- 1Health Sciences Research Unit, Nursing, Nursing School of Coimbra, Coimbra, Portugal
- 2Nursing School of Coimbra, Coimbra, Portugal
- 3University of Coimbra, Coimbra, Portugal
- 4School of Health Sciences, Polytechnic Institute of Leiria, Leiria, Portugal
- 5ciTechCare—Center for Innovative Care and Health Technology, Polytechnic Institute of Leiria, Leiria, Portugal
Urinary incontinence (UI) during pregnancy and after childbirth can negatively impact women's lifestyles, health, and well-being. It is a common problem that is often normalized by both healthcare professionals and women. This integrative review examines the influence of UI on women's quality of life (QoL) during the postpartum period and identifies the main affected domains. It will also contribute to the discussion of the results of a primary study. Fourteen studies were included in this review, mainly from Brazil and Spain, with most using quantitative methods. The findings indicate that UI negatively affects the QoL of women during the postpartum period, with mixed UI causing greater discomfort despite stress UI being more frequent. The main affected domains are general health perception, physical functioning, daily life activities, psychological/emotional/mental and social aspects, and sexuality. Effective interventions should promote women's self-care and enhance their awareness and recognition of the problem. These interventions should go beyond physical aspects to address emotional and psychological dimensions, such as low self-esteem and self-image, secrecy, embarrassment, and reluctance to seek help. Nurse midwives have specialized skills and can work within multidisciplinary teams to improve the QoL of women with UI at a time of increased vulnerability.
1 Introduction
Urinary incontinence (UI) during pregnancy and after childbirth is a common problem that is often normalized by both healthcare professionals and women, which can lead to changes that negatively impact women's lifestyles, health, and well-being in the postpartum period (1).
Postpartum UI is defined as the involuntary loss of urine experienced during the postpartum period and up to 12 months after delivery. Among its types, postpartum stress urinary incontinence (SUI) is the most common and is characterized by involuntary loss of urine during physical effort, exertion, sneezing, or coughing (2). Postpartum urgency urinary incontinence (UUI) refers to the involuntary loss of urine associated with a sudden and urgent need to urinate. Lastly, postpartum mixed urinary incontinence (MUI) is defined as the involuntary loss of urine associated with both urgency and physical effort, exertion, sneezing, or coughing (2).
Between six weeks and one year postpartum, the weighted mean prevalence of UI is 31%, ranging from 10% to 63%. A decrease in prevalence is typically observed during the first three months postpartum due to the natural recovery of the pelvic floor, followed by an increase associated with the return to daily activities (3).
Pregnancy and childbirth are risk factors for the occurrence of postpartum UI (4, 5), especially postpartum SUI (1, 4, 6). Women who experience urine leakage during pregnancy are more likely to develop postpartum UI (4, 7). Other factors include pre-pregnancy changes, physiological changes related to pregnancy, and lack of guidance from healthcare professionals (5).
Postpartum UI is often underestimated and perceived as a normal consequence of childbirth by both healthcare professionals and women (4). This perception leads to a lack of effective preventive interventions and low rates of help-seeking, diagnosis, or treatment among women (8).
Quality of life (QoL) is a subjective concept that can be difficult to discuss scientifically due to its widespread use in everyday language (9). The World Health Organization defines QoL as an individual's perception of their position in life in the context of their culture and value systems and in relation to their goals, expectations, standards, and concerns. It encompasses their physical health, psychological state, level of independence, social relationships, personal beliefs, and relationship with the environment. Measuring QoL helps assess the impact of environment, disease, and health interventions (10).
QoL assessment instruments have been developed across different cultural contexts and usually include six domains: physical, psychological, level of independence, social relationships, environment, and spirituality/religion/personal beliefs (10).
However, addressing QoL during the postpartum period—a phase that profoundly impacts all its domains—requires recognizing it as a time of increased vulnerability for women. This period is marked by significant physiological, psychological, and social changes, as women adapt to a new reality, identity, and role (11). In this process, women should understand that motherhood is a role that does not exclude them from other areas and that self-care should not take second place to caregiving duties.
This integrative literature review aims to explore the influence of UI on women's QoL during the postpartum period and identify the main affected domains. It serves as the starting point for a future primary study that will assess the QoL of women with postpartum UI within the first 12 months after childbirth. In parallel, a phenomenological primary study will be conducted to explore the lived experiences of these women. By synthesizing the findings from these studies, this integrative literature review contributes to a deeper understanding of the topic.
