- Department of Reproductive Health, School of Public Health, College of Medicine and Health Science, Bahir Dar University, Bahir Dar, Ethiopia
Background: In Africa, over one-third of women experience multiple abortions, often due to inadequate access to effective modern contraceptives. This highlights a critical gap in understanding the patterns and predictors of post-abortion contraceptive (PAC) use. To address this issue, a systematic review and meta-analysis were conducted to assess the uptake of PAC and associated factors among African women who received abortion services.
Methods: Following the PRISMA guideline, all articles published between January 1, 2015, and December 30, 2023, were systematically retrieved from multiple databases. Articles reporting PAC uptake among African women were included. The pooled prevalence of Post-abortion contraceptive uptake was determined using a random effects model. The variation between the included studies was assessed using a funnel plot and I2 heterogeneity statistics. Sources of heterogeneity: Subgroup analysis was performed by country, publication period, study design, and sub-African region.
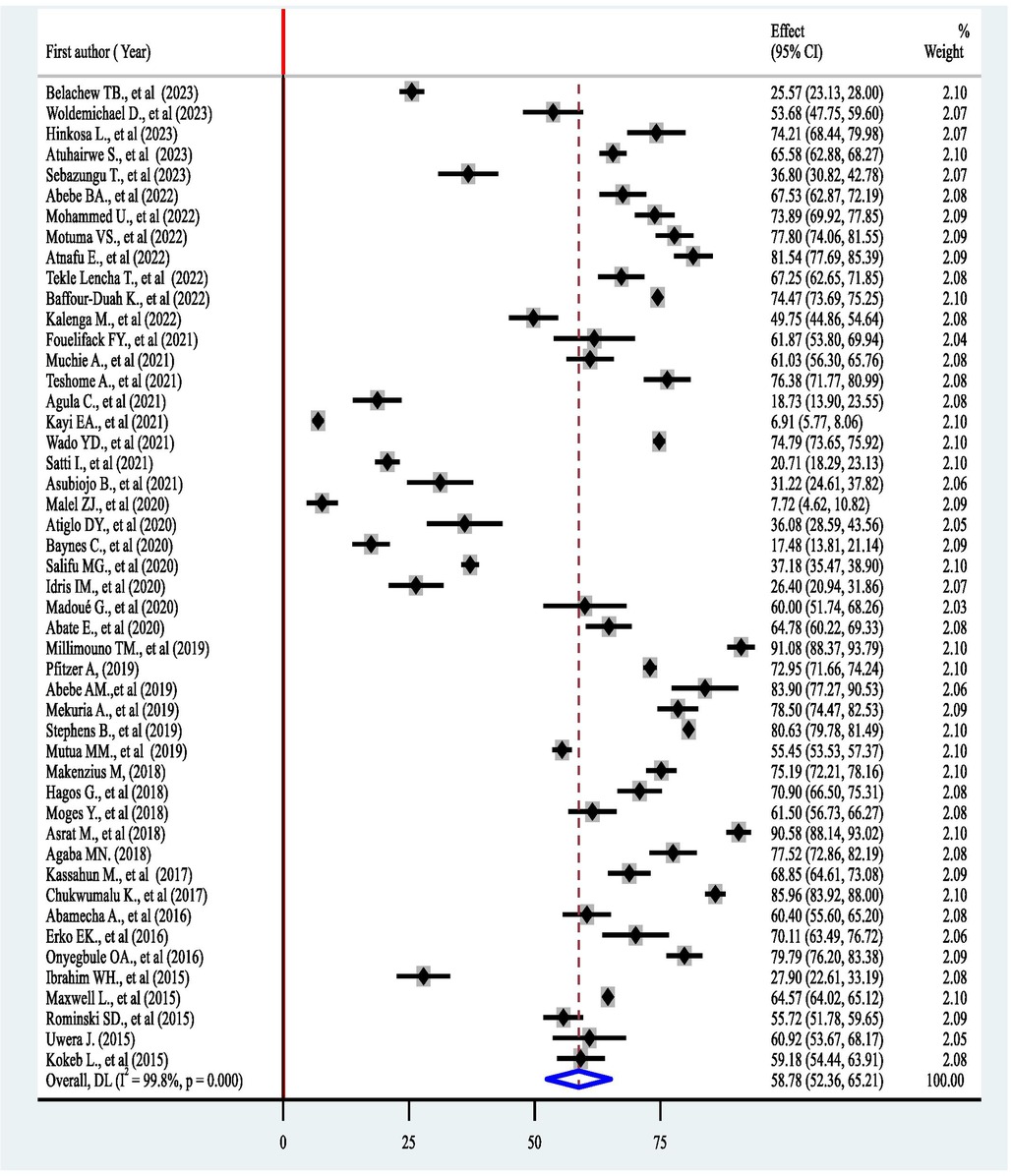
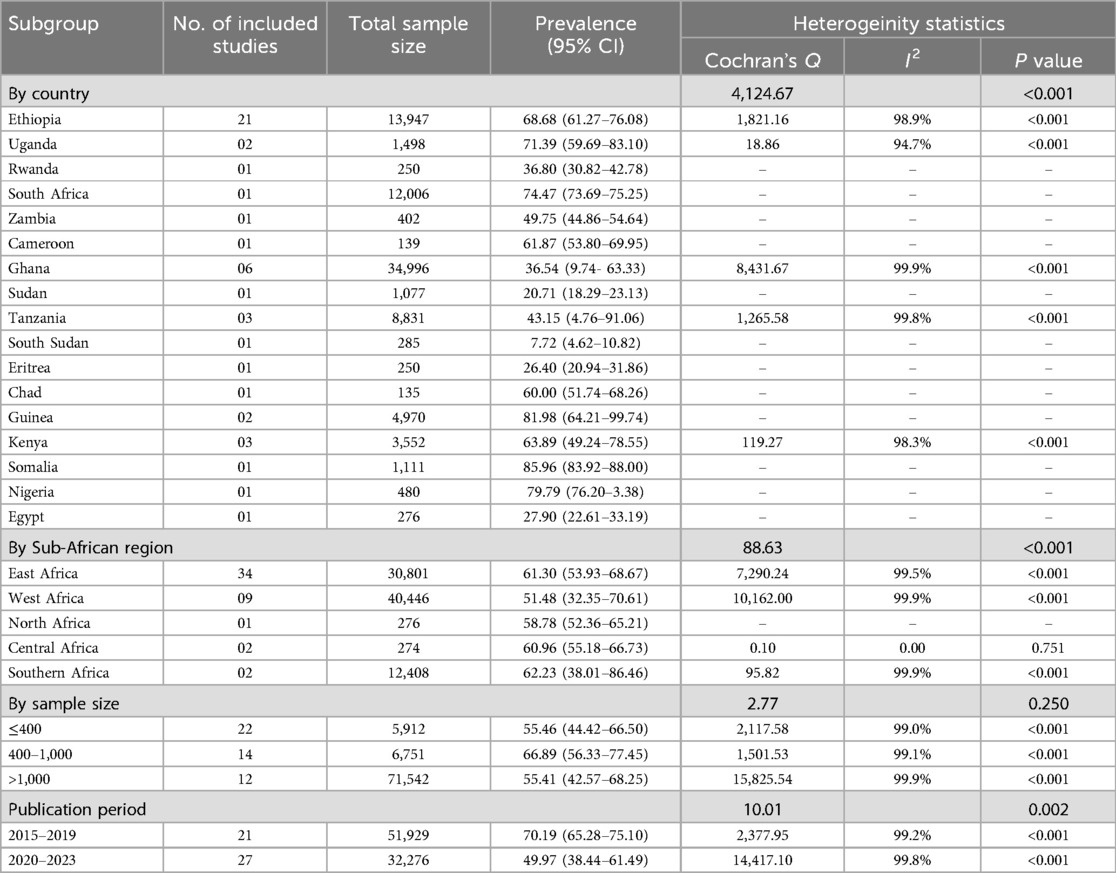
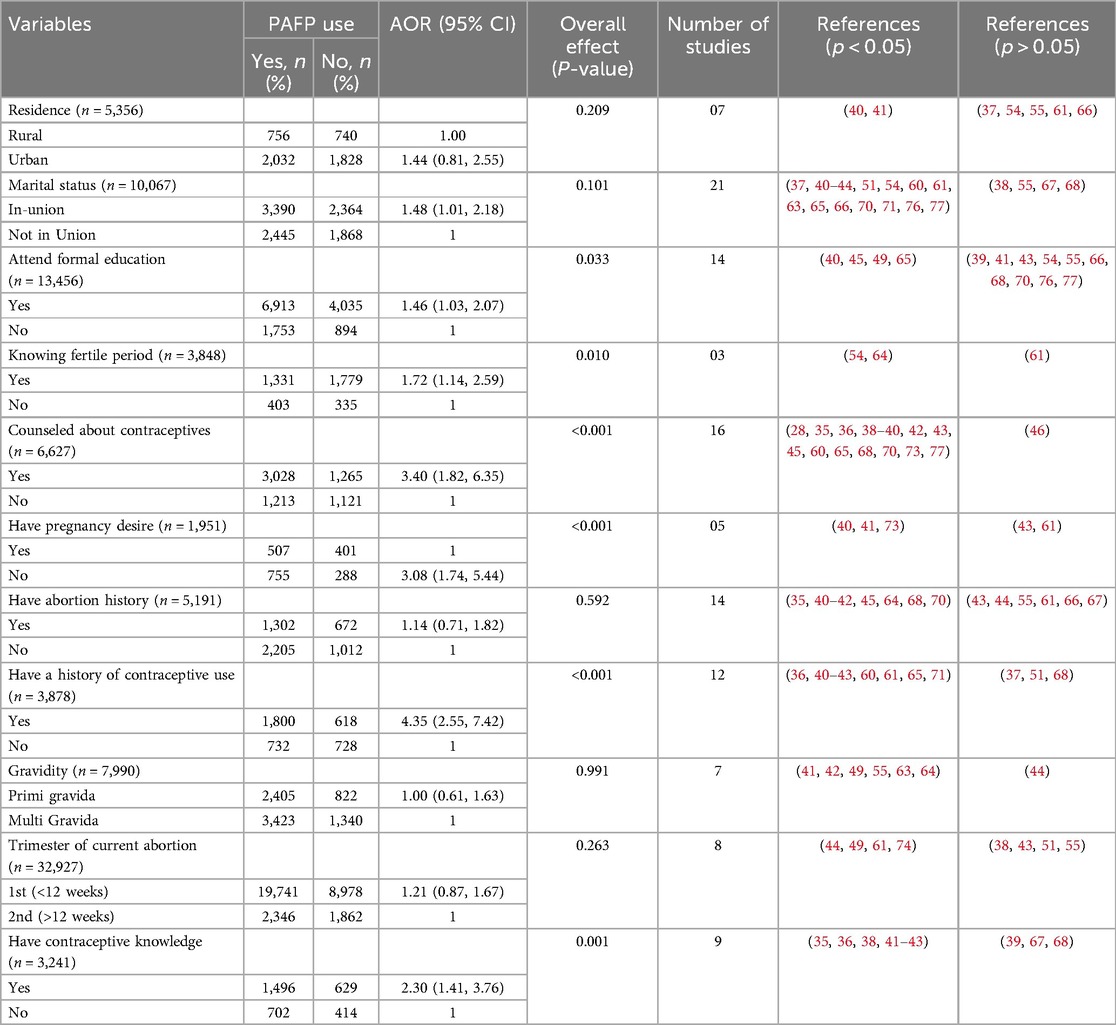
Results: From 48 articles, a total of 84,205 women who underwent abortion services were included in the analysis. The pooled prevalence of PAC uptake in Africa was 58.78% (95% CI: 52.36–65.21), with high heterogeneity (I2 = 99.8%, 95% CI: 99.2%-99.9%; P < 0.001). The subgroup analysis revealed variation by country, publication period, and sub-African region. The most widely used contraceptive methods were injectables (30.27%), followed by implants (25.13%), oral contraceptive pills (22.34%), and IUDs (10.47%). Attending formal education (OR = 1.46, 95% CI = 1.03, 2.07), knowing the period of fertility (OR = 1.72, 95% CI = 1.14, 2.59), counseling about contraceptives (OR = 3.40, 95% CI = 1.82, 6.35), not having a desire for pregnancy (OR = 3.08, 95% CI = 1.74, 5.35, 95% CI = 2.55, 7.42), and possessing contraceptive knowledge (OR = 2.30, 95% CI = 1.41, 3.76) had a statistically significant combined effect on PAC uptake in Africa.
Conclusion: The uptake of PAC in Africa stands at 58.78%, which is considered low according to the World Health Organization's recommendation that all women should postpone conception for six months following an abortion. There was also a decline of 20.22% between 2020 and 2023 compared to the pooled uptake between 2015 and 2019. To address this, it is crucial to enhance women's awareness of post-abortion contraception, the conception risks after abortion, and to strengthen client-centered counseling alongside women's education.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD42024505129, PROSPERO CRD42024505129.
Introduction
Maternal mortality and morbidity remain significant global challenges, despite ongoing efforts to meet Sustainable Development Goal (SDG) target 3.1, which aims to reduce the global maternal mortality ratio to below 70 per 100,000 live births by 2030 (1). In 2020, an estimated 287,000 maternal deaths occurred worldwide. Ninety-five percent of maternal deaths occurred in low- and low-middle-income countries, and more than two-thirds (70%) occurred in sub-Saharan Africa (SSA) (2). Pregnancies ended with unsafe abortion can lead to maternal mortality and morbidity (3). Unsafe abortion is one of the leading causes of maternal mortality worldwide, accounting for over 13% of maternal deaths, which translates to more than 38,900 lives lost annually (4, 5).
Globally, approximately half of all pregnancies are unintended, which results in induced abortion (6); from 2015 to 2019, an estimated 121 million unintended pregnancies and 73.3 million abortions were reported each year (4). Approximately 60% of unintended pregnancies and 30% of all pregnancies result in induced abortion. Furthermore, approximately 45% of all abortions are considered unsafe, with 97% of these unsafe procedures occurring in developing countries and marginalized populations (4, 7, 8). Family planning is an essential maternal and child health service package that has the potential to reduce maternal deaths by 32%, child deaths by 10%, and unwanted pregnancies by 71% (9).
Family planning significantly benefits the health of women, children, and the community at large (10, 11). As a result of modern contraceptives, from 2019 to 2020, a total of 121 million unintended pregnancies, 21 million unsafe abortions, and 125 thousand maternal deaths were averted (12). Failing to use family planning causes unintended pregnancies that result in abortion and abortion-related complications, and death (4).
The provision of post-abortion family planning (PAFP) is one of the essential integrated postabortion care services that significantly contribute to reducing unintended pregnancies, further repeated abortions, and maternal deaths (13). The WHO recommends postponing conception for at least six months after termination of pregnancy, and all women are expected to receive post-abortion contraceptives before leaving health facilities (7). However, research evidence indicates that a significant number of women who received abortion services left the health facility without using any contraceptives, 34.2% in Ethiopia (14), 46% in Kenya (15), and 80% in Tanzania (16). Routine family planning services, such as the PAFP, should be provided for all women regardless of their socio-economic status (9, 17–19).
