- 1Department of Obstetrics and Gynecology, Beijing Chao-Yang Hospital, Capital Medical University, Beijing, China
- 2Clinical Medical College, Hebei University, Baoding, Hebei, China
Background: Hypertensive disorders of pregnancy (HDP) are a significant cause of maternal and perinatal morbidity and mortality worldwide. This study aims to use the Global Burden of Disease 2021 database to analyze the prevalence trends and disease burden of HDP across the globe from 2019 to 2021.
Methods: We analyzed four key metrics related to HDP (prevalence, incidence, mortality, and DALYs) using data from the GBD Database. Trends were assessed using the estimated annual percentage change (EAPC) and changes in disease burden.
Results: In 2021, global HDP prevalence cases, incidence cases, mortality cases, and DALYs were 3.51 million, 18.00 million, 37.58 million, and 2.44 million, respectively, with percentage changes of 14%, 15%, −29%, and −29% over the study period. Prevalence and incidence rates increased (EAPCs: −0.7 and −0.67), while mortality and DALYs rates decreased (EAPCs: −2.29 and −2.28). Low Socio-demographic Index (SDI) regions had the highest HDP burden, accounting for about half of the global total. The 25–29 age group had the highest incidence cases.
Conclusion: Over the past 32 years, HDP prevalence cases and incidence cases have risen globally, but death cases and DALYs cases have significantly decreased, particularly in low SDI regions and the 25–29 age group. The global HDP burden is higher in regions with lower SDI. Our findings highlight regional and age-related disparities in HDP, providing a basis for targeted interventions and prevention strategies.
Introduction
Hypertensive disorders of pregnancy (HDP) encompass a spectrum of conditions characterised by the coexistence of pregnancy and hypertension, which can precipitate substantial maternal and fetal mortality (1). These disorders are clinically stratified based on the temporal onset of hypertension and the severity of the clinical manifestations (2). Globally, HDP exhibits a prevalence that varies significantly across different regions. Literature reviews indicate HDP global prevalence is between 5 and 10% (3), a prevalence of 7% in the United States (4), 5%–6.4% in China (5), and notably higher rates of 10% in economically disadvantaged areas of Africa (6).
HDP exert a plethora of detrimental effects on both the mother and the fetus. Maternal consequences are particularly severe, with pre-eclampsia and eclampsia posing significant risks for placental abruption, seizures, cerebrovascular accidents, multi-organ dysfunction, and, in extreme cases, maternal mortality (7, 8). A meta-study showed that patients with HDP were 3.6 times more likely than normal women to develop chronic hypertension (9). Additionally, chronic hypertension is associated with long-term damage to the renal and cardiovascular systems (10). Fetal repercussions are predominantly characterised by intrauterine growth restriction, preterm birth, fetal hypoxia, and the potential for stillbirth (11, 12). Advanced maternal age is a significant predictor of hypertensive disorders during pregnancy, with women over 35 years of age exhibiting a twofold increased risk compared to their younger counterparts (13). Additionally, nutritional factors, particularly diets deficient in calcium and magnesium (14), have been implicated in the mechanism of pregnancy-associated hypertension.
The Global Burden of Disease (GBD) 2021 Database (https://ghdx.healthdata.org/gbd-2021) encompasses a comprehensive array of data spanning from 1990 to 2021; HDP has significantly impacted global health, as evidenced by a substantial rise in global incidence from 16.3 million cases in 1990 to 18.08 million in 2019, reflecting a 10.92% increase. In 2019, there were 27,834 HDP-related deaths, marking a 30.05% decrease from 1990 levels (15). Acknowledging the variability in HDP incidence and mortality rates, appositional status, and limited access to quality healthcare further exacerbate the risk, especially in different countries and regions, within populations experiencing economic disadvantages, underscoring the need for tailored public health strategies. Currently, there is no global consensus on the diagnostic criteria for HDP resulting in inconsistent diagnostic standards across different regions. This inconsistency poses certain challenges when assessing the global incidence, prevalence, mortality, and disability-adjusted life years (DALYs) of HDP. Therefore, when assessing the disease burden in low SDI (Socio-demographic Index) and middle SDI regions, it is precisely because of the lack of uniform diagnostic criteria that leads to an uneven distribution of the disease burden within each region (16). A meta-analysis found that low- and middle-income countries face significant constraints and barriers to the management of HDP, such as insufficient therapeutic medications, lack of diagnostic reagents, insufficient infrastructure, and insufficient knowledge of treatment among healthcare professionals (17). The impact of HDP extends to critical global health indicators, including DALYs, years of life lost due to premature mortality (YLLs), and years lived with disability (YLDs) (15, 16).
The detrimental impact of HDP on maternal and infant health is well recognized. However, research on its contribution to the global burden of disease remains relatively limited. This study aims to address this gap by conducting an in-depth analysis of the most recent data from the GBD 2021 database. It provides a detailed examination of the disease burden of HDP across different regions and age groups worldwide, thereby offering more targeted and scientifically sound evidence for research in this field and the formulation of public health policies.
Methods
Data sources and disease definition
The GBD 2021 database provides annual estimates of incidence and mortality for 371 diseases and injuries across 204 countries and territories from 1990 to 2021 (18). The SDI is a standardized composite measure ranging from 0 to 1 that allows comparisons across geographic regions and time. It is calculated based on national per capita income, average years of education among individuals aged 15 and older, and total fertility rate, and categorizes countries and regions into five levels: low, low-middle, middle, high-middle, and high. The GBD 2021 database is widely used to assess the global burden of health issues, analyze trends in diseases and risk factors, and provide data support for public health policy-making. HDP refer to hypertension that arises after 20 weeks of gestation and returns to normal within 12 weeks postpartum. The diagnostic criterion is typically a blood pressure of ≥140/90 mmHg, corresponding to ICD-10 code O13.
DALYs
DALYs are a comprehensive measure of disease burden, combining YLLs and YLDs. One DALY represents one lost year of healthy life. YLLs are calculated based on the number of deaths and standard life expectancy loss, while YLDs are derived from the number of incident cases, disability weights, and the duration of the condition. DALYs are widely used to assess the impact of diseases and injuries on population health and are a core metric in the GBD study. They provide a basis for health policy decisions, resource allocation, and evaluation of the cost-effectiveness of public health interventions (16).
Estimated annual percent change
Estimated Annual Percent Change (EAPC) is a statistical metric used to measure the trend in disease indicators over a specific period. It is calculated through linear regression analysis and reflects the rate of increase or decrease in a given metric. Unlike simple comparisons between the starting and ending years, EAPC offers a more detailed understanding of time trends, helping researchers and public health professionals more accurately assess changes in disease burden (16).
Results
Global level
Globally, there has been a notable escalation in the prevalence cases, incidence cases, mortality cases, and DALYs cases in HDP. Specifically, the prevalence of HDP cases has risen from 3.07 million in 1990 to 3.51 million in 2021, marking a 14% increase. Similarly, the incidence of HDP cases has shown a 15% increase, escalating from 15.61 million in 1990 to 18.00 million in 2021. Conversely, mortality cases have significantly declined, decreasing from 53.17 thousand in 1990 to 37.58 thousand in 2021, corresponding to a 29% reduction. Moreover, the burden of HDP, as measured by DALYs, has also witnessed a substantial decrease, plummeting from 3.44 million in 1990 to 2.44 million in 2021, indicating a 29% reduction (Table 1 and Supplementary Tables S1–S3, Figure 1A). Contrary to the global trend, the prevalence rates, incidence rates, mortality rates and DALYs rates of HDP within WCBA declined from 1990 to 2021. EAPC for these metrics was −0.7 (−0.76 to −0.64), −0.67 (−0.73 to −0.62), −2.29 (−2.33 to −2.24), and −2.28 (−2.33 to −2.23). These figures underscore a significant reduction in the epidemiological burden of HDP in the WCBA, contradicting the global escalation observed elsewhere (Table 1 and Supplementary Tables S1–S3, Figure 1A).
