- 1Department of Health Informatics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 2Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Background: Sub-Saharan Africa has the highest rate of maternal death due to pregnancy-related complications. The delayed onset of Antenatal care (ANC) is a major underlying factor for maternal mortality. The overall well-being and health of pregnant women and their fetuses greatly depend on the timely initiation of ANC care. This study aims to identify the top predictors of delayed antenatal care initiation in East Africa, including Ethiopia, to provide input for policymakers.
Methodology: We employed secondary data from the Demographic Health Surveys conducted across ten East African countries between 2016 and 2023. After preprocessing the data, which included cleaning and feature selection through Recursive Feature Elimination, we addressed class imbalance using Synthetic Minority Over-sampling Technique (SMOTE). We then applied seven supervised learning algorithms to develop a robust machine learning model. The LGBM Classifier emerged as the top performer for predicting delayed antenatal care initiation, achieving accuracy of 75%, an AUC score of 81%, an F1 score of 78%, a recall of 79%, and a precision of 77%. Additionally, we employed association rule mining to further analyze.
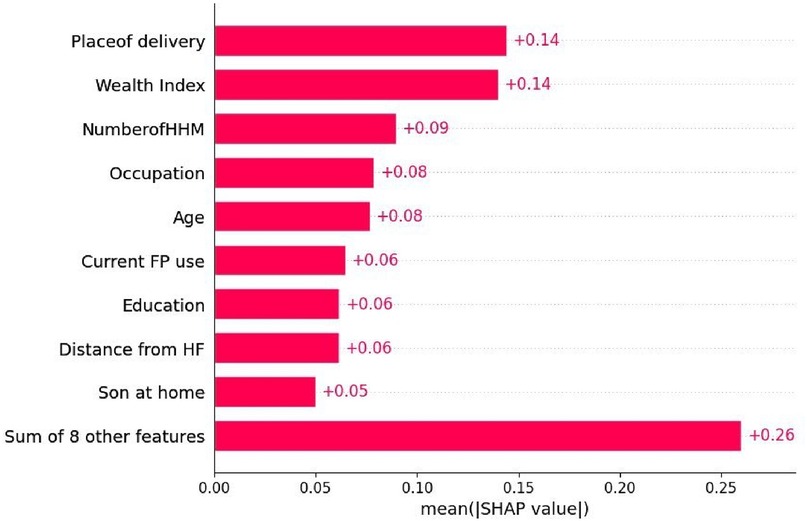
Result: Home delivery, low household income, a large number of household members, unemployment, being a younger woman, not using family planning methods, low educational level, and rural residence are predictors of delayed antenatal care initiation.
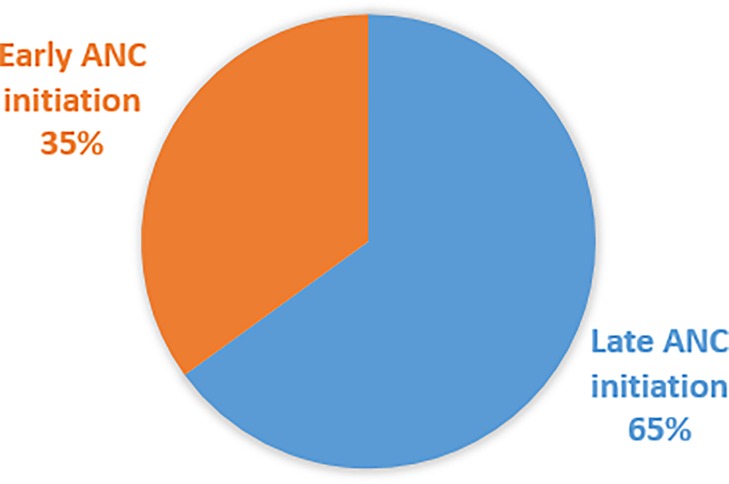
Conclusion: The prevalence of late antenatal care (ANC) initiation is high (65%). Promote family planning utilization, targeted health literacy campaigns, youth-friendly programs, expand mobile clinics, and promote skilled birth attendance to increase timely ANC initiation are recommended.
Introduction
One major concern for global health is the elevated incidences of maternal and infant mortality (1). Globally about 260,000 deaths in 2023, 92% of them preventable and mostly occurring in low- and middle-income countries for 180,000 and the highest lifetime risk at 1 in 49 woman (2, 3). Despite international efforts to lower maternal mortality, globally, pregnancy-related problems still kill thousands of women, with sub-Saharan Africa responsible for almost 70% of these deaths (4).
A WHO report showed that maternal death rates are highly discrepant between developing and developed nations, with rates of 430 and 13 per 100,000 live births, respectively (5).
The delayed onset of antenatal care (ANC) is a major underlying factor for maternal mortality (6). The overall well-being and health of pregnant women and their fetuses are greatly dependent on timely ANC care initiation (7). Preterm delivery and low birth weight are common results of delaying ANC check-ups (8). Globally, 75% of neonatal deaths are caused by preterm deliveries (9). Another consequence of missing ANC visits is anemia, often caused by low intake of iron and folic acid (10). With the right iron and folate supplements, pregnancy-related anemia can be effectively controlled and avoided (11).
The fundamental building block for delivering outstanding pregnant woman services is the timely implementation of promotion, preventive, screening, and diagnostic initiatives (12, 13). Those are strategies to realize the World Health Organization's (WHO) vision of quality health service for all pregnant mothers everywhere (12). Pregnancy-related services, such as ANC, improve and offer integrated service delivery with components related to prevention to mother to child transmission (PMTC) and HIV prevention (14). Due to the quality of ANC services, HIV-positive women can deliver HIV-negative infants (15).
Antenatal care is “the care of the woman during pregnancy” (16). Antenatal care has integrated pillars which include risk identification, prevention, and management, and health promotion related to pregnancy (12). Early prenatal care visits are vital for improving the physical, mental, and social well-being of women, and their children (17). Essential antenatal care services like birth planning, emergency preparedness, and childbirth readiness are vital to ensuring positive outcomes for women and their babies (18). A balanced diet is essential for women's health during pregnancy to promote healthy fetal growth and development, avoid stunting and wasting, and ensure great pregnancy outcomes (19).
Also, one of the WHO's strategies for reducing maternal and perinatal deaths is to enhance early and ongoing antenatal care, which is recommended to include a minimum of eight visits (20). The first ANC care visit is a crucial benchmark for subsequent antenatal care. The first antenatal care visit, also known as the “early ANC visit”, should take place within the first 12 weeks of pregnancy (WHO). Evidence revealed that timely initiation with eight ANC contact visits reduced maternal mortality by 20% (20).
Early antenatal care provision helps prevent negative pregnancy outcomes like low birth weight, premature delivery, jaundice, and early detection and treatment of syphilis, anemia, and malaria (21). On-time ANC initiation enables women to recognize potential risk factors and enhance their nutritional status (22). Early initiation of ANC is the cornerstone of early identification and treatment.
However, the incidence of early prenatal care visits differs by 57.9% between rich and poor countries (23). According to a study conducted in 19 African nations, 37.15% of pregnant women had their first antenatal care (ANC) contact during the 14th gestational week (8). Furthermore, according to the 2016 EDHS, only 20% of expectant mothers received their first antenatal care (ANC) visit before reaching 16 weeks of gestational age (24). A systematic review study also showed that 64% of Ethiopian women delay seeking antenatal care during pregnancy (25).
The evidence indicated that there were notable regional differences in the early initiation of first antenatal care. Tanzania (76%) (26), New Zealand (17%) (27), Gambia (56%) (28), Afghanistan (66.9%) (29), Malawi (75.6%) (30), (44.8%), Mozambique (60%) (31), and parts of Ethiopia (47%, 58%, 59%, 63%, 66%, 70%, 71.2%, and 78.4%) (32–39).