The PCC (Population, Concept, and Context) mnemonic (12) was used to outline the following review questions: Q1: How does UI influence women's QoL during the postpartum period? and Q2: What are the main domains of women's QoL affected by UI during the postpartum period?
A preliminary search was conducted to identify recent studies addressing these questions. While there are reviews on QoL in the postpartum period, many do not specifically address UI or examine the QoL of women with UI without specifically focusing on the postpartum period. Some reviews explore risk factors (13), prevalence and treatment options (14), or the impact of UI on the QoL of postpartum women but exclude multiparous women and those over 40 years old (15).
2 Materials and methods
The integrative review method was used to achieve the objective of this review. This method combines research studies conducted using different methodologies and synthesizes knowledge to better understand the current state of evidence on a specific phenomenon. It is particularly valuable to understand issues relevant to health care and public policies (16). The integrative review method consists of five stages: problem identification, literature search, data evaluation, data analysis, and data presentation (16).
A literature search was conducted between July and October 2024, covering articles published between 1997 and 2024. This time frame was chosen because the King's Health Questionnaire (KHQ), one of the first specific instruments to assess QoL in women with UI, was published in 1997 (17). Unlike broader QoL assessment tools, the KHQ is tailored specifically to UI. Currently, there is no specific instrument to assess postpartum UI, nor has a systematic literature review on this specific topic been published after this date.
This review includes studies that focused on women with postpartum UI up to one year after childbirth and that address QoL assessment, regardless of the type of study or data collection instrument. Full-text articles available in Portuguese, English, Spanish, and French were considered eligible. The literature search was conducted in multiple databases: MEDLINE (via PubMed), CINAHL Complete (via EBSCO), Nursing & Allied Health Collection: Comprehensive (via EBSCO), MedicLatina (via EBSCO), Academic Search Complete (via EBSCO), SciELO, Web of Science, Scopus, and the Open Access Scientific Repositories of Portugal (RCAAP). Additionally, specific guidelines, such as those from the Royal College of Obstetricians and Gynaecologists (RCOG), were consulted. The search query used was: “quality of life AND urinary incontinence AND postpartum”. The query was adapted to each search engine and inclusion criteria were applied. Two independent reviewers screened the studies. There was no need for a third reviewer to resolve any discrepancies. After title/abstract and full-text screening, 14 studies published between 2004 and 2023 were included in this review based on their relevance and the inclusion criteria (Figure 1).
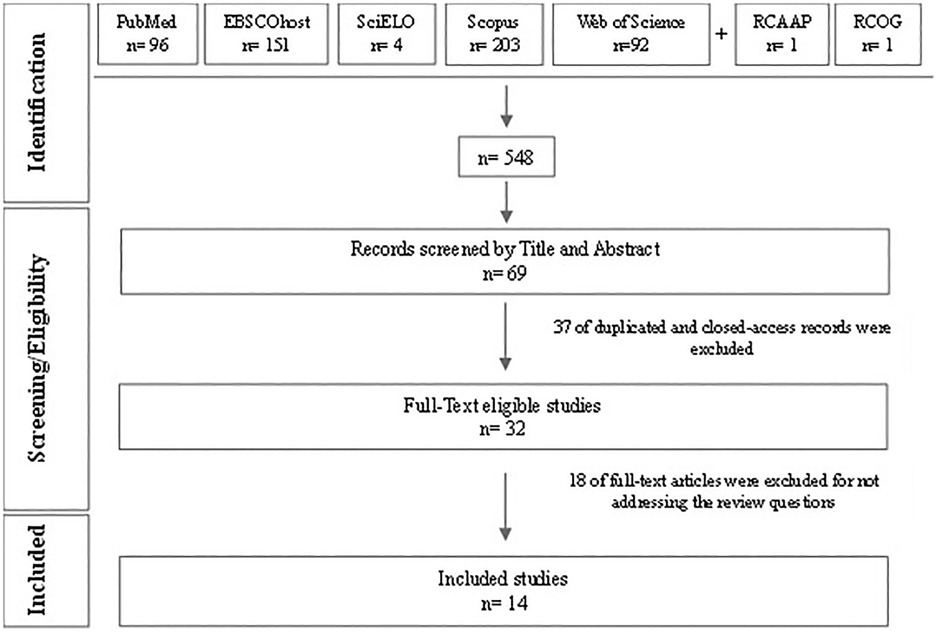
Figure 1. Flowchart of the study selection process adapted from the PRISMA-ScR flowchart (46).
