- 1Department of Biomedical Sciences, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia
- 2Department of Occupational Health and Safety, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia
Background: Globally, sexually transmitted infections (STIs) continue to be a major public health problem. STIs are a major cause of morbidity and mortality in many developing countries due to their effects on reproductive and child health and their role in spreading HIV infection. This study ' to determine the factors associated with STIs among women in Ivory Coast using data from the 2021 Ivory Coast Demographic and Health Survey (DHS).
Methods: A total of 14,877 women from the 2021 Ivory Coast Demographic and Health Survey participated in this study. The Ivory Coast DHS employed a community-based cross-sectional study design for data collection. STATA version 14 was used for data extraction, recoding, descriptive analysis, and analytical analysis. Bivariable analysis was performed to identify factors for multivariable analysis. In the multivariable analysis, factors with a significance level of P < 0.05 were considered significant predictors of STIs among reproductive-age women. Finally, frequency, percentage, and odds ratios with a 95% confidence interval were reported.
Result: This study includes a total weighted sample of 14,877 women from the 2021 Ivory Coast Demographic and Health Survey. The prevalence of STIs among reproductive-age women in the last 12 months was 6.82%, with a 95% CI (6.42, 7.23). The results of the multivariate analysis showed that among women, STIs were statistically and significantly associated with age range of 20–24 years [adjusted odds ratio (AOR): 1.558, 95% CI: (1.108, 2.359); P = 0.011], 25–29 years [AOR: 1.523, 95% CI: (1.089, 2.129); P = 0.014], and 30–34 years [AOR: 1.655, 95% CI: (1.191, 2.300); P = 0.003]; living in Denguele [AOR:2.138, 95% CI: (1.328, 3.439); P = 0.002], Montagnes [AOR: 2.930, 95% CI: (1.909, 4.497); P = 0.0001], and Zanzan [AOR: 2.330, 95% CI: (1.476, 3.679); P = 0.0001]; being married [AOR: 0.705, 95% CI: (0.520, 0.975); P = 0.034]; being Muslim [AOR: 0.785, 95% CI: (0.621, 0.993); P = 0.011]; listening to radio at least once a week [AOR: 1.524, 95% CI: (1.241, 1.871); P = 0.0001]; watching television less than once a week [AOR: 1.649, 95% CI: (1.156, 2.352); P = 0.006]; using the internet almost every day [AOR: 1.359, 95% CI: (1.081, 1.708); P = 0.008]; having a history of a terminated pregnancy [AOR: 1.170, 95% CI: (1.017, 1.376); P = 0.043]; using modern contraceptives [AOR: 1.213, 95% CI: (1.032,1.427); P = 0.0001]; and being tested for HIV [AOR: 1.342, 95% CI: (1.149, 1.569); P = 0.0001].
Conclusion and recommendations: This study found that nearly seven out of a hundred reproductive-age women in Ivory Coast had sexually transmitted infections, influenced by factors such as age group, region, religion, marital status, media exposure (reading magazines, watching television, and using the internet), history of a terminated pregnancy, and contraceptive utilization. Therefore, healthcare providers and policymakers should focus on these specific predictors to reduce STIs among reproductive-age women.
Introduction
The term “sexually transmitted infections” (STIs) refers to a pathogen that causes infection through sexual contact (1). Naturally, STIs affect individuals within partnerships and larger sexual networks, and in turn, the general population (2, 3). STIs are a global public health issue, especially in developing countries (4), contributing significantly to morbidity (the rate of disease) and mortality (the rate of death) in the population (5). The World Health Organization (WHO) reported 374 million new cases of curable STIs annually in 2021 (6), with sub-Saharan Africa accounting for 40% of the global burden (7). Currently, over a million STIs are acquired daily, with approximately half a billion new cases of STIs reported annually worldwide (8, 9). In Côte d’Ivoire, epidemiological studies have revealed that over 10% of women have STIs (10). In addition, a cross-sectional study of women in Côte d’Ivoire found that 5.5% had chlamydial infections and 3.7% had gonococcal infections (11).
The greater impact of STIs on women compared with men is partly due to the female anatomy. The female urogenital system is more exposed and vulnerable to STIs compared with the male urogenital anatomy, particularly because the vaginal mucosa is thin, delicate, and easily penetrated by infectious agents (12). The cervix located at the distal end of the vagina connects to the upper genital tract, including the uterus, endometrium, fallopian tubes, and ovaries. STIs can cause a variety of symptoms and complications across different parts of the female reproductive tract, including genital ulcer disease, vaginitis, pelvic inflammatory disease, infertility, cervical cancer, and pregnancy complications (13), and drug resistance is a major threat to efforts aimed at reducing the burden of STIs worldwide (14).
Several studies demonstrated that STIs among women are associated with sociodemographic, socioeconomic, and geographic factors such as age groups, marital status, sex of household head, place of residence, education status, religion, and media exposure (15, 16).
To improve the quality of life and accomplish the goal of eradicating new HIV infections, the Ivory Coast government has endorsed a number of international commitments and strategies (17–20). However, while HIV prevention and treatment have received more public health attention in recent years than STIs, other STIs have received less attention. Although several studies have been conducted in the Ivory Coast to address this issue in different settings (19, 21–25), there is no updated and reliable national-level evidence on the factors associated with STIs among reproductive-age women. Furthermore, most of these studies lack representativeness, as they were conducted in specific regions rather than at the national level. Therefore, this study aimed to identify the factors associated with STIs among women in Ivory Coast at the national level using the Ivory Coast Demographic and Health Survey (DHS). Furthermore, policymakers and other stakeholders may prefer national-level findings, which serve as a foundation for designing and implementing appropriate intervention programs aimed at reducing the rate of STIs among women. In addition, this study also serves as a valuable reference for future research in this field.
Methods and materials
Study setting and period
Ivory Coast is a country in West Africa, located between 4°30′ and 10°30′ north latitude. It extends over an area of 322,462 km2 and is bordered to the north by Mali and Burkina Faso, to the west by Liberia and Guinea, to the east by Ghana, and to the south by the Atlantic Ocean. According to the 2021 population census, the country had 29,389,150 inhabitants, with 45% aged <18 years old. Women aged 15–49 represented 24% of the total population. The National Institute of Statistics (INS) carried out the 2021 Ivory Coast Demographic and Health Survey from 8 September to 30 December 2021, with technical assistance from the International Classification of Functioning, Disability, and Health (ICF) and specialized departments of the Ministry of Health, Public Hygiene, and Universal Health Coverage (26, 27).
Data source/data extraction
The data used in this analysis were obtained from the 2021 Ivory Coast Demographic and Health Survey, accessible through the DHS portal at https://dhsprogram.com/data/dataset_admin/index.cfm. Permission was obtained through an online request by explaining the purpose of the study (26, 27).
Study design
This study employed a community-based cross-sectional design, as the DHS used this design to collect data.
