- 1Applied Psychology, Faculty of Education, Western University, London, ON, Canada
- 2Western Institute for Neuroscience, Western University, London, ON, Canada
- 3Neuroscience, Schulich School of Medicine and Dentistry, Western University, London, ON, Canada
- 4Psychiatry, Schulich School of Medicine and Dentistry, University of Western Ontario, London, ON, Canada
Introduction: Perinatal individuals are at an increased risk of experiencing psychological distress, which often manifests in a combination of co-occurring symptoms of anxiety, depression, and stress. During the COVID-19 pandemic, the rates of psychological distress experienced by perinatal women dramatically increased, in some cases doubling or even tripling. This increase is concerning as psychological distress can impact the health and wellbeing of mothers and their offspring, including an offspring's neurocognitive, physical, mental, and socio-emotional development. The strategies a perinatal individual uses to cope with psychological distress are modifiable and, therefore, can be targeted to help improve outcomes for mothers and their offspring.
Methods: This rapid review describes and synthesizes the literature related to coping with perinatal psychological distress during the COVID-19 pandemic. This review included twenty-four cross-sectional studies.
Results: Perinatal individuals reported using various coping strategies to deal with the COVID-19 pandemic, including social strategies (e.g., connecting with others); physical strategies (e.g., exercising); cognitive strategies (e.g., positive re-appraisal); and spiritual strategies (e.g., prayer). An avoidant style of coping and its accompanying behaviours, including disengagement, substance use, and distraction via screen time/social media use, were significantly associated with higher levels of psychological distress. Strategies associated with lower levels of psychological distress included sleep and social support.
Discussion: Future studies should address the impact of technology on coping and the long-term impact of coping styles used during the COVID-19 pandemic on the wellbeing of mothers and their offspring. Although this rapid review centered on the COVID-19 context, its findings are broadly relevant to women worldwide who continue to experience prolonged stressors such as climate change, poverty, and conflict.
Introduction
Perinatal psychological distress describes the presence of emotional distress manifesting as symptoms of depression, anxiety, and stress from pregnancy through 1-year after delivery (1). The symptoms of depression, anxiety, and stress can often co-occur and can sometimes reach clinical significance, warranting a diagnosis (1, 2). Compared to the general population, perinatal individuals are at an increased risk of experiencing psychological distress, likely due to the marked physical, emotional, and social changes that are characteristic of the perinatal period (3). Evidence suggests that perinatal psychological distress is related to a lower quality of life and poorer physical health in those affected (4, 5).
The prevalence of psychological distress amongst perinatal individuals has significantly increased during the COVID-19 pandemic (6). Compared to pre-pandemic levels, symptoms of stress, depression, and anxiety were all found to dramatically increase amongst perinatal individuals around the world during the COVID-19 pandemic (6–14).
Perinatal psychological distress not only affects the wellbeing of mothers, but it can also negatively impact their offspring. The literature suggests that both prenatal and postpartum maternal psychological distress is associated with adverse outcomes in offspring. These include low birth weight (15), altered fetal, infant, and childhood brain development (16–18), adverse cognitive, socio-emotional, and motor outcomes (19), and an increased risk of neurodevelopmental and mental health disorders (17, 19).
Studies conducted during the COVID-19 pandemic, specifically, have documented altered infant outcomes related to perinatal psychological distress. These include altered infant brain structure (20–22), functional brain connectivity (20) and development, including differences in motor- (23), socioemotional- (24, 25), and cognitive- (22) functioning.
The research on the effects of perinatal psychological distress during the COVID-19 pandemic has led to identifying some modifiable risk- and protective factors (20, 23). For example, Papadopoulos and colleagues (23) found that during the COVID-19 pandemic, the duration of psychological distress in mothers was a risk factor for adverse infant motor development. Specifically, the 2-month-old infants who were most at risk of motor impairment were those whose mothers were depressed during both pre-and post-natal periods. In addition, social support was observed to protect infants from the negative impacts of maternal perinatal psychological distress during the COVID-19 pandemic (20). A study conducted by Manning and colleagues (20) demonstrated that perinatal distress altered the functional brain connectivity in 3-month-old infants whose mothers received low social support. Such studies emphasize the importance of identifying modifiable factors that can mitigate the negative impact that psychological distress has on perinatal individuals and their offspring.
One crucial, modifiable factor is coping - including different coping styles and strategies. Generally, avoidant coping styles, including strategies such as denial, distraction, substance use, and disengagement, are ineffective in dealing with perinatal psychological distress (26, 27). On the other hand, the efficacies of spiritual strategies and active coping styles, such as problem-focused coping (planning, information, and positive appraisal) and emotion-focused coping (venting, self-blame, acceptance, humour, religion, and emotional support) are variable, with their effectiveness being dependent on one's current situation (26, 27).
The COVID-19 pandemic was an unprecedented, worldwide, and chronic stressor accompanied by many restrictions that impacted lives on a day-to-day basis (27). Therefore, it is essential to examine coping among perinatal individuals within the context of the COVID-19 pandemic, as the insights gained can inform future guidelines for managing psychological distress in response to disaster-related and other long-term stressors. Although this review focuses on pandemic-related coping, the findings have broader relevance for women globally who face ongoing challenges such as climate change, poverty, and conflict. Identifying adaptive coping mechanisms is urgently needed to support the mental health and wellbeing of both mothers and their offspring across diverse and prolonged stress contexts. Although there is a substantial body of literature regarding coping and perinatal psychological distress during the COVID-19 pandemic, it has yet to undergo a structured review. Therefore, this rapid review aims to describe and synthesize the literature related to perinatal coping strategies, styles, and perinatal psychological distress during the COVID-19 pandemic by answering two questions: What coping strategies and styles did perinatal individuals use during the COVID-19 pandemic?; What is the relationship between psychological distress (depression, anxiety, stress) and the different coping styles/strategies used by perinatal individuals during the COVID-19 pandemic?
Methods
Search strategy
On July 8, 2024, the PsycINFO (ProQuest), PubMed, Scopus, Web of Science, and Google Scholar databases were searched for relevant literature. The search terms used included various combinations of terms related to coping (“coping,” “coping techniques,” “ coping styles,” “resilience,” and “Brief COPE”), the perinatal period (“pregnancy,” “pregnant,” “postpartum,” and “perinatal”), psychological distress (“mental health,” “depression,” “stress,” “anxiety,” “distress,” and “psychological distress”), and the COVID-19 pandemic (“COVID-19,” and “pandemic”) with Boolean operators (“AND”). The search filters included: 2020–2024, English, full-text, and peer-reviewed.
Selection criteria
The inclusion criteria were full-text peer-reviewed studies with primary data collection from 100 or more participants published between 2020 and 2024. The target population was perinatal individuals (pregnant to 12- months postpartum) at any point during the COVID-19 pandemic (from March 11, 2020, to May 5, 2023). The target topics for the studies were those that focused on coping styles, coping strategies and the relationship between coping styles and strategies and psychological distress —stress, anxiety, and depression. The stress, anxiety, and depression did not need to be directly related to COVID-19; rather, the distress simply had to occur during the COVID-19 pandemic period.
The exclusion criteria were books, editorials, dissertations, protocol documents, case reports, and reviews (rapid, systematic, meta-analyses). Studies were also excluded if participants in the sample had a serious health condition (e.g., HIV, Hepatitis) or were over 12 months postpartum, and if distress was measured in terms other than stress, anxiety, or depression (e.g., trauma).
Data extraction & synthesis
One author (A.P.) extracted data from all the studies included in the final review. The data extracted from each study included author names, year of publication, country of origin, participant information, study design, sampling methods, study instruments, and relevant results. One author (A.P.) employed a narrative style to synthesize the results from the 24 papers included in the final review.