3 Results
The included studies were published between 2004 and 2023, with three published in the last five years (18–20). Most of the studies were from Brazil and Spain and used quantitative methods. While most studies focused on postpartum women, three studies included participants during pregnancy (21–23). The most used instruments to assess QoL were the KHQ, the 36-Item Short Form Survey (SF-36), and the Incontinence Impact Questionnaire, Short Form (IIQ-7). The KHQ and the IIQ-7 are instruments related to the health-related QoL (HRQoL) of women with UI (17) and the impact of UI on women's lives (24), respectively.
Data were extracted using a table that included the following elements: author(s)/year of publication/country, type of study/methodology, population/sample, data collection instrument, and main findings (Table 1) to facilitate data analysis and presentation.
3.1 Q1—how does UI influence women’s QoL during the postpartum period?
UI has a negative impact on women's QoL during pregnancy and after childbirth, persisting at least until 12 months postpartum, especially SUI (20, 25).
The impact of UI on QoL is greater during the postpartum period than during pregnancy due to lifestyle changes after childbirth or post-partum related morbidities (22).
UI is strongly associated with lower with HRQoL (26, 27). Among the different types of UI, MUI has the greatest negative impact, causing more discomfort than SUI and UUI (18, 28, 29), even though SUI is the most common type (25).
At six months postpartum, UI continues to have a significant impact on women's QoL (30). However, the same study found no correlation between the type of UI and QoL.
UI is one of the leading factors contributing to a decrease in QoL, alongside other issues such as depressive symptoms, lactation problems, and postpartum sexual health concerns (19).
Although its prevalence is high in the postpartum period, UI is even more common during pregnancy, especially in the third trimester (25). It occurs more frequently after vaginal delivery (21), with most women with postpartum UI having had a forceps-assisted delivery (23, 27). The incidence of UI reaches 45% between one and three years postpartum (26).
Although UI is usually mild to moderate, cases of severe UI also occur (18, 25). Even when the volume of leakage is small, its frequent occurrence can significantly disrupt daily life and reduce QoL during the postpartum period (31). As postpartum UI symptoms become more severe, their impact on women's QoL increases (18), often resulting in lifestyle changes such as using absorbent pads to avoid wetting clothes and limiting physical and social activities to avoid potentially embarrassing situations. However, these restrictive behaviors may lead to psychological discomfort and negatively affect both physical health and interpersonal relationships (18). Urine leakage during sexual activity also has a negative impact on women's sexual lives, with most partners being aware of their UI (25). In addition, urine leakage during coughing, sneezing, or physical activities is common (31).
3.2 Q2—what are the main domains of women’s QoL affected by UI during the postpartum period?
The included studies highlight some of the most affected QoL domains due to postpartum UI. These domains were grouped according to the WHOQOL Group's definition of QoL (10) and the terminology used by the respective authors.
Women with UI scored lower in the following domains: general health perception (19, 23, 25, 26, 28, 31), physical limitations (19, 26, 28, 29, 31), daily life activities (20, 28, 31), psychological/emotional/mental aspects (18, 19, 26, 29–31), social aspects (18, 20, 22, 29–31), and sexuality (25).
Other domains include incontinence impact (25, 28, 31), behavioral impact (18), economic impact (30), sleep and energy (22, 23), and vitality (31).
4 Discussion
The analysis of the included studies reveals a predominance of research from Brazil and Spain, with most studies focusing on postpartum women. In contrast, only a few studies examined pregnancy-related issues. Although postpartum UI is typically defined as the period from childbirth up to one year postpartum (2), both pregnancy and childbirth are considered risk factors for UI. Moreover, pregnant women experiencing urine leakage are more likely to develop postpartum UI (4, 7). Therefore, some studies addressing postpartum UI include data from the pregnancy period (21–23).
Although the research includes studies published up to and including 2024, only three were published in the last five years. Notably, the majority of these studies used quantitative methods. This predominance of quantitative research underscores the need for qualitative studies, which could provide deeper insights into how and why postpartum UI affects key QoL domains.
One of the most used instruments to assess QoL was the KHQ. The KHQ has proven reliable and valid for evaluating the quality of life in women with UI. It considers various dimensions, including personal and daily life limitations, emotional aspects, social relationships, and urinary symptoms. Its comprehensive approach is valuable for guiding effective interventions and ensuring appropriate clinical follow-up and treatment (32).
This review highlighted the importance of recognizing UI as a frequent problem during the postpartum period and its significant impact on the QoL of postpartum women.
