- Simon Business School, University of Rochester, Rochester, NY, United States
Type 1 diabetes is an invisible disability requiring major life changes and constant monitoring. It can become particularly challenging to control during a major life transition. This study examines the composition and nature of the social networks of college students living with type 1 diabetes. A total of 17 respondents with type 1 diabetes and 18–25 years of age participated in network interviews. Network Canvas facilitated online data collection. The results show that efforts to protect the wellbeing of college students with T1D require active participation of university organizations and certain individuals from students' formal and informal connections. Such connections define students' support networks in college and provide access to social capital. Practical implications and recommendations for university leadership and students' parents are discussed.
Introduction
Type 1 diabetes (T1D) self-management requires immense lifestyle changes, including diet modification, constant blood glucose monitoring, and insulin administration, to reduce the chance of life-threatening complications (Gannoni and Shute, 2010). Thus, it can be especially challenging to maintain while transitioning through life stages (Hanna, 2012). During emerging adulthood (age 18–25), young adults with T1D experience many changes, including moving out of parental homes and enrolling in college. Moving to a college far from home may be the first time for a young adult with T1D to take responsibility for all the aspects of their diabetes care.
This period is associated with psychosocial and emotional challenges (Weitzman et al., 2020), where diabetes care omissions often occur (Chiang et al., 2014). T1D affects all aspects of college life and complicates college living, impacting the students' physical and emotional wellbeing with T1D. However, despite potential severe health risks caused by a lack of proper diabetes self-care (Balfe and Jackson, 2007), little is known about emerging adults embarking on a new higher education journey and transitioning to unfamiliar organizational environments. Thus, this study aims to fill this gap in research by exploring the composition and nature of students' social environment in college, focusing on social support and its effect on diabetes self-management.
Network theory and social support
In network theory, the interconnectedness between network members is the mechanism that enables action, meaning that the interactions rather than other factors primarily define behaviors and outcomes (Borgatti and Halgin, 2011). Those interactions are activated through communication. Every day, people shape the interactions they are involved in through the mutual construction of conversations that lead to other forms of exchange, such as conflict (e.g., Harrison, 2007), support (e.g., Chewning and Montemurro, 2016), or interorganizational collaborations (Doerfel et al., 2010). Research has shown that social capital can be useful for achieving specific material outcomes, such as finding a job (e.g., Mouw, 2003) or promotion (e.g., Burt R. S., 2000), and health outcomes that depend on social support (e.g., Brashers et al., 2004). In its core, social capital provides social support through social ties with certain patterns of social ties generating greater benefits to the embedded actors (Burt S., 2000).
As a component of social capital, social support has been identified as an important factor in managing health issues (Brashers et al., 2004). It operates through several major mechanisms, such as instrumental, emotional, informational, and appraisal aid (Gottlieb and Bergen, 2010; Taylor, 2011; Thoits, 1995). The social support perspective mainly examines the quality and content of personal social ties rather than the structure of ties and defines them as attributes of resources available to individuals (House et al., 1988). Thus, the goal for social support researchers is to identify how patterns of interactions in personal networks affect the flow of resources to the individual and affect outcomes of interest. As flexible structures, support networks are created by individuals. Moody and Paxton (2009) argue that social capital and social networks provide better predictions when used together because “full specification of theory in the social capital field requires attention to the structure of social networks. Simultaneously, the full specification of theory in the social networks field requires attention to the content of social capital” (p. 1496). Thus, the current study has two goals. First, to explore the composition students' social networks in the context of T1D management. Second, to determine the nature of social capital students access and utilize in college. The overarching aim is to construct a picture of students' social reality and understand its influence on organizational assimilation and diabetes management.
T1D and social ties
Both network structures and social support elicited from them are widely described determinants of health experience and outcomes (Perry and Pescosolido, 2015). They are reported to strongly influence health outcomes by affecting health-related behaviors (Christakis and Fowler, 2007; Väänänen et al., 2008). Social interaction through communication is a central mechanism linking social networks and health, with resource flow for managing illness through communication networks providing advice, information, emotional support, and affirmation (Perry and Pescosolido, 2015). The extent to which people can successfully activate communicative ties and thus secure access to necessary resources can affect individual wellbeing and explain the role of social network characteristics in this process (Perry and Pescosolido, 2015). How much benefit the social network resources can provide depends on activating proper ties with the necessary type of aid (Lin, 1999). People tend to utilize their social network ties when they do not have enough personal resources to cope with the consequences of the illness themselves (Schwarzer and Leppin, 1991). As a result, what members of social networks (e.g., communications in an emergency, emotional problems, or material help) are mobilized is an important factor in response to illness (Perry and Pescosolido, 2015). Young adults with health conditions like T1D have complex illness management needs coupled with the drive to pursue educational and personal goals. To ensure that these young individuals are adequately supported during their transitions, a strong network of support is crucial (Johnston et al., 2016). While in certain non-health-related instances, people solely rely on close relationships for support (e.g., Rienties and Hosein, 2020), for young adults with a chronic illness, organizational support might be vital to enhance wellbeing.
College students are expected to cope with T1D by activating communicative ties with people and organizations that possess relevant knowledge, recommend or provide treatment, and provide emotional, informational, and instrumental support. In addition, the network structure helps define the context in which all network interactions occur and has implications for the type of information exchanged among its members. Coleman (1988) notes that social capital lies in “information channels.” This notion of information channels refers to the connections that help people find relevant information. For example, if a student is registered with the Office of Disability Services, which accumulates relevant information about college policies regarding T1D. In that case, a student has a reduced need for additional information seeking. Thus, through information channels, people receive information that could later influence or lead to action (Coleman, 1988). Communicative practices with people from one's social environment can facilitate the flow of information and provide the individual with useful information about opportunities and choices previously unavailable (Lin, 1999). Such interactions are especially valuable in times of uncertainty (transition to college) and health crises (Brashers et al., 2004; Perry and Pescosolido, 2015). Thus, in a college social environment rich in social capital, students are more likely to rely on individuals and organizations for support. For example, they may seek emotional support from a college counseling center or borrow glycose test strips from other students with T1D. In a social environment poor with social capital, however, students may experience gaps in their social support network structure that may adversely influence social support availability and individual health outcomes. However, existing literature does not inform what formal and informal social support sources benefit students and whether the nature of activated ties influences diabetes self-management. Thus, the following research questions assess the importance of formal and informal social support sources in students' lives.
RQ1: What kind of formal social support do students with T1D need in college?
RQ2: What kind of informal social support do students with T1D need in college?
Young adults with T1D want to live as regular college students. However, while moving away from home, students become disconnected from their local medical and support systems and may not have immediate access to all necessary services (Hanna, 2012). As a result, negative health consequences, including death, may occur. The mortality of young people with T1D is much higher than that of the general population (Laing et al., 2005). For example, Strachan et al. (2000) describe the tragic outcome of two fatal cases of students with T1D during their first term at college. Their report highlights the vulnerability of students with T1D when they move from their parental home and start college life (Strachan et al., 2000).
