- 1Department of Human Anatomy, School of Medicine, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 2Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 3Departments of Health Informatics, Teda Health Science College, Gondar, Ethiopia
- 4Department of Human Physiology, School of Medicine, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 5Department of General Midwifery, School of Midwifery, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 6Department of Reproductive Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 7Department of Internal Medicine, School of Medicine, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 8Department of Anesthesia, School of Medicine, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 9Department of Optometry, School of Medicine, University of Gondar, Comprehensive Specialized Hospital, Gondar, Ethiopia
- 10Department of Health Informatics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 11Department of Medical Nursing, Teda Health Science College, Gondar, Ethiopia
Background: Maternal health is crucial for women's well-being during pregnancy, childbirth, and postpartum. Antenatal care (ANC) is essential for monitoring health and preventing complications, yet only 35.5% of women in low- and middle-income regions attend the recommended ANC visits. This study explores the socioeconomic and regional factors influencing ANC visits in Senegal.
Methods: Data from the 2023 Senegal Demographic and Health Survey (DHS) on maternal health were analyzed. A stratified two-stage sampling design selected 400 enumeration areas, and 4,543 women aged 15–49 participated. Independent variables included age, education, wealth, healthcare access, and region. Multilevel Poisson regression in Stata 17 was used to assess factors affecting ANC visits, considering both individual and community-level variables to examine regional disparities and healthcare access.
Results: Among the 4,543 women, 97.63% attended at least one ANC visit, but only 7.69% completed eight or more. Wealth, media access, education, and regional location significantly influenced ANC attendance. Women from middle-income households attended 6% more visits (AIRR: 1.06, 95% CI: 1.02–1.11), and those from wealthy households attended 8% more (AIRR: 1.08, 95% CI: 1.03–1.14). Women with media access attended 11% more visits (AIRR: 1.11, 95% CI: 1.06–1.15). Regional disparities were evident, with women in Thiès (AIRR: 0.80, 95% CI: 0.73–0.87), Matam (AIRR: 0.83, 95% CI: 0.75–0.92), and Kédougou (AIRR: 0.83, 95% CI: 0.75–0.91) attending fewer visits compared to those in Dakar.
Conclusions: This study identifies significant socioeconomic and regional disparities in ANC utilization in Senegal. Wealth, education, media access, and regional location strongly influence ANC attendance. Targeted policies focusing on maternal health education, healthcare infrastructure, and financial support, particularly in underserved areas, are necessary to improve ANC access and maternal and child health outcomes.
Introduction
Maternal health is the cornerstone of public health, encompassing women's well-being during pregnancy, childbirth, and postpartum while prioritizing safety for both mother and child (1). A core component of maternal health is antenatal care (ANC), which the World Health Organization (WHO) defines as “care provided by skilled healthcare professionals to pregnant women and adolescent girls to ensure the best health conditions for both mother and baby” (2).
ANC involves routine check-ups to monitor mother and fetus health, allowing for early complication detection and providing crucial health education on pregnancy and parenting (3). Moreover, ANC contacts offer critical guidance on nutrition, vaccinations, screenings, and emotional support while facilitating timely referrals to specialized care when necessary (4).
WHO envisions a world where every pregnant woman and newborn has access to quality care throughout pregnancy, childbirth, and the postnatal period (5). To achieve this, it advocates for high-quality ANC services as part of a broader global goal toward equitable, people-centered universal health coverage (5). Despite these efforts, approximately 15% of pregnancies experience life-threatening complications requiring immediate skilled intervention (6).This statistic is especially troubling in low- and middle-income countries, where complications during pregnancy and childbirth are leading causes of death and disability among reproductive-age women (7).
Multiple studies have demonstrated a positive correlation between ANC visits and improved maternal and neonatal health outcomes. Research indicates that increased ANC visits reduce both maternal and neonatal morbidity (8) and mortality (9–11). For instance, a single ANC visit is associated with a 1.04% reduction in neonatal mortality and a 1.07% reduction in infant mortality. Achieving at least four ANC visits with one provided by a skilled healthcare professional further decreases these risks by an additional 0.56% and 0.42%, respectively. Moreover, a single ANC visit lowers the probability of low birth weight by 3.82%, while additional visits reduce risks of stunting and underweight by 4.11% and 3.26%, respectively (12). While ANC visits improve health outcomes, their effectiveness also depends on the quality of care, including the healthcare provider's skills and the availability of essential services (13).
Unfortunately, only 35.5% of pregnant women in low- and middle-income regions attend ANC at least four times, often due to financial barriers, limited facility access, and lack of awareness. Socioeconomic status, parental education, rural residence, and maternal age also affect ANC attendance, highlighting the urgent need for improved community awareness and strengthened health education programs (14). In many developing countries, maternal mortality persists as a significant public health challenge despite global initiatives. In sub-Saharan Africa, approximately 66% of global maternal deaths occur, with persistently high maternal mortality ratios despite national health insurance and safe motherhood efforts (15). Globally, ANC has proven to be an effective intervention for reducing maternal and infant mortality rates, aligning with Sustainable Development Goal (SDG) 3.1, which aims to reduce maternal mortality to below 70 per 100,000 live births by 2030 (16, 17).
In Senegal, ANC utilization has improved over recent years, thanks to government and organizational efforts to increase access to maternal health services, particularly in rural areas. Policies such as the Maternal Mortality Prevention Program (1990) and the Health Policy (1995) prioritize maternal and reproductive health, aligning with international goals to reduce maternal and neonatal mortality (18). However, barriers to adequate ANC remain, particularly due to the out-of-pocket costs for essential services like diagnostic tests and medications, which limit access for many women in low-income settings (19).
Furthermore, while nearly all pregnant women in Senegal attend at least one ANC visit, only about half complete the minimum recommended four visits. This highlights a quality gap in ANC, with counseling and education often insufficient or entirely lacking (20). To improve maternal and neonatal outcomes, the WHO now advises increasing ANC contacts to at least eight, beginning in the first trimester and continuing throughout the pregnancy (2, 21). Yet, financial difficulties, limited transportation, and sociocultural factors still hinder full ANC attendance, particularly in underserved regions (22–24).
This study analyzes 2023 Demographic and Health Survey (DHS) data to identify factors influencing ANC attendance in Senegal, with emphasis on socioeconomic and regional disparities. Through multilevel Poisson regression analysis, it aims to reveal barriers to ANC utilization, offering insights for policy and resource allocation to improve maternal health and support global health goals.
Methods
Study area, data source, and study period
Senegal is located in West Africa, bordered by the Atlantic Ocean to the west and sharing land borders with Mauritania, Mali, Guinea, Guinea-Bissau, and surrounding The Gambia. With a population of over 17 million people as of 2023, Senegal is classified as a low- to middle-income country, with considerable socioeconomic disparities and a predominantly young population. The GDP per capita was reported at approximately $1,641 USD in 2023, reflecting gradual economic growth but with many citizens still living under the poverty line (25).