Among studies assessing the prevalence or incidence of UI, SUI emerges as the most frequent type following childbirth (21, 25, 31), although one study suggests that MUI is more prevalent (23). A systematic review on the prevalence and incidence of UI further confirms that SUI is the most prevalent type during the postpartum period (3). Nevertheless, women with MUI generally report a lower QoL than those with SUI, particularly in terms of restrictive behavior. This is attributed to the combined symptoms of SUI and UUI, with MUI causing greater discomfort (18, 28). Even the study reporting a low impact of UI on QoL acknowledges the presence of moderate to mild symptoms six months postpartum (33).
The majority of the selected studies highlight the limitations imposed by postpartum UI on physical functioning, daily life activities, and social domains (18–20, 22, 26, 28–31). These findings support the conclusions of a 2022 literature review on the impact of UI on QoL among postpartum women (15), which noted a tendency toward isolation. In addition, these factors can also negatively affect emotional and psychological well-being, potentially contributing to depressive symptoms (15), as suggested by some of the selected studies (18, 19, 26, 29–31). While UI increases depressive moods in postpartum women, its impact extends further, affecting their emotional well-being, emotional reactions, energy levels, sleep, physical activities, and social relationships (34). Furthermore, UI negatively affects their clothing choices, participation in leisure activities, daily routines, QoL, and overall health (35). A systematic review on the association between UI and postpartum depression found that UI increases the risk of developing postpartum depression by 45% (36).
The stigma surrounding postpartum UI arises from widespread misconceptions that view it as a deviation from the norm, often linked to poor hygiene and lack of self-control. These perceptions contribute to self-stigma, which undermines self-esteem, increases anxiety, and discourages women from seeking healthcare (37). Rooted in community values associating UI with uncleanliness, this stigma is often internalized, worsening mental health. Although some women are aware of the negative impact of UI on their mental health, many still feel embarrassed to discuss their condition with friends and family (37).
One of the selected studies—a theoretical-critical reflection on women's knowledge of UI (35)—highlights that fear of exposing their feelings, dignity, and self-worth to both professionals and society often compels women to conceal their condition. This concealment can compromise bodily autonomy, affecting partner acceptance, sexuality, self-image, and self-esteem. As a result, many women avoid seeking help or engaging with prevention, treatment, and recovery efforts for UI. A study on help-seeking behavior among postpartum women with UI in China and Indonesia found that, despite the high prevalence of UI, only half of the affected women sought professional help. Barriers to seeking help included insufficient social support, lack of awareness regarding available treatment options, and a lack of proactive engagement from healthcare professionals in addressing UI during consultations. Additionally, factors such as symptom severity and perceived QoL were found to negatively influence the likelihood of seeking professional help (38).
Dissatisfaction with QoL is considered a key motivator for seeking treatment, particularly pelvic floor physical therapy (20). To overcome barriers to help-seeking behavior, it is essential to improve access to healthcare services, strengthen social support systems, and ensure that women have easy access to healthcare professionals who can provide accurate information and appropriate treatment options (38). Similarly, a study examining barriers to help-seeking behavior among women with stigmatized pelvic health symptoms, including UI, identified stigma, lack of knowledge, and the minimization of symptoms by healthcare professionals as significant obstacles. This study recommend strategies to reduce stigma, increase symptom awareness, provide training for healthcare professionals, and improve access to healthcare services as key enablers of help-seeking behavior (39).
Although addressed by only one of the selected studies, specifically one that assesses the extent to which UI affects QoL (25), without controversy from the others, the impact of UI on sexual activity and partner acceptance is evident, with sexuality identified as one of the QoL domains affected by UI. A study on factors associated with persistent sexual dysfunction and pain 12 months postpartum found that the continued presence of bothersome postpartum UI, along with higher levels of patient-perceived daily stress, was strongly associated with sexual dysfunction (40).
All affected QoL domains, particularly the decline in general health perception, are closely linked not only to childbirth and postpartum morbidities but also to lifestyle changes and the adjustments required after a child's birth. Four of the selected studies specifically address the impact of UI on HRQoL (23, 26, 28, 31). During the postpartum period, women tend to prioritize their baby's needs over their health, delaying self-recognition of symptoms and help-seeking behaviors aimed at improving QoL (34).
The normalization of UI by healthcare professionals is highlighted in a study on the main factors contributing to the development of UI in women during the postpartum period (5), as well as in a study examining risk factors for postpartum UI among nulliparous women (8). It is recommended that healthcare professionals recognize UI as a prevalent condition that affects the QoL of postpartum women, as this recognition could facilitate women's self-recognition of their symptoms and break the cycle of omission, neglect, or complacency from both patients and professionals. This need for awareness is further emphasized in a study aimed at sensitizing healthcare professionals and health managers to the scope and implications of UI-related issues (35).
