- ICMR-NIIRNCD, Jodhpur, India
Background: Low Birth Weight (LBW) significantly affects childhood survival, with the socio-demographic characteristics (maternal age, child's gender, education, maternal diseases and others) contributing to it. The study aims to identify social determinants contributing to LBW, which can further be useful in developing local interventions to rectify the problem in an Indian rural context.
Methodology: The cross-sectional study was conducted in the Jalore district of Rajasthan, India. A total of 92 delivery cases, including LBW (n = 46) and cases with normal birth weight (n = 46), became part of the research. A pre-tested questionnaire collected information from study participant groups enumerating deliveries from selected Primary Health Centres (PHCs) related to LBW and non-LBW deliveries in a 1:1 ratio.
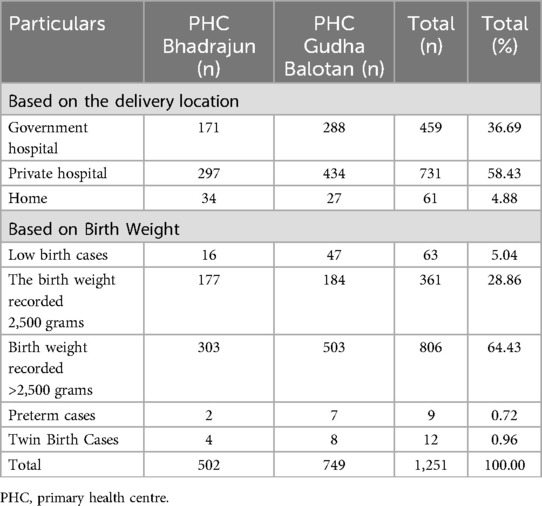
Results: The study recorded a total of 1,251 deliveries, of which 63 resulted in the LBW (<2,500 grams), nine were premature, 12 were twin births, and 361 were normal weight deliveries (≥2,500 grams). LBW was prevalent in underprivileged communities within nuclear families, having an average birth weight of 2.12 kilograms. Reduced meal frequency (1–2 times a day) for women is also linked to higher LBW risk.
Conclusion: Many factors, like complications during pregnancy, awareness of pregnancy planning, and nutritional intake, are associated with the likelihood of LBW occurrences. Many maternal risk factors for LBW are modifiable through early detection by imparting education and awareness to pregnant women in their first trimester. The findings emphasize the significance of targeted interventions and awareness programs to address specific risk factors and improve birth outcomes in rural Indian communities.
Introduction
Birth weight serves as both a crucial measure of maternal well-being and a strong predictor of neonatal and childhood health outcomes. The newborn's birth weight is ideally documented within the first hours of delivery and captured before significant postnatal weight loss takes place. A newborn with low birth weight (LBW) is characterized as a live baby weighing less than 2,500 grams at birth. According to WHO estimates, approximately 25 million babies with LBW are born annually, and 5 million of them experience global mortality (1). According to the National Family Health Survey (NFHS-5) (2), the Infant Mortality Rate (IMR) in India was reported to be 26.6%. The LBW babies are at a higher risk of mortality within their first month, and those who survive confront lifelong consequences (3, 4). The public health data reveals that 98.8% of live births were recorded in India, with Rajasthan having a percentage of 98.2%. The LBW rate was recorded as 14.5% in Rajasthan (5). The NFHS-5 records a prevalence of 18.2% LBW in India, while in Rajasthan, it was 17.7% (2).
A child's birth weight is a critical determinant of susceptibility to childhood illnesses and overall survival. It is a widely accepted measure for assessing health status and is a key focal point in health policy discussions (6). Low birth weight (<2,500 grams) babies face a twenty-fold higher risk of neonatal death compared to normal weight babies (≥2,500 grams) (7). LBW is strongly linked to fetal and neonatal mortality, morbidity, impaired growth, cognitive development, as well as the onset of chronic diseases in later life. The impact of LBW on cardiovascular risk and metabolic disorders among children, adolescents, and young adults is noteworthy. During early childhood, LBW babies may exhibit heightened blood pressure, impaired vascular growth, increased peripheral vascular resistance, and cardiomyocyte remodeling (8).