Sampling procedure
To ensure representativeness, the sampling process for the 2021 Ivory Coast Demographic and Health Survey was created, taking into account the country's 14 administrative districts as well as both urban and rural residential areas. The selection procedure for drawing the sample had two stages. At the first level, 539 clusters were selected for investigation, 261 of which were found in urban areas and 278 in rural areas. The National Institute of Statistics conducted a census mapping in 2019 to create a list of clusters, which served as the basis for systematically selecting clusters with a probability proportional to household size. This process was carried out prior to the 2021 Population and Housing Census (RGPH) (26, 27). At the second level, a sample of 15,092 households was selected at a rate of 28 households per cluster, 7,308 of which were located in urban areas and 7,784 in rural areas (Figure 1).
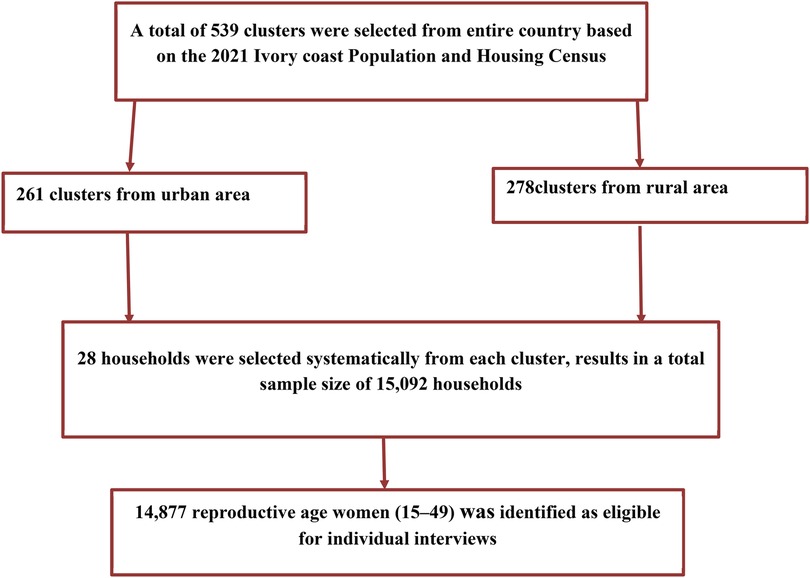
Figure 1. The sampling process of reproductive-age women (27).
Study population
All women aged 15–49 who were either long-term residents of the selected households or guests who had spent the night before the survey were eligible to be interviewed. Data were collected from 14,877 reproductive-age women through face-to-face interviews using a standardized women's questionnaire. In this study, STIs among reproductive-age women were the outcome variable (27).
Study variables
The outcome variable for this study was STIs among women. This variable has a binary result (yes or no). Women were asked whether they had a disease they had acquired a disease through sexual contact in the past 12 months. If they had not acquired STIs in the last 12 months, responses were labeled as “no” and coded as “0”; otherwise, responses were labeled as “yes” and coded as “1”.
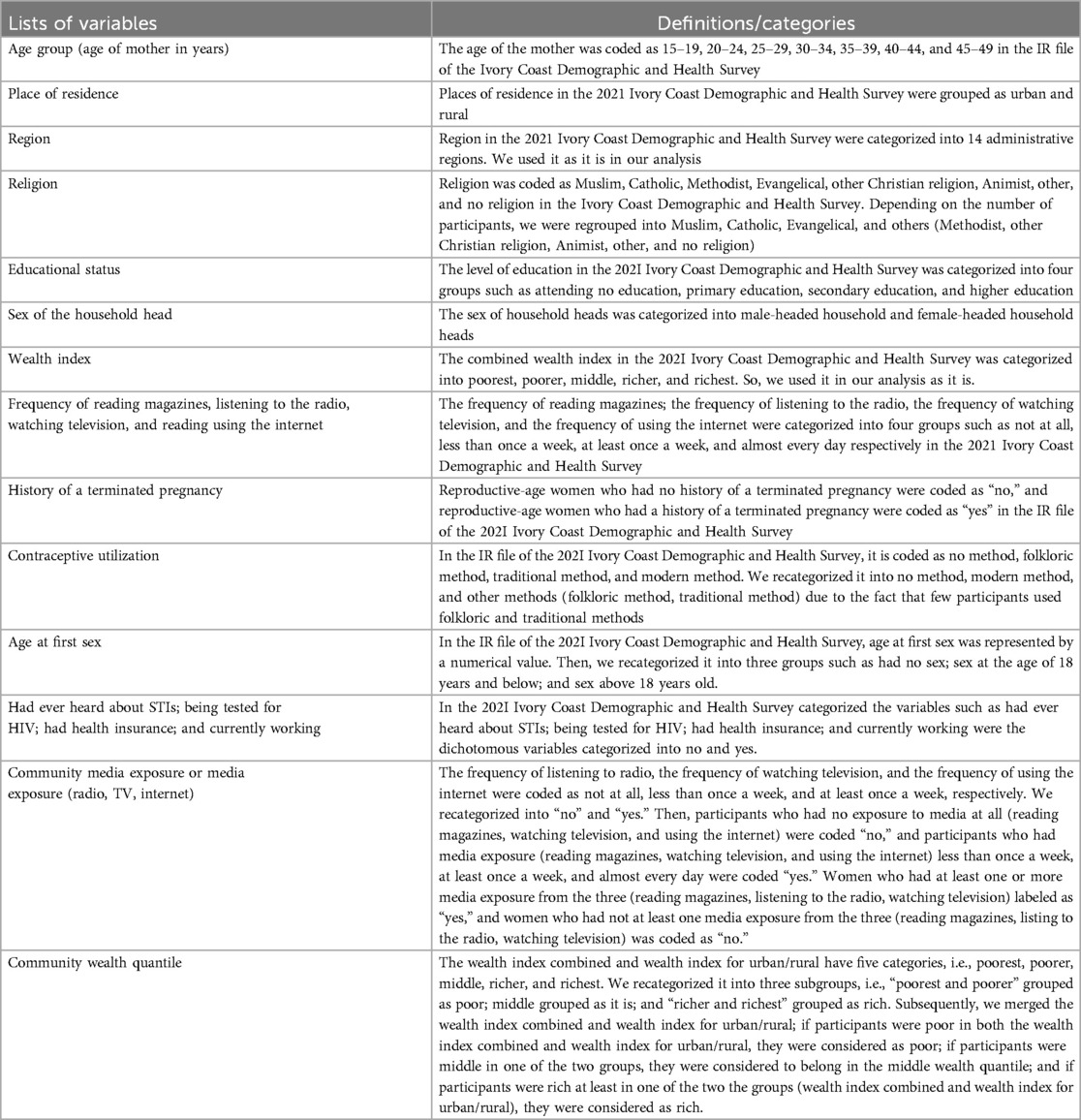
The independent variables included age group, place of residence, region, religion, educational status, marital status, sex of the household head, wealth index, media exposure (reading magazines, watching television, and using the internet), history of a terminated pregnancy, had health insurance, contraceptive utilization, being tested for HIV, currently working, number of unions, community media exposure, and community wealth quantile (Table 1).