Administratively, Senegal is divided into 14 regions, each with distinct geographic, cultural, and economic characteristics. These regions include Dakar, Diourbel, Fatick, Kaffrine, Kaolack, Kédougou, Kolda, Louga, Matam, Saint-Louis, Sédhiou, Tambacounda, Thiès, and Ziguinchor. The capital, Dakar, located on the Cape Verde Peninsula, is the country's economic and political hub and exhibits high levels of urbanization. In contrast, other regions, such as Kolda and Sédhiou, are more rural and agrarian, with less developed infrastructure and access to healthcare services (26).
This study utilizes secondary data from the Senegal Demographic and Health Survey 2023. Conducted every five years, the DHS is designed to provide updated health indicators across the country, particularly in the areas of maternal and child health, family planning, vaccination, and healthcare utilization. Data collection for the 2023 survey was a collaborative effort led by the Agence Nationale de la Statistique et de la Démographie (ANSD) with technical assistance from USAID's DHS Program (27).
Sampling and study population
The 2023 Senegal DHS used a stratified two-stage sampling design. In the first stage, 400 enumeration areas were selected independently for urban and rural strata, comprising 186 urban and 214 rural areas. In the second stage, households within these areas were systematically chosen from household listings.
Several datasets were available, including men's (MR), women's (IR), children's (KR), births (BR), and household (HR) records. For this study, the analysis focused on children's data (KR file), capturing a sample of 4,853 women aged 15 to 49.
The final analysis included women aged 15–49 who reported at least one pregnancy within five years prior to the survey. Cases with incomplete data on ANC attendance, socioeconomic factors, or key variables were excluded, yielding a weighted sample of 4,543 women. This sample size supports robust analysis of factors affecting ANC visits across individual and community levels.
Study variables
The study's dependent variable is antenatal care attendance, defined as the number of ANC visits each participant attended during her most recent pregnancy. Originally recorded as a range from 0 to 18 visits, ANC visits were recoded to categorize responses as follows: 0 up to 7 visits (i.e., 1, 2, 3 … 7), and ≥8 visits.
The independent variables are categorized into socio-demographic, family and reproductive, and community and health access factors. Socio-demographic factors include age (categorized into age groups: 15–24, 25–34, 35–44, and over 44), women's education level (no education, primary, secondary, or higher), maternal working status (employed or not), husband's education level (no education, primary, secondary and above, or unknown), wealth index (poor, middle, or rich), and household media exposure (access or no access). Family and reproductive factors comprise pregnancy planning status (planned or unplanned), the number of children (0, 1–2, 3–4, or 5 or more), history of terminated pregnancies (yes or no), and autonomy in healthcare decision-making (yes or no). Finally, community and health access factors include distance to a health facility (perceived as a barrier or not), residence type (urban or rural), and region (administrative regions such as Dakar, Ziguinchor, Diourbel, Saint-Louis, among others). These independent variables provide a comprehensive view of both individual and community-level factors potentially influencing ANC utilization in Senegal.
Data management
This study utilized data from the Demographic and Health Surveys program, which can be accessed at https://www.dhsprogram.com, focusing on outcome and independent variables from the Children's Recode (KR) dataset. Data extraction, coding, and analysis were carried out using Stata version 17, incorporating weighted data (v005) to ensure representativeness at the national level. To enhance accuracy, variables with over 5% missing values or those deemed irrelevant were excluded during data cleaning and preparation.
Method of data analysis
Researchers often face theoretical challenges when analyzing count variables, which represent the frequency of event occurrences within a given timeframe (e.g., 0, 1, 2, etc.). As count variables can't be negative, they are limited to non-negative integers, including zero (28).
The Poisson regression model is a primary tool for analyzing count data, representing count outcomes as functions of one or more independent variables. This model assumes that observations are independent over time and that the mean and variance of the dependent variable are equal.
Goodness-of-fit tests confirmed the model's adequacy, with a deviance statistic of 3207.311 and a Pearson statistic of 2774.969, both showing p-values of 1.000, which indicates a strong fit. The data's mean was 4.24, and the variance was 3.96, resulting in a mean-to-variance ratio of approximately 1.07. This near equivalence supports the equi-dispersion assumption, justifying the use of the Poisson model. Given these results, we applied the Poisson model to interpret predictor effects on ANC visits, while monitoring for any influential observations or residual patterns (29).
The analysis included four model stages. First, a null model (without exposure variables) was used to assess random effects and the feasibility of multi-level modeling. The second model (Model II) introduced individual-level variables to assess their effects on ANC visits. The third model (Model III) added community-level variables, examining the impact of factors such as healthcare access and residence type on ANC visits. The final model (Model IV) combined both individual and community-level factors to evaluate their combined influence on ANC utilization. The multilevel Poisson regression equation used is (30, 31):
Where: λit, represents the expected number of ANC visits for individual i in community t, Xit, denotes the fixed effects of individual-level covariates (such as age, education, and employment status), and Zi reflects the random effects of community-level covariates (such as region and access to healthcare). Additionally, is the random intercept for community i, which accounts for unobserved heterogeneity between communities, while represents the residual error term for individual i in community t.
Fixed effects were used to estimate associations between covariates and ANC visits, with variables having p-values ≤ 0.20 included in the final model. The adjusted incident rate ratio (AIRR) was presented as the primary measure, with significance set at p < 0.05. Random effects evaluated barriers across communities using metrics like the intra-class correlation coefficient (ICC), median incident rate ratio (MIRR), and proportional change in variance (PCV) (32). The variance inflation factor (VIF), with a mean of 4.61, confirmed low multicollinearity. Finally, the model comparison selected the model with the lowest deviance as the best fit.
Operational definitions
The number of antenatal care visits indicates how many times women, who gave birth in the five years leading up to the survey, received prenatal care for their most recent birth (2).
Autonomy in healthcare decision-making refers to the ability of individuals to make informed choices about their own health and medical care without undue influence or coercion. It emphasizes the importance of personal agency, allowing individuals to express their preferences and take an active role in decisions affecting their health and treatment options (33).
Results
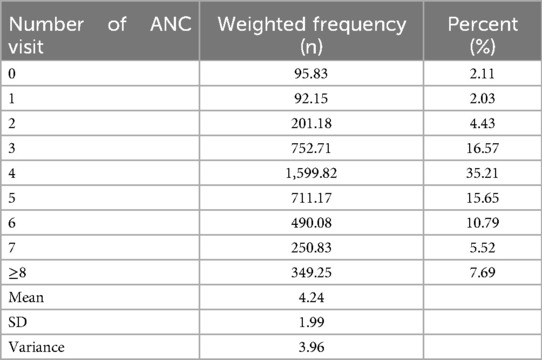
In a weighted sample of 4,543 pregnant women, the median and mode number of antenatal care visits during pregnancy were four among those who had given birth in the last five years. Overall, 97.63% of women attended at least one ANC visit (95% CI: 0.97, 0.98), and 74.86% received four or more visits (95% CI: 0.72, 0.75) in Senegal. However, only 7.69% of women completed eight or more ANC visits (Table 1).