Numerous factors interconnected with the infant, the mother, and the physical environment influence the duration of gestation and fetal growth, further impacting birth weight (9). These include tobacco exposure, inadequate antenatal care, maternal hypertension, low socioeconomic status, maternal anaemia, prenatal care visits, and maternal education. The risk of delivering an LBW baby is 4.1 times higher in women exposed to any tobacco product compared to those without exposure (10). Socio-cultural factors inevitably shape the healthcare vulnerability of rural populations (11). Limited awareness about healthcare measures and a lack of education and resources often contribute to inadequate health-seeking behaviour and poor health outcomes. Despite several government efforts to improve maternal health over the last two decades, disparities persist between various social groups. Identifying factors associated with the risk of LBW allows for targeted interventions, such as counselling mothers when feasible. Addressing these factors can reduce perinatal mortality and morbidity. It is imperative to enhance the quality and utilization of antenatal care, offer nutritional education for improved pregnancy weight gain, advocate for proper spacing, discourage tobacco use, and effectively manage risk factors like anaemia and hypertension (12). This study aims to identify maternal and socio-demographic factors associated with the risk of LBW deliveries in rural Rajasthan, using a matched case-control design.
Methodology
This cross-sectional study was conducted in Ahore Block of Jalore district, Rajasthan, from February 2021 to August 2022. As per Census of India 2011, the district has a population of 1,828,730, of which Ahore block contributes 239,642 population with a low literacy rate and economic backwardness. There are 10 primary healthcare centres (PHCs) under the district's primary healthcare system. Out of these, two PHCs-Bhadrajun (with five sub-health centres) and Gudhabalotan (with nine sub-health centres) became part of the current research. The required primary information on childbirths and the status of pregnant women and would-be mothers was gathered from these sub-health centres (SHCs).
Sample size
As preterm birth is one of the major factors associated with LBW, an estimation of its prevalence was taken as a basis for the sample size to be covered in the hospital survey. Assuming 10% as the preterm babies, at a 5% level of significance and 10% relative precision, about 900 deliveries were enumerated to estimate the point prevalence of preterm babies. 1,251 deliveries were recorded during the study, including 63 deliveries resulting in LBW. Of 63 LBW deliveries, three denied consent to participate in the study, and 14 were found unavailable, resulting in a total of 46 cases that became part of the study sample. To compare and contrast, a similar number of 46 deliveries with non-LBW babies were selected, considering a similar case match based on the age and locality of the participant.
Inclusion and exclusion criteria
The study includes mothers of live-born singleton term babies, with cases defined as birth weights under 2,500 grams (<2,500 grams) as well as 2,500 grams or more (≥2,500 grams). Exclusions were incomplete records, congenital anomalies, twin births, uncontactable cases after three home visits, and home deliveries.
Data collection
A pre-tested questionnaire was utilized to interview and collect the required information from the eligible mothers (study participants) through face-to-face conversation. The content was developed in the local language to understand the respondents better. The collected data was then translated into English with the help of a language expert to communicate findings in a research paper form. The variables under study include the basic socio-demographic profiles and the personal and obstetric history of the participants.
Data analysis
Data was analyzed using SPSS V.28. In addition to descriptive statistics, the Least Absolute Shrinkage and Selection Operator (LASSO) logistic regression was used to identify the factors associated with the birth of LBW babies. In this study, the authors have utilized R version 4.3.1 to perform logistic LASSO regression to identify the key predictors of LBW. They adjusted the lambda sequence to avoid very small values and fitted the logistic LASSO regression model with the glmnet package. The optimal lambda value was identified through cross-validation using the cv.glmnet function, and the best lambda was selected based on the minimum cross-validation error. The authors performed bootstrapping with 1,000 iterations to calculate the coefficients’ standard errors.
Results
Table 1 presents the PHC-wise details of deliveries reported. 1,251 deliveries were recorded from two PHCs, including 63 deliveries resulting in LBW, nine premature, 12 twin births, and 361 normal weight deliveries (≥2,500 grams). The average weight of LBW babies was 2.12 kg, while it was 3 kg for normal healthy babies. Out of 1,251 recorded deliveries, 36.69% (n = 459) took place in government institutions, 58.43% (n = 731) in private health facilities, and 4.88% (n = 61) occurred at home.