The authors conclude that to improve the situation, health professionals and college authorities must do everything possible to protect the safety of students with T1D and improve T1D care in the college environment. From a social network perspective (Coleman, 1988), social capital includes social organizations established to facilitate specific processes and actions. The connections essential for students' wellbeing are not limited to family members and peers but also extend to health, dining, sport, and counseling college centers, disability services offices, student associations, and Greek-letter organizations. Such connections define students' support networks and provide access to social capital vital for self-management and quality of life. In contrast, specific constraints (e.g., gaps in communication between students and focal system members) of the support structure may adversely affect those outcomes. Social capital impacts health by bolstering social support and providing access to resources, which affects attitudes and behaviors responsible for positive health outcomes; these social processes then affect health-related behaviors, eventually impacting individuals' health (Kawachi and Berkman, 2001). Hence, the efforts to protect the wellbeing of college students with T1D require the active participation of diabetes healthcare professionals, college organizations, peers, families, and students themselves (Chiang et al., 2014). Most colleges have a disability services office that assists students with disabilities, including specific accommodations and modifications. Effective communication with this office can facilitate a smooth transition to college and, as a result, help avoid omissions in diabetes care. Another important communication tie to establish is a student health clinic where a professional health team can effectively manage T1D. In contrast with schools, colleges are not required to have trained T1D personnel. Peer connections are important for all students, but for students with T1D, they may be vital in emergencies when someone needs to administer glucagon (a hormone treating severely low blood sugar) (Gordon et al., 2011). It can also help if they know other students with diabetes who can assist and provide the necessary support. All these connections define the support network of a student with T1D. However, it is unclear whom students with T1D include in their social support network and what elements of this system impact diabetes management and diabetes-related quality of life. The following research question addresses this issue.
RQ3: What kind of ties do students with T1D activate to maintain effective diabetes self-care and diabetes-related quality of life?
Method
Participants
Study participants were recruited from the College Diabetes Network (CDN). The CDN is a non-profit organization helping young adults with T1D with their life-changing transition to college by building social capital and resource platforms and seeking to achieve positive health outcomes through information sharing, resources, and social support. The inclusion criteria for this study were (1) a diagnosis of T1D, (2) an emerging adult (age of 18–25 years), and (3) a student residing on campus or living independently/with roommates. A total of 17 informants participated in the study. The participants reported ages ranged from 19 to 25 years, and the reported time with diabetes ranged from 8 months to 16 years. Most participants self-identified as female (n = 14), followed by male (n = 2) and transgender female (n = 1). All participants were from different areas of the United States. Regarding ethnicity, most participants self-identified as White (n = 13), followed by Hispanic (n = 2), Black (n = 1), and Asian (n = 1). Most participants were sophomores (n = 7), followed by juniors (n = 5), seniors (3), freshmen (n = 1), and graduate students (n = 1).
Approach
Data was collected using an egocentric approach. It focuses on individuals in a network and their external connections. Personal acquaintances, group memberships, and types of relationships define this approach (Coleman, 1988). As Hanneman and Riddle (2005) notice, examining variation in individuals' behavior requires an understanding of their local circumstances and how they are embedded in the social structures, which is the point of the egocentric approach. Generally, the egocentric approach is much less limiting than sociometric because ego network research allows us to flexibly define the boundaries of personal networks per the stated research questions. Thus, the egocentric approach can elicit alters from different contexts compared to the sociometric approach, which is usually restricted to one domain. This study explores non-network outcomes as functions of network-based mechanisms (Perry et al., 2018; p. 196) and uses an egocentric model to gather personal network information among college students with T1D.
Procedures
Network data collection comes with major methodological challenges (Perry et al., 2018). Web-based name generators can be completed with little researcher involvement and help eliminate the problem of the interviewer effect (Eagle and Proeschold-Bell, 2015). However, self-report name-generating questions can be extremely taxing for participants, especially when individual networks are large (McCarty et al., 2007). In response to such concerns, ego network data collection tools have begun incorporating rich visual components and response methods designed to be more interactive and keep respondents engaged. For example, Network Canvas (Birkett et al., 2021) is a novel interactive tool developed specifically for egocentric data collection, which combines researcher-controlled face-to-face data collection supported by rich interactive visuals to enhance respondents' attention.
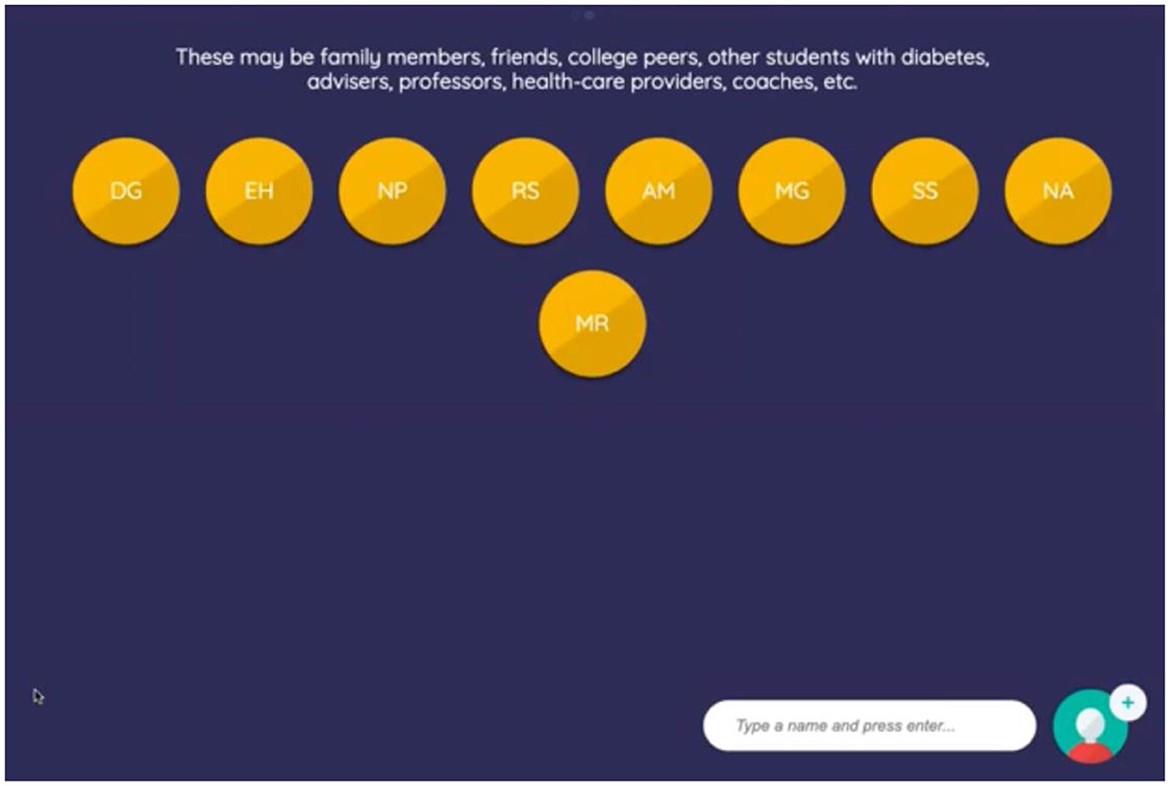
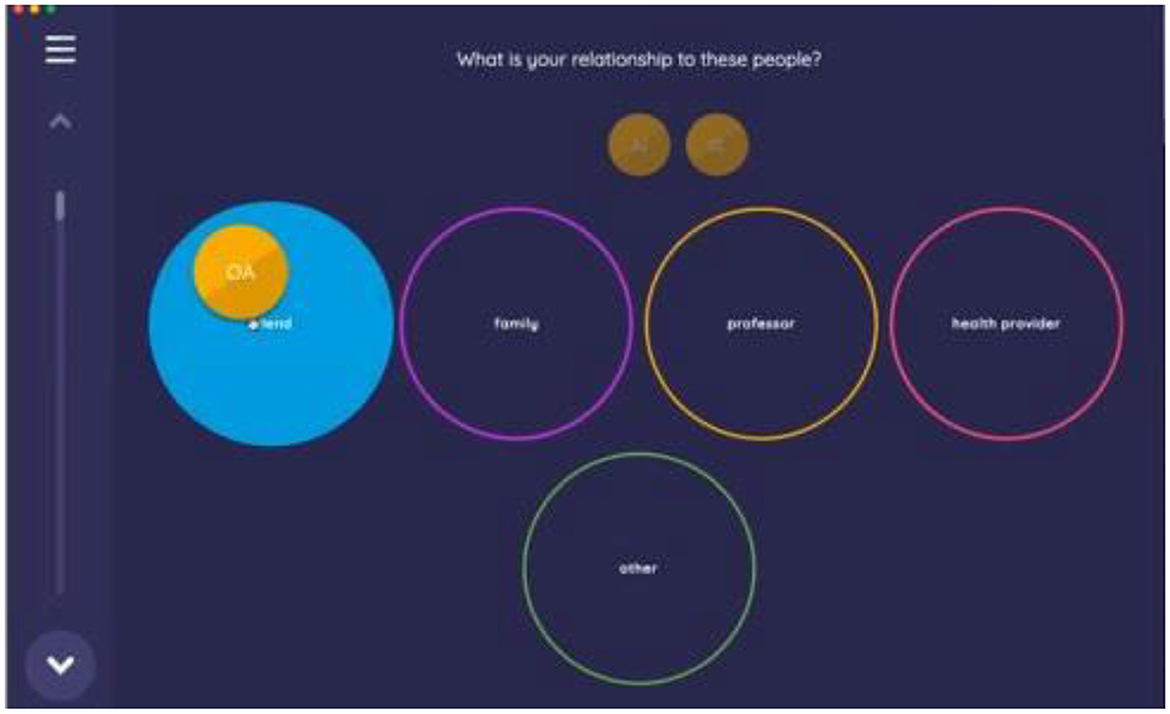
Participants were introduced to the software and asked to request remote control over the researcher's screen in Zoom. Thus, participants independently manipulated the app features while the researcher controlled the process, asked questions relevant to the study's research aims, and answered participants' questions when needed (see Figures 1, 2).