Based on the evidence, factors such as negative attitudes, low literacy levels, unplanned pregnancies, and lack of awareness regarding the importance of early ANC visits, along with maternal educational status, age, marital status, economic status, place of residence, parity, exposure to mass media, and distance from health facilities, are common significant contributors to delayed ANC initiation (26, 30, 40–42).
To our knowledge, there is no published study using machine learning (ML) to investigate the late initiation of AN (algorithms, previous studies conducted within small study areas and small sample sizes are non-representative of generalizability. ML algorithms are used to assess large amounts of data to confirm the predictors' role in a given problem which is good for generalizability and used as input for health policymakers for decision-making (43).
Materials and methods
Study setting
East African countries' DHS dataset was used in this study. East Africa is one of the largest regions on the African continent, including Kenya, Tanzania, Uganda, Rwanda, Burundi, and parts of Ethiopia, South Sudan, and Somalia (44).
Data source
The data on delayed antenatal visits was extracted from the Demographic Health Survey (DHS) 2016 to 2023 of ten East African countries, namely Burundi, Ethiopia, Kenya, Zimbabwe, Madagascar, Malawi, Mozambique, Rwanda, Tanzania, and Uganda, which were selected for this study based on the availability of recent DHS data and their high burden of Maternal mortality, as well as delays in the initiation of antenatal.
Population and eligibility criteria
The source population for this study was all pregnant women (aged 15–49) in ten East African nations who received ANC visits. The study population consisted of women who began ANC after 14 weeks of gestation.
Sample size determination and sampling technique
Using the most recent DHS data, we generated a weighted sample of 77,865 pregnant women who have ANC visits from the ten East African countries. The study used the standard two-stage stratified cluster sampling design employed by the DHS. In the first stage, enumeration areas (EAs) were selected randomly within each stratum using probability proportional to size. In the second stage, households within each selected EA were chosen through systematic random sampling. Eligible women aged 15–49 in the selected households were then interviewed using the DHS individual women's questionnaire
Study variables and measurements
Delay initiation of antenatal care was the outcome variable, categorized as: 1 = Yes (first antenatal care initiation within the 16th week of gestational age or four months) and 0 = No (initiation after this time).
Predictor Variables adapted from different (33, 34, 36, 38, 45–48) which include Socio-demographic factors: Age of women, type of place of residence, highest educational level, number of household member, sex of household head, currently marital status, sons at home, Getting medical help for self, and distance from the health facility.
Socio-economic factors: mobile ownership, literacy, Respondent occupation, internet usage, Wealth index.
Maternal health service utilization-related factors: Current use by method type, the total number of children ever born, place of delivery, and delivery by CS.
Operational definitions
Delayed antenatal care refers to starting the first ANC appointment after 4 months of gestational age (38).
Machine learning is an application of artificial intelligence that involves algorithms and data that automatically analyze and predict without human intervention (49).
Data management and analysis
STATA version 17 and Microsoft Excel 2019 were used to clean and weighted the data. Python 3.9 was used with incorporating key packages such as Pandas, scikit-learn, matplotlib, scikit-plot, and others. These packages facilitated data preprocessing, splitting, feature selection, model training, and final outcome prediction (50).
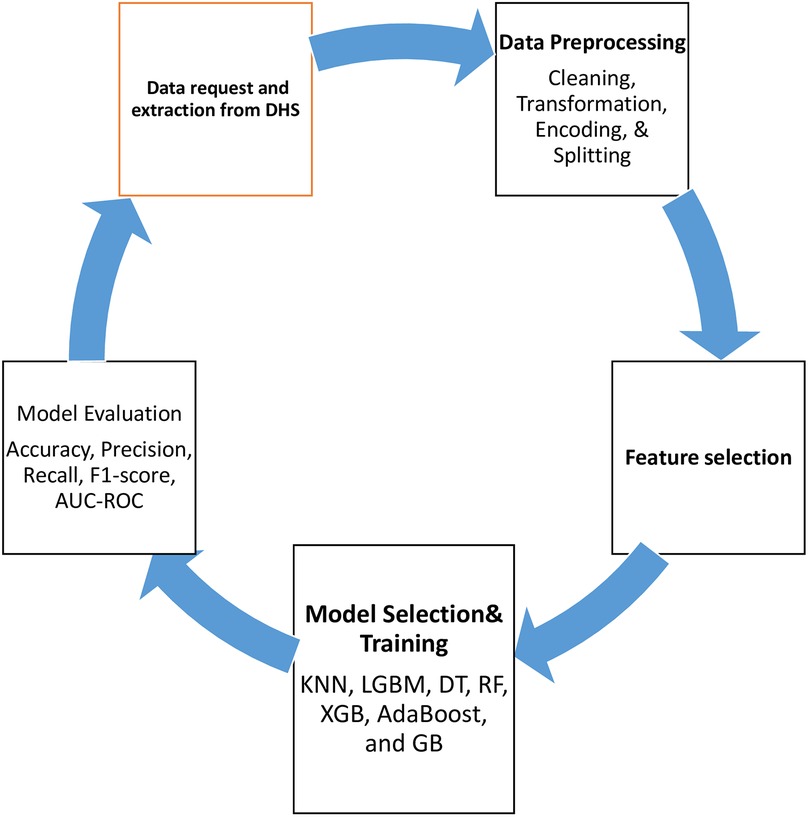
We employed data analysis procedures that included pre-processing techniques such as data cleaning to eliminate any duplicates, missing values, or outliers from the dataset. We also used the seven steps of the machine learning framework (51).
Data collection
For this study, data was gathered from ten East African countries to train the model and enhance its predictive accuracy. Specifically, data on delayed antenatal visits was extracted from the Demographic Health Surveys (DHS) from 2016 to 2023. The countries included in the study were Burundi, Ethiopia, Kenya, Zimbabwe, Madagascar, Malawi, Mozambique, Rwanda, Tanzania, and Uganda. These countries were chosen due to the availability of recent DHS data and their significant levels of maternal mortality and delays in initiating antenatal care.
Data preprocessing
According to previous evidence, data quality significantly impacts machine learning (ML) model performance and can lead to incorrect interventions or decisions. To mitigate these risks, data cleaning is a critical issue in the machine learning process, as it helps ensure the reliability and accuracy of the model's outcomes (52).
In this study, we focus on comprehensive data-cleaning techniques essential for machine learning. We address missing values through various imputation methods, such as mean, median, and mode, and remove rows or columns with excessive missing data. For instance, missing age values are filled with the median age of the dataset. The interquartile range (IQR) approach and boxplot analysis were used to identify and handle outliers. Furthermore, we address outliers, normalize and standardize features, and use One-Hot Encoding, Min-Max Normalization, and Ordinal Encoding for categorical, numerical, and ordinal data, respectively. These preprocessing steps ensure that the data is appropriately formatted and ready for machine learning algorithms (53). As seen in Figure 1.
