- 1Department of Midwifery, College of Medicine and Health Sciences, Debre Markos University, Debre-Markos, Ethiopia
- 2Department of Public Health, College of Medicine and Health Sciences, Debre Markos University, Debre-Markos, Ethiopia
Background: Gestational diabetes mellitus (GDM) is the most common metabolic complication during pregnancy and is associated with an increased risk of maternal and neonatal adverse outcomes. Despite it being the most prevalent complication and leading to poor pregnancy outcomes, there have been very few studies assessing awareness of GDM among pregnant women in Ethiopia. Therefore, this study aimed to determine the awareness of GDM and its associated factors among pregnant women in public hospitals in the East Gojjam Zone, Northwest Ethiopia.
Methods: An institution-based cross-sectional study was conducted from June to August 2024. A systematic random sampling technique was utilized to select 423 participants. The data were collected using an interviewer-administered questionnaire. The collected data were analyzed using SPSS version 25. Binary logistic regression was fitted to assess the association between the explanatory variables and the outcome variable. Variables with a p-value less than 0.05, along with corresponding 95% confidence intervals, were used to declare statistical significance.
Results: This study found that 27.0% (95% CI: 0.23–0.31) of the pregnant women were aware of GDM. The most common source of information about GDM was friends at 53.2%, followed by family and healthcare professionals. Factors such as partner involvement [adjusted odds ratio (AOR) = 0.58; 95% CI = (0.35–0.95)], family history of chronic medical conditions [AOR = 5.20; 95% CI = (2.40–11.25)], mistimed but wanted pregnancies [AOR = 3.36; 95% CI = (1.40–8.10)], and being Muslim [AOR = 2.89; 95% CI = (1.34–6.24)] were significantly associated with awareness of GDM.
Conclusion: Only a small proportion of pregnant women were aware of GDM. Mistimed but desired pregnancies, partner involvement, and family history of chronic medical conditions were significantly associated with GDM awareness. In order to mitigate the growing burden of GDM, healthcare professionals need to do more to educate women about GDM during their prenatal care follow-ups.
1 Background
Gestational diabetes mellitus (GDM) is the presence of glucose intolerance during pregnancy that was not present before (1). Pregnancy often leads to insulin resistance, increasing the risk of developing diabetes (2). The main factors contributing to hyperglycemia in GDM are insulin resistance in peripheral tissues and inadequate insulin secretion by pancreatic beta-cells (3, 4).
Gestational diabetes mellitus is a common metabolic issue that occurs during pregnancy and is considered a significant public health concern with risks to the mother and child (5, 6). Globally, the prevalence of GDM varies from 1% to 28%, with an average prevalence of 15% (7). The International Diabetes Federation estimates that one out of six pregnancies is affected by diabetes, with GDM accounting for 86.4% of all cases of hyperglycemia during pregnancy (8). However, 87.6% of the burden and its consequences are found in low-and middle-income countries (LMICs), including in Africa, where obstetric and neonatal care is poor (9).
A review showed that the burden of GDM in the sub-Saharan African region was 14.3%, with the highest rates found in Central Africa at 20.4% and East Africa at 16.8%. A study conducted in Northwest Ethiopia showed that nearly 13% of women were diagnosed with GDM (10). This highlights the hidden challenges that GDM poses to the health of mothers and newborns in low- and middle-income countries such as Ethiopia.
Having gestational diabetes mellitus can lead to negative outcomes for the newborn, such as macrosomia, respiratory distress, premature birth, jaundice, hypoglycemia, stillbirth, and increased risk of neonatal intensive care unit admission (11–14). Additionally, neonatal GDM exposure raises the likelihood of hypertension, obesity, and type 2 diabetes mellitus (T2DM) later in life (15, 16). Gestational diabetes is also associated with a higher risk of adverse pregnancy outcomes, such as cesarean delivery, pregnancy-induced hypertension, premature rupture of membranes, antepartum hemorrhage, and postpartum hemorrhage (5, 14, 15, 17). Generally, GDM is a disease with high health and economic costs, but can be prevented or mitigated through proper antenatal screening, prompt diagnosis, early initiation of treatment, and ongoing monitoring, in which awareness is the baseline (13).
In the developed world, pregnant women are routinely screened for GDM. Despite sharing the highest burden in terms of prevalence and poor pregnancy outcomes, women are rarely screened for GDM in low- and middle-income countries (18). This can be due to economic issues and health system policies that have not implemented the recommendation of universal screening. However, the low screening rates are primarily due to a lack of awareness among pregnant women (19).
Awareness of GDM among pregnant women could be a key strategy in the primary prevention of the disease. This is because awareness of the condition among pregnant women leads to the adoption of healthy lifestyles and better health-seeking behaviors, including early screening, diagnosis, and management of the disease, all of which improve outcomes (20, 21).
