- 1Department of Nursing and Midwifery, Ga West Municipal Hospital-Ghana Health Service, Accra, Ghana
- 2Department of Accountancy, Faculty of Business and Management Studies, Sunyani Technical University, Sunyani, Ghana
- 3Department of Marketing and Supply Chain Management, School of Business, University of Cape Coast, Cape Coast, Ghana
- 4Department of Maternal and Child Health, School of Nursing and Midwifery, University of Ghana, Accra, Ghana
Maternal health has been a focal point of global attention since the 1980s, with initiatives like Safe Motherhood, Millennium Development and Sustainable Development Goals aiming to improve the well-being of women and infants worldwide. Despite these efforts, high maternal and neonatal mortality rates persist, particularly in middle-income countries, including Ghana, highlighting the need for urgent action. From 2000 to 2020, Ghana successfully halved its maternal mortality ratio from 499 to 263 deaths per 100,000 live births through various interventions and strategies, which is still higher than the global average. Emergency obstetric and neonatal care (EmONC) plays a vital role in preventing maternal and neonatal deaths, yet disparities in its distribution and delivery exist, particularly in Ghana. An evaluation of EmONC facilities in Ghana highlighted the challenges of infrastructure, human resources, logistics, and equipment in meeting the World Health Organisation standards for EmONC within national, regional, rural, and urban health facilities. This critical analysis paper aims to highlight these challenges and propose comprehensive solutions for improved delivery of EmONC services. Addressing these challenges requires comprehensive efforts to improve infrastructure, human resources, and supply chain logistic support. A two-pronged approach is recommended. One recommendation focuses on upgrading existing facilities and recruiting and retaining healthcare professionals in rural and underserved areas. The second recommendation calls for increasing the capability of delivery of EmONC by improving training efficiency and focusing on facilities missing only one or two of the seven key services required for basic emergency obstetric and newborn care.
1 Introduction
Maternal mortality refers to deaths occurring in women during pregnancy or within 42 days after childbirth (1). In contrast, pregnancy-related death encompasses any death that occurs during pregnancy or within one year after its termination, regardless of the cause, including accidental or incidental factors (2). The maternal mortality ratio (MMR), an estimate of maternal mortality per 100,000 live births within a specific time, is a metric for evaluating obstetric care quality and overall healthcare delivery (3). Globally, women experience complications during pregnancy or postpartum, resulting in 223 deaths per 100,000 live births annually (4, 5). Although recent efforts have decreased MMRs in low-middle-income countries, high rates persist (3, 6–9). Moreover, 2.3 million neonates die annually, and 1.9 million are stillborn globally (10, 11). Additionally, numerous women and infants suffer from disabilities related to childbirth. Most of these mortalities and disabilities are preventable. Although some complications during pregnancy and birthing cannot be foreseen or averted, almost all of them can be effectively managed with competent and efficient emergency obstetrics and newborn care (EmONC) (4).
From 2,000 to 2020, Ghana has successfully halved its maternal mortality ratio (MMR) from 499 to 263 deaths per 100,000 live births, but this rate is still higher than the global average (12). Various policy interventions by the government have contributed to this success (3). These initiatives include the National Health Insurance (NHI) Act 2003, which aims to provide all residents with quality, affordable healthcare services (3). The free maternal healthcare policy, Safe Motherhood Programme, Life Saving Skills Programme, Integrated Management of Childhood Illness, Focused Antenatal Care, and Accelerated Child Survival and Development have also contributed to reducing maternal and neonatal mortality (13, 14). The Ghana Essential Health Intervention Programme (GEHIP) has bolstered the Community Health Planning Services (CHPS), which ensures healthcare accessibility in rural communities (14). The CHPS programme is a national strategy aimed at enhancing healthcare delivery within communities and strengthening primary healthcare in rural areas. This initiative was established to offer a range of services, including health education, health promotion, management of minor ailments, community mobilisation for health initiatives, referral services, and home visits (15). Despite these concerted efforts, maternal and newborn deaths remain elevated (16) compared to the global standard (5, 17).
EmONC encompasses a set of interventions for mothers and newborns experiencing severe complications in the course of pregnancy, delivery, and postpartum (18). It is estimated that accessible and high-quality EmONC could prevent three-fourths of maternal mortality (19). However, its effectiveness relies on the readiness of health facilities to deliver care, the quality of care provided, and the functionality, timeliness, and organisation of referral systems within a given context (18).
High quality EmONC entails enhancing the capabilities of health facilities to deliver essential services aimed at preventing avoidable deaths during childbirth (20). It involves upgrading selected health centres and referral hospitals to ensure an adequate reserve of basic drugs, materials, and equipment and trained healthcare professionals to deliver quality services consistently (20). EmONC is categorised into basic EmONC (BEmONC) and comprehensive EmONC (CEmONC). BEmONC facilities provide essential functions such as administering oxytocic drugs and antibiotics as well as performing procedures like manual removal of the placenta and basic neonatal resuscitation. CEmONC facilities provide all BEmONC functions along with additional services such as caesarean sections and blood transfusions (20). The UN guidelines recommend a minimum of five EmONC facilities per 500,000 people, with not less than one offering comprehensive care (21). In contrast, Ghana has set a more stringent target, aiming for at least five EmONC facilities per 200,000 people, including one offering comprehensive care (19).
