- 1Department of Public Health Sciences, Pennsylvania State University College of Medicine, Hershey, PA, United States
- 2Institute of Energy and the Environment, Pennsylvania State University, University Park, PA, United States
- 3Department of Global Health, University of Washington, Seattle, WA, United States
- 4Department of Epidemiology, School of Public Health, Boston University, Boston, MA, United States
- 5Department of Biobehavioral Health, Pennsylvania State University, College of Health & Human Development, University Park, PA, United States
- 6College of Health and Medical Sciences, Haramaya University, Dire Dawa, Ethiopia
- 7Department of Health Policy Planning and Management, College of Health Sciences, School of Public Health, University of Ghana, Legon, Ghana
- 8Department of Epidemiology and Disease Control, College of Health Science, School of Public Health, University of Ghana, Legon, Ghana
- 9Faculty of Public Health, Department of Health, Behavior and Society, Institute of Health, Jimma University, Jimma, Ethiopia
Introduction: Stillbirth remains a major public health issue in low- and middle-income countries (LMICs). Ghana's 2021 stillbirth rate (21.4 per 1,000 births) exceeds the United Nations Sustainable Development Goal (SDG) target of 12 per 1,000 births by 2030. Unclean household cooking fuels have been associated with adverse pregnancy outcomes, including stillbirth. In Ghana, women conduct about 64% of household cooking, often in poorly ventilated settings with particulate levels above World Health Organization (WHO) guidelines. We assessed the association between household cooking fuel type and stillbirth among Ghanaian women.
Methods: We conducted a cross-sectional analysis using data from the 2022 Ghana Demographic and Health Survey. The sample included 10,654 women aged 15–49 years with ≥1 recorded pregnancy. The primary exposure was household cooking fuel (clean vs. unclean per WHO guidelines). Outcomes were (1) stillbirth, defined as fetal loss at ≥7 months’ gestation, and (2) stillbirth rate per 1,000 total births. Survey-weighted bivariate screening (p < 0.05) identified candidate covariates for inclusion in multivariable, survey-weighted logistic regression models. Adjusted odds ratios (AORs) and 95% confidence intervals (CIs) were reported. Given the cross-sectional design, estimates reflect associations, not causation.
Results: The overall stillbirth rate was 15.85 per 1,000 births. Unclean cooking fuel use was associated with 44% higher odds of stillbirth (AOR: 1.44; 95% CI: 1.05–1.99; p = 0.0258). Other factors associated with higher odds were age ≥30 years (AOR: 2.17; 95% CI: 1.59–2.95; p < 0.001), moderate-to-poor health (AOR: 1.78; 95% CI: 1.39–2.28; p < 0.001), and alcohol consumption (AOR: 1.43; 95% CI: 1.06–1.93; p = 0.0195).
Discussion: In this nationally representative sample, unclean cooking fuel use was associated with increased odds of stillbirth. Expanding access to clean fuels and leveraging antenatal care services for culturally responsive clean-energy counseling may help reduce stillbirth risk. Prospective studies with exposure monitoring are needed to establish temporality.
1 Introduction
Stillbirth remains a major public health concern globally, particularly in low- and middle-income countries (LMICs) where the burden of fetal loss and early neonatal death is disproportionately high (1–5). Although the global stillbirth rate declined from 21.4 to 13.9 per 1,000 total births between 2000 and 2019, this 35% reduction has lagged behind more substantial declines observed in maternal and under-five mortality indicators during the same period (1, 6). Stillbirth prevention has historically received less attention than other mortality indicators in national health agendas and global reporting frameworks (7, 8). Sustainable Development Goal 3.2 (SDG 3.2) calls for reducing stillbirths to 12 per 1,000 total births by 2030; many LMICs remain off track to meet this target (2, 9, 10). Sub-Saharan Africa and South Asia collectively account for 84% of all stillbirths globally (11), and West and Central Africa experience rates up to eight times higher than those in Western Europe (6). In Ghana, the stillbirth rate remains high, with recent estimates of 21.4 per 1,000 total births in 2021 (12, 13).
Many stillbirths are preventable. Recent efforts to reduce them have focused primarily on clinical interventions, such as skilled birth attendance, improved antenatal care, and emergency obstetric services (14–17). In parallel, environmental exposures are increasingly recognized as potential contributors, with numerous studies reporting associations (18, 19). One emerging area of interest is household cooking fuels and their relation to maternal and neonatal health outcomes (18, 19).
Unclean cooking fuels —such as firewood, charcoal, animal dung, and crop residues— are widely used in Ghana, particularly in rural and low-income households (20–22). Incomplete combustion of these fuels during cooking produces high concentrations of indoor air pollutants, like fine particulate matter (PM2.5), carbon monoxide (CO), and nitrogen oxides (NOx), often at levels exceeding World Health Organization (WHO) safety guidelines (18, 22–26). Repeated exposure to these particulate emissions has been associated with hypertensive disorders in pregnancy, placental dysfunction, and fetal hypoxia— conditions that are established risk factors for stillbirth (18, 22–26) (Figure 1).
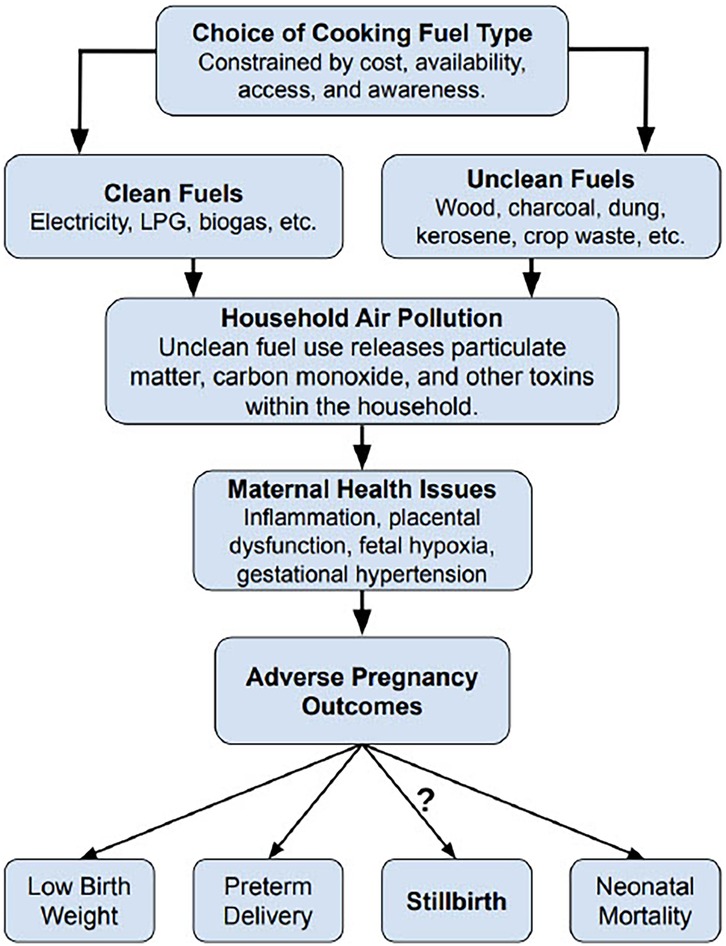
Figure 1. Conceptual framework linking cooking fuel type to stillbirth in Ghana. Fuel choice —often shaped by socioeconomic and contextual factors— may be associated with use of unclean cooking fuels. Combustion of these fuels emits harmful pollutants, notably fine particulate matter (PM2.5) and carbon monoxide (CO). PM2.5 consists of inhalable particles ≤2.5 μm that can reach the alveoli and enter the bloodstream. CO is a colorless, odorless gas that binds hemoglobin and can reduce oxygen delivery to the placenta and fetus. These pollutants contribute to household air pollution and prolonged exposure has been associated with adverse pregnancy outcomes. Stillbirth remains an underexplored outcome along this hypothesized pathway in Ghana.
Although Ghana has launched national programs to promote clean cooking technologies [e.g., liquified petroleum gas (LPG) stoves] (27), adoption remains limited because of structural and cultural barriers (21). Over 80% of Ghanaian households still rely on traditional solid fuels; women perform nearly 64% of the household cooking, often in poorly ventilated settings (20, 21). Barriers to clean fuel adoption include high up-front costs for LPG stoves, inconsistent fuel supply chains, limited public awareness, and cultural preferences for traditional cooking methods (21, 28–30).
While the health consequences of household air pollution from unclean fuels are well documented for outcomes such as respiratory illness, low birth weight, and under-five mortality, few studies have examined stillbirth as a primary outcome—even fewer within Ghana (22, 23, 31). Much of the available literature on cooking fuel and stillbirth draws from older or regional datasets, limiting generalizability to Ghana's evolving social, economic, and policy landscape (32). As stillbirth prevention increasingly becomes a policy priority in Ghana, understanding the role of modifiable environmental exposures like household cooking fuel is critical (27, 32, 33).