Quality & risk of bias assessments
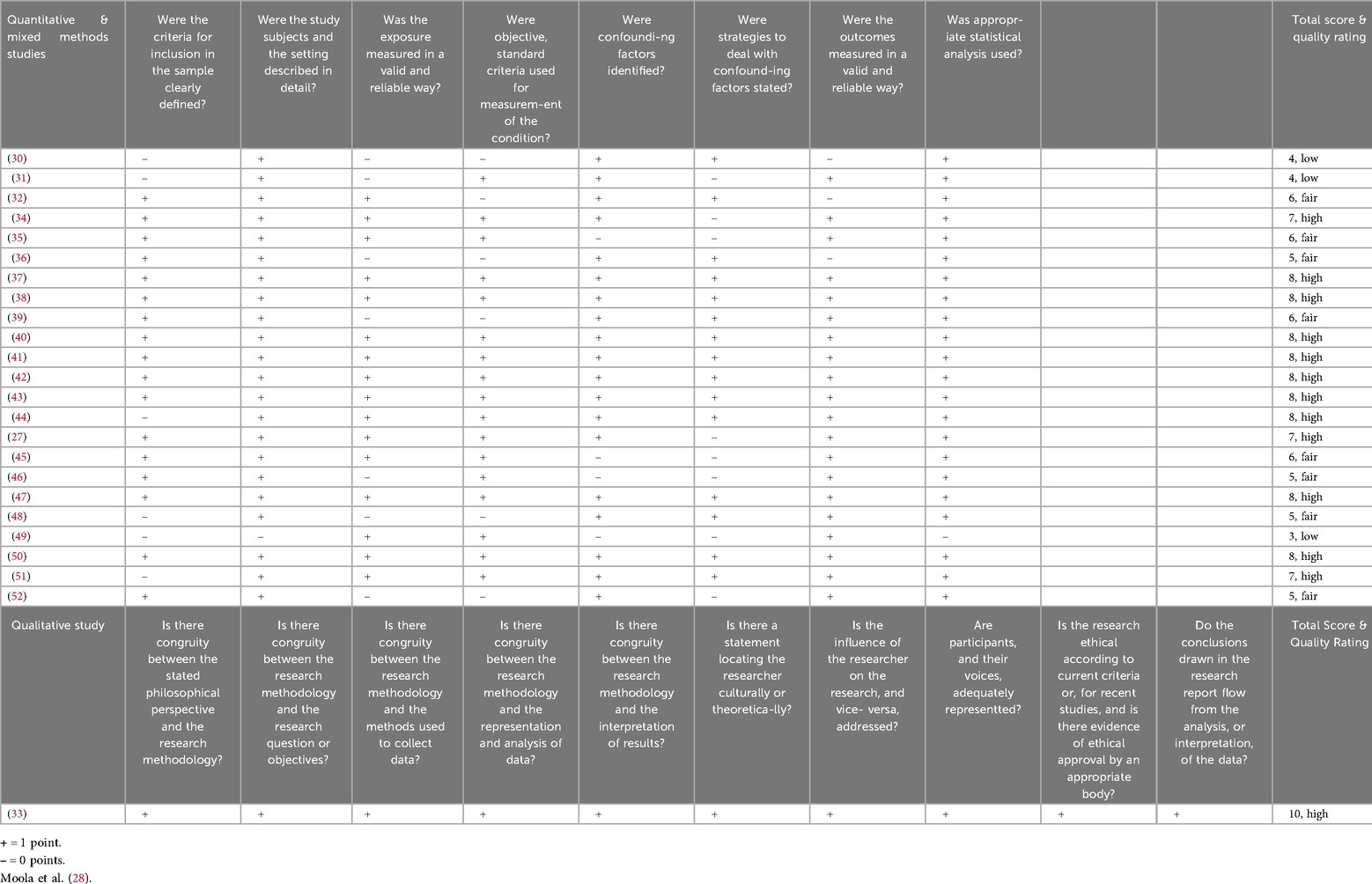
One author (A.P.) thoroughly evaluated the quality of the evidence and the risk of bias for each of the 24 studies included in the final review. The Joanna Briggs Institute's (JBI) cross-sectional and qualitative critical appraisal tools were used to evaluate evidence quality (28). The cross-sectional critical appraisal tool, consisting of 8 questions, was used to evaluate the quantitative and mixed-methods studies. A score of 7 or higher on the cross-sectional critical appraisal tool indicates high-quality evidence (28). The qualitative critical appraisal tool, consisting of 10 questions, was used to assess the evidence quality of the single qualitative study included in the final review (28). A score of 9 or higher on the qualitative critical appraisal tool indicates high-quality evidence (28).
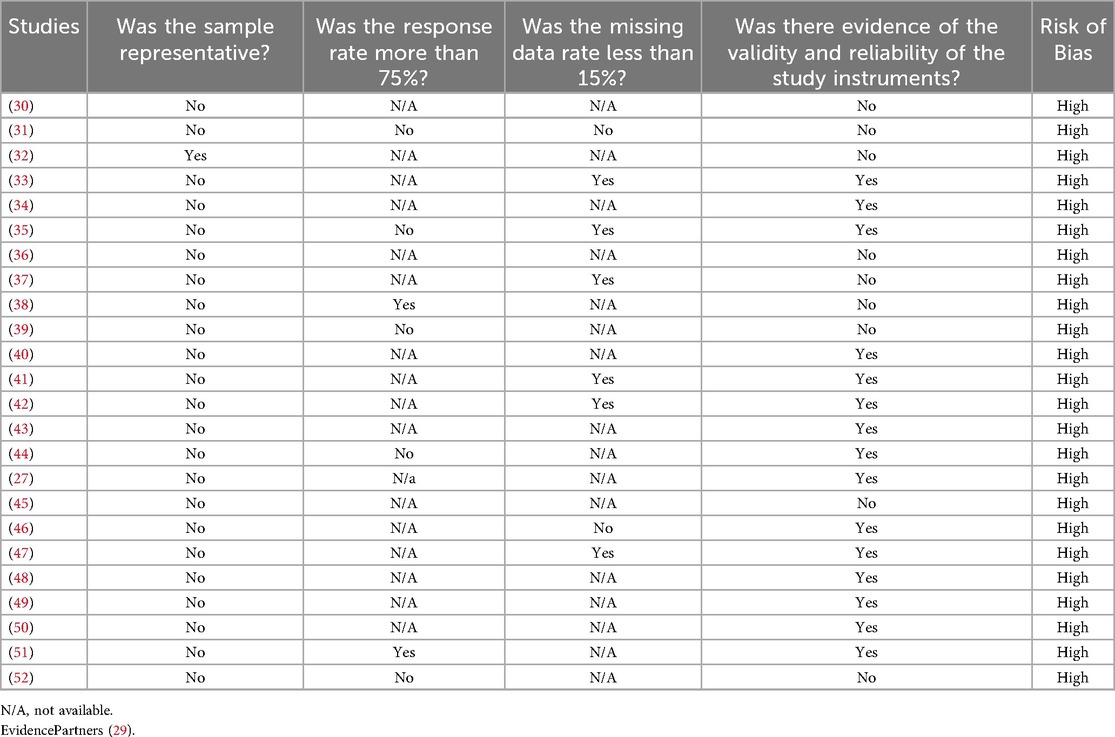
A modified protocol from McMaster's CLARITY group was used to evaluate the risk of bias in the studies (29). The risk of bias was assessed by examining the representativeness of the participant sample, the validity of the study instruments used, and, if available, the studies' response rates and amounts of missing data. Indicators of a high risk of bias included non-probabilistic sampling methods, a lack of evidence regarding the reliability and validity of the study instruments, a response rate under 75%, or a missing data rate of more than 15% (29).