The WHO (7) and various national abortion guidelines (20–22) have set forth recommendations advocating for the provision of family planning services prior to discharge from healthcare facilities. These recommendations are grounded in the obligation of states to uphold sexual and reproductive health rights, which aim to postpone conception for six months and/or mitigate unintended pregnancies that may lead to repeat abortions (7, 23). Despite various efforts, a significant number of women leave these institutions without accessing essential post-abortion care services. Empirical evidence shows that between 20% and 37% of women undergo subsequent abortions, which can be attributed to the insufficient use of effective modern contraceptive methods following their initial procedure (24–26).
Although there is evidence regarding PAFP uptake at the country (27–29) and sub-continent-level (30, 31) in Africa, there is a notable lack of studies assessing its predictors. Furthermore, up-to-date data are critical for implementing intervention measures to reduce unmet family planning needs. A comprehensive understanding of the prevalence and determinants of PAFP at the continental level can foster a collaborative understanding among international stakeholders and stimulate advocacy for actions. Consequently, this systematic review and meta-analysis sought to evaluate the pooled prevalence of post-abortion contraceptive uptake and the associated predictors among women who have received abortion services in Africa. The insights derived from this research could be instrumental in developing context-specific, women-centered PAFP services for African women. Additionally, the investigation into the unintended pregnancies and the prevalence of abortions reveals that the findings could be substantially mitigate maternal morbidity and mortality within the African continent.
Methods and materials
Study protocol and eligibility
This study aimed to determine the pooled prevalence of post-abortion contraceptive (PAC) uptake and its determinants among women seeking abortion services in Africa through a systematic review and meta-analysis of both published and unpublished studies were performed.
The review included all cross-sectional and cohort studies conducted in various regions of Africa, focusing on the uptake and utilization of post-abortion contraceptives, reported in studies published in English between January 1, 2015, and December 30, 2023. The year 2015 was deliberately chosen as the starting point for the review since it marked the beginning of the implementation of the Sustainable Development Goals (1). The decision to exclude the older studies aimed to focus on the most relevant and current data that accurately reflects contemporary practices and trends, in line with the Sustainable Development Goals. Furthermore, the review excluded articles that had inconsistent outcome measures and/or lacked sufficient outcomes. The review and meta-analysis adhered to the guidelines outlined in the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) reporting checklist (32).
Sources of information and search strategies
We searched several databases, including PubMed, Medline, Researchgate, Africa Journal Online, and Europe PMC, to retrieve relevant findings on post-abortion contraceptive uptake. We used the following mesh terms (“Abortion, Induced”), AND (“Contraceptive Agents”, OR “Family Planning Services”), AND (“Africa”), as well as a combination with specific African countries (Supplementary File S1). Additionally, we utilized Google Scholar to find unpublished articles and materials from the institutional repositories. All the search results were compiled using EndNote citation management software. Articles were last searched on January 01, 2024.
Study selection, data extraction, and quality assurance
Using the EndNote X8 citation manager, duplicated articles were removed. Initially, all the retrieved articles were evaluated against the eligibility criteria by carefully reading the articles’ titles and abstracts. For an article to be considered eligible, its title and abstract had to include the outcome of interest: post-abortion contraceptive uptake, along with subjects involved, which were women who received abortion services, and the study setting, which needed to be in Africa. Articles that met these inclusion criteria based solely on their title or abstract were selected for full document review. Two investigators independently assessed the eligibility of each study. If any discrepancies arose between the two investigators, we discussed the differences and reviewed the full text jointly to reach a consensus. Factors considered during a consensus discussion were alignment with the research question, study design, population, outcomes, and the clarity of reporting. In our evaluation of unpublished literature, we considered several key factors: using a scientific way to determine sample size, the appropriateness of participant selection, the validity and reliability of the survey tool, the mechanisms in place to control for confounding factors and bias, and the ethical acceptability of the studies. These considerations were particularly important given that these articles did not provide evidence of peer review.
