), 11239. doi:10.1038/s41598-024-62009-y
Shim, Y., Lee, J., Seo, J., Park, C. K., Shin, S., Han, H., et al. (2022). Optical genome mapping identifies clinically relevant genomic rearrangements in prostate cancer biopsy sample. Cancer Cell Int. 22 (1), 306. doi:10.1186/s12935-022-02728-2
Speir, M. L., Bhaduri, A., Markov, N. S., Moreno, P., Nowakowski, T. J., Papatheodorou, I., et al. (2021). UCSC cell browser: visualize your single-cell data. Bioinformatics 37 (23), 4578–4580. doi:10.1093/bioinformatics/btab503
Sudmant, P. H., Rausch, T., Gardner, E. J., Handsaker, R. E., Abyzov, A., Huddleston, J., et al. (2015). An integrated map of structural variation in 2,504 human genomes. Nature 526 (7571), 75–81. doi:10.1038/nature15394
Tariq, M., Belmont, J. W., Lalani, S., Smolarek, T., and Ware, S. M. (2011). SHROOM3 is a novel candidate for heterotaxy identified by whole exome sequencing. Genome Biol. 12 (9), R91. doi:10.1186/gb-2011-12-9-r91
Trinh, J., Schaake, S., Gabbert, C., Lüth, T., Cowley, S. A., Fienemann, A., et al. (2024). Optical genome mapping of structural variants in Parkinson's disease-related induced pluripotent stem cells. BMC Genomics 25 (1), 980. doi:10.1186/s12864-024-10902-1
Valkama, A., Vorimo, S., Kumpula, T. A., Räsänen, H., Savolainen, E.-R., Pylkäs, K., et al. (2023). Optical genome mapping as an alternative to FISH-based cytogenetic assessment in chronic lymphocytic leukemia. Cancers 15 (4), 1294. doi:10.3390/cancers15041294
Vetrini, F., D'Alessandro, L. C. A., Akdemir, Z. C., Braxton, A., Azamian, M. S., Eldomery, M. K., et al. (2016). Bi-allelic mutations in PKD1L1 are associated with laterality defects in humans. Am. J. Hum. Genet. 99 (4), 886–893. doi:10.1016/j.ajhg.2016.07.011
Wagener, R., Brandes, D., Jung, M., Huetzen, M. A., Bergmann, A. K., Panier, S., et al. (2024). Optical genome mapping identifies structural variants in potentially new cancer predisposition candidate genes in pediatric cancer patients. Int. J. Cancer 154 (4), 607–614. doi:10.1002/ijc.34721
Wang, J., Chen, W., Huang, X., Gao, H., Feng, Z., Tan, C., et al. (2025). Identification of candidate genes harboring pathogenic variants in congenital heart disease and laterality defects in Chinese population. Front. Genet. 16, 1582718. doi:10.3389/fgene.2025.1582718
Ware, S. M., Peng, J., Zhu, L., Fernbach, S., Colicos, S., Casey, B., et al. (2004). Identification and functional analysis of ZIC3 mutations in heterotaxy and related congenital heart defects. Am. J. Hum. Genet. 74 (1), 93–105. doi:10.1086/380998
Weischenfeldt, J., Symmons, O., Spitz, F., and Korbel, J. O. (2013). Phenotypic impact of genomic structural variation: insights from and for human disease. Nat. Rev. Genet. 14 (2), 125–138. doi:10.1038/nrg3373
Wolfe, K., McQuillin, A., Alesi, V., Boudry Labis, E., Cutajar, P., Dallapiccola, B., et al. (2018). Delineating the psychiatric and behavioral phenotype of recurrent 2q13 deletions and duplications. Am. J. Med. Genet. B. Neuropsychiatr. Genet. 177 (4), 397–405. doi:10.1002/ajmg.b.32627
Xiao, B., Luo, X., Liu, Y., Ye, H., Liu, H., Fan, Y., et al. (2024). Combining optical genome mapping and RNA-seq for structural variants detection and interpretation in unsolved neurodevelopmental disorders. Genome Med. 16 (1), 113. doi:10.1186/s13073-024-01382-9
Yoshiba, S., Shiratori, H., Kuo, I. Y., Kawasumi, A., Shinohara, K., Nonaka, S., et al. (2012). Cilia at the node of mouse embryos sense fluid flow for left-right determination via Pkd2. Science 338 (6104), 226–231. doi:10.1126/science.1222538
Yu, H. E., Hawash, K., Picker, J., Stoler, J., Urion, D., Wu, B. L., et al. (2012). A recurrent 1.71 Mb genomic imbalance at 2q13 increases the risk of developmental delay and dysmorphism. Clin. Genet. 81 (3), 257–264. doi:10.1111/j.1399-0004.2011.01637.x
Yu, H.-C., Coughlin, C. R., Geiger, E. A., Salvador, B. J., Elias, E. R., Cavanaugh, J. L., et al. (2016). Discovery of a potentially deleterious variant in TMEM87B in a patient with a hemizygous 2q13 microdeletion suggests a recessive condition characterized by congenital heart disease and restrictive cardiomyopathy. Cold Spring Harb. Mol. Case Stud. 2 (3), a000844. doi:10.1101/mcs.a000844
Keywords: congenital heart disease, heterotaxy, optical genome mapping, structural variations, candidate genes
Citation: Min S, Sun J, Chen W, Feng Z, Zhuang Q, Gao Y, Lin S, Sun S, Lu Y, Li S, Tian X, Huang G, Sheng W and Huang X (2025) Optical genome mapping uncovers clinically relevant structural variants in congenital heart disease with heterotaxy. Front. Genet. 16:1673539. doi: 10.3389/fgene.2025.1673539
Received: 26 July 2025; Accepted: 20 November 2025;
Published: 05 December 2025.
Edited by:
Emanuele Bobbio, Sahlgrenska University Hospital, SwedenReviewed by:
Thomas Brand, Imperial College London, United KingdomAli Rashidi Nezhad, Tehran University of Medical Sciences, Iran
Copyright © 2025 Min, Sun, Chen, Feng, Zhuang, Gao, Lin, Sun, Lu, Li, Tian, Huang, Sheng and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Sheng, c2hlbmdfd2VpQGZ1ZGFuLmVkdS5jbg==; Xianghui Huang, eG1oeGgyMDEzQDE2My5jb20=
†These authors have contributed equally to this work and shared first authorship
 Shaojie Min
Shaojie Min Jingwei Sun
Jingwei Sun Weicheng Chen
Weicheng Chen Zhiyu Feng1
Zhiyu Feng1 Guoying Huang
Guoying Huang Wei Sheng
Wei Sheng Xianghui Huang
Xianghui Huang