Results
Search results
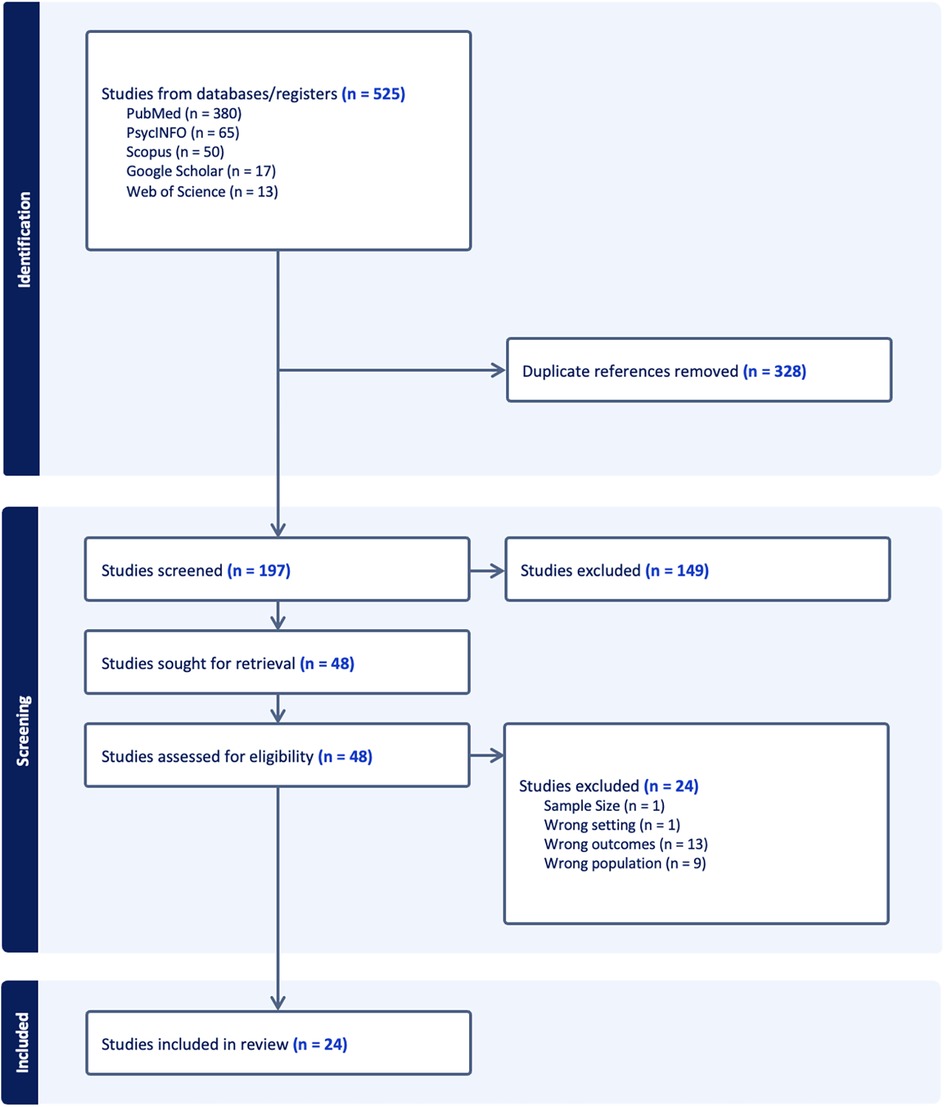
The initial search yielded 525 studies, and 328 duplicates were removed. One author (A.P.) screened the titles and abstracts of the 197 remaining studies and removed 149 for failing to meet the selection criteria (outlined in the methods section). One author (A.P.) retrieved and reviewed the full texts of the remaining 48 studies. A total of 24 studies met the eligibility criteria and were selected to be included in the rapid review. See Figure 1 includes a PRISMA flowchart outlining the search process and results.
Data extraction
The extracted data are presented below in Table 1. The last row of Table 1 explains the abbreviations used in the study instruments column.
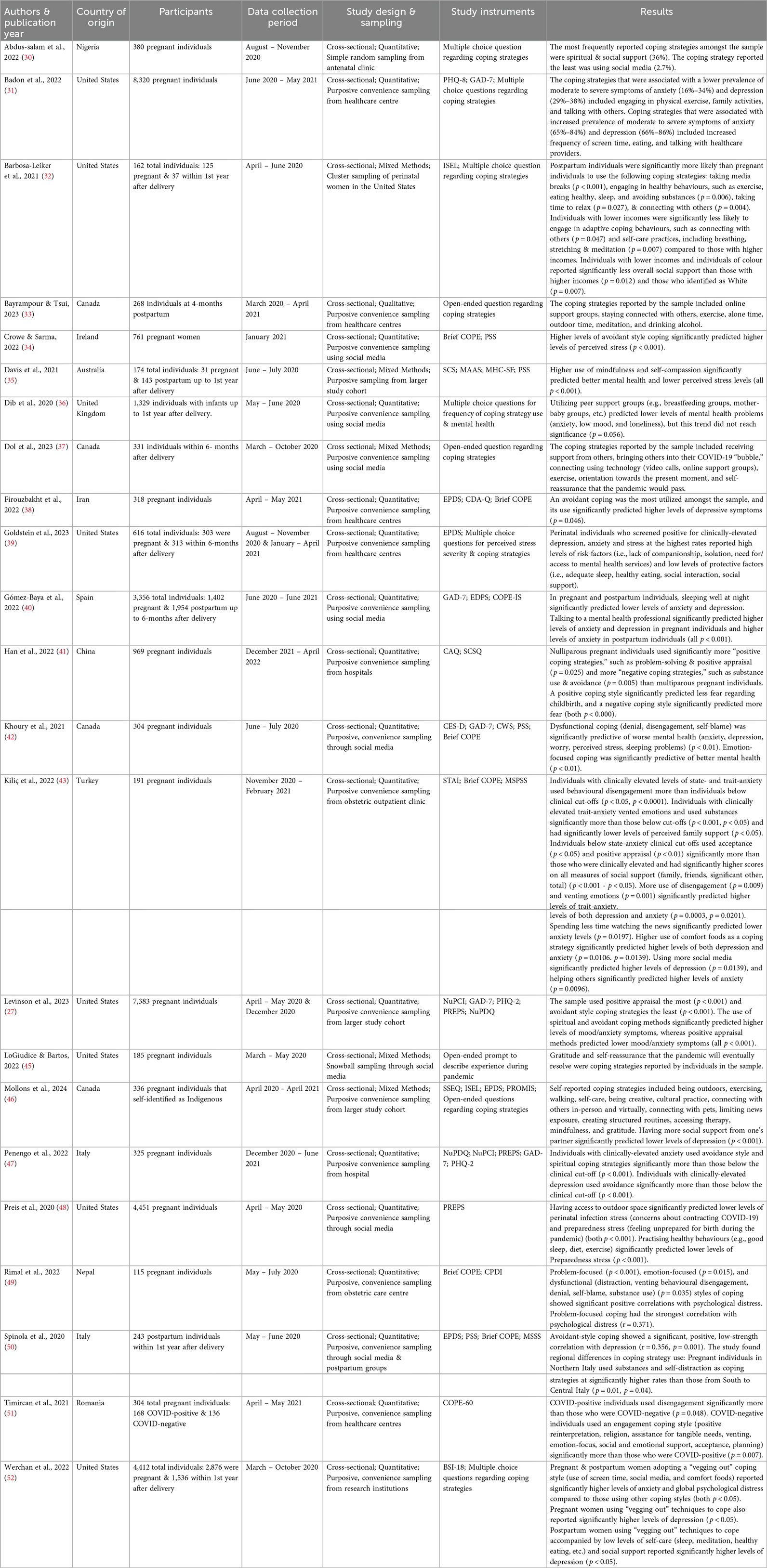
Table 1. Summary of reviewed studies. Coping strategies & styles and their relationship with psychological distress in perinatal individuals during the COVID-19 pandemic.
Study characteristics results
For detailed information regarding study characteristics, including countries of origin, study design, sampling methods, participants, data collection periods, and study instruments, refer to Table 1.
Countries
The studies used in this rapid review were from 13 countries of origin. Eight studies were from the United States, four were from Canada, two were from Italy, and single studies were from Nigeria, Ireland, Australia, the United Kingdom, Iran, Spain, China, Turkey, Nepal, and Romania.
Study design
All the studies included in the final review employed a cross-sectional study design. Six studies used mixed methods (quantitative & qualitative), 17 studies used quantitative methods, and one study used qualitative methods.
Sampling methods
Most studies used purposive, convenience sampling techniques to identify eligible individuals online or within healthcare centres. One study used simple random sampling to select individuals from an antenatal clinic to take part in the study (30), one study used snowball sampling methods to recruit individuals through social media (45), and one study used cluster sampling (32).