To address this identified gap, the current study analyzed newly released data from the 2022 Ghana Demographic and Health Survey (DHS) to assess whether unclean cooking fuel use was independently associated with higher odds of stillbirth among Ghanaian women. Given Ghana's rapid development alongside persistent health inequities, these findings may inform national public health strategies and broader global efforts to reduce preventable fetal deaths. By centering environmental exposures within the broader maternal-health agenda, this study underscores the importance of interdisciplinary, multisectoral approaches to stillbirth prevention.
2 Materials and methods
2.1 Participants
This study used individual-level data from the 2022 Ghana DHS, a cross-sectional, nationally representative survey that collects information on demographic, maternal, and child health indicators (34). The survey employed a stratified two-stage sampling design to select 18,450 households across 618 clusters in Ghana, yielding interviews with 15,014 women aged 15–49 years. Our analytic sample comprised de facto Ghanaian women of reproductive age in the Individual Recode file (GHIR8BFL.SAV). To focus the analysis on pregnancy-related outcomes, we further restricted the sample to women with at ≥1 recorded pregnancy, resulting in a final weighted sample of 10,654 women. Ethical approval for the 2022 Ghana DHS was obtained by the Ghana Health Service Ethical Review Committee and the Institutional Review Board of Inner-City Fund (ICF) International. Written informed consent was obtained from all participants at the time of data collection (34).
2.2 Stillbirth definition(s)
The primary outcome was stillbirth, defined as fetal loss at ≥7 months (≥28 weeks) of gestation, consistent with the WHO definition (35). In the DHS Women's Questionnaire, pregnancy duration was recorded in completed months based on maternal recall (34). We derived a binary variable indicating whether a woman had ever experienced a stillbirth: coded as “1” if any reported pregnancy lasted ≥7 months and resulted in a fetus classified as “born dead,” and “0” otherwise. This outcome represents the prevalence of stillbirth among all women in the sample. We also calculated each woman's stillbirth rate, defined as the number of stillbirths divided by the sum of live births and stillbirths, scaled per 1,000 births. Data were available for up to 20 recorded pregnancies per woman.
2.3 Type of cooking fuel
The primary exposure was the type of household cooking fuel. In the 2022 Ghana DHS Household Questionnaire, the respondent is asked a single, mutually exclusive question: “What type of fuel does your household mainly use for cooking?” (34). Following WHO guidance, responses were recoded to a binary indicator for cooking fuel type — clean vs. unclean (36). Clean fuels included electricity, LPG, natural gas, alcohol (i.e., ethanol), and biogas. Unclean fuels (e.g., solid fuels) included kerosene, coal or lignite, charcoal, wood, straw, shrubs, grass, agricultural crop waste, processed biomass pellets, garbage, plastic, sawdust, and animal dung.
Women missing data on their primary cooking fuel type or with unclassifiable fuel types (n = 200; 1.9% of total weighted sample) were coded as missing. To assess differential missingness, design-adjusted chi-squared tests were used. Missingness was not significantly associated with place of residence, educational status, wealth, drinking water source, radio use, age at first birth, contraceptive use, body mass index (BMI), self-reported health status, alcohol consumption, or sexually transmitted infection (STI) history (all p > 0.05). Missing cooking fuel type data were slightly more common among younger women (p < 0.001) and among those who had ever experienced a stillbirth (p < 0.01). Complete-case estimates are presented; these limitations are noted in the Discussion.
2.4 Other variables
Sociodemographic covariates included maternal age (15–29 years vs. ≥30 years), place of residence (urban vs. rural), education status (no schooling to secondary vs. higher education), and the DHS wealth index, a composite indicator reflecting household ownership of assets and access to amenities (e.g., poor, middle, rich).
Household-level covariates included the primary source of drinking water, classified as improved (e.g., piped water, covered boreholes, protected wells, rainwater collection, bottled water) or unimproved (e.g., unprotected wells, surface water sources such as rivers and lakes). Classifications were consistent with WHO and United Nations Children's Fund (WHO/UNICEF) Joint Monitoring Program definitions (37, 38). Exposure to media was approximated by radio usage, classified dichotomously (listens vs. does not listen to the radio).
Maternal characteristics comprised age at first birth (<15–24 years vs. ≥25 years), current contraceptive use (yes vs. no), and BMI (kg/m2). Because BMI had substantial missingness (49.3%), we examined correlates of missingness with design-adjusted chi-squared tests. BMI missingness was not associated with the primary exposure (cooking fuel type, p = 0.81) and outcome (ever-stillbirth, p = 0.34), nor with maternal age, education, residence, self-reported health status, alcohol use, or other household-level factors (all p > 0.05). Although associations were noted with wealth index (p = 0.04; <4 percentage point difference across groups) and contraceptive use (p = 0.001; < 4 percentage point difference across groups), the absence of strong systematic patterns suggested data were plausibly missing at random. Therefore, missing BMI values were imputed using multiple imputation with predictive mean matching (m = 5) via the “mice” package in R. Variables included as predictors in the BMI imputation model were maternal age, education, wealth index, parity, source of drinking water, smoking status, and the survey sample weight to account for complex survey design. Imputed BMI was used in descriptive summaries; BMI was not included in the final multivariable model.
Smoking status was based on women's current use of tobacco products and categorized as “smokes” (e.g., currently uses tobacco) or “does not smoke” (e.g., no current tobacco use). Alcohol consumption was measured based on the respondents' reported frequency of alcohol use in the past month. This variable was dichotomized into two categories: “consumes alcohol,” which included women who reported drinking alcohol at any frequency within the past month, vs. “does not drink.” Self-reported health status reflected respondents' personal assessment of their overall health. Women rated their health status using DHS categories: “very good,” “good,” “moderate,” “bad,” or “very bad.” These were subsequently collapsed into two groups for analysis, specifically “good” (including “very good” and “good”) and “moderate-to-bad” (including “moderate,” “bad,” and “very bad”). Presence of any STI in the past year was self-reported (e.g., “yes,” “no,” or “don't know,” with the latter treated as missing).
Maternal healthcare variables —number of antenatal care (ANC) visits for the most recent pregnancy, place of delivery (home, public facility, private/other), and whether the woman had a cesarean section— were summarized descriptively only. In the DHS, these items are collected only for pregnancies within 5 years preceding the survey; consequently, they were missing for >50% of our analytic sample. Because this missingness is determined by survey design and depends on the recency of pregnancies, it is not missing at random and it is directly related to our outcome (e.g., ever-stillbirth, stillbirth rate). Multiple imputation was therefore not inappropriate. To avoid selection bias from conditioning on the five-year pregnancy subcohort, we excluded these variables from bivariate screening and multivariable models.
To ensure model reliability and sufficient statistical power, all candidate covariates were assessed for minimum sample sizes and event counts before the bivariate analyses. Variables with fewer than 100 observations or less than 10% representation in the unweighted sample were collapsed into broader categories. Only covariates that met both theoretical relevance as potential confounders and minimum case count thresholds (≥100 observations and ≥10 stillbirth events) were carried forward into the survey-weighted bivariate analyses. Statistically significant covariates (p < 0.05) were retained for inclusion in the multivariable model. Four variables met these criteria and were retained: maternal age (15–29 years vs. ≥30 years), cooking fuel type (clean vs. unclean), self-reported health status (good vs. moderate-to-poor), and alcohol use (no use vs. current use). Final model diagnostics confirmed no convergence issues or inflated standard errors.
2.5 Statistical analysis
The DHS employs a complex sampling design involving stratification, clustering, and sampling weights (34). To account for this design in our analyses, survey weights were normalized, and clusters and strata were incorporated into a survey design object using the survey package in R Studio. All estimates were weighted and design-adjusted.
Weighted descriptive statistics were calculated for the primary exposure and covariates (Table 1). Univariable logistic regression estimated crude associations between each covariate and the outcome of ever-stillbirth. All models were weighted and specified using the svyglm() function with a quasibinomial family. Weighted odds ratios (ORs) and 95% confidence intervals (CIs) were reported.