Stakeholder perspectives on substandard EmONC in Ghana underscore several key issues. These include the concentration of EmONC services in central locations, inadequate funding, limited opportunities for hands-on training, delays in the recruitment of newly trained essential personnel, and a lack of provider engagement in the profession (22). The “three delays’ model aids in pinpointing potential points of delay in handling obstetric complications (23). The first, second and third delay encompasses delays in seeking medical attention, locating and accessing the healthcare facility and receiving care at healthcare facilities, which can stem from various factors such as facility organisation, care quality, and the availability of staff and equipment (24). All hospitals in Ghana are expected to provide the full range of EmONC services (25). However, an evaluation of EmONC facilities in Ghana highlighted infrastructure, human resources, logistics and equipment challenges in meeting the World Health Organisation standards for EmONC within all health facilities (19, 25). Addressing these challenges is crucial to efficiently managing obstetric emergencies (23). Here, we explore the context of these challenges and propose comprehensive solutions.
2 Infrastructure
Ghana's health system is characterised by a high degree of decentralisation. It is managed by the Ministry of Health (MoH) in collaboration with sub-agencies such as the Ghana Health Services (GHS) and the National Health Insurance Authority (NHIA). The MoH is primarily responsible for policy and regulatory oversight and managing teaching hospitals. At the same time, the GHS is tasked with promoting access to health services at the community, sub-district, district, and regional levels. The NHIA administers the National Health Insurance Scheme (NHIS) (26). Both the public and private sectors are vital stakeholders in the healthcare system. The public sector is structured into several tiers: national (teaching hospitals), regional hospitals, district (public and mission hospitals), sub-district (public health centres), maternity homes and community (CHPS). Modern healthcare services are supplemented by traditional medicine, which remains popular, especially among rural populations (27).
In 2011, Ghana undertook a national survey of its 1,268 healthcare facilities. Among these were 273 District hospitals, three teaching hospitals, 518 health centres, nine regional hospitals, 139 CHPS, 165 Maternity homes, and 161 health clinics (19). Facilities were categorised as BEmONC if they offered all seven BEmONC signal functions (28) such as administering oxytocic drugs, antibiotics, and anticonvulsants, manual removal of the placenta and basic neonatal resuscitation within the preceding three months, while those providing all the seven BEmONC plus caesarean sections and blood transfusions were graded as CEmONC (19). Using the more stringent requirement of a minimum of five EmONC facilities per 200,000 individuals, including at least one facility offering CEmONC, there should ideally be 485 basic facilities and 121 comprehensive facilities. However, the national assessment found that only 13 facilities met the criteria for BEmONC, resulting in a shortfall of 472 facilities. Additionally, 76 comprehensive facilities meet the standard for CEmONC, leaving a gap of 45 (19). Conversely, according to the United Nation Development programme, a 2020 assessment revealed that only 52 health facilities had the capacity to deliver CEmONC, falling significantly short of the national target of 155 facilities (29).
From 2022 to 2023 Ghana Harmonised Facilities Assessment (GHFA) report, of the 1,421 health facilities surveyed, 66% of facilities reported offering BEmONC. Only 15% delivered all seven BEmONC signal functions. 39% of polyclinics and 10% of health centres offer all seven BEmONC signal functions. However, 17% of district hospitals and 49% of general hospitals do not offer all seven basic EmONC (BEmONC) signal functions (25). On the other hand, the availability of CEmONC services remains limited. Only 16% of facilities reported offering caesarean section services, and 18% provided blood transfusions. While 20% of facilities identified as offering CEmONC services, just 10% met the full criteria by providing all nine signal functions. Although 15% of health centres claimed to offer CEmONC, a closer look revealed that fewer than 2% actually provided either blood transfusion or caesarean section services, indicating a significant gap between reported and actual capacity. Yet, 17% of district hospitals and 53% of general hospitals lack the full complement of nine comprehensive EmONC (CEmONC) signal functions (25).
Bosomprah et al. (2016) conducted a study aimed at policy recommendations for addressing deficiencies in the delivery of signal function services and their distribution throughout the country (see Figure 1). Results found that out of 1,159 maternity facilities surveyed, only 89 (7.7%) were equipped to provide all the necessary basic or comprehensive EmONC signal functions once in the three months preceding the national survey. Accordingly, just 21% of births in healthcare facilities occurred in operational EmONC facilities, while a further 30% took place in facilities lacking one or two basic signal functions. Thus, addressing these deficiencies in signal functions could potentially improve the ratio of births in fully operational facilities to over 50% (30). Regionally, there is significant variation in the availability of EmONC facilities, with most facilities located in urban areas, and a few located in rural areas especially in the three northern regions (upper west, upper East and Northern) as CHPS and health centres, which is not mandated or cannot provide EmONC (19, 25, 31). The assessment (19) included 216 facilities from the Greater Accra region, 148 facilities from the Ashanti region, and 96 facilities from the Upper West region. The Ashanti and Greater Accra Regions have the largest gaps, with 97 and 87 facilities, respectively, while the Upper West Region has the smallest gap, with only 12 facilities that meet facility per population. Also, 80% of health facilities in the northern region of Ghana failed to meet the criteria for providing EmONC (31). For CEmONC facilities, the Greater Accra Region faces the largest shortfall of 13 facilities per population. Regarding Basic EmONC, Ashanti has the greatest deficit, needing 91 more facilities, whereas Upper West has the smallest deficit, needing only 14 facilities in addition to existing facilities in order to meet expected access points per population of individual region (19). Per recent GHFA report, nearly all regions indicated that at least 50% of their sampled facilities provided some BEmONC services (25). With the exception of the Greater Accra region, all other regions had fewer than 30% of facilities capable of delivering CEmONC services (25).