Participants
The total number of participants across all 24 studies was 35,757. In the mixed methods studies, the participant samples ranged between 162 (32) and 336 participants (46). In the quantitative studies, the participant samples ranged between 115 (49) and 8,320 participants (31). The sample size of the single qualitative study was 268 participants (33).
Data collection period
All studies collected data between 2020 and 2022. Thirteen studies collected data exclusively in 2020, ranging from March through December. Seven studies collected data from 2020 through 2021, ranging from April 2020 through June 2021. Three studies collected data exclusively in 2021, ranging from January through May. One study collected data from December 2021 through April 2022.
Study instruments
All the studies used self-report measures to collect data regarding the participants coping strategies, coping styles, and levels of psychological distress, including anxiety, stress, and depression.
Measures of coping
Six studies used multiple-choice questions to gather information on the coping strategies used by participants. Five studies used open-ended questions to ask participants to describe how they coped during the COVID-19 pandemic. The standardized measure of coping that was used most often was the Coping Styles Scale Brief Form (Brief COPE), and it was used in six studies. The Brief COPE is a 28-question, standardized, self-report measure of coping styles and strategies (53). The questions include information about receiving emotional support, watching TV, religious practices, acceptance, and beyond (53). Participants rate the frequency they use each coping strategy on a 4-point Likert scale from 1, “I haven't been doing this at all,” to 4, “I’ve been doing this a lot” (53). The items on the Brief COPE load onto three different subscales that represent different coping styles, including avoidant, problem-focused, and emotion-focused coping styles (53). The avoidant coping style is characterized by self-distraction, denial, substance use, and disengagement (53). The problem-focused coping style is characterized by planning and positive reframing, and the emotion-focused coping style is characterized by self-blame, acceptance, humour, venting, receiving emotional support, and religious practices (53). Other standardized measures of coping that were used by either 1 or 2 studies included in the review were the COPE-IS, NuPCI, ISEL, SCS, MAAS, SCSQ, MSPSS, SSEQ, MSSS, and COPE-60.
Measures of psychological distress
Six of the studies included in the final review focused only on coping styles and strategies and did not include psychological distress as an outcome measure (30, 32, 33, 37, 45, 51). Of the remaining eighteen studies, three used stress to measure psychological distress (34, 35, 48), two used anxiety (41, 43), and the remainder used some combination of depression, anxiety, and stress.
The standardized measure of anxiety that was used most often was the General Anxiety Disorder-7 (GAD-7), and it was used in five studies. The GAD-7 is a self-report measure that assesses symptoms of general anxiety disorder that an individual has experienced in the last two weeks (54). The GAD-7 includes seven items that are rated on a 4-point Likert scale, assessing the frequency that each symptom is experienced from 0, “not at all,” to 3, “nearly every day” (54). Scores above 4 indicate mild anxiety, scores above 9 indicate moderate anxiety and scores above 15 indicate severe anxiety (54). The GAD-7 is a useful scale for perinatal populations (55).
The standardized measure of depression that was used most often was the Edinburgh Postnatal Depression Scale (EPDS), and it was used in four studies. The EPDS is a self-report measure used in perinatal populations to measure symptoms of depression experienced in the week prior (56). The EPDS includes ten items that are rated on a 4-point Likert scale that assesses the frequency that each depressive symptom is experienced from 0, “not at all/never”, to 3, “quite often, most of the time, etc.” (56). Scores of 13 or more indicate that depression might be present (56).
The standardized measure of stress that was used most often was the PSS, and it was used in four studies. The PSS is a self-report measure that assesses the frequency of perceived stress symptoms in the past month using ten items rated on a 5-point Likert Scale ranging from 0, “never,” to 4, “very often” (57). Perceived stress indicates how much an individual feels stress subjectively (57). Scores 14 and above indicate moderate perceived stress, and scores 27 and above indicate high perceived stress (57). The PSS has been validated in perinatal samples (58).
Other psychological stress measures used in 1–3 studies include the BSI-18, PHQ, PREPS, STAI, CAQ, CDA-Q, CES-D, CPDI, CWS, MHC-SF, and PROMIS. Additionally, some studies used un-standardized measures to evaluate psychological distress, such as multiple-choice questions.
Quality & risk of bias assessment results
Of the 17 quantitative and six mixed-methods studies included in the review, 12 were determined to provide high-quality evidence (scoring seven or higher on the JBI cross-sectional study appraisal tool). Of the 11 quantitative and mixed methods studies that did not meet the high-quality evidence cut-off, most scored between 5 and 6, which indicates fair quality evidence, with two studies scoring 3–4, which indicates lower quality evidence. The studies below the high-quality evidence cut-off mostly lost points for lacking a detailed account of participant inclusion criteria and for lacking evidence regarding the reliability and validity of their study instruments. For example, measuring coping and psychological distress using measures, such as open-ended or multiple-choice questions that were not standardized or validated prior to use. The single qualitative study was deemed to be high quality (scoring above 9) according the JBI qualitative study appraisal tool. A detailed breakdown of the critical appraisal of evidence quality is in Appendix A.
All the studies included in the review were determined to have a high probability of being biased due to a lack of representativeness in the participant samples. The samples tended to mainly capture individuals with high levels of education and high socioeconomic status. The study samples also tended to lack ethnic and racial diversity, with many study samples being predominantly White. In addition, the sampling methods used by all, but one study were non-probabilistic. Many studies used online recruitment methods, had participants complete surveys online, and some studies used open-ended questions or multiple-choice measures without testing their psychometric properties, which all increased the risk of bias. A detailed breakdown of the results of the risk of bias assessment can be found in Appendix B.
Coping strategies & styles results
This rapid review aimed to answer the question: “What coping strategies and styles did perinatal individuals use during the COVID-19 pandemic?” The following results were observed.
Overall, perinatal individuals used a wide range of coping strategies and styles throughout the COVID-19 pandemic. One author (A.P.) grouped the main coping strategies and styles reported into four categories: social, cognitive, physical, and spiritual/cultural.
An important social strategy reported by perinatal individuals was receiving support from others, including social- (30, 39, 43, 46, 51, 52), instrumental- (44, 49, 51), and emotional- support (42, 51). Staying connected with others was another critical coping strategy reported by perinatal individuals (31–33, 36, 37, 39, 44). Further, perinatal individuals also reported connecting with other pregnant and postpartum mothers via online support groups (33, 36, 44), and some connected with mental health/healthcare professionals (31, 39, 40, 44).
The cognitive strategies perinatal individuals reported using during the COVID-19 pandemic included meditation/mindfulness (33, 35, 37, 44, 46), self-compassion (35), self-reassurance that the pandemic will pass (37, 45), positive re-framing/reinterpretation/appraisal (27, 42, 43, 49), acceptance of the current situation (42–44), and gratitude (44–46). Perinatal individuals also used disengagement for avoidance of stressors (27, 32, 34, 38, 42, 47, 49–51). Some notable examples included self-distraction from thoughts and problems via increased time spent on social media and watching television (30, 31, 44, 52) or by avoiding information overload by limiting time spent on social media or watching the news (32, 44, 46, 52).
The most common physical coping strategy reported included exercise, like walking and stretching (31–33, 37, 44, 46, 48). Other strategies included eating, whether it be healthy eating (32, 39, 44) or eating comfort foods (31, 52) and sleep (32, 39, 40, 42, 44, 48, 52). Some individuals reported avoiding substances such as drugs and alcohol (32), and some reported using these substances as a coping strategy (34, 43, 49–51).
Lastly, some individuals used spiritual or cultural practices as a coping mechanism during the COVID-19 pandemic (27, 44, 46, 47). In one study from Nigeria, spiritual coping was reported as the most frequently used strategy among the pregnant individuals in the sample (30). Spending time alone (33) and spending time outdoors (31, 44, 46, 48) were also reported and classified here as spiritual coping strategies.