The respondents' mean age was 29.07 years (SD ± 6.91), with most women aged 25–34 years (44.83%), followed by those 15–24 years (30.43%). Women aged 35–44 accounted for 23.48%, while only 1.26% were over 44. In terms of education, over half (54.84%) had no formal education, while 25.66% had secondary education or higher. Among their husbands, 60.67% had no education, with 17.09% reaching secondary level or above.
Regarding wealth status, 46.55% of the women were in the poor category, 34.03% in the rich, and the rest in the middle-income group. Media access was high, with 87.46% of households having access, while 12.54% lacked it.
Most women had 1–2 children (44.91%), while 30.73% had 3–4 children, and 23.66% had five or more. Only 0.70% were childless. Additionally, 17.86% had experienced a pregnancy loss. For healthcare decision-making, 67.94% of women lacked autonomy, with only 32.06% able to make independent healthcare choices.
A majority (58.15%) reported that distance to healthcare facilities was not a barrier. Most women lived in rural areas (62.11%), while 37.89% resided in urban settings. Regional representation was highest in Dakar (18.32%), followed by Thiès (14.07%) and Diourbel (11.27%), with the lowest in Kédougou (1.42%) and Sédhiou (3.66%) (Table 2).
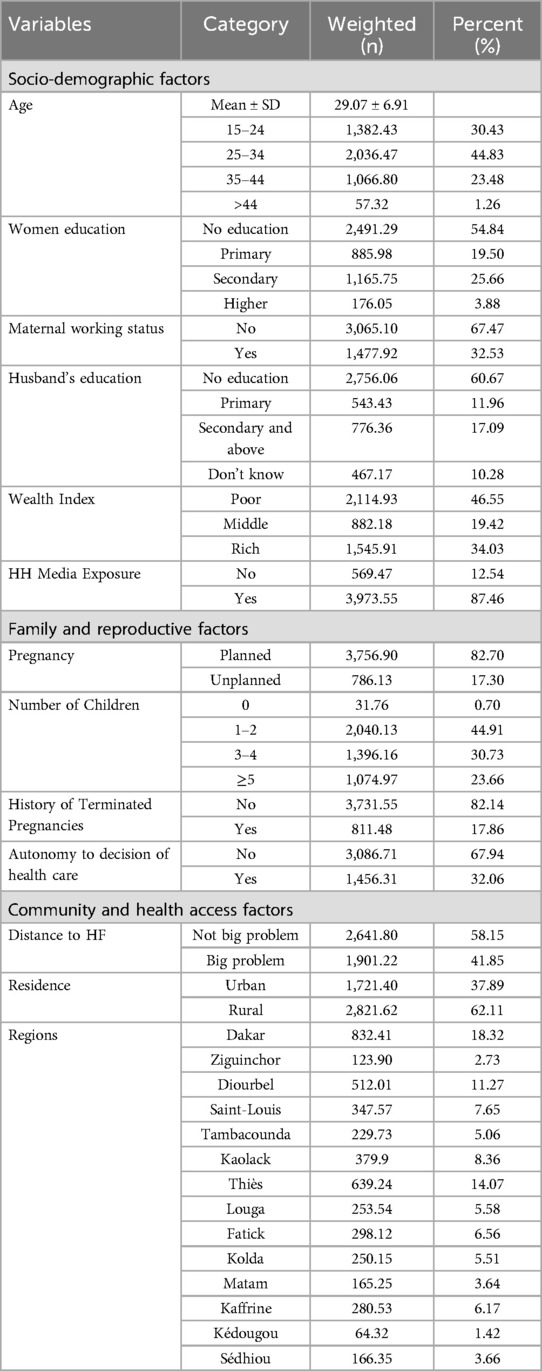
Table 2. Socio-demographic characteristics of women who gave birth within the last five years preceding the survey in Senegal, SDHS 2023 (N = 4,543).
Multilevel poisson regression analysis
Random effect, fixed effect and model fitness
Analyzing both fixed and random effects ensures comprehensive insights into ANC utilization. Fixed effects identify individual predictors, while random effects uncover contextual variations across clusters. Together, they integrate personal and structural influences, providing robust conclusions about factors affecting ANC visits at both individual and broader contextual levels.
Following an assessment of multiple count models, the mixed-effects Poisson regression model was selected as the best fit due to the sample's characteristics: the mean number of antenatal care visits (4.24) slightly exceeded the variance (3.96), and the Likelihood Ratio (LR) test yielded a highly significant p-value (<0.0001). Additionally, we evaluated for excess zeros to determine if zero-inflated models might be more appropriate, though none proved necessary.
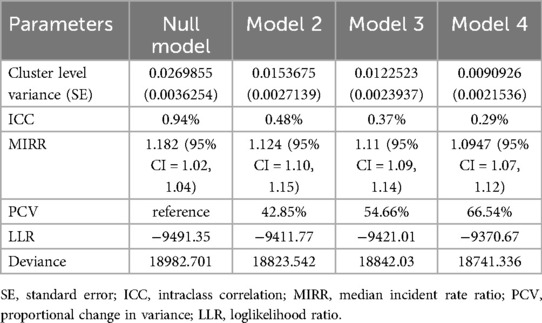
To assess clustering effects, we calculated several measures of variability. The intra-class correlation coefficient indicated that only 0.94% of the total variability in ANC visits was due to cluster effects (Table 3). While this small cluster effect often suggests that a standard Poisson regression model could be enough (with a log-likelihood ratio of −9452.41), we conducted further analysis to ensure robustness (34). A likelihood ratio test comparing the multilevel model to the standard model produced a chi-squared statistic with a p-value of <0.001, supporting the multilevel model by rejecting the null hypothesis of no between-cluster variability in ANC visit rates.
The Median Incident Rate Ratio (MIRR) provided additional insights into cluster-level variation, measuring the median relative difference in ANC visit rates between high- and low-visit clusters. A significant MIRR of 1.18 (95% CI: 1.02–1.04) affirmed that the multilevel model captured meaningful variation beyond the standard model (35).
We further evaluated the Percent Change in Variance (PCV) to quantify the variation explained by individual- and cluster-level factors. The deviance test, with values progressively decreasing from the null model to Model IV, confirmed Model IV as the best fit. The final model explained approximately 66.54% of the total variability in ANC visits, underscoring its effectiveness (Table 3).
In the final model, several factors were significantly associated with the frequency of ANC visits in Senegal, with wealth status, household media exposure, husband's education, and regional location playing key roles (Table 4).