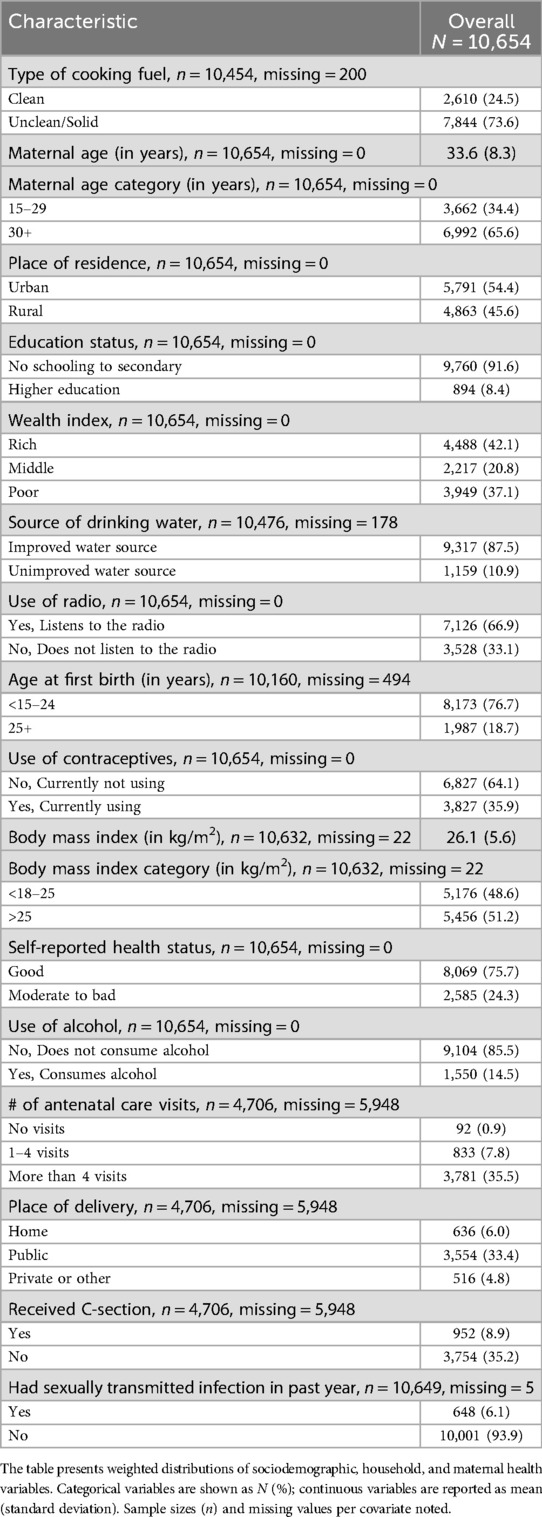
Table 1. Weighted sample characteristics of women aged 15–49 with background variables (N = 10,654).
Bivariate analyses were conducted to examine unadjusted associations between stillbirth and covariates hypothesized to be linked to both cooking fuel use and stillbirth (Table 2). For each covariate level, two outcome measures were reported: (1) the weighted prevalence of ever-stillbirth, and (2) the stillbirth rate per 1,000 total births (Table 2). The first metric reflects the weighted proportion of women who had ever experienced a stillbirth within each level of the covariate. Meanwhile, the second metric captures the intensity of stillbirths relative to the total number of pregnancies. We used design-adjusted chi-square tests to assess whether stillbirth significantly differed across covariate levels. Variables with a p < 0.05 were retained for inclusion in the final multivariable logistic regression model.
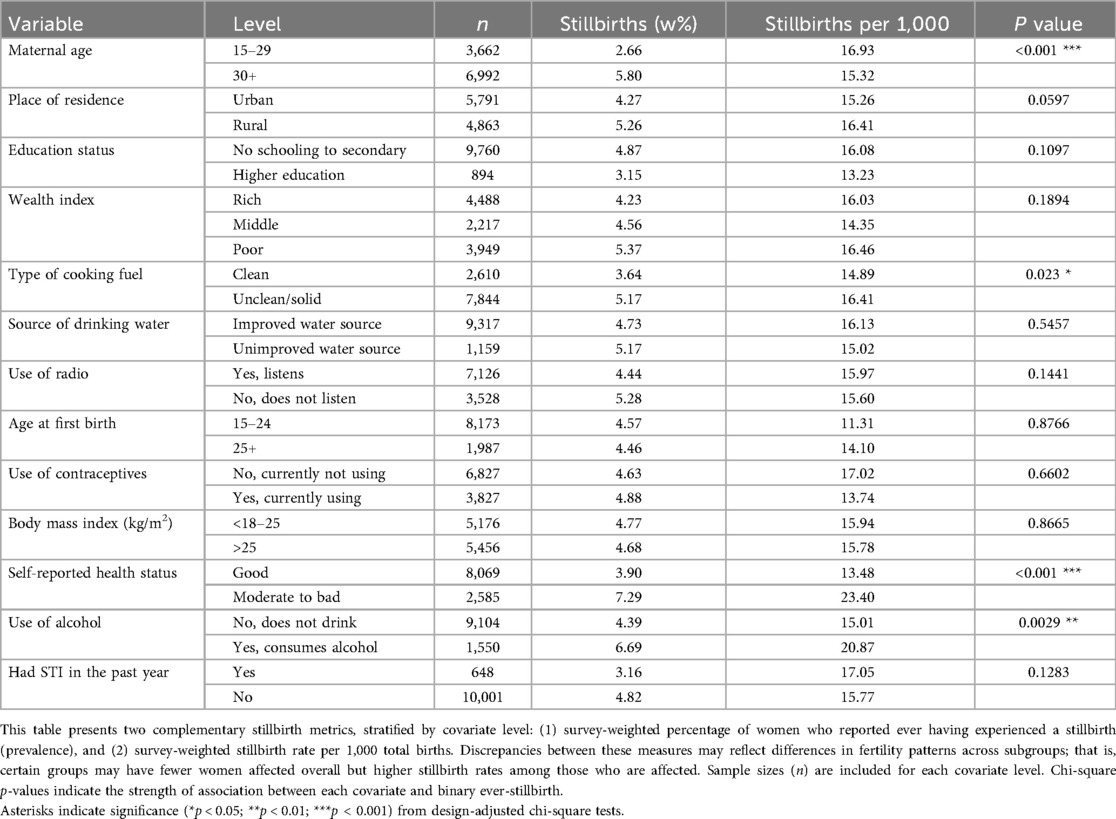
Table 2. Weighted bivariate analysis of stillbirth outcomes stratified by covariates among Ghanaian women aged 15–49.
A multivariable logistic regression model was fit to assess independent associations with stillbirth using the svyglm() function; a quasibinomial distribution was specified (Table 3). Adjusted odds ratios (AORs) and corresponding 95% confidence intervals (CIs) were obtained by exponentiating model coefficients and standard errors. Statistical significance of covariates was assessed using design-adjusted chi-square tests.
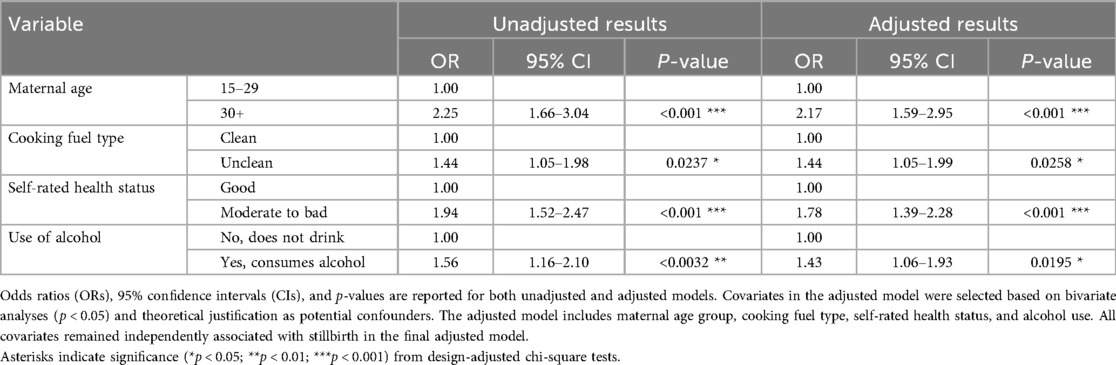
Table 3. Unadjusted and adjusted logistic regression model estimates for risk of stillbirth by sample characteristics.
3 Results
3.1 Sample characteristics
Table 1 presents the weighted demographic, household, and maternal characteristics for 10,654 Ghanaian women aged 15–49 years. The average maternal age was 33.6 years (SD 8.3), with nearly two-thirds of women (65.6%) aged 30 or older. Over half resided in urban areas (54.4%), and most had completed up to a secondary-level education (91.6%). Approximately one-third of participants (37.1%) were in the poorest wealth tertile (Table 1). Most women (73.6%) reported using unclean or solid fuels as their primary cooking fuel; 24.5% used clean fuels. Most respondents lived in households with access to improved drinking water sources (87.5%).
Media exposure was moderate, with 66.9% reporting that they listened to the radio. Nearly four in five women (76.7%) had their first birth between the ages of 15 and 24. Mean BMI was 26.1 kg/m2 (SD 5.6), with roughly half of the sample (51.2%) having a BMI over 25 kg/m2 (Table 1). Regarding other health variables, 14.5% reported any alcohol use in the past month, 35.9% reported current contraceptive use, and 24.3% rated their health as moderate to poor. A small proportion (6.1%) reported having a sexually transmitted infection (STI) in the past year (Table 1).
Among women with available maternal healthcare data (n = 4,706), 35.5% reported more than four ANC visits during their most recent pregnancy (Table 1). Most deliveries occurred in public health facilities (33.4%), while home births (6.0%) and births in private or other settings (4.8%) were less common. Cesarean section deliveries were reported by 8.9% (Table 1).
3.2 Bivariate associations with stillbirth
Across the weighted sample, the stillbirth rate was 15.85 per 1,000 births (Figure 2). Table 2 presents both the weighted prevalence of ever experiencing a stillbirth and the stillbirth rate per 1,000 births, stratified by covariate levels. Stillbirth outcomes differed by maternal age, cooking fuel type, self-reported health status, and alcohol use.