The importance of qualified, multidisciplinary care in preventing, treating, and guiding women who may dismiss their symptoms as irrelevant (15) during the postpartum period cannot be underestimated (22).
Although the selected studies do not focus primarily on solutions, all address the need for intervention in their conclusions, as UI is a condition that does not resolve spontaneously and impacts multiple domains of QoL. The recommended interventions include early screening for risk factors (21, 22, 25, 28, 29), educational interventions (18, 23, 25, 26, 28, 31), emotional and psychological support (19, 20, 23, 25, 27, 29, 30), and pelvic floor rehabilitation programs (18, 20, 22, 25, 27, 30, 31, 33).
Patient perspectives are essential for improving clinical care, as they emphasize the importance of listening to patient concerns and optimizing treatments to better meet their needs (41). Effective two-way communication between clinicians and patients facilitates shared decision-making (20). Given the significant impact of UI on QoL, clinicians caring for postpartum women should routinely screen for UI and provide appropriate evaluation and treatment options (30). Increased awareness and attention from healthcare professionals, particularly nurse midwives, can support the development of effective health interventions. These professionals play a crucial role in the prevention, guidance, and management of health issues affecting women throughout their life cycle, including the prenatal and postpartum periods.
Enhancing patient education and equipping healthcare professionals with the skills to address UI sensitively and provide appropriate treatment are essential. Implementing standardized assessments and stigma-reducing strategies, such as supervised physical activity programs and the creation of safe, inclusive spaces, can significantly improve outcomes for women with postpartum UI (42).
In addition, the National Institute for Health and Care Excellence (NICE) guidelines emphasize the importance of cultural sensitivity when addressing pelvic floor dysfunction. Many women may feel embarrassed discussing their symptoms and may assume that healthcare professionals are equally uncomfortable with the topic. To provide more effective support, the use of digital information sources, such as apps or videos, and a community-based multidisciplinary team approach is recommended. Encouraging lifestyle changes and providing a supervised pelvic floor muscle training program for at least three months are essential. Additionally, the psychological impact of symptoms should be discussed and integrated into a management plan (43).
Lifestyle changes include weight loss (since excess weight is a risk factor), timed voiding to prevent excessive bladder filling (particularly in cases of SUI), and fluid restriction (44). Pelvic floor physical therapy is considered an effective first-line treatment, either alone or combined with biofeedback, electrostimulation, or the use of vaginal cones, for reducing UI and improving pelvic floor muscle contraction (44, 45). Pharmacotherapy is commonly used in the treatment of UUI, with antimuscarinic agents (which inhibit involuntary detrusor muscle contractions) and beta-agonists (which relax the detrusor muscle and increase bladder capacity) being the main classes of medication. Vaginal estrogen may also be considered, particularly for postmenopausal women. In more severe cases, surgery, such as the placement of a synthetic sling to support the bladder neck, may be an option (44).
It is crucial to reflect on the role of healthcare professionals and highlight the importance of multidisciplinary and intersectoral collaboration in healthcare, ultimately improving the QoL of women with UI during the postpartum period, which is particularly vulnerable.
This review has some limitations, including the restriction to articles published in Portuguese, English, Spanish, and French, which may have led to the exclusion of relevant studies in other languages. Additionally, the heterogeneity of the included studies—with varying sample characteristics and measurement instruments—may affect the generalizability of the findings.
5 Conclusion
This integrative review included studies published on various databases, as well as gray literature, over an extended time period, reflecting the lack of reviews addressing the proposed objective.
UI is a common condition that often goes unrecognized by both postpartum women and healthcare professionals. It has a negative impact on the QoL of women during the highly vulnerable postpartum period. The most affected QoL domains include general health perception, physical limitations, daily life activities, psychological/emotional/mental and social aspects, and sexuality.
Despite its high prevalence, UI should not be normalized or overlooked by healthcare professionals. Recognizing and valuing women's perceptions of their health and QoL is essential for increasing awareness of the problem among both women and healthcare professionals. This, in turn, can drive the development and integration of effective strategies in education and clinical practice.