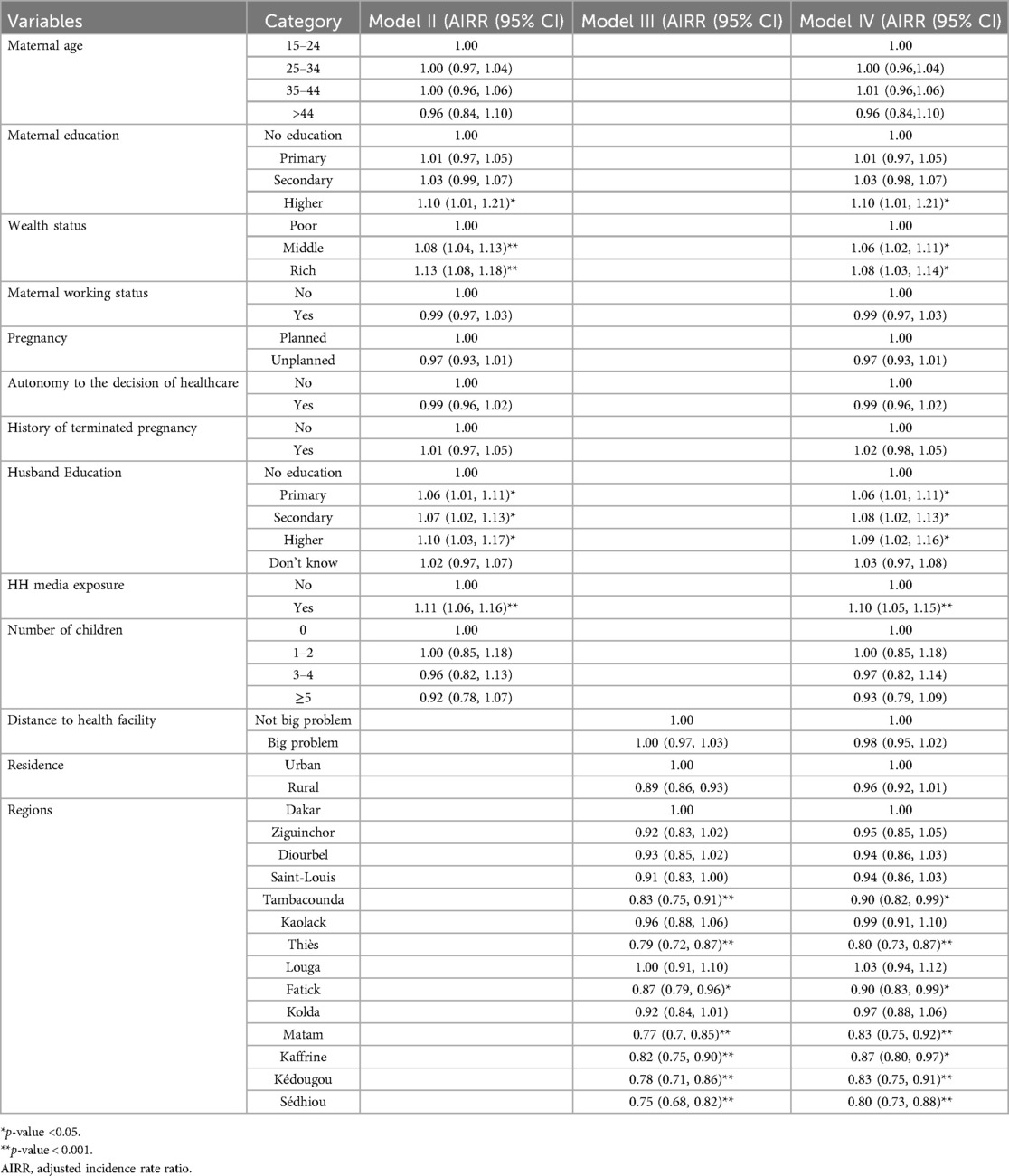
Table 4. Multilevel poisson regression on the number of antenatal care visits among women who gave birth within the last five years preceding the survey in Senegal, SDHS 2023.
Women from middle- and high-income households attended significantly more ANC visits compared to those from poorer households. Specifically, women in middle-income households had a 6% higher rate of ANC visits (AIRR: 1.06, 95% CI: 1.02–1.11), while women in high-income households had an 8% higher rate of visits (AIRR: 1.08, 95% CI: 1.03–1.14). Additionally, women in households with media exposure had 11% more ANC visits than those without media access (AIRR: 1.11, 95% CI: 1.06–1.15).
Educational attainment also influenced ANC attendance. Women with higher education had 10% more ANC visits compared to those with no formal education. The husband's education was also positively associated with ANC attendance: women whose husbands had a primary education attended 6% more ANC visits (AIRR: 1.07, 95% CI: 1.01–1.11), those whose husbands completed secondary education attended 8% more visits (AIRR: 1.08, 95% CI: 1.02–1.13), and women with husbands who attained higher education had 9% more visits (AIRR: 1.09, 95% CI: 1.02–1.16), all compared to women with husbands who had no formal education.
Regional disparities were observed. Women in the Thiès region were 20% less likely to attend ANC visits (AIRR: 0.80, 95% CI: 0.73–0.87), and those from Matam (AIRR: 0.83, 95% CI: 0.75–0.92), Kédougou (AIRR: 0.83, 95% CI: 0.75–0.91), and Sédhiou (AIRR: 0.80, 95% CI: 0.73–0.88) also had significantly fewer visits. Additionally, women from Tambacounda (AIRR: 0.90, 95% CI: 0.82–0.99) and Fatick (AIRR: 0.90, 95% CI: 0.83–0.99) showed a lower likelihood of attending ANC visits compared to those residing in Dakar.
Discussions
Antenatal care is a critical indicator of maternal healthcare, essential for reducing maternal and child mortality and supporting global health objectives (36). In this study, 97.63% of Senegalese women attended at least one ANC visit (95% CI: 0.97, 0.98), with 72.39% achieving the minimum four visits (95% CI: 0.71, 0.74). However, only 7.69% met the WHO-recommended eight visits, a rate higher than Gabon (3.66%) but lower than Nigeria (19.17%) and consistent with sub-Saharan Africa's average (8.9%) (37, 38).
Since 2016, WHO guidelines recommend eight ANC contacts to reduce perinatal mortality and improve care experiences (39). This analysis, using multilevel Poisson regression and recent national data, highlights ANC utilization gaps in Senegal, influenced by factors such as maternal and partner education, wealth index, media exposure, and geographic region.
This study shows that women with higher education were 10% more likely to attend ANC visits than those without formal education, emphasizing the positive role of education in maternal healthcare utilization. This association between education and ANC attendance is well-documented across various countries, including Senegal (40), Ghana (41), Cameroon (42), Zambia (43), Uganda (44), Ethiopia (45), Bangladesh (46), Nepal (47), East Africa (48), and Sub-Saharan Africa (49).