Participants were initially asked to list up to 10 individuals who had significantly impacted their lives since moving to college by entering a person's name or initials and clicking “enter.” Once the list of connections was compiled, name-interpreting questions were used to further explore the participants' diabetes networks. To streamline the process and avoid overwhelming participants with separate questions for each network member, the protocol included name interpreter questions that requested attributes for all network members at once. For example, participants were asked, “What is your relationship to these people?” and instructed to drag and drop the circles containing each person's name into a response box corresponding to categories such as friend, family, professor, healthcare provider, or other (with an option to type the answer).
Following this, social support questions were introduced. The interviewer guided participants in categorizing the individuals and organizations within their network based on the type of social support they provided. During this process, the interviewer also inquired about the context of the support, the meanings participants attributed to these experiences, and the reasons for assigning each individual or organization to a specific category. Participants were then asked to provide examples of the emotional, instrumental, and informational social support they received.
This process was repeated for formal social support networks, where participants identified organizations that had contributed to their success in college by providing various types of support. As part of the data collection, participants were required to specify individuals by providing names or initials and to name the organizations they mentioned (e.g., sorority, CDN). They were then asked to clarify their relationship with each named individual (e.g., “friend with T1D”) and to provide an explanation and example of the support received from individuals and organizations.
This detailed information was essential for accurately categorizing and coding the individuals and organizations into the predefined categories discussed in the manuscript. The analysis, therefore, focuses on a bipartite network structure, where two distinct types of nodes—individuals and organizations—are represented. These connections are depicted differently within the network to highlight the diverse support systems within the student body. This bipartite network model effectively showcases the complexity and richness of the social support structures analyzed in this study.
Analysis
All categories of network members were evaluated in-depth regarding the various types of support they provided. First, a taxonomic analysis of each subject's social support network was conducted guided by Spradley (1979)'s method to discover the composition of students' diabetes-related social support system. Interview transcripts and video recordings were uploaded to NVivo for coding and analysis. Structural questions about networks' composition elicited major categories of network members, and a taxonomy of students' formal and informal support systems was developed. A taxonomy can be developed as a box diagram, a set of lines and nodes, or an outline (Spradley, 1979, p. 148). In this study, the internal structure of major domains was outlined using the taxonomic analysis technique. Then, the componential analysis was employed, a systematic search for the significant components associated with researched cultural symbols. This study's product of componential analysis was a detailed description of (1) the participants' social environment composition and (2) the cultural meaning attributed to diabetes-related social support phenomenon.
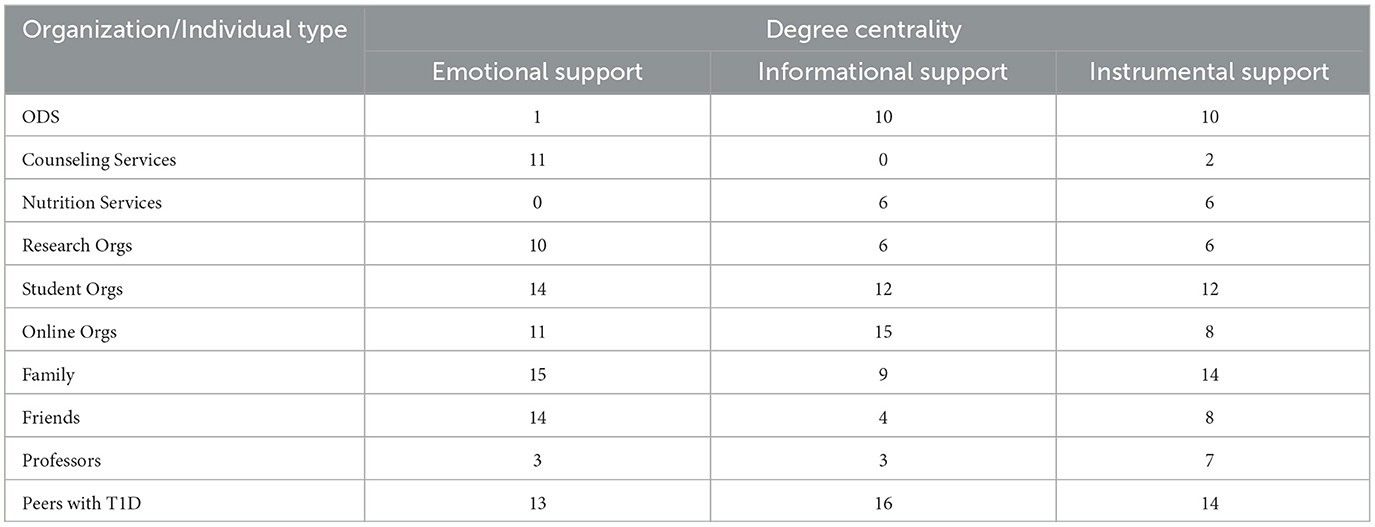
In addition, a network was constructed to visualize the social structure of students' support systems and access the centrality of its components. Interview data were used to guide the network visualizations. Based on participants' reported connections, support networks were created in UCINET (Borgatti et al., 2002). Network visualizations were performed for three types of social support separately, including emotional (Figure 3), informational (Figure 4), and instrumental (Figure 5) support.