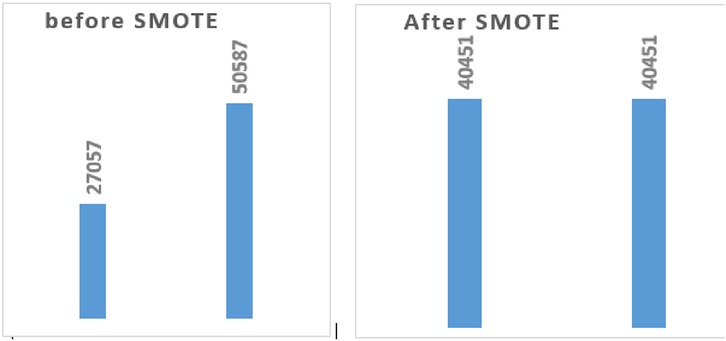
Balancing dataset
Another essential stage in using machine learning models to make accurate predictions is balancing the data prior to model training (54). To prevent machine learning models from producing biased or unreliable results, especially those that perform poorly in the minority class (late initiation of antenatal care) For instance, the study data indicated “YES” (27,507) and “NO” (50,587). To balance this imbalance, we used the Synthetic Minority Over-sampling Technique (SMOTE) to increase both classes to 40,451 instances each. As seen in (Figure 2).
Model selection
For this study, the dataset was divided into two subsets: 80% (6,473 samples) for training and 20% (1,618 samples) for validation and testing, using machine learning techniques.
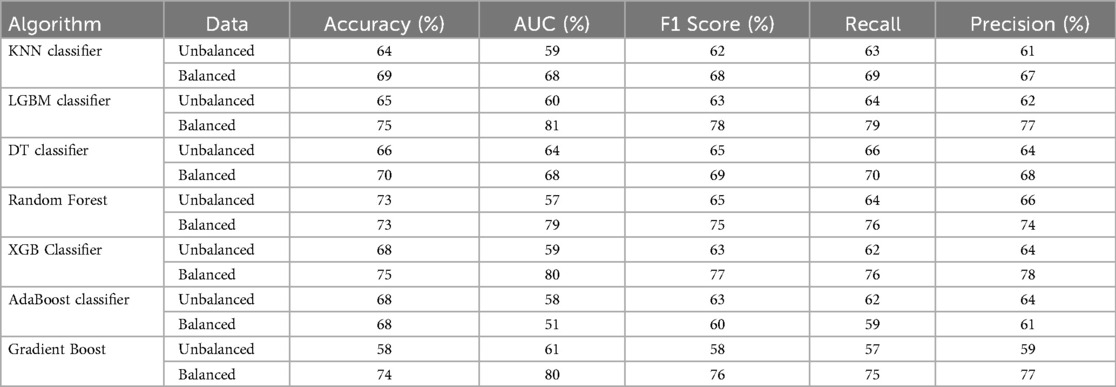
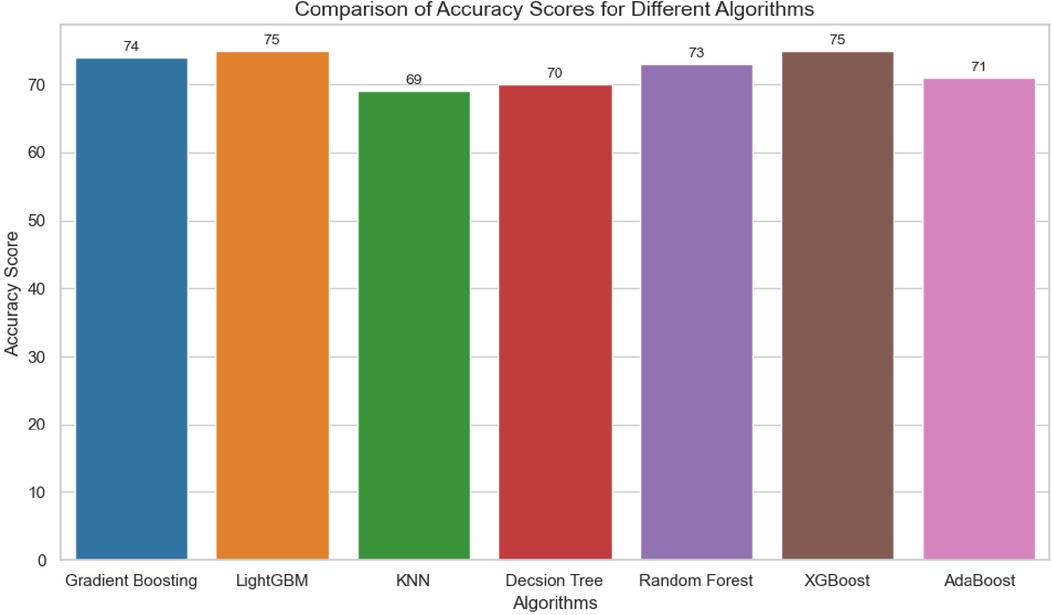
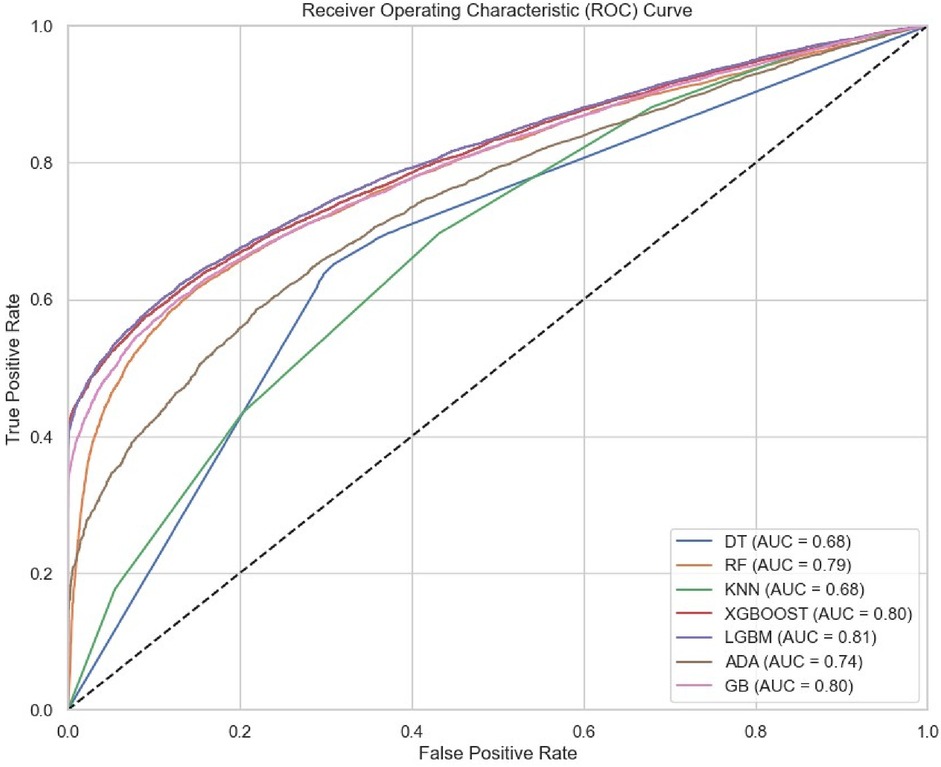
Furthermore, since the data is intended for classification and is supported by previous research, we considered the following models: AdaBoost Classifier, Decision Tree Classifier, Gradient Boosting Classifier, K-Nearest Neighbors Classifier, LightGBM Classifier, Random Forest Classifier, and Extreme Gradient Boosting Classifier. Additionally, to illustrate the relationship between various factors and the delayed initiation of antenatal care, we employed the unsupervised machine learning approach known as the Apriori algorithm. After testing various classifiers on balanced training data, the LGBM Classifier emerged as the top performer for predicting delayed antenatal care initiation, achieving 81% accuracy and an area under the ROC curve of 81%.
Model training
After selecting the model, we trained it using both balanced and unbalanced data and compared their performance through tenfold cross-validation. Following this comparison, the LightGBM model was chosen and subsequently trained with balanced data for the final prediction on unseen test data.