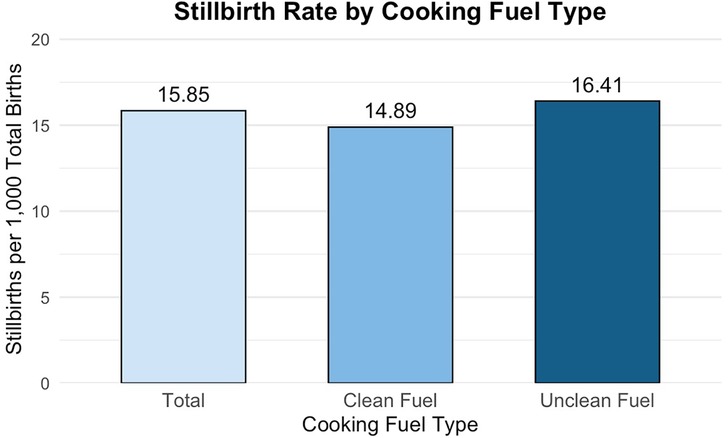
Figure 2. Stillbirths per 1,000 total births by cooking fuel type among Ghanaian women. This figure displays stillbirth rates per 1,000 total births for the overall sample and stratified by cooking fuel type among Ghanaian women aged 15–49 years. Estimates were derived using survey-weighted means to reflect the nationally representative sample. While overall stillbirth rate was 15.85 stillbirths per 1,000 total births, women in households using unclean fuels experienced a significantly higher stillbirth rate (16.41 stillbirths per 1,000 total births) compared to those using clean fuels (14.89 stillbirths per 1,000 total births).
Use of unclean cooking fuels was associated with a higher lifetime prevalence of ever having experienced a stillbirth (5.17% vs. 3.64% among women using clean fuels; p = 0.023) and a higher stillbirth rate (16.41 vs. 14.89 per 1,000 births).
Age ≥30 years was associated with a higher prevalence of ever having experienced a stillbirth (5.80% vs. 2.66% among women aged 15–29 years; p < 0.001). By contrast, the stillbirth rate per 1,000 total births was slightly lower among women aged ≥30 years (15.32 vs. 16.93 per 1,000 births among women aged 15–29 years). This pattern is consistent with higher average parity among older women aged ≥30 years (mean = 4.2 lifetime pregnancies) compared to younger women aged 15–29 years (mean = 1.7 lifetime pregnancies).
Self-rated health was associated with stillbirth outcomes. Women who reported “moderate-to-poor” health had a 7.29% ever-stillbirth prevalence and a stillbirth rate of 23.40 per 1,000 births, compared with 3.90% and 13.48 per 1,000 births among those reporting good health (p < 0.001). Alcohol use in the past month was associated with higher ever-stillbirth prevalence (6.69% vs. 4.39% among women who did not consume; p = 0.003) and a higher stillbirth rate (20.87 vs. 15.01 stillbirths per 1,000 births among women who did not consume).
3.3 Multivariable logistic regression
Table 3 and Figure 3 present univariable and adjusted multivariable logistic regression estimates for variables retained after bivariate screening. After adjustment, unclean (vs. clean) cooking fuel use was associated with 44% higher odds of ever having experienced a stillbirth (AOR=1.44; 95% CI: 1.05–1.99; p = 0.0258). Maternal age ≥30 years (vs. 15–29 years) was associated with more than twice the odds of ever having experienced a stillbirth (AOR=2.17; 95% CI: 1.59–2.95; p < 0.001). Moderate-to-poor self-reported health (vs. good self-reported health) associated with a 78% higher odds of stillbirth (AOR=1.78; 95% CI: 1.39–2.28; p < 0.001). Any alcohol use in the past month (vs. none) was associated with a 43% higher odds of ever having experienced a stillbirth (AOR=1.43; 95% CI: 1.06–1.93; p = 0.0195).
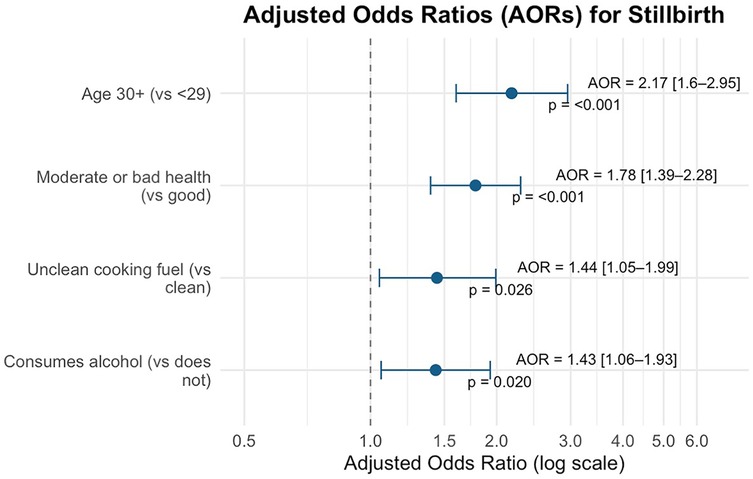
Figure 3. Forest plot of adjusted odds ratios (AORs) for stillbirth. This forest plot presents adjusted odds ratios (AORs) and 95% confidence intervals (CIs) from the final survey-weighted multivariable logistic regression model examining factors associated with ever experiencing a stillbirth. All covariates shown were statistically significant at p < 0.05, and had CIs that did not contain the null value. AORs greater than 1 indicate increased odds of stillbirth, while the vertical dashed line marks the null value (AOR=1), indicating no association.
4 Discussion
This study contributes new evidence to the growing literature on environmental exposures and maternal health in Ghana by examining the association between cooking fuel type and stillbirth. Previous research has linked household air pollution from unclean cooking fuel to adverse pregnancy outcomes globally (18, 25, 26, 31); yet, few studies have explored the relationship between cooking fuel type and stillbirth at the population level in Ghana using recent, nationally representative data. We observed that unclean cooking fuel use was associated with 44% higher adjusted odds of ever having experienced a stillbirth (AOR 1.44, 95% CI: 1.05–1.99; p = 0.0258). This finding aligns with global and regional evidence associating unclean cooking fuels with adverse pregnancy outcomes (32), as well as with a recent meta-analysis showing a 38% increase in stillbirth odds (39). The stillbirth rate observed in our sample (15.85 per 1,000 total births) remains above the SDG 3.2 target of 12 per 1,000 total births (12). Our results underscore the need to address unclean fuel use as a key, yet under-recognized, contributor to preventable stillbirths.
4.1 Biological pathways linking cooking fuel use to stillbirth
The biological mechanisms linking unclean cooking fuels to stillbirth are well-supported by experimental and epidemiological evidence (22, 24, 32, 40–42). Solid fuels such as firewood, charcoal, and crop residues, when burned in poorly ventilated settings, release high concentrations of harmful pollutants. These pollutants—including fine particulate matter (PM2.5) and carbon monoxide (CO)—are byproducts of incomplete combustion (22, 25, 26, 43). Such emissions may have direct toxic effects on both maternal and fetal physiology (23, 32, 42).
Inhaled particulate matter can penetrate deep into the lungs, enter the maternal bloodstream, and is thought to trigger systemic inflammation, oxidative stress, and cellular damage to the placenta (24, 44–46). These biological insults may compromise placental function and are associated with fetal growth restriction and intrauterine death (18, 47). Simultaneously, CO binds with high affinity to maternal hemoglobin, potentially reducing oxygen delivery to the placenta and fetus (45, 46). Chronic CO exposure can induce fetal hypoxia and acidemia — conditions strongly associated with stillbirth (26, 46).
Although direct measures of household air pollution (e.g., PM2.5 concentration or indoor CO levels) were not available in this dataset, the observed associations between unclean fuel use and stillbirth are consistent with these well-established mechanistic pathways.
4.2 Intersecting maternal risk factors and their implications for stillbirth
Beyond fuel use, several maternal characteristics were independently associated with stillbirth in Ghana, including maternal age ≥30 years, poor self-reported health, and alcohol use. Maternal age ≥30 years was associated with more than twice the odds of ever having experienced a stillbirth (AOR=2.17; 95% CI: 1.59–2.95; p < 0.001), consistent with broader evidence linking older mothers to increased obstetric risks (48–50). In bivariate analyses, older women (≥30 years) showed a higher lifetime prevalence of ever-stillbirth yet a slightly lower stillbirth rate per 1,000 total births, compared to younger women (15–29 years). This apparent discrepancy is consistent with the outcome metric definitions, whereby prevalence reflects whether a woman has ever experienced a stillbirth across her reproductive lifespan. In contrast, the rate is standardized by the number of births in the denominator. In our sample, women aged ≥30 years had a higher mean parity (4.2 vs. 1.7 births), which increases the denominator and can yield a lower per 1,000 stillbirth rate even when a greater share of women have ever experienced a stillbirth.