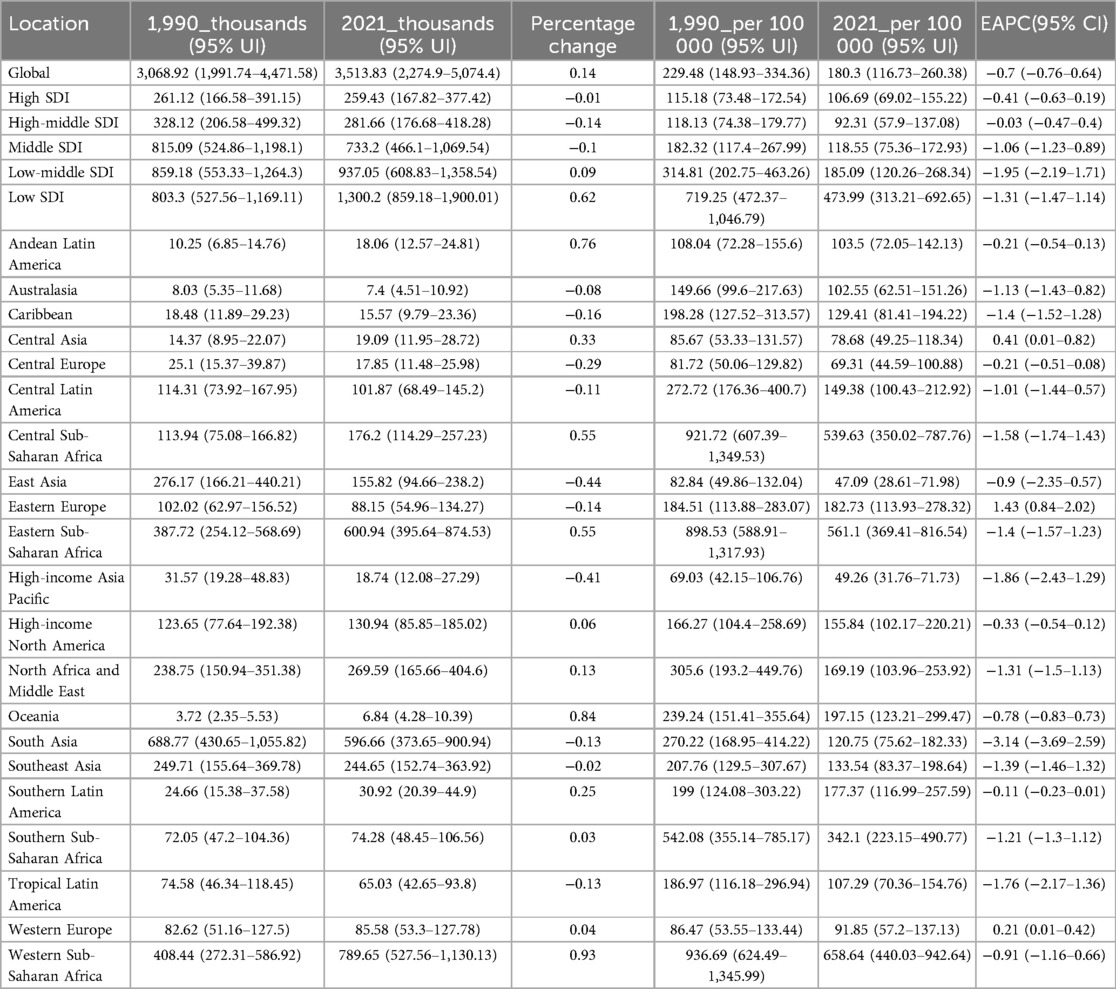
Table 1. The prevalence of hypertensive disorders of pregnancy cases and rates among WCBA in 1990 and 2021, and the trends from 1990 to 2021.
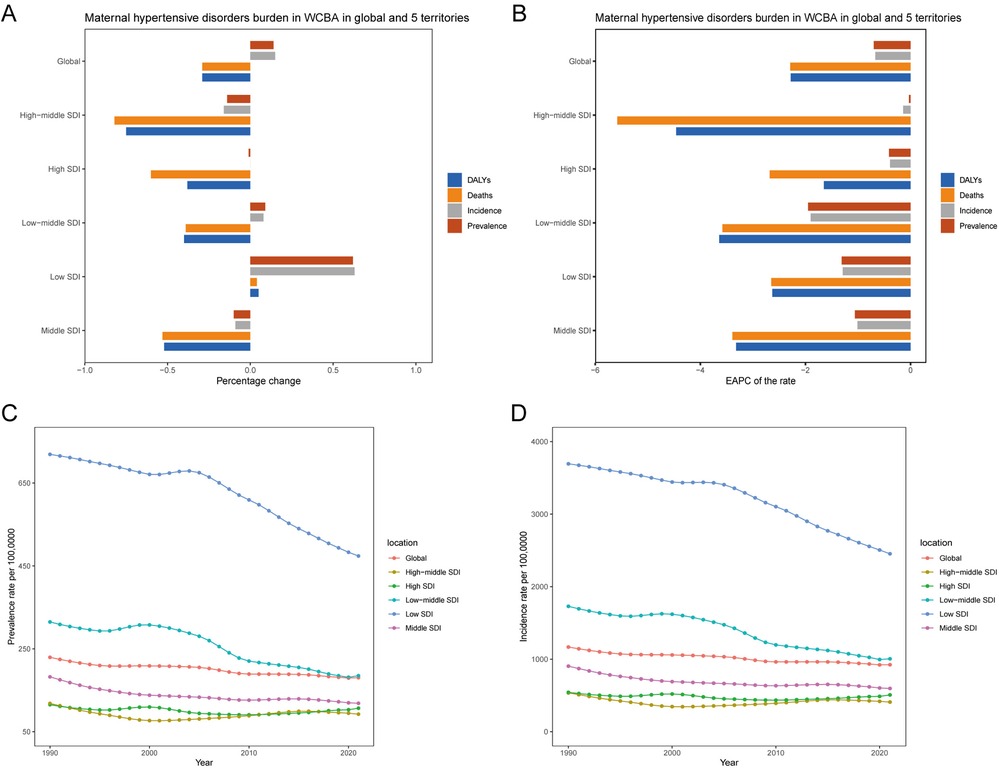
Figure 1. Global and regional temporal trends in HDP burden within WCBA. (A) Percentage changes in the number of prevalent cases, incident cases, deaths, and DALYs from 1990 to 2021. (B) EAPC in prevalence, incidence, mortality, and DALY rates from 1990 to 2021. (C) Prevalence rates per 100,000 individuals from 1990 to 2021 in global and five distinct territories. (D) Incidence rates per 100,000 individuals from 1990 to 2021 in global and five distinct territories.
It indicated that the growth of the burden of disease is slowing down and may even be on the decline in certain regions or populations. This may be closely related to the implementation of public health measures, advances in medical technology or improvements in socio-economic conditions.