The reviewers independently collected the data from all accessible databases and records using a standardised form. During the data extraction, variables such as the author, year of publication, country, study subject, study design, sample population, number of cases (participants with the outcome), prevalence, contraceptive method type, and available predictor variables were captured and recorded using Microsoft Excel 2016 (Supplementary File S2). The overall process of study identification, screening, and selection process is presented using the 2020 updated PRISMA flow diagram (Figure 1).
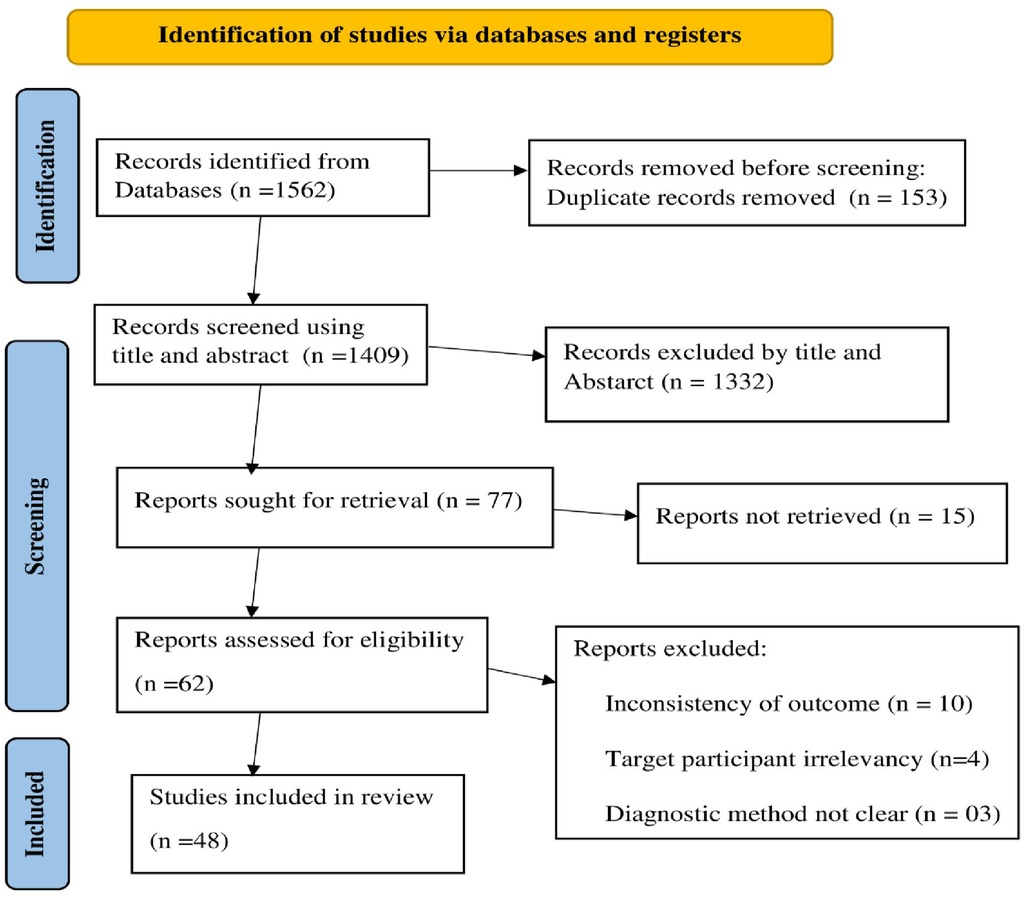
Figure 1. PRISMA flow diagram of the studies included in the systematic review and meta-analysis (32).
Measurement of the outcome
The first outcome variable of this study, the pooled prevalence of post-abortion contraceptive uptake in Africa, was calculated by dividing the total number of women who use modern contraceptives by the total number of women who received post-abortion services in the included studies (sample size) multiplied by 100. The second outcome variable of this study was the determinants of post-abortion contraceptive use in Africa, which were measured using an adjusted odds ratio. A separate met-analysis for each determinats of PAFP uptake was done using a subset of studies that reported adjusted odd ratios (AORs). A minimum of two studies was required for inclusion in each analysis. Data for each potential determinant factor was extracted in a two-by-two format in the Excel spreadsheet, and then the adjusted odds ratio was calculated for each factor. The potential determinant factors included in the analysis were residence (rural, urban), educational status (not attend formal education, attend formal education), marital status (in-union, not in-union), the desire of pregnancy (had pregnancy desire, had not pregnancy desire), knew of the fertile period (yes, no), post-abortion contraceptive counseling (yes, no), had a history of abortion (yes, no), trimester of abortion [first (<12 wks), second (>12 wks of gestation)], history of contraceptive use (yes, no), had contraceptive knowledge (yes, no), and gravidity (primigravida, multigravida).
Data synthesis and statistical analysis
The data were imported into Stata version 15.1 from a Microsoft Excel sheet for analysis. The outcome variable, post-abortion contraceptive uptake, was calculated by dividing the number of women who use modern contraceptives by the total number of women who received post-abortion services, multiplied by 100. The pooled prevalence of post-abortion contraceptive uptake with a 95% confidence interval (95% CI) was determined using a random effects model.
The heterogeneity among the included studies was examined using I2 statistics. Heterogeneity was considered to exist when the P-value of I2 was less than 0.05. I2 statistics of 25, 50, and 75% represented low, moderate, and high heterogeneity, respectively (33). An Egger regression asymmetry test for meta-analysis was used to assess publication bias. A P-value <0.05 indicated the presence of publication bias.
Sub-group analysis and meta-regression were performed to verify the sources of heterogeneity. Additionally, a sensitivity analysis was carried out to ensure the robustness of the result and to check the influence of individual studies. To examine the influence of a single study, a pooled effect of PAC use with a 95% CI was calculated, leaving one study at a time. Meta-regression analysis was done to identify factors associated with the pooled effect of PAC uptake. The adjusted odds ratio with 95% CI was reported to show the strength of the association. Variables with a P-value <0.05 were considered statistically significant, highlighting their potential influence on PAC utilization.
Results
Initially, a total of 1,562 articles were identified from different electronic databases, 153 of which were removed due to duplication. After screening the articles by title and abstract, 77 articles were selected for full-text retrieval. Fifteen additional articles were removed due to a lack of full-text articles or because they were published in languages other than English. Finally, of the 62 retrieved full-text articles, 48 articles were included in the analysis (Figure 1).
Characteristics of the included studies
A total of 48 full-length articles published between January 1, 2015, and December 30, 2023, were included in this systematic review and meta-analysis. These articles originated from different countries, with a notable majority from Ethiopia (21 studies) and Ghana (6 studies). In terms of subregions, East Africa accounted for the highest number, with a total of 34 studies. The analysis encompassed data from 84,205 women who received postabortion care. On average, 1,754 women were included in each study, with sample sizes varying from 118 participants in Ethiopia to 29,056 in Ghana. Furthermore, 94% of the studies employed a cross-sectional design (Table 1).
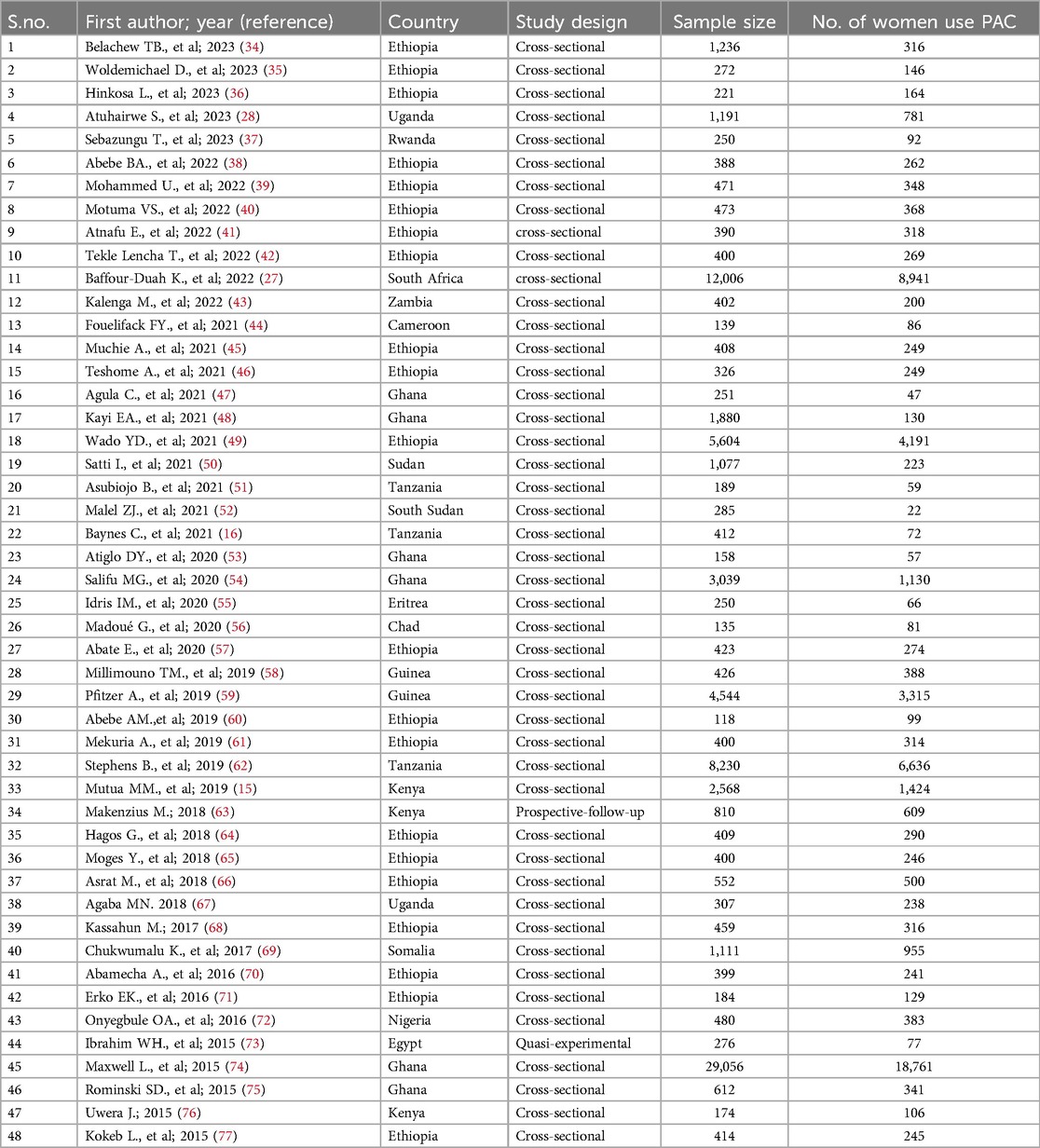
Table 1. Characteristics of the 48 studies included in the systematic review and meta-analysis to estimate the pooled prevalence of postabortion contraceptive use in Africa.