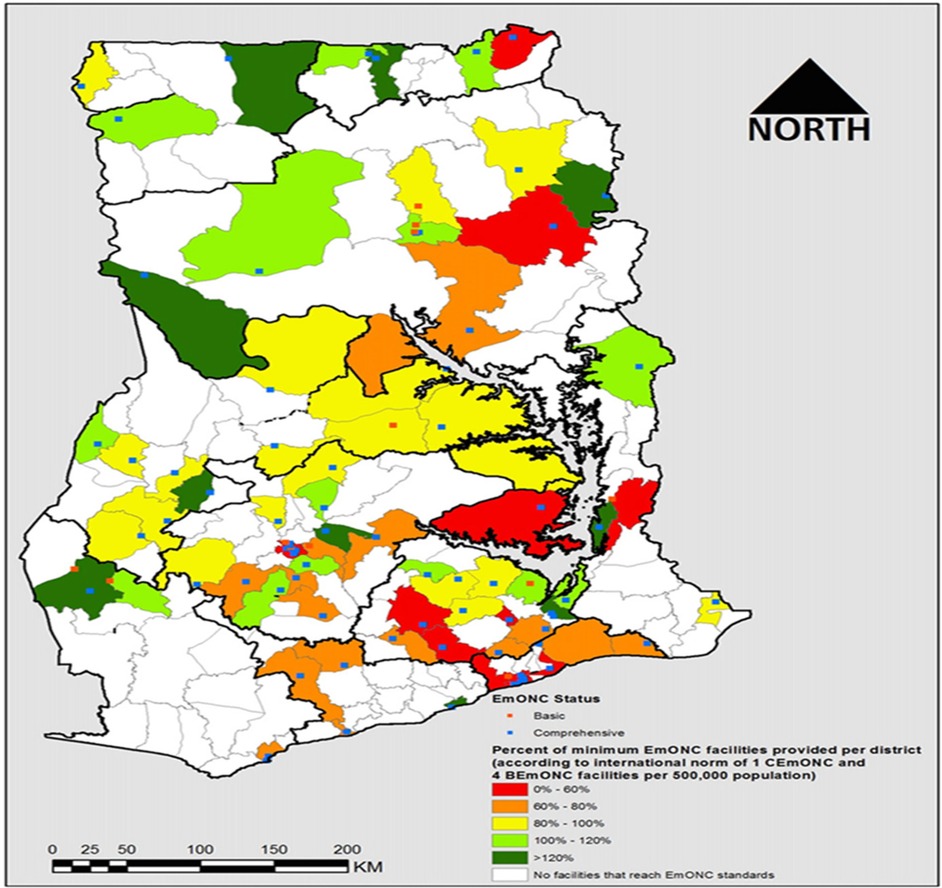
Figure 1. The percentage of the minimum acceptable number of fully functioning EmONC facilities per district (30).
The lack of medications and personnel capable of dealing with pregnancy complications at the appropriate level of a facility affects referral rates and increases delays in care. Bailey et al. (32) identified a strong correlation between readiness to perform EmONC and referral to the next level of care. In this study, over half of births took place in district hospitals but only 21% of these were prepared to treat postpartum haemorrhage and abortion complications. As expected, facilities with adequate supplies numbers of midwives, and enhanced communication and transportation systems referred out fewer women.
An additional infrastructure problem is the unequal geographical distribution of prepared health facilities, which can result in poor maternal and neonatal outcomes. In contrast, a study of four districts in Ghana covering 95 facilities found that 67% of emergency facilities were located in the least populated districts (33). However, this study also found that only 6% of basic health facilities were equipped to perform all EmONC signal functions, and only 3% of emergency facilities could perform all aspects of CEmONC. Moreover, 39% of maternal and neonatal mortality cases occurred at facilities incapable of providing basic emergency services (33).
3 Human resources
Human resources play a pivotal role in all aspects of EmONC services, significantly influencing its quality, particularly for complications requiring clinical procedures (34). In Ghana, highly skilled health workers tend to be concentrated in urban areas and work predominantly in public institutions, leaving rural and underserved regions with less skilled personnel (35).
Similar to other countries in Africa, Ghana has a pressing shortage of healthcare professionals (36). A study of the types and distributions of healthcare professionals found that 74% of CHPS zones failed to meet the requirement of having one midwife, although 91% of health centres did have at least one midwife (35). Further, only 29% of primary hospitals have an obstetrician-gynaecologist (35).
Greater Accra region boasts the highest ratios of obstetricians/gynaecologists (7.2), general practitioners (27.2), and midwives (62.6) per 200,000 people. In contrast, the Northern region has the lowest numbers, with only 0.4 obstetricians/gynaecologists, 3.2 general practitioners, and 25.0 midwives per 200,000 population. Most health centres, clinics, maternity homes, and CHPS zones typically have just one midwife or none (19).