Author contributions
FL: Writing – original draft, Writing – review & editing, Conceptualization, Investigation, Methodology, Project administration, Visualization. CH: Writing – review & editing, Supervision. ML: Writing – review & editing. IM: Writing – review & editing, Supervision, Methodology.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The corresponding author gratefully acknowledges the support of the Health Sciences Research Unit: Nursing, Nursing School of Coimbra, and the Foundation for Science and Technology (FCT) under grant reference project UIDB/00742/2020.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Yan M, Lv X, Jin X, Li S, Shen X, Zhang M, et al. The mediating effect of the prolonged second stage of labor on delivery mode and urinary incontinence among postpartum women: evidence from Shandong, China. Int Urogynecol J. (2022) 33:1549–56. doi: 10.1007/s00192-021-05007-2
2. Doumouchtsis S, Tayrac R, Lee J, Daly O, Melendez-Munoz J, Lindo F, et al. An international continence society (ICS) international urogynecological association (IUGA) joint report on the terminology for the assessment and management of obstetric pelvic floor disorders. Continence. (2022) 4:100502. doi: 10.1016/j.cont.2022.100502
3. Moossdorff-Steinhauser HFA, Berghmans BCM, Spaanderman MEA, Bols EMJ. Prevalence, incidence and bothersomeness of urinary incontinence between 6 weeks and 1 year post-partum: a systematic review and meta-analysis. Int Urogynecol J. (2021) 32:1675–93. doi: 10.1007/s00192-021-04877-w
4. Gao J, Liu X, Zuo Y, Li X. Risk factors of postpartum stress urinary incontinence in primiparas: what should we care. Medicine (Baltimore). (2021) 100(20):e25796. doi: 10.1097/MD.0000000000025796
5. Donoso M, Reis E, Amorim T, Silqueira S, Pinheiro E, Matos S. Main aspects that favor the development of urinary incontinence in postpartum women. Rev Enferm Aten Saúde. (2020) 9(1):144–59. doi: 10.18554/reas.v7i2.2398
6. Bonasia K, Clancy A, Stairs J. Prevalence and risk factors for urinary incontinence up to 2 years postpartum: a cross-sectional population-based study. Int Urogynecol J. (2023) 34:2467–72. doi: 10.1007/s00192-023-05571-9
7. Leroy L, Lúcio A, Lopes M. Risk factors for urinary incontinence in the puerperium. Rev Esc Enferm USP. (2016) 50(2):200–7. doi: 10.1590/50080-623420160000200004
8. Elbiss HM, Abu-Zidan FM. Postpartum urinary incontinence of nulliparous women: a prospective cohort study. Medicine (Baltimore). (2023) 102(9):e33171. doi: 10.1097/MD.0000000000033171
9. Pais-Ribeiro J. The importance of quality of life for health psychology. In: Cruz JP, Jesus SN, Nunes C, editors. Well-Being and Quality of Life. Alcochete: Textiverso (2009). p. 31–49.
10. WHOQOL Group. Development of the WHOQOL: rationale and current status. Int J Ment Health. (1994) 23(3):24–56. doi: 10.1080/00207411.1994.11449286
11. Mendes I. Ajustamento Materno e paterno: Experiências Vivenciadas Pelos Pais no pós-parto. 1st ed Coimbra: Mar da Palavra – Edições (2009). p. 305.
12. Aromataris E, Lockwood C, Porritt K, Pilla B, Jordan Z. JBI Manual for Evidence Synthesis. Adelaide: JBI (2024). doi: 10.46658/JBIMES-24-01
13. Wang K, Xu X, Jia G, Jiang H. Risk factors for postpartum stress urinary incontinence: a systematic review and meta-analysis. Reprod Sci. (2020) 27(12):2129–45. doi: 10.1007/s43032-020-00254-y
14. Gonzales AL, Barnes KL, Qualls CR, Jeppson PC. Prevalence and treatment of postpartum stress urinary incontinence: a systematic review. Female Pelvic Med Reconstr Surg. (2021) 27(1):e139–145. doi: 10.1097/SPV.0000000000000866
15. Miranda ACP, Bezerra ENB, Ferreira GM, Freitas MVS, Duarte TB. Impacto da qualidade de vida em mulheres com incontinência urinária no puerpério: revisão da literatura. Revistaft. (2022) 26(116):10–21. doi: 10.5281/zenodo.7309918
16. Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. (2005) 52(5):546–53. doi: 10.1111/j.1365-2648.2005.03621.x