Model evaluation
Model evaluation is crucial to determine the model's strengths and weaknesses and test the model's capacity to generalize and yield precise predictions on data that hasn't been seen yet (55). We assessed the models' effectiveness in classifying delayed initiation of antenatal care using metrics such as accuracy, precision, recall, F1 score, and AUC- In this study, the LightGBM model emerged as the best performer, with an AUC-ROC of 81 and an accuracy of 75. Seen in Table 1 and Figures 3, 4.
Feature selection
Appropriate feature selection can enhance model performance by providing relevant data, reducing over fitting, speeding up training, and improving interpretability (56). We used Recursive Feature Elimination (RFE), a wrapper-based feature selection method, along with SHAP values to identify the most relevant features for our machine learning model Significant features are important for policymakers to have access to these important insights to inform their decision-making.
We employed the Recursive Feature Elimination (RFE) method, and a wrapper-based feature selection approach, to identify the most pertinent features for our machine learning model. The performance of the ML model depends on the quality and the relevance of the features. Significant features are important for policymakers to have access to these important insights to inform their decision-making. As seen in Figure 5.
Association rule mining
Association rule mining is among the most important and popular data mining techniques, used for discovering hidden patterns and relationships based on specific confidence intervals and lift, thereby addressing limitations in feature selection (57) (Figure 6).
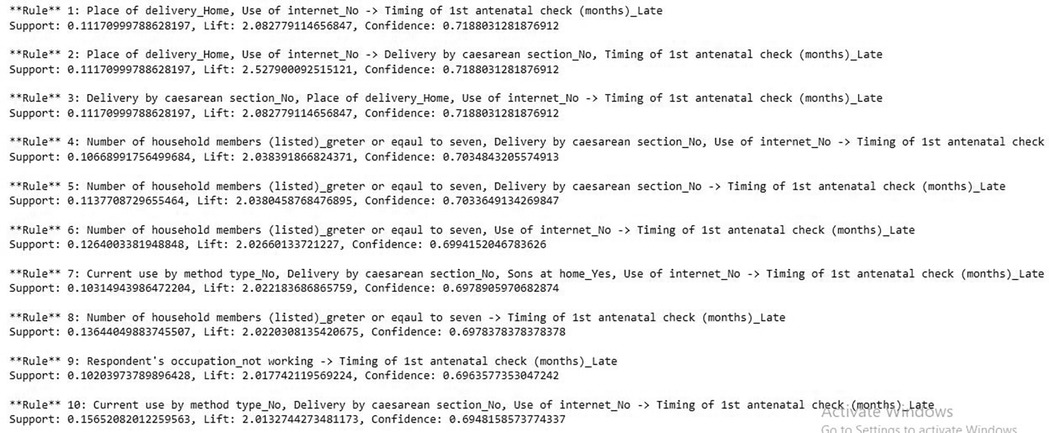
Figure 6. Association rule mining for predicting delayed antenatal care initiation among pregnant women.
Results
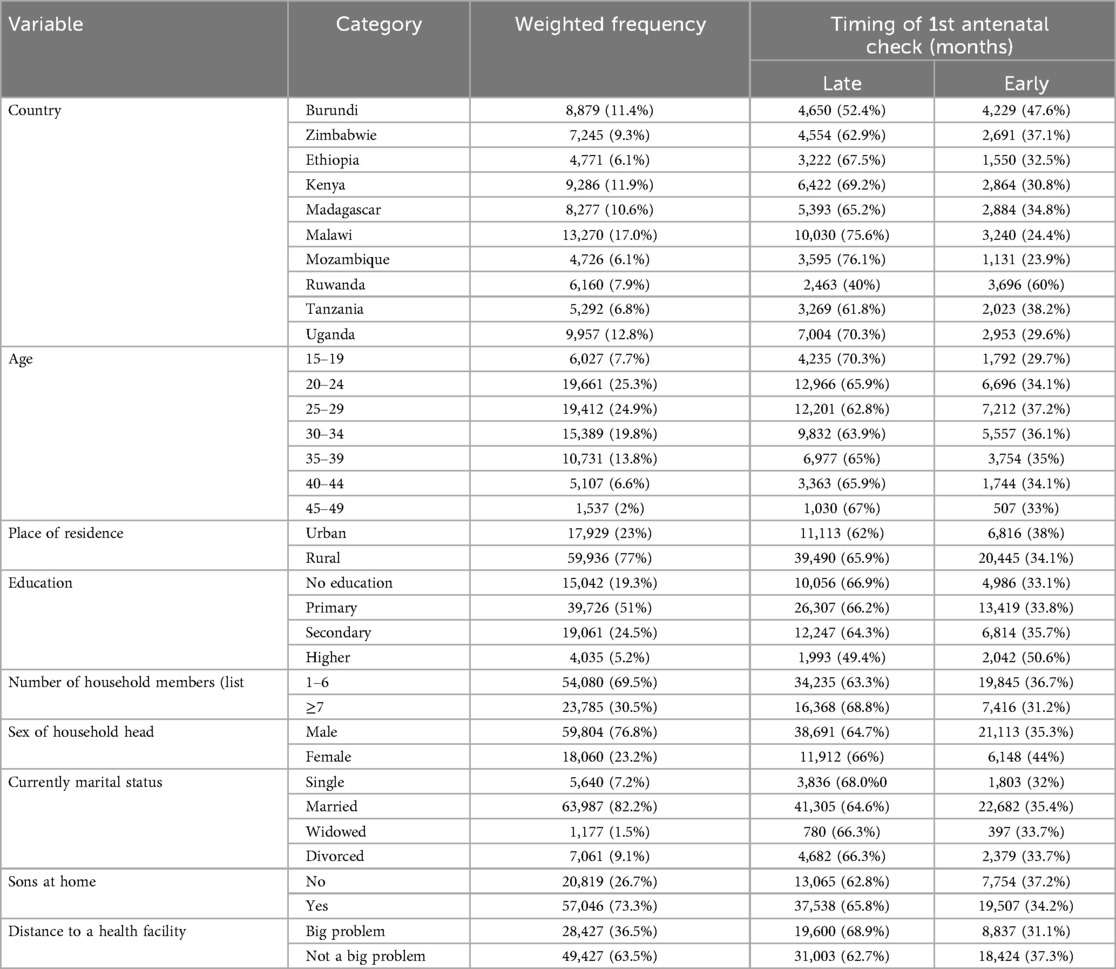
Socio-demographic characteristics
This study contained a total of 77,865 (weighted) study participants. The majority of the study participants were from Burundi, 8879 (11.4%), Kenya, 9286 (11.9%), Malawi, 13,270 (17.0%), and Uganda, 9,957 (12.8%).
The majority of study participants, aged 20–24 and 25–29, accounted for approximately 25.3% (19,661) and 24.9% (19,412), respectively. The majority of the women lived in urban areas: 59,936 (77%). Additionally, 63,987 (82.2%) were married, while 24,872 (8.3%) were single. More than half of the study participants had primary education: 39,726 (51%). Seen in Table 2.