For instance, data indicates that 42% of doctors are in Greater Accra alone, and up to 81% are concentrated in just five regions—Greater Accra, Ashanti, Central, Northern, and Volta (37). Teaching hospitals in these regions collectively house over 60% of all doctors in Ghana. This is largely due to the perception that urban areas offer better working conditions, including career development opportunities, lighter workloads, better clinical infrastructure, enhanced social life, improved accommodation, and higher income (38, 39). This uneven distribution results in unmet health needs in rural and remote areas, leading to lower life expectancy and higher rates of preventable maternal and under-5 mortality (37). Several studies in Ghana have reported the impact of unequal distribution of human resources of EmONC service (20, 31, 40, 41).
The delivery of EmONC depends on having personnel available and ensuring they are trained to perform the needed services (24). A systematic review focusing on the human resources aspect of EmONC revealed that staff shortages pose a significant barrier to delivering high-quality EmONC services (34). The GHFA report indicated that 71% of health facilities offered delivery services, with 67% providing 24/7 delivery care by a skilled provider (25). Additionally, skill deficiencies in essential healthcare professionals further exacerbate the challenge of delivering quality EmONC (20, 31). Typically, BemONC training is delivered as a 10-day course where healthcare professionals who provide direct maternal and neonatal care gather at a site away from their facility and receive both didactic and hands-on practice. This intensive experience, although effective, can be expensive and time-consuming and does not ensure that all personnel at a facility are trained in BEmONC (42).
Lastly, barriers to effective management of emergency referrals include inadequate healthcare personnel to manage patient management during transit, someone to accompany more stable patients, and provision of sufficient patient information to the receiving facility (41). These challenges were also highlighted by Afari et al. (2014), who emphasised that the scarcity of healthcare professionals results in limited clinical expertise and management, compromised quality of care, and inadequate supervision and interventions.
4 Supply chain logistics and equipment
EmONC's effectiveness heavily depends on the availability of supply chain logistics and equipment. These resources are crucial for providing timely and appropriate care to women and newborns in critical situations. Without an adequate supply of medications and equipment, health facilities may struggle to perform essential procedures and interventions, leading to increased risks of maternal and newborn morbidity and mortality. Additional factors are essential for the medications on hand to be effective. For example, effective oxytocin requires ensuring that the initial packing uses an adequate amount of the active ingredient and that the medication is stored at 2–8°C (43). A recent survey in Ghana found that 90% of health clinics and hospitals had a refrigerator to store oxytocin but only 40% of CHPS zones doing deliveries did have refrigerator (44). An older study analysed samples of two drugs for the prevention and treatment of postpartum haemorrhage and found the median percent of active ingredients were only 64% and 50% for oxytocin and ergometrine, respectively (45). Regarding the supply of logistics and equipment, the national assessment on EmONC reported that all teaching and regional hospitals are well-equipped, whereas only 74% of district hospitals, health centres, and CHPS zones have adequate supplies (19).
Recently, GHFA (25) found that the availability of essential life-saving commodities such as oxytocin injection, magnesium sulfate injection, and misoprostol tablets is high in hospitals, with coverage exceeding 96%. However, availability is significantly lower at health centres and CHPS compounds. Additionally, only 44% of health centres and 14% of CHPS have newborn resuscitation equipment. These commodities and equipment are expected to be available only in facilities staffed with midwives (25). Moreover, among facilities providing CEmONC services, only 63% of regional hospitals and 41% of district hospitals had a functional anaesthesia machine (25). A recent study among postpartum women in Ghana found deficiencies in medication and equipment, further compromising the delivery of high-quality care (20). According to a study by Daniels & Abuosi (2020), healthcare professionals also encountered obstacles to the referral process, including underutilisation of ambulance services and inadequate availability of beds, medications, and blood.
Emergency Transport System (ETS) serves as a critical link between healthcare facilities and families of women in need of urgent maternal transport. Community involvement is fundamental to improving emergency transport services. National data from Ghana in 2011 indicate that only 33% of health facilities rely on the national ambulance system for emergency referrals. In contrast, 51% use private transport options such as taxis or buses, while 46% expect clients to arrange their own transport. Among maternity units, 70% depend on private transport, whereas 62% of CHPS compounds assume clients will organise their own transportation (19). However, according to the 2022–2023 Ghana Harmonised Health Facilities Assessment Report, only 32% of health facilities nationwide have access to an emergency transport system. Access is particularly limited at the primary care level, with just 18% of CHPS compounds, 29% of health centres, 39% of polyclinics, and 40% of clinics and maternity homes equipped with such systems (25).
According to Oguntude et al. (46), community members perceive the ETS as reliable and responsive to women's emergency needs. Sunguya et al. (47) highlight that collaboration with local taxi drivers supports the timely referral of pregnant women, while the repair and upgrading of ambulances and coordination with receiving facilities further enhance the emergency response. A systematic review by Wilson et al. (48) identifies several potential solutions to maternal transport challenges, including motorcycle ambulance programmes, partnerships with taxi services, community education efforts, financial subsidies, and regular maintenance of vehicles.
5 Recommendations
There are still gaps in Ghana meeting national and global EmONC guidelines, so solutions are needed to address these disparities. A two-pronged approach is recommended. One recommendation focuses on upgrading existing facilities and recruiting and retaining healthcare professionals in rural and underserved areas. The second calls for an increase in the capability of delivery of EmONC by improving training efficiency and focusing on facilities missing only 1–2 signal functions.
5.1 Improving the provision of health care in rural and underserved areas
Through the Ministry of Health, the government must implement measures to improve underserved areas, including CHPS zones and a majority of the facilities in the Northern Region. Supply issues to CHPS zones should be a focus of efforts, so these facilities can meet the primary care needs of the community. Strategies for maintaining adequate electricity for the limited medication supply requiring refrigeration and supply chain issues need to be developed. Evidence shows that well-equipped health facilities assist with healthcare worker retention and satisfaction (49).