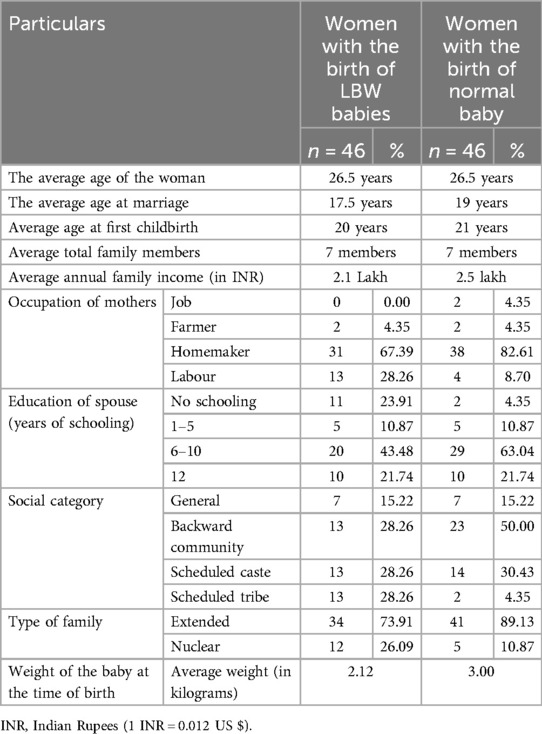
Table 2 shows the Socio-demographic characteristics of mothers. The average age of the respondents was 26.5 years. The average age of women at marriage was 17.5 years in the case of LBW deliveries and 19 years recorded for normal deliveries. It was found that the average age of the women at the first childbirth was 20 years, compared to 21 years for women with normal weight deliveries. A variation was seen in family annual income, where households with LBW cases recorded an income of Indian rupees (INR) 2.1 lakh, whereas it was INR 2.5 lakh for the other group. LBW incidences were recorded as higher among labourers. The study results show that LBW incidents were higher in nuclear families.
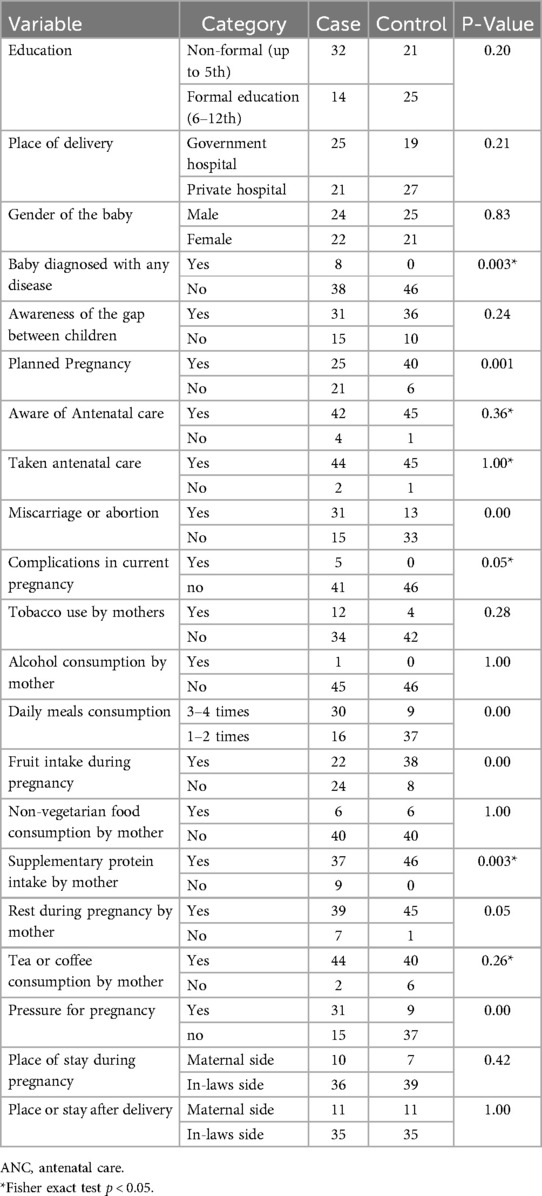
Table 3 compares case (LBW babies) and control (non-LBW babies) groups, evaluating various factors influencing low birth weight. However, notable associations were observed in several other factors. Being diagnosed with any disease showed a significant link with LBW occurrences. Additionally, variables such as awareness of pregnancy planning, history of miscarriage, complications in pregnancy, daily meals taken, fruit consumption, extra protein intake, and pressure during pregnancy exhibited statistically significant associations with LBW. The findings suggest that, although some factors may not exhibit a strong association with LBW, others, such as being diagnosed with diseases during pregnancy, awareness of pregnancy planning, nutritional intake, and specific pregnancy-related complications, may have the potential to influence the likelihood of LBW occurrences.