Post-abortion contraceptive uptake in Africa
In this systematic review encompassing 48 studies, the proportion of women using post-abortion contraceptives (PAC) varies significantly, with rates ranging from 6.92% in Ghana (48) to 91.08% in urban Guinea (58). The pooled prevalence of PAC uptake was found to be 58.78% (95% CI: 52.36–65.21). The I2 statistics indicated substantial heterogeneity (I2 = 99.8%, 95% CI: 99.2%–99.9%; P < 0.001) (Figure 2) Cochran's Q statistic was 20,014.24, with a p-value < 0.001, and the overall effect test yielded a z of 17.930 (p < 0.001). Consequently, subgroup analysis based on country, study design, sample size, and sub-region within Africa was performed to identify the sources of heterogeneity.
Sub-group analysis
The subgroup analysis was performed using the following variables: country, sub-African regions, publication period, and sample size. According to the subgroup analysis by country, the highest prevalence of post-abortion contraceptive uptake (85.96%) was in Somalia, followed by 81.98% in Guinea, while the lowest was 7.72% in South Sudan, followed by 20.71% in Sudan. The country-level I2 statistics revealed heterogeneity between studies from the same countries (p < 0.001). On the other hand, the subgroup analysis of the Sub-African region showed the highest post-abortion contraceptive uptake in the southern African region (62.23%, 95% CI: 38.01–86.46) and the lowest in the West African region (51.48%, 95% CI: 32.35–70.61). However, a significant difference was not observed between the sub-African region. Regarding the sample size, heterogeneity was not observed among the three groups of samples: samples below or equal to 400, 400–1,000, or more than 1,000 (p = 0.250). However, there was heterogeneity within the groups in each sample (Table 2).
Publication bias
The funnel plot (Figure 3) and bias coefficient (Egger's test; b = −0.096, 95% CI = 0.372–0.180, P = 0.489) for studies published on contraceptive uptake among post-abortion women in Africa indicated no publication bias or small study effect present (Figure 3).
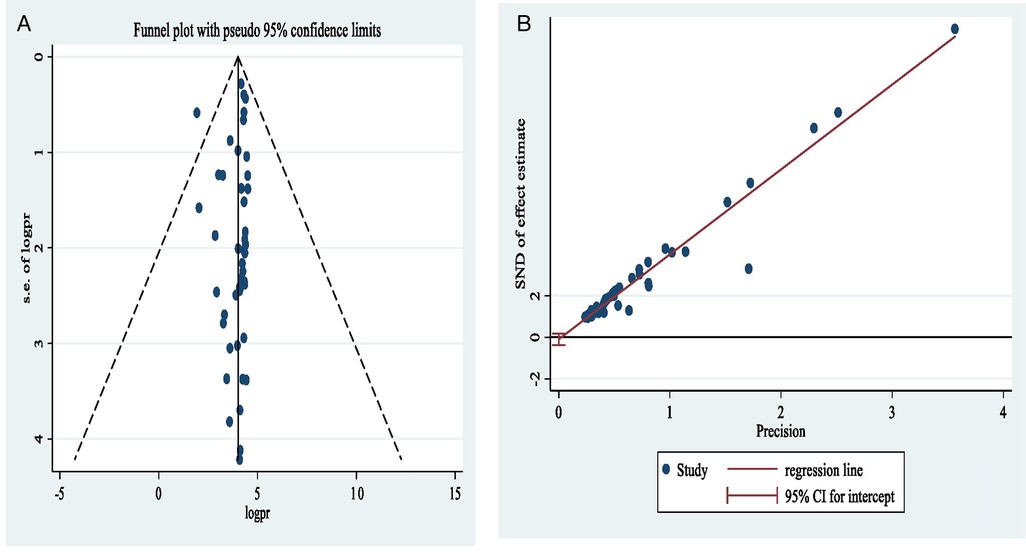
Figure 3. Funnel plot (A) and Egger's publication bias plot (B) of the logit event rate postabortion contraceptive uptake in Africa.
Sensitivity analysis
To further investigate the sources of heterogeneity in the pooled prevalence of post-abortion contraceptive use in Africa and to ensure its robustness, we execute a sensitivity analysis. According to the sensitivity analysis result, post-abortion contraceptive uptake in Africa varied between 59.92% following the removal of Kayi EA., et al. (2021) (48) and 58.09% following the removal of Millimouno TM, et al. (2019) (58). Based on this analysis, the pooled prevalence of PAC uptake was robust and had no strong evidence that showed a single study influence (Table 3).
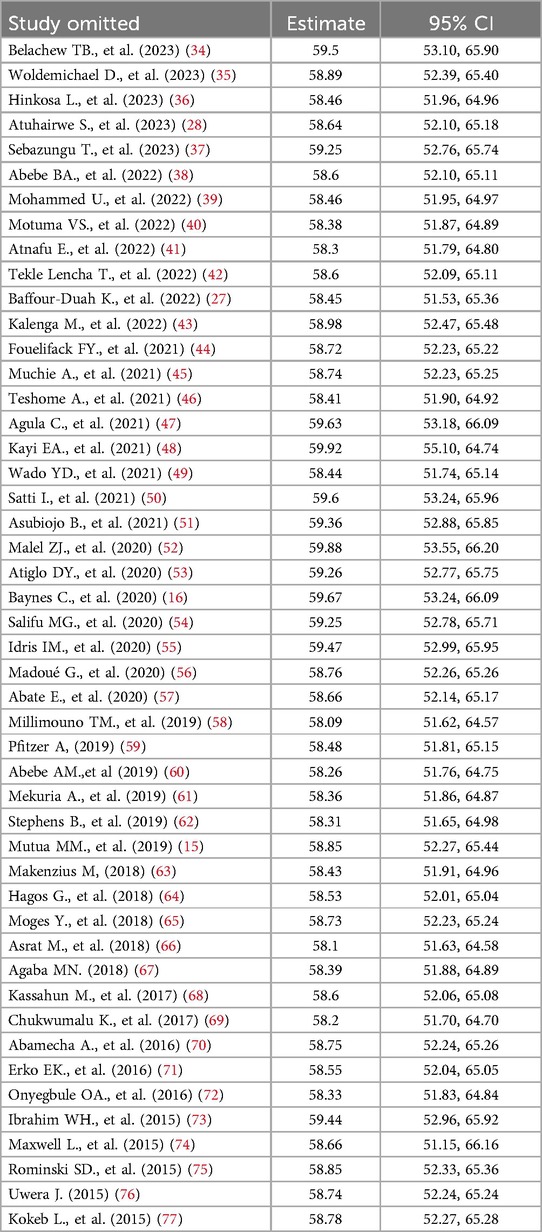
Table 3. Sensitivity analysis of pooled prevalence postabortion contraceptive use with a 95% in Africa for a single study was omitted.
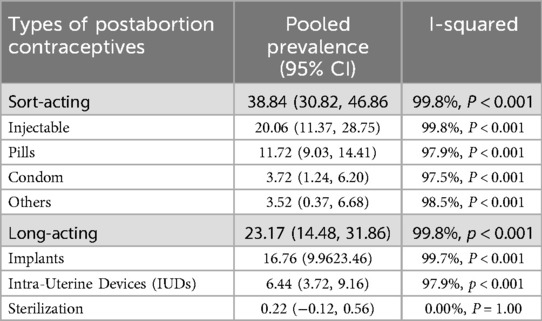
Types of post-abortion contraceptive use
Of a total of 48 studies, 28 (58.3%) examined the types of modern contraceptives that women received after undergoing an abortion. The pooled prevalence of post-abortion modern contraceptive uptake in these studies was 62.01%. Among the participants, 32, 705 (38.84%) received short-acting modern contraceptive methods, while 19,510 (23.17%) received long-acting modern contraceptive methods. Notably, more than half of the post-abortion contraceptive users received injectables, 16,892(20.06%) or implants, 14,113 (16.76%) (Table 4).