Policymakers need to develop effective deployment strategies to facilitate the movement of personnel to these high-need areas and ensure an equitable distribution of healthcare professionals. Experiments in other African countries have shown that higher wages and offering continuing education and career development opportunities are the most effective incentives (50). Healthcare workers, especially new graduates, want to be supported by a manager or mentor (51). Additionally, subsidised housing has also shown to be helpful in recruitment and retention. Ghana may want to develop its discrete-choice experiments in developing a tailored incentive package for recruiting and retaining healthcare workers in rural areas (52). In the long term, Ghana should consider a rural pipeline program that identifies students interested in healthcare in rural communities and provides tuition assistance for education (49). Additionally, programs should examine their curriculum to ensure that rural health subjects are taught and that students receive some training in rural health environments (49). When rural healthcare is part of training, retention and rural outcomes are improved as students often return to their communities where they have an intimate understanding of the social and cultural aspects of the community and its intersection with health (53).
Although Ghana's maternal health services are integrated into the NHIS, substantial gaps in human resources and logistical capacity hinder effective service delivery (25). To this end, adopting the cost-benefit analysis of priority health system strengthening interventions proposed by Asuning et al. (54) offers a strategic pathway for maximising health returns through targeted, efficient investments aligned with national health financing goals. The analysis found that over 15 years (2018–2032), addressing the national gap in EmONC facilities in Ghana is projected to cost approximately GH¢ 835 million, discounted at 8% (54). This cost estimate encompasses investments in staff capacity, logistical support, and minor extensions or renovations of existing infrastructure. In contrast, the projected economic benefits, primarily from averting neonatal deaths and reducing morbidity through nationwide EmONC scale-up, are estimated at GH¢ 5.8 billion (54).
5.2 Increase the capability of delivering EmONC
The traditional 10-day course for teaching EmONC should be replaced with an evidenced-based lower, intensity but high-frequency method. A cluster-randomized trial conducted from March 2014 to February 2017 across 40 public and mission hospitals in three regions of Ghana found this approach resulted in a sustained decrease in facility-based newborn mortality and intrapartum stillbirths (42). This approach provides two 2-day didactic and simulation sessions for all persons involved with birth at a facility. These 2-day sessions are a month apart and between sessions, participants receive SMS text messages with reminders and short quizzes as well as mentoring by an on-site person designated as an EmONC mentor. The SMS messaging continues for up to 10 months after the last 2-day session. For facilities with a small number of workers, an outside EmONC mentor could be identified who could be available and meet regularly by SMS messaging or telephone. This system would allow for a less costly and more efficient method of training a greater number of healthcare workers in EmONC and maintaining their skills.
A geospatial study by Bosomprah and colleagues showed the most efficient strategy for having the greatest benefit in decreasing the number of poor maternal and neonatal outcomes would be to prioritise improving facilities that were missing only 1 or 2 signal functions first (30). Unfortunately, their study mapped facilities that were surveyed in 2010. For this to be an effective strategy, a new survey of birthing facilities would be needed to update the information to proceed. There are a few studies that have conducted more limited surveys of EmONC services that could be used as a starting point in a prioritisation list (30–33).
6 Limitation
This critical analysis is constrained by limited data availability, relying primarily on findings from the National assessment for EmONC in Ghana conducted in 2011 (19), which may not accurately reflect the current state of EmONC services in Ghana. However, more recent data from the 2022–2023 GHFA (25) report were incorporated to supplement and update the earlier information.
7 Conclusions
Improving maternal and child health remains a top priority for the Ghanaian Ministry of Health. Despite substantial progress, a substantial gap exists in facilities providing functional EmONC services. Ghana continues to face significant challenges concerning infrastructure, skilled personnel, equipment and supplies to support EmONC in decreasing maternal and newborn morbidity and mortality.
Addressing these challenges requires comprehensive efforts to improve infrastructure, human resources, and supply chain logistics support. Upgrading facilities that lack just one or two signal functions will enable Ghana to approach the global criteria for the accessibility of EmONC services (30) and will prevent an estimated 6,666 neonatal deaths and 28,486 annual neonatal deaths over a 15-year implementation period (54).
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
ES: Validation, Writing – review & editing, Methodology, Data curation, Conceptualization, Writing – original draft, Investigation, Resources, Formal analysis, Software. GS: Investigation, Writing – review & editing, Conceptualization, Validation, Software, Resources, Writing – original draft, Project administration, Methodology, Data curation, Formal analysis. RO: Resources, Formal analysis, Validation, Methodology, Data curation, Investigation, Writing – review & editing. EA: Supervision, Writing – review & editing, Writing – original draft, Formal analysis, Data curation, Conceptualization, Methodology, Validation, Investigation.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We acknowledge Dr Mary Barger of the University of California, who reviewed this work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
BEmONC, Basic Emergency Obstetric and Neonatal Care; CEmONC, Comprehensive Emergency Obstetric and Neonatal Care; CHPS, Community Health Planning Services; EmONC, emergency obstetric and neonatal care; GHFA, Ghana Harmonised Facilities Assessment; GEHIP, Ghana Essential Health Initiative Programme; GHS, Ghana Health Service; MMR, maternal mortality ratio; MoH, Ministry of Health; NHI, National Health Insurance; NHIA, National Health Insurance Authority; NHIS, National Health Insurance Scheme.