A review of evidence confirmed that improving women's awareness of GDM is crucial for prevention, early management, and improving the long-term outcomes of the condition (22). In LMICs, very few studies have assessed the awareness of GDM among pregnant women (23), including in Ethiopia. Most of the available research conducted in Ethiopia has shown the burden of GDM, its associated factors, and its adverse outcomes.
Determining the existing GDM awareness gap among pregnant women is necessary to tackle the problem, plan appropriate strategies, and improve maternal and child health. Therefore, this study aimed to assess GDM awareness and its associated factors in Northwest Ethiopia.
2 Methods
2.1 Study area and period
This study was conducted from June to August 2024 in public hospitals in East Gojjam. The zone is found in the Amhara Region of Ethiopia, bordered to the south by the Oromia Region, to the west by West Gojjam, to the north by Debub Gondar, and to the east by Debub Wollo. The zone had an estimated population of 2,719,118 in 2020 (24). Based on the 2019 East Gojjam Zone Administration Office report, the zone had an estimated 91,634 women of reproductive age. This zone has 10 public hospitals, including one general hospital, eight primary hospitals, and one comprehensive specialized hospital, as well as 104 health centers and 406 health posts (25).
2.2 Study design
An institution-based cross-sectional study design was utilized.
2.3 Population
2.3.1 Source population
All pregnant women who had antenatal care (ANC) follow-ups at the public hospitals in the East Gojjam Zone.
2.3.2 Study population
All eligible pregnant women who had antenatal care follow-ups at the public hospitals in the East Gojjam Zone during the actual data collection period
2.4 Eligibility criteria
All pregnant women who had antenatal care follow-ups and were available at the time of data collection were included in this study, while pregnant women with pre-existing type-1 or type-2 diabetes and those who were seriously sick or unable to communicate during data collection were excluded.
2.5 Sample size determination
The assumption of the single population proportion formula was utilized to compute the sample size.
where n = the desired sample size, Zα/2 = the critical value corresponding to a 95% confidence interval (Zα/2 = 1.96), d = the margin of error (5%), and p = the estimated population proportion, which was 48% from the study conducted in Oromia, Ethiopia (26).
.
After considering a 10% non-response rate, the final sample size (Nf) = ni × (1/1-non-response rate); thus, Nf = 384 × (1/1–0.1) = 427.
2.6 Sampling procedure and method
A sample of five public hospitals was selected using a simple random sampling technique from the 10 public hospitals located in the East Gojjam Zone. The antenatal care registration book of each hospital was used to proportionally allocate the calculated sample size and determine the sampling fraction (k) (calculated using the population size divided by the sample size). The first mother was chosen using a simple random sampling technique among mothers who had an antenatal care follow-up on the day of data collection. Then, a systematic random sampling technique was used to select participants until the required sample size was achieved.
2.7 Study variables
2.7.1 Dependent variable
⮚ Awareness of GDM
2.7.2 Independent variables
⮚ Sociodemographic variables
⮚ Obstetric-related variables
⮚ Lifestyle and medical disease-related variables
2.8 Data collection tool and procedure
The data were collected using a face-to-face interviewer-administered questionnaire adapted from previously published articles (26, 27). The tool included the patient's background information and obstetric and medical history, as well as 15 questions assessing awareness of GDM, including its risk factors, diagnosis, treatment, and complications. The questions on risk factors assessed the patient’s awareness of the risk of GDM in patients with obesity prior to pregnancy, excessive weight gain during the present pregnancy, history of diabetes mellitus during previous pregnancies, and family history of diabetes.
Awareness of the course of GDM and its consequences to the unborn baby and mother was assessed by questions on whether GDM usually disappeared after delivery and whether women with GDM and children born to these women were at an increased risk for future T2DM and obesity.
To assess the patient’s awareness of the screening and diagnosis of GDM, questions on the type of test used and the timing of the test during pregnancy were asked. The options for the type of test used were urine test, blood test, blood test after a glucose load, and I do n't know. For the timing of the test, the options given were 12–16 weeks (3–4 months), 24–28 weeks (6–7 months), during delivery, and I do n't know. The answer 24–28 weeks (6–7 months) was considered the correct answer.
The patient’s awareness of the treatment for GDM was assessed using a question with the following options: diet and exercise, oral antidiabetic drugs, insulin injections, and I do n't know. Diet and exercise, insulin injections, and oral antidiabetic drugs were considered the correct response. Each correct response was given a score of 1 and each woman was scored out of a total of 15.
The tool was prepared in English and then translated into Amharic (the local language). It was then translated back into English to check its consistency. The face and content validity of the Amharic version questionnaires were assessed by four experts to control the threat to the validity of the data from the proposed instrument. In addition, the tool was pretested with 22 pregnant women who met the study criteria and was revised by experienced academic researchers. A well-structured tool, consisting of a chart review and interviewer-administered questions, was utilized to collect the data. The tool included sociodemographic information, obstetric and medical-related data, lifestyle-related data, and information on awareness of GDM. Five BSc midwives and five MSc professionals were recruited as data collectors and supervisors, respectively.