Factors associated with post-abortion contraceptive uptake
The meta-analysis was performed on 29 of the included articles and included 11 identified potential predictor variables. The findings revealed that women who attended formal education (OR = 1.46, 95% CI = 1.03, 2.07), were married and/or in union (OR = 1.48, 95% CI = 1.01, 2.18), had awareness the period of fertility (OR = 1.72, 95% CI = 1.14, 2.59), were counseled about contraceptives (OR = 3.40, 95% CI = 1.82, 6.35), did not desire to become pregnant (OR = 3.08, 95% CI = 1.74, 5.44), had a history of contraceptive use (R = 4.35, 95% CI = 2.55, 7.42), and had contraceptive knowledge (OR = 2.30, 95% CI = 1.41, 3.76) had a statistically significant combined effect on post-abortion contraceptive uptake, with an overall effect of P < 0.05. However, residence, history of abortion, trimester of current abortion, and gravidity did not have significant combined effects on postabortion contraceptive use (Table 5).
Discussion
Africa is a continent that has a high number of the least safe abortion service categories (78) and low accessibility and quality of family planning programs (79, 80). The provision of post-abortion contraceptive services is among the comprehensive abortion care packages that help to improve the health and well-being of women and reduce the repeated burden of abortion and related complications. To the best of the authors' knowledge, this study is the first to assess the predictors of postabortion contraceptives in Africa.
In this systematic review, 58.78% (95% CI: 52.36–65.21) of post-abortion contraceptive uptake was reported, which suggests that a potentially high impact could be expected on the risk of unintended pregnancy that will cause recurrent abortion. A similar finding was reported in a systematic review performed in Eastern Africa (67.86, 95% CI: 63.59, 72.12) (30) and Ethiopia (63.64%, 95% CI: 57.75–69.53) (29). However, the current finding was lower than that of a study performed in India (81%) (81), Nepal (79%) (82), the pooled prevalence of eight low-income countries (73%) (83), and 10 sub-Saharan and Asian countries (77%) (31). The possible reasons might be differences in the accessibility and quality of comprehensive post-abortion care services, women's knowledge of contraceptives, and women's desire for childbirth. The women's level of awareness of the fertile period, previous exposure to any contraceptive method, and current marital status might also contribute to the aforementioned differences.
According to our subgroup analysis, the lowest post-abortion contraceptive uptake was reported in South Sudan (7.7%) and Sudan (20.7%), and the highest was reported in Somalia (86%) and Guinea (82%). The reason for this great disparity in post-abortion contraceptive uptake between different countries could be the difference in national abortion and contraceptive strategies. The population culture, religion, population policy, and population stability of each country also have impacts on these differences.
According to the publication period, articles published before 2020 had a higher pooled prevalence of post-abortion contraceptive uptake (70.19%) than did articles published after 2020 (49.97%). A possible reason might be the influence of COVID-19. In the era of COVID-19, most health systems became fragile, and most routine health services were interrupted; the provision of contraceptive services was affected by the COVID-19 pandemic (84). One study revealed that at the time of the COVID-19 lockdown, women's access to contraception decreased from 70% to 60% (85). Moreover, the changing focus of the government health system and nongovernmental organizations in addressing the newly emerging and re-emerging diseases and other primary health care activities makes the provision of postabortion family planning services more challenging (86, 87).
Approximately two-thirds (64.10%, 95% CI: 53.56–74.65) of the post-abortion contraceptive acceptors used short-acting contraceptives. Among the specific contraceptive methods used, the most widely used contraceptive methods were injectables (30.27%, 95% CI: 18.96–41.57), followed by implants (25.13%, 95% CI: 16.75–33.51), oral contraceptive pills (22.34%, 95% CI: 16.76–27.92), IUDs (10.47%, 95% CI: 7.17–13.77), and male condoms (6.78%, 95% CI: 3.00–10.55%). Sterilization was the least used contraceptive method; only 0.34% of women used it. These findings are similar to those of studies performed in Nepal, East Africa, and developing countries (30, 82, 83). However, the current findings were different from those of a study performed in Atlanta, USA; 56% of post-abortion women used IUDs, implants, or sterilization (88). In a study done in China, approximately half of the participants used long-acting post-abortion contraceptives, and the three most utilized types of contraceptives were condoms (41.3%), IUDs (40.3%), and sterilization (9.2%) (89). This difference might be due to differences in participants' knowledge of effective and safe contraceptives, the quality of counseling, or the availability of different contraceptive methods. Most women in developing countries, including Africa, face many challenges in using the most preferred contraceptive method; inadequate trained providers, limited contraceptive method mix availability, and stockouts are among them (86, 90). In addition, participants' myths and misconceptions about each contraceptive method type and provider attitude and skill in delivering the service would have an impact on the aforementioned differences.
According to the results of this systematic review and meta-analysis, women who attended formal education had greater odds of using post-partum contraceptives than women who did not. These findings were supported by other studies (91–94). This might be because education has the power to increase women's contraceptive knowledge and attitudes (95). On the other hand, contraceptive knowledge and attitudes have an impact on the use of postabortion contraceptives. In this study, women who had contraceptive knowledge had higher odds of using post-abortion contraceptives. Other previous studies performed in the USA, China, and Singapore also supported these findings (96–98).
Like in other previous studies (29, 30, 99–101), the pooled odds ratio of post-abortion contraceptive uptake was greater among women who received post-abortion contraceptive counseling than among those who did not receive it. This is because counseling has the power to change the behavior of individuals by addressing the unique perceptions and attitudes of women through the use of person-centered, well-structured counseling approaches (100, 102, 103). Postabortion contraceptive counseling can enable women to make informed decisions about their fertility. In addition, counseling can enable women to understand the period of fertility (a period at risk for conception) (104). In this study, women who were aware of the fertility period had higher pooled odds of using postabortion contraceptives than women who were not aware of this period.
In this study, a history of contraceptive use was positively associated with post-abortion contraceptive use. These findings are supported by previous studies performed in Eastern Africa, Pakistan, and Nepal, as well as a systematic review performed in Ethiopia (29, 30, 101, 105). As a result of being exposed to family planning services, women would develop a positive lived experience with different contraceptives, and they are less affected by different contraceptive myths and misconceptions. A study in Nigeria revealed that women with lower misconception scores were significantly more likely to use modern contraceptives (106, 107). Moreover, women who have a history of contraceptive use have better information about the service than women who do not; this might have a positive effect on the use of current postabortion contraceptives. A study performed in Colombia reported a history of contraceptive use as an enabler of current contraceptive use (108).
The desire for pregnancy is another important variable that is significantly associated with postabortion contraceptive uptake; the pooled odds ratio of post-abortion contraceptive uptake was greater among women who did not desire pregnancy than among their counterparts. This was similar to the findings of a study performed in China (98). However, in a study performed in Brazil, planning of pregnancy and fertility desire were not significantly associated with postabortion contraceptive uptake (104).
Limitations of the study
This systematic review and meta-analysis have some limitations; the study didn't report the pooled prevalence of post-abortion contraceptive uptake among women who had a demand for contraceptives separately due to the unavailability of clearly stated data from the included studies. Additionally, many of the included studies were cross-sectional, which restricts the ability to infer cause-and-effect relationships due to the simultaneous measurement of exposure and outcome. While the application of the random effect model is appropriate for accounting for study variability, this approach can lead to wide confidence intervals and may not fully address the underlying sources of heterogeneity. Consequently, the pooled prevalence estimate should be interpreted considering these methodological constraints.
Conclusion
Post-abortion contraceptive uptake in Africa is low; among five women, two leave the facility without modern contraceptives. Even this figure reaches 50% or more in studies published after 2020. The main predictors identified for post-abortion contraceptive uptake were attending formal education, marital status, knowledge of the fertility period, post-abortion contraceptive counseling, history of contraceptive use, desire for pregnancy, and contraceptive knowledge. Therefore, efforts should be made to strengthen post-abortion counseling, women's education, and awareness creation about the period of fertility and contraceptives. Moreover, strengthening awareness creation programs for post-abortion women to postpone the desire for pregnancy at least six months after termination of pregnancy is paramount to reduce the cycling of abortion. These findings might also provide useful information for policymakers and programmers in developing policy briefs and evidence-based intervention modalities to improve post-abortion contraceptive use in low-income countries.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
GD: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MA: Conceptualization, Data curation, Formal analysis, Methodology, Supervision, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2025.1478797/full#supplementary-material
Supplementary File S1 | Searching strategy.docx.
Supplementary File S2 | Data base.xlsx.
Supplementary File S3 | PRISMA_2020_checklist.docx.
Supplementary File S4 | Forest plot of the subgroup analysis.docx.
Supplementary File S5 | Forest-polt of factors for PAC use in Africa.docx.
Abbreviations
IUDs, intra uterine devices; PAC, post-abortion contraceptive; PAFP, post-abortion family planning; SDG, sustainable development goal; WHO, World Health Organization.
References
1. Assembly UG. Transforming our world: the 2030 agenda for sustainable development, 21 October 2015. A/RES/70/1 (2015).
2. World Health Organization. Maternal mortality key facts. World Health Organization. Available at: https://www.who.int/news-room/fact-sheets/detail/maternal-mortality (Accessed April 26, 2024).