Increased educational attainment in low- and middle-income countries (LMICs) often correlates with better health outcomes and healthcare access. Educated women tend to have greater autonomy, health literacy, and decision-making power, leading to higher ANC attendance through improved awareness of prenatal care, as well as overcoming logistical and financial barriers (36, 43, 47, 48).
Additionally, this study found that a husband's education level also influences women's ANC attendance. Women whose husbands had primary education were 6% more likely to attend ANC visits, with this likelihood rising to 8% and 9% when husbands had secondary or higher education. This underscores the supportive role that educated husbands can play in maternal healthcare, as seen in studies from Ethiopia (50), Nepal (51, 52), Indonesia (53), Pakistan (50), East Africa (54), and Sub-Saharan Africa (55, 56).
Educated husbands are generally more aware of the benefits of maternal healthcare, and they provide both financial and logistical support. They often prioritize healthcare spending and encourage their wives to seek timely care, particularly in patriarchal societies where men frequently make household healthcare decisions (57–59).
Women from middle-income households are 6% more likely, and those from high-income households 8% more likely, to attend ANC visits compared to women from low-income households, suggesting that financial resources in these households mitigate barriers like transportation costs, clinic fees, and time off work, promoting consistent ANC attendance (60). Studies from Angola (61), Ethiopia (36, 49), Guinea (62), Ghana (63), Nigeria (3), Sub-Saharan Africa (49), Nepal (64) reinforce this association, highlighting that economic stability enhances ANC use by improving health information access, covering expenses, and fostering autonomy in health decisions.
In Senegal, however, the income-related increase in ANC attendance is relatively modest (6% for middle-income and 8% for high-income households), likely due to additional factors facilitating ANC access across income groups. Senegal's healthcare infrastructure, with extensive facilities, shorter travel distances, and affordable or free transport, fosters more equitable access (65, 66). Although ANC services are not entirely free, essential services like malaria prophylaxis, anti-tetanus vaccinations, and HIV testing are often provided at no cost (19), reducing financial obstacles for low-income households.
Media exposure also significantly affects health-seeking behaviors, as women with regular media access are 10% more likely to attend ANC visits than those with limited exposure. This trend, observed in Nigeria (67), Uganda (68), Sub-Saharan (49), India (69), Nepal (70), and Bangladesh (71) demonstrates how media access increases health literacy and engagement with maternal healthcare by providing information on prenatal care benefits, services, and local initiatives (72). Additionally, media exposure fosters a supportive environment for ANC, especially in traditional societies, where family support for healthcare is crucial (73).
Regional disparities within Senegal further illustrate these trends. Compared to Dakar, regions like Tambacounda (IRR: 0.90, 95% CI: 0.82–0.99), Thiès (0.80, 95% CI: 0.73–0.87), Fatick (0.90, 95% CI: 0.83–0.99), Matam (0.83, 95% CI: 0.75–0.92), Kaffrine (0.87, 95% CI: 0.80–0.97), Kédougou (0.83, 95% CI: 0.75–0.91), and Sédhiou (0.80, 95% CI: 0.73–0.88) exhibit lower adjusted incidence rate ratios (IRRs) for ANC visits, likely due to factors beyond income. Dakar, with 19% of hospital users, benefits from 38% of the national hospital budget, creating a resource concentration that leaves regions like Fatick, with only 2% of healthcare resources, underserved despite high primary healthcare demand (74).
Urban-rural disparities in access further affect ANC attendance. Dakar has a robust transport network, whereas remote areas like Sédhiou face limited public transport options, increasing indirect costs such as travel expenses and restricting regular ANC access (75). Rural regions also struggle with healthcare worker shortages; Dakar's healthcare worker density is significantly higher than in regions like Kaffrine and Kédougou, where retaining trained staff is a challenge (65). Together, these disparities in infrastructure, economic resources, and workforce availability contribute to lower ANC attendance in these underserved areas relative to Dakar (60).
This study utilizes nationally representative DHS data, analyzed with a multilevel Poisson regression model to account for count-based ANC visits and hierarchical data structures, enhancing methodological rigor. However, its cross-sectional design limits causal inference, and self-reported measures may introduce bias. While perceived distance to healthcare facilities (measured as a self-reported barrier) was not statistically significant, incorporating geospatial (GIS) analysis in future research could provide deeper insights into the role of geographic distance.
Conclusions
This study underscores persistent inequities in antenatal care utilization in Senegal, particularly among rural women, those with limited education, and low-income households. While national progress has been made in expanding ANC access, structural barriers such as uneven healthcare resource distribution, financial constraints, and gaps in health literacy continue to hinder equitable maternal care. Addressing these disparities is essential to advancing maternal and child health outcomes and achieving Senegal's commitments to national and global health equity goals.
To reduce these disparities, targeted policy interventions are necessary. Expanding community-based maternal health education programs, including those for both women and men, can increase ANC attendance. Strengthening healthcare infrastructure and distributing healthcare workers more evenly, especially in underserved regions like Tambacounda and Kaffrine, is crucial. Additionally, providing financial support such as transportation subsidies will help improve access for low-income households. Collaborating with local media to promote maternal health information can enhance health literacy, particularly in rural areas.
Improving transportation infrastructure will further reduce costs and improve overall access to care. Moreover, incorporating spatial analysis into future research will provide insights into the impact of physical proximity on ANC access, enabling the development of targeted interventions, such as mobile clinics in remote regions.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
Access to the data was granted through an online request to the Measure DHS program. Since the publicly available dataset lacked any personal identifiers, ethics approval was not necessary. We registered with the DHS web archive, requested the dataset at https://www.dhsprogram.com, and received permission to download the files, ensuring compliance with all relevant guidelines and regulations.
Author contributions
HN: Conceptualization, Data curation, Formal analysis, Methodology, Software, Writing – original draft, Writing – review & editing. AshG: Software, Visualization, Writing – original draft. MG: Data curation, Methodology, Software, Writing – review & editing. MM: Validation, Visualization, Writing – original draft. BM: Conceptualization, Data curation, Investigation, Writing – original draft. DB: Formal analysis, Methodology, Validation, Visualization, Writing – original draft. TG: Methodology, Writing – original draft, Writing – review & editing. YB: Formal analysis, Software, Writing – review & editing. AmaG: Data curation, Methodology, Writing – review & editing. MT: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. NB: Formal analysis, Methodology, Software, Writing – original draft. WT: Investigation, Methodology, Supervision, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We are grateful to the DHS programmes for letting us use the relevant DHS data in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Correction Note
This article has been corrected with minor changes. These changes do not impact the scientific content of the article.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ANC, antenatal care; ANSD, agence nationale de la statistique et de la démographie (national agency for statistics and demographics); DHS, demographic and health survey; LMIC, low- and middle-income countries; SDG, sustainable development goal; USAID, United States agency for international development; WHO, world health organization.