SDI regional level
In 2021, low SDI regions had the highest absolute HDP across prevalence cases, incidence cases, mortality cases and DALYs cases in WCBA. Specifically, these regions accounted for 1.30 million prevalent cases (0.86–1.90), 6.73 million incident cases (5.70–7.94), 18.31 thousand mortality cases (14.98–22.31), and 1.18 million DALYs cases (0.97–1.43). Notably, these figures constituted approximately 50% of the global HDP burden (Table 1 and Supplementary Tables S1–S3, Figures 1C,D and Supplementary Figures S1A,B). Prevalence cases, incidence cases, mortality cases, and DALYs cases of HDP showed a progressive decline with decreasing SDI. The low SDI regions experienced the most significant percentage changes in prevalence cases and incidence cases, approximately 60%. In contrast, the high-middle SDI regions demonstrated the largest percentage changes in mortality cases and DALYs cases, around 75%. Conversely, the high SDI regions had the smallest percentage changes in prevalence cases and incidence cases, approximately 1%, and the low SDI regions showed the least change in mortality cases and DALYs cases, approximately 5% (Table 1 and Supplementary Table S1–S3, Figure 1A). Significantly, between 1990 and 2021, the low-middle SDI region exhibited a marked decline in both the prevalence rates and incidence rates of HDP, with an EAPC of −1.95 (−2.19 to −1.71) and −1.9 (−2.08 to −1.73). In parallel, the high-middle SDI region witnessed a pronounced reduction in mortality rates and DALY rates, with an EAPC of −5.58 (−5.68 to −5.48) and −4.46 (−4.57 to −4.36) (Table 1 and Supplementary Tables S1–S3, Figure 1B). In 2021, regions with low and low-middle SDI demonstrated relatively elevated prevalence rates, incidence rates, mortality rates, and DALYs rates associated with HDP. Concurrently, the low SDI region experienced the most rapid decline in prevalence rates and incidence rates, while the high-middle SDI region showed the steepest decrease in mortality rates and DALY rates.
The results indicate that low SDI regions bear the heaviest burden in terms of prevalence cases, incidence cases, mortality cases, and DALYs cases, while high SDI regions have the lightest burden. This suggests that the global burden of HDP is closely related to the SDI.
GBD regional level
Over the period from 1990 to 2021, WCBA experienced a temporal increase in the absolute numbers of prevalence cases, incidence cases, mortality cases and DALYs cases associated with HDP, with these increases observed in approximately half of the regions. Notably, Andean Latin America, Sub-Saharan Africa, North Africa and Middle East, Central Asia, North Africa and Middle East, Sub-Saharan Africa, Central Asia and Oceania, and Western Europe have demonstrated a consistent upward trend in prevalence cases and incidence cases over the past three decades. Regions such as the Caribbean, Oceania Central and Western Sub-Saharan Africa have shown increasing trends in mortality cases and DALYs cases, all of which are predominantly characterised by low and low-middle SDI regions. Over the past 32 years, the most significant increases in both prevalence rates and DALY rates were observed in Oceania and Western Sub-Saharan Africa, with EAPC for prevalence rates of −0.78 (−0.83 to −0.73) and −0.91 (−1.16 to −0.66), and for DALY rates of −0.59 (−0.78 to −0.39) and −1.75 (−1.84 to −1.66) (Table 1 and Supplementary Tables S1–S3, Figures 2A–D and Supplementary Figures S2A,B). The incidence rates and mortality rates of HDP in WCBA followed a similar pattern to the prevalence rates. The high-income Asia Pacific region has shown a significant downward trend in the absolute cases and rates of prevalence, incidence, mortality, and DALYs of HDP, suggesting a decreasing burden of HDP within this region. This trend is likely closely associated with improvements in healthcare infrastructure and economic conditions.
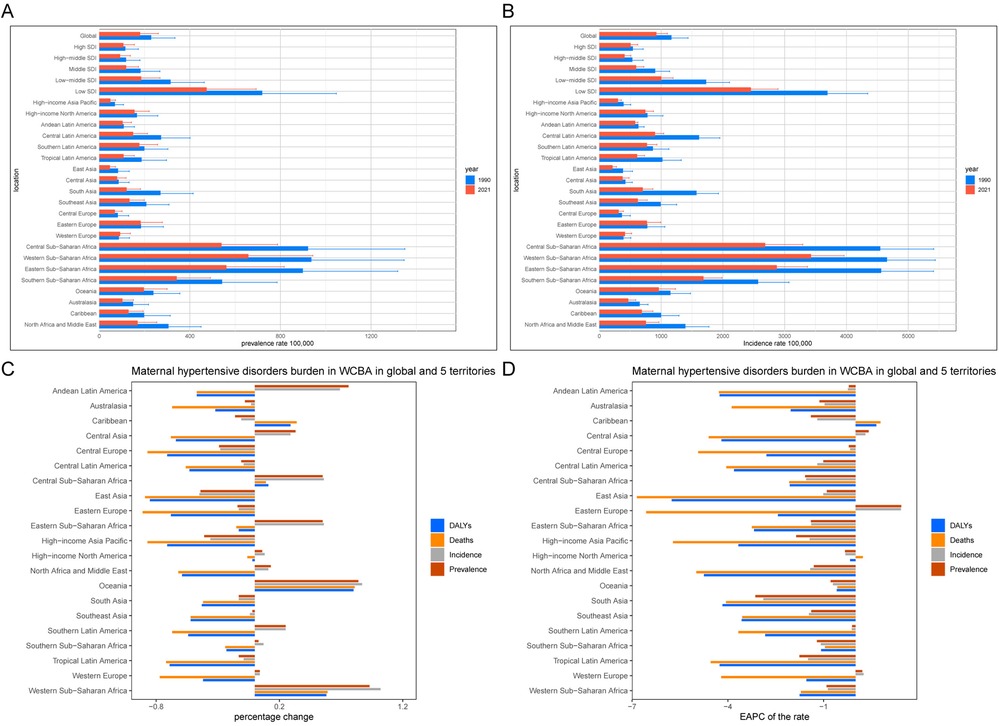
Figure 2. Regional temporal trends in HDP burden within WCBA. (A) Prevalence rates per 100,000 population in 1990 and 2021. (B) Incidence rates per 100,000 population in 1990 and 2021. (C) Percentage changes in the number of prevalent cases, incident cases, deaths, and DALYs from 1990 to 2021. (D) EAPC in prevalence, incidence, mortality, and DALY rates from 1990 to 2021.
Overall, these trends reveal significant geographical disparities and dynamic changes in the global burden of HDP. In low and low-middle SDI regions, such as Andean Latin America, Sub-Saharan Africa, and Central Asia, the burden of HDP continues to increase. This may be related to the limited medical resources, weak public health systems, and relatively underdeveloped socio-economic conditions in these areas. In contrast, the HDP burden has significantly decreased in the high-income Asia Pacific region, reflecting progress in healthcare, socio-economic status, and education in that area.
Countries level
Between 1990 and 2021, approximately 56% of countries within the WCBA exhibited increasing prevalence cases and incidence cases of HDP. In contrast, only 15% to 20% of these countries displayed an increasing trend in mortality cases and DALYs cases associated with HDP. The most significant increases in prevalence cases and incidence cases were noted in Qatar and the United Arab Emirates, with percentage changes ranging from 273% to 352%. Conversely, the most substantial increases in mortality cases and DALYs cases were observed in Chad and Papua New Guinea, with percentage changes ranging from 101% to 166%. However, the most pronounced decrease in prevalence rates was recorded in Guatemala, a low SDI country, with an EAPC of −7.15 (−7.95 to −6.34). Nepal, also a low SDI country, experienced the most significant decline in incidence rates, with an EAPC of −3.83 (−4.12 to −3.54). The highest decrease in mortality rates was observed in Qatar, a high SDI country, with an EAPC of −9.87 (−10.22 to −9.51). Turkey, a high-middle SDI country, recorded the steepest reduction in DALY rates, with an EAPC of −8.51 (−9.12 to −7.90) (Supplementary Tables S4–S7, Figures 3A–D and Supplementary Figures S3A–D).