References
1. World Health Organisation. Trends in maternal mortality 2000 to 2020: estimates by WHO, UNICEF, UNFPA, World Bank Group and UNDESA/Population Division (2023). Available online at: https://www.who.int/publications-detail-redirect/9789240068759 (Accessed April 26, 2024).
2. Joseph KS, Lisonkova S, Boutin A, Muraca GM, Razaz N, John S, et al. Maternal mortality in the United States: are the high and rising rates due to changes in obstetrical factors, maternal medical conditions, or maternal mortality surveillance? Am J Obstet Gynecol. (2024) 230(4):440.e1–440.e13. doi: 10.1016/j.ajog.2023.12.038
3. Adedia D, Nanga S, Appiah SK, Lotsi A, Abaye DA. Box-Jenkins methodology in predicting maternal mortality records from a public health facility in Ghana. Open J Appl Sci. (2018) 8(6):189–202. doi: 10.4236/ojapps.2018.86016
4. World Health Organisation. Maternal mortality (2024). Available online at: https://www.who.int/news-room/fact-sheets/detail/maternal-mortality (Accessed May 26, 2024).
5. UNICEF. Maternal mortality rates and statistics. UNICEF DATA (2024). https://data.unicef.org/topic/maternal-health/maternal-mortality/ (Accessed August 8, 2024).
6. Galaa SZ, Haruna U, Dandeebo G. Trends and causes of maternal mortality at the Wa Regional Hospital, Ghana: 2005–2010. Ghana J Dev Stud. (2016) 13(1):1. doi: 10.4314/gjds.v13i1.5
7. World Health Organisation. New global targets to prevent maternal deaths: Access to a “continuum of care” needed, before, during and after pregnancy and childbirth (2021). Available online at: https://www.who.int/news/item/05-10-2021-new-global-targets-to-prevent-maternal-deaths (Accessed May 26, 2024).
8. World Health Organization. Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division: Executive Summary. Geneva: World Health Organization (2019). Available online at: https://iris.who.int/handle/10665/327596
9. Yarney L. Does knowledge on socio-cultural factors associated with maternal mortality affect maternal health decisions? A cross-sectional study of the greater Accra region of Ghana. BMC Pregnancy Childbirth. (2019) 19(1):47. doi: 10.1186/s12884-019-2197-7
10. UNICEF Data. Never Forgotten: The situation of stillbirth around the globe. UNICEF DATA (2023). Available online at: https://data.unicef.org/resources/never-forgotten-stillbirth-estimates-report/ (Accessed May 26, 2024).
11. World Health Organisation. Newborn mortality (2024). Available online at: https://www.who.int/news-room/fact-sheets/detail/newborn-mortality (Accessed May 26, 2024).
12. The World Bank. Gender indicator for Ghana. World Bank Gender Data Portal (2024). Available online at: https://liveprod.worldbank.org/en/economies/ghana (Accessed June 12, 2024).
13. Asuming PO, Kanmiki EW, Wong B. Cost Benefit Analysis of Priority Health System Strengthening Interventions in Ghana. Copenhagen: Copenhagen Consensus Centre (2020). Available online at: http://www.jstor.org/stable/resrep23674.1 (Accessed May 11, 2024).
14. Awoonor-Williams JK, Tindana P, Dalinjong PA, Nartey H, Akazili J. Does the operations of the national health insurance scheme (NHIS) in Ghana align with the goals of primary health care? Perspectives of key stakeholders in northern Ghana. BMC Int Health Hum Rights. (2016) 16(1)21. doi: 10.1186/s12914-016-0096-9
15. Adusei AB, Bour H, Amu H, Afriyie A. Community-based health planning and services programme in Ghana: a systematic review. Front Public Health. (2024) 12:1337803. doi: 10.3389/fpubh.2024.1337803
16. Ghana Statistical Service—GSS, Ghana Health Service—GHS, ICF. Ghana Maternal Health Survey 2017. GSS, GHS, and ICF (2018). Available online at: http://dhsprogram.com/pubs/pdf/FR340/FR340.pdf (Accessed March 05, 2024).
17. Arora A. Levels and trends in child mortality. UNICEF DATA (2024). Available online at: https://data.unicef.org/resources/levels-and-trends-in-child-mortality-2024/ (Accessed August 8, 2024).
18. Alemayehu M, Yakob B, Khuzwayo N. Effective coverage of emergency obstetric and newborn care services in Africa: a scoping review. Open Access Emerg Med. (2023) 15:93–108. doi: 10.2147/OAEM.S403145
19. Ghana Ministry of Health, Ghana Health Service, UNICEF, UNFPA, WHO, AMDD. National assessment for emergency obstetric and newborn care: Ghana (2011). Available online at: http://www2.statsghana.gov.gh/nada/index.php/catalog/73/download/311 (Accessed May 10, 2024).
20. Ayawine A, Atinga RA. We know it is not good, but we are constrained”: a study on quality of emergency obstetric and newborn care in northern Ghana. Heliyon. (2023) 9(4):e15250. doi: 10.1016/j.heliyon.2023.e15250
21. World Health Organisation, UNPF United Nations Children’s Fund, Averting Maternal Death and Disability. Monitoring emergency obstetric care: A handbook (2009). Available online at: https://www.who.int/publications-detail-redirect/9789241547734 (Accessed May 10, 2024).