Comparisons: perinatality, income, race, parity, region & COVID
One study compared coping between pregnant and postpartum individuals and between individuals of races and income levels (32). This study found that postpartum individuals were significantly more likely than pregnant individuals to take breaks from social media p < 0.001), engage in healthy behaviours (exercise, eating healthy, sleep, avoiding substances) (p = 0.006), take time to relax (p = 0.027), & connect with others (p = 0.004). They also found that individuals with higher income levels were significantly more likely to engage in adaptive coping behaviours such as connecting with others (p = 0.047) and self-care practices such as breathing, stretching, and meditation (p = 0.007). Individuals with higher income levels also had more access to social support than those with lower incomes (p = 0.012). Finally, they found that non-Hispanic White individuals had significantly higher levels of social support than individuals of other races (p = 0.0007).
One study found that pregnant individuals with no other living children made significantly more use of coping strategies in general than individuals with one or more living children (41). They found this was true for coping strategies they termed to be both “positive” (problem-solving and positive appraisal) (p = 0.025) and “negative” (substance use, avoidance) (p = 0.005) (41).
A study conducted in Italy with 325 pregnant individuals found a significant difference in coping strategies between individuals residing in different regions of Italy (50). Pregnant individuals in Northern Italy used substances and self-distraction significantly more than those in Central/Southern Italy (p = 0.01, p = 0.04) (50).
Finally, one study compared coping between COVID-positive and COVID-negative pregnant individuals (51). They observed that COVID-positive individuals used an avoidant style of coping (denial, substance use, mental and behavioural disengagement) significantly more than COVID-negative individuals (p = 0.048) and used an engagement coping style (positive reinterpretation, humour, religion, assistance for tangible needs, venting, emotion-focus, social and emotional support, acceptance, planning) significantly less (p = 0.007) (51).
Psychological distress, coping styles & strategies results
This rapid review also aimed to answer the question: “What is the relationship between psychological distress (depression, anxiety, stress) and the different coping styles/strategies used by perinatal individuals during the COVID-19 pandemic?” The following results were observed.
Coping styles & psychological distress
The coping styles that were found to be significantly associated with higher levels of psychological distress included an avoidant-coping style (27, 34, 38, 42, 43, 47, 49, 50) and a problem-focused coping style (49). There were conflicting results regarding the association between psychological distress and an emotion-focused coping style. A study of 304 pregnant individuals conducted in Canada found an emotion-focused coping style to be associated with lower levels of distress via mediation analysis (42); however, using correlation analysis, a study conducted in Nepal of 115 pregnant individuals found emotion-focused coping to be associated with higher levels of distress (49).
Coping strategies & psychological distress
On a finer scale, the individual coping strategies that were found to be significantly associated with lower levels of psychological distress included physical exercise (31, 48), connecting with others (31), getting a good night's sleep (40, 44, 48), eating healthy (48), positive appraisal (27, 43), social support (43, 46), spending less time watching the news (44), mindfulness (35), self-compassion (35), and going outdoors (48).
The coping strategies that were found to be significantly associated with higher levels of psychological distress included increased screen time/social media use (31, 44, 52), eating comfort foods (31, 44, 52), talking with mental health/healthcare providers (31, 40), religious/spiritual practices (27, 47), venting emotions (43), the use of substances (43), disengagement (43), and helping others (43).
Discussion
This rapid review aimed to describe and synthesize the literature on coping strategies and styles and their relationship with psychological distress in perinatal individuals during the COVID-19 pandemic. A rapid review methodology was selected to promptly consolidate and synthesize findings. Although the acute phase of the pandemic has concluded, women globally are continually exposed to long-term, high-stress situations such as climate change, economic instability, displacement, and conflict. The COVID-19 pandemic, also a prolonged and widespread stressor, offers a relevant context for understanding coping among perinatal individuals. While this review focused on pandemic-related experiences, the findings may be generalizable to other ongoing crises affecting women's mental health and wellbeing worldwide.
The findings of this review confirmed that perinatal individuals used several different coping strategies during the COVID-19 pandemic. The strategies used included those from social, cognitive, physical, and spiritual/cultural domains. They also adopted various styles, including avoidance, emotion-focused, and problem-focused coping styles. The most cited coping strategy was staying connected with others, appearing in eight studies (31–33, 36, 37, 39, 40, 44). Some individuals explained that bringing additional people into their “COVID-19 bubble” was imperative to coping (37). The next most cited strategies were physical exercise, appearing in seven studies (31–33, 37, 44, 46, 48), and social support, appearing in six studies (30, 39, 43, 46, 51, 52). Notably, in all the studies included in this rapid review, the same general coping strategies were reported and used by perinatal individuals worldwide.
High-quality evidence was insufficient to draw definitive conclusions about the relationship between psychological distress and a problem-focused coping style. However, evidence presented in this review suggests that problem-focused coping was not linked to lower levels of psychological distress for perinatal individuals during the COVID-19 pandemic. It follows that problem-focused coping, which focuses mainly on solving and planning, might not be a beneficial coping style during a situation like the COVID-19 pandemic, as individuals very much lacked control over their situations (e.g., lockdown rules, hospital regulations, etc.) and it was difficult to plan or problem-solve with frequently changing guidelines (59). However, positive appraisal as an individual coping strategy that falls under the problem-focused coping style was associated with lower levels of distress.
The evidence regarding emotion-focused coping was conflicting, although certain aspects of emotion-focused coping were found to likely be more beneficial than others, such as acceptance, and emotional support whereas other strategies such as venting were likely to be less helpful (27, 42, 43, 51).
The review yielded a large body of evidence with eight studies suggesting an avoidant-style coping was associated with higher levels of psychological distress in perinatal individuals around the world during the COVID-19 pandemic. Of the eight studies, seven were rated as high quality in the critical appraisal (see Appendix A). The body of evidence for this coping style in relation to psychological distress included a large-scale study of 7,383 pregnant participants conducted in the United States (27), a study of 761 pregnant participants from Ireland (34), and six studies ranging between 115 and 325 pregnant participants from Iran, Canada, Turkey, Italy, and Nepal (38, 42, 43, 47, 49). One additional study included 243 postpartum participants from Italy (50). The finding that avoidant-style coping was associated with higher levels of psychological distress is in line with literature regarding coping-styles and perinatal individuals before the COVID-19 pandemic (26, 27).
It also follows that coping behaviours that are generally associated with an avoidant-style of coping, such as eating comfort foods, disengagement, using substances, and screen time/using social media, were associated with higher levels of psychological distress (31, 43, 44, 52). Many perinatal individuals used avoidant-style coping strategies to try and cope with psychological distress during the COVID-19 pandemic. The frequent use of these strategies suggests that perinatal individuals require more support, including informational resources, to help them learn about and employ alternative, more beneficial strategies for coping. An interesting finding from comparison studies was that individuals in difficult but temporary situations used avoidant coping strategies more. For example, avoidant strategies were used more often by individuals who had an ongoing infection with the COVID-19 virus (51) and by individuals living in Northern Italy, where for some time, the impact of COVID-19 was large, with hospital systems being overwhelmed, large death tolls, and a high risk of contagion (50). While avoidant-style coping strategies might not be recommended for long-term distress, the literature suggests that some avoidant-style strategies may be warranted for use on a short-term basis and could be beneficial as a harm-reduction tool (i.e., using distraction to stop the use of more harmful behaviour, like using substances) (26, 50, 51).
The individual coping strategies that are likely to be the most beneficial, as they had a good amount of high-quality evidence (see Appendix A) regarding their relationship with lower levels of psychological distress included getting a good night's sleep (40, 44, 48), positive appraisal (27, 43), and social support (43, 46). An unexpected finding was that talking with mental health/healthcare providers was associated with higher levels of psychological distress (31, 40). However, this method of coping was primarily used by individuals with very high levels of psychological distress (31, 40). A cohort study design would have been more beneficial to better assess the use of this strategy, for example, to determine whether baseline psychological distress levels decrease when talking to a mental health professional over time. Religious practice was also associated with higher levels of psychological distress, which could also indicate that individuals with high levels of distress utilized these techniques often (27, 47). In addition, the studies included in this review did not necessarily capture the nuanced differences between positive (e.g., trust in God, comfort through reading scripture, etc.) and negative (e.g., questioning God, struggles in finding meaning, etc.) religious coping methods that could affect the way this style of coping is related to psychological distress (60).