Factors associated with the birth of low-birth weight babies
Table 4 presents the LASSO logistic regression analysis results, highlighting the factors influencing LBW. It is utilized to handle multicollinearity and perform variable selection, especially given the number of predictors. LASSO helps identify the most relevant variables by shrinking some coefficients to zero, improving model interpretability. The significant coefficients identified in the model highlight several vital predictors of LBW. Babies diagnosed with chronic diseases have higher odds of being born with LBW, as indicated by a coefficient of 1.2512 (SE: 0.7508, CI: 0.0000, 2.4239). Pregnancies complicated by medical issues are strongly associated with higher odds of LBW, with a coefficient of 2.0861 (SE: 0.7552, CI: 0.0000, 3.2753). Women experiencing pressure to conceive are more likely to have LBW babies, as shown by a coefficient of 0.9670 (SE: 0.5761, CI: 0.0000, 2.0059). Reduced meal frequency (1–2 times a day) correlates with higher LBW risk, with a coefficient of 1.0436 (SE: 0.5882, CI: 0.0000, 2.2391). A history of miscarriage or abortion is associated with increased odds of LBW (coefficient: 0.8377, SE: 0.4931, CI: 0.0000, 1.8658). Marrying at an age younger than 18 years is linked to higher LBW risk, indicated by a coefficient of 0.5546 (SE: 0.5101, CI: 0.0000, 1.7349). Variables, such as maternal education, place of delivery, awareness about the gap between the pregnancies, ANC awareness, tobacco use, fruit intake, rest during pregnancy, tea or coffee consumption, occupation of women, type of family and social support, were not selected by the LASSO model and suggested that these factors do not have a significant association with LBW in this context. Other variables showed no clear association with LBW risk.
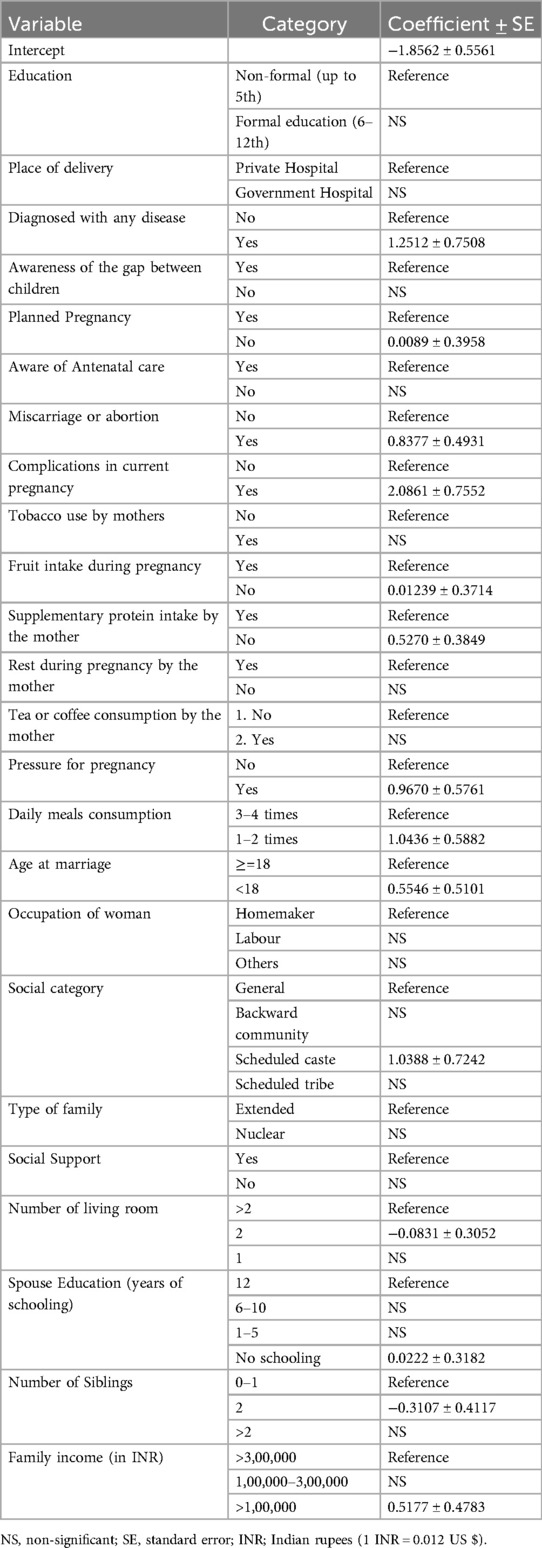
Table 4. Details of lasso regression coefficients for the association of mothers’ characteristics with LBW .
Discussion
The current research provides insights into LBW and its associated factors in rural Rajasthan. The study provides a comparison between LBW and non-LBW cases as per a pre-defined inclusion and exclusion criteria. LBW was more common among labourers recognized as underprivileged communities, especially in nuclear families. Similar results were documented by previous research (13) showing that mothers from lower socioeconomic strata and disadvantaged populations are known to have higher occurrences of LBW. Factors such as disease diagnosis during pregnancy, awareness of pregnancy planning, nutritional intake, and specific complications influenced the likelihood of LBW occurrences. Results revealed a strong association between a history of miscarriage and such outcomes. LBW is strongly associated with preterm birth. Mothers with a familial history of preterm birth face a higher risk. Maternal education strongly correlates with the frequency of preterm birth and LBW instances. Low socio-economic conditions increase the risk of LBW deliveries compared to better conditions. Infections during pregnancy