22. Ayawine A, Asaarik MJA, Atinga RA. Stakeholder opinions on perceived sub-standard emergency obstetric and newborn care in Ghana. BMC Health Serv Res. (2024) 24(1):461. doi: 10.1186/s12913-024-10936-x
23. United Nations Population Fund. Setting standards for emergency obstetric and newborn care (2014). Available online at: https://www.unfpa.org/resources/setting-standards-emergency-obstetric-and-newborn-care (Accessed May 11, 2024).
24. Actis Danna V, Bedwell C, Wakasiaka S, Lavender T. Utility of the three-delays model and its potential for supporting a solution-based approach to accessing intrapartum care in low- and middle-income countries. A qualitative evidence synthesis. Glob Health Action. (2020) 13(1):1819052. doi: 10.1080/16549716.2020.1819052
25. Ghana Ministry of Health, Ghana Health Service, World Health Organisation. Ghana Harmonized Health Facility Assessment 2022–2023 (2023).
26. Amoah PA, Nyamekye KA, Owusu-Addo E. A multidimensional study of public satisfaction with the healthcare system: a mixed-method inquiry in Ghana. BMC Health Serv Res. (2021) 21(1):1320. doi: 10.1186/s12913-021-07288-1
27. Nketiah-Amponsah E, Hiemenz U. Determinants of consumer satisfaction of health care in Ghana: does choice of health care provider matter? Glob J Health Sci. (2009) 1(2):50. doi: 10.5539/gjhs.v1n2p50
28. Otolorin E, Gomez P, Currie S, Thapa K, Dao B. Essential basic and emergency obstetric and newborn care: from education and training to service delivery and quality of care. Int J Gynaecol Obstet. (2015) 130:S46–53. doi: 10.1016/j.ijgo.2015.03.007
29. UNDP. Draft Country Programme Document for Ghana: Second Regular Session 2022 (2022). Available online at: https://www.undp.org/executive-board/documents-for-sessions/second-regular-session-2022 (Accessed June 11, 2025).
30. Bosomprah S, Tatem AJ, Dotse-Gborgbortsi W, Aboagye P, Matthews Z. Spatial distribution of emergency obstetric and newborn care services in Ghana: using the evidence to plan interventions. Int J Gynaecol Obstet. (2016) 132(1):130–4. doi: 10.1016/j.ijgo.2015.11.004
31. Kyei-Onanjiri M, Carolan-Olah M, Awoonor-Williams JK, McCann TV. Review of emergency obstetric care interventions in health facilities in the upper east region of Ghana: a questionnaire survey. BMC Health Serv Res. (2018) 18(1):184. doi: 10.1186/s12913-018-2980-6
32. Bailey PE, Awoonor-Williams JK, Lebrun V, Keyes E, Chen M, Aboagye P, et al. Referral patterns through the lens of health facility readiness to manage obstetric complications: national facility-based results from Ghana. Reprod Health. (2019) 16(1):19. doi: 10.1186/s12978-019-0684-y
33. Kaselitz E, James KH, Aborigo RA, Agorinya I, Moyer CA, Williams J. Understanding the gap in emergency obstetric and neonatal care in Ghana through the PREventing maternal and neonatal deaths (PREMAND) study. Int J Gynaecol Obstet. (2019) 145(3):343–9. doi: 10.1002/ijgo.12803
34. Dogba M, Fournier P. Human resources and the quality of emergency obstetric care in developing countries: a systematic review of the literature. Hum Resour Health. (2009) 7(1):7. doi: 10.1186/1478-4491-7-7
35. Asamani JA, Ismaila H, Plange A, Ekey VF, Ahmed A-M, Chebere M, et al. The cost of health workforce gaps and inequitable distribution in the Ghana health service: an analysis towards evidence-based health workforce planning and management. Hum Resour Health. (2021) 19(1):43. doi: 10.1186/s12960-021-00590-3
36. World Health Organisation. WHO health workforce support and safeguards list 2023 (2023). Available online at: https://www.who.int/publications-detail-redirect/9789240069787 (Accessed June 8, 2024).
37. WHO-Africa. Stakeholders urged to take action to improve the distribution of doctors in Ghana. WHO | Regional Office for Africa (2022). Available online at: https://www.afro.who.int/countries/ghana/news/stakeholders-urged-take-action-improve-distribution-doctors-ghana (Accessed June 7, 2024).
38. Amalba A, Abantanga FA, Scherpbier AJJA, van Mook WNKA. Working among the rural communities in Ghana—why doctors choose to engage in rural practice. BMC Med Educ. (2018) 18(1):133. doi: 10.1186/s12909-018-1234-y
39. Snow R, Herbst CH, Haddad D, Kwansah J, Antwi J, Ekey VF. The Distribution of Health Workers. Washington, DC: World Bank (2012). p. 49–64. Available online at: http://www.jstor.org/stable/resrep26302.10 (Accessed June 7, 2024).