17. Kelleher CJ, Cardozo LD, Khullar V, Salvatore S. A new questionnaire to assess the quality of life of urinary incontinent women. BJOG. (1997) 104:1374–79. doi: 10.1111/j.1471-0528.1997.tb11006.x
18. Liang Y, Chen Y, Yu X, Li X. Quality of life among women with postpartum urinary incontinence: a cross-sectional study. Gynecol Obstet Clin Med. (2021) 1:164–8. doi: 10.1016/j.gocm.2021.07.008
19. Martínez-Galiano JM, Hernández-Martínez A, Rodríguez-Almagro J, Delgado-Rodríguez M, Rubio-Alvarez A, Gómez-Salgado J. Women’s quality of life at 6 weeks postpartum: influence of the discomfort present in the puerperium. Int J Environ Res Public Health. (2019) 16(2):253. doi: 10.3390/ijerph16020253
20. Li J, Li T, Huang S, Chen L, Cai W. Motivations, psychosocial burdens, and decision-making modes of post-partum women with stress urinary incontinence engaging in pelvic floor physical therapy: a qualitative research. Int Urogynecol J. (2023) 34:1803–13. doi: 10.1007/s00192-023-05466-9
21. Lin YH, Chang SD, Hsieh WC, Chang YL, Chueh HY, Chao AS, et al. Persistent stress urinary incontinence during pregnancy and one year after delivery; its prevalence, risk factors and impact on quality of life in Taiwanese women: an observational cohort study. Taiwan J Obstet Gynecol. (2018) 57(3):340–5. doi: 10.1016/j.tjog.2018.04.003
22. Valeton CT, Amaral VF. Evaluation of urinary incontinence in pregnancy and postpartum in curitiba mothers’ program: a prospective study. Int Urogynecol J. (2011) 22(7):813–8. doi: 10.1007/s00192-011-1365-8
23. Dolan LM, Walsh D, Hamilton S, Marshall K, Thompson K, Ashe RG. A study of quality of life in primigravidae with urinary incontinence. Int Urogynecol J Pelvic. (2004) 15(3):160–4. doi: 10.1007/s00192-004-1128-x
24. Uebersax JS, Wyman JF, Shumaker SA, McClish DK. Short forms to assess life quality and symptom distress for urinary incontinence in women: the incontinence impact questionnaire and the urogenital distress inventory. Neurourol Urodyn. (1995) 14(2):131–9. doi: 10.1002/nau.1930140206
25. Lima JDA, Lopes MHB. Qualidade de vida em mulheres com incontinência urinária no puerpério. ESTIMA. (2016) 9(2):65–72. Available at: https://www.revistaestima.com.br/estima/article/view/65
26. Walton LM, Ambia SU, Schbley BH. Incidence and impact of urinary incontinence, morbidities, and health-related quality of life (HRQOL) for postpartum Bangladeshi women. Int J Matern Child Health. (2014) 2(2):86–100. doi: 10.12966/ijmch.05.09.2014
27. Triviño-Juárez JM, Romero-Ayuso D, Nieto-Pereda B, Forjaz MJ, Criado-Álvarez JJ, Arruti-Sevilla B, et al. Health-related quality of life of women at the sixth week and sixth month postpartum by mode of birth. Women Birth. (2017) 30(1):29–39. doi: 10.1016/j.wombi.2016.06.005
28. Lopes DBM. Self-reported postpartum urinary incontinence: incidence, risk factors, and health-related quality of life of women in northern paraná (Doctoral thesis). School of Nursing, University of São Paulo, São Paulo (2014). doi: 10.11606/T.7.2014.tde-06112014-125743
29. Van der Woude DA, Pijnenborg JMA, de Vries J. Health status and quality of life in postpartum women: a systematic review of associated factors. Eur J Obstet Gynecol Reprod Biol. (2015) 185:45–52. doi: 10.1016/j.ejogrb.2014.11.041
30. Handa VL, Zyczynski HM, Burgio KL, Fitzgerald MP, Borello-France D, Janz NK, et al. The impact of fecal and urinary incontinence on quality of life 6 months after childbirth. Am J Obstet Gynecol. (2007) 197(6):636.e1–e6. doi: 10.1016/j.ajog.2007.08.020
31. Leroy LS, Lopes MHBM. Urinary incontinence in the puerperium and its impact on the health-related quality of life. Rev Lat Am Enfermagem. (2012) 20(2):346–53. doi: 10.1590/s0104-11692012000200018
32. Viana R, Viana S, Neto F, Mascarenhas T. Adaptation and validation of the king’s health questionnaire in Portuguese women with urinary incontinence. Int Urogynecol J. (2015) 26(2):275–81. doi: 10.1007/s00192-015-2628-6
33. Arrue M, Ibañez L, Paredes J, Murgiondo A, Belar M, Sarasqueta C, et al. Stress urinary incontinence six months after first vaginal delivery. Eur J Obstet Gynecol Reprod Biol. (2010) 150(2):210–4. doi: 10.1016/j.ejogrb.2010.02.039