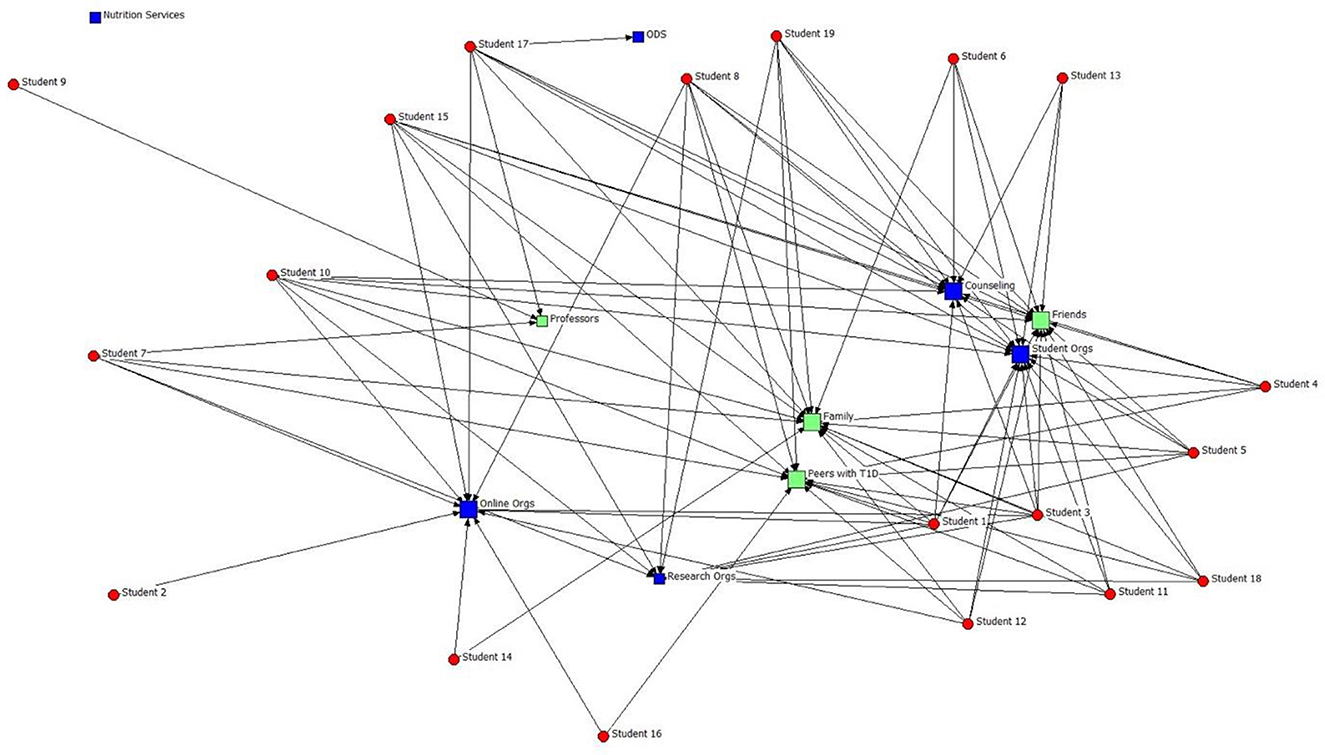
Figure 3. Emotional Support Network with 10 alters. Red: students (egos); Blue: organizations (alters); Green: individuals (alters). The size of the blue and green nodes represents the category importance in terms of instrumental support.
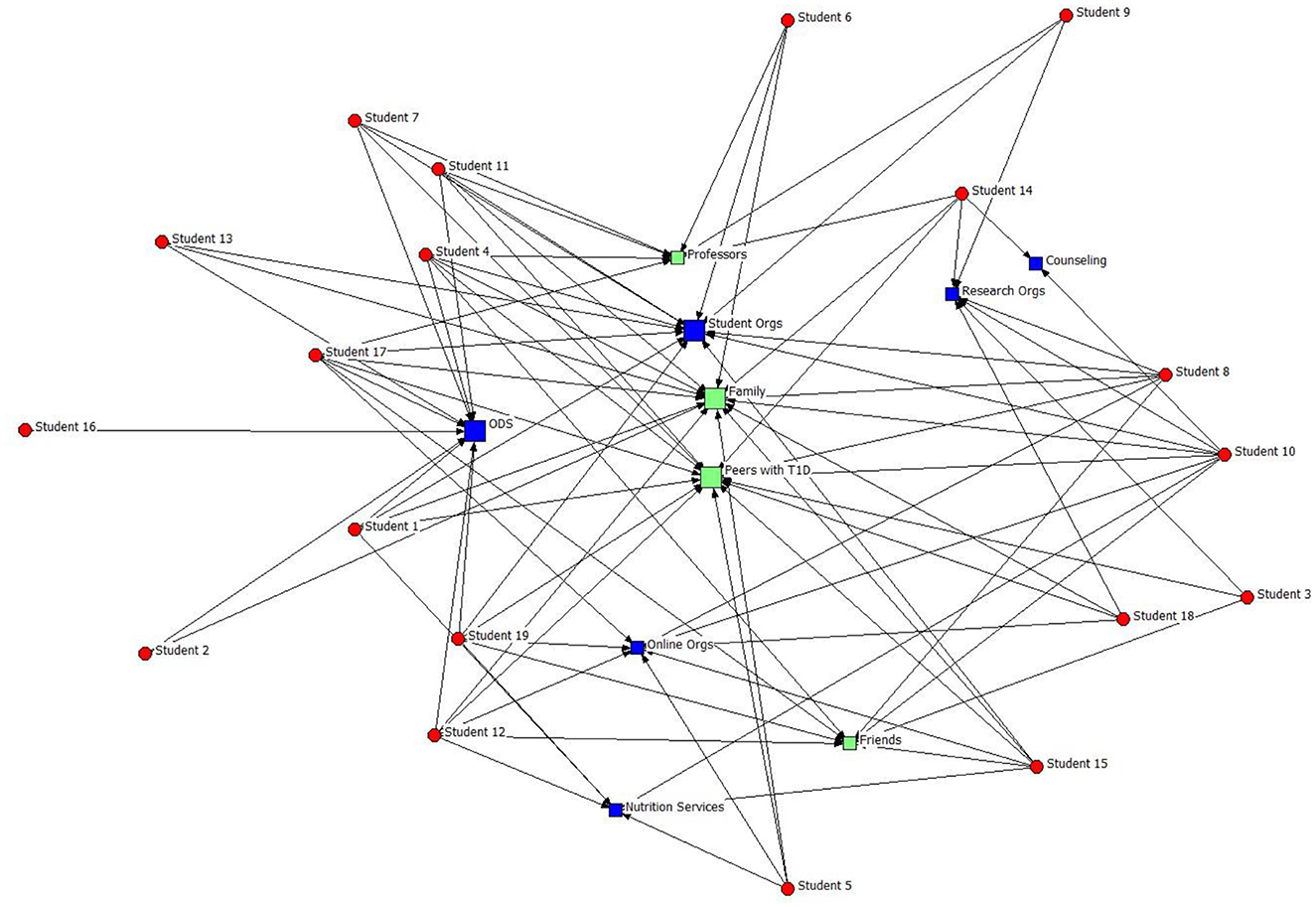
Figure 4. Informational Support Network with 10 alters. Red: students (egos); Blue: organizations (alters); Green: individuals (alters). The size of the blue and green nodes represents the category importance in terms of instrumental support.