With COVID-19 limiting the ability to engage with others in-person, the results from this rapid review suggest that many individuals used technology to cope with psychological distress. This ranged from joining online peer support groups, to engaging in video calls, to accessing social media. The evidence suggests that technology's value regarding coping is variable (30–33, 37, 44, 52). Although no direct evidence was accrued from the studies in this review, based on the evidence that social support was effective in reducing symptoms of psychological distress (43, 46), technology is likely to be helpful if used to maintain contact with and receive social support from others – via video call and online support groups. Where the evidence suggests technology is most likely not helpful, is when it is used for distraction (31, 44, 52) or when it results in an overload of negative information, such as consuming excessive COVID-19 related news programming (44).
Limitations
All studies included in this review employed a cross-sectional design, therefore no inferences regarding causality or directionality of the relationships between coping style/strategy and psychological distress can be made. In addition, an overwhelming majority of the studies used non-probabilistic sampling methods, leading to unrepresentative samples of the population at large. The generalizability of the findings is limited as most studies had high representation of perinatal individuals with high socioeconomic statuses, high levels of education, and to those who identify as white. The different instruments used for measurement of coping and psychological distress in the studies also brings variation to the constructs and limits the result comparisons that can be made across studies. Caution was taken regarding the recommendations put forth based on the results of this rapid review. Due to the nature and limited timeframe of this rapid review, we focused on summarizing key findings across studies rather than conducting in-depth comparative analyses of differences between countries, healthcare systems, or pandemic phases, which typically require more extensive data synthesis methods such as meta-analysis.
Recommendations & conclusions
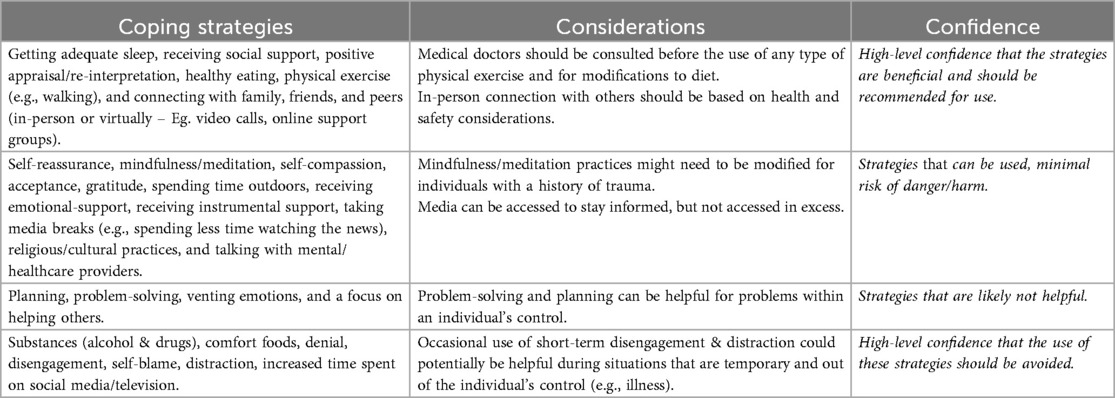
Overall, perinatal individuals used many different strategies to cope with psychological distress during the COVID-19 pandemic. Many individuals used avoidant-style coping, and it was reliably and consistently associated with higher levels of psychological distress. This result indicates the need to focus on providing clinical support and resources for coping to those experiencing perinatal psychological distress during disaster situations. Based on the evidence provided in this review, mental health intervention efforts for perinatal individuals during disaster situations should prioritize building quality sleep habits, building positive appraisal skills (e.g., cognitive behavioural therapy), and teaching individuals how to build and maintain supportive social networks. A priority would also be to guide individuals in the use of technology, with a focus on differentiating between technology use that has evidence of being beneficial in support coping (e.g., online support groups, video calls) and use that could be detrimental (e.g., excessive exposure to news outlets). For a detailed review of the coping strategies presented in this rapid review and recommendations regarding their use during disasters and similar situations, please refer to Appendix C.
Future directions
As the COVID-19 pandemic increased the use of and reliance on technology for many worldwide, further studies examining the role and nuance of technology in coping should be a priority. In addition, future longitudinal studies should investigate the long-term impact of different coping styles and strategies perinatal individuals used during the COVID-19 pandemic. Importantly, the insights gained from this research can extend beyond the pandemic, informing support strategies for perinatal individuals facing other prolonged or large-scale stressors, such as climate change, economic hardship, or conflict. Clinicians are encouraged to prioritize and provide increased support, time, and resources to perinatal individuals to help mitigate psychological distress not only during pandemics, but in a wide range of disaster-related and chronic stress contexts. Overall, this topic warrants a larger, comprehensive systematic review.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
AP: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. EGD: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was undertaken thanks to funding from the Canada Research Chairs Program.
Acknowledgments
The authors thank the publishers and authors of the original studies used in this rapid review.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Obrochta CA, Chambers C, Bandoli G. Psychological distress in pregnancy and postpartum. Women Birth. (2020) 33(6):583–91. doi: 10.1016/j.wombi.2020.01.009
2. Rallis S, Skouteris H, McCabe M, Milgrom J. A prospective examination of depression, anxiety and stress throughout pregnancy. Women Birth. (2014) 27(4):e36–42. doi: 10.1016/j.wombi.2014.08.002
3. Tang X, Lu Z, Hu D, Zhong X. Influencing factors for prenatal stress, anxiety and depression in early pregnancy among women in Chongqing, China. J Affect Disord. (2019) 253:292–302. doi: 10.1016/j.jad.2019.05.003
4. Maita H, Kobayashi T, Osawa H. Postpartum depression and health related quality of life: a necessary assessment. Int J Fam Commun Med. (2017) 1(1):11–7. doi: 10.15406/ijfcm.2017.01.00005
5. Sadat Z, Abedzadeh-Kalahroudi M, Kafaei Atrian M, Karimian Z, Sooki Z. The impact of postpartum depression on quality of life in women after child’s birth. Iran Red Crescent Med J. (2014) 16(2):e14995. doi: 10.5812/ircmj.14995
6. Ahmad M, Vismara L. The psychological impact of COVID-19 pandemic on women’s mental health during pregnancy: a rapid evidence review. Int J Environ Res Public Health. (2021) 18(13):7112. doi: 10.3390/ijerph18137112