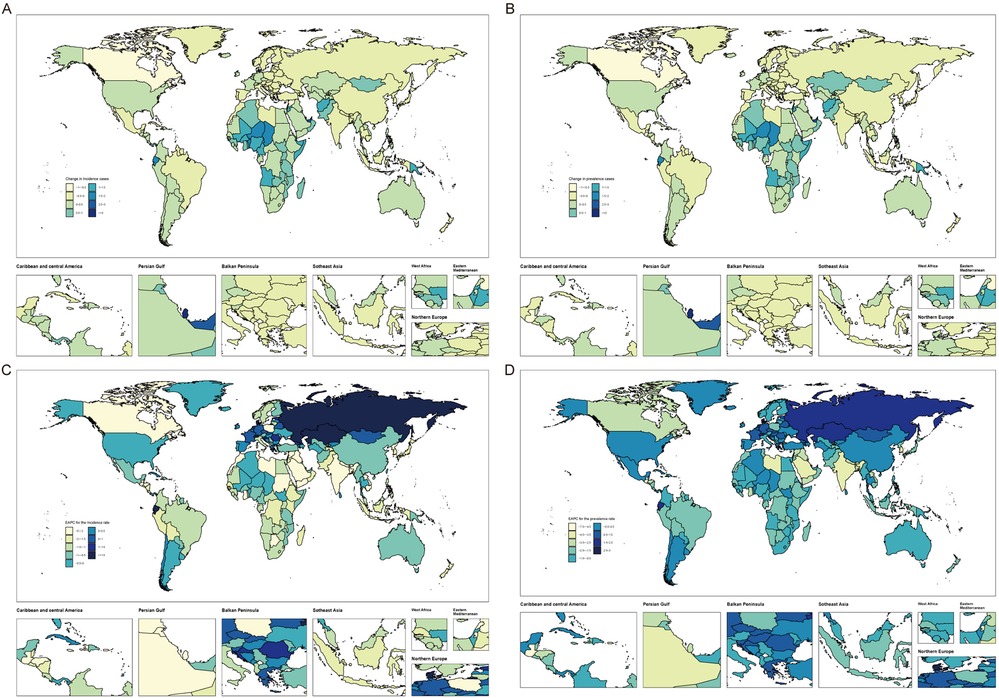
Figure 3. Global temporal trends in HDP burden within WCBA. (A) Percentage changes in incident cases across 204 countries from 1990 to 2021. (B) Percentage changes in prevalent cases across 204 countries from 1990 to 2021. (C) EAPC in incident rates across 204 countries from 1990 to 2021. (D) EAPC in prevalent rates across 204 countries from 1990 to 2021.
The observed data reveal a distinct dichotomy in the epidemiological trends of HDP. Specifically, reductions in prevalence and incidence rates are noted in low SDI regions, whereas declines in mortality rates and DALYs rates are more pronounced in high SDI areas. This divergence underscores the intricate and multifaceted interplay between socio-economic determinants and health outcomes within the context of HDP.
Age distribution pattern
Analysis of the prevalence cases, incidence cases, mortality cases, and DALYs cases number of the percentage change among the WCBA global population reveals significant variations with age (Figure 4A and Supplementary Figures S4A–C). The 45–49 age group demonstrated the lowest percentage changes at 7%, 4%, 0%, and 0%, respectively, for prevalence cases, incidence cases, mortality cases, and DALYs cases. However, the 30–34 age group exhibited the most pronounced percentage changes, with 50%, 50%, 27%, and 20% for prevalence cases, incidence cases, mortality cases, and DALYs cases. These increments are approximately 7–12 times higher than those observed in the 45–49 age group, underscoring the disparate impact of HDP across different age cohorts (Table 2 and Supplementary Tables S8–S10).
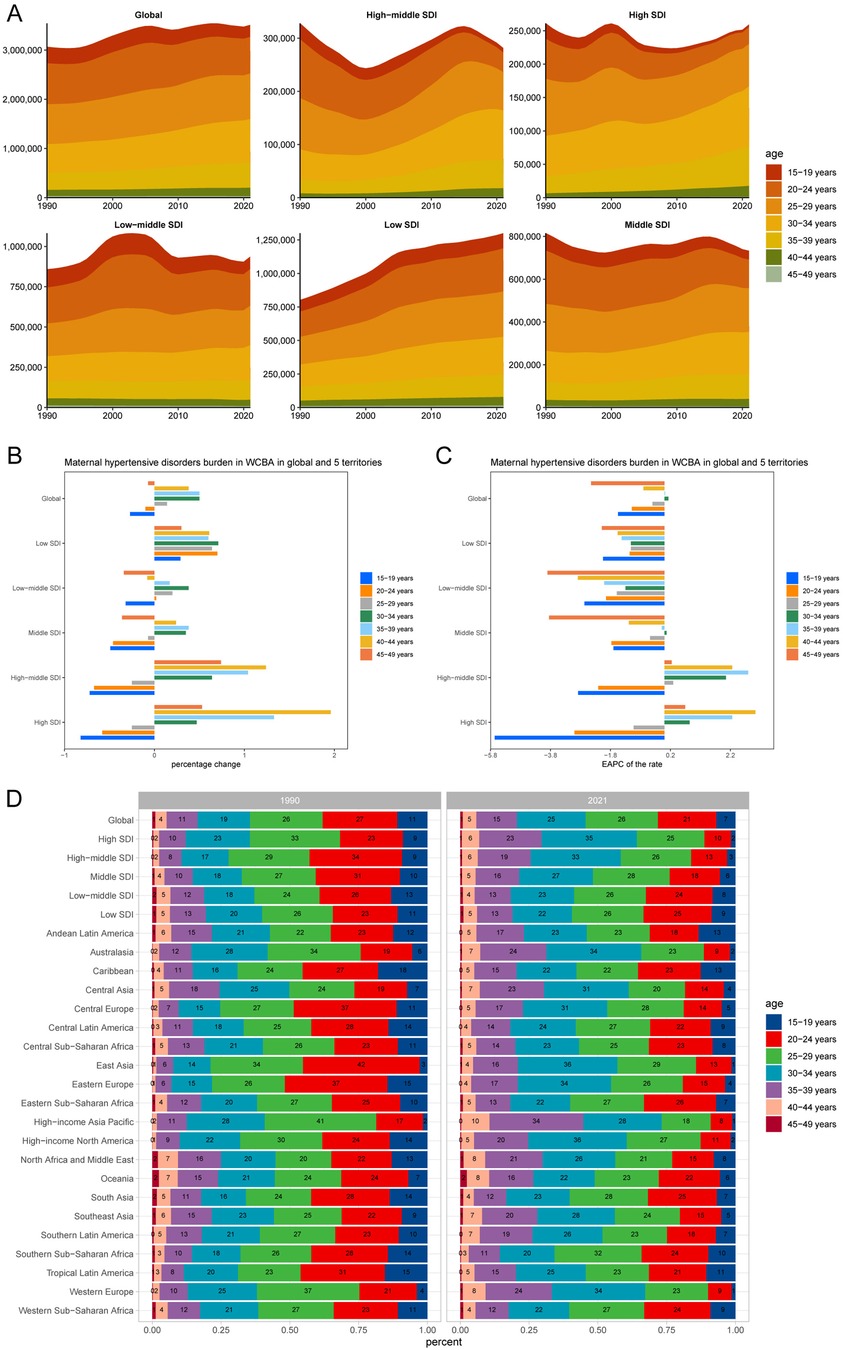
Figure 4. Age-patterned temporal trends in HDP burden within WCBA across different regions. (A) Prevalent cases across seven age groups (15–49 years, in 5-year intervals) from 1990 to 2021, globally and in five territories with varying levels of SDI. (B) Percentage changes in prevalent cases across seven age groups, globally and in five territories, from 1990 to 2021. (C) EAPC in prevalent cases across seven age groups, globally and in five territories, from 1990 to 2021. (D) Distribution of prevalent cases across seven age groups as percentages, globally, in five territories, and 21 GBD regions, in 1990 and 2021.