Data management and analysis
Data extraction, recoding, descriptive analysis, and analytical analysis were all performed using STATA version 14. We carried out weighting by dividing the total number of women in the entire country by the appropriate survey sampling proportion and the standard weights of the women. Bivariate analysis was first employed to identify the potential factors associated with STIs among reproductive-age women. This initial analysis assessed the relationship between each independent variable and the outcome variable (STIs), allowing for the identification of factors that showed significant associations with STIs. Variables that demonstrated a significant relationship with the outcome in the bivariate analysis, indicated by P < 0.05, were included in the multivariate analysis. The multivariate analysis was then conducted to examine the independent effect of each selected variable while controlling for potential confounding factors. Only those variables with P < 0.05 in the multivariate analysis were considered significant predictors of STIs. Finally, the percentage and odd ratios were provided, together with their 95% confidence intervals.
Ethical consideration
This study used secondary data from the Demographic and Health Survey (DHS), which did not require ethical review or participant consent. The data ensured confidentiality, adhering to DHS privacy protocols. The integrity of the data was preserved, as it was originally collected following ethical guidelines. Data use complied with DHS guidelines and respected the informed consent provided by participants. No new data were collected, and there was no direct participant interaction. The findings were presented responsibly to minimize misinterpretation.
Results
Sociodemographic characteristics of the participants
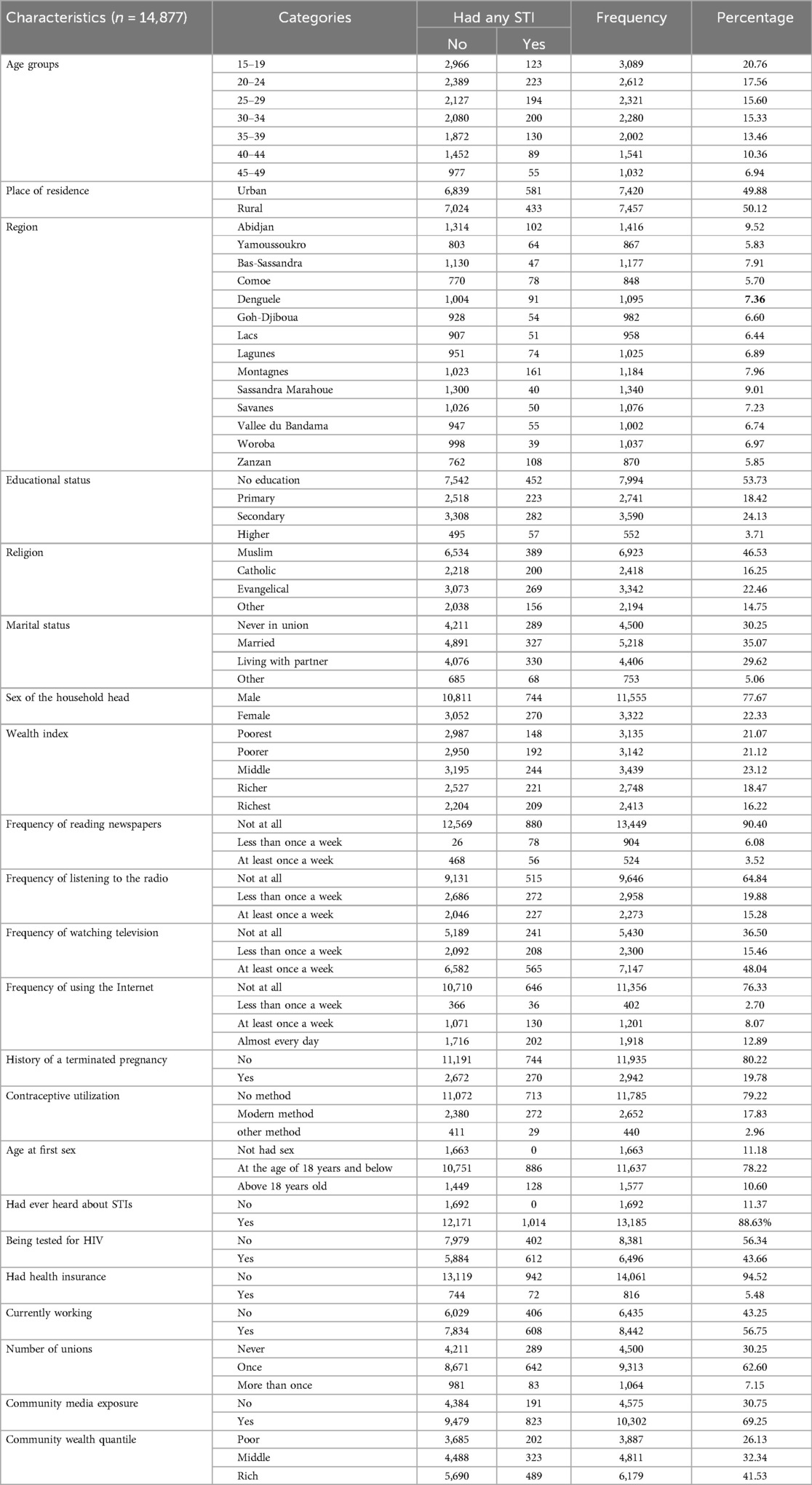
A total of 14,877 women participated in this investigation. Approximately 3,089 participants (20.76%) were in the 15–19 age range; 7,457 (50.12%) were rural residents; 1,416 (9.52%) were from the Abidjan region; 7,994 (53.73%) were non-educated; 6,923 (46.53%) were Muslims; and 5,218 (35.07%) were married. Households headed by men accounted for 11,555 (77.67%); 3,439 (23.12%) were in the middle wealth quantile; 13,449 (90.40%) did not read at all; 9,646 (64.84%) did not listen to the radio. Television was watched at least once a week by 7,147 (48.04%), and 11,356 (76.33%) did not use the internet at all. In terms of reproductive health, 2,942 (19.78%) had a history of a terminated pregnancy; 2,652 (17.83%) utilized modern contraceptives; and 11,637 (77.22%) had their first sex at the age of 18 and below. Health insurance coverage was reported by 14,061 (94.52%); 8,381 (56.34%) were never tested for HIV; 13,185 (88.63%) had ever heard of STIs; 8,442 (56.75%) were currently working; 9,313 (62.60%) had single union; 10,302 (69.25%) had community media exposure; and 6,179 (41.53%) belonged to the rich wealth quantile (Table 2).
Prevalence of sexually transmitted infections
The prevalence of STIs among women in the 12 months preceding the survey was 6.82%, with a 95% CI (6.42–7.23). The highest prevalence of STIs was observed in the Montagnes region (161 cases, 15.88%), followed by Zanzan (108 cases, 10.65%) and Abidjan (102 cases, 10.06%). In contrast, the lowest prevalence was recorded in Bas-Sassandra (47 cases, 4.64%), Sassandra-Marahoué (40 cases, 3.94%), and Woroba (39 cases, 3.85%) (Table 3).