are a major cause of LBW cases. Body Mass Index (BMI) plays a crucial role in LBW birth, and an interpregnancy interval of less than one year significantly impacts LBW birth rates. Mothers using multivitamins and folic acid during pregnancy have lower chances of LBW birth, while malnourished women are at a higher risk (14). The postponement of prenatal care initiation can be attributed to factors such as a lack of access to health services, maternal age, parity, or socioeconomic status. Economic hardship hinders individuals from accessing medical services, travelling for referrals, and acquiring essential food and sanitary products. These challenges, in turn, indirectly impact a baby's birth weight (15).
Mother's age, educational attainment and socioeconomic status greatly impact LBW in India (13). The adolescent mothers are more likely to have LBW babies (16). Confirming the same, the current research reiterates that marrying at an age younger than 18 years is linked to higher LBW risk. Among the examined socioeconomic factors, including maternal illiteracy, manual labour, nuclear family structure, poor socioeconomic status, consanguinity history, and tobacco consumption, a notable proportion of LBW cases was observed in mothers aged below 20 and above 30 years. Risk factors associated with LBW encompass elements such as insufficient iron intake (less than 180 tablets), inadequate weight gain (less than 6.53 kg) during the second and third trimesters, presence of comorbidities during pregnancy, attendance at antenatal care, and experiencing preterm birth. The literature emphasizes that various socio-demographic factors continue to play a crucial role in causing LBW among newborns (9). This underscores LBW as a complex, multi-faceted phenomenon. Mother's education, parity, pregnancy planning, twin birth and maternal smoking during pregnancy were significant determinants of LBW in developing nations (Islam and Khan, 2016; Islam et al., 2020) Furthermore, maternal health conditions such as hypertension, diabetes, and anaemia were identified as significant risk factors for delivering LBW babies, as highlighted in a study conducted in Kerala (17). Among the reported birth weights, 22 per cent of children had LBW, indicating a weight below 2.5 kg (17). The research also shows significant evidence highlighting that pregnancies complicated by medical issues and women experiencing pressure to conceive are more likely to have LBW babies (18). It found that the gender of the baby, type of family, socioeconomic status, maternal educational level, maternal occupation, anaemia, and iron-folic acid intake significantly influenced LBW in rural contexts in India. LBW prevalent in Northern India has been linked to infant deaths (19), finding that previous LBW is the strongest indicator for subsequent delivery of an LBW baby and may further exacerbate the risk of other adverse perinatal outcomes. They also highlight the importance of utilizing multiple co-occurring risk factors and the impact of compounding risks in determining preterm birth and LBW.