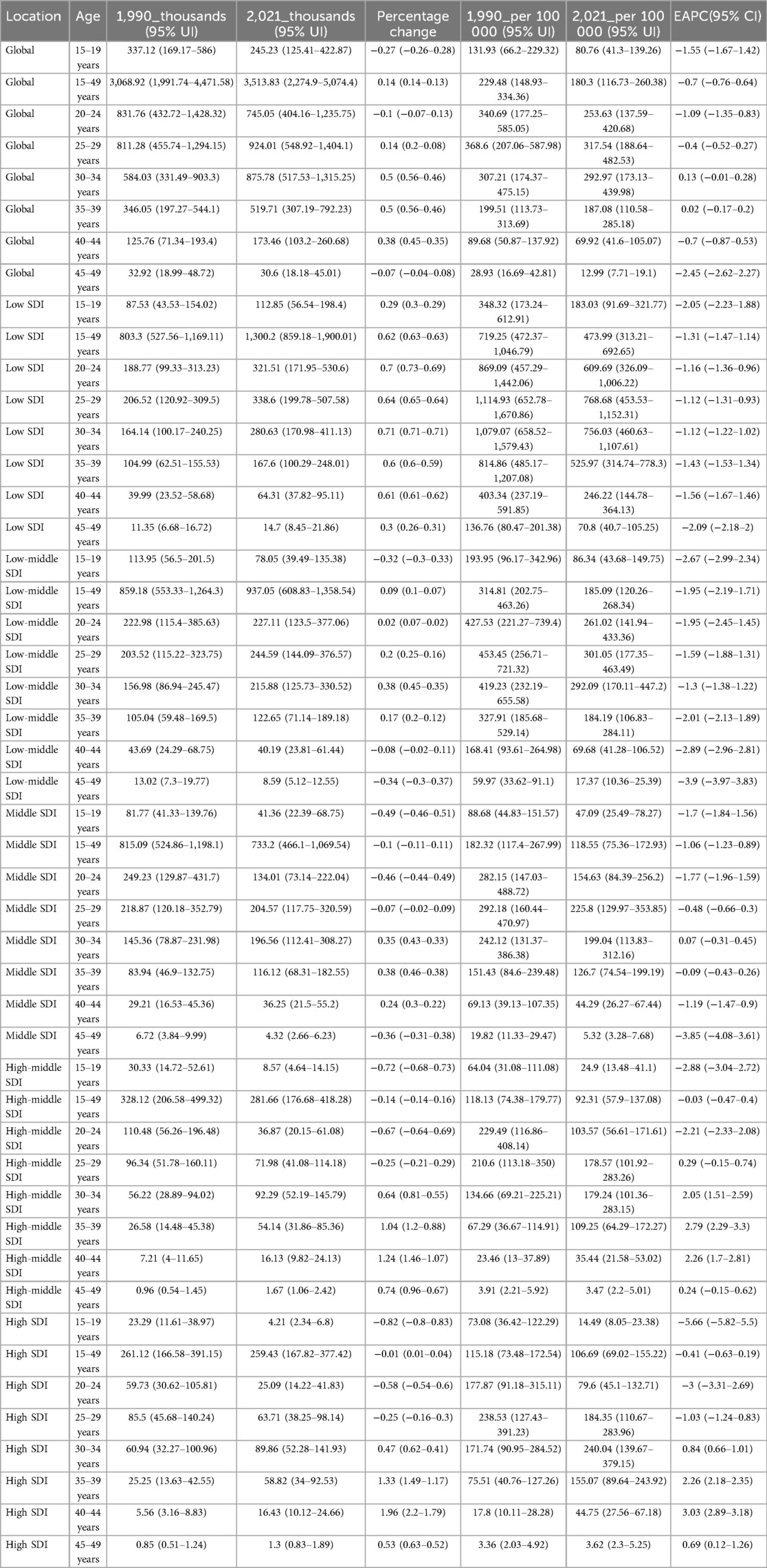
Table 2. The prevalence of hypertensive disorders of pregnancy cases and rates among WCBA in 1,990 and 2021, and the trends in age patterns.
The percentage change in prevalence cases of HDP across the five SDI regions demonstrates distinct age-related trends. In low SDI regions, the prevalence cases initially increase and then decrease with age. In contrast, other SDI regions exhibit a pattern of initial decline, followed by an increase, and eventually a leveling off. For example, in the high SDI region, the percentage change in prevalence cases rises from −0.82 in the 15–19 age group to 1.96 in the 40–44 age group, before declining to 0.53 in the 45–49 age group. The age group with the highest percentage change in prevalence cases peaks at 30–34 years in low and low-middle SDI regions, at 35–39 years in middle SDI regions, and at 40–44 years in high SDI regions. As SDI increases, the percentage change in prevalence of HDP tends to rise with age (Table 2 and Supplementary Tables S8–S10, Figure 4B).
Over the past 32 years, trend analysis from 1990 to 2021 indicates that incidence rates among the 25–49 age groups (25–29 age group, 30–34 age group, 35–39 age group, 40–44 age group, and 45–49 age group) show increasing trends with EAPC of −0.36 (−0.46 to −0.25), 0.1 (−0.04 to 0.24), −0.01 (−0.19 to 0.17), −0.63 (−0.81 to −0.45), and −2.1 (−2.29 to −1.91). Conversely, incidence rates in the 15–24 age groups (15–19 age group and 20–24 age group) exhibit decreasing trends. The 30–39 age group (30–34 age group and 35–39 age group) experienced the highest increase in incidence rates (Supplementary Table S8, Figure 4B and Supplementary Figures S5A,B). In 2021, the 25–29 age group reported the highest incidence cases of HDP globally, with 4.67 million cases (3.58–5.96) and incidence rates of 1605.08 per 100,000 (1,232–2,048.78), surpassing all other age groups (Supplementary Table S8). Furthermore, the 20–24 age group demonstrated the fastest decreases in mortality rates and DALY rates of HDP, with EAPC of −2.47 (−2.63 to −2.31) and −2.39 (−2.56 to −2.23). In contrast, the 40–44 age group showed the fastest increases in mortality and DALY rates, with EAPC of −1.59 (−1.73 to −1.44) and −2.07 (−2.32 to −1.81) (Table 2 and Supplementary Tables S8–S10, Figure 4C and Supplementary Figures S5C–F). This suggests that the burden of HDP was most pronounced in the 40–44 age group.
Among the 21 regions, East Asia exhibited the most decline in HDP cases in the 20–24 age group. Specifically, the prevalence cases dropped from 42% to 13%, incidence cases decreased from 43% to 13%, mortality cases fell from 28% to 16%, and DALY cases reduced from 32% to 16%. In contrast, the High-income Asia Pacific region is the most significant increase in the 35–39 age group. The prevalence cases rose from 11% to 34%, incidence cases increased from 11% to 32%, mortality cases escalated from 14% to 25%, and DALY cases augmented from 12% to 30%. These observations suggest a shift in the distribution of HDP cases within WCBA, transitioning from younger to older age groups (Figure 4D and Supplementary Figures S6A–C).
Based on the aforementioned findings, it is evident that the prevalence cases, incidence cases, mortality cases, and DALYs cases of HDP exhibit distinct age-related patterns across different SDI regions. In low SDI regions, a higher burden of HDP is observed among younger age groups, with a notable decline as age increases. This trend may be attributed to the limited availability of medical resources and inadequate health education in these areas, which disproportionately affect younger women. Conversely, in high SDI regions, the burden of HDP is more pronounced among older age groups. This phenomenon may be explained by the presence of more complex underlying health conditions and the trend of delayed childbearing among older women in these regions.