3. Filippi V, Chou D, Ronsmans C, Graham W, Say L. Levels and causes of maternal mortality and morbidity. In: Black RE, Laxminarayan R, Temmerman M, Walker N, editors. Reproductive, Maternal, Newborn, and Child Health: Disease Control Priorities, 3rd ed. (Vol. 2). Washington (DC): The International Bank for Reconstruction and Development / The World Bank (2016). p. 51–70. doi: 10.1596/978-1-4648-0348-2_ch3
4. Bearak J, Popinchalk A, Ganatra B, Moller A-B, Tunçalp Ö, Beavin C, et al. Unintended pregnancy and abortion by income, region, and the legal status of abortion: estimates from a comprehensive model for 1990–2019. Lancet Glob Health. (2020) 8(9):e1152–e61. doi: 10.1016/S2214-109X(20)30315-6
5. World Health Organization. Preventing unsafe abortion: evidence brief. World Health Organization (2019). Available at: https://www.who.int/publications/i/item/WHO-RHR-19.21 (Accessed November 23, 2023).
6. World Health Organization. Trends in maternal mortality 2000 to 2017: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division (2019).
8. United Nations Population Fund. Nearly Half of All Pregnancies Are Unintended—a Global Crisis, Says New UNFPA Report. New York: United Nations Population Fund (2022).
9. World Health Organization. Packages of Interventions for Family Planning, Safe Abortion Care, Maternal, Newborn, and Child Health. World Health Organization (2010). Available at: https://coilink.org/20.500.12592/qjrwtt (Accessed November 23, 2023).
10. Starbird E, Norton M, Marcus R. Investing in family planning: key to achieving the sustainable development goals. Glob Health Sci Pract. (2016) 4(2):191–210. doi: 10.9745/GHSP-D-15-00374
11. Bongaarts J, Cleland JC, Townsend J, Bertrand JT, Gupta MD. Family planning programs for the 21st century: rationale and design (2012).
14. Shiferaw BM, Kokeb LN, Bantie GM, Workie HM. Post-abortion contraceptive utilization and associated factors among women who attended abortion services: a health facility cross-sectional study. SAGE Open Med. (2024) 12:20503121231223617. doi: 10.1177/20503121231223617
15. Mutua MM, Achia TNO, Manderson L, Musenge E. Spatial and socio-economic correlates of effective contraception among women seeking post-abortion care in healthcare facilities in Kenya. PLoS One. (2019) 14(3):e0214049. doi: 10.1371/journal.pone.0214049
16. Baynes C, Yegon E, Lusiola G, Achola J, Kahando R. Post-abortion fertility desires, contraceptive uptake and unmet need for family planning: voices of post-abortion care clients in Tanzania. J Biosoc Sci. (2020) 53(6):908–23. doi: 10.1017/S0021932020000607
17. Ministry of Health of Ethiopia. National guideline for family planning services in Ethiopia. Federal Democratic Republic of Ethiopia, Ministry of Health (2020).
18. Ministry of Health DoFH, Family Planning Program. National Family Planning Guidelines for Service Providers. 6th ed. Nairobi, Kenya: RMHSU (2018).
19. Leone G. Sierra Leone Family Planning Costed Implementation Plan. Freetown: Ministry of Health and Sanitation (2017).
20. Federal Ministry of Health N. National Guidelines on Safe Termination of Pregnancy for Legal Indications. (2018).
21. Ministry of Health, Ethiopia. Technical and Procedural Guideline for Abortion Care Services in Ethiopia. Third Edition. Ethiopia, Addis Ababa (2023).
22. NDoH. National clinical guideline for implementation of the choice on termination of pregnancy act. In: Health NDo, editor. ED. 1 ed: National Department of Health, Republic of South Africa (2019)
23. Federal Ministry of Health. Technical and procedural guidelines for safe abortion services in Ethiopia. Ethiopia, Addis Ababa (2014).
24. Alemayehu B, Addissie A, Ayele W, Tiroro S, Woldeyohannes D. Magnitude and associated factors of repeat induced abortion among reproductive age group women who seek abortion Care Services at Marie Stopes International Ethiopia Clinics in Addis Ababa, Ethiopia. Reprod Health. (2019) 16(1):76. doi: 10.1186/s12978-019-0743-4
25. Behulu GK, Fenta EA, Aynalem GL. Repeat induced abortion and associated factors among reproductive age women who seek abortion services in Debre Berhan town health institutions, central Ethiopia, 2019. BMC Res Notes. (2019) 12(1):499. doi: 10.1186/s13104-019-4542-3
26. Geta G, Seyoum K, Gomora D, Kene C. Repeat-induced abortion and associated factors among reproductive-age women seeking abortion services in south Ethiopia. Womens Health. (2022) 18:17455057221122565. doi: 10.1177/17455057221122565
27. Baffour-Duah K, Olorunfemi G, Shimange-Matsose L. Pre and intra-COVID-19 trends of contraceptive use among women who had termination of pregnancy at Charlotte Maxeke Johannesburg Academic Hospital, Johannesburg, South Africa (2010–2020). PLoS One. (2022) 17(12):e0277911. doi: 10.1371/journal.pone.0277911
28. Atuhairwe S, Hanson C, Tumwesigye NM, Gemzell-Danielsson K, Byamugisha J. Second trimester post-abortion family planning uptake and associated factors in 14 public health facilities in central Uganda: a cross-sectional study. Contracept Reprod Med. (2023) 8(1):1–9. doi: 10.1186/s40834-022-00199-4
29. Wake GE, Fitie GW, Tizazu MA. A systematic review and meta-analysis on post-abortion contraceptive utilization and associated factors in Ethiopia. Front Public Health. (2022) 10:883710. doi: 10.3389/fpubh.2022.883710
30. Bizuneh AD, Azeze GG. Post-abortion family planning use, method preference, and its determinant factors in Eastern Africa: a systematic review and meta-analysis. Syst Rev. (2021) 10(1):172. doi: 10.1186/s13643-021-01731-4
31. Benson J, Andersen K, Healy J, Brahmi D. What factors contribute to postabortion contraceptive uptake by young women? A program evaluation in 10 countries in Asia and Sub-Saharan Africa. Glob Health Sci Pract. (2017) 5(4):644–57. doi: 10.9745/ghsp-d-17-00085
32. Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. Br Med J. (2021) 372:1–36. doi: 10.1136/bmj.n160
33. Aromataris E, Munn Z. JBI Manual for Evidence Synthesis JBI (2020). Available at: https://synthesismanual.jbi.global (Accessed November 15, 2023).
34. Belachew TB, Negash WD, Asmamaw DB, Fetene SM, Addis B, Baykeda TA, et al. Prevalence and predictors of post-abortion modern contraceptive utilization among reproductive age women in Ethiopia. Sci Rep. (2023) 13(1):15932. doi: 10.1038/s41598-023-42911-7
35. Woldemichael D, Agero G, Jima A, Woldemichael B. Postabortion family planning utilization and associated factors among women seeking abortion services: a cross-sectional study. Can J Fam Youth. (2023) 15(3):157–71. doi: 10.21203/rs.3.rs-74227/v1
36. Hinkosa L, Deti M, Tesfaye T, Bekele D, Diriba A. Postabortion contraceptives uptake and its associated factors among clients visiting abortion care services in public hospitals in West Shewa zone, Oromia regional state, Ethiopia, 2021. SAGE Open Med. (2023) 11:20503121231187735. doi: 10.1177/20503121231187735
37. Sebazungu T, Ruzindana K, Kitessa D, Magriples U. Factors affecting immediate use of contraception among women hospitalised for abortion in two public hospitals in Kigali, Rwanda: a cross-sectional study. East Afr Health Res J. (2023) 7(1):20. doi: 10.24248/eahrj.v7i1.704
38. Abebe BA, Abdissa G, Ganfure G, Mossisa M. Postabortion contraceptive utilization, preferences, and associated factors among women receiving abortion care services in health facilities of Ambo town, Ethiopia. Int J Reprod Med. (2022) 2022:2681478. doi: 10.1155/2022/2681478
39. Mohammed U, Lemi H, Manekullih E. Post abortion family planning utilization and associated factors among women received abortion services at Adama Hospital Medical College, Oromia, Ethiopia. J Gynecol Obstetr. (2022) 10(1):6–13. doi: 10.11648/j.jgo.20221001.12
40. Motuma VS, Yadeta TA, Alemu A, Yuya M, Eshetu B, Balis B, et al. Postabortion family planning and associated factors among women attending abortion service in dire Dawa town health facilities, eastern Ethiopia. Front Reprod Health. (2022) 4:860514. doi: 10.3389/frph.2022.860514
41. Atnafu E, Geda B, Oljira L, Atnafe G, Tamiru D, Birhanu A, et al. Postabortion contraceptive acceptance rate and its determinants among women receiving abortion service before discharge from the health facilities in Harar, eastern Ethiopia. Obstet Gynecol Int. (2022) 2022:4050844. doi: 10.1155/2022/4050844
42. Tekle Lencha T, Alemayehu Gube A, Mesele Gessese M, Tsegay Abadi M. Post-abortion family planning utilization and associated factors in health facilities of Wolaita zone, southern Ethiopia: mixed study. PLoS One. (2022) 17(6):e0267545. doi: 10.1371/journal.pone.0267545
