- 1Faculty of Medicine, University of Medical Sciences and Technology, Kigali, Rwanda
- 2Department of Obstetrics and Gynecology, College of Medicine, Qassim University, Buraydah, Saudi Arabia
Introduction: Limited studies have assessed the accuracy of mid-upper arm circumference (MUAC) in diagnosing nutritional status among pregnant women in Sub-Saharan Africa, and none in Rwanda. This study aimed to evaluate the effectiveness of MUAC in detecting obesity among pregnant women at Kacyiru Hospital in Kigali, Rwanda.
Methods: This cross-sectional study was conducted at Kacyiru Hospital, a district hospital in Kigali, Rwanda. Standard procedures were used to measure MUAC, weight, and height, from which body mass index (BMI) was calculated. Receiver operating characteristic (ROC) curves were created to determine cutoff points using Youden's index (YI).
Results: A total of 689 women were enrolled. The median (interquartile range) age and gravidity were 29.0 (26.0–33.0) years and 2 (1–3), respectively. Among the 592 women (85.9%) with gestational ages of ≥20.0 weeks, 5 (0.7%) were underweight and 195 (28.3%) were obese. There was a significant correlation between BMI and MUAC (r = 0.78) across all women and within the early (r = 0.774) and late pregnancy subgroups. The optimal MUAC cutoff for detecting obesity (BMI ≥ 30.0 kg/m²) was ≥27.5 cm in both early and late pregnancies (YI = 0.58, sensitivity = 0.91, specificity = 0.67), with a high predictive value [area under the receiver operating characteristic curve (AUROCC) = 0.88, 95% confidence interval (CI) = 0.85–0.90]. In early pregnancy, the best MUAC cutoff was ≥29.5 cm (YI = 0.73, sensitivity = 0.92, specificity = 0.80), with a high predictive value (AUROCC = 0.87, 95% CI = 0.77–0.97). In late pregnancy, the best MUAC cutoff was ≥27.5 cm (YI = 0.62, sensitivity = 0.92, specificity = 0.71), with a high predictive value (AUROCC = 0.89, 95% CI = 0.87–0.92).
Conclusion: MUAC is a reliable indicator for detecting obesity in pregnant women. Further research with larger sample sizes and follow-up studies is needed to assess MUAC's ability to detect underweight status and related adverse pregnancy effects.
Introduction
Recent global reports (1) have highlighted a significant increase in the prevalence of overweight or obesity across all age groups, including in Sub-Saharan countries such as Rwanda (2). This trend extends to pregnant women worldwide (3). Being overweight or obese during pregnancy is associated with numerous adverse maternal and perinatal outcomes, such as gestational diabetes mellitus, gestational hypertension, increased rates of operative delivery, preterm birth, congenital malformations, and postpartum hemorrhage (4).
Preventing obesity during pregnancy and its complications requires effective measures. These measures depend on accurately assessing the extent of the problem, typically achieved through body mass index (BMI) evaluation (5, 6). However, BMI assessment is not without limitations, including the need for technical training and complex calculations. In contrast, mid-upper arm circumference (MUAC) exhibits minimal changes during pregnancy, making it a more reliable indicator of nutritional status during this period (7). Therefore, identifying an optimal alternative to BMI for assessing obesity is crucial (8).
Previous studies have demonstrated a significant positive correlation between MUAC and BMI among adults, including women of reproductive age, in various populations (8–10). However, limited data exist on the correlation between BMI and MUAC during pregnancy, with varying levels of correlation reported (7, 11–13). These studies have suggested different MUAC cutoff points for detecting obesity during pregnancy (7, 11). Moreover, MUAC has been proven effective in accurately detecting not only obesity but also excessive gestational weight gain (14) and undernutrition, along with their associated adverse effects, such as low birth weight (15). Few studies have examined the accuracy of MUAC in diagnosing nutritional status among pregnant women in Sub-Saharan Africa, and none have examined it in Rwanda. Given that anthropometric parameters, including MUAC, can vary across populations, there is an urgent need to establish local cutoff points for use during antenatal care. Therefore, this study aimed to assess MUAC's performance in detecting obesity among pregnant women in Rwanda.