HDP burden associated with SDI
In 2021, a significant inverse correlation was observed between the SDI and the health metrics of HDP within the WCBA, including prevalence rates, incidence rates, mortality rates, and DALY rates. Across the 21 regions, the disease burden of HDP in WCBA remained relatively stable when the SDI value was between 0.5 and 0.7. Interestingly, the burden of HDP peaked at an SDI value of 0.8. Notably, regions such as Central Sub-Saharan Africa and Southern Sub-Saharan Africa exhibited a higher burden of HDP than anticipated. In contrast, areas like East Asia, Central Europe, and Central Asia had a lower burden than expected (Figure 5 and Supplementary Figures S7A–C). It indicated that the relationship between HDP burden and SDI is not a simple linear one. This complex relationship may be influenced by a combination of factors specific to each region, such as population structure, distribution of healthcare resources, lifestyle, and socio-economic conditions.
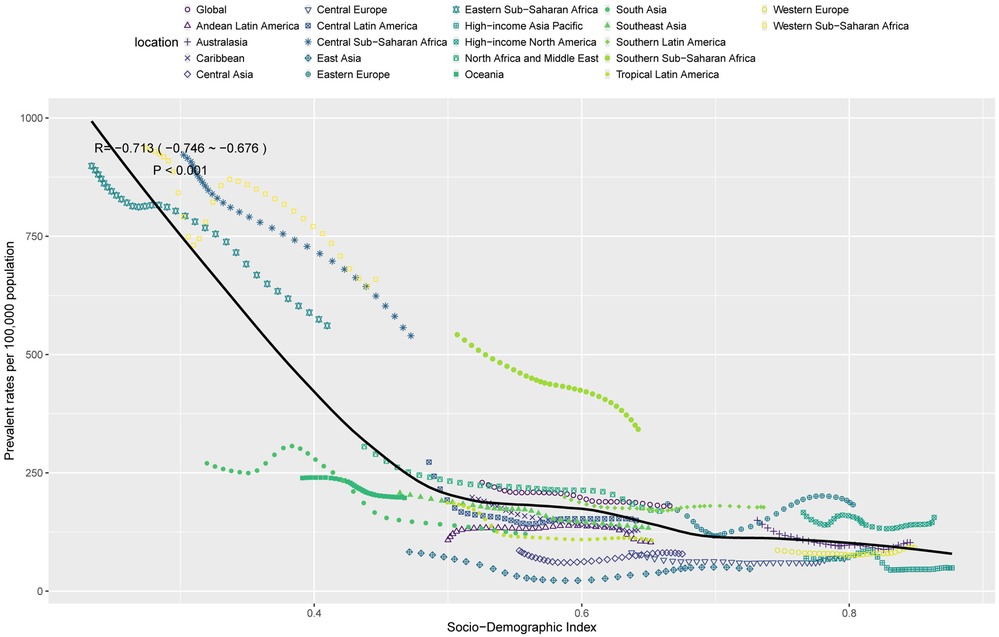
Figure 5. Correlation between SDI and prevalence rates per 100,000 population of HDP in WCBA across 21 GBD regions.
Discussion
The GBD database analysis indicates a persistent global escalation in the incidence of HDP from 1990 to 2019, characterised by significant regional and age-specific disparities (3). However, the advent of the Coronavirus Disease 2019 (COVID-19) pandemic from 2019 to 2021 has posed tremendous challenges to delivering quality health services, with the potential impact on health outcomes still under investigation. For instance, COVID-19 infection during pregnancy can exacerbate the risk of severe maternal morbidity (19), subsequently leading to an elevated incidence of preterm births (20) and the necessity for cesarean deliveries (21). Additionally, the isolation imposed by the pandemic has been associated with a higher prevalence of postnatal depression among affected women (22–24). There is also evidence suggesting a potential link between maternal infections and the development of neurodevelopmental disorders in offspring (25). The infection results in prolonged hospital stays for mothers and infants (26) and escalates healthcare expenditure due to increased hospitalisation costs (27). Ongoing longitudinal studies further investigate these associations to elucidate the long-term implications of maternal COVID-19 infection on maternal and child health (28). Despite these adversities, the prevalence and morbidity of HDP in 2021 remained persistently elevated compared to 1990 levels, yet there was a notable reduction in patient fatalities and DALYs. This observed decline may be intricately linked to the targeted policy interventions implemented by the WHO, which have been instrumental even amidst the unprecedented health crisis of COVID-19.
Fan et al. observed a notable DALYs cases escalation among patients with D2M in regions characterised by middle-high and high SDI, signifying an augmented health burden in these locales (29). Conversely, the prevalence cases of childhood anaemia under five years of age exerts a considerable health burden, particularly in regions with lower SDI, where the economic implications of this condition are exacerbated (30). Asian women exhibit a heightened propensity for cancer, which subsequently amplifies the global health burden associated with this disease in lower SDI (31). Similarly, the level of SDI is negatively correlated with the prevalence cases, incidence cases, mortality cases and DALYs cases of HDP. The higher the SDI, the higher the economic and health care level, the better the care for HDP, and consequently, the lower the corresponding prevalence cases, incidence cases, mortality cases, and DALYs cases.
Over the past 32 years, the most significant increases in prevalence rates and DALY rates of HDP were showed in Western Sub-Saharan Africa and Andean Latin America, which may be attributed to social factors such as dietary habits (32, 33), industrialisation or urbanisation (34), inadequate health care services (35), and poor air quality (36). Our study also shows that prevalence and incidence are still increasing in most countries, but mortality and DALYs are decreasing in most countries. This suggests that, at the global level, healthcare and public health management efforts are positively affecting and reducing the causes of HDP.
Regarding age patterns, the global burden of HDP will be particularly severe in the 25–29 age group in 2021. In this age group, women in this stage of life have the highest fertility rates and the most significant burden. This highlights the importance of special attention and health management for this age group. The prevalence cases, incidence cases, mortality cases and DALYs cases of HDP have varied globally with age and economy over the last 32 years. The age group 30–39 years showed the most significant percentage change among them. In this case, the number of HDP cases transitioned from low to high age groups, showing a trend of increasing and decreasing first, and the peak of the number of cases showed a gradual backward shift in the age group with rising SDI. The higher the age of women in the reproductive years, the higher the complications of childbirth and the higher the prevalence of HDP. Advanced age (37) and economic disparities (38) are all significant risk factors for increased prevalence and morbidity. In economically developed regions, the implementation of standardized control strategies coupled with adequate financial investment enables effective intervention at the early stages of disease. This approach can effectively curb the further progression of illness, thereby preventing the exacerbation of the condition. Such early interventions not only contribute to the improvement of patients’ health outcomes but also significantly reduce the economic burden imposed by the disease on the region.
Currently, the global prevalence cases and incidence cases of HDP are still on the rise, while mortality cases and DALYs cases are on the decline. This indicates the progress of global medical technology and the effective implementation of public health interventions (39). In the future, it is necessary to continue strengthening global public health interventions. The global burden is uneven, with the level of SDI being the main reason (16). In the future, more attention needs to be paid to low SDI regions to improve the accessibility of medical resources. In low SDI regions, the burden is heavier among young women, while in high SDI regions, the burden is heavier among older women. Based on the above phenomenon, personalized policy-making and interventions are needed. For young women in low SDI regions, local policies should strengthen basic health care, increase the coverage of health education, and provide targeted maternal health services (40). For older women in high SDI regions, specialized medical services for older pregnant women should be provided, chronic disease management should be strengthened, and pre-pregnancy, pregnancy, and postpartum health consultations should be offered (41–43).