7. Berthelot N, Lemieux R, Garon-Bissonnette J, Drouin-Maziade C, Martel É, Maziade M. Uptrend in distress and psychiatric symptomatology in pregnant women during the coronavirus disease 2019 pandemic. Acta Obstet Gynecol Scand. (2020) 99(7):848–55. doi: 10.1111/aogs.13925
8. Boekhorst MGBM, Muskens L, Hulsbosch LP, Van Deun K, Bergink V, Pop VJM, et al. The COVID-19 outbreak increases maternal stress during pregnancy, but not the risk for postpartum depression. Arch Womens Mental Health. (2021) 24(6):1037–43. doi: 10.1007/s00737-021-01104-9
9. Lebel C, MacKinnon A, Bagshawe M, Tomfohr-Madsen L, Giesbrecht G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J Affect Disord. (2020) 277:5–13. doi: 10.1016/j.jad.2020.07.126
10. Stepowicz A, Wencka B, Bieńkiewicz J, Horzelski W, Grzesiak M. Stress and anxiety levels in pregnant and post-partum women during the COVID-19 pandemic. Int J Environ Res Public Health. (2020) 17(24):9450. doi: 10.3390/ijerph17249450
11. Suárez-Rico BV, Estrada-Gutierrez G, Sánchez-Martínez M, Perichart-Perera O, Rodríguez-Hernández C, González-Leyva C, et al. Prevalence of depression, anxiety, and perceived stress in postpartum Mexican women during the COVID-19 lockdown. Int J Environ Res Public Health. (2021) 18(9):4627. doi: 10.3390/ijerph18094627
12. Wu Y, Zhang C, Liu H, Duan C, Li C, Fan J, et al. Perinatal depressive and anxiety symptoms of pregnant women during the coronavirus disease 2019 outbreak in China. Am J Obstet Gynecol. (2020) 223(2):240.e1–e9. doi: 10.1016/j.ajog.2020.05.009
13. Zanardo V, Manghina V, Giliberti L, Vettore M, Severino L, Straface G. Psychological impact of COVID-19 quarantine measures in northeastern Italy on mothers in the immediate postpartum period. Int J Gynecol Obstet. (2020) 150(2):184–8. doi: 10.1002/ijgo.13249
14. Zilver SJM, Broekman BFP, Hendrix YMGA, de Leeuw RA, Mentzel SV, van Pampus MG, et al. Stress, anxiety and depression in 1466 pregnant women during and before the COVID-19 pandemic: a Dutch cohort study. J Psychosom Obstet Gynaecol. (2021) 42(2):108–14. doi: 10.1080/0167482X.2021.1907338
15. Misgina KH, Levine L, Boezen HM, Bezabih AM, van der Beek EM, Groen H. Influence of perinatal distress on adverse birth outcomes: a prospective study in the Tigray region, northern Ethiopia. PLoS One. (2023) 18(7):e0287686. doi: 10.1371/journal.pone.0287686
16. Lebel C, Walton M, Letourneau N, Giesbrecht GF, Kaplan BJ, Dewey D. Prepartum and postpartum maternal depressive symptoms are related to children’s brain structure in preschool. Biol Psychiatry (1969). (2016) 80(11):859–68. doi: 10.1016/j.biopsych.2015.12.004
17. Mandl S, Alexopoulos J, Doering S, Wildner B, Seidl R, Bartha-Doering L. The effect of prenatal maternal distress on offspring brain development: a systematic review. Early Hum Dev. (2024) 192:106009. doi: 10.1016/j.earlhumdev.2024.106009
18. Moog NK, Nolvi S, Kleih TS, Styner M, Gilmore JH, Rasmussen JM, et al. Prospective association of maternal psychosocial stress in pregnancy with newborn hippocampal volume and implications for infant social-emotional development. Neurobiol Stress. (2021) 15:100368. doi: 10.1016/j.ynstr.2021.100368
19. Jeličić L, Veselinović A, Ćirović M, Jakovljević V, Raičević S, Subotić M. Maternal distress during pregnancy and the postpartum period: underlying mechanisms and child’s developmental outcomes: a narrative review. Int J Mol Sci. (2022) 23(22):13932. doi: 10.3390/ijms232213932
20. Manning KY, Long X, Watts D, Tomfohr-Madsen L, Giesbrecht GF, Lebel C. Prenatal maternal distress during the COVID-19 pandemic and associations with infant brain connectivity. Biological Psychiatry (1969). (2022) 92(9):701–8. doi: 10.1016/j.biopsych.2022.05.011
21. Weiner S, Wu Y, Kapse K, Vozar T, Cheng JJ, Murnick J, et al. Prenatal maternal psychological distress during the COVID-19 pandemic and newborn brain development. JAMA Network Open. (2024) 7(6):e2417924. doi: 10.1001/jamanetworkopen.2024.17924
22. Wu Y, Espinosa KM, Barnett SD, Kapse A, Quistorff JL, Lopez C, et al. Association of elevated maternal psychological distress, altered fetal brain, and offspring cognitive and social-emotional outcomes at 18 months. JAMA Network Open. (2022) 5(4):e229244. doi: 10.1001/jamanetworkopen.2022.9244
23. Papadopoulos A, Nichols ES, Mohsenzadeh Y, Giroux I, Mottola MF, Van Lieshout RJ, et al. Prenatal and postpartum maternal mental health and neonatal motor outcomes during the COVID-19 pandemic. J Affect Disord Rep. (2022) 10:100387. doi: 10.1016/j.jadr.2022.100387
24. Duguay G, Garon-Bissonnette J, Lemieux R, Dubois-Comtois K, Mayrand K, Berthelot N. Socioemotional development in infants of pregnant women during the COVID-19 pandemic: the role of prenatal and postnatal maternal distress. Child Adolesc Psychiatry Ment Health. (2022) 16(1):28. doi: 10.1186/s13034-022-00458-x
25. Khoury JE, Atkinson L, Gonzalez A. A longitudinal study examining the associations between prenatal and postnatal maternal distress and toddler socioemotional developmental during the COVID-19 pandemic. Infancy. (2024) 29(3):412–36. doi: 10.1111/infa.12584
26. Guardino CM, Dunkel Schetter C. Coping during pregnancy: a systematic review and recommendations. Health Psychol Rev. (2014) 8(1):70–94. doi: 10.1080/17437199.2012.752659
27. Levinson A, Lobel M, Preis H, Mahaffey B. Coping with subjective and objective stress during a pandemic pregnancy: implications for maternal mental health. Arch Womens Mental Health. (2023) 26(6):819–29. doi: 10.1007/s00737-023-01357-6
28. Moola S, Munn Z, Sears K, Sfetcu R, Currie M, Lisy K, et al. Conducting systematic reviews of association (etiology): the Joanna Briggs Institute’s approach. Int J Evid Based Healthc. (2015) 13(3):163–9. doi: 10.1097/XEB.0000000000000064
29. EvidencePartners. Risk of bias instrument for cross-sectional surveys of attitudes and practices contributed by the CLARITY Group at McMaster University. DistillerSR (2023). Available online at: https://www.distillersr.com/resources/methodological-resources/tool-to-assess-risk-of-bias-in-cohort-studies-distillersr (Accessed July 23, 2024).