The present study suggests using educational interventions focusing on promoting national programmes, i.e., Poshan Abhiyaan, Pradhan Mantri Surakshit Matritva Abhiyan and Integrated Child Development Services (ICDS), for emphasis on nutrition and comprehensive and quality antenatal care for pregnant women and mothers. The ICDS scheme supports pregnant women by providing supplementary nutrition, antenatal care and health education through Anganwadi centres. It ensures better maternal health by addressing malnutrition, immunisation, and promoting institutional deliveries. These efforts help improve birth outcomes, especially in rural and underserved areas (19). Prioritizing policies to address LBW risk factors is crucial for significantly reducing infant mortality. Utilizing the media to raise awareness about LBW complications and implementing WHO-recommended public-private partnerships in the health sector can enhance survival outcomes for newborns with LBW (20). The factors can be effectively prevented through simple family actions, and mothers can easily adopt them. Maternal health programs should focus on encouraging and monitoring complete iron tablet intake during pregnancy. Families can support mothers by ensuring adequate rest, nutrition, and healthy behaviour to mitigate the identified risk factors (21). In some communities, pregnant women are restricted from eating sufficient food, not only due to poverty but also because of cultural practices or beliefs (22). There is a need for nationally representative data on the prevalence of LBW generated from community-based surveys (23–26). Future research should examine indicators like BMI, anaemia, smoking, alcohol use, and history of LBW during pregnancy. Tailored home-based neonatal care setups and revised awareness campaigns are essential for LBW babies (16). Establishing a portal for LBW at birth, recording weight, and providing supervision up to age five can help prevent under-5 mortality (16). Interventions targeting improvements in antenatal care access, maternal health, and nutritional status may help deal with the problem of LBW babies (13).
Strengths and limitations
While discussing the study's implications, it is essential to highlight its strengths and limitations. The study involved a large sample size to strengthen the reliability of the findings. It provided a detailed analysis of various maternal, socio-economic and health-related factors influencing LBW occurrence. However, the study design is cross-sectional, which limits its ability to establish causal relationships. The design discloses the correlation but doesn’t establish cause and effect among the variables under study. As a result, the associations identified in this study should be interpreted as correlations rather than causal links. Another limitation may persist due to a possible recall bias, since many responses are self-reported by the study participants. Furthermore, the study does not account for home deliveries or the associated cases of LBW, potentially missing important data relevant to the findings. Incorporating a limited number of participant cases (n = 92) could impact the generalizability of the study findings.
Conclusions
LBW was more prevalent in underprivileged communities and particularly in nuclear families. The average weight of LBW babies was 2.12 kg, compared to 3 kg in the healthy control group. Factors like disease diagnosis during pregnancy, awareness of pregnancy planning, nutritional intake, and specific complications were found to impact the likelihood of LBW occurrences. The significant coefficients identified in the model highlight several vital predictors of LBW. Pregnancies complicated by medical issues and women experiencing pressure to conceive are more likely to have LBW babies. Babies diagnosed with chronic diseases and reduced meal frequency for women (1–2 times a day) and marrying at an age younger than 18 years correlate with higher LBW risk. A history of miscarriage or abortion is strongly associated with increased odds of LBW. By minimizing the burden of LBW, India may progress towards achieving the Sustainable Development Goals target of reducing child mortality and malnutrition by 2030.