References
1. O'Dair MA, Demetri A, Clayton GL, Caldwell D, Barnard K, Burden C, et al. Does provision of antenatal care in southern Asia improve neonatal survival? A systematic review and meta-analysis. AJOG Glob Rep. (2022) 2:100128. doi: 10.1016/j.xagr.2022.100128
2. World Health Organization. WHO recommendations on Antenatal Care for a Positive Pregnancy Experience. Geneva: World Health Organization (2016).
3. Fagbamigbe AF, Idemudia ES. Wealth and antenatal care utilization in Nigeria: policy implications. Health Care Women Int. (2017) 38:17–37. doi: 10.1080/07399332.2016.1225743
4. Fagbamigbe AF, Idemudia ES. Barriers to antenatal care use in Nigeria: evidences from non-users and implications for maternal health programming. BMC Pregnancy Childbirth. (2015) 15:1–10. doi: 10.1186/s12884-015-0527-y
5. de Masi S, Bucagu M, Tunçalp Ö, Peña-Rosas JP, Lawrie T, Oladapo OT, et al. Integrated person-centered health care for all women during pregnancy: implementing world health organization recommendations on antenatal care for a positive pregnancy experience. Glob Health Sci Pract. (2017) 5(2):197–201. doi: 10.9745/GHSP-D-17-00141
6. Muluneh AG, Animut Y, Ayele TA. Spatial clustering and determinants of home birth after at least one antenatal care visit in Ethiopia: Ethiopian demographic and health survey 2016 perspective. BMC Pregnancy Childbirth. (2020) 20:1–13. doi: 10.1186/s12884-020-2793-6
7. Rurangirwa AA, Mogren I, Nyirazinyoye L, Ntaganira J, Krantz G. Determinants of poor utilization of antenatal care services among recently delivered women in Rwanda; a population based study. BMC Pregnancy Childbirth. (2017) 17:1–10. doi: 10.1186/s12884-017-1328-2
8. Howell EA. Reducing disparities in severe maternal morbidity and mortality. Clin Obstet Gynecol. (2018) 61:387–99. doi: 10.1097/GRF.0000000000000349
9. Onambele L, Ortega-Leon W, Guillen-Aguinaga S, Forjaz MJ, Yoseph A, Guillen-Aguinaga L, et al. Maternal mortality in Africa: regional trends (2000–2017). Int J Environ Res Public Health. (2022) 19:13146. doi: 10.3390/ijerph192013146
10. Kasagama E, Todd J, Renju J. Factors associated with changes in adequate antenatal care visits among pregnant women aged 15–49 years in Tanzania from 2004 to 2016. BMC Pregnancy Childbirth. (2022) 22:18. doi: 10.1186/s12884-021-04350-y
11. Mzembe T, Chikwapulo V, Kamninga TM, Vellemu R, Mohamed S, Nthakomwa L, et al. Interventions to enhance healthcare utilisation among pregnant women to reduce maternal mortality in low-and middle-income countries: a review of systematic reviews. BMC Public Health. (2023) 23:1734. doi: 10.1186/s12889-023-16558-y
12. Kuhnt J, Vollmer S. Antenatal care services and its implications for vital and health outcomes of children: evidence from 193 surveys in 69 low-income and middle-income countries. BMJ Open. (2017) 7:e017122. doi: 10.1136/bmjopen-2017-017122
13. Hussen MA, Worku BT. Quality of antenatal care service and factors associated with client satisfaction at public health facilities of Bele Gasgar District. J Patient Exp. (2022) 9:23743735221083163. doi: 10.1177/23743735221083163
14. Fenta SM, Ayenew GM, Getahun BE. Magnitude of antenatal care service uptake and associated factors among pregnant women: analysis of the 2016 Ethiopia demographic and health survey. BMJ open. (2021) 11:e043904. doi: 10.1136/bmjopen-2020-043904
15. World Health Organization. Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group, and the United Nations Population Division: Executive Summary. Geneva: World Health Organization (2019).
16. Osman ASA, Ahmed MA, Mohamed MH, Ilić P, Asumah MN. Factors affecting the utilization of antenatal care among married women of reproductive age in Merca, Lower Shebelle, Somalia. J Biosci Med. (2022) 10:165–75. doi: 10.4236/jbm.2022.1011013
17. Asumah MN, Mohammed MY, Abubakari A, Padhi BK. Improving maternal health services utilization in Ghana: should digital health be considered? Correspondence. Ann Med Surg. (2023) 85:625–6. doi: 10.1097/MS9.0000000000000247
18. Saad-Haddad G, DeJong J, Terreri N, Restrepo-Méndez MC, Perin J, Vaz L, et al. Patterns and determinants of antenatal care utilization: analysis of national survey data in seven countdown countries. J Glob Health. (2016) 6:010404. doi: 10.7189/jogh.06.010404
19. Koster W, Ondoa P, Sarr AM, Sow AI, Schultsz C, Sakande J, et al. Barriers to uptake of antenatal maternal screening tests in Senegal. SSM Popul Health. (2016) 2:784–92. doi: 10.1016/j.ssmph.2016.10.003
20. McKinnon B, Sall M, Vandermorris A, Traoré M, Lamesse-Diedhiou F, McLaughlin K, et al. Feasibility and preliminary effectiveness of group antenatal care in Senegalese health posts: a pilot implementation trial. Health Policy Plan. (2020) 35:587–99. doi: 10.1093/heapol/czz178
21. Ekholuenetale M, Nzoputam CI, Barrow A, Onikan A. Women’s enlightenment and early antenatal care initiation are determining factors for the use of eight or more antenatal visits in Benin: further analysis of the demographic and health survey. J Egypt Public Health Assoc. (2020) 95(1):13. doi: 10.1186/s42506-020-00041-2
22. Tunçalp Ö, Pena-Rosas JP, Lawrie T, Bucagu M, Oladapo OT, Portela A, et al. WHO Recommendations on antenatal care for a positive pregnancy experience-going beyond survival. BJOG. (2017) 124:860–2. doi: 10.1111/1471-0528.14599
23. Ogundele OJ, Pavlova M, Groot W. Socioeconomic inequalities in reproductive health care services across sub-saharan Africa. A systematic review and meta-analysis. Sex Reprod Healthc. (2020) 25:100536. doi: 10.1016/j.srhc.2020.100536
24. Bee M, Shiroor A, Hill Z. Neonatal care practices in sub-Saharan Africa: a systematic review of quantitative and qualitative data. J Health Popul Nutr. (2018) 37:1–12. doi: 10.1186/s41043-018-0141-5
27. SDaHS. Agence Nationale de la Statistique et de la Démographie (ANSD) & The DHS Program. (2023) (2023).
28. Hall DB. Zero-inflated poisson and binomial regression with random effects: a case study. Biometrics. (2000) 56:1030–9. doi: 10.1111/j.0006-341X.2000.01030.x
29. Greene W. Functional forms for the negative binomial model for count data. Econ Lett. (2008) 99:585–90. doi: 10.1016/j.econlet.2007.10.015