Limitation
This study has several limitations. First, the estimates presented are not exhaustive, as HDP encompass various clinical subtypes with distinct symptoms, leading to potential misdiagnosis, particularly in economically underdeveloped regions where disease recognition is inadequate, resulting in an underestimation of the burden. Second, the GBD data, which this study relies on, heavily depends on modelling due to the absence of primary data in many countries. Furthermore, the global impact of COVID-19, including delayed births and constrained healthcare resources, may have compromised the accuracy of raw data.
Conclusions
Overall, the global burden of HDP has exhibited a significant downward trend over the past 32 years. From the perspective of socio-economic factors, a negative correlation exists between DALYs burden and the SDI, regardless of specific regions or countries. The increase in disease burden is particularly pronounced in low SDI regions. In terms of age distribution patterns, the global burden of HDP peaked in the 25–29 age group in 2021. However, the most significant increase in HDP burden occurred in the 30–39 age group. Moreover, as SDI increases, the age group with the most substantial burden increase tends to shift towards older ages. Given these findings, it is imperative to implement targeted interventions based on the characteristics of different regions, economic statuses, and age groups in order to effectively mitigate the associated economic burden.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
ZT: Writing – original draft. CM: Investigation, Software, Writing – review & editing. JL: Conceptualization, Writing – review & editing. CL: Funding acquisition, Resources, Visualization, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We sincerely appreciate all the participants of the GBD 2021 for their contribution.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fgwh.2025.1533843/full#supplementary-material
Abbreviations
WCBA, women of childbearing age; GBD, global burden of disease; DALYs, disability-adjusted life years YLLs years of life lost; YLDs, years lived with disability; YLLs, years of life lost due to premature mortality; UI, uncertainty intervals; SDI, socio-demographic index; EAPC, estimated annual percentage change; CI, confidence intervals; HDP, hypertensive disorders of pregnancy.
References
1. Cífková R. Hypertension in pregnancy: a diagnostic and therapeutic overview. High Blood Press Cardiovasc Prev. (2023) 30(4):289–303. doi: 10.1007/s40292-023-00582-5
2. Metoki H, Iwama N, Hamada H, Satoh M, Murakami T, Ishikuro M, et al. Hypertensive disorders of pregnancy: definition, management, and out-of-office blood pressure measurement. Hypertens Res. (2022) 45(8):1298–309. doi: 10.1038/s41440-022-00965-6
3. Fu R, Li Y, Li X, Jiang W. Hypertensive disorders in pregnancy: global burden from 1990 to 2019, current research hotspots and emerging trends. Curr Probl Cardiol. (2023) 48(12):101982. doi: 10.1016/j.cpcardiol.2023.101982
4. Kwapong YA, Boyer T, Adebowale O, Ogunwole SM, Vaught AJ, Ndumele CE, et al. Association of prepregnancy cardiometabolic health with hypertensive disorders of pregnancy among historically underrepresented groups in the United States. J Am Heart Assoc. (2024) 31:e035526. doi: 10.1161/JAHA.124.035526
5. Zhao W, Di J, Huang A, Yang Q, Hu H. Incidence and risk factors of hypertensive disorders of pregnancy—8 provinces, China, 2014–2018. China CDC weekly. (2021) 3(22):476–82. doi: 10.46234/ccdcw2021.122
6. Noubiap JJ, Bigna JJ, Nyaga UF, Jingi AM, Kaze AD, Nansseu JR, et al. The burden of hypertensive disorders of pregnancy in Africa: a systematic review and meta-analysis. J Clin Hypertens. (2019) 21(4):479–88. doi: 10.1111/jch.13514
7. Li X, Zhang W, Lin J, Liu H, Yang Z, Teng Y, et al. Hypertensive disorders of pregnancy and risks of adverse pregnancy outcomes: a retrospective cohort study of 2368 patients. J Hum Hypertens. (2021) 35(1):65–73. doi: 10.1038/s41371-020-0312-x
8. Yang L, Huang C, Zhao M, Lee PMY, Zhang C, Yu Y, et al. Maternal hypertensive disorders during pregnancy and the risk of offspring diabetes mellitus in childhood, adolescence, and early adulthood: a nationwide population-based cohort study. BMC Med. (2023) 21(1):59. doi: 10.1186/s12916-023-02762-5
9. Xu J, Li T, Wang Y, Xue L, Miao Z, Long W, et al. The association between hypertensive disorders in pregnancy and the risk of developing chronic hypertension. Front Cardiovasc Med. (2022) 9:897771. doi: 10.3389/fcvm.2022.897771
10. Tassi A, Sala A, Mazzera I, Restaino S, Vizzielli G, Driul L. Long-term outcomes of patients with preeclampsia, a review of the literature. Hypertens Pregnancy. (2023) 42(1):2217448. doi: 10.1080/10641955.2023.2217448
11. Conti-Ramsden F, Fleminger J, Lanoue J, Chappell LC, Battersby C, UK Neonatal Collaborative. The contribution of hypertensive disorders of pregnancy to neonatal unit admissions and iatrogenic preterm delivery at <34 + 0 weeks’ gestation in the UK: a population-based study using the national neonatal research database. BJOG: An Int J Obstet Gynaecol. (2025) 132(3):306–17. doi: 10.1111/1471-0528.17976
12. Venkatesh KK, Perak AM, Wu J, Catalano P, Josefon JL, Costantine MM, et al. Impact of hypertensive disorders of pregnancy and gestational diabetes mellitus on offspring cardiovascular health in early adolescence. Am J Obstet Gynecol. (2025) 232(2):218.e1–218.e12. doi: 10.1016/j.ajog.2024.04.037
13. Zhou Y, Yin S, Sheng Q, Yang J, Liu J, Li H, et al. Association of maternal age with adverse pregnancy outcomes: a prospective multicenter cohort study in China. J Glob Health. (2023) 13:04161. doi: 10.7189/jogh.13.04161
14. Hernandez-Castro I, Rifas-Shiman SL, Lin P-ID, Chavarro JE, Gold DR, Zhang M, et al. First trimester prenatal metal mixtures, vitamins, and hypertensive disorders of pregnancy in the project viva cohort. Environ Int. (2024) 190:108909. doi: 10.1016/j.envint.2024.108909
15. Wang W, Xie X, Yuan T, Wang Y, Zhao F, Zhou Z, et al. Epidemiological trends of maternal hypertensive disorders of pregnancy at the global, regional, and national levels: a population-based study. BMC Pregnancy Childbirth. (2021) 21(1):364. doi: 10.1186/s12884-021-03809-2
16. Jiang L, Tang K, Magee LA, von Dadelszen P, Ekeroma A, Li X, et al. A global view of hypertensive disorders and diabetes mellitus during pregnancy. Nat Rev Endocrinol. (2022) 18(12):760–75. doi: 10.1038/s41574-022-00734-y
17. Escobar MF, Benitez-Díaz N, Blanco-Londoño I, Cerón-Garcés C, Peña-Zárate EE, Guevara-Calderón LA, et al. Synthesis of evidence for managing hypertensive disorders of pregnancy in low middle-income countries: a scoping review. BMC Pregnancy Childbirth. (2024) 24(1):622. doi: 10.1186/s12884-024-06796-2