Table 3. Prevalence of sexually transmitted infections among reproductive-age women in Ivory Coast in 2021.
Bivariable analysis on factors analysis associated with sexually transmitted infections
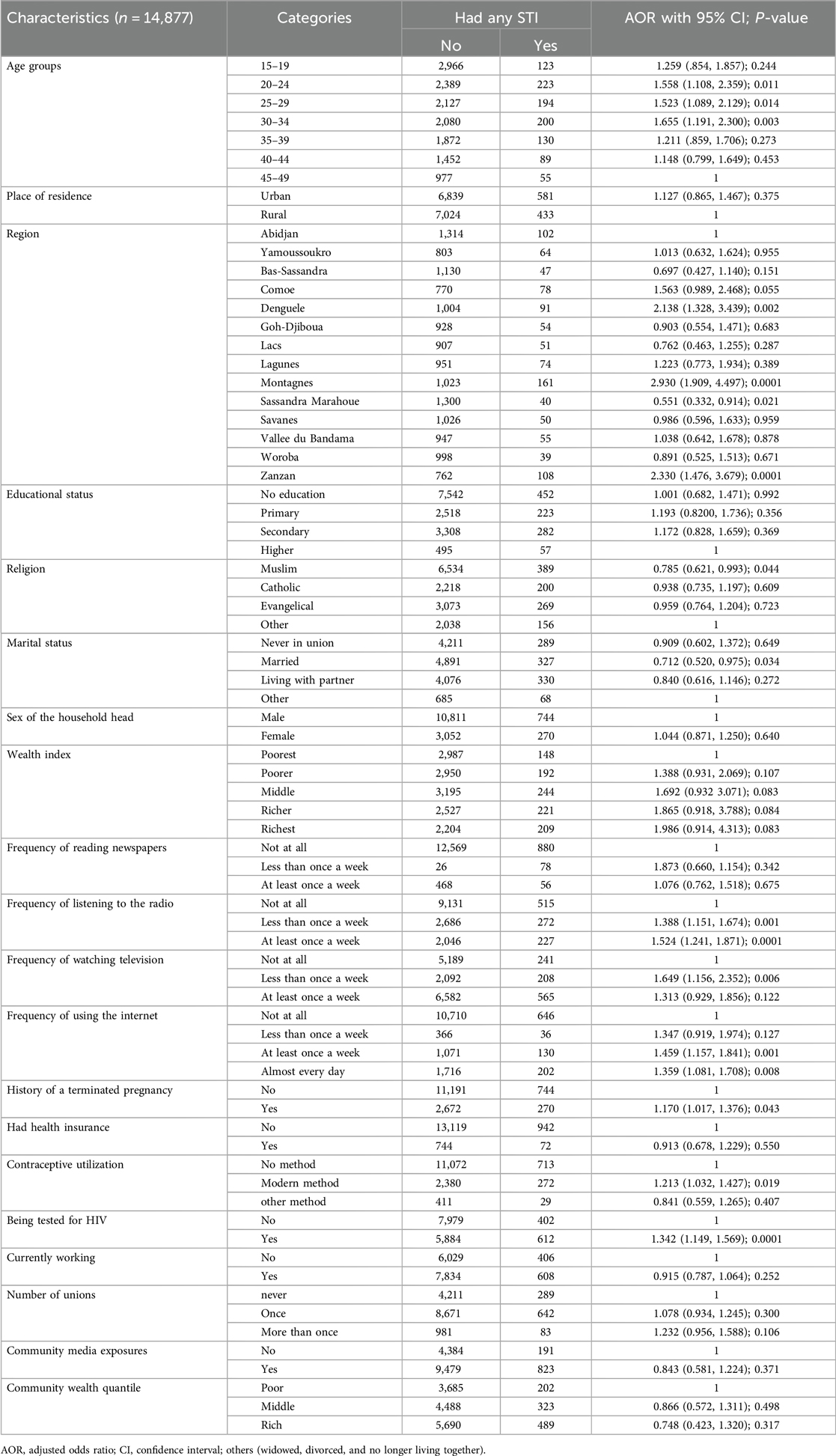
The results of the bivariable analysis showed that STIs among women were statistically and significantly associated with the following factors: age range of 20–24 years [crude odds ratio (COR): 1.770, 95% CI: (1.254, 2.359); P = 0.001], 25–29 years [COR: 1.734, 95% CI: (1.258, 2.391); P = 0.001], and 30–34 years [COR: 1.841, 95% CI: (1.337, 2.534); P = 0.0001]; living in Montagnes [COR: 2.027, 95% CI: (1.561, 2.632); P = 0.0001]; living in an urban area [COR: 1.378, 95% CI: (1.211, 1.567); P = 0.0001]; having no education [COR: 0.538, 95% CI: (0.391, 0.739); P = 0.0001]; religion [COR: 0.538, 95% CI: (0.391, 0.739); P = 0.0001]; being married [COR: 0.673, 95% CI: (0.512, 0.885); P = 0.005]; being the head of a female-headed household [COR: 1.285, 95% CI: (1.112, 1.485); P = 0.001]; being in the richest wealth category [COR: 1.913, 95% CI: (1.539, 2.379); P = 0.0001]; having a history of a terminated pregnancy [COR: 1.521, 95% CI: (1.303, 1.774); P = 0.0001]; having health insurance [COR: 1.347, 95% CI: (1.048, 1.731); P = 0.0001]; being tested for HIV [COR: 2.064, 95% CI: (1.812, 2.351); P = 0.0001]; being currently employed [COR: 1.152, 95% CI: (1.011, 1.312); P = 0.032]; having community media exposure [COR: 1.992, 95% CI: (1.695, 2.341); P = 0.0001]; and being wealthy [COR: 1.567, 95% CI: (1.323, 1.856); P = 0.0001]. The above-stated variables were considered for multivariable analysis (Table 4).
Multivariable analysis on factors associated with sexually transmitted infections
The results of the multivariate analysis showed that among women, STIs were statistically and significantly associated with age group, region, religion, marital status, frequency of reading magazines, frequency of listening to radio, frequency of watching television, frequency of using the internet, history of a terminated pregnancy, contraceptive utilization, and being tested for HIV. The findings of the study demonstrated that the odds of STIs between the age range of 20–24 years [adjusted odds ratio (AOR): 1.558, 95% CI: (1.108, 2.359); P = 0.011], 25–29 years [AOR: 1.523, 95% CI: (1.089, 2.129); P = 0.014], and 30–34 years [AOR: 1.655, 95% CI: (1.191, 2.300); P = 0.003] were more likely compared to women whose ages were between 45 and 49 years old. The odds of STIs among women who were living in Denguele [AOR: 2.138, 95% CI: (1.328, 3.439); P = 0.002], Montagnes [AOR: 2.930, 95% CI: (1.909, 4.497); P = 0.0001], and Zanzan [AOR: 2.330, 95% CI: (1.476, 3.679); P = 0.0001] were more likely relative to women who were living in Abidjan. The odds of STIs among women who were married were 0.712 times less likely [AOR: 0.705, 95% CI: (0.520, 0.975); P = 0.034] relative to women who were others (divorced, widowed, and not living together). The odds of STIs among women who were Muslim were 0.785 (0.621, 0.993) times less likely [AOR: 0.785, 95% CI: (0.621, 0.993); P = 0.011] relative to other religions.