Methods
Study area
This cross-sectional study was conducted at Kacyiru Hospital, a district hospital in Kigali, Rwanda, with a specialized maternal and child health unit that provides comprehensive services, including antenatal care, labor and delivery, obstetric and gynecological surgeries, and family planning. The medical staff comprises obstetrics and gynecology consultants, specialists, general practitioners, midwives, and nurses. Approximately 70–90 women attend antenatal consultations daily.
Study population
The study population included all pregnant women attending antenatal consultations at Kacyiru Hospital.
Inclusion criteria
The participants included all healthy pregnant women in early and late pregnancies carrying single fetuses and residing in Rwanda, as well as those who provided informed consent before participation.
Exclusion criteria
The following women were excluded: those with multiple pregnancies; those with chronic diseases, such as HIV, diabetes mellitus, hypertension, and thyroid disease; those who refused to participate; and those with pregnancy complications, such as hyperemesis gravidarum.
Sampling technique and sample size calculation
Hospital records indicated that 2,078 women attended antenatal consultations three months before the study initiation. Therefore, the required sample size of 689 women was determined by dividing the expected number of women (2,078) by the required sample size (689), yielding a ratio of approximately 3:1. Based on the selection criteria, eligible women were asked to sign an informed consent form. Their age, parity, and the date of their last menstrual period were recorded. Gestational age was calculated from the last menstrual period and confirmed by early-pregnancy ultrasound. MUAC was measured with a non-stretchable tape measure, with the midpoint between the acromion and olecranon processes used as the measurement point. Height was measured using a Seca 786 combinable stadiometer with a weighing scale (Hammer Steindamm 3–25, 22089 Hamburg, Deutschland, Germany). The participants stood barefoot, ensuring their heels, buttocks, and shoulder blades touched the back plate, with their heads positioned in the Frankfurt horizontal plane. Weight was measured using the same Seca 786 scale after the participants removed heavy clothing and shoes. Each measurement was taken twice, and the average was calculated; a third measurement was taken if there was any discrepancy between the initial measures. All instruments were calibrated daily. BMI was calculated using the standard formula: weight (kg)/height (m)2. The <18.5 kg/m2 and ≥30.0 kg/m2 BMI cutoff points were used to identify underweight and obese women, respectively.
Sample size calculation
Using an online sample size calculator (16) and based on a previous publication (17), we assumed that 30% of pregnant women in Kigali, Rwanda, would be obese. We further assumed that MUAC would have a sensitivity of 95% in detecting obesity among these pregnant women. A sample size of 689 women was used to achieve a 95% confidence interval with a precision of 0.05.
Statistics
The data were analyzed using SPSS for Windows, version 22.0 (IBM Corp., NY, USA). The age, gravidity, BMI, and MUAC of the participants were assessed for normality using the Shapiro–Wilk test and found to be non-normally distributed. Therefore, these data were expressed as median (interquartile range, IQR) and compared between women at early and late gestational ages using the non-parametric Mann–Whitney U test. A receiver operating characteristic (ROC) analysis was performed to assess the sensitivity, specificity, and optimal cutoffs of MUAC for detecting obesity in pregnant women. The ROC parameters were determined based on the highest Youden's index (YI), calculated as YI = sensitivity + specificity−1.
Results
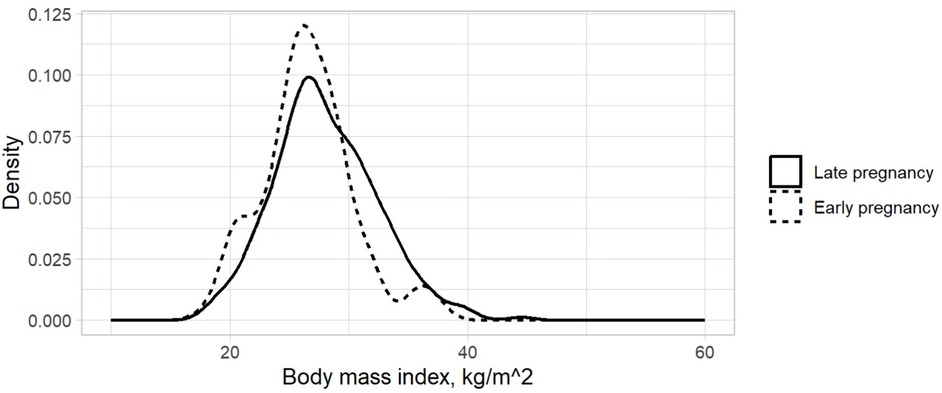
A total of 689 women were enrolled in the study. The median (IQR) age and gravidity of the participants were 29.0 (26.0–33.0) years and 2 (1–3), respectively. MUACs were 22.2–39.0 (median: 27.5) cm (Figure 1). The gestational ages were 8.0–40.0 (median: 33.0) weeks, and 592 (85.9%) of the women were at gestational ages ≥20.0 weeks. BMIs were 18.0–44.6 (median: 27.3 kg/m²) (Figure 2). Only 5 (0.7%) women were underweight, while 195 (28.3%) were classified as obese.