Furthermore, the biological plausibility of higher lifetime odds of ever having experienced a stillbirth at older ages is supported, as older women face increased cumulative placental stress, chromosomal abnormalities, hypertensive disorders, along with other obstetric complications over a longer reproductive lifespan (2, 48–50). These patterns may reflect age-related physiologic changes and a greater burden of subclinical placental insufficiency that could interact with household air pollution exposures (51, 52). Longer duration of solid fuel use among older women may also be associated with markers of placental dysfunction and adverse pregnancy outcomes (42, 52). Conversely, the slightly higher per-1,000 stillbirth rate observed among younger women may be consistent with features of biological immaturity, limited socioeconomic resources, reduced access to antenatal care, and less engagement in preventive health behaviors—each of which could plausibly elevate the stillbirth risk in this subgroup (53–56). Because lower socioeconomic status (SES) is associated with both younger maternal age and reliance on solid fuels, the higher stillbirth rate observed among younger women may partly reflect confounding between age, SES, and fuel type, complicating isolation of an age-specific effect independent of fuel exposure (21, 57, 58).
Women who perceived their health as moderate-to-poor were associated with a higher odds of ever having experienced a stillbirth (AOR = 1.78; 95% CI: 1.39–2.28; p < 0.001) compared to those reporting good health. While subjective, self-rated health is widely recognized as a valid proxy for overall well-being and may reflect underlying chronic conditions, nutritional status, or psychosocial stress (59, 60). In this context, women with poorer self-reported health may have less physiological reserve to tolerate insults like hypoxia or inflammation resulting from household air pollution (59–61). It is also plausible that women reporting moderate-to-poor health may have higher burdens of chronic conditions like hypertension, anemia, or respiratory disease that, together with unclean fuel use, compound the risk of stillbirth (25). These environmental exposures—often invisible in clinical assessments—could convey a broader physiological burden that increases the risk of poor pregnancy outcomes.
Any alcohol use in the past month was associated with a higher odds of ever having experienced a stillbirth (AOR = 1.43; 95% CI: 1.06–1.93; p = 0.0195). This finding is consistent with prior research demonstrating that maternal alcohol use elevates stillbirth risk via multiple physiological pathways (62, 63). Alcohol can directly injure the fetus and placenta, and heavy prenatal alcohol use has been linked to fetal growth restriction, placental abruption, and fetal death (63). Combined prenatal drinking and smoking has also been shown to increase the odds of stillbirth nearly threefold, underscoring how alcohol may amplify the harm of smoke-borne toxins common to both tobacco and biomass combustion (64, 65). Beyond its physiological impacts, alcohol use may serve as a behavioral marker of reduced engagement in health-promoting practices, such as transitions to cleaner cooking methods (66). That is, alcohol use could compete with cleaner fuel adoption, either directly through financial diversion or indirectly through reduced maternal prioritization of environmental health (66, 67).
4.3 Integrating environmental risk screening into maternal health services
Our results highlight that stillbirth in Ghana is a multifactorial public health issue, arising from an interplay between environmental exposures and maternal characteristics. Traditionally, antenatal screening and prenatal care protocols in Ghana focus solely on medical and obstetric risk factors like diabetes, hypertension, or prior obstetric history (68). Our findings suggest that questions about a woman's household environment —specifically, her cooking fuel type and kitchen ventilation practices— may help to integrate environmental exposures into a more holistic approach to prenatal care. For example, it may prove beneficial for maternal healthcare providers to routinely ask pregnant women about their primary cooking fuel type and where they cook as part of the intake history. This type of screening may help to flag women at higher risk of stillbirth due to household air pollution.
In resource-limited communities, counseling delivered by community health workers (CHW), especially women from the communities they serve, may be another culturally grounded way to promote healthier behaviors around both fuel use and pregnancy health. For instance, if a pregnant woman is found to be cooking indoors with solid fuels, health workers can counsel her on strategies to potentially mitigate smoke exposure, such as improving airflow, keeping children away from the cooking area, or switching to a cleaner fuel if possible. However, when cleaner fuels are unaffordable or unavailable, ANC and CHW programs may promote cooking outdoors, including in covered outdoor shelters or shared community cooking spaces. This low-cost approach is quick to implement; yet, feasibility may be limited by several barriers. For instance, prolonged seasonal rains could render open cooking areas unusable (69, 70), and safety and privacy concerns might deter women from cooking outside after dark (71–73). Ingrained cooking traditions that favor indoor solid fuel use may further limit willingness to shift cooking outdoors (72, 74). Programs should assess these barriers locally and co-design solutions to these barriers in partnership with women's groups and community leaders.
In areas where clean fuel programs or subsidies do exist, antenatal clinics might serve as a point of referral —connecting expectant mothers with community initiatives that provide improved cookstoves, LPG cylinder exchanges, or solar cookers. Integrating such environmental health checks into maternal services would require some training and awareness-raising among healthcare staff, but would align with a more holistic approach to female reproductive care. Ghanaian women, who overwhelmingly bear the burden of household cooking, are disproportionately exposed to the harms of indoor air pollution (29). Therefore, protecting pregnant women from harmful environmental exposures in the home should be seen as part of the continuum of prenatal care, just as important as providing iron supplements or blood pressure monitoring (75). Any intervention aiming to reduce stillbirth should therefore be attuned to the lived realities of women's household cooking roles.
4.4 Future research directions
While this analysis leveraged nationally representative survey data, it relied on proxy measures (e.g., cooking fuel type) to estimate exposure to household air pollution. To clarify temporality and evaluate potential causal pathways, future prospective longitudinal studies in Ghana should incorporate direct environmental measurements. One priority is the in-home monitoring of indoor air quality in Ghanaian households — for instance, using portable monitoring devices to measure PM₂.₅ and CO levels during cooking hours. Such exposure measurements would enable dose-response analyses to determine how much reduction in indoor air pollution is needed to lower stillbirth risk meaningfully. It might also confirm whether unclean fuel use is a valid proxy for indoor air pollution, especially considering factors like stove efficiency and household ventilation.
The role of ventilation and housing design in modifying exposure also warrants closer investigation. Even when cleaner fuels are not immediately available, interventions like cooking outdoors or installing chimneys can drastically reduce indoor pollutant concentrations (41). Studies that document kitchen characteristics (i.e., outdoor vs. indoor kitchen, presence of windows, use of ventilation hoods) could assess how these features interact with cooking fuel type to influence stillbirth outcomes. Such investigations may guide interim risk reduction strategies, especially given that policy implementation can take up to 20 years to enact (76). Simple architectural modifications in homes can substantially lower smoke accumulation and toxin exposure (41). Urban planners and architects could incorporate ventilation considerations into housing programs, ensuring that low-cost homes have provisions for safe cooking. Similarly, development projects might include community cooking centers that serve multiple households.
In parallel, implementation research is needed to address sociocultural and structural barriers to clean fuel adoption. Although clean cooking technologies exist, uptake remains low because those at highest risk of household air pollution exposure cannot access or afford these newer appliances (77, 78). Additionally, cultural preferences, perceived safety concerns, and cost-related obstacles all contribute to continued reliance on solid fuels (72–74, 77, 79). For example, some households report that traditional foods taste better when cooked over open flames or that LPG refills are expensive and difficult to access (32).
Future research should delve into these barriers by engaging with the community through interviews, focus groups, and behavioral trials to design interventions that are culturally acceptable and address practical constraints. At the forefront of these efforts, local cooking habits should be readily accommodated, and cooking devices must be adapted in a user-friendly, culturally sensitive way. Involving women in Ghana in this process is crucial to ensure that the technology is adopted and yields its intended benefits. This could include exploring micro-financing schemes for LPG purchases or community education to dispel myths about new stove technologies. Multidisciplinary research —combining environmental science, public health, and social science— is needed to translate these epidemiological findings into effective stillbirth prevention strategies on the ground.
4.5 Strengths and limitations
By drawing on the 2022 Ghana Demographic and Health Survey, we analyzed a large, nationally representative sample of reproductive-aged women, yielding stillbirth estimates that carry direct relevance for current policy discussions. Our survey-weighted analytic framework accounted for clustering and stratification. Further, multiple imputation for missing BMI values mitigated potential selection bias. All covariates were selected a priori based on biological and epidemiological relevance, which reinforces the internal validity of our adjusted estimates.
However, several limitations must be acknowledged. First, the cross-sectional design precludes establishing temporality; findings indicate associations rather than causal effects, and reverse causation cannot be excluded.
With regard to our primary outcome of ever-stillbirth, it is important to note that stillbirth classification in the DHS relies on maternal recall of gestational age (in months) and birth outcome (34). This introduces the risk of (a) misclassification around the ≥7-month threshold (e.g., late miscarriages recorded as stillbirths or vice versa) and (b) confusion between stillbirths and early neonatal deaths. These issues characteristic of population survey data are well documented (1, 7). In addition, under-reporting of stillbirths —potentially due to stigma or grief— may bias actual ever-stillbirth prevalence downward; however, the direction of bias is uncertain until further studies are conducted.