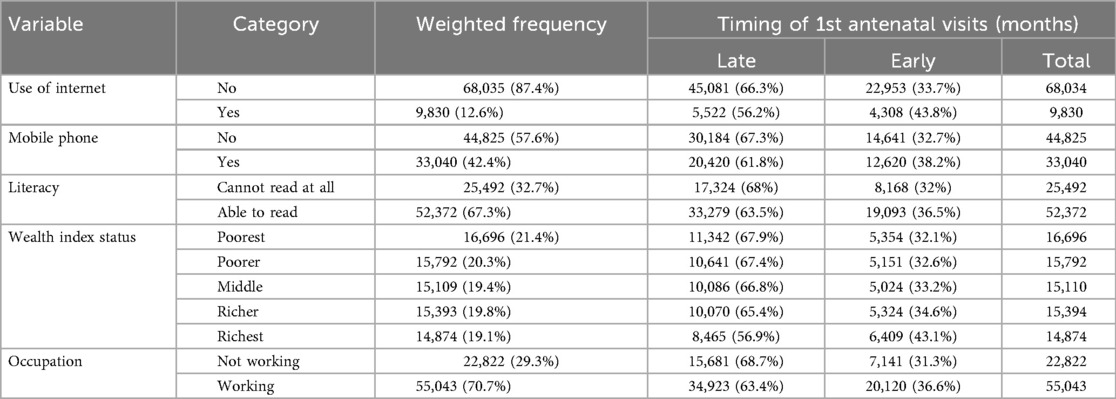
Socioeconomic-related characteristics
The study included a total of 77,865 individuals (weighted). Of these, 68,035 (87.4%) had no internet access, and 34,036 (43.6%) had a mobile phone. Among those who were able to read, 51,967 (66.5%) did so, while approximately 18,039 (23.1%) had the poorest wealth index, and 54,526 (69.8%) of women were working. Seen in Table 3.
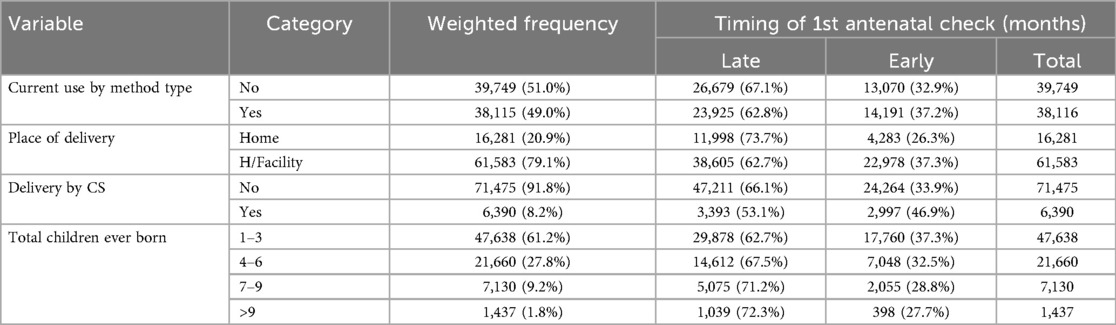
Maternal health service utilization and fertility-related factors
The study involved 77,865 individuals (weighted), with 49.0% using current methods, and 78.8% delivering at health facilities. Most participants (91.8%) were delivered by C-section, and about 60.4% had 1 to 3 children. see in Table 4.
Overall initiation of the first antenatal care visit
Out of the total, only 35% of pregnant women initiated ANC early (Figure 7).
Association rule mining
Apriori algorithms:
Rule 1: If place of delivery = home, internet access = no, Then the probability of delay antenatal care initiation is 71.8% (lift = 2.8).
Rule 2: If place of delivery = home, internet access = no, delivery by Cesarean section = no, Then the probability of delayed antenatal care initiation is 71.8% (lift = 2.5).
Rule 3: If number of HH member >7 delivery by Cesarean section = no, internet = no, Then the probability of delayed antenatal care initiation is 70% (lift = 2.03).
Rule 4: If number of HH member >7 internet access = no, Then the probability of delayed antenatal care initiation is 69% (lift = 2.02).
Rule 5: If number of HH member >7 delivery by Cesarean section = no, Then the probability of delayed antenatal care initiation is 70% (lift = 2.03).
Rule 6: If current use by method = no, delivery by Cesarean section = no, sons at home = yes, internet access = no, Then the probability of delayed antenatal care initiation is 69% (lift = 2.02).
Rule 7: If number of HH member > 7 Then the probability of delayed antenatal care initiation is 69% (lift = 2.02).
Rule 8: If respondent occupation = not work Then the probability of delayed antenatal care initiation is 69% (lift = 2.01).
Rule 9: If current use by method = no, delivery by Cesarean section = no, internet access = no, Then the probability of delayed antenatal care initiation is 69% (lift = 2.01).
Discussion
This study aims to identify the top predictors of delayed antenatal care initiation in East Africa, including Ethiopia, to provide input for policymakers. The LGBM model demonstrated superior performance compared to other classifiers, achieving an accuracy of 75%, an AUC score of 81%, an F1 score of 78%, a recall of 79%, and a precision of 77%. The performance of the LGBM model is supported by previous machine learning studies (58, 59). Its superior performance can be attributed to its efficiency, advanced learning strategy, ability to capture complex patterns, and better generalization. LGBM identified.
In this study, the overall delayed initiation of antenatal care in ten East African countries is 65% which is in line study conducted in Afghanistan (66.9%) (29), and Mozambique (60%) (31). However, higher than the studies conducted in some parts of Ethiopia (47%, 58%, 59%) (32–34), New Zealand (17%) (27), and Gambia (56%) (28), lower than a study done in Malawi (75.6%) (30).
A possible explanation for this difference could be that this study encompasses a broader scope, covering ten countries, whereas previous studies focused on a single country.
This study found that women who delivered at home had an increased likelihood of initiating antenatal care lately. This is supported by previous studies (38, 60, 61). The possible explanation for this finding could be that women who deliver at home often have lower awareness about the importance and timing of antenatal care (ANC), and may not fully understand the potential complications and risks to themselves and their babies associated with missing ANC. Additionally, the majority of women who deliver at home live in rural areas and have a low level of education.
Also, the study showed that women from poor households had an increased likelihood of delayed initiation of antenatal care. This is supported by previous studies (62, 63). The possible explanation is that women from poor families tend to give less attention to healthcare-seeking behaviors, as they are often more focused on meeting basic living needs. As a result, the probability of early antenatal care initiation is low among this group.
This study found that having a large number of household members, increases the likelihood of late initiation of antenatal care (ANC), this is supported by previous studies (47, 61, 64). The possible explanations could be women from larger households may experience increased domestic responsibilities, such as caring for children, elders, or managing household tasks, which can limit their time and ability to seek health services early in pregnancy.
This finding also showed that women with no occupation had an increased likelihood of late initiation of antenatal care (ANC), and this is supported by previous studies (31, 42, 65) The possible explanation could be women with no occupation may delay ANC due to financial dependence, limited decision-making power, and lower exposure to health information, which reduces awareness of the importance of early care.
This finding showed that being a younger woman increases the likelihood of late initiation of antenatal care (ANC), this is supported by previous studies (32, 66, 67). Younger women, especially adolescents, may delay ANC due to lack of awareness about the importance and timing of antenatal care. They are also more likely to face social stigma, especially in cases of unintended or early pregnancies, making them reluctant to seek care early. Additionally, they often have limited autonomy in health decision-making and may depend on others financially or socially, which can further delay ANC initiation.
Women who do not use family planning methods are woman increases the likelihood of late initiation of antenatal care, this is supported by previous evidence (66, 68, 69). The possible explanation for this could be unplanned pregnancies, limited awareness of maternal health, and reduced engagement with healthcare services.
Women with a low level of education are increases the likelihood of late initiation of antenatal care, as supported by previous studies (34, 38, 61, 70). Women with lower education levels often have limited knowledge about the importance and timing of antenatal care. They may not be fully aware of the benefits of early ANC in detecting and preventing pregnancy-related complications. Additionally, lower educational attainment is frequently associated with reduced decision-making power, low health literacy, and less access to health information.