43. Kalenga M, Kumwenda A, Vwalika B. Uptake of post-abortion contraception and associated factors at the Women and Newborn Hospital, Lusaka, Zambia. Med J Zambia. (2022) 49:35. Available at: https://search.ebscohost.com/login.aspx?direct=true&profile=ehost&scope=site&authtype=crawler&jrnl=0047651X&AN=161315909&h=axJtU%2F36UZ6Wy8VfkEkoYm%2BIQbXmXOUQPhiHab9Q2vsj7v6LSQE9QxFuLWZQrgMrqUeTHG8wZN1B3gY7LiAbDA%3D%3D&crl=c
44. Fouelifack FY, Mba CC, Ofeh AM, Tebeu PM. Determinants of contraceptive methods use after voluntary induced abortion at the Yaounde Central Hospital, Cameroon. Int J Reprod Contracept Obstet Gynecol. (2021) 10(8):2950–5. doi: 10.18203/2320-1770.ijrcog20212939
45. Muchie A, Getahun FA, Bekele YA, Samual T, Shibabaw T. Magnitudes of post-abortion family planning utilization and associated factors among women who seek abortion service in Bahir Dar town health facilities, northwest Ethiopia, facility-based cross-sectional study. PLoS One. (2021) 16(1):e0244808. doi: 10.1371/journal.pone.0244808
46. Teshome A, Wondafrash M, Gashawbeza B, Nigatu B, Asrat M, Compton SD. Post-abortion contraceptive adoption in Ethiopia. Int J Gynaecol Obstet. (2021) 154(1):157–61. doi: 10.1002/ijgo.13555
47. Agula C, Henry EG, Asuming PO, Agyei-Asabere C, Kushitor M, Kanmiki EW, et al. Contraception before and after induced abortion: trajectories of women in selected urban-poor settlements of Accra, Ghana. Afr J Reprod Health. (2021) 25(6):20–31. doi: 10.29063/ajrh2021/v25i6.3
48. Kayi EA, Biney AAE, Dodoo ND, Ofori CAE, Dodoo FN-A. Women’s post-abortion contraceptive use: are predictors the same for immediate and future uptake of contraception? Evidence from Ghana. PLoS One. (2021) 16(12):e0261005. doi: 10.1371/journal.pone.0261005
49. Wado YD, Dijkerman S, Fetters T. An examination of the characteristics and contraceptive acceptance of post-abortion clients in Ethiopia. Women Health. (2021) 61(2):133–47. doi: 10.1080/03630242.2020.1844358
50. Satti I, Satti MY, Salim NA, Mahmoud AO. Post-abortion care services at red sea state, Sudan. J Family Med Prim Care. (2021) 10(2):780. doi: 10.4103/jfmpc.jfmpc_2167_20
51. Asubiojo B, Ng’wamkai PE, Shayo BC, Mwangi R, Mahande MJ, Msuya SE, et al. Predictors and barriers to post abortion family planning uptake in Hai district, northern Tanzania: a mixed methods study. East Afr Health Res J. (2021) 5(2):182. doi: 10.24248/eahrj.v5i2.671
52. Malel ZJ, Henry BB, Legge S, Palmieri J, Agarth A. Introduction of postpartum and post abortion family planning into three hospitals in South Sudan. South Sudan Med J. (2020) 13(3):90–4. Available at: http://www.southsudanmedicaljournal.com/archive/august-2020/introduction-of-postpartum-and-post-abortion-family-planning-into-three-hospitals-in-south-sudan.html
53. Atiglo DY, Biney AAE. Postpartum and post-abortion contraceptive use among unmarried young women in Ghana. J Biosoc Sci. (2021) 53(3):459–70. doi: 10.1017/S0021932020000309
54. Salifu MG, Mohammed K. Prevalence and predictors of contraceptive use among women aged 15–49 years with induced abortion history in Ghana. Adv Prev Med. (2020) 2020:2630905. doi: 10.1155/2020/2630905
55. Idris IM. Factors influencing contraception usage: a cross-sectional study among mothers receiving abortion services in Orotta Maternity Hospital, Eritrea. Int J Sex Reprod Health Care. (2020) 3(1):70–4. doi: 10.17352/ijsrhc.000016
56. Madoué G, Lhagadang F, Saleh A, Gama S. Contraception method following spontaneous abortion in N’djamena Mother and Child Hospital. South Sudan Med J. (2020) 13(1):9–11. doi: 10.36346/SARJNHC.2019.v01i02.005
57. Abate E, Smith YR, Kindie W, Girma A, Girma Y. Prevalence and determinants of post–abortion family planning utilization in a tertiary hospital of northwest Ethiopia: a cross-sectional study. Contracept Reprod Med. (2020) 5:1–6. doi: 10.1186/s40834-020-00143-4
58. Millimouno TM, Delamou A, Sidibé S, Kolie D, Leno JP, Delvaux T, et al. The uptake of modern contraceptive methods among clients of post-abortion care services in urban Guinea. Central Afr J Public Health. (2019) 5(5):203–11. doi: 10.11648/j.cajph.20190505.14
59. Pfitzer A, Hyjazi Y, Arnold B, Aribot J, Hobson RD, Pleah TG, et al. Findings and lessons learned from strengthening the provision of voluntary long-acting reversible contraceptives with postabortion care in Guinea. Glob Health Sci Pract. (2019) 7(Supplement 2):S271–84. doi: 10.9745/GHSP-D-18-00344
60. Abebe AM, Wudu Kassaw M, Estifanos Shewangashaw N. Postabortion contraception acceptance and associated factors in Dessie Health Center and Marie Stopes International Clinics, South Wollo Northeast, Amhara Region, 2017. Int J Reprod Med. (2019) 2019:1327351. doi: 10.1155/2019/1327351
61. Mekuria A, Gutema H, Wondiye H, Abera M. Postabortion contraceptive use in Bahir Dar, Ethiopia: a cross-sectional study. Contracept Reprod Med. (2019) 4(1):1–6. doi: 10.1186/s40834-019-0099-8
62. Stephens B, Mwandalima IJ, Samma A, Lyatuu J, Mimno K, Komwihangiro J. Reducing barriers to postabortion contraception: the role of expanding coverage of postabortion care in Dar es Salaam, Tanzania. Glob Health Sci Pract. (2019) 7(Suppl 2):S258–70. doi: 10.9745/GHSP-D-19-00146
63. Makenzius M, Faxelid E, Gemzell-Danielsson K, Odero TMA, Klingberg-Allvin M, Oguttu M. Contraceptive uptake in post-care, secondary outcomes from a randomised controlled trial, Kisumu, Kenya. PLoS One. (2018) 13(8):e0201214. doi: 10.1371/journal.pone.0201214
64. Hagos G, Tura G, Kahsay G, Haile K, Grum T, Araya T. Family planning utilization and factors associated among women receiving abortion services in health facilities of central zone towns of Tigray, northern Ethiopia: a cross-sectional study. BMC Womens Health. (2018) 18(1):83. doi: 10.1186/s12905-018-0582-4
65. Moges Y, Hailu T, Dimtsu B, Yohannes Z, Kelkay B. Factors associated with uptake of post-abortion family planning in Shire town, Tigray, Ethiopia. BMC Res Notes. (2018) 11(1):928. doi: 10.1186/s13104-018-4029-7
66. Asrat M, Bekele D, Rominski SD. 4. Post-abortion contraceptive acceptance and choice determinants among women receiving abortion care at Saint Paul’s Hospital, Addis Ababa, Ethiopia. Ethiopian J Reprod Health. (2018) 10(1):14. doi: 10.69614/ejrh.v10i1.22
67. Agaba MN. Contraceptive use and choice following abortion and associated factors among female youth in Nakawa and Kawempe Divisions, Kampala-Uganda (2018).
68. Kassahun M. Utilization of Post Abortion Family Planning and Associated Factors among Women Coming to Abortion Services in Selected Abortion Clinics at Addis Ababa. Ethiopia: Addis Ababa University (2017).
69. Chukwumalu K, Gallagher MC, Baunach S, Cannon A. Uptake of postabortion care services and acceptance of postabortion contraception in Puntland, Somalia. Reprod Health Matters. (2017) 25(51):48–57. doi: 10.1080/09688080.2017.1402670
70. Abamecha A, Shiferaw A, Kassaye A. Assessment of post abortion contraceptive intention and associated factors among abortion clients in Gambella Health Facilities, Gambella Town, South West Ethiopia. Int J Med Sci Clin Inventions. (2016) 3(8):2061–70. doi: 10.18535/ijmsci/v3i8.7
71. Erko E, Abera M, Admassu B. Safe abortion care, utilization of post abortion contraception and associated factors, Jimma, Ethiopia. J Womens Health Care. (2016) 4(4):5–9. doi: 10.4172/2167-0420.1000321
72. Onyegbule O, Onumajuru C, Ododo N, Idih E, Onyegbule P. Uptake of post-abortion contraception among women who had manual vacuum aspiration at Federal Medical Centre, Owerri: a 5-year review. Trop J Obstet Gynaecol. (2016) 33(2):228–31. doi: 10.4103/0189-5117.192234
73. Ibrahim WH, El-Nashar IM, Youness EM, Arief AF. Effect of family planning counseling on post abortion women’s awareness and practice of using contraceptive methods. Assiut Sci Nurs J. (2015) 3(5):159–67. doi: 10.21608/asnj.2015.59017
74. Maxwell L, Voetagbe G, Paul M, Mark A. Does the type of abortion provider influence contraceptive uptake after abortion? An analysis of longitudinal data from 64 health facilities in Ghana. BMC Public Health. (2015) 15:586. doi: 10.1186/s12889-015-1875-2
75. Rominski SD, Morhe ES, Lori J. Post-abortion contraception choices of women in Ghana: a one-year review. Glob Public Health. (2015) 10(3):345–53. doi: 10.1080/17441692.2014.992799
76. Uwera J. Determinants of modern contraceptive uptake following immediate post abortion counselling among 15- 24 year old clients, Fhok 2014: University of Nairobi (2015).