The odds of STIs among reproductive-age women who listened to radio at least once a week [AOR: 1.524, 95% CI: (1.241, 1.871); P = 0.0001]; watching television less than once a week [AOR: 1.649, 95% CI: (1.156, 2.352); P = 0.006]; and using the internet almost every day [AOR: 1.359, 95% CI: (1.081, 1.708); P = 0.008] were more likely relative to their counterparts. The odds of STIs among women with a history of a terminated pregnancy were 1.170 times more likely [AOR: 1.170, 95% CI: (1.017, 1.376); P = 0.043] compared to their counterparts. The odds of STIs among women who use modern contraceptives were 1.213 times more likely [AOR: 1.213, 95% CI: (1.032, 1.427); P = 0.0001] compared to women who didn’t use contraceptives. The odds of STIs among women who were tested for HIV were 1.342 times more likely [AOR: 1.342, 95% CI: (1.149, 1.569); P = 0.0001] compared to women who were not tested for HIV (Table 5).
Discussions
The prevalence of STIs among women was 6.82% (95% CI: 6.42%, 7.23%) in the 12 months. This finding was lower than the studies which were conducted in Swaziland (19.4%) (28), eastern India (43.6%) (29), Ethiopia (16.7%) (30), Brazil (20.2%) (31), Uganda (26.0%) (32), and Tanzania (30%) (33). This finding was higher than the studies which were conducted in Hong Kong (2.5%) (34). The variations observed in the study could be attributed to several factors, including the study period, estimation method, sample size, socioeconomic status, and geographic location are the potential causes of these variations. This could be further explained by the fact that the cross-sectional study design may influence the results, as it captures the data at a single point in time and cannot establish causal relationships (35). However, the large sample size utilized in this study strengthens the finding by providing greater statistical power and ensuring a more representative analysis of the population (36). Additionally, participants’ cultural, educational, behavioral, and sociodemographic profiles may influence their health-seeking behaviors regarding STIs (STIs) (37). Furthermore, access to media and health facilities can also play a significant role, as these factors affect individuals’ awareness, knowledge, and ability to seek care (38).
The results of the multivariate analysis showed that among women, STIs were statistically and significantly associated with age group, marital status, religion, media exposure (listening to radio, watching television, and using the internet), history of a terminated pregnancy, contraceptive utilization, and being tested for HIV.
The findings of the study demonstrated that the odds of STIs between the ages of 20 and 34 were more likely compared to women whose ages were between 45 and 49 years old. This finding was concurrent with studies that were in sub-Saharan Africa (39), South Africa (40), Uganda (41), and Bangladesh (42). Young people are at a greater risk of acquiring STIs for several reasons. Young women are often sexually active and may engage in unsafe sexual behaviors, such as having multiple partners, sex without a condom, or sex under the influence of drugs or alcohol, which increases their vulnerability to STIs. Additionally, some young people do not undergo the recommended STI tests, and many are hesitant to discuss their sexual health openly and honestly with a doctor or nurse (43). Furthermore, women at this specific childbearing age (25–34 years) may have a higher coital frequency and have unprotected sex to meet the demands of having children (44, 45).
The odds of STIs among women who were living in Denguele, Montagnes, and Zanzan were more likely relative to women who were living in Abidjan. This might be due to the variations in healthcare facilities, health-seeking behaviors, access to media, socioeconomic and sociocultural factors, knowledge, attitude, and practice toward risky sexual behaviors across the regions, which contribute to the regional differences in STIs in Ivory Coast. This can be more explained by the fact that Abidjan, Ivory Coast's economic capital, has experienced significant urbanization, with its urban population reaching 53.1% in 2023. This urban growth has led to improved infrastructure and services, offering residents better access to healthcare, education, and employment opportunities. In contrast, regions like Denguele, Montagnes, and Zanzan remain less urbanized, facing challenges such as limited healthcare facilities and fewer educational institutions (46–48).
The likelihood of STIs was lower in Muslim women compared to women of other religions. This was supported by the studies that were conducted in Saudi Arabia (49), Since extramarital sex is forbidden in Islam, women believe that religion is protecting them from STIs, which also contributes to the low-risk perception (50–53). Low-risk perceptions about STIs among Muslim women contribute to the low prevalence of STIs due to underreporting, under-detection, and under-documentation of STIs. This could be further explained by Muslim women having poor knowledge regarding STI signs and symptoms, prevention, diagnosis, and treatment, in addition to many misconceptions; negative attitudes toward people infected with HIV/AIDS were common, and attitudes were highly influenced by misconceptions and insufficient knowledge. Women with STIs often face blame and judgment, which discourages them from seeking healthcare due to confidentiality concerns (54).
The odds of STIs among women who were married were less likely relative to women who were others (widowed, divorced, and no longer living together). This finding was in line with studies which were conducted in sub-Saharan Africa (55). This might be because societal norms and expectations related to marriage, which value fidelity and monogamy, are frequently linked to marriage. These social norms have the potential to discourage women from engaging in risky behavior by discouraging extramarital affairs (56). Those social norms, rooted in religious and social beliefs such as the principle of "no sex before marriage" have the potential to discourage women from engaging in risky behaviors like extramarital affairs, thereby contributing to a low incidence of sexually transmitted infections (STIs) among married women (56). Moreover, marriage can foster emotional closeness and fulfillment, which lessens the perception of the need to pursue satisfaction through risky extramarital sex.
The odds of STIs among reproductive-age women who listened to the radio at least once a week; watching television less than once a week; and using the internet almost every day were more likely relative to their counterparts. Were more likely relative to their counterparts. This might be that some media particularly internet-mediated platforms, including social media, video-sharing sites, and online forums, can expose adolescent women to sexually explicit content. This exposure may influence their attitudes, perceptions, and behaviors related to sexual activity, potentially leading to risky sexual behaviors such as early sexual initiation, unprotected sex, and multiple sexual partners (57). Therefore, raising awareness about the proper use of media, particularly internet platforms, could be a key strategy for reducing STIs among women (58–60). In contrast to this finding, several works of literature revealed that media exposure reduces the risks of STIs among women (61–63). This could be because the symptoms of most STIs are subtle and often undetected in women. Therefore, women who had media exposure could get better information and knowledge about STIs, which increases the rate of reporting STIs (64, 65) and early diagnosis of STIs. It offers the best opportunity for effective treatment, preventing complications and reducing the further transmission of STIs (66).