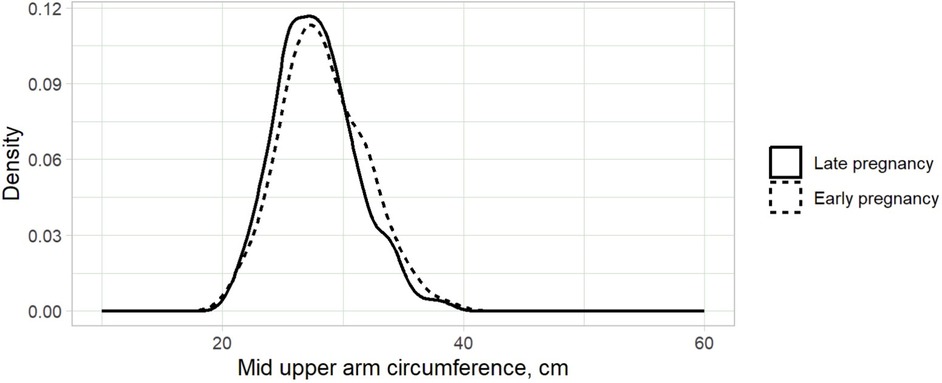
Figure 1. Kernel density plot of mid-upper arm circumference for pregnant women in Kigali, Rwanda, 2024.
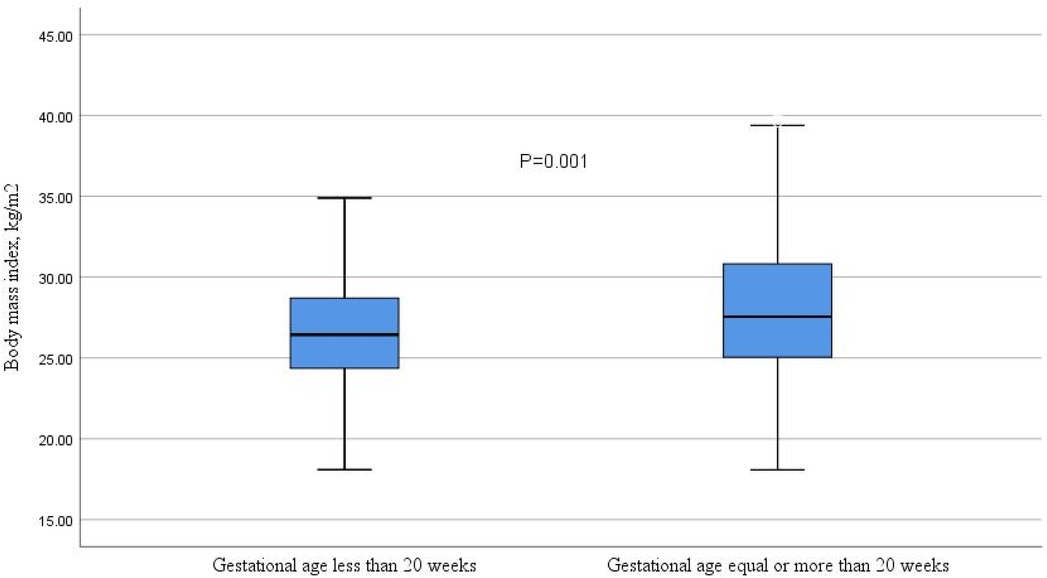
The median (IQR) BMI was significantly higher in women in late pregnancy (Figure 3). However, age, gravidity, and MUAC did not differ significantly between women in early and late pregnancies (Table 1). BMI and gestational age were positively correlated in all women (r = 0.188, P < 0.001), particularly in those in late pregnancy (r = 0.152, P < 0.001). In contrast, no significant correlation was found between BMI and gestational age among women in early pregnancy (r = 0.067, P = 0.517). A significant correlation was observed between BMI and MUAC in all women (r = 0.78, P < 0.001), as well as in both early pregnancy (r = 0.774, P < 0.001) and late pregnancy (r = 0.806, P < 0.001) (Figure 4).