Data availability statement
The original contributions presented in the study are included in the article; further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by ICMR-National Institute for Implementation Research on Non-Communicable Diseases, Jodhpur, India. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
RS: Conceptualization, Methodology, Project administration, Resources, Visualization, Writing – original draft, Writing – review & editing. RH: Formal analysis, Funding acquisition, Writing – original draft, Writing – review & editing. MK: Data curation, Funding acquisition, Methodology, Writing – original draft, Writing – review & editing. PG: Data curation, Funding acquisition, Writing – review & editing. PK: Data curation, Formal analysis, Investigation, Writing – review & editing. BB: Formal analysis, Methodology, Software, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. ICMR-NIIRNCD, Jodhpur, India.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Suryakantha A. Community Medicine with Recent Advances. New Delhi: Jaypee Brothers Medical Publishers (P) Ltd (2017). doi: 10.5005/jp/books/12912
2. International Institute for Population Sciences (IIPS) and ICF. National family health survey (NFHS-5) India 2019–21. Demographic Health Surveys. (2021) I:1–714.
3. Martínez-Galiano JM, Hernández-Martínez A, Rodríguez-Almagro J, Delgado-Rodríguez M. Quality of life of women after giving birth: associated factors related with the birth process. J Clin Med. (2019) 8:324. doi: 10.3390/jcm8030324
6. United Nations. The millennium development goals report. United Nations (2015):72. 978-92-1-101320-7
7. WHO. Low birth weight. WHO. Available online at: https://www.who.int/data/nutrition/nlis/info/low-birth-weight (Accessed July 12, 2024).
8. Jańczewska I, Wierzba J, Jańczewska A, Szczurek-Gierczak M, Domżalska-Popadiuk I. Prematurity and low birth weight and their impact on childhood growth patterns and the risk of long-term cardiovascular sequelae. Children. (2023) 10:1599. doi: 10.3390/children10101599
9. Bhue PK, Acharya HP, Pradhan SK, Biswal P, Swain AP, Satapathy DM. Socio-demographic factors associated with low birth weight in a tertiary care hospital of Odisha. Int J Community Med Public Health. (2018) 5:1797. doi: 10.18203/2394-6040.ijcmph20181493
10. Diabelková J, Rimárová K, Urdzík P, Dorko E, Houžvičková A, Andraščíková Š, et al. Risk factors associated with low birth weight. Cent Eur J Public Health. (2022) 30:S43–9. doi: 10.21101/cejph.a6883
11. Sangwan RK. Health, Human Rights and Ethics: A Sociological Study in Hospital Setting. Jaipur: Rawat Publications (2017).
12. Mumbare SS, Maindarkar G, Darade R, Yenge S, Tolani MK, Patole K. Maternal risk factors associated with term low birth weight neonates: a matched-pair case control study. Indian Pediatr. (2012) 49:25–8. doi: 10.1007/s13312-012-0010-z
13. Scaria L, Soman B, George B, Ahamed Z, Hariharan S, Jeemon P. Determinants of very low birth weight in India: The National Family Health Survey-4. Wellcome Open Res. (2022) 7:20. doi: 10.12688/wellcomeopenres.17463.2
14. Khan MW, Arbab M, Murad M, Khan MB, Abdullah S. Study of factors affecting and causing low birth weight. J Sci Res. (2014) 6:387–94. doi: 10.3329/jsr.v6i2.17090
15. Vahdaninia M, Tavafian SS, Montazeri A. Correlates of low birth weight in term pregnancies: a retrospective study from Iran. BMC Pregnancy Childbirth. (2008) 8:12. doi: 10.1186/1471-2393-8-12
16. Singh D, Manna S, Barik M, Rehman T, Kanungo S, Pati S. Prevalence and correlates of low birth weight in India: findings from national family health survey 5. BMC Pregnancy Childbirth. (2023) 23:456. doi: 10.1186/s12884-023-05726-y