18. Cen J, Wang Q, Cheng L, Gao Q, Wang H, Sun F. Global, regional, and national burden and trends of migraine among women of childbearing age from 1990 to 2021: insights from the global burden of disease study 2021. J Headache Pain. (2024) 25(1):96. doi: 10.1186/s10194-024-01798-z
19. de Montalvão França APF, Paixão JTR, de Souza Fonseca RR, Laurentino RV, de Montalvão Leite LGF, Veras ASF, et al. Clinical characteristics of pregnant women with COVID-19 and infection outcomes in one of the largest cities in the Brazilian Amazon. BMC Infect Dis. (2024) 24(1):1175. doi: 10.1186/s12879-024-09982-x
20. Khalil EM, Madney YM, Hassan M, Fahmy AM, Alshammari SO, Alshammari QA, et al. Maternal and fetal outcome of COVID-19 infection among pregnant women. Medicina. (2024) 60(10):1676. doi: 10.3390/medicina60101676
21. Yeniocak AS, Tercan C, Dagdeviren E, Arabaci O, Arabaci EEG. Impact of SARS-CoV-2 infection and vaccination on cesarean section outcomes: a retrospective analysis. Ann Saudi Med. (2024) 44(5):306–18. doi: 10.5144/0256-4947.2024.306
22. Oh DS, Kim E, Normand R, Lu G, Shook LL, Lyall A, et al. SARS-CoV-2 infection elucidates features of pregnancy-specific immunity. Cell Rep. (2024) 43(11):114933. doi: 10.1016/j.celrep.2024.114933
23. Blocklinger KL, Gumusoglu SB, Kenney AS, Faudel AJ, Faro E, Brandt D, et al. Depression in the time of COVID-19: examination of prenatal and postpartum depression, rurality, and the impact of COVID-19. J Affect Disord. (2024) 370:337–47. doi: 10.1016/j.jad.2024.10.081
24. Evans C, Clancy G, Evans K, Booth A, Nazmeen B, Sunney C, et al. Optimising digital clinical consultations in maternity care: a realist review and implementation principles. BMJ Open. (2024) 14(10):e079153. doi: 10.1136/bmjopen-2023-079153
25. Hill RA, Gibbons A, Suwakulsiri W, Taseska A, Darke H, Malhotra A, et al. Investigating the impact of severe maternal SARS-CoV-2 infection on infant DNA methylation and neurodevelopment. Mol Psychiatry. (2024) 30:1976–84. doi: 10.1038/s41380-024-02808-x
26. Metersky ML, Rodrick D, Ho S-Y, Galusha D, Timashenka A, Grace EN, et al. Hospital COVID-19 burden and adverse event rates. JAMA Network Open. (2024) 7(11):e2442936. doi: 10.1001/jamanetworkopen.2024.42936
27. Hitch D, Angeles MR, Lau E, Nicola-Richmond K, Bennett C, Said CM, et al. Hospital costs of COVID-19, post-COVID-19 condition and other viral pneumonias: a cost comparison analysis. Med J Aust. (2024) 221(Suppl 9):S23–30. doi: 10.5694/mja2.52465
28. Muñoz-Chápuli Gutiérrez M, Prat AS, Vila AD, Claverol MB, Martínez PP, Recarte PP, et al. Post-COVID-19 condition in pregnant and postpartum women: a long-term follow-up, observational prospective study. EClinicalMedicine. (2024) 67:102398. doi: 10.1016/j.eclinm.2023.102398
29. Fan S, Xu J, Wu J, Yan L, Ren M. Spatiotemporal trends of type 2 diabetes due to low physical activity from 1990 to 2019 and forecasted prevalence in 2050: a global burden of disease study 2019. J Nutr Health Aging. (2024) 28(11):100402. doi: 10.1016/j.jnha.2024.100402
30. Liu Y, Ren W, Wang S, Xiang M, Zhang S, Zhang F, et al. Global burden of anemia and cause among children under five years 1990–2019: findings from the global burden of disease study 2019. Front Nutr. (2024) 11:1474664. doi: 10.3389/fnut.2024.1474664
31. Huang Z, Wang J, Liu H, Wang B, Qi M, Lyu Z, et al. Global trends in adolescent and young adult female cancer burden, 1990–2021: insights from the global burden of disease study. ESMO Open. (2024) 9(11):103958. doi: 10.1016/j.esmoop.2024.103958
32. Bosu WK. An overview of the nutrition transition in West Africa: implications for non-communicable diseases. Proc Nutr Soc. (2015) 74(4):466–77. doi: 10.1017/S0029665114001669
33. Nahla K, Ibrahim BA, Bahaa-Eldin EAR. Association between dietary patterns and pregnancy induced hypertension: a case control study from Sudan. Afr Health Sci. (2022) 22(4):368–74. doi: 10.4314/ahs.v22i4.42
34. Bhuiyan MA, Galdes N, Cuschieri S, Hu P. A comparative systematic review of risk factors, prevalence, and challenges contributing to non-communicable diseases in south Asia, Africa, and caribbeans. J Health Popul Nutr. (2024) 43(1):140. doi: 10.1186/s41043-024-00607-2
35. Olujitan M, Ayanbadejo PO, Umeizudike K, Oyapero A, Okunseri C, Butali A. Periodontal diseases in Africa. Periodontology 2000. (2024). doi: 10.1111/prd.12617
36. Creed IF, Erratt KJ, Henley P, Tsimbiri PF, Bend JR, Shivoga WA, et al. A geo-gender-based analysis of human health: the presence of cut flower farms can attenuate pesticide exposure in African communities, with women being the most vulnerable. J Glob Health. (2024) 14:04064. doi: 10.7189/jogh.14.04064
37. Noah AI, Comeaux CR, Hill AV, Perez-Patron MJ, DePaoli Taylor B. Maternal characteristics impact the relationship between fetal sex and superimposed preeclampsia. Pregnancy Hypertens. (2024) 38:101165. doi: 10.1016/j.preghy.2024.101165
38. Alur A, Phipps JE, Simmons LA. Socioecological factors influencing the risk of developing hypertensive disorders of pregnancy in India: a rapid review. BMC Pregnancy Childbirth. (2024) 24(1):669. doi: 10.1186/s12884-024-06879-0
39. Belizán JM, Gibbons L, Cormick G. Maternal mortality reduction: a need to focus actions on the prevention of hypertensive disorders of pregnancy. Int J Equity Health. (2021) 20(1):194. doi: 10.1186/s12939-021-01535-x
40. Adu-Bonsaffoh K, Tamma E, Nwameme AU, Browne JL. Health professionals’ perspectives on clinical challenges in managing hypertensive disorders of pregnancy and recommendations for improving care: a multi-center qualitative study. Front Global Women’s Health. (2022) 3:968914. doi: 10.3389/fgwh.2022.968914
41. Zhao X, Kong W, Jiang Y, Sui F. Global burden, trends and inequalities of maternal hypertensive disorders among reproductive-age women of advanced maternal age, 1990–2021: a population-based study. Front Global Women’s Health. (2025) 6:1513909. doi: 10.3389/fgwh.2025.1513909
42. Lee JY, Lee SH. Hypertensive disorders of pregnancy: advances in understanding and management. Clin Hypertens. (2025) 31:e1. doi: 10.5646/ch.2025.31.e1
Keywords: GBD 2021, women of childbearing age, disease burden, hypertensive disorders in pregnancy, DALYs
Citation: Tang Z, Ma C, Liu J and Liu C (2025) Global, regional, and national trends and burden of hypertensive disorders in pregnancy among women of childbearing age from 1990 to 2021. Front. Glob. Women's Health 6:1533843. doi: 10.3389/fgwh.2025.1533843
Received: 19 December 2024; Accepted: 24 April 2025;
Published: 9 May 2025.
Edited by:
Muhabaw Shumye Mihret, University of Gondar, EthiopiaReviewed by:
SiewMooi Ching, Universiti Putra Malaysia, MalaysiaYixiao Wang, Southeast University, China
Copyright: © 2025 Tang, Ma, Liu and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chongdong Liu, bGl1Y2hvbmdkb25nQGNjbXUuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
‡ORCID:
Chongdong Liu
orcid.org/0000-0001-8885-194X
 Zhongyun Tang
Zhongyun Tang Chao Ma
Chao Ma Jin Liu1,†
Jin Liu1,† Chongdong Liu
Chongdong Liu