30. StataCorp L. Stata Multilevel Mixed-effects reference Manual. College Station, TX: StataCorp LP 9 (2013). p. 218–41.
31. Merlo J, Chaix B, Ohlsson H, Beckman A, Johnell K, Hjerpe P, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health. (2006) 60:290–7. doi: 10.1136/jech.2004.029454
32. Austin PC, Merlo J. Intermediate and advanced topics in multilevel logistic regression analysis. Stat Med. (2017) 36:3257–77. doi: 10.1002/sim.7336
33. Duah HO, Adisah-Atta I. Determinants of health care decision making autonomy among mothers of children under five years in Ghana: analysis of 2014 Ghana demographic and health survey. Int J Womens Health Wellness. (2017) 3:2474–1353. doi: 10.23937/2474-1353/1510062
34. Merlo J, Chaix B, Yang M, Lynch J, Råstam L. A brief conceptual tutorial of multilevel analysis in social epidemiology: linking the statistical concept of clustering to the idea of contextual phenomenon. J Epidemiol Community Health. (2005) 59:443–9. doi: 10.1136/jech.2004.023473
35. Austin PC, Stryhn H, Leckie G, Merlo J. Measures of clustering and heterogeneity in multilevel P oisson regression analyses of rates/count data. Stat Med. (2018) 37:572–89. doi: 10.1002/sim.7532
36. Mamuye Azanaw M, Gebremariam AD, Teshome Dagnaw F, Yisak H, Atikilt G, Minuye B, et al. Factors associated with numbers of antenatal care visits in rural Ethiopia. J Multidiscip Healthc. (2021) 14:1403–11. doi: 10.2147/JMDH.S308802
37. Phommachanh S, Essink DR, Jansen M, Broerse JE, Wright P, Mayxay M. Improvement of quality of antenatal care (ANC) service provision at the public health facilities in Lao PDR: perspective and experiences of supply and demand sides. BMC Pregnancy Childbirth. (2019) 19:1–13. doi: 10.1186/s12884-019-2345-0
38. Benova L, Tunçalp Ö, Moran AC, Campbell OMR. Not just a number: examining coverage and content of antenatal care in low-income and middle-income countries. BMJ Glob Health. (2018) 3:e000779. doi: 10.1136/bmjgh-2018-000779
39. Demissie KA, Jejaw M, Wondimu BG, Mersha YT, Demsash ES, Dessie SG, et al. Only 9% of mothers have eight and more ANC visit in 14 sub-saharan African countries; evidence from the most recent DHS 2018–2023: a multilevel analysis. BMC Public Health. (2024) 24:1631. doi: 10.1186/s12889-024-19145-x
40. Diallo MA, Mbaye N, Aidara I. Effect of women’s literacy on maternal and child health: evidence from demographic health survey data in Senegal. Int J Health Plann Manage. (2023) 38:773–89. doi: 10.1002/hpm.3624
41. Ekholuenetale M, Nzoputam CI, Barrow A. Prevalence and socioeconomic inequalities in eight or more antenatal care contacts in Ghana: findings from 2019 population-based data. Int J Women’s Health. (2021) 13:349–60. doi: 10.2147/IJWH.S306302
42. Ahinkorah BO, Seidu A-A, Budu E, Mohammed A, Adu C, Agbaglo E, et al. Factors associated with the number and timing of antenatal care visits among married women in Cameroon: evidence from the 2018 Cameroon demographic and health survey. J Biosoc Sci. (2022) 54:322–32. doi: 10.1017/S0021932021000079
43. Muyunda B, Makasa M, Jacobs C, Musonda P, Michelo C. Higher educational attainment associated with optimal antenatal care visits among childbearing women in Zambia. Front Public Health. (2016) 4:127. doi: 10.3389/fpubh.2016.00127
44. Turyasiima M, Tugume R, Openy A, Ahairwomugisha E, Opio R, Ntunguka M, et al. Determinants of first antenatal care visit by pregnant women at community based education, research and service sites in Northern Uganda. East Afr Med J. (2014) 91(9):317–22. https://www.ajol.info/index.php/eamj/article/view/11107726640281
45. Yehualashet DE, Seboka BT, Tesfa GA, Mamo TT, Seid E. Determinants of optimal antenatal care visit among pregnant women in Ethiopia: a multilevel analysis of Ethiopian mini demographic health survey 2019 data. Reprod Health. (2022) 19:61. doi: 10.1186/s12978-022-01365-2
46. Mohammad KA, Zahura FT, Rahman MM. Importance of maternal education on antenatal care visits in Bangladesh. Bangladesh J Sci Res. (2017) 30:23–33. doi: 10.3329/bjsr.v30i1-2.36117
47. Shrestha B. Mother’s education and antenatal care visits in Nepal. Tribhuvan Univ J. (2018) 32:153–64. doi: 10.3126/tuj.v32i2.24712
48. Tessema ZT, Minyihun A. Utilization and determinants of antenatal care visits in East African countries: a multicountry analysis of demographic and health surveys. Adv Public Health. (2021) 2021:6623009. doi: 10.1155/2021/6623009
49. Gebeyehu FG, Geremew BM, Belew AK, Zemene MA. Number of antenatal care visits and associated factors among reproductive age women in Sub-Saharan Africa using recent demographic and health survey data from 2008 to 2019: a multilevel negative binomial regression model. PLOS Glob Public Health. (2022) 2:e0001180. doi: 10.1371/journal.pgph.0001180
50. Mumtaz Z, Salway SM. Gender, pregnancy and the uptake of antenatal care services in Pakistan. Sociol Health Illn. (2007) 29:1–26. doi: 10.1111/j.1467-9566.2007.00519.x
51. Mullany BC, Becker S, Hindin M. The impact of including husbands in antenatal health education services on maternal health practices in urban Nepal: results from a randomized controlled trial. Health Educ Res. (2007) 22:166–76. doi: 10.1093/her/cyl060
52. Mullany BC. Barriers to and attitudes towards promoting husbands’ involvement in maternal health in Katmandu, Nepal. Soc Sci Med. (2006) 62:2798–809. doi: 10.1016/j.socscimed.2005.11.013
53. Wulandari RD, Laksono AD, Matahari R. Does Husband’s education level matter to antenatal care visits? A study on poor households in Indonesia. Indian J Community Med. (2022) 47:192–5. doi: 10.4103/ijcm.ijcm_981_21
54. Raru TB, Ayana GM, Zakaria HF, Merga BT. Association of higher educational attainment on antenatal care utilization among pregnant women in east Africa using demographic and health surveys (DHS) from 2010 to 2018: a multilevel analysis. Int J Women’s Health. (2022) 14:67–77. doi: 10.2147/IJWH.S350510