77. Kokeb L, Admassu E, Kassa H, Seyoum T. Utilization of post abortion contraceptive and associated factors among women who came for abortion service: a hospital-based cross-sectional study. J Fam Med Dis Prev. (2015) 1(10.23937):2469–5793. doi: 10.23937/2469-5793/1510022
78. Singh S, Remez L, Sedgh G, Kwok L, Onda T. Abortion worldwide 2017: uneven Progress and unequal AccessAbortion worldwide 2017: uneven Progress and unequal access (2018).
79. United Nations Department of Economic and Social Affairs PD. World Family Planning 2022: Meeting the changing needs for family planning: Contraceptive use by age and method. UN DESA/POP/2022/TR/NO 4 (2022).
80. Haakenstad A, Angelino O, Irvine CM, Bhutta ZA, Bienhoff K, Bintz C, et al. Measuring contraceptive method mix, prevalence, and demand satisfied by age and marital status in 204 countries and territories, 1970–2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2022) 400(10348):295–327. doi: 10.1016/S0140-6736(22)00936-9
81. Banerjee SK, Gulati S, Andersen KL, Acre V, Warvadekar J, Navin D. Associations between abortion services and acceptance of postabortion contraception in six Indian states. Stud Fam Plann. (2015) 46(4):387–403. doi: 10.1111/j.1728-4465.2015.00039.x
82. Mehata S, Bhattarai N, Menzel J, Shah M, Khanal P, Tofigh S, et al. Prevalence and correlates of postabortion long-acting reversible contraceptive (LARC) use among young women (24 and below) in Nepal: strategy in the search for improvements. Reprod Health. (2019) 16(1):1–9. doi: 10.1186/s12978-019-0708-7
83. Benson J, Andersen K, Brahmi D, Healy J, Mark A, Ajode A, et al. What contraception do women use after an abortion? An analysis of 319,385 cases from eight countries. Glob Public Health. (2018) 13(1):35–50. doi: 10.1080/17441692.2016.1174280
84. Nanda K, Lebetkin E, Steiner MJ, Yacobson I, Dorflinger LJ. Contraception in the era of COVID-19. Glob Health Sci Pract. (2020) 8(2):166–8. doi: 10.9745/GHSP-D-20-00119
85. Maheshwari B, Manchanda G, Sharma P, Setiya T. Abortion and contraception practices in the COVID-19 era. Int J Reprod Contracept Obstet Gynecol. (2021) 10(5):1874–8. doi: 10.18203/2320-1770.ijrcog20211504
86. Tsui AO, Brown W, Li Q. Contraceptive practice in Sub-Saharan Africa. Popul Dev Rev. (2017) 43(Suppl 1):166–91. doi: 10.1111/padr.12051
87. Aly J, Haeger KO, Christy AY, Johnson AM. Contraception access during the COVID-19 pandemic. Contracept Reprod Med. (2020) 5:17. doi: 10.1186/s40834-020-00114-9
88. Nielsen TC, Michel KG, White R, Wall KM, Christiansen-Lindquist L, Lathrop E, et al. Predictors of more effective contraceptive method use at 12 weeks post-abortion: a prospective cohort study. J Womens Health. (2019) 28(5):591–9. doi: 10.1089/jwh.2018.7210
89. Tong C, Luo Y, Li T. Factors associated with the choice of contraceptive method following an induced abortion after receiving PFPS counseling among women aged 20–49 years in Hunan province, China. Healthcare. (2023) 11(4):535. doi: 10.3390/healthcare11040535
90. Schivone GB, Blumenthal PD. Contraception in the developing world: special considerations. Semin Reprod Med. (2016) 34(3):168–74. doi: 10.1055/s-0036-1571437
91. Beyene FY, Tesfu AA, Wudineh KG, Sendeku FW, Ayenew AA. Utilization and its factors of post abortion modern contraceptive in Ethiopia: a systematic review and meta-analysis. Reprod Health. (2021) 18(1):143. doi: 10.1186/s12978-021-01195-8
92. Tang L, Wu S, Li J, Wang K, Xu J, Temmerman M, et al. Post-abortion family planning counselling practice among abortion service providers in China: a nationwide cross-sectional study. Eur J Contracept Reprod Health Care. (2017) 22(1):24–9. doi: 10.1080/13625187.2016.1255939
93. Azmat SK, Hameed W, Ishaque M, Mustafa G, Ahmed A. Post-abortion care family planning use in Pakistan. Pak J Public Health. (2012) 2(2):4. Available at: https://ecommons.aku.edu/pakistan_fhs_mc_chs_chs/897/
94. Kumari N, Dutta M, Shekhar C. Post abortion contraceptive behavior among Indian women. Int J Reprod Contracept Obstet Gynecol. (2017) 6(5):2022. doi: 10.18203/2320-1770.ijrcog20171969
95. Bamufleh RA, Al-Zahrani AE, Yousuf SA. Systematic review: contraceptive knowledge and use in Saudi Arabia. J Gynecol Obstet. (2017) 5:69–77. doi: 10.11648/j.jgo.20170506.11
96. Guzzo KB, Hayford SR. Adolescent reproductive and contraceptive knowledge and attitudes and adult contraceptive behavior. Matern Child Health J. (2018) 22(1):32–40. doi: 10.1007/s10995-017-2351-7
97. Gosavi A, Ma Y, Wong H, Singh K. Knowledge and factors determining choice of contraception among Singaporean women. Singapore Med J. (2016) 57(11):610–5. doi: 10.11622/smedj.2015181
98. Luo Z, Gao L, Anguzu R, Zhao J. Long-acting reversible contraceptive use in the post-abortion period among women seeking abortion in mainland China: intentions and barriers. Reprod Health. (2018) 15(1):85. doi: 10.1186/s12978-018-0543-2
99. Yu Q, Fang Z. A review of the development and effect of contraceptive counseling after abortion. 亚洲社会药学. (2022) 17(1):61–9. Available at: http://ajsp.magtechjournal.com/CN/Y2022/V17/I1/61
100. Adelman S, Free C, Smith C. Predictors of postabortion contraception use in Cambodia. Contraception. (2019) 99(3):155–9. doi: 10.1016/j.contraception.2018.11.010
101. Maqbool S, Shan H, Shaheen L. Contraceptive uptake among post abortion clients in the local population of Sargodha district, Pakistan. J Islamic Int Med Coll. (2019) 14(4):174–8. Available at: https://journals.riphah.edu.pk/index.php/jiimc/article/view/1192
102. Che Y, Dusabe-Richards E, Wu S, Jiang Y, Dong X, Li J, et al. A qualitative exploration of perceptions and experiences of contraceptive use, abortion and post-abortion family planning services (PAFP) in three provinces in China. BMC Womens Health. (2017) 17(1):113. doi: 10.1186/s12905-017-0458-z
103. Mwadhi MK, Bangha M, Wanjiru S, Mbuthia M, Kimemia G, Juma K, et al. Why do most young women not take up contraceptives after post-abortion care? An ethnographic study on the effectiveness and quality of contraceptive counselling after PAC in Kilifi county, Kenya. Sex Reprod Health Matters. (2023) 31(1):2264688. doi: 10.1080/26410397.2023.2264688
104. Borges ALV, OlaOlorun F, Fujimori E, Hoga LAK, Tsui AO. Contraceptive use following spontaneous and induced abortion and its association with family planning services in primary health care: results from a Brazilian longitudinal study. Reprod Health. (2015) 12(1):94. doi: 10.1186/s12978-015-0087-7
105. Jha R, Jha SK. Factors Influencing Postabortion Contraceptive Choice among Women of Janakpur (2019).
106. Saad A, Akinsulie B, Ega C, Akiode A, Awaisu A. Misconceptions and current use of contraception among women of reproductive age in six major cities in Nigeria. Eur J Contracept Reprod Health Care. (2018) 23(6):415–20. doi: 10.1080/13625187.2018.1533546
107. Dingeta T, Oljira L, Worku A, Berhane Y. Low contraceptive utilization among young married women is associated with perceived social norms and belief in contraceptive myths in rural Ethiopia. PLoS One. (2021) 16(2):e0247484. doi: 10.1371/journal.pone.0247484
Keywords: post-abortion, contraceptive, family planning (FP), abortion, systematic review & metaanalysis, Africa
Citation: Dagnew GW and Asresie MB (2025) Post-abortion contraceptive uptake, choices, and factors associated with it among women seeking abortion services in Africa: a systematic review and meta-analysis. Front. Glob. Women's Health 6:1478797. doi: 10.3389/fgwh.2025.1478797
Received: 10 August 2024; Accepted: 30 May 2025;
Published: 16 June 2025.
Edited by:
Stephen Kennedy, University of Oxford, United KingdomReviewed by:
Japheths Onyango Ogendi, Maseno University, KenyaFaith Mbehero, Planned Parenthood Federation of America, United States
Copyright: © 2025 Dagnew and Asresie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gizachew Worku Dagnew, Z2l6LndvcmsxMkBnbWFpbC5jb20=
 Gizachew Worku Dagnew
Gizachew Worku Dagnew Melash Belachew Asresie
Melash Belachew Asresie