2.9 Assurance of data quality
A 2-day training session was provided to both data collectors and supervisors by the principal investigator about the objective of the study, the data collection tool, procedure, and how to fill out the questionnaire. The tool was pretested at Fenote Selam public hospital on 5% of the sample size to ensure the consistency and completeness of the questionnaire. Data collectors were supervised throughout the course of the data collection period. Then, the overall process was coordinated and controlled by the principal investigator. The principal investigator, supervisors, and data collectors had a discussion meeting after data collection to ensure completeness. Codes were given to the questionnaires during data collection. Furthermore, the collected data were entered into EpiData version 4.2 to minimize data entry errors and kept in the form of a file in a secure place. The results of the study were used only for the study's purpose.
2.10 Data analysis
The collected data were entered into EpiData version 4.2. It was then exported to SPSS version 25 for analysis. Descriptive statistics, such as frequency and summary statistics, were used to describe the characteristics of the study participants. A binary logistic regression model was used to determine the factors associated with the outcome variable. The model's fitness was assessed using the Hosmer–Lemeshow goodness-of-fit test for the adjusted model [chi-square (χ²) = 8.93, p = 0.35], which indicated a good fit. Multicollinearity among the independent variables was evaluated using variance inflation factors (VIFs), and no significant multicollinearity was detected. In the bivariable logistic regression, all explanatory variables with a p-value of 0.25 or less were considered for the multivariable logistic regression analysis. An adjusted odds ratio (AOR) with its corresponding 95% confidence intervals was used to indicate the association between the dependent and independent variables, and a p-value less than 0.05 indicated statistical significance.
2.11 Ethical clearance
Ethical clearance was obtained from the Institutional Ethical Review Board of the College of Medicine and Health Sciences, Debre Markos University (Approval No.: CMHS/R/C/Ser/D/315/01/16). Responsible officials and managers at each hospital were informed and permission was obtained. The participants (legal guardian/next of kin) provided written informed consent to participate in this study, and were informed that they had the right to withdraw from the study at any time.
2.12 Operational definitions of variables
The awareness score was determined based on the participants’ correct answers, with 1 point given for each correct answer and 0 for incorrect responses. It was measured using 15 awareness questions and categorized as “good awareness of GDM” (>9 out of 15), “fair awareness of GDM” (6–9 out of 15), and “poor awareness of GDM” (0–5 out of 15). Finally, pregnant women with good or fair knowledge were considered to be aware of GDM, and those with poor knowledge were considered to be unaware (21, 23).
3 Results
3.1 Demographic characteristics of participants
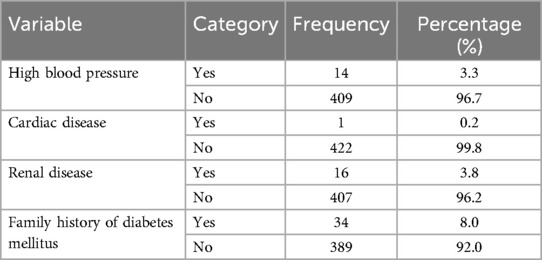
In total, 423 (99.1%) respondents participated in this study. The mean maternal age of the participants was 26.64 (SD 4.96) years, of which 63.6% were ≥25 years. Almost all of the respondents (421, 99.5%) were married. Approximately 30% of the study participants had attended college or higher education, while 56 (13.2%) had not received any formal education. Over half (51.8%) of the study participants were housewives (Table 1).
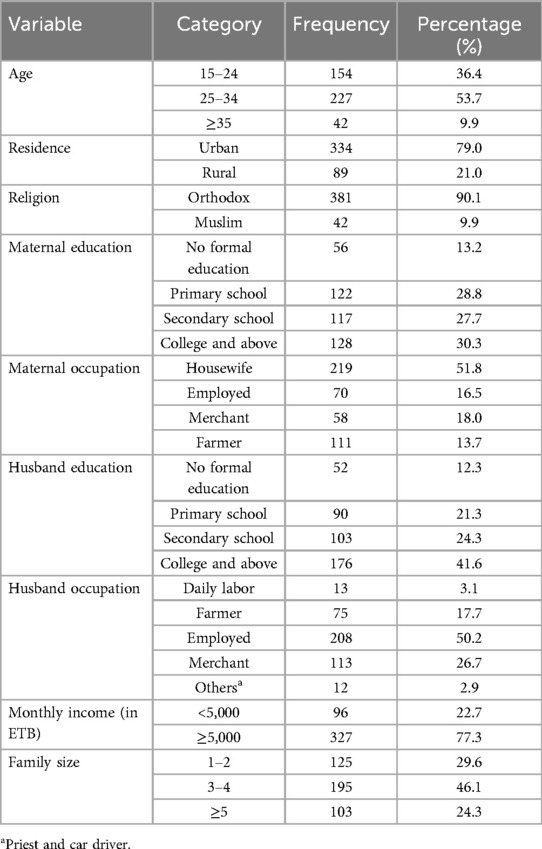
Table 1. Demographic characteristics of the study participants in the East Gojjam Zone public hospitals, Northwest Ethiopia, in 2024 (n = 423).