When compared to their counterparts, the likelihood of STIs was higher in women who had a history of a terminated pregnancy. This finding was in line with the studies which were conducted in Ethiopia (67), China (68), Ethiopia (69, 70), and Shandong province of China (71). The scientific explanation for this could be that having a history of abortion may increase women's susceptibility to sexually transmitted infections, especially when performed unsafely by unskilled or traditional practitioners without adherence to aseptic techniques, facilitating STI transmission (26, 72). Furthermore, this might be because the fact that those women who had a history of termination of pregnancy would have better access to reproductive health care services, sexual health services, and a better understanding of the symptoms of STIs, which prevents underreporting and underscreening of STIs and contributes to high detection rates of STIs among women who had a history of a terminated pregnancy.
The odds of STIs among women who use modern contraceptives were higher compared to women who did not use contraceptives. This finding was in line with the studies which were conducted in Bangladesh (42) and India (73). This may be because most contraceptive methods (non-barrier methods) are not highly effective in preventing both pregnancy and STIs. Furthermore, we speculated that many reproductive-age women perceive the risk of pregnancy to be higher than the risk of STIs. As a result, these women often use modern contraceptives, particularly emergency contraceptives, to prevent pregnancy but engage in unprotected or unsafe sexual activities, which contributes to the high incidence of STIs among women. Additionally, the inappropriate use of barrier methods, such as condoms, results in a 21%–40% failure rate in protecting against STIs (74).
STIs among women who were tested for HIV were more likely compared to women who were not tested for HIV. This finding was supported by the studies which were conducted in sub-Saharan Africa (75). Since most STIs are asymptomatic, the reasons for these variations might be that women who were tested for HIV might have more awareness about the symptoms of HIV and other STIs, which results in a high rate of screening and self-reporting of STIs. On the other hand, women who weren’t tested for HIV might not know their status results in low self-reporting of STIs.
Conclusion
This study found that nearly seven out of a hundred reproductive-age women in Ivory Coast had sexually transmitted infections, influenced by factors such as age group, region, religion, marital status, media exposures, history of a terminated pregnancy, and contraceptive utilization. Therefore, to reduce STIs among reproductive-age women, the governments of Ivory Coast and other concerned stakeholders should give special attention to women whose ages are between 20 and 34 years old, a highly risky region, promoting the media that were broadcasting STI prevention information and creating awareness about STIs for women who had a history of a terminated pregnancy and who used modern contraceptive methods.
Strengths and limitations of this study
This study has several strengths, including the standardized Demographic and Health Survey (DHS) design and a large, representative sample which enhances the generalizability of the findings across the diverse populations. The use of nationally representative data improves the reliability of estimates and allows for a comprehensive understanding of factors associated with STIs among reproductive-age women in Ivory Coast.
However, certain limitations should be considered. Recall bias may be present in retrospective data, as participants may not accurately remember past events, making it difficult to ensure data accuracy. Additionally, the cross-sectional study design limits the ability to establish temporal or causal relationships between predictor variables and STIs among women, restricting the ability to determine whether specific predictors directly contribute to STI acquisition. Furthermore, reliance on self-reported STIs without laboratory confirmation may introduce reporting bias, as some participants may underreport or overreport their condition due to stigma, lack of awareness, or misunderstanding of symptoms. Despite these limitations, the study provides valuable insights into the factors associated with STIs among reproductive-age women and the need for targeted public health interventions to reduce the burden of STIs in this vulnerable population.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://dhsprogram.com/data/dataset_admin/index.cfm.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
GM: Conceptualization, Formal Analysis, Methodology, Validation, Writing – original draft, Writing – review & editing. BK: Data curation, Investigation, Project administration, Resources, Software, Supervision, Visualization, Writing – original draft, Writing – review & editing.
Funding
The authors declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors would like to thank Measure DHS for their permission to access the 2021 Ivory Coast Demographic and Health Survey datasets.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hazra A, Collison MW, Davis AM. CDC sexually transmitted infections treatment guidelines, 2021. Jama. (2022) 327:870–1. doi: 10.1001/jama.2022.1246
2. Low N, Broutet N, Adu-Sarkodie Y, Barton P, Hossain M, Hawkes S. Global control of sexually transmitted infections. Lancet. (2006) 368(9551):2001–16. doi: 10.1016/S0140-6736(06)69482-8
3. Peredo C. Sexually transmitted infections (STI) in Chile. Rev Medica Clin Las Condes. (2021) 32(5):611–6.
5. Kejela G, Soboka B. Assessment of knowledge, attitude and preventive practices towards sexually transmitted infections among preparatory school students in Shone Town, Southern Ethiopia, 2014. J Heal med Inf. (2015) 6(183):2. doi: 10.4172/2157-7420.1000183
8. World Health Organization (WHO). Sexually transmitted infections (STIs) fact sheet no. 110. Int (2013).
10. La Ruche G, Djéha D, Boka-Yao A, Digbeu N, Coulibaly IM. The fight against sexually transmitted diseases in Ivory Coast: what strategies can we use in the face of HIV/AIDS? Sante. (2000) 10(4):287–92.11111247
11. Diallo MO, Ettiègne-Traoré V, Maran M, Kouadio J, Brattegaard K, Makke A, et al. Sexually transmitted diseases and human immunodeficiency virus infections in women attending an antenatal clinic in Abidjan, Côte d’Ivoire. Int J STD AIDS. (1997) 8(10):636–8. doi: 10.1258/0956462971918904
12. CDC. 10 ways STDs impact women differently from men. CDC Fact Sheet (2011): p. 1. Available online at: www.cdc.gov/std/%0Ahttp://www.cdc.gov/nchhstp/newsroom/docs/STDs-Women-042011.pdf (Accessed February 13, 2024).
13. Smolarczyk K, Mlynarczyk-Bonikowska B, Rudnicka E, Szukiewicz D, Meczekalski B, Smolarczyk R, et al. The impact of selected bacterial sexually transmitted diseases on pregnancy and female fertility. Int J Mol Sci. (2021) 22(4):2170. doi: 10.3390/ijms22042170
14. World Health Organization (WHO). Global health sector strategies on, respectively, HIV, viral hepatitis and sexually transmitted infections for the period 2022–2030 (2022).
15. World Health Organization (WHO). Sexually transmitted infections: Policy brief on social determinants and health equity (2022).
16. Chersich MF, Luchters S, Reid SR. Socioeconomic and demographic factors influencing sexually transmitted infections among women. J Sex Heal. (2018).
17. THE Global Fund. Côte d’Ivoire and Global Fund launch new grants to continue fight against AIDS, TB and malaria and strengthen health systems.
18. Centers for Disease Control and Prevention. Sexually transmitted infections in developing countries. A Glance. (2007):1–6.
19. Vuylsteke B, Semdé G, Sika L, Crucitti T, Ettiègne Traoré V, Buvé A, et al. HIV and STI prevalence among female sex workers in Côte d’Ivoire: why targeted prevention programs should be continued and strengthened. PLoS One. (2012) 7(3):e32627. doi: 10.1371/journal.pone.0032627
20. World Health Organization. Sexually transmitted infections: implementing the Global STI Strategy (2017). Available online at: https://www.WhoInt/Publications/I/Item/Sexually-Transmitted-Infections-Implementing-the-Global-Sti-Strategy (Accessed August 15, 2024).