55. Tessema ZT, Tesema GA, Yazachew L. Individual-level and community-level factors associated with eight or more antenatal care contacts in sub-Saharan Africa: evidence from 36 sub-Saharan African countries. BMJ open. (2022) 12:e049379. doi: 10.1136/bmjopen-2021-049379
56. Adedokun ST, Yaya S. Correlates of antenatal care utilization among women of reproductive age in sub-saharan Africa: evidence from multinomial analysis of demographic and health surveys (2010–2018) from 31 countries. Arch Public Health. (2020) 78:1–10. doi: 10.1186/s13690-020-00516-w
57. Bloom SS, Wypij D, Das Gupta M. Dimensions of women’s autonomy and the influence on maternal health care utilization in a north Indian city. Demography. (2001) 38:67–78. doi: 10.1353/dem.2001.0001
58. Furuta M, Salway S. Women’s position within the household as a determinant of maternal health care use in Nepal. Int Fam Plan Perspect. (2006) 32:17–27. doi: 10.1363/3201706
59. Forbes F, Wynter K, Wade C, Zeleke BM, Fisher J. Male partner attendance at antenatal care and adherence to antenatal care guidelines: secondary analysis of 2011 Ethiopian demographic and health survey data. BMC Pregnancy Childbirth. (2018) 18:1–11. doi: 10.1186/s12884-018-1775-4
60. Samba M, Thiam I, Paul E. Which socio-economic groups benefit most from public health expenditure in Senegal? A dynamic benefit incidence analysis. SSM Popul Health. (2024) 28:101714. doi: 10.1016/j.ssmph.2024.101714
61. Shibre G, Zegeye B, Idriss-Wheeler D, Ahinkorah BO, Oladimeji O, Yaya S. Socioeconomic and geographic variations in antenatal care coverage in Angola: further analysis of the 2015 demographic and health survey. BMC Public Health. (2020) 20:1–10. doi: 10.1186/s12889-020-09320-1
62. Shibre G, Zegeye B, Idriss-Wheeler D, Yaya S. Factors affecting the utilization of antenatal care services among women in Guinea: a population-based study. Fam Pract. (2021) 38:63–9. doi: 10.1093/fampra/cmaa053
63. Ziblim S-D, Yidana A, Mohammed A-R. Determinants of antenatal care utilization among adolescent mothers in the Yendi municipality of northern region, Ghana. Ghana J Geogr. (2018) 10(1):78–97. https://www.ajol.info/index.php/gjg/article/view/170407
64. Shrestha G. Factors related to utilization of antenatal care in Nepal: a generalized linear approach. J Kathmandu Med Coll. (2013) 2:69–74. doi: 10.3126/jkmc.v2i2.10629
65. Paul E, Ndiaye Y, Sall FL, Fecher F, Porignon D. An assessment of the core capacities of the Senegalese health system to deliver universal health coverage. Health Policy OPEN. (2020) 1:100012. doi: 10.1016/j.hpopen.2020.100012
66. Zhang Y, Chen J, Zhang C, Chen L. Senegal Health System Analysis and Its Implications to Global Health Cooperation. (2021).
67. Atsiya AP, Okuwa AA. Mass media Exposure and Antenatal Care Visits in Nigeria. Abuja: A Publication of Department of Peace Studies and Conflict Resolution Faculty of Social Sciences National Open University of Nigeria (2021). p. 107.
68. Sserwanja Q, Mutisya LM, Musaba MW. Exposure to different types of mass media and timing of antenatal care initiation: insights from the 2016 Uganda demographic and health survey. BMC Women’s Health. (2022) 22:1–8. doi: 10.1186/s12905-022-01594-4
69. Dhawan D, Pinnamaneni R, Bekalu M, Viswanath K. Association between different types of mass media and antenatal care visits in India: a cross-sectional study from the national family health survey (2015–2016). BMJ Open. (2020) 10:e042839. doi: 10.1136/bmjopen-2020-042839
70. Acharya D, Adhikari R, Kreps GL. Does exposure of mass media associate with utilisation of ANC services? A trend analysis from Nepal demographic and health surveys. Int J Health Plann Manage. (2021) 36:2145–61. doi: 10.1002/hpm.3285
71. Ahmed A, Sultana R, Rahman MM, Islam MR. Effect of Media Exposure and Related Factors on Antenatal Care Visits Among Pregnant Women in Bangladesh: A Study Based on BDHS 2017–18 Data. (2024).
72. Ogwu SO, Onwe JC, Mokobia NA, Onyeka-Okite E, Okiwelu K. Mass media exposure and the utilization of maternal health services in Nigeria. UBS J Business Econ Policy. (2023) 1:73–83. https://journals.unizik.edu.ng/ubsjbep/article/view/3228
73. Fatema K, Lariscy JT. Mass media exposure and maternal healthcare utilization in South Asia. SSM Popul Health. (2020) 11:100614. doi: 10.1016/j.ssmph.2020.100614
74. Centre de Recherche en Économie Générationnelle (CREG). Senegal-Demographic-Dividend-Effort-Index-Report-2021-CREG. Dakar: Centre de Recherche en Économie Générationnelle (CREG) (2021).
Keywords: antenatal care, multilevel poisson regression, Senegal, demographic health survey, 2023
Citation: Negash HK, Gebiru AM, Getnet M, Melese M, Mengistie BA, Bitew DA, Godana TN, Bizuneh YB, Getahun AB, Tilahun MM, Baykemagn ND and Tassew WC (2025) Antenatal care visits and associated factors in Senegal: a multilevel poisson regression analysis of the 2023 DHS survey. Front. Glob. Women's Health 6:1524361. doi: 10.3389/fgwh.2025.1524361
Received: 7 November 2024; Accepted: 12 May 2025;
Published: 27 May 2025;
Corrected: 4 June 2025.
Edited by:
Tafadzwa Dzinamarira, ICAP in Zimbabwe, ZimbabweReviewed by:
Qingxia Kong, Erasmus University Rotterdam, NetherlandsDieudonne Mpunga, Kinshasa School of Public Health, Democratic Republic of Congo
Copyright: © 2025 Negash, Gebiru, Getnet, Melese, Mengistie, Bitew, Godana, Bizuneh, Getahun, Tilahun, Baykemagn and Tassew. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Habtu Kifle Negash, aGFidHVrOEBnbWFpbC5jb20=
 Habtu Kifle Negash
Habtu Kifle Negash Ashebir Mamay Gebiru2,3
Ashebir Mamay Gebiru2,3 Mihret Getnet
Mihret Getnet Mihret Melese
Mihret Melese Berihun Agegn Mengistie
Berihun Agegn Mengistie Desalegn Anmut Bitew
Desalegn Anmut Bitew Tilahun Nega Godana
Tilahun Nega Godana Yosef Belay Bizuneh
Yosef Belay Bizuneh Amare Belete Getahun
Amare Belete Getahun Mikias Mered Tilahun
Mikias Mered Tilahun Nebebe Demis Baykemagn
Nebebe Demis Baykemagn Worku Chekol Tassew
Worku Chekol Tassew