3.2 Maternal obstetrical characteristics
More than three-fifths (63.1%) of the women were multigravida; 393 (92.9%) of the women who participated had experienced a planned and wanted pregnancy. Approximately 12% (52, 12.3%) of the participants had a history of a bad obstetric complication, with abortions accounting for 71.2% of these cases, followed by early neonatal death and stillbirth in 17.3% and 11.5%, respectively. Approximately half (214, 50.5%) of the study participants were in their second trimester of pregnancy (Table 2).
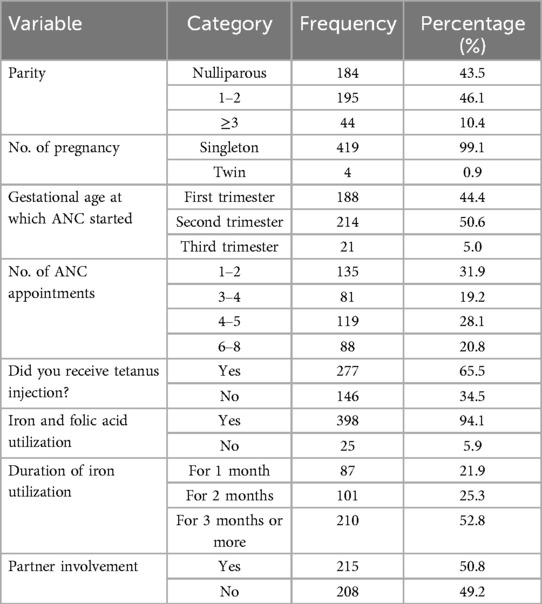
Table 2. Obstetrical characteristics of the pregnant women in the East Gojjam Zone public hospitals, Northwest Ethiopia, in 2024 (n = 423).
3.3 Lifestyle and medical history-related factors
Of the study participants, 8 (1.9%) had chronic medical disease, among which HIV accounted for 50% of these cases, followed by hepatitis and psychosis in the remaining 50%. All HIV-positive participants received antiretroviral therapy. Approximately 10% of the participants had a family history of chronic medical disease, with diabetes mellitus and hypertension being the most commonly noted conditions (Table 3).
3.4 Awareness of gestational diabetes mellitus
Participants were grouped into three categories based on their scores, with “good awareness of GDM” defined as a score of >9 out of 15, “fair awareness” as a score of 6–9 out of 15, and “poor awareness” as a score of 0–5 out of 15. Ultimately, women with good or fair awareness were considered to be aware of GDM, while those with poor knowledge were deemed to be unaware. Accordingly, the research revealed that only 27.0% (95% CI: 0.23–0.31) of the pregnant women were aware of GDM (Figure 1).
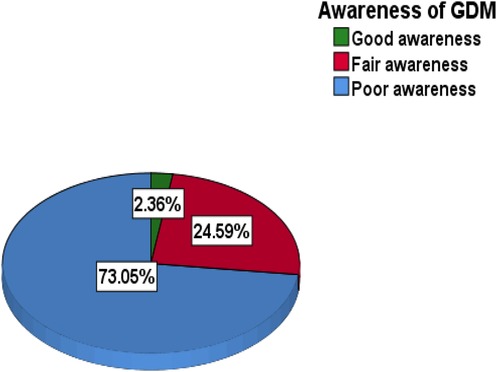
Figure 1. Levels of gestational diabetes mellitus awareness among pregnant women at public health institutions in the East Gojjam Zone public hospitals, Northwest Ethiopia, in 2024.
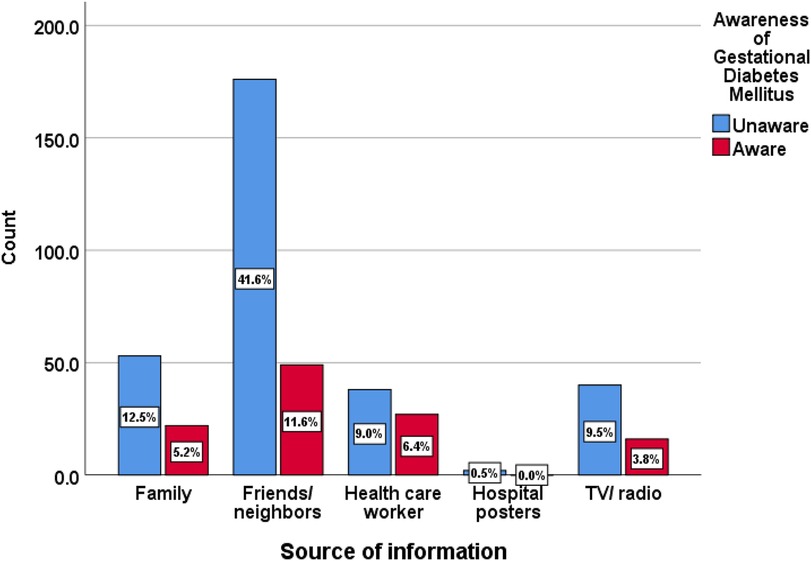
3.5 Source of information about GDM
Various sources of information about GDM were identified, with friends being the most common at 53.2%, followed by family members at 17.7% and healthcare professionals at 15.4% (Figure 2).