Another limitation is with respect to exposure measurement. We used the household's primary type of cooking fuel as a proxy for household air pollution. The DHS does not record in-home PM₂.₅ and CO levels, stove efficiency, indoor cooking layout, or kitchen ventilation practices. These unmeasured covariates can critically moderate a woman's actual exposure to indoor air pollutants. For example, it is possible that some women who use LPG may also burn charcoal at times, or some women who use solid fuels may cook outdoors or have well-ventilated kitchens. This introduces the potential for exposure misclassification, potentially diluting the association and pushing estimates toward the null. In addition, the primary fuel type was missing for <2% of respondents, with slightly higher missingness among younger women and among those reporting a prior stillbirth. Although the proportion is small, our complete-case approach may introduce minor selection bias.
This study design also makes our findings susceptible to residual and unmeasured confounding. That is, the DHS does not capture several clinically important covariates, such as maternal anemia, hypertensive disorders in pregnancy, and gestational diabetes. Omission of these factors could lead to residual confounding and may bias estimates toward or away from the null. Future studies should measure these variables directly.
Other key covariates included in our final multivariable model, like alcohol intake and self-rated health, were self-reported and may be subject to social-desirability bias.
The exclusion of several important maternal healthcare variables is another limitation. The number of antenatal care visits, place of delivery, and caesarean section were missing for >50% of our analytic sample because the DHS collects them only for pregnancies within the five years preceding the survey. Because this missingness is not at random, incorporating these variables would have required restricting the analysis to pregnancies within the five years preceding the survey. That restriction would both reduce our sample size and alter our outcome from “ever-stillbirth” over the life course to stillbirths occurring within a five-year window prior to the survey. Pregnancy recency is also correlated with maternal age, parity, and health-seeking behavior; conditioning on it could introduce selection bias and yield estimates that are not comparable with those based on lifetime reproductive history. Accordingly, we did not perform a restricted-sample sensitivity analysis. Instead, we summarized these variables descriptively and excluded them from bivariate screening and multivariable models, acknowledging that their omission may introduce omitted-variable bias that could either over- or under-estimate the association between fuel type and stillbirth.
Finally, while our findings are broadly consistent with work from other LMICs, cultural and infrastructural differences may limit generalizability beyond Ghana. Due to these limitations, we recommend that policy makers interpret these estimates with caution.
5 Conclusion
In conclusion, this study provides evidence that unclean cooking fuel use may be associated with stillbirth in Ghana, even after adjusting for key covariates. While Ghana has made significant headway in reducing stillbirth, further reductions may be supported by strategies that reduce household air pollution —alongside improvements in clinical care. Integrating environmental risk checks within antenatal services may be a pragmatic step while stronger evidence accumulates. Because these data cannot establish temporality or causation, prospective longitudinal studies are needed. Those studies should include direct household air pollution measurements (e.g., PM₂.₅, CO) and richer clinical and environmental covariates to clarify pathways and to estimate the potential impact of clean-cooking interventions on stillbirths in Ghana.
Data availability statement
The Demographic and Health Survey datasets analyzed in this study are publicly available from The DHS Program (https://www.dhsprogram.com) upon registration and approval. The 2022 Ghana IR (women's) file (filename: GHIR8BFL) can be requested from the DHS Program microdata repository. Additionally, the analysis code used in this study is available from the corresponding author upon reasonable request. No DHS data can be shared without prior approval and access is via The DHS Program as described above.
Ethics statement
The studies involving humans were approved by ICF Institutional Review Board, Ghana Health Service Ethical Review Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
KW: Conceptualization, Writing – original draft, Visualization, Methodology, Formal analysis, Writing – review & editing, Data curation. KS: Writing – review & editing, Validation. GH: Writing – review & editing, Validation. HS: Writing – review & editing. KR: Writing – review & editing, Validation. LB: Writing – review & editing. EK: Writing – review & editing. CN: Writing – review & editing. AG: Writing – review & editing. AY: Formal analysis, Validation, Data curation, Supervision, Writing – review & editing, Conceptualization, Methodology, Project administration, Resources, Investigation, Visualization, Funding acquisition, Software.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors thank the Ghana Statistical Service, USAID DHS program, and ICF International for granting access to the 2022 Ghana DHS dataset. We are grateful to the field staff and survey respondents whose participation made this research possible. Indirect support was provided through the 2024 Institute of Energy and the Environment (IEE) Seed Grant Program, awarded by Penn State Health IEE department [IO Number: 46000000820]. This grant provided salary support for a research assistant (KPW) who helped with manuscript preparation only. The funder had no role in study design, data collection, analysis, decision to submit, or writing of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lawn JE, Blencowe H, Waiswa P, Amouzou A, Mathers C, Hogan D, et al. Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet. (2016) 387(10018):587–603. doi: 10.1016/S0140-6736(15)00837-5
2. Lawn JE, Blencowe H, Oza S, You D, Lee AC, Waiswa P, et al. Every newborn: progress, priorities, and potential beyond survival. Lancet. (2014) 384(9938):189–205. doi: 10.1016/S0140-6736(14)60496-7
3. Lawn JE, Gravett MG, Nunes TM, Rubens CE, Stanton C, the GAPPS Review Group. Global report on preterm birth and stillbirth (1 of 7): definitions, description of the burden and opportunities to improve data. BMC Pregnancy Childbirth. (2010) 10(1):S1. doi: 10.1186/1471-2393-10-S1-S1
4. McClure EM, Saleem S, Goudar SS, Garces A, Whitworth R, Esamai F, et al. Stillbirth 2010–2018: a prospective, population-based, multi-country study from the global network. Reprod Health. (2020) 17(2):146. doi: 10.1186/s12978-020-00991-y
5. Mcclure EM, Pasha O, Goudar SS, Chomba E, Garces A, Tshefu A, et al. Epidemiology of stillbirth in low-middle income countries: a global network study. Acta Obstet Gynecol Scand. (2011) 90(12):1379–85. doi: 10.1111/j.1600-0412.2011.01275.x
6. Hug L, You D, Blencowe H, Mishra A, Wang Z, Fix MJ, et al. Global, regional, and national estimates and trends in stillbirths from 2000 to 2019: a systematic assessment. Lancet. (2021) 398(10302):772–85. doi: 10.1016/S0140-6736(21)01112-0
7. Blencowe H, Cousens S, Jassir FB, Say L, Chou D, Mathers C, et al. National, regional, and worldwide estimates of stillbirth rates in 2015, with trends from 2000: a systematic analysis. Lancet Glob Health. (2016) 4(2):e98–108. doi: 10.1016/S2214-109X(15)00275-2
8. Frøen JF, Friberg IK, Lawn JE, Bhutta ZA, Pattinson RC, Allanson ER, et al. Stillbirths: progress and unfinished business. Lancet. (2016) 387(10018):574–86. doi: 10.1016/S0140-6736(15)00818-1
9. Every Newborn Action Plan. Available online at: https://www.who.int/initiatives/every-newborn-action-plan (Accessed January 22, 2025).
10. United Nations. The Sustainable Development Goals Report (2024). Available online at: https://unstats.un.org/sdgs/report/2024/ (Accessed April 15, 2025).
11. A neglected tragedy: The global burden of stillbirths 2020 | UNICEF (2020). Available online at: https://www.unicef.org/reports/neglected-tragedy-global-burden-of-stillbirths-2020 (Accessed January 22, 2025).
12. WHO. World Health Organization; GHO | Global Observatory on eHealth - Key Indicators | Ghana - key indicators. Available online at: https://apps.who.int/gho/data/node.goe.ki-GHA?lang=en (Accessed April 13, 2025).