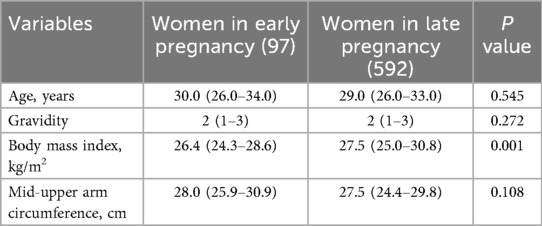
Table 1. Comparison of age, gravidity, body mass index, and mid-upper arm circumference between women in early and late gestational ages at Kigali, Rwanda, 2024.
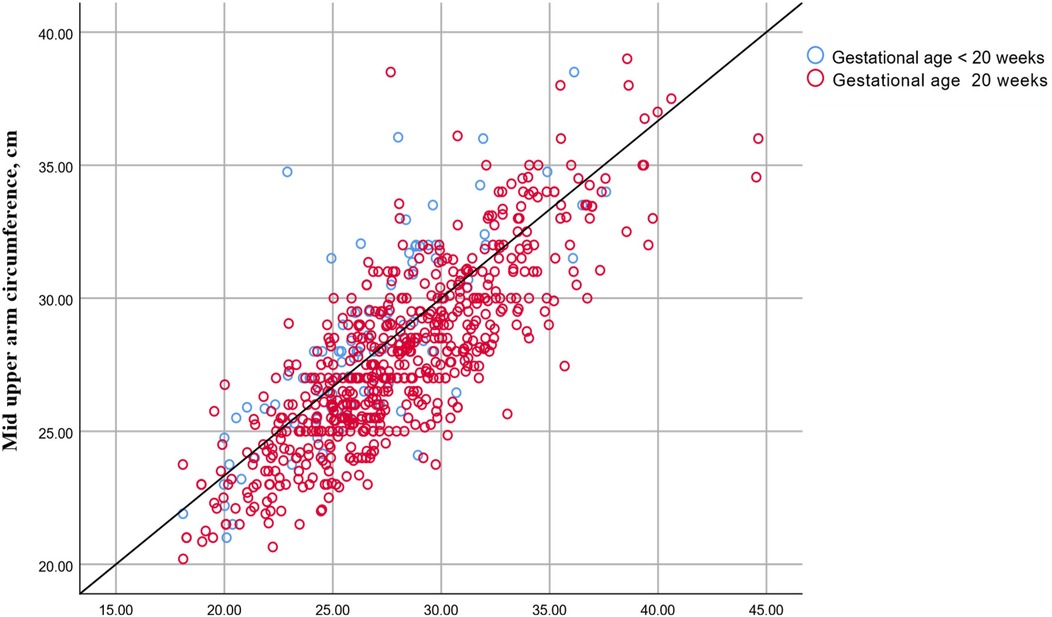
Figure 4. Correlation between body mass index and mid-upper arm circumference in pregnant women in Kigali, Rwanda, 2024.
The optimal MUAC cutoff for detecting obesity (BMI ≥ 30.0 kg/m2) was ≥ 27.5 cm in both early and late pregnancies [YI = 0.58, sensitivity = 0.91, specificity = 0.67], with a high predictive value [area under the receiver operating characteristic curve (AUROCC) = 0.88, 95% confidence interval (CI) = 0.85–0.90]. In early pregnancy, the best MUAC cutoff was ≥29.5 cm (YI = 0.73, sensitivity = 0.92, specificity = 0.80), with a high predictive value (AUROCC = 0.87, 95% CI = 0.77–0.97). In late pregnancy, the best MUAC cutoff was ≥27.5 cm (YI = 0.62, sensitivity = 0.92, specificity = 0.71), with a high predictive value (AUROCC = 0.89, 95% CI = 0.87–0.92) (Table 2, Figure 5).