This study also shows that women who live far from health facilities have an increased likelihood of late initiation of antenatal care, this is supported by previous evidence (16, 37, 38). The explanation for this finding could be that traveling long distances can take hours or a full day, making it difficult for women who have household duties. Financial constraints, including both direct and indirect costs of accessing health care services, increase with distance from health facilities. In addition, women living in rural areas may have lower levels of awareness and limited practice of visiting health facilities.
This finding shows that having a son at home increases the likelihood of delayed initiation of antenatal care (71). Having a son at home might reduce a woman's perceived need for early antenatal care, either due to cultural satisfaction, prior positive pregnancy experience, or competing household responsibilities.
Strength and limitation of the study
Our findings interpreted with consideration of certain limitations associated with the use of secondary data, as it may introduce biases that could impact the overall generalizability of the results. The DHS data lacks several key behavioral variables that could influence ANC initiation, and it is not designed to support causal inference. Under the strengths section, using hybrid algorithms that combine both supervised and unsupervised learning approaches enhances the accuracy, robustness, and adaptability of models, making them valuable tools in this study and cover wide stud area.
Conclusion
The prevalence of late antenatal care (ANC) initiation is high, at 65%, in the study area. Home delivery, low household income, a large number of household members, unemployment, being a younger woman, not using family planning methods, low educational level, and rural residence are predictors of delayed antenatal care initiation.
Promote family planning utilization, targeted health literacy campaigns, youth-friendly programs, expand mobile clinics, and promote skilled birth attendance increase timely ANC initiation are recommended.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
NB: Conceptualization, Formal analysis, Investigation, Project administration, Software, Writing – original draft, Writing – review & editing. ET: Investigation, Software, Validation, Writing – original draft, Writing – review & editing. MM: Data curation, Investigation, Methodology, Project administration, Validation, Writing – original draft, Writing – review & editing. TY: Data curation, Methodology, Project administration, Writing – original draft, Writing – review & editing. MT: Formal analysis, Investigation, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. FA: Conceptualization, Data curation, Investigation, Methodology, Project administration, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. AZ: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We are grateful to the MEASURE DHS program for granting us data access authorization, which enabled us to conduct this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Souza JP, Day LT, Rezende-Gomes AC, Zhang J, Mori R, Baguiya A, et al. A global analysis of the determinants of maternal health and transitions in maternal mortality. Lancet Glob Health. (2024) 12(2):e306–16.38070536
2. WHO. Maternal Mortality. (2025). Available online at: https://www.who.int/news-room/fact-sheets/detail/maternal-mortalit (Accessed June 20, 2025).
4. Sitaula S, Basnet T, Agrawal A, Manandhar T, Das D, Shrestha P. Prevalence and risk factors for maternal mortality at a tertiary care centre in Eastern Nepal- retrospective cross sectional study. BMC Pregnancy Childbirth. (2021) 21(1):471. doi: 10.1186/s12884-021-03920-4
5. MacDorman MF, Declercq E, Thoma ME. Trends in maternal mortality by sociodemographic characteristics and cause of death in 27 states and the District of Columbia. Obstet Gynecol. (2017) 129(5):811–8. doi: 10.1097/AOG.0000000000001968
6. Thakkar N, Alam P, Saxena D. Factors associated with underutilization of antenatal care in India: results from 2019 to 2021 national family health survey. PLoS One. (2023) 18(5):e0285454. doi: 10.1371/journal.pone.0285454
7. Konje ET, Magoma MTN, Hatfield J, Kuhn S, Sauve RS, Dewey DM. Missed opportunities in antenatal care for improving the health of pregnant women and newborns in Geita district, Northwest Tanzania. BMC Pregnancy Childbirth. (2018) 18(1):394. doi: 10.1186/s12884-018-2014-8
8. Abdo R, Demelash M, Seid AM, Mussema A. First trimester antenatal care contact in Africa: a systematic review and meta-analysis of prevalence and contributing factors. BMC Pregnancy Childbirth. (2023) 23(1):742. doi: 10.1186/s12884-023-06034-1
9. Pusdekar YV, Patel AB, Kurhe KG, Bhargav SR, Thorsten V, Garces A, et al. Rates and risk factors for preterm birth and low birthweight in the global network sites in six low-and low middle-income countries. Reprod Health. (2020) 17:1–16. doi: 10.1186/s12978-020-01029-z
10. Yismaw AE, Tulu HB, Kassie FY, Araya BM. Iron-folic acid adherence and associated factors among pregnant women attending antenatal care at Metema District, Northwest Ethiopia. Front Public Health. (2022) 10:978084. doi: 10.3389/fpubh.2022.978084
11. Asres AW, Samuel S, Daga WB, Tena A, Alemu A, Workie SB, et al. Association between iron-folic acid supplementation and pregnancy-induced hypertension among pregnant women in public hospitals, Wolaita Sodo, Ethiopia 2021: a case-control study. BMC Public Health. (2023) 23(1):843. doi: 10.1186/s12889-023-15794-6
12. World Health Organization (WHO). WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience. Geneva: World Health Organization (2016).
13. U.S. Department of Health and Human Services, Office of the Surgeon General. Strategies and Actions: Improving Maternal Health and Reducing Maternal Mortality and Morbidity. Washington, DC: U.S. Department of Health and Human Services (2020).
14. Bollinger L, Adesina A. Cost-Effectiveness of Integrating PMTCT and MNCH Services: An Application of the LiST Model for Malawi, Mozambique, and Uganda. DHS Occasional Paper No. 7. Rockville, MD: ICF International (2013).
15. Leta M, Adem S, Daniel B. Assessment of quality antenatal care-linked HIV counseling and testing as an intervention for prevention of mother-to-child transmission of HIV at government health facilities in Harari region, Eastern Ethiopia. SAGE Open Med. (2021) 9:20503121211047757. doi: 10.1177/20503121211047757
16. Belete AG, Debere MK, Gurara MK, Sidamo NB, Shimbre MS, Teshale MY. Time to initiation of antenatal care and its predictors among pregnant women who delivered in Arba Minch town public health facilities, Gamo Zone, Southern Ethiopia, 2023: a retrospective follow-up study. Reprod Health. (2024) 21(1):73. doi: 10.1186/s12978-024-01818-w
17. Gamberini C, Angeli F, Ambrosino E. Exploring solutions to improve antenatal care in resource-limited settings: an expert consultation. BMC Pregnancy Childbirth. (2022) 22(1):449. doi: 10.1186/s12884-022-04778-w
18. Limenih MA, Belay HG, Tassew HA. Birth preparedness, readiness planning and associated factors among mothers in Farta district, Ethiopia: a cross-sectional study. BMC Pregnancy Childbirth. (2019) 19:1–10. doi: 10.1186/s12884-019-2325-4
19. Dewidar O, John J, Baqar A, Madani MT, Saad A, Riddle A, et al. Effectiveness of nutrition counseling for pregnant women in low-and middle-income countries to improve maternal and infant behavioral, nutritional, and health outcomes: a systematic review. Campbell Syst Rev. (2023) 19(4):e1361. doi: 10.1002/cl2.1361
20. Chilot D, Aragaw FM, Belay DG, Asratie MH, Merid MW, Kibret AA, et al. Effectiveness of eight or more antenatal contacts on health facility delivery and early postnatal care in low-and middle-income countries: a propensity score matching. Front Med (Lausanne). (2023) 10:10.