13. Poulin D, Nimo G, Royal D, Joseph PV, Nimo T, Nimo T, et al. Infant mortality in Ghana: investing in health care infrastructure and systems. Health Aff Sch. (2024) 2(2):qxae005. doi: 10.1093/haschl/qxae005
14. Bernis L de , Kinney MV, Stones W, ten Hoope-Bender P, Vivio D, Leisher SH, et al. Stillbirths: ending preventable deaths by 2030. Lancet. 2016;387(10019):703–16. doi: 10.1016/S0140-6736(15)00954-X
15. Dah AK, Osarfo J, Ampofo GD, Appiah-Kubi A, Mbroh H, Azanu WK, et al. Stillbirth incidence and determinants in a tertiary health facility in the volta region of Ghana. PLoS One. (2023) 18(12):e0296076. doi: 10.1371/journal.pone.0296076
16. Goldenberg R, Griffin J, Kamath-Rayne B, Harrison M, Rouse D, Moran K, et al. Clinical interventions to reduce stillbirths in sub-Saharan Africa: a mathematical model to estimate the potential reduction of stillbirths associated with specific obstetric conditions. BJOG Int J Obstet Gynaecol. (2018) 125(2):119–29. doi: 10.1111/1471-0528.14304
17. McClure EM, Saleem S, Pasha O, Goldenberg RL. Stillbirth in developing countries: a review of causes, risk factors and prevention strategies. J Matern Fetal Neonatal Med. (2009) 22(3):183–90. doi: 10.1080/14767050802559129
18. Amegah AK, Quansah R, Jaakkola JJK. Household air pollution from solid fuel use and risk of adverse pregnancy outcomes: a systematic review and meta-analysis of the empirical evidence. PLoS One. (2014) 9(12):e113920. doi: 10.1371/journal.pone.0113920
19. Hammad M, Nomani MA, Rahman MHU. Solid fuel combustion and adverse pregnancy outcomes: a nationwide study on stillbirth in India. Public Health. (2024) 237:367–73. doi: 10.1016/j.puhe.2024.10.036
20. Abraham JD. Gender-based planning of meals at the household level in Ghana. Afr J Food Agric Nutr Dev. (2023) 23(6):23590–616. doi: 10.18697/ajfand.121.22750
21. Ansah RK, Boadi RK, Obeng-Denteh W, Asosega KA, Tawiah K. Exploring cooking fuel choices among Ghanaian women of reproductive age: a socio-economic analysis from a statistical mechanics perspective. PLoS One. (2025) 20(1):e0317004. doi: 10.1371/journal.pone.0317004
22. Moro A, Nonterah EA, Klipstein-Grobusch K, Oladokun S, Welaga P, Ansah PO, et al. Early life ambient air pollution, household fuel use, and under-5 mortality in Ghana. Environ Int. (2024) 187:108693. doi: 10.1016/j.envint.2024.108693
23. Amir-ud-Din R, Kumar R, Naeem N, Khan M. Air pollution and under-5 child mortality: linking satellite and IPUMS-DHS data across 41 countries in south Asia and sub-Saharan Africa. BMC Public Health. (2024) 24(1):2996. doi: 10.1186/s12889-024-20476-y
24. Corsini E, Vecchi R, Marabini L, Fermo P, Becagli S, Bernardoni V, et al. The chemical composition of ultrafine particles and associated biological effects at an alpine town impacted by wood burning. Sci Total Environ. (2017) 587–588:223–31. doi: 10.1016/j.scitotenv.2017.02.125
25. Pope DP, Mishra V, Thompson L, Siddiqui AR, Rehfuess EA, Weber M, et al. Risk of low birth weight and stillbirth associated with indoor air pollution from solid fuel use in developing countries. Epidemiol Rev. (2010) 32:70–81. doi: 10.1093/epirev/mxq005
26. Siddika N, Balogun HA, Amegah AK, Jaakkola JJK. Prenatal ambient air pollution exposure and the risk of stillbirth: systematic review and meta-analysis of the empirical evidence. Occup Environ Med. (2016) 73(9):573–81. doi: 10.1136/oemed-2015-103086
27. Nuhu P, Bukari D, Banye EZ. Driving improved cooking technology uptake in Ghana: an analysis of costs and benefits. Energy Sustain Dev. (2022) 66:26–43. doi: 10.1016/j.esd.2021.10.008
28. Ali J, Khan W. Factors affecting access to clean cooking fuel among rural households in India during COVID-19 pandemic. Energy Sustain Dev. (2022) 67:102–11. doi: 10.1016/j.esd.2022.01.006
29. Rehfuess EA, Puzzolo E, Stanistreet D, Pope D, Bruce NG. Enablers and barriers to large-scale uptake of improved solid fuel stoves: a systematic review. Environ Health Perspect. (2014) 122(2):120–30. doi: 10.1289/ehp.1306639
30. Sharma D, Ravindra K, Kaur M, Prinja S, Mor S. Cost evaluation of different household fuels and identification of the barriers for the choice of clean cooking fuels in India. Sustain Cities Soc. (2020) 52:101825. doi: 10.1016/j.scs.2019.101825
31. Akombi BJ, Ghimire PR, Agho KE, Renzaho AM. Stillbirth in the African great lakes region: a pooled analysis of demographic and health surveys. PLoS One. (2018) 13(8):e0202603. doi: 10.1371/journal.pone.0202603
32. Weber E, Adu-Bonsaffoh K, Vermeulen R, Klipstein-Grobusch K, Grobbee DE, Browne JL, et al. Household fuel use and adverse pregnancy outcomes in a Ghanaian cohort study. Reprod Health. (2020) 17(1):29. doi: 10.1186/s12978-020-0878-3
33. Woolley KE, Dickinson-Craig E, Bartington SE, Oludotun T, Kirenga B, Mariga ST, et al. Effectiveness of interventions to reduce household air pollution from solid biomass fuels and improve maternal and child health outcomes in low- and middle-income countries: a systematic review protocol. Syst Rev. (2021) 10(1):33. doi: 10.1186/s13643-021-01590-z
34. Ghana Statistical Service (GSS) and ICF. Ghana Demographic and Health Survey 2022 (2024). Available online at: https://microdata.worldbank.org/index.php/catalog/6122 (Accessed April 16, 2025).
35. Organization WH. Neonatal and perinatal mortality: country, regional and global estimates. World Health Organization (2006). Available online at: https://iris.who.int/handle/10665/43444 (Accessed April 16, 2025).
36. Organization WH. Defining clean fuels and technologies (2025). Available online at: https://www.who.int/tools/clean-household-energy-solutions-toolkit/module-7-defining-clean (Accessed April 16, 2025).
37. Boahen E, Owusu L. Addressing Water Quality Challenges in Ghana’s Greater Accra Region: A Review for Sustainable Access to Safe Drinking Water. OSF (2023). Available online at: https://osf.io/23avu (Accessed January 22, 2025).
38. Velleman Y, Mason E, Graham W, Benova L, Chopra M, Campbell OMR, et al. From joint thinking to joint action: a call to action on improving water, sanitation, and hygiene for maternal and newborn health. PLoS Med. (2014) 11(12):e1001771. doi: 10.1371/journal.pmed.1001771
39. Luo M, Liu T, Ma C, Fang J, Zhao Z, Wen Y, et al. Household polluting cooking fuels and adverse birth outcomes: an updated systematic review and meta-analysis. Front Public Health. (2023) 11:978556. doi: 10.3389/fpubh.2023.978556
40. Agrawal S, Yamamoto S. Effect of indoor air pollution from biomass and solid fuel combustion on symptoms of preeclampsia/eclampsia in Indian women. Indoor Air. (2015) 25(3):341–52. doi: 10.1111/ina.12144
41. Daba C, Asmare L, Demeke Bayou F, Arefaynie M, Mohammed A, Tareke AA, et al. Exposure to indoor air pollution and adverse pregnancy outcomes in low and middle-income countries: a systematic review and meta-analysis. Front Public Health. (2024) 12:1356830. doi: 10.3389/fpubh.2024.1356830
42. Xue T, Tong M, Li J, Wang R, Guan T, Li J, et al. Estimation of stillbirths attributable to ambient fine particles in 137 countries. Nat Commun. (2022) 13(1):6950. doi: 10.1038/s41467-022-34250-4
43. Wylie BJ, Coull BA, Hamer DH, Singh MP, Jack D, Yeboah-Antwi K, et al. Impact of biomass fuels on pregnancy outcomes in central east India. Environ Health. (2014) 13(1):1. doi: 10.1186/1476-069X-13-1
44. Austin KF, Mejia MT. Household air pollution as a silent killer: women’s status and solid fuel use in developing nations. Popul Environ. (2017) 39(1):1–25. doi: 10.1007/s11111-017-0269-z
45. Fullerton DG, Bruce N, Gordon SB. Indoor air pollution from biomass fuel smoke is a major health concern in the developing world. Trans R Soc Trop Med Hyg. (2008) 102(9):843–51. doi: 10.1016/j.trstmh.2008.05.028
46. Perera FP, Jedrychowski W, Rauh V, Whyatt RM. Molecular epidemiologic research on the effects of environmental pollutants on the fetus. Environ Health Perspect. (1999) 107(suppl 3):451–60. doi: 10.1289/ehp.99107s3451
47. Kannan S, Misra DP, Dvonch JT, Krishnakumar A. Exposures to airborne particulate matter and adverse perinatal outcomes: a biologically plausible mechanistic framework for exploring potential effect modification by nutrition. Environ Health Perspect. (2006) 114(11):1636–42. doi: 10.1289/ehp.9081
48. Aref-Adib M, Freeman-Wang T, Ataullah I. The older obstetric patient. Obstet Gynaecol Reprod Med. (2008) 18(2):43–8. doi: 10.1016/j.ogrm.2007.12.001
49. Carolan M. The graying of the obstetric population: implications for the older mother. J Obstet Gynecol Neonatal Nurs. (2003) 32(1):19–27. doi: 10.1177/0884217502239797
50. Grotegut CA, Chisholm CA, Johnson LNC, Brown HL, Heine RP, James AH. Medical and obstetric complications among pregnant women aged 45 and older. PLoS One. (2014) 9(4):e96237. doi: 10.1371/journal.pone.0096237
51. Management of Stillbirth. Available online at: https://www.acog.org/clinical/clinical-guidance/obstetric-care-consensus/articles/2020/03/management-of-stillbirth (Accessed May 9, 2025).