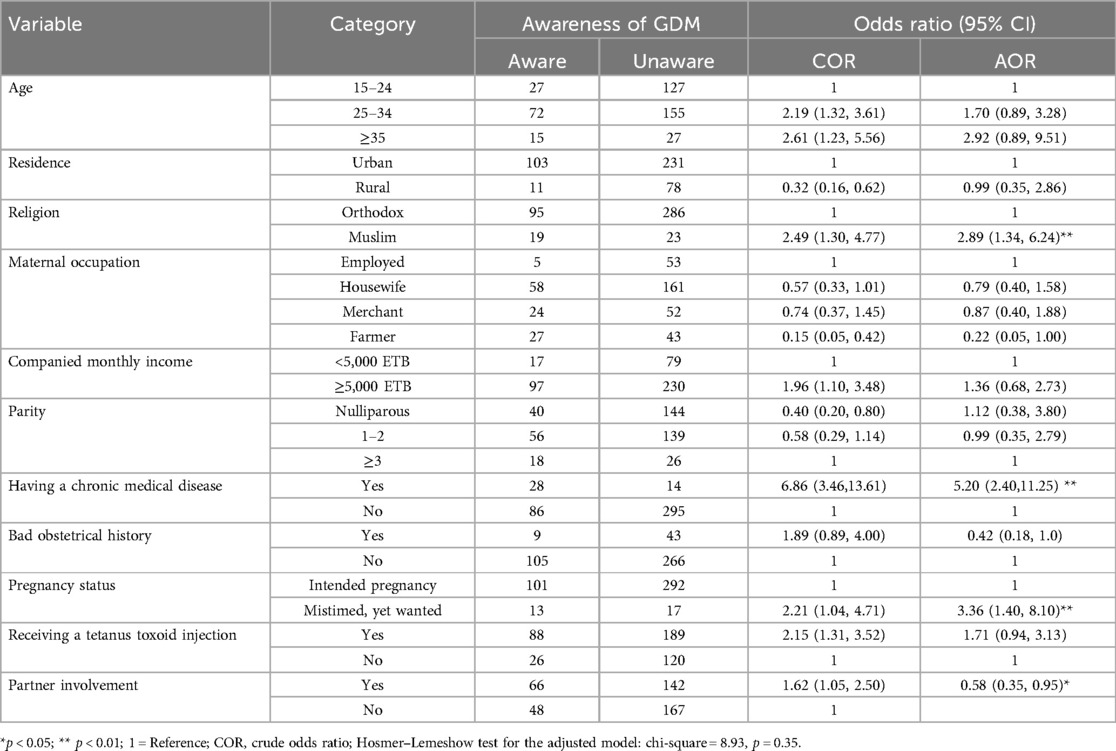
3.6 Factors associated with GDM awareness
In the bivariable logistic regression model, we considered various factors for further analysis, including maternal age, residence, religion, occupation, income, parity, receipt of tetanus toxoid injection and iron supplementation, pregnancy status, family history of medical disease, obstetrical history, past medical conditions, and partner involvement (all with p < 0.25).
In the final multivariable logistic regression model, several factors emerged as significantly associated with awareness of GDM. Women who were Muslim were 2.9 times more likely to have good awareness compared to Orthodox women (CI 1.34, 6.24; p = 0.007). Partner involvement also played a role; women who did not have an involved partner were less likely to have good awareness compared to those with involved partners (AOR: 0.58; CI 0.35, 0.95; p = 0.03). A family history of chronic medical disease (diabetes, hypertension, or both) increased the likelihood of good GDM awareness by 5.2 times (CI 2.40, 11.25; p < 0.001). Additionally, women with mistimed but wanted pregnancies were 3.4 times more likely to have good GDM awareness compared to those with planned and wanted pregnancies (CI 1.40, 8.10; p = 0.007) (Table 4).
4 Discussion
This study evaluated awareness of GDM and its associated factors among pregnant women in public hospitals in the East Gojjam Zone, Northwest Ethiopia. In this study, only 27% of the participants were aware of GDM. This finding is consistent with previous studies conducted in India (22%) (20), Uganda (31%) (23), Saudi Arabia (28), Nigeria (28.8%) (18), and Kenya (29.0%) (29). This implies that awareness of GDM among women is relatively comparable across different countries, despite variations in socioeconomic status.