21. Peltzer K, Pengpid S, Tiembre I. Mental health, childhood abuse and HIV sexual risk behaviour among university students in Ivory Coast. Ann Gen Psychiatry. (2013) 12(1):18. doi: 10.1186/1744-859X-12-18
22. Vuylsteke B, Semde G, Sika L, Crucitti T, Ettiegne Traore V, Buve A, et al. High prevalence of HIV and sexually transmitted infections among male sex workers in Abidjan, Cote d’Ivoire: need for services tailored to their needs. Sex Transm Infect. (2012) 88(4):288–93. doi: 10.1136/sextrans-2011-050276
23. Namey E, Perry B, Headley J, Yao AK, Ouattara ML, Shighata C, et al. Understanding the financial lives of female sex workers in Abidjan, Côte d’Ivoire: implications for economic strengthening interventions for HIV prevention. AIDS Care. (2018) 30(Suppl 3):6–17. doi: 10.1080/09540121.2018.1479031
24. UNAIDS. Côte d’Ivoire : epidemiological fact sheets on HIV/AIDS and sexually transmitted diseases (2004). Available online at: http://data.unaids.org/publications/fact-sheets01/cotedivoire_en.pdf (Accessed August 27, 2024).
25. Chedid C, Arikawa S, Messou E, Tiendrebeogo T, Horo A, Zahui A, et al. High prevalence of RTIs/STIs among HIV-positive women on ART: the WETIV-R cohort study in Abidjanuary, Ivory Coast (2018).
28. Ginindza TG, Stefan CD, Tsoka-Gwegweni JM, Dlamini X, Jolly PE, Weiderpass E, et al. Prevalence and risk factors associated with sexually transmitted infections (STIs) among women of reproductive age in Swaziland. Infect Agent Cancer. (2017) 12(1):1–12. doi: 10.1186/s13027-017-0140-y
29. Das S, Dasgupta A. Community based study of reproductive tract infections among women of the reproductive age group in a rural community of eastern India. Int J Community Med Public Heal. (2018) 6(1):330. doi: 10.18203/2394-6040.ijcmph20185268
30. Asres AW, Endalew MM, Mengistu SY. Prevalence and trends of sexually transmitted infections among pregnant women in Mizan Tepi University Teaching Hospital, Southwest Ethiopia: a cross-sectional study. Pan Afr Med J. (2022) 42:111. doi: 10.11604/pamj.2022.42.111.30871
31. Soledade M, Benedetti G, Miranda LD, Higa SN, Stella A, Nogami A, et al. Sexually transmitted infections in women deprived of liberty in Roraima, Brazil. Rev Saude Publica. (2020) 54:105. doi: 10.11606/s1518-8787.2020054002207
32. Masanja V, Wafula ST, Ssekamatte T, Isunju JB, Mugambe RK, Van Hal G. Trends and correlates of sexually transmitted infections among sexually active Ugandan female youths: evidence from three demographic and health surveys, 2006–2016. BMC Infect Dis. (2021) 21(1):59. doi: 10.1186/s12879-020-05732-x
33. Masatu ES, Kajura A, Mujuni F, Chibwe E, Nyawale HA, Rambau P, et al. High prevalence of sexually transmitted infections among asymptomatic women opting for the intrauterine contraceptive device use in Mwanza, Tanzania: an urgent call for control interventions. SAGE Open Med. (2022) 10: 20503121221097536. doi: 10.1177/20503121221097536
34. Wong WCW, Tucker JD, Man HK, Emch M, Yang LG, Zhao Y. Prevalence and contextual risk factors of sexually transmitted infections in Hong Kong: abridged secondary publication. Hong Kong Med J. (2021) 27(3):1–4.
35. Wang X, Cheng Z. Cross-sectional studies: strengths, weaknesses, and recommendations. Chest. (2020) 158(1S):S65–71. doi: 10.1016/j.chest.2020.03.012
36. Andrade C. Sample size and its importance in research. Indian J Psychol Med. (2020) 42(1):102–3. doi: 10.4103/IJPSYM.IJPSYM_504_19
37. Johnson K, Lee H. Socioeconomic status and health outcomes: examining the role of geographic location and access to healthcare. Health Econ Rev. (2019).
38. Davis T, Miller P, Clark L. Media access and healthcare utilization: bridging the gap in sexual health awareness. J Health Commun. (2021).
39. Dadzie LK, Agbaglo E, Okyere J, Aboagye RG, Arthur-Holmes F, Seidu AA, et al. Self-reported sexually transmitted infections among adolescent girls and young women in sub-Saharan Africa. Int Health. (2022) 14(6):545–53. doi: 10.1093/inthealth/ihab088
40. Francis SC, Mthiyane TN, Baisley K, Mchunu SL, Ferguson JB, Smit T, et al. Prevalence of sexually transmitted infections among young people in South Africa: a nested survey in a health and demographic surveillance site. PLoS Med. (2018) 15(2):e1002512. doi: 10.1371/journal.pmed.1002512
41. Rutaremwa G, Agaba P, Nansubuga EA, Nankinga O. Association between risky sexual behaviour and having STIs or HIV among young persons aged 15–24 years in Uganda. PaaConfexCom. (2015):1–18. Available online at: https://www.google.com/search?q=Association+between+Risky+Sexual+Behaviour+and+having+STIs+or+HIV+among+young+persons+aged+15-24+years+in+Uganda&rlz=1C1RLNS_enNG864NG864&oq=Association+between+Risky+Sexual+Behaviour+and+having+STIs+or+HIV+among+young+pers
42. Huda MN, Ahmed MU, Uddin MB, Hasan MK, Uddin J, Dune TM. Prevalence and demographic, socioeconomic, and behavioral risk factors of self-reported symptoms of sexually transmitted infections (STIs) among ever-married women: evidence from nationally representative surveys in Bangladesh. Int J Environ Res Public Health. (2022) 19(3):1906. doi: 10.3390/ijerph19031906
43. Kaestle CE, Morisky DE, Wiley DJ. Sexual intercourse and the age difference between adolescent females and their romantic partners. Perspect Sex Reprod Health. (2002) 34(6):304. doi: 10.2307/3097749
44. Gaskins AJ, Sundaram R, Buck Louis GM, Chavarro JE. Predictors of sexual intercourse frequency among couples trying to conceive. J Sex Med. (2018) 15(4):519–28. doi: 10.1016/j.jsxm.2018.02.005
45. Konishi S, Saotome TT, Shimizu K, Oba MS, O’Connor KA. Coital frequency and the probability of pregnancy in couples trying to conceive their first child: a prospective cohort study in Japan. Int J Environ Res Public Health. (2020) 17(14):4985. doi: 10.3390/ijerph17144985
47. Sehi GT, Houngbedji CA, Parker DM, Macharia PM. Geographic accessibility to public healthcare facilities and spatial clustering during the wet and dry seasons in Cote d’Ivoire. medRxiv. Rxiv:2023.11.21.23298865 (2023). Available online at: http://medrxiv.org/content/early/2023/11/22/2023.11.21.23298865.abstract (Accessed March 22, 2025).