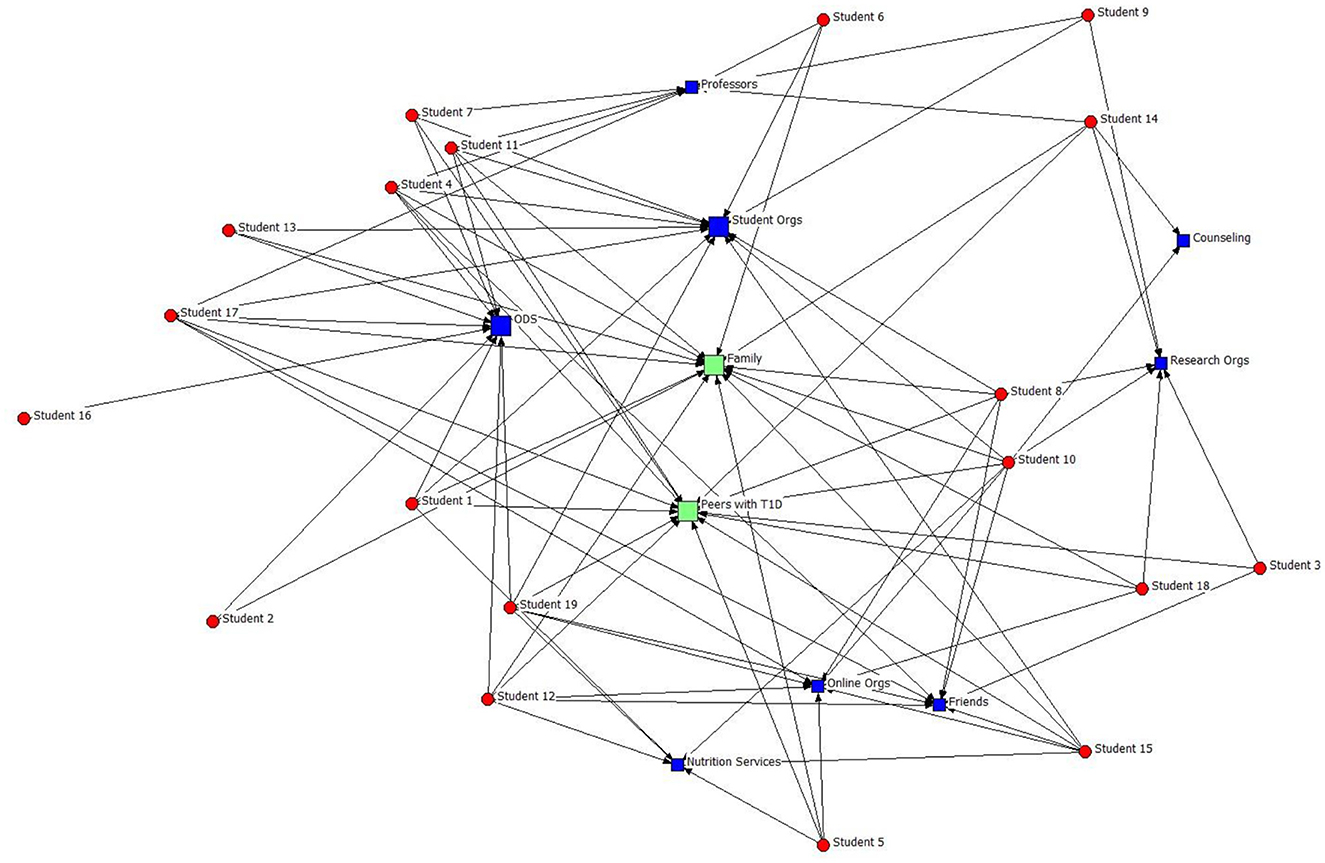
Figure 5. Instrumental support network with 10 alters. Red: students (egos); Blue: organizations (alters); Green: individuals (alters). The size of the blue and green nodes represents the category importance in terms of instrumental support.
Centrality
Centrality analysis in UCINET was used to assess the connections named by participants. The degree centrality of a node is the number of edges related to this node (Borgatti and Everett, 1997). It means that the degree of an alter is the number of egos who mentioned it. Those categories reported most frequently have a higher degree of centrality and thus are seen by students as important because they represent the most supportive organizations/individuals in a network. A more peripheral location means that a connection was mentioned fewer times by participants in regard to social support.
Results
RQs 1–2 explored the composition of students' support networks and types of support provided by formal and informal connections. Disability services, counseling services, nutrition services, research centers and institutes, student groups, and online communities were reported by participants to constitute their formal social support networks. The median formal diabetes network size consisted of four connections. Family, friends, peers with type 1 diabetes, roommates, and professors were reported by participants to constitute their informal social support networks. The median informal diabetes network size consisted of eight connections.
Formal social support
RQ 1 asked about the kinds of formal (organizational) social support students with T1D need in college. Participants' experiences highlighted the importance that many of them placed on using services provided by the college to students with T1D. Overall, different types of social support, including instrumental, informational, and emotional, were provided to students by various campus-based and online organizations.
Office of disability services
First, 9 students mentioned the Office of Disability Services (ODS) as an essential source of diabetes-related information and tangible help. ODS's informational support promoted early class registration, flu shots, nutritional programs, and available accommodations. ODS's instrumental support included letters of accommodation sent to professors, classroom modifications, living accommodations approvals, priority class registration, and diabetes supply storage.
I had to register with my school's disability services just because my blood sugar could fluctuate at any time for any given reason, and that could affect my academic performance (Mary, 20 y.o., female).
Specifically, 5 participants acknowledged that registering with ODS “gave extra flexibility” in class (e.g., phone use, ringer on, food, water, etc.). However, 6 students mentioned some challenges related to communication with ODS.
I was trying to get a single because freshman year, my roommate actually took me to a meeting with the RA [resident assistant] because me giving myself insulin at night would wake her up. I do not know how. She was just a very sensitive sleeper, and she had her own issues, but she convoluted it, so it was basically my fault giving myself insulin. That was a big fight, and I was really afraid. I tried, I asked them to give me a single [room] since obviously my diabetes is negatively affecting someone else's life. They said no. It was not a valid enough excuse to get a single (Angela, 19 y.o., female).
Ella (24 y.o., female) also expressed concerns that ODS tended to “single out people who have physical disabilities rather than invisible disabilities” and thus was “less adapting to students with diabetes.” For this reason, she recognized that “people with diabetes have to really advocate for what they want and make demands because otherwise, you would not get that.” A similar concern shared by 5 participants was related to the amount of required documentation necessary to register with ODS or request accommodations. Students reported starting the application process and not finishing because it was complicated or rejected due to missing documents or errors.
I had to start all over again, and it was just very difficult, so one of my professors helped me fast-track it so that I could get the accommodations (Tom, 22 y.o., male).
Counseling services
For all participants, ODS was not the only source of support. For example, 11 students reported that counseling services provided by the university helped them cope with emotional challenges right after transitioning to university life and over time.
They [the university] offer free counseling services for students and faculty with T1D, so I have taken use of that before. It is very nice (Alice, 23 y.o., female).
When asked about specific aspects of emotional challenges, most (n = 14) acknowledged the anxiety stemming from the need to manage T1D in college and constant worry about “highs and lows” that “spreads to other areas of life.” (Susan, 19 y.o., female)
Nutrition services
A total of 6 participants reported using university-provided nutrition services for tangible support that helped them control T1D, including dietician consultations, nutrition clubs, and cooking classes. Students who took advantage of personalized nutrition and wellness plans created by a Registered Dietitian reported feeling confident in their ability to eat healthily and control blood sugar fluctuations.
She definitely helped me a lot to get clarity toward the foods that I should be avoiding and the foods that I should be ingesting more of. It helped because I am sort of a picky eater, but she was able to help me provide substitutes for certain foods that I did not like. It was a very good experience (Paul, 20 y.o, male).
During the interviews, some participants (n = 6) were surprised to learn about nutrition services' presence on certain campuses and expressed willingness to use them if an opportunity becomes available.
Research centers and institutes
A total of 8 participants noted that having diabetes-focused research centers and institutes on campus helped students feel more connected to their university and access necessary social support, including emotional, tangible, and informational support. For example, students reported getting internships in diabetes research labs and feeling appreciated for having a life experience with the disease in addition to the necessary qualifications.
I am at […] university, and we do have a Diabetes Institute, so I feel like that helped make it a little more accessible and friendly for students with diabetes because they are pretty engaged. It is mainly their research enter (Kaley, 22 y.o., female).
Student groups
Many participants (n = 14) noted that various student groups located on campus provided necessary social support. When asked about specific organizations providing emotional, instrumental, and informational support, students named sororities/fraternities, student coalitions (e.g., the Coalition of Black Students), Residence Hall Associations, and College Diabetes Network (CDN) Chapters; 11 students acknowledged that the CDN Chapters on campus were of immense help in all aspects of peer support.