However, the finding of this study was not comparable with other studies conducted in Ethiopia (48%) (26), Bangladesh (89.4%) (30), Nigeria (86.9%) (31), Egypt (69.6%) (27), and India, which reported awareness levels of 41.7% (22) and 74.4% (21). These variations could be attributed to differences in access to information. The studies conducted in Nigeria (86.9%) (31) and Egypt (69.6%) (27) reported that healthcare professionals were the primary source of information, while in this study, the most frequently cited sources of information about GDM were friends, followed by family and mass media. These findings emphasize the limited role of healthcare providers in Ethiopia regarding disseminating information about GDM. This highlights the need for improved communication strategies within the healthcare system to raise awareness among pregnant women and mitigate the growing burden of GDM.
The current study found that having a family history of chronic medical conditions was associated with increased awareness of GDM. This finding is comparable with previous studies conducted in Central Ethiopia and Bangladesh (30), which reported that a family history of diabetes was significantly linked to a higher awareness of GDM. This implies that women with affected relatives may be more familiar with the condition and its characteristics, leading to a better understanding of GDM (26).
This study also found a significant religious difference in awareness of GDM, with Muslim women being 2.9 times more likely to be aware of GDM compared to Orthodox Christian women. This may be due to the majority of Muslim participants in this study residing in urban areas, where access to health education and other social facilities that promote GDM awareness is readily available. This finding was also supported by prior studies conducted in India (20) and Kenya (32); they found similar findings regarding religious differences in GDM awareness among pregnant women.
Moreover, the study found that partner involvement in antenatal care follow-up plays a pivotal role in boosting awareness of GDM. Pregnant women without partner involvement were 42% less likely to be aware of GDM compared to those whose partners were involved. Previous studies have also supported this finding (33, 34). This indicates the importance of considering partner-based strategies in antenatal care follow-up, which can improve awareness and self-management of GDM.
Women who had mistimed but desired pregnancies were 3.4 times more likely to be aware of GDM compared to those with intended pregnancies. This is supported by previous studies (35, 36). A possible reason for this finding may be that a woman who has mistimed but still desired pregnancy may feel more pressure to have a healthy pregnancy. This could lead them to be more proactive in seeking out prenatal care, including health information on potential risks such as GDM.
5 Conclusion
Only a small proportion of the pregnant women in this study were aware of GDM. The most common sources of information about GDM were friends and family. Mistimed but desired pregnancies, partner involvement, and a family history of chronic medical conditions were significantly associated with GDM awareness. In order to mitigate the growing burden of GDM, healthcare professionals need to do more to educate women about GDM during their prenatal care follow-ups.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study involving humans was approved by the Institutional Ethical Review Board of the College of Medicine and Health Sciences, Debre Markos University. The study was conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
GM: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. KS: Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing. FB: Data curation, Project administration, Supervision, Writing – original draft, Writing – review & editing. MM: Project administration, Supervision, Writing – original draft, Writing – review & editing. MY: Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. MF: Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. AH: Project administration, Software, Supervision, Writing – original draft, Writing – review & editing. TG: Conceptualization, Methodology, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Financial support was received solely for data collection from Debre Markos University.
Acknowledgments
We would like to thank the study participants, data collectors, supervisors, and East Gojjam Zone Public Health Hospital's antenatal care unit staff who supported this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ANC, antenatal care; GDM, gestational diabetes mellitus.
References
1. World Health Organization. Diagnostic Criteria and Classification of Hyperglycaemia First Detected in Pregnancy. Geneva: World Health Organization (2013). Available online at: https://www.who.int/publications/i/item/WHO-NMH-MND-13.2 (Accessed May 26, 2024).