21. Vasconcelos A, Sousa S, Bandeira N, Alves M, Papoila AL, Pereira F, et al. Antenatal screenings and maternal diagnosis among pregnant women in Sao Tome & Principe—Missed opportunities to improve neonatal health: a hospital-based study. PLOS Global Public Health. (2022) 2(12):e0001444. doi: 10.1371/journal.pgph.0001444
22. Oyato BT, Abasimel HZ, Tufa DG, Gesisa HI, Tsegaye TG, Awol M. Time to initiation of antenatal care and its predictors among pregnant women in Ethiopia: a multilevel mixed-effects acceleration failure time model. BMJ Open. (2024) 14(4):e075965. doi: 10.1136/bmjopen-2023-075965
23. Moller A-B, Petzold M, Chou D, Say L. Early antenatal care visit: a systematic analysis of regional and global levels and trends of coverage from 1990 to 2013. Lancet Glob Health. (2017) 5(10):e977–e83. doi: 10.1016/S2214-109X(17)30325-X
24. Bollinger L, Adesina A. CSA: Ethiopian Demographic and Health Survey. Addis Ababa: Central Statistical Agency (CSA) [Ethiopia] and ICF International (2016).
25. Tesfaye G, Loxton D, Chojenta C, Semahegn A, Smith R. Delayed initiation of antenatal care and associated factors in Ethiopia: a systematic review and meta-analysis. Reprod Health. (2017) 14:1–17. doi: 10.1186/s12978-017-0412-4
26. Mgata S, Maluka SO. Factors for late initiation of antenatal care in Dar es Salaam, Tanzania: a qualitative study. BMC Pregnancy Childbirth. (2019) 19:1–9. doi: 10.1186/s12884-019-2576-0
27. Corbett S, Chelimo C, Okesene-Gafa K. Barriers to early initiation of antenatal care in a multi-ethnic sample in South Auckland, New Zealand. NZ Med J. (2014) 127(1404):53–61.
28. Nigatu SG, Birhan TY. The magnitude and determinants of delayed initiation of antenatal care among pregnant women in Gambia; evidence from Gambia demographic and health survey data. BMC Public Health. (2023) 23(1):599. doi: 10.1186/s12889-023-15506-0
29. Samiah S, Stanikzai MH, Wasiq AW, Sayam H. Factors associated with late antenatal care initiation among pregnant women attending a comprehensive healthcare facility in Kandahar Province, Afghanistan. Indian J Public Health. (2021) 65(3):298–301. doi: 10.4103/ijph.IJPH_62_21
30. Palamuleni ME. Factors associated with late antenatal initiation among women in Malawi. Int J Environ Res Public Health. (2024) 21(2):143. doi: 10.3390/ijerph21020143
31. Reis-Muleva B, Duarte LS, Silva CM, Gouveia LMR, Borges ALV. Antenatal care in Mozambique: number of visits and gestational age at the beginning of antenatal care. Rev Lat Am Enfermagem. (2021) 29:e3481. doi: 10.1590/1518-8345.4964.3481
32. Girma N, Abdo M, Kalu S, Alemayehu A, Mulatu T, Hassen TA, et al. Late initiation of antenatal care among pregnant women in Addis Ababa city, Ethiopia: a facility based cross-sectional study. BMC Women’s Health. (2023) 23(1):13. doi: 10.1186/s12905-022-02148-4
33. Debelo BT, Danusa KT. Level of late initiation of antenatal care visit and associated factors amongst antenatal care attendant mothers in Gedo General Hospital, West Shoa Zone, Oromia Region, Ethiopia. Front Public Health. (2022) 10:866030. doi: 10.3389/fpubh.2022.866030
34. Gidey G, Hailu B, Nigus K, Hailu T, G/her W, Gerensea H. Timing of first focused antenatal care booking and associated factors among pregnant mothers who attend antenatal care in Central Zone, Tigray, Ethiopia. BMC Res Notes. (2017) 10:1–6. doi: 10.1186/s13104-017-2938-5
35. Kidie AA, Asmamaw DB, Belachew TB, Fetene SM, Baykeda TA, Endawkie A, et al. Socioeconomic inequality in timing of ANC visit among pregnant women in Ethiopia, 2019. Front Public Health. (2024) 12:1243433. doi: 10.3389/fpubh.2024.1243433
36. Tesfaye M, Dessie Y, Demena M, Yosef T. Late antenatal care initiation and its contributors among pregnant women at selected public health institutions in Southwest Ethiopia. Pan Afr Med J. (2021) 39(1):264. doi: 10.11604/pamj.2021.39.264.22909
37. Shewaye M, Cherie N, Molla A, Tsegaw A, Yenew C, Tamiru D, et al. A mixed-method study examined the reasons why pregnant women late initiate antenatal care in Northeast Ethiopia. PLoS One. (2023) 18(7):e0288922. doi: 10.1371/journal.pone.0288922
38. Tola W, Negash E, Sileshi T, Wakgari N. Late initiation of antenatal care and associated factors among pregnant women attending antenatal clinic of Ilu Ababor Zone, southwest Ethiopia: a cross-sectional study. PLoS One. (2021) 16(1):e0246230. doi: 10.1371/journal.pone.0246230
39. Emiru AA, Alene GD, Debelew GT. Individual, household, and contextual factors influencing the timing of the first antenatal care attendance in Northwest Ethiopia: a two-level binary logistic regression analysis. Int J Women’s Health. (2020) 12:463–71. doi: 10.2147/IJWH.S250832
40. Ahinkorah BO, Seidu AA, Budu E, Mohammed A, Adu C, Agbaglo E, et al. Factors associated with the number and timing of antenatal care visits among married women in Cameroon: evidence from the 2018 Cameroon Demographic and Health Survey. J Biosoc Sci. (2022) 54(2):322–32. doi: 10.1017/S0021932021000079
41. Ali N, Elbarazi I, Alabboud S, Al-Maskari F, Loney T, Ahmed LA. Antenatal care initiation among pregnant women in the United Arab Emirates: the mutaba'ah study. Front Public Health. (2020) 8:211. doi: 10.3389/fpubh.2020.00211
42. Iradukunda LI, Ogunbode OO, Arulogun OS. Antenatal care utilisation among adolescent mothers in Ngozi Province, Burundi. J West Afr Coll Surg. (2024) 14(2):174–9. doi: 10.4103/jwas.jwas_93_23
43. Quazi S. Artificial intelligence and machine learning in precision and genomic medicine. Med Oncol. (2022) 39(8):120. doi: 10.1007/s12032-022-01711-1
44. Raru TB, Ayana GM, Zakaria HF, Merga BT. Association of higher educational attainment on antenatal care utilization among pregnant women in east africa using Demographic and Health Surveys (DHS) from 2010 to 2018: a multilevel analysis. Int J Women’s Health. (2022) 14:67–77.
45. Wilder B, Pons-Duran C, Goddard FG, Hunegnaw BM, Haneuse S, Bekele D, et al. Development of prediction models for antenatal care attendance in Amhara region, Ethiopia. JAMA Netw Open. (2023) 6(5):e231598. doi: 10.1001/jamanetworkopen.2023.15985
46. Hailu GA, Weret ZS, Adasho ZA, Eshete BM. Quality of antenatal care and associated factors in public health centers in Addis Ababa, Ethiopia, a cross-sectional study. PLoS One. (2022) 17(6):e0269710. doi: 10.1371/journal.pone.0269710
47. Mlandu C, Matsena-Zingoni Z, Musenge E. Trends and determinants of late antenatal care initiation in three East African countries, 2007–2016: a population based cross-sectional analysis. PLOS Glob Public Health. (2022) 2(8):e0000534. doi: 10.1371/journal.pgph.0000534
48. Redi T, Seid O, Bazie GW, Amsalu ET, Cherie N, Yalew M. Timely initiation of antenatal care and associated factors among pregnant women attending antenatal care in Southwest Ethiopia. PLoS One. (2022) 17(8):e0273152. doi: 10.1371/journal.pone.0273152
49. Haleem A, Javaid M, Qadri MA, Singh RP, Suman R. Artificial intelligence (AI) applications for marketing: a literature-based study. Int J Intell Netw. (2022) 3:119–32. doi: 10.1016/j.ijin.2022.08.005
50. Tyagi S, Mittal S, editor. Sampling approaches for imbalanced data classification problem in machine learning. Proceedings of ICRIC 2019: Recent Innovations in Computing, Springer (2020).