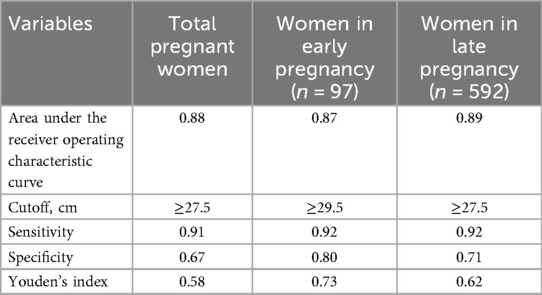
Table 2. Performance of mid-upper arm circumference for detecting obesity in pregnant women in Kigali, Rwanda, 2024.
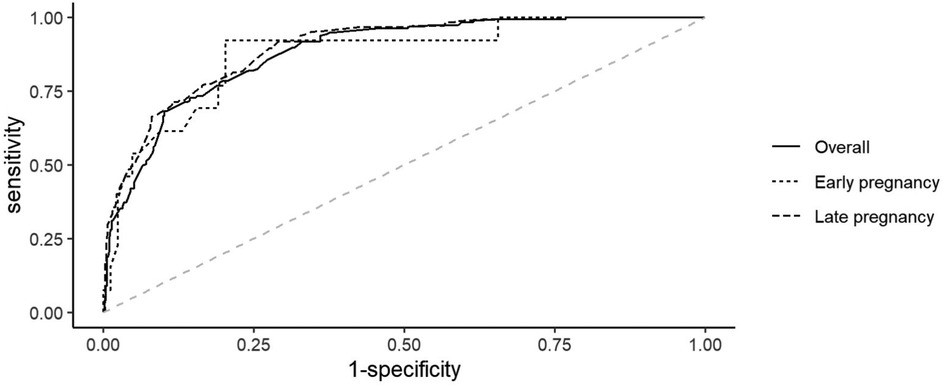
Figure 5. Receiver operating curve of mid-upper arm circumference for diagnosing obesity in pregnant women in Kigali, Rwanda, 2024.
Discussion
MUAC and BMI were significantly correlated among pregnant women (r = 0.78). This correlation was consistently observed in early (r = 0.774) and late (r = 0.806) pregnancies. These findings are consistent with previous studies that reported strong correlations between MUAC and BMI among pregnant women (7, 11–13). For instance, a study in Sudan found that MUAC and BMI were positively correlated among 688 pregnant women, with correlations of 0.734 in early pregnancy (<20 weeks) and 0.703 in late pregnancy (≥20 weeks) (12). Similarly, Fakier et al. reported that MUAC and BMI were strongly correlated in South Africa (r = 0.93) in early pregnancy (<20 weeks) and (r = 0.92) in late pregnancy (≥20 weeks) (11). Miele et al., in a large Brazilian study involving 1,165 pregnant women, reported significant correlations (r = 0.872) in the first trimester, (r = 0.870) in the second trimester, and (r = 0.831) in the third trimester (7). Cooley et al., in a study across London and Dublin with 2,912 pregnant women, also found that MUAC and BMI were positively correlated (r = 0.836) (13). Previous studies among non-pregnant women have shown that MUAC and BMI are positively correlated. For example, studies in Sudan (r = 0.639) (8), Iran (r = 0.91) (18), and India (r = 0.86) (19).
We identified a MUAC cutoff point of ≥27.5 cm for detecting obesity, demonstrating good predictive value (AUROCC = 0.88, YI = 0.58, sensitivity = 0.91, specificity = 0.67). A slightly higher MUAC cutoff of 28.0 cm was reported in Sudanese women in early pregnancy, albeit with somewhat lower accuracy (YI = 0.61, sensitivity = 76%, specificity = 86%) (12). For late pregnancy in the same study, the MUAC cutoff was 29 cm (YI = 0.67, sensitivity = 80.0%, specificity = 87.0%) (12). Comparatively, our identified MUAC cutoff point for obesity (≥27.5 cm) was lower than that reported in South Africa (30.5 cm) (11) and Brazil (30.15 cm for early pregnancy and 30.6 cm for late pregnancy) (7). These differences in MUAC cutoffs and their respective sensitivities and specificities may stem from variations in nutritional status, sociodemographic characteristics, genetics, and methodological differences. To determine the cutoff points, we used YI, which was not used in most previous studies. Although BMI differed significantly between early and late pregnancies, MUAC did not differ significantly between these stages in our study. Previous research has also noted variations in BMI across pregnancy stages (7), highlighting the potential advantage of using MUAC over BMI for assessing nutritional status during pregnancy.