2. Baz B, Riveline J-P, Gautier J-F. Gestational diabetes mellitus: definition, aetiological and clinical aspects. Eur J Endocrinol. (2016) 174(2):R43–51. doi: 10.1530/EJE-15-0378
3. Plows JF, Stanley JL, Baker PN, Reynolds CM, Vickers MH. The pathophysiology of gestational diabetes mellitus. Int J Mol Sci. (2018) 19(11):3342. doi: 10.3390/ijms19113342
4. Barbour LA, McCurdy CE, Hernandez TL, Kirwan JP, Catalano PM, Friedman JE. Cellular mechanisms for insulin resistance in normal pregnancy and gestational diabetes. Diabetes Care. (2007) 30(Supplement 2):S112–9. doi: 10.2337/dc07-s202
5. Muche AA, Olayemi OO, Gete YK. Effects of gestational diabetes mellitus on risk of adverse maternal outcomes: a prospective cohort study in northwest Ethiopia. BMC Pregnancy Childbirth. (2020) 20(1):1–13. doi: 10.1186/s12884-020-2759-8
6. Macaulay S, Ngobeni M, Dunger DB, Norris SA. The prevalence of gestational diabetes mellitus amongst black South African women is a public health concern. Diabetes Res Clin Pract. (2018) 139:278–87. doi: 10.1016/j.diabres.2018.03.012
7. Jiwani A, Marseille E, Lohse N, Damm P, Hod M, Kahn JG. Gestational diabetes mellitus: results from a survey of country prevalence and practices. J Matern Fetal Neonatal Med. (2012) 25(6):600–10. doi: 10.3109/14767058.2011.587921
8. Cho N, Shaw J, Karuranga S, Huang Y, da Rocha Fernandes J, Ohlrogge A, et al. IDF diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. (2018) 138:271–81. doi: 10.1016/j.diabres.2018.02.023
9. Ogurtsova K, da Rocha Fernandes J, Huang Y, Linnenkamp U, Guariguata L, Cho NH, et al. IDF diabetes atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. (2017) 128:40–50. doi: 10.1016/j.diabres.2017.03.024
10. Muche AA, Olayemi OO, Gete YK. Prevalence of gestational diabetes mellitus and associated factors among women attending antenatal care at Gondar town public health facilities, Northwest Ethiopia. BMC Pregnancy Childbirth. (2019) 19(1):1–13. doi: 10.1186/s12884-019-2492-3
11. Metzger BE, Contreras M, Sacks D, Watson W, Dooley S, Foderaro M, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. (2008) 358(19):1991–2002. doi: 10.1056/NEJMoa0707943
12. Ringholm L, Damm P, Mathiesen ER. Improving pregnancy outcomes in women with diabetes mellitus: modern management. Nat Rev Endocrinol. (2019) 15(7):406–16. doi: 10.1038/s41574-019-0197-3
13. Wendland EM, Torloni MR, Falavigna M, Trujillo J, Dode MA, Campos MA, et al. Gestational diabetes and pregnancy outcomes-a systematic review of the World Health Organization (WHO) and the International Association of Diabetes in Pregnancy Study Groups (IADPSG) diagnostic criteria. BMC Pregnancy Childbirth. (2012) 12(1):1–13. doi: 10.1186/1471-2393-12-23
14. Natamba BK, Namara AA, Nyirenda MJ. Burden, risk factors and maternal and offspring outcomes of gestational diabetes mellitus (GDM) in sub-Saharan Africa (SSA): a systematic review and meta-analysis. BMC Pregnancy Childbirth. (2019) 19(1):1–11. doi: 10.1186/s12884-019-2593-z
15. Wang Z, Kanguru L, Hussein J, Fitzmaurice A, Ritchie K. Incidence of adverse outcomes associated with gestational diabetes mellitus in low-and middle-income countries. Int J Gynaecol Obstet. (2013) 121(1):14–9. doi: 10.1016/j.ijgo.2012.10.032
16. Boka A, Nigatu D. Assessment of adverse birth outcomes and associated factors among diabetic pregnant mothers who delivered at Mettu Karl Hospital, Illubabor Zone, south west Ethiopia-2018. Intern Med. (2019) 9(302):2. doi: 10.4172/2165-8048.1000300
17. Ewnetu S, Kebede T, Mekonnen A, Alebachew M, Shibeshi W. Effects of level of glycaemic control in reduction of maternal and perinatal complications among pregnant diabetic women at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. Ethiopian Pharmaceutical J. (2016) 32(2):159–70. doi: 10.4314/epj.v32i2.6
18. Ogu RN, Maduka O, Agala V, Alamina F, Adebiyi O, Edewor U, et al. Gestational diabetes mellitus knowledge among women of reproductive age in Southern Nigeria: implications for diabetes education. Int Q Community Health Educ. (2020) 40(3):177–83. doi: 10.1177/0272684X19876526
19. Dennison R, Fox R, Ward R, Griffin S, Usher-Smith J. Women’s views on screening for type 2 diabetes after gestational diabetes: a systematic review, qualitative synthesis and recommendations for increasing uptake. Diabetic Med. (2020) 37(1):29–43. doi: 10.1111/dme.14081
20. Dhyani V, Mahantashetti NS, Ganachari M, Kambar S, Ghatnatti V. Awareness of gestational diabetes mellitus among pregnant women attending a tertiary health center. Indian J Health Sci Biomed Res (KLEU). (2018) 11(1):51. doi: 10.4103/kleuhsj.kleuhsj_130_17
21. Shriraam V, Rani MA, Sathiyasekaran B, Mahadevan S. Awareness of gestational diabetes mellitus among antenatal women in a primary health center in South India. Indian J Endocrinol Metab. (2013) 17(1):146. doi: 10.4103/2230-8210.107861
22. Baskar K, Priya V, Gayathri R. Awareness of gestational diabetes and its risk factors among pregnant women in Thiruvallur district. Drug Invent Today. (2019) 11(6):1486–9.