51. Shah AD, Bartlett JW, Carpenter J, Nicholas O, Hemingway H. Comparison of random forest and parametric imputation models for imputing missing data using MICE: a CALIBER study. Am J Epidemiol. (2014) 179(6):764–74. doi: 10.1093/aje/kwt312
52. Borrohou S, Fissoune R, Badir H, Tabaa M. Data cleaning in machine learning: improving real life decisions and challenges. International Conference on Advanced Intelligent Systems for Sustainable Development, Springer (2022).
53. Chen X, Aljrees T, Umer M, Saidani O, Almuqren L, Mzoughi O, et al. Cervical cancer detection using K nearest neighbor imputer and stacked ensemble learningmodel. Digit Health. (2023) 9:20552076231203802. doi: 10.1177/20552076231203802
54. Gudivada V, Apon A, Ding J. Data quality considerations for big data and machine learning: going beyond data cleaning and transformations. Int J Adv Softw. (2017) 10(1):1–20.
55. Kebede SD, Sebastian Y, Yeneneh A, Chanie AF, Melaku MS, Walle AD. Prediction of contraceptive discontinuation among reproductive-age women in Ethiopia using Ethiopian demographic and health survey 2016 dataset: a machine learning approach. BMC Med Inform Decis Mak. (2023) 23(1):9. doi: 10.1186/s12911-023-02102-w
56. Velliangiri S, Alagumuthukrishnan S. A review of dimensionality reduction techniques for efficient computation. Procedia Comput Sci. (2019) 165:104–11. doi: 10.1016/j.procs.2020.01.079
57. Fister I Jr, Fister I, Fister D, Podgorelec V, Salcedo-Sanz S. A comprehensive review of visualization methods for association rule mining: taxonomy, challenges, open problems and future ideas. Expert Syst Appl. (2023) 33:120901.
58. Briza AC, Piedad E, Peramo EC, editors. Simpler machine learning methods outperform deep learning in motor fault detection. 2024 International Conference on Artificial Intelligence in Information and Communication (ICAIIC), IEEE (2024).
59. Indah YM, Aristawidya R, Fitrianto A, Erfiani E, Jumansyah LRD. Comparison of random forest, XGBoost, and LightGBM methods for the human development Index classification. Jambura J Math. (2025) 7(1):14–8. doi: 10.37905/jjom.v7i1.28290
60. Imo CK. Influence of women’s decision-making autonomy on antenatal care utilisation and institutional delivery services in Nigeria: evidence from the Nigeria demographic and health survey 2018. BMC Pregnancy Childbirth. (2022) 22(1):141. doi: 10.1186/s12884-022-04478-5
61. Mare KU, Andargie GG, Moloro AH, Mohammed AA, Mohammed OA, Wengoro BF, et al. Late initiation of antenatal care visit amid implementation of new antenatal care model in sub-saharan African countries: a multilevel analysis of multination population survey data. PLoS One. (2025) 20(1):e0316671. doi: 10.1371/journal.pone.0316671
62. Alem AZ, Yeshaw Y, Liyew AM, Tesema GA, Alamneh TS, Worku MG, et al. Timely initiation of antenatal care and its associated factors among pregnant women in sub-Saharan Africa: a multicountry analysis of demographic and health surveys. PLoS One. (2022) 17(1):e0262411. doi: 10.1371/journal.pone.0262411
63. Shiferie F, Abate FW, Shifraw T, Eglovitch M, Amanuel H, Chan GJ, et al. Health care seeking behaviors of pregnant women in rural amhara, Ethiopia: a qualitative study of perceptions of pregnant women, community members, and health care providers. Pan Afr Med J. (2023) 45(1):142. doi: 10.11604/pamj.2023.45.142.39771
64. Weldemariam S, Damte A, Endris K, Palcon MC, Tesfay K, Berhe A, et al. Late antenatal care initiation: the case of public health centers in Ethiopia. BMC Res Notes. (2018) 11(1):562. doi: 10.1186/s13104-018-3653-6
65. Edessa A, Dida N, Teferi E. Early initiation of antenatal care and its associated factors among antenatal care followers at public health facilities in ambo town administration, central Ethiopia. J Family Med Prim Care. (2023) 12(1):67–75. doi: 10.4103/jfmpc.jfmpc_725_22
66. Dibaba B, Bekena M, Dingeta T, Refisa E, Bekele H, Nigussie S, et al. Late initiation of antenatal care and associated factors among pregnant women attending antenatal clinic at Hiwot Fana Comprehensive Specialized Hospital, Eastern Ethiopia: a cross-sectional study. Front Glob Womens Health. (2024) 5:1431876. doi: 10.3389/fgwh.2024.1431876
67. Kourouma KR, Agbre-Yace ML, Doukour D, Tano-Kamelan A, Coulibaly-Kone AS, N'Dia AF, et al. Feasibility of the eight or more contacts of the WHO new antenatal care model in cote d'Ivoire: an antenatal care providers’ perspective. Afr J Reprod Health. (2021) 25(5):150–60.37585869
68. Tang X, Ding L, Feng Y, Wang Y, Zhou C. Antenatal care use and its determinants among migrant women during the first delivery: a nation-wide cross-sectional study in China. BMC Pregnancy Childbirth. (2019) 19(1):355. doi: 10.1186/s12884-019-2520-3
69. Tessema ZT, Tesema GA, Yazachew L. Individual-level and community-level factors associated with eight or more antenatal care contacts in sub-Saharan Africa: evidence from 36 sub-saharan African countries. BMJ Open. (2022) 12(3):e049379. doi: 10.1136/bmjopen-2021-049379
70. Dewau R, Muche A, Fentaw Z, Yalew M, Bitew G, Amsalu ET, et al. Time to initiation of antenatal care and its predictors among pregnant women in Ethiopia: cox-gamma shared frailty model. PLoS One. (2021) 16(2):e0246349. doi: 10.1371/journal.pone.0246349
Keywords: ANC, machine learning, artificial intelligence, east Africa, pregnancy
Citation: Baykemagn ND, Taye EA, Melaku MS, Yehuala TZ, Tewelgne MF, Arage FG and Zegeye AT (2025) Predicting delayed antenatal care initiation among pregnant women in East Africa: using machine learning algorithms. Front. Glob. Women's Health 6:1488391. doi: 10.3389/fgwh.2025.1488391
Received: 30 August 2024; Accepted: 26 August 2025;
Published: 3 October 2025.
Edited by:
Miodrag Zivkovic, Singidunum University, SerbiaReviewed by:
Akhtarul Islam, Khulna University, BangladeshAdenike Ogah, University of Zambia, Zambia
Copyright: © 2025 Baykemagn, Taye, Melaku, Yehuala, Tewelgne, Arage and Zegeye. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nebebe Demis Baykemagn, bmViZWJlMkBnbWFpbC5jb20=
 Nebebe Demis Baykemagn
Nebebe Demis Baykemagn Eliyas Addisu Taye1
Eliyas Addisu Taye1 Mequannent Sharew Melaku
Mequannent Sharew Melaku