I started a chapter when I was diagnosed. So far, I have recruited about only three people. One of them is in my fraternity and the other is Alice (name changed for privacy). Those two together have been such an immense help for me. If I forget to order my prescription and they have the extra insulin that I need… I don't know, they are always there for me emotionally (Leila, 22 y.o, female).
Moreover, 4 students reported that they only wanted to attend a college with a CDN chapter. They reported relying on CDN's informational recourses while preparing for higher education transition and acknowledged the importance of T1D support groups after transitioning.
When I was looking into colleges, and I was looking at [university name], I checked to see if they did have a College Diabetes Network before making my official decision to go there (Tanya, 19 y.o., female).
First, CDN chapters helped them overcome challenges related to diabetes supplies by offering instrumental support; 7 participants reported borrowing continuous glucose monitors, insulin pens, and extra insulin when the pumps were ripped off by accident or while waiting for insurance approval and prescription delivery. Second, 9 participants noted that since not all their friends understood what it meant to live with T1D and the pressure it puts on a person, they appreciated the emotional support provided by CDN members. Students reported sharing stories and laughing, which helped alleviate their stress and anxiety. Lastly, 7 participants noted that CDN members shared vital informational support by sharing essential information about available university services and accommodations, which otherwise would have remained unknown. For example, one student reported not knowing about T1D accommodations until connected to CDN. However, the information about the presence of CDN Chapters on campuses was also only sometimes readily available to students.
I think there are support resources, but they are kind of hidden. I knew back in high school that I wanted to join the CDN, but most people do not know what it is, so I wish they would change that to be more visible (Paul, 20 y.o, male).
Online communities
Lastly, 11 participants reported relying on online social support from various organizations in addition to university-provided services; 5 students recognized that sharing personal feelings about diabetes stress was easier online in dedicated Facebook groups. The same 5 students reported being a part of Tik Tok and Twitter communities and receiving informational and emotional support from them. For those participants who did not want to build close personal connections but wanted to ask “general questions” and “stay connected,” online communities were the first choice.
I am excited to post there when I hit my 3 years. My “diaversary” is what we call a diabetic anniversary. I will post it in there with a picture of me and my devices showing to celebrate, you know, 3 years (Susan, 19 y.o., female).
In addition, 5l students had taken the opportunity of starting a CDN Chapter on campus and recruited other students with T1D to join the group. They expressed gratitude to CDN for providing funding and scholarships for college students with T1D.
They [CDN] were fantastic, and a couple years ago, they had a scholarship for students to go to diabetes conferences, and I won one of them. I was able to go to the American Association of Diabetes Educators conference. I represented the organization there, and so that was pretty fun (Kathy, 22 y.o., female).
Informal support
RQ2 asked about the kinds of informal social support students with T1D need in college.
Family
All students who attended out-of-state colleges admitted that moving away from parental homes was the hardest transition due to the lack of familiarity with the new environment and difficulty managing diabetes routine. Those participants were disconnected from constant family support but relied on parents' remote help. First, 15 participants acknowledged that they routinely turned to parents for emotional support by calling them to talk about academic life, relationships, and “to vent.” Second, in terms of instrumental support, 10 participants recognized that their parents were usually the first choice for issues with insurance coverage and financial questions. Family members also assisted in diabetes management, including meal planning and glycose level control.
When I was first diagnosed, I used a nutritionist for the dining halls. My father was the one who is super concerned about me and my health, so he arranged a meeting between the two of us (Tom, 22 y.o, male).
Lastly, 9 students who used Dexcom, a continuous glucose monitoring system for diabetes management, indicated that their parents followed glucose levels in the app and received phone alerts when students' blood sugars dropped low.
My mom normally wakes up because she has my Dexcom alerts on her phone as well, and then she will call me until I wake up. One time she had to call the housing director, and they came up to my room (Hailey, 21 y.o., female).
However, since parents could no longer control their children's diabetes management, participants reported activating other connections for additional social support in college.
Friends and roommates
Most participants (n = 14) recognized their roommates as essential individuals in emergencies; having someone familiar with participants' status and needs provided “security and confidence.” Roommates who knew where to find emergency supplies and juice boxes, who were not disturbed by Dexcom alarms going off at night and were trained to administer glucagon by participants were considered “the best.” All participants agreed that glucagon administration was the most important issue to discuss with roommates. While some expressed gratitude to their friends for administering the correct amounts of insulin when unconscious (n = 5), others (n = 4) voiced concerns and reported being in “constant worry.”
I have to teach all of my friends how to use glucagon. When I ask them a month or so later, “do you remember how to use it,” nobody ever remembers how to use it, which is scary because then I am the one that is going to have a seizure. I do not want everybody to be thinking about it always because I would not wish that on my worst enemy, but if I am in trouble, I do need it to be on their mind (Tanya, 19 y.o., female).
Professors
Several participants (n = 5) indicated that they received the most support from professors directly or indirectly involved in diabetes research.
I started working in a T1D lab with a professor who was really passionate about that, and they were big support as well (Kaley, 22 y.o., female).
Others (n = 2) explained that professors helped handle the disability accommodations. For example, some professors called Disability Services and helped with the application submission process and paperwork. Most participants (n = 12) agreed that the best thing professors could do is simply be aware of students' health needs and understand that sometimes diabetes is out of an control.
Peers with T1D
Most participants (n = 16) acknowledged that having other people with T1D in their support system was crucial for successful diabetes management and emotional stability. One participant noted that “it is definitely better knowing diabetic friends.” Several participants (n = 7) indicated that their closest friendships started from diabetes.
I was in a lab class and did not have a partner, so I was paired up with the senior. We do not have anything in common, and he just looks like he does not want to be sitting with me. I am eating because my blood sugar was low, and he was like, “you are brave for eating in the lab.” I said, “well, I am diabetic, so if they have an issue with it, they should bring it directly to me,” and then he pulled out his pump and said that he was diabetic too. We became really good friends (Averly, 21 y.o., female).
Several (n = 11) acknowledged that sometimes it was hard to explain things to people who do not have diabetes, and that is when peers with diabetes became of immense help. For example, given that most people with T1D try to keep a certain food routine, dining with other T1D people released the participants from the pressure of “counting carbs under the table” and “explaining how diabetes works.”
Diabetes is a very important part of my identity, so I do like to connect with other people who have it. I am the only one in my family that has it, which is actually quite odd because it is genetic, so it is really nice to share stories and just laugh about it (Susan, 19 y.o., female).
Network composition
RQ3 explored the ties that students activate to maintain effective diabetes self-care and diabetes-related quality of life. Network visualizations (Figures 3–5) show the most important organizational/individual components in students' networks regarding access to three types of resources. Visualization of students' formal and informal networks allowed for examining supportive communication network composition and the implications that such connections held for the flow of information or other resources in students' networks. The number of organizations with a high degree of centrality reflects the tendency of students to seek formal support services provided by universities. Specifically, the high degree centrality of organizations such as ODS, student organizations, counseling services, and online organizations in students' formal networks shows that these entities constitute a core support system for students. Similar to formal support, the number of individuals with a high degree of centrality in students' networks reflects the tendency of students to rely on informal diabetes-related support. Specifically, the high degree centrality of peers with T1D, family, and friends in students' informal networks shows that these people provide the most diabetes-related support. Overall, the student networks reflect a diversity of supportive partnerships, including the ODS, counseling services, nutrition services, research organizations, student groups, online organizations, family, friends/roommates, professors, and peers with T1D.