23. Byakwaga E, Sekikubo M, Nakimuli A. Level of and factors associated with awareness of gestational diabetes mellitus among pregnant women attending antenatal care at Kawempe National Referral Hospital: a cross sectional study. BMC Pregnancy Childbirth. (2021) 21(1):1–8. doi: 10.1186/s12884-021-03927-x
24. Zeleke HM, Assefa B, Sergo T, Mekonnen N. Self-care practice and associated factors among hypertensive follow-up patients at East Gojjam Zone public hospitals, North West Ethiopia, 2021. Research Square [Preprint]. (2021). doi: 10.21203/rs.3.rs-303339/v1
25. Aynalem BY, Melesse MF. Health extension service utilization and associated factors in East Gojjam zone, Northwest Ethiopia: a community-based cross-sectional study. PLoS One. (2021) 16(8):e0256418. doi: 10.1371/journal.pone.0256418
26. Dissassa HD, Tufa DG, Geleta LA, Dabalo YA, Oyato BT. Knowledge on gestational diabetes mellitus and associated factors among pregnant women attending antenatal care clinics of North Shewa Zone public hospitals, Oromia Region, Central Ethiopia: a cross-sectional study. BMJ Open. (2023) 13(9):e073339. doi: 10.1136/bmjopen-2023-073339
27. Saad H, Aziz AA, Emad E, Gaber M. Awareness of gestational diabetes problem among Sohag Governorate women. Egypt J Intern Med. (2023) 35(1):52. doi: 10.1186/s43162-023-00236-x
28. Almutairi A, Almadawi T, Alharbi A, Aldmak A, Alharbi A, Albdrani A. The awareness regarding the effect of maternal diabetes on infants among women of childbearing age. Int J Med Dev Ctries. (2020) 4(6):947–52. doi: 10.24911/IJMDC.51-1580974725
29. Siuluta N, Sato M, Linh LK, Wanjihia V, Changoma MS, Huy NT, et al. Assessment of gestational diabetes mellitus knowledge, attitudes, and practices and associated factors among pregnant women at a district hospital in coastal Kenya. Trop Med Health. (2024) 52(1):74. doi: 10.1186/s41182-024-00630-3
30. Bhowmik B, Afsana F, Ahmed T, Siddiquee T, Pathan F, Mahtab H, et al. Evaluation of knowledge regarding gestational diabetes mellitus: a Bangladeshi study. Public Health. (2018) 161:67–74. doi: 10.1016/j.puhe.2018.04.017
31. Chikeme PC. Gestational diabetes mellitus: awareness, risk factors, perceived effects, and lifestyle intervention among pregnant women in a Nigerian tertiary health institution. Indian J Med Sci. (2024) 76:22–7. doi: 10.25259/IJMS_200_2022
32. Maina WK, Ndegwa ZM, Njenga EW, Muchemi EW. Knowledge, attitude and practices related to diabetes among community members in four provinces in Kenya: a cross-sectional study. Pan Afr Med J. (2011) 7(1). doi: 10.4314/pamj.v7i1.69095
33. Guo M, Shi WX, Parsons J, Forbes A, Kong M, Zhang YP, et al. The effects of a couple-based gestational diabetes mellitus intervention on self-management and pregnancy outcomes: a randomised controlled trial. Diabetes Res Clin Pract. (2023) 205:110947. doi: 10.1016/j.diabres.2023.110947
34. Guo M, Parsons J, Forbes A, Shi WX, Kong M, Zhang YP, et al. A qualitative study exploring partner involvement in the management of gestational diabetes mellitus: the experiences of women and partners. J Clin Nurs. (2024) 33(2):653–63. doi: 10.1111/jocn.16887
35. Yazdkhasti M, Pourreza A, Pirak A, Abdi F. Unintended pregnancy and its adverse social and economic consequences on health system: a narrative review article. Iran J Public Health. (2015) 44(1):12–21.26060771
Keywords: gestational diabetes mellitus, awareness, factors, pregnant women, Ethiopia
Citation: Mihiret GT, Solomon Wondmu K, Baye F, Minale M, Yechale M, Fikrie Melese M, Haimanot AB and Getaneh T (2025) Awareness of gestational diabetes mellitus and its associated factors among pregnant women in public hospitals in the East Gojjam Zone, Northwest Ethiopia: a cross-sectional study. Front. Glob. Women's Health 6:1535344. doi: 10.3389/fgwh.2025.1535344
Received: 27 November 2024; Accepted: 11 July 2025;
Published: 8 August 2025.
Edited by:
Yudhy Dharmawan, Diponegoro University, IndonesiaReviewed by:
Maria Rizzo, University of Messina, ItalySahaya Sona Thresa, Shri Sathya Sai Medical College and Research Institute (SSSMCRI), India
Copyright: © 2025 Mihiret, Solomon Wondmu, Baye, Minale, Yechale, Fikrie Melese, Haimanot and Getaneh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Getachew Tilaye Mihiret, Z2V0YWNoZXdfdGlsYXllQGRtdS5lZHUuZXQ=; Z2V0YWNoZXd0aWxheWUzMjIzQGdtYWlsLmNvbQ==
 Getachew Tilaye Mihiret
Getachew Tilaye Mihiret Kumlachew Solomon Wondmu
Kumlachew Solomon Wondmu Fekadu Baye
Fekadu Baye Mulunesh Minale1
Mulunesh Minale1 Misganaw Fikrie Melese
Misganaw Fikrie Melese Temesgen Getaneh
Temesgen Getaneh