30. Abdus-salam RA, Balogun RO, Lawal TV, Lawal OO, Lawal RO, Abdulmalik JO, et al. Assessment of anxiety and depression, and coping mechanisms during COVID-19 lockdown among pregnant women. Heliyon. (2022) 8(10):e10902. doi: 10.1016/j.heliyon.2022.e10902
31. Badon SE, Croen LA, Ferrara A, Ames JL, Hedderson MM, Young-Wolff KC, et al. Coping strategies for COVID-19 pandemic-related stress and mental health during pregnancy. J Affect Disord. (2022) 309:309–13. doi: 10.1016/j.jad.2022.04.146
32. Barbosa-Leiker C, Smith CL, Crespi EJ, Brooks O, Burduli E, Ranjo S, et al. Stressors, coping, and resources needed during the COVID-19 pandemic in a sample of perinatal women. BMC Pregnancy Childbirth. (2021) 21(1):171. doi: 10.1186/s12884-021-03665-0
33. Bayrampour H, Tsui MYE. Postpartum people’s experiences of and responses to the COVID-19 pandemic during the first year of the pandemic: a descriptive qualitative study. Womens Health. (2023) 19:17455057231157480. doi: 10.1177/17455057231157480
34. Crowe S, Sarma K. Coping with COVID-19: stress, control and coping among pregnant women in Ireland during the COVID-19 pandemic. BMC Pregnancy Childbirth. (2022) 22(1):274. doi: 10.1186/s12884-022-04579-1
35. Davis JA, Gibson LY, Bear NL, Finlay-Jones AL, Ohan JL, Silva DT, et al. Can positive mindsets be protective against stress and isolation experienced during the COVID-19 pandemic? A mixed methods approach to understanding emotional health and wellbeing needs of perinatal women. Int J Environ Res Public Health. (2021) 18(13):6958. doi: 10.3390/ijerph18136958
36. Dib S, Rougeaux E, Vázquez-Vázquez A, Wells JCK, Fewtrell M. Maternal mental health and coping during the COVID-19 lockdown in the UK: data from the COVID-19 new mum study. Int J Gynecol Obstet. (2020) 151(3):407–14. doi: 10.1002/ijgo.13397
37. Dol J, Hughes B, Aston M, McMillan D, Tomblin Murphy G, Campbell-Yeo M. Impact of COVID-19 restrictions on the postpartum experience of women living in eastern Canada during the early pandemic period: a cross-sectional study. J Nurs Scholarsh. (2023) 55(1):178–86. doi: 10.1111/jnu.12843
38. Firouzbakht M, Rahmani N, Sharif Nia H, Omidvar S. Coping strategies and depression during the COVID-19 pandemic in pregnant women: a cross sectional study. BMC Psychiatry. (2022) 22(1):153. doi: 10.1186/s12888-022-03792-8
39. Goldstein E, Brown RL, Lennon RP, Zgierska AE. Latent class analysis of health, social, and behavioral profiles associated with psychological distress among pregnant and postpartum women during the COVID-19 pandemic in the United States. Birth. (2023) 50(2):407–17. doi: 10.1111/birt.12664
40. Gómez-Baya D, Gómez-Gómez I, Domínguez-Salas S, Rodríguez-Domínguez C, Motrico E. The influence of lifestyles to cope with stress over mental health in pregnant and postpartum women during the COVID-19 pandemic. Curr Psychol. (2023) 42(26):22164–83. doi: 10.1007/s12144-022-03287-5
41. Han L, Bai H, Lun B, Li Y, Wang Y, Ni Q. The prevalence of fear of childbirth and its association with intolerance of uncertainty and coping styles among pregnant Chinese women during the COVID-19 pandemic. Front Psychiatry. (2022) 13:935760. doi: 10.3389/fpsyt.2022.935760
42. Khoury JE, Atkinson L, Bennett T, Jack SM, Gonzalez A. Coping strategies mediate the associations between COVID-19 experiences and mental health outcomes in pregnancy. Arch Womens Mental Health. (2021) 24(6):1007–17. doi: 10.1007/s00737-021-01135-2
43. Kiliç A, Gök K, Kökrek Z, Kapudere B, Tüten N, Bostancı MS, et al. The relationship of probable clinical anxiety with attitude-behaviour, coping styles and social support in healthy pregnant women during the late period COVID-19 pandemic. J Obstet Gynaecol. (2022) 42(7):2970–8. doi: 10.1080/01443615.2022.2124850
44. Kinser PA, Jallo N, Amstadter AB, Thacker LR, Jones E, Moyer S, et al. Depression, anxiety, resilience, and coping: the experience of pregnant and new mothers during the first few months of the COVID-19 pandemic. J Womens Health. (2021) 30(5):654–64. doi: 10.1089/jwh.2020.8866
45. LoGiudice JA, Bartos S. Mixed-methods study of the experience of pregnancy during the COVID-19 pandemic. J Obstet Gynecol Neonatal Nurs. (2022) 51(5):548–57. doi: 10.1016/j.jogn.2022.07.001
46. Mollons M, Levasseur-Puhach S, Kaur J, Doyle J, Giesbrecht G, Lebel CA, et al. Mixed-methods study exploring health service access and social support linkage to the mental well-being of Canadian indigenous pregnant persons during the COVID-19 pandemic. BMJ Open. (2024) 14(3):e078388. doi: 10.1136/bmjopen-2023-078388
47. Penengo C, Colli C, Cesco M, Croccia V, Degano M, Ferreghini A, et al. Stress, coping, and psychiatric symptoms in pregnant women in outpatient care during the 2021s-wave COVID- 19 pandemic. Front Psychiatry. (2022) 12:775585. doi: 10.3389/fpsyt.2021.775585
48. Preis H, Mahaffey B, Heiselman C, Lobel M. Vulnerability and resilience to pandemic-related stress among U.S. Women pregnant at the start of the COVID-19 pandemic. Soc Sci Med. (2020) 266:113348. doi: 10.1016/j.socscimed.2020.113348
49. Rimal SP, Thapa K, Shrestha R. Psychological distress and coping among pregnant women during the COVID 19 pandemic. J Nepal Health Res Counc. (2022) 20(1):234–40. doi: 10.33314/jnhrc.v20i01.4063
50. Spinola O, Liotti M, Speranza AM, Tambelli R. Effects of COVID-19 epidemic lockdown on postpartum depressive symptoms in a sample of Italian mothers. Front Psychiatry. (2020) 11:589916. doi: 10.3389/fpsyt.2020.589916
51. Timircan M, Bratosin F, Vidican I, Suciu O, Turaiche M, Bota AV, et al. Coping strategies and health-related quality of life in pregnant women with SARS-CoV-2 infection. Medicina (Kaunas, Lithuania). (2021) 57(10):1113. doi: 10.3390/medicina57101113
52. Werchan DM, Hendrix CL, Ablow JC, Amstadter AB, Austin AC, Babineau V, et al. Behavioral coping phenotypes and associated psychosocial outcomes of pregnant and postpartum women during the COVID-19 pandemic. Sci Rep. (2022) 12(1):1209. doi: 10.1038/s41598-022-05299-4
53. Carver CS. You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med. (1997) 4(1):92–100. doi: 10.1207/s15327558ijbm0401_6
54. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166(10):1092–7. doi: 10.1001/archinte.166.10.1092
55. Simpson W, Glazer M, Michalski N, Steiner M, Frey BN. Comparative efficacy of the generalized anxiety disorder 7-item scale and the Edinburgh postnatal depression scale as screening tools for generalized anxiety disorder in pregnancy and the postpartum period. Can J Psychiatry. (2014) 59(8):434–40. doi: 10.1177/070674371405900806
56. Cox J, Holden J, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. (1987) 150(6):782–6. doi: 10.1192/bjp.150.6.782
57. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24(4):385–96. doi: 10.2307/2136404
58. Chaaya M, Osman H, Naassan G, Mahfoud Z. Validation of the Arabic version of the Cohen perceived stress scale (PSS-10) among pregnant and postpartum women. BMC Psychiatry. (2010) 10(1):111. doi: 10.1186/1471-244x-10-111
59. García FE, Barraza-Peña CG, Wlodarczyk A, Alvear-Carrasco M, Reyes-Reyes A. Psychometric properties of the brief-COPE for the evaluation of coping strategies in the Chilean population. Psicol Rreflex Crit. (2018) 31(1):22. doi: 10.1186/s41155-018-0102-3
60. Vitorino LM, Chiaradia R, Low G, Cruz JP, Pargament KI, Lucchetti ALG, et al. Association of spiritual/religious coping with depressive symptoms in high- and low-risk pregnant women. J Clin Nurs. (2018) 27(3-4):e635–42. doi: 10.1111/jocn.14113
Appendix A: Critical appraisal: evidence quality
Critical appraisal of evidence quality was completed using the JBI cross-sectional and qualitative study appraisal tools.For quantitative and mixed methods studies the scores representative of a study providing high-quality evidence is 7+ and or qualitative studies the scores representative of high-quality evidence is 9+.
Appendix B: Critical appraisal: risk of bias
Critical appraisal of the studies for risk of bias was completed using a modified version of the McMaster CLARITY Group's Risk of Bias assessment tool.Indicators of a high risk of bias included: non-probabilistic sampling methods, study instruments lacking established evidence of validity and reliability, response rates of less than 75%, and missing data rates of greater than 15%.
Appendix C: Recommendations: coping styles & strategies
Recommendations for coping strategy use amongst perinatal individuals during natural disasters or similar situations, based on research from the COVID-19 pandemic.
Keywords: perinatal, distress, coping, COVID-19, depression, anxiety
Citation: Papadopoulos A and Duerden EG (2025) Coping styles, strategies and psychological distress amongst perinatal individuals during the COVID-19 pandemic: a rapid review. Front. Glob. Women’s Health 6:1666741. doi: 10.3389/fgwh.2025.1666741
Received: 15 July 2025; Accepted: 31 October 2025;
Published: 13 November 2025.
Edited by:
Chonnakarn Jatchavala, Prince of Songkla University, ThailandReviewed by:
Thammanard Charernboon, Thammasat University, ThailandRapphon Sawaddisan, Prince of Songkla University, Thailand
Copyright: © 2025 Papadopoulos and Duerden. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Emma G. Duerden, ZWR1ZXJkZW5AdXdvLmNh
 Alissa Papadopoulos
Alissa Papadopoulos Emma G. Duerden
Emma G. Duerden