49. Alomair N, Alageel S, Davies N, Bailey JV. Muslim women’s perspectives on the barriers to sexually transmitted infections testing and diagnosis in Saudi Arabia. Front Public Heal. (2023) 11:1248695. doi: 10.3389/fpubh.2023.1248695
50. Hearld KR, Wu D, Budhwani H. HIV testing among Muslim women in the United States: results of a national sample study. Health Equity. (2021) 5(1):17–22. doi: 10.1089/heq.2020.0041
51. DeJong J, Shepard B, Roudi-Fahimi F, Ashford L. Young people’s sexual and reproductive health in the Middle East and North Africa. Reprod Heal. (2007) 14(78):8.
52. Abu-Raddad LJ, Hilmi N, Mumtaz G, Benkirane M, Akala FA, Riedner G, et al. Epidemiology of HIV infection in the Middle East and North Africa. AIDS. (2010) 24:S5–23. doi: 10.1097/01.aids.0000386729.56683.33
53. Abdullah A, Mark H. A mixed methods study of the factors associated with HIV testing among young people in Saudi Arabia. J AIDS HIV Res. (2018) 10(6):96–102. doi: 10.5897/JAHR2017.0446
54. Alomair N, Alageel S, Davies N, Bailey JV. Sexually transmitted infection knowledge and attitudes among Muslim women worldwide: a systematic review. Sex Reprod Heal Matters. (2020) 28(1):1731296. doi: 10.1080/26410397.2020.1731296
55. Tenkorang EY. Marriage, widowhood, divorce and HIV risks among women in sub-Saharan Africa. Int Health. (2014) 6(1):46–53. doi: 10.1093/inthealth/ihu003
57. Lin WH, Liu CH, Yi CC. Exposure to sexually explicit media in early adolescence is related to risky sexual behavior in emerging adulthood. PLoS One. (2020) 15(4):e0230242. doi: 10.1371/journal.pone.0230242
58. Juyani AK, Zarei F, Maasoumi R. Efficacy of mobile-based educational intervention using instructional systems design in promoting preventive behaviors for sexually transmitted infections among Iranian women: a randomized controlled trial. BMC Public Health. (2024) 24(1):510. doi: 10.1186/s12889-024-18002-1
59. Scull TM, Dodson CV, Evans-Paulson R, Reeder LC, Geller J, Stump KN, et al. Evaluating the mechanisms and long-term effects of a web-based comprehensive sexual health and media literacy education program for young adults attending community college: study protocol for a three-arm randomized controlled trial. Trials. (2022) 23(1):521. doi: 10.1186/s13063-022-06414-6
60. Swanton R, Allom V, Mullan B. A meta-analysis of the effect of new-media interventions on sexual-health behaviours. Sex Transm Infect. (2015) 91(1):14–20. doi: 10.1136/sextrans-2014-051743
61. Parra LA, Hastings PD. Integrating the neurobiology of minority stress with an intersectionality framework for LGBTQ-Latinx populations. New Dir Child Adolesc Dev. (2018) 2018(161):57–70.29972624
62. Huda M, Sikder A, Rahman M, Mohiuddin M, Islam MS. Access to mass media and awareness of sexually transmitted diseases (STDs) among the truck drivers in Dhaka city: do mass media make them aware? South Asian J Soc Sci. (2016) 1(1):1–16.
63. Maviso M, Kalembo FW. Prevalence and determinants of not testing for HIV among young adult women in Papua New Guinea: findings from the demographic and health survey, 2016–2018. BMJ Open. (2024) 14(3):e075424–10. doi: 10.1136/bmjopen-2023-075424
64. Patel VV, Masyukova M, Sutton D, Horvath KJ. Social media use and HIV-related risk behaviors in young Black and Latino gay and bi men and transgender individuals in New York City: implications for online interventions. J Urban Health. (2016) 93(2):388–99. doi: 10.1007/s11524-016-0025-1
65. Vermund SH, Geller AB, Crowley JS. Sexually transmitted infections. Sex Transm Infect. (2020):1–750.31959704
67. Chernet A, Yesuf A, Alagaw A. Seroprevalence of hepatitis B virus surface antigen and factors associated among pregnant women in Dawuro zone, SNNPR, Southwest Ethiopia: a cross sectional study. BMC Res Notes. (2017) 10:1–5. doi: 10.1186/s13104-017-2702-x
68. Dong Y, Zhang H, Wang Y, Tao H, Xu S, Xia J, et al. Multiple abortions and sexually transmitted infections among young migrant women working in entertainment venues in China. Women Health. (2015) 55(5):580–94. doi: 10.1080/03630242.2015.1022811
69. Birhane BM, Simegn A, Bayih WA, Chanie ES, Demissie B, Yalew ZM, et al. Self-reported syndromes of sexually transmitted infections and its associated factors among reproductive (15–49 years) age women in Ethiopia. Heliyon. (2021) 7(7):e07524. doi: 10.1016/j.heliyon.2021.e07524
70. Zenebe MH, Mekonnen Z, Loha E, Padalko E. Prevalence, risk factors and association with delivery outcome of curable sexually transmitted infections among pregnant women in Southern Ethiopia. PLoS One. (2021) 16(3):e0248958. doi: 10.1371/journal.pone.0248958
71. Chen S, van den Hoek A, Shao C, Wang L, Liu D, Zhou S, et al. Prevalence of and risk indicators for STIs among women seeking induced abortions in two urban family planning clinics in Shandong province, People’s Republic of China. Sex Transm Infect. (2002) 78:e3. doi: 10.1136/sti.78.3.e3
73. Shabnam S. Sexually transmitted infections and spousal violence: the experience of married women in India. Indian J Gend Stud. (2017) 24(1):24–46. doi: 10.1177/0971521516678530
74. Cates WJ, Stone KM. Family planning, sexually transmitted diseases and contraceptive choice: a literature update–part I. Fam Plann Perspect. (1992) 24(2):75–84. doi: 10.2307/2135469
Keywords: prevalence, sexually transmitted infections, Ivory Coast, reproductive, women
Citation: Mankelkl G and Kinfe B (2025) Factors associated with sexually transmitted infections among reproductive age women in Ivory Coast: evidenced by 2021 Ivory Coast Demographic and Health Survey. Front. Glob. Women's Health 6:1490762. doi: 10.3389/fgwh.2025.1490762
Received: 3 September 2024; Accepted: 31 March 2025;
Published: 2 May 2025.
Edited by:
Pooja Chitneni, Brigham and Women's Hospita and Harvard Medical School, United StatesReviewed by:
Erick Kiprotich Yegon, Jomo Kenyatta University of Agriculture and Technology, KenyaAlison Footman, AVAC, United States
Copyright: © 2025 Mankelkl and Kinfe. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gosa Mankelkl, Z29zYTEyMjAxbEBnbWFpbC5jb20=
 Gosa Mankelkl
Gosa Mankelkl Beletu Kinfe
Beletu Kinfe