52. Saenen ND, Martens DS, Neven KY, Alfano R, Bové H, Janssen BG, et al. Air pollution-induced placental alterations: an interplay of oxidative stress, epigenetics, and the aging phenotype? Clin Epigenetics. (2019) 11(1):124. doi: 10.1186/s13148-019-0688-z
53. Kang G, Lim JY, Kale AS, Lee LY. Adverse effects of young maternal age on neonatal outcomes. Singapore Med J. (2015) 56(3):157–63. doi: 10.11622/smedj.2014194
54. Noori N, Proctor JL, Efevbera Y, Oron AP. The effect of adolescent pregnancy on child mortality in 46 low- and middle-income countries. BMJ Glob Health. (2022) 7(5):e007681. doi: 10.1136/bmjgh-2021-007681
55. Mekonnen T, Dune T, Perz J. Maternal health service utilisation of adolescent women in sub-Saharan Africa: a systematic scoping review. BMC Pregnancy Childbirth. (2019) 19(1):366. doi: 10.1186/s12884-019-2501-6
56. Ganchimeg T, Ota E, Morisaki N, Laopaiboon M, Lumbiganon P, Zhang J, et al. Pregnancy and childbirth outcomes among adolescent mothers: a world health organization multicountry study. BJOG Int J Obstet Gynaecol. (2014) 121(Suppl 1):40–8. doi: 10.1111/1471-0528.12630
57. Dongzagla A, Adams AM. Determinants of urban household choice of cooking fuel in Ghana: do socioeconomic and demographic factors matter? Energy. (2022) 256:124613. doi: 10.1016/j.energy.2022.124613
58. Senkyire EK, Boateng D, Boakye FO, Logo DD, Ohaja M. Socio-economic factors associated with adolescent pregnancy and motherhood: analysis of the 2017 Ghana maternal health survey. PLoS One. (2022) 17(12):e0272131. doi: 10.1371/journal.pone.0272131
59. Viirman F, Hesselman S, Wikström AK, Skoog Svanberg A, Skalkidou A, Sundström Poromaa I, et al. Self-rated health before pregnancy and adverse birth outcomes in Sweden: a population-based register study. Birth Berkeley Calif. (2021) 48(4):541–9. doi: 10.1111/birt.12567
60. Yang H, Deng Q, Geng Q, Tang Y, Ma J, Ye W, et al. Association of self-rated health with chronic disease, mental health symptom and social relationship in older people. Sci Rep. (2021) 11(1):14653. doi: 10.1038/s41598-021-94318-x
61. Kananen L, Enroth L, Raitanen J, Jylhävä J, Bürkle A, Moreno-Villanueva M, et al. Self-rated health in individuals with and without disease is associated with multiple biomarkers representing multiple biological domains. Sci Rep. (2021) 11(1):6139. doi: 10.1038/s41598-021-85668-7
62. Aliyu MH, Wilson RE, Zoorob R, Chakrabarty S, Alio AP, Kirby RS, et al. Alcohol consumption during pregnancy and the risk of early stillbirth among singletons. Alcohol Fayettev N. (2008) 42(5):369–74. doi: 10.1016/j.alcohol.2008.04.003
63. CDC. Alcohol and Pregnancy. About Alcohol Use During Pregnancy (2025). Available online at: https://www.cdc.gov/alcohol-pregnancy/about/index.html (Accessed April 16, 2025).
64. Balmes JR. Household air pollution from domestic combustion of solid fuels and health. J Allergy Clin Immunol. (2019) 143(6):1979–87. doi: 10.1016/j.jaci.2019.04.016
65. Columbia University Irving Medical Center. Stillbirth Risk Triples When Women Smoke and Drink During Pregnancy (2021). Available online at: https://www.cuimc.columbia.edu/news/stillbirth-risk-triples-when-women-smoke-and-drink-during-pregnancy (Accessed May 9, 2025).
66. (PDF) Clustering of multiple health risk behaviours and association with socio-demographic characteristics and psychological distress among adolescents in Ghana: A latent class analysis. ResearchGate (2024). https://www.researchgate.net/publication/347490127_Clustering_of_multiple_health_risk_behaviours_and_association_with_socio-demographic_characteristics_and_psychological_distress_among_adolescents_in_Ghana_A_latent_class_analysis (Accessed May 9, 2025).
67. Chen J, Liao H, Zhang T. Empowering women substantially accelerates the household clean energy transition in China. Energy Policy. (2024) 187:114048. doi: 10.1016/j.enpol.2024.114048
68. Addressing the continuum of maternal and newborn care in Ghana: implications for policy and practice | Health Policy and Planning | Oxford Academic. Available online at: https://academic.oup.com/heapol/article/31/10/1355/2567066 (Accessed May 9, 2025).
69. Coony Jd’E, De Martino SA, Kundu S, Sousa Lourenco JI. Ghana - Energy Sector Transformation Initiative Project: Improved Cookstoves, a Way to Care for One’s Family - Behavioral Diagnostics Note. World Bank. Available online at: https://documents.worldbank.org/pt/publication/documents-reports/documentdetail/957001614057884515 (Accessed Sept 28, 2025).
70. The landscape of energy for cooking in Ghana: A review | Climate & Clean Air Coalition. Available online at: https://www.ccacoalition.org/resources/landscape-energy-cooking-ghana-review (Accessed Sept 28, 2025).
71. Barstow CK, Nagel CL, Clasen TF, Thomas EA. Process evaluation and assessment of use of a large scale water filter and cookstove program in Rwanda. BMC Public Health. (2016) 16(1):584. doi: 10.1186/s12889-016-3237-0
72. Tamire M, Addissie A, Skovbjerg S, Andersson R, Lärstad M. Socio-cultural reasons and community perceptions regarding indoor cooking using biomass fuel and traditional stoves in rural Ethiopia: a qualitative study. Int J Environ Res Public Health. (2018) 15(9):2035. doi: 10.3390/ijerph15092035
73. Woolley KE, Bartington SE, Thomas GN, Pope FD, Muhizi A, Mugabe C, et al. Women’s perceptions and attitudes to household air pollution exposure and capability to change cooking behaviours in urban Rwanda. Sustainability. (2022) 14(3):1608. doi: 10.3390/su14031608
74. Adhikari B, Kang SSY, Dahal A, Mshamu S, Deen J, Pell C, et al. Acceptability of improved cook stoves-a scoping review of the literature. PLOS Glob Public Health. (2025) 5(1):e0004042. doi: 10.1371/journal.pgph.0004042
75. WHO recommendations on antenatal care for a positive pregnancy experience. Available online at: https://www.who.int/publications/i/item/9789241549912 (Accessed May 9, 2025).
76. Rubin R. It takes an average of 17 years for evidence to change practice-the burgeoning field of implementation science seeks to speed things up. JAMA. (2023) 329(16):1333–6. doi: 10.1001/jama.2023.4387
77. Clean cooking fuel for cleaner air in Ghanaian households | emLab. Available online at: https://emlab.ucsb.edu/blog/clean-cooking-fuel-cleaner-air-ghanaian-households (Accessed May 9, 2025).
78. Ghana Country Action Plan (CAP) | Clean Cooking Alliance. https://cleancooking.org/reports-and-tools/ghana-country-action-plan-cap/ (Accessed May 9, 2025).
79. Younger A, Alkon A, Harknett K, Kirby MA, Elon L, Lovvorn AE, et al. Effects of a LPG stove and fuel intervention on adverse maternal outcomes: a multi-country randomized controlled trial conducted by the household air pollution intervention network (HAPIN). Environ Int. (2023) 178:108059. doi: 10.1016/j.envint.2023.108059
Keywords: stillbirth, unclean cooking fuel, household air pollution, maternal health, environmental risk factors, Ghana, demographic and health survey
Citation: West KP, Sznajder KK, Hwang G, Sauve HE, Roba KT, Baatiema L, Kenu E, Noora CL, Gizaw AT and Yilma AN (2025) Unclean cooking fuel use and stillbirth in Ghana: evidence from the 2022 DHS. Front. Glob. Women's Health 6:1636924. doi: 10.3389/fgwh.2025.1636924
Received: 28 May 2025; Accepted: 6 October 2025;
Published: 23 October 2025.
Edited by:
Keith Dana Thomsen, Washington River Protection Solutions, United StatesReviewed by:
Abdul-Moomin Adams, SD Dombo University of Business and Integrated Development Studies, GhanaAli Moro, C.K Tedam University of Technology and Applied Sciences, Ghana
Copyright: © 2025 West, Sznajder, Hwang, Sauve, Roba, Baatiema, Kenu, Noora, Gizaw and Yilma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abebayehu N. Yilma, YW55NTEyNkBwc3UuZWR1
 Kirstin P. West
Kirstin P. West Kristin K. Sznajder1,2
Kristin K. Sznajder1,2 Hannah E. Sauve
Hannah E. Sauve Leonard Baatiema
Leonard Baatiema Abebayehu N. Yilma
Abebayehu N. Yilma