Discussion
This study explores the composition of students' social networks in the context of T1D management and determines the nature of social capital available in college. It presents a picture of students' social reality and its influence on organizational assimilation and diabetes management. In line with the previous research showing connections between social networks and health (Perry and Pescosolido, 2015) and identifying social support as an important factor in managing heath issues (Brashers et al., 2004), this study findings suggest that diabetes management in college relies heavily on social support accessibility. Given that social capital impacts health by bolstering social support and providing access to resources, affecting attitudes and behaviors responsible for positive health outcomes (Kawachi and Berkman, 2001), this research extends the existing literature on diabetes management and social support by providing a unique perspective on specific components of students' supportive networks. Specifically, it illustrates how organizational support from different formal sources and informal support from certain individuals is activated through emotional, instrumental, and informational aid.
Network composition
In line with existing literature highlighting the complexity of diabetes care and its team-based nature (Chiang et al., 2014), findings from this study indicate that efforts to protect the wellbeing of college students with T1D require the active participation of university organizations and certain individuals from students' formal and informal connections. Specifically, family, friends, peers with type 1 diabetes, roommates, and professors were reported by participants to constitute their informal social support networks. Disability, counseling, nutrition services, research centers and institutes, student groups, and online communities formed participants' organizational social support networks. Such connections define students' support network in college and provide access to social capital (Lin, 1999), a vital resource for diabetes care and college adjustment.
Next, this study suggests a link between students' diabetes management and university-designed support system. Study results (see Table 1) demonstrate that students receive different kinds of social support from different sources. These findings suggest that universities' formal support systems might not be actually providing the forms of support they intended to and thus have important implications for practitioners. Social support is one of the six attributes of the institutional culture defining a “disability-friendly” campus (Wilson, 2010). In this study, respondents' perspectives provided a unique insight into supportive network connections on campus, constituting a “disability-friendly” campus in relation to independent diabetes self-management and quality of life. University leadership should strive to create a “disability-friendly” campus for students with T1D by addressing gaps in support and resources.
Nature of social support
The results supported the utility of both formal and informal connections in terms of successful diabetes management in college, showing their ability to provide resources through emotional, informational, and instrumental support.
First, this study findings illustrate that students cope with T1D by activating communicative ties with people and organizations that possess relevant knowledge. Social capital lies in information channels (Coleman, 1988) which can be defined in this context as connections that help students find relevant information. For example, if a student is registered with ODS, which accumulates relevant information about university policies regarding T1D, a student has a reduced need for additional information seeking. Thus, in line with the literature (Lin, 1999), this study illustrates that communicative practices with people from one's social environment can facilitate the flow of information and provide the individual with useful information about health-related opportunities and choices previously unavailable. Similar to formal support, students benefited from informational support provided by peers with T1D, including vital information about available accommodations and ODS services on campus. Thus, consistent with the literature (Coleman, 1988), students received information through various information channels that could later influence their health-related actions. As this study shows, such interactions are especially valuable in times of transition and uncertainty.
Second, this study results show that while students build new formal and informal network connections on campus, they still rely on the previously existing support system for emotional support. Previous research highlighted the prevalence of symptoms of depression and anxiety in young adults with T1D and suggested its potential negative influence on diabetes management and glycemic control (Buchberger et al., 2016). This study shows that the transition to higher education systems puts an additional burden on youth with T1D. Students need help coping with emotional challenges like anxiety and constant worry about diabetes self-care and its long-term effect on their health. Thus, universities should consider providing free counseling services for students with T1D to conduct a regular psychosocial assessment and facilitate their transition and adaptation to college. Another important practical implication of this study results is the presence of CDN chapters on campus. Overall, the vital role of CDN is in bringing students with T1D together and providing peer support. It might be that the pervasive impact of diabetes on daily life is hard to explain to people without the illness. Thus, students rely on peers with the same experiences and can relate to the challenges. University leadership should collaborate with CDN on establishing chapters on every campus to assist students with T1D.
Third, the need for instrumental aid for diabetes care is hard to underestimate, and universities should be actively involved in this process. Given that students with T1D may need various accommodations, they are usually required to submit such requests through different service groups. As the current study illustrates, one prominent example is ODS. Students with T1D may legally seek placement to access a kitchen and private space to perform diabetes self-care, have a refrigerator in the room, live close to a dining hall, health center, campus transportation, and classes (Gordon et al., 2011). In this study, ODS was an essential source of diabetes-related instrumental support, including letters of accommodation sent to professors, classroom modifications, living accommodations approvals, priority class registration, and diabetes supply storage. This study results indicate that an early-established relationship with the ODS facilitates college transition and might improve diabetes management in college.
In addition, while students might become disconnected from their previous support systems during transition to college, this study shows that they still rely on family members for instrumental support. It might be that most of the students in this study (age group 18–25) remained on their parents' health insurance plans, so it was natural for them to keep parents involved in the process of ordering diabetes supplies and scheduling doctor appointments. Thus, parents who take an active part in helping their children manage diabetes, might consider establishing connection with ODS or other services on campus (e.g., nutrition) to serve as brokers of social capital (Burt R. S., 2000).
In addition, this research demonstrates that students' social networks were organized by engaged ties processes (Doerfel, 2018). Engagement means a deeper level of involvement between people and organizations. Various communicative practices, including social support, facilitate it. As Doerfel (2018) argues, engagement involves diverse relationships that do not need to be centralized around one organization. Indeed, this study illustrates that students' relationships were complimentary and embedded within a larger organizational network comprised of a diverse collection of individuals, groups, and organizations. These relationships are essential to managing scarce resources and turbulent environments. Thus, student support networks were dispersed across different organizations depending on the type of aid they provided. In addition, while network structure provided insights into students' helpful connections, recognizing the nature and quality of the communication was a salient component of an engaged communication network of students with T1D. Although social capital research usually categorizes ties as bridging or bonding, the quality of the interactions in terms of engagement demonstrates the distinctiveness of these supportive connections and the dynamic quality of networks (Doerfel, 2018). Thus, ego networks with diverse engaged ties provide opportunities for effective diabetes management and increase the quality of life of students with T1D. Future research can explore engaged networks in the context of other chronic illnesses and disabilities.
Conclusions and limitations
This research has limitations. First, convenience sampling was used to recruit participants in the study. Thus, the results may only partially reflect the experiences of all college students living with T1D. Collaboration with CDN on participant recruitment was beneficial in getting access to this hard-to-reach population. However, the sample might also be biased toward CDN members. Conducting a study with a random sample of students with T1D could provide additional insight.
Second, the lack of demographic diversity in this research is a limitation. One of the major challenges in this research was recruiting minority young adults, who currently represent the largest growing population with T1D but rarely participate in research. Recruiting people with disabilities to serve as both participants and decision-makers should be done by future studies to address systemic inequities in health and organizational settings.
Third, this study employed an egocentric approach in analyzing students' networks. Although the choice was justified by the nature of the research questions posed in this research, the egocentric approach has limitations. Specifically, it burdens study participants by forcing them to identify the alters based on their perceptions, making them vulnerable to recall and perception errors. Although every effort was made to make the network data collection less tiresome for participants by applying interactive data collection design, recall, and perception errors could still occur.
Forth, this study does not collect any data on the changes in the respondents' health-related behaviors or objective health-related outcomes. Future studies could also explore higher-level characteristics of students' social networks beyond dyadic level.
Lastly, due to the bipartite nature of the network, some traditional measures may not be directly applicable. However, future research could employ several advanced analytical techniques to further explore the network dynamics revealed in this study. For instance, incorporating betweenness centrality could help identify key nodes that serve as bridges within the network, while assortativity analysis might uncover patterns of homophily or diversity among the nodes. These approaches would enrich the analysis and provide deeper insights into the complexities of the network.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Institutional Review Board, University of Miami, Coral Gables, USA. The studies were conducted in accordance with the local legislation and institutional requirements. The Ethics Committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants' legal guardians/next of kin because verbal consent was approved in place of written.