17. Pawar A, Kumar D. Maternal factors associated with low birth weight: a case control study in rural Kerala. Int J Community Med Public Health. (2017) 4:3793. doi: 10.18203/2394-6040.ijcmph20174252
18. Kumar M, Verma R, Khanna P, Bhalla K, Kumar R, Dhaka R, et al. Prevalence and associate factors of low birth weight in North Indian babies: a rural based study. Int J Community Med Public Health. (2017) 4:3212. doi: 10.18203/2394-6040.ijcmph20173815
19. Kiplagat S, Ravi K, Sheehan DM, Srinivas V, Khan A, Trepka MJ, et al. Sociodemographic patterns of preterm birth and low birth weight among pregnant women in rural Mysore district, India: a latent class analysis. J Biosoc Sci. (2023) 55:260–74. doi: 10.1017/S0021932022000037
20. Jana A, Saha UR, Reshmi RS, Muhammad T. Relationship between low birth weight and infant mortality: evidence from National Family Health Survey 2019–21, India. Arch Public Health. (2023) 81:28. doi: 10.1186/s13690-023-01037-y
21. Kc A, Basel PL, Singh S. Low birth weight and its associated risk factors: health facility-based case-control study. PLoS One. (2020) 15:e0234907. doi: 10.1371/journal.pone.0234907
22. Nagar M, Maurya NK. Impact of nutritional practices and food taboos on pregnant women in India: a comprehensive review. Res Rev J Food Sci Technol. (2024) 13:15–22. Available online at: https://journals.stmjournals.com/agriculture/article=2024/view=175784/ (Accessed February 12, 2025).
23. Bhilwar M, Upadhyay RP, Yadav K, Kumar R, Chinnakali P, Sinha S, et al. Estimating the burden of “weighing less”: a systematic review and meta-analysis of low birth-weight in India. Natl Med J India. (2016) 29:73–81.27586210
24. Islam MM, Khan MHR. Incidence of and risk factors for small size babies in Bangladesh. Int J Community Fam Med. (2016) 1:123.
25. Islam MM, Ababneh F, Akter T, Khan HR. Prevalence and risk factors for low birth weight in Jordan and its association with under-five mortality: a population-based analysis. East Mediterr Health J. (2020) 26(10):1273–84.33103755
26. Census of India. “Census of India: Rajasthan (Series 09) District Census Handbook: Jalor.” Census of India, Directorate of Census Operations, Rajasthan, Ministry of Home Affairs, Government of India (2011). Available online at: censusindia.gov.in/nada/index.php/catalog/1078/download/3326/DH_2011_0818_PART_A_DCHB_JALOR.pdf
Keywords: low-birth weight, social determinants, maternal health factors, nutrition and diet, behavioural health practices
Citation: Sangwan RK, Huda RK, Khetan M, Gazta P, Kumar P and Babu BV (2025) Low birth weight and associated factors in rural population of Rajasthan, India. Front. Glob. Women's Health 6:1587991. doi: 10.3389/fgwh.2025.1587991
Received: 10 March 2025; Accepted: 30 June 2025;
Published: 16 July 2025.
Edited by:
Rubeena Zakar, University of the Punjab, PakistanReviewed by:
Md Hasinur Rahaman Khan, University of Dhaka, BangladeshMelissa Liher Martínez-Shaw, University of Cádiz, Spain
Copyright: © 2025 Sangwan, Huda, Khetan, Gazta, Kumar and Babu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ramesh Kumar Sangwan, cmFtZXNoMjE5ODc5QGdtYWlsLmNvbQ==
†These authors share first authorship
‡These authors share second authorship
§ORCID:
Ramesh Kumar Sangwan
orcid.org/0000-0002-3127-4026
Ramesh Kumar Huda
orcid.org/0000-0002-1239-3660
Mukti Khetan
orcid.org/0000-0002-1017-1474
Parul Gazta
orcid.org/0000-0002-8858-1182
Pankaj Kumar
orcid.org/0000-0002-4439-4908
Bontha V. Babu
orcid.org/0000-0001-5096-2222
 Ramesh Kumar Sangwan
Ramesh Kumar Sangwan Ramesh Kumar Huda
Ramesh Kumar Huda Mukti Khetan
Mukti Khetan Parul Gazta‡,§
Parul Gazta‡,§ Bontha V. Babu
Bontha V. Babu