40. Afari H, Hirschhorn LR, Michaelis A, Barker P, Sodzi-Tettey S. Quality improvement in emergency obstetric referrals: qualitative study of provider perspectives in Assin north district, Ghana. BMJ Open. (2014) 4(5):e005052. doi: 10.1136/bmjopen-2014-005052
41. Daniels AA, Abuosi A. Improving emergency obstetric referral systems in low and middle income countries: a qualitative study in a tertiary health facility in Ghana. BMC Health Serv Res. (2020) 20(1):32. doi: 10.1186/s12913-020-4886-3
42. Gomez PP, Nelson AR, Asiedu A, Addo E, Agbodza D, Allen C, et al. Accelerating newborn survival in Ghana through a low-dose, high-frequency health worker training approach: a cluster randomized trial. BMC Pregnancy Childbirth. (2018) 18:72. doi: 10.1186/s12884-018-1705-5
43. World Health Organisation, UNICEF, UNFPA. WHO/UNICEF/UNFPA joint statement on appropriate management of oxytocin—A key commodity for maternal health. Published online 2019. chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/. Available online at: https://iris.who.int/bitstream/handle/10665/311524/WHO-RHR-19.5-eng.pdf?ua=1 (Accessed March 10, 2024).
44. Aggrey A, Diogo C, Kimera D, Yeager B, Rausher M. Streamlining the oxytocin supply chain to ensure increased access to high quality oxytocin and improved maternal health outcomes in Ghana. Presented at: PPH Community of Practice Meeting. (2020) USAID Global Health Supply Chain Program. Available online at: https://www.jhpiego.org/wp-content/uploads/2020/07/Oxytocin-Supply_Yeager_Aggrey_FINAL.pdf (Accessed June 7, 2024).
45. Stanton C, Koski A, Cofie P, Mirzabagi E, Grady BL, Brooke S. Uterotonic drug quality: an assessment of the potency of injectable uterotonic drugs purchased by simulated clients in three districts in Ghana. BMJ Open. (2012) 2(3):e000431. doi: 10.1136/bmjopen-2011-000431
46. Oguntunde O, Yusuf FM, Nyenwa J, Dauda DS, Salihu A, Sinai I. Emergency transport for obstetric emergencies: integrating community-level demand creation activities for improved access to maternal, newborn, and child health services in northern Nigeria. Int J Womens Health. (2018) 10:773–82. doi: 10.2147/IJWH.S180415
47. Sunguya BF, Ngowi JE, Njiro BJ, Munishi C, Ndumwa HP, Kengia J, et al. Lessons learnt and best practices in scaling up an emergency transportation system to tackle maternal and neonatal mortality: a qualitative study of key stakeholders in Shinyanga, Tanzania. BMJ Open. (2024) 14(2):e073859. doi: 10.1136/bmjopen-2023-073859
48. Wilson A, Hillman S, Rosato M, Skelton J, Costello A, Hussein J, et al. A systematic review and thematic synthesis of qualitative studies on maternal emergency transport in low- and middle-income countries. Int J Gynaecol Obstet. (2013) 122(3):192–201. doi: 10.1016/j.ijgo.2013.03.030
49. Kolié D, Van De Pas R, Codjia L, Zurn P. Increasing the availability of health workers in rural sub-saharan Africa: a scoping review of rural pipeline programmes. Hum Resour Health. (2023) 21(1):20. doi: 10.1186/s12960-023-00801-z
50. Kolstad JR. How to make rural jobs more attractive to health workers. Findings from a discrete choice experiment in Tanzania. Health Econ. (2011) 20(2):196–211. doi: 10.1002/hec.1581
51. Gumede DM, Taylor M, Kvalsvig JD. Engaging future healthcare professionals for rural health services in South Africa: students, graduates and managers perceptions. BMC Health Serv Res. (2021) 21(1):220. doi: 10.1186/s12913-021-06178-w
52. Edson A, Akiko M. How to Recruit and Retain Health Workers in Rural and Remote Areas in Developing Countries (English). Washington, DC: World Bank group (2023). Available online at: http://documents.worldbank.org/curated/en/273821468154769065/How-to-recruit-and-retain-health-workers-in-rural-and-remote-areas-in-developing-countries
53. World Health Organisation. Retention of the Health Workforce in Rural and Remote Areas: A Systematic Review. (2020).
54. Asuming PO, Kanmiki EW, Wong B. Ghana priorities: Maternal and child health. (2020). Available online at: https://copenhagenconsensus.com/publication/ghana-priorities-maternal-and-child-health (Accessed December 22, 2023).
Keywords: EmONC, inequalities, maternal mortality, distribution, policy, Ghana, emergency obstetric and neonatal care
Citation: Senkyire E, Senkyire G, Owusu RT and Asiedua E (2025) A policy in stagnation: addressing inequalities in the distribution of emergency obstetric and neonatal care in Ghana. Front. Glob. Women's Health 6:1614200. doi: 10.3389/fgwh.2025.1614200
Received: 18 April 2025; Accepted: 8 July 2025;
Published: 18 July 2025.
Edited by:
Ana Afonso, NOVA University of Lisbon, PortugalReviewed by:
Alexandra P. Leader, Eastern Virginia Medical School, United StatesYusrawati Yusrawati, Medical Faculty of Andalas University, Indonesia
Sabita Tuladhar, LMU Munich University Hospital, Germany
Copyright: © 2025 Senkyire, Senkyire, Owusu and Asiedua. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ephraim Senkyire, c2Vua3lpcmU4OEBnbWFpbC5jb20=
†These authors share first authorship
 Ephraim Senkyire
Ephraim Senkyire Gloria Senkyire
Gloria Senkyire Rullmann Twi Owusu
Rullmann Twi Owusu Ernestina Asiedua
Ernestina Asiedua