Given the variability in BMI across gestational ages, assessing weight gain during pregnancy might offer a better indicator of nutritional status. Nonetheless, MUAC reliably assesses the rate of gestational weight gain as well (14).
Strengths and limitations
Strengths: This study addresses an important gap in maternal health research in Rwanda, where limited data exist on the use of MUAC as a screening tool for obesity in pregnancy. The sample size (n = 689) is large and provides sufficient statistical power to support the findings. Methods are clearly described, including calibration of instruments and standardized measurement protocols, which strengthens reliability. Use of ROC analysis and Youden's index to determine optimal MUAC cutoff points is statistically robust and appropriate. Findings are relevant to antenatal care in low-resource settings, where BMI measurements may be more difficult to obtain.
Limitations: Very few underweight women were included (0.7%, n = 5), which prevents meaningful conclusions on MUAC's ability to detect undernutrition. Pre-pregnancy BMI and gestational weight gain were not assessed, limiting understanding of MUAC's predictive role throughout pregnancy. The single-center, hospital-based setting in Kigali restricts generalizability to the wider Rwandan or Sub-Saharan African population. The cross-sectional design precludes conclusions on causality or prediction of maternal/neonatal outcomes. Analyzing factors such as education, income, and dietary habits could provide insights into the underlying causes of obesity and undernutrition. Moreover, we did not follow these women until delivery and assessed their maternal and perinatal outcomes, whether associated with BMI or MUAC. Investigating the relationship between MUAC and specific pregnancy complications (e.g., gestational diabetes, preterm birth, low birth weight) would enhance the clinical relevance of the study.
Conclusion
MUAC demonstrates good reliability in detecting obesity among pregnant women. Future research with larger sample sizes and longitudinal follow-up is warranted to further investigate MUAC's utility in detecting underweight and assessing pregnancy-related adverse effects.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval was obtained from the Scientific Research Committee, Faculty of Medicine, University of Medical Sciences and Technology, Kigali, Rwanda (# 19/02/2024). Informed written consent was obtained from all pregnant women. Personal identification information was not recorded on the questionnaire, and the collected information was kept confidential. All methods were performed in accordance with appropriate guidelines and regulations.
Author contributions
MA: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft. NA: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft. IA: Conceptualization, Methodology, Project administration, Resources, Software, Supervision, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The Researchers would like to thank the Deanship of Graduate Studies and Scientific Research at Qassim University for financial support (QU-APC-2025).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Phelps NH, Singleton RK, Zhou B, Heap RA, Mishra A, Bennett JE, et al. Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3,663 population-representative studies with 222 million children, adolescents, and adults. Lancet (London, England). (2024) 403:1027–50. doi: 10.1016/S0140-6736(23)02750-2
2. Keino BC, Carrel M. Spatial and temporal trends of overweight/obesity and tobacco use in East Africa: subnational insights into cardiovascular disease risk factors. Int J Health Geogr. (2023) 22:20. doi: 10.1186/S12942-023-00342-7
3. Poston L, Caleyachetty R, Cnattingius S, Corvalán C, Uauy R, Herring S, et al. Preconceptional and maternal obesity: epidemiology and health consequences. Lancet Diabetes Endocrinol. (2016) 4:1025–36. doi: 10.1016/S2213-8587(16)30217-0