34. Suar G, Cevik F, Simal Yavuz N, Ozerdogan N. Urinary incontinence in the postpartum 1-year period: its prevalence and effect on psychosocial status of women. Low Urin Tract Symptoms. (2023) 15(5):191–9. doi: 10.1111/luts.12495
35. Benício CDAV, Luz MHBA, Carvalho NV, de Brito BAM, Ferreira JLS. Conhecimento das mulheres incontinentes sobre incontinência urinária: uma reflexão teórico-crítica. ESTIMA. (2017) 15(1):58–61. doi: 10.5327/Z1806-3144201700010010
36. Gallego-Gómez C, Rodríguez-Gutiérrez E, Torres-Costoso A, Martínez-Vizcaíno V, Martínez-Bustelo S, Quezada-Bascuñán CA, et al. Urinary incontinence increases risk of postpartum depression: systematic review and meta-analysis. Am J Obstet Gynecol. (2024) 231(3):296–307.e11. doi: 10.1016/j.ajog.2024.02.307
37. Rocha J, Brandão P, Melo A, Torres S, Mota L, Costa F. Assessment of urinary incontinence in pregnancy and postpartum: observational study. Acta Med Port. (2017) 30(7-8):568–72. doi: 10.20344/amp.7371
38. Liang S, Chen Z, Tang W, Andarini E, Kou L, Li Y, et al. Prevalence and predictors of help-seeking behavior among postpartum women with urinary incontinence in China and Indonesia: a cross-sectional survey based on andersen help-seeking model. Midwifery. (2024) 128:103885. doi: 10.1016/j.midw.2023.103885
39. Jouanny C, Abhyankar P, Maxwell M. A mixed methods systematic literature review of barriers and facilitators to help-seeking among women with stigmatised pelvic health symptoms. BMC Womens Health. (2024) 24(1):217. doi: 10.1186/s12905-024-03063-6
40. Bhandari Randhawa S, Rizkallah A, Nelson DB, Duryea EL, Spong CY, Pruszynski JE, et al. Factors associated with persistent sexual dysfunction and pain 12 months postpartum. Sex Reprod Healthc. (2024) 41:101001. doi: 10.1016/j.srhc.2024.101001
41. Du C, Lee W, Moskowitz D, Lucioni A, Kobashi KC, Lee UJ. I leaked, then I reddit: experiences and insight shared on urinary incontinence by reddit users. Int Urogynecol J. (2020) 31(2):243–8. doi: 10.1007/s00192-019-04165-8
42. Cox JM, Sánchez-Polán M, Mota P, Barakat R, Nagpal TS. A scoping review exploring stigma associated with postpartum urinary incontinence. Int Urogynecol J. (2023) 34(9):1997–2005. doi: 10.1007/s00192-023-05526-0
43. National Institute for Health and Care Excellence. Pelvic floor dysfunction: prevention and non-surgical management: NICE guideline. Manchester: National Institute for Health and Care Excellence (NICE) (2021). Available at: https://www.nice.org.uk/guidance/ng210/chapter/Recommendations#communicating-with-and-providing-information-to-women-with-pelvic-floor-dysfunction (Accessed March 7, 2025).
44. Trowbridge ER, Hoover EF. Evaluation and treatment of urinary incontinence in women. Gastroenterol Clin North Am. (2022) 51:157–75. doi: 10.1016/j.gtc.2021.10.010
45. Alouini S, Memic S, Couillandre A. Pelvic floor muscle training for urinary incontinence with or without biofeedback or electrostimulation in women: a systematic review. Int J Environ Res Public Health. (2022) 19(5):2789. doi: 10.3390/ijerph19052789
Keywords: women, urinary incontinence, postpartum period, quality of life, nursing
Citation: Lopes FD, Henriques C, Lopes MdS and Mendes IM (2025) Quality of life of women with urinary incontinence in the postpartum period: an integrative literature review. Front. Glob. Women's Health 6:1562572. doi: 10.3389/fgwh.2025.1562572
Received: 17 January 2025; Accepted: 18 April 2025;
Published: 1 May 2025.
Edited by:
Rui Viana, Fernando Pessoa Foundation, PortugalReviewed by:
Telma Pires, Instituto Politécnico de Bragança, PortugalThuane Da Roza, Santa Catarina State University, Brazil
Copyright: © 2025 Lopes, Henriques, Lopes and Mendes. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Filipa Daniela Lopes, ZmlsaXBhLmxvcGVzMjRAZXNlbmZjLnB0
 Filipa Daniela Lopes
Filipa Daniela Lopes Carolina Henriques
Carolina Henriques Maria da Saudade Lopes4,5
Maria da Saudade Lopes4,5 Isabel Margarida Mendes
Isabel Margarida Mendes