4. Zhang Y, Lu M, Yi Y, Xia L, Zhang R, Li C, et al. Influence of maternal body mass index on pregnancy complications and outcomes: a systematic review and meta-analysis. Front Endocrinol (Lausanne). (2024) 15:1280692. doi: 10.3389/FENDO.2024.1280692
5. Bailey KV, Ferro-Luzzi A. Use of body mass index of adults in assessing individual and community nutritional status. Bull World Health Organ. (1995) 73(5):673–80. PMID: 8846494.8846494
7. Miele MJ, Souza RT, Calderon I, Feitosa F, Leite DF, Rocha Filho E, et al. Proposal of MUAC as a fast tool to monitor pregnancy nutritional status: results from a cohort study in Brazil. BMJ Open. (2021) 11:e047463. doi: 10.1136/bmjopen-2020-047463
8. Musa IR, Omar SM, Adam I. Mid-upper arm circumference as a substitute for body mass index in the assessment of nutritional status among adults in Eastern Sudan. BMC Public Health. (2022) 22:2056. doi: 10.1186/S12889-022-14536-4/TABLES/3
9. Sultana T, Karim MN, Ahmed T, Hossain MI. Assessment of under nutrition of Bangladeshi adults using anthropometry: can body mass index be replaced by mid-upper-arm-circumference? PLoS One. (2015) 10:e0121456. doi: 10.1371/journal.pone.0121456
10. Eleraky L, Issa R, Maciel S, Mbwana H, Rybak C, Frank J, et al. High prevalence of overweight and its association with mid-upper arm circumference among female and male farmers in Tanzania and Mozambique. Int J Environ Res Public Health. (2021) 18:9128. doi: 10.3390/IJERPH18179128
11. Fakier A, ChB M, Petro G, Fawcus S. Mid-upper arm circumference: a surrogate for body mass index in pregnant women. S Afr Med J. (2017) 107:606–10. doi: 10.7196/SAMJ.2017.vi7.12255
12. Salih Y, Omar SM, AlHabardi N, Adam I. The mid-upper arm circumference as a substitute for body mass index in the assessment of nutritional status among pregnant women: a cross-sectional study. Medicina. (2023) 59:1001. doi: 10.3390/medicina59061001
13. Cooley SM, Donnelly JC, Walsh T, Durnea U, Collins C, Rodeck CH, et al. The relationship between body mass index and mid-arm circumference in a pregnant population. J Obstet Gynaecol. (2011) 31:594–6. doi: 10.3109/01443615.2011.597892
14. Ng CM, Badon SE, Dhivyalosini M, Hamid JJM, Rohana AJ, Teoh AN, et al. Associations of pre-pregnancy body mass index, middle-upper arm circumference, and gestational weight gain. Sex Reprod Healthc. (2019) 20:60–5. doi: 10.1016/J.SRHC.2019.03.002
15. Ambreen S, Yazdani N, Alvi AS, Qazi MF, Hoodbhoy Z. Association of maternal nutritional status and small for gestational age neonates in peri-urban communities of Karachi, Pakistan: findings from the PRISMA study. BMC Pregnancy Childbirth. (2024) 24:214. doi: 10.1186/S12884-024-06420-3
16. Arifin WN. Sample size calculator (web) [Internet]. (2025). Available online at: http://wnarifin.github.io (Accessed November 03, 2024).
17. Mukabutera A, Nsereko E, Aline U, Didier Umwungerimwiza Y, Cyprien M. Overweight or obesity prevalence, trends and risk factors among women in Rwanda: a cross-sectional study using the Rwanda demographic and health surveys, 2000. Rwanda J. (2016) 3:14–20. doi: 10.4314/rj.v3i1.3F
18. Khadivzadeh T. Mid upper arm and calf circumferences as indicators of nutritional status in women of reproductive age. East Mediterr Heal J. (2002) 8:612–8. doi: 10.26719/2002.8.4-5.612
Keywords: pregnancy, age, mid-upper arm circumference, body mass index, obesity
Citation: Ali MH, AlHabardi N and Adam I (2025) Assessment of mid-upper arm circumference for detecting obesity in pregnant women: a cross-sectional study. Front. Glob. Women's Health 6:1554068. doi: 10.3389/fgwh.2025.1554068
Received: 8 January 2025; Accepted: 29 October 2025;
Published: 17 November 2025.
Edited by:
Olutosin Ademola Otekunrin, University of Ibadan, NigeriaReviewed by:
Jim Philip, NMC Specialty Hospital, United Arab EmiratesHala Zakaria, Glucare Integrated Diabetes Center, United Arab Emirates
Copyright: © 2025 Ali, AlHabardi and Adam. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Moayad H. Ali, bW9heWFkaGFtYWQxMEBnbWFpbC5jb20=
 Moayad H. Ali1*
Moayad H. Ali1* Nadiah AlHabardi
Nadiah AlHabardi Ishag Adam
Ishag Adam