Author contributions
EM: Conceptualization, Data curation, Methodology, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the School of Communication, University of Miami under SoC Dissertation Award.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Balfe, M., and Jackson, P. (2007). Technologies, diabetes and the student body. Health Place 13, 775–787. doi: 10.1016/j.healthplace.2007.01.001
Birkett, M., Melville, J., Janulis, P., Phillips, G. 2nd, Contractor, N., and Hogan, B. (2021). Network Canvas: key decisions in the design of an interviewer assisted network data collection software suite. Soc. Netw. 66, 114–124. doi: 10.1016/j.socnet.2021.02.003
Borgatti, S. P., and Everett, M. G. (1997). Network analysis of 2-mode data. Soc. Netw. 19, 243–269. doi: 10.1016/S0378-8733(96)00301-2
Borgatti, S. P., Everett, M. G., and Freeman, L. C. (2002). Ucinet for Windows: Software for Social Network Analysis. Harvard, MA: Analytic Technologies, 12–15.
Borgatti, S. P., and Halgin, D. S. (2011). On network theory. Organ. Sci. 22, 1168–1181. doi: 10.1287/orsc.1100.0641
Brashers, D. E., Neidig, J. L., and Goldsmith, D. J. (2004). Social support and the management of uncertainty for people living with HIV or AIDS. Health Commun. 16, 305–331. doi: 10.1207/S15327027HC1603_3
Buchberger, B., Huppertz, H., Krabbe, L., Lux, B., Mattivi, J. T., and Siafarikas, A. (2016). Symptoms of depression and anxiety in youth with type 1 diabetes: a systematic review and meta-analysis. Psychoneuroendocrinology 70, 70–84. doi: 10.1016/j.psyneuen.2016.04.019
Burt, R. S. (2000). The network structure of social capital. Res. Org. Behav. 22, 345–423. doi: 10.1016/S0191-3085(00)22009-1
Burt, S. (2000). The strategic role of retail brands in British grocery retailing. Eur. J. Mark. 39, 88. doi: 10.1108/03090560010331351
Chewning, L. V., and Montemurro, B. (2016). The structure of support: mapping network evolution in an online support group. Comput. Human Behav. 64, 355–365. doi: 10.1016/j.chb.2016.07.006
Chiang, J. L., Kirkman, M. S., Laffel, L. M. B., Peters, A. L., and Type 1 Diabetes Sourcebook Authors (2014). Type 1 diabetes through the life span: a position statement of the American Diabetes Association. Diabetes Care 37, 2034–2054. doi: 10.2337/dc14-1140
Christakis, N. A., and Fowler, J. H. (2007). The spread of obesity in a large social network over 32 years. New Engl. J. Med. 357, 370–379. doi: 10.1056/NEJMsa066082
Coleman, J. S. (1988). Social capital in the creation of human capital. Am. J. Sociol. 94, S95–S120.
Doerfel, M. L. (2018). “Engaging partnerships,” in The Handbook of Communication Engagement (John Wiley and Sons, Inc.), 231–252. doi: 10.1002/9781119167600.ch16
Doerfel, M. L., Lai, C.-H., and Chewning, L. V. (2010). The evolutionary role of interorganizational communication: modeling social capital in disaster contexts. Hum. Commun. Res. 36, 125–162. doi: 10.1111/j.1468-2958.2010.01371.x
Eagle, D. E., and Proeschold-Bell, R. J. (2015). Methodological considerations in the use of name generators and interpreters. Soc. Netw. 40, 75–83. doi: 10.1016/j.socnet.2014.07.005
Gannoni, A. F., and Shute, R. H. (2010). Parental and child perspectives on adaptation to childhood chronic illness: a qualitative study. Clin. Child Psychol. Psychiatry 15, 39–53. doi: 10.1177/1359104509338432
Gordon, K., Rapp, J. A., Dimmick, B. L., and Jackson, C. (2011). Going to College with Diabetes: A Self Advocacy Guide for Students. Denver, CO: American Diabetes Association. Available at: https://diabetes.org/sites/default/files/2023-10/going-to-college-with-diabetes.pdf (accessed June 2023).
Gottlieb, B. H., and Bergen, A. E. (2010). Social support concepts and measures. J. Psychosom. Res. 69, 511–520. doi: 10.1016/j.jpsychores.2009.10.001
Hanna, K. M. (2012). A framework for the youth with type 1 diabetes during the emerging adulthood transition. Nurs. Outlook 60, 401–410. doi: 10.1016/j.outlook.2011.10.005
Hanneman, R. A., and Riddle, M. (2005). Introduction to social network methods. University of California Riverside.
Harrison, T. R. (2007). My professor is so unfair: student attitudes and experiences of conflict with faculty. Confl. Resol. Quart. 24, 349–368. doi: 10.1002/crq.178
House, J. S., Umberson, D., and Landis, K. R. (1988). Structures and processes of social support. Ann. Rev. Sociol. 14, 293–318. doi: 10.1146/annurev.so.14.080188.001453
Johnston, B., Jindal-Snape, D., and Pringle, J. (2016). Life transitions of adolescents and young adults with life-limiting conditions. Int. J. Palliat. Nurs. 22, 608–617. doi: 10.12968/ijpn.2016.22.12.608
Kawachi, I., and Berkman, L. F. (2001). Social ties and mental health. J. Urban Health 78, 458–467. doi: 10.1093/jurban/78.3.458
Laing, S. P., Jones, M. E., Swerdlow, A. J., Burden, A. C., and Gatling, W. (2005). Psychosocial and socioeconomic risk factors for premature death in young people with type 1 diabetes. Diabetes Care 28, 1618–1623. doi: 10.2337/diacare.28.7.1618
McCarty, C., Killworth, P. D., and Rennell, J. (2007). Impact of methods for reducing respondent burden on personal network structural measures. Soc. Networks 29, 300–315. doi: 10.1016/j.socnet.2006.12.005
Moody, J., and Paxton, P. (2009). Building bridges: linking social capital and social networks to improve theory and research. Am. Behav. Sci. 52, 1491–1506. doi: 10.1177/0002764209331523
Mouw, T. (2003). Social capital and finding a job: do contacts matter? Am. Sociol. Rev. 68, 868–898. doi: 10.2307/1519749
Perry, B. L., and Pescosolido, B. A. (2015). Social network activation: the role of health discussion partners in recovery from mental illness. Soc. Sci. Med. 125, 116–128. doi: 10.1016/j.socscimed.2013.12.033
Perry, B. L., Pescosolido, B. A., and Borgatti, S. P. (2018). Egocentric Network Analysis: Foundations, Methods, and Models. Cambridge: Cambridge University Press.
Rienties, B., and Hosein, A. (2020). Complex transitions of early career academics (ECA): a mixed method study of with whom ECA develop and maintain new networks [Original Research]. Front. Educ. 5:137. doi: 10.3389/feduc.2020.00137
Schwarzer, R., and Leppin, A. (1991). Social support and health: a theoretical and empirical overview. J. Soc. Pers. Relat. 8, 99–127. doi: 10.1177/0265407591081005
Strachan, M. W., MacCuish, A. C., and Frier, B. M. (2000). The care of students with insulin- treated diabetes mellitus living in university accommodation: scope for improvement? Diab. Med. 17, 70–73. doi: 10.1046/j.1464-5491.2000.00203.x
Thoits, P. A. (1995). Stress, coping, and social support processes: where are we? What next? J. Health Soc. Behav. 26, 53–79.
Väänänen, A., Kouvonen, A., Kivimäki, M., Pentti, J., and Vahtera, J. (2008). Social support, network heterogeneity, and smoking behavior in women: the 10-town study. Am. J. Health Prom. 22, 246–255. doi: 10.4278/0701094R1.1
Weitzman, E. R., Magane, K. M., Chen, P.-H., Amiri, H., Naimi, T. S., and Wisk, L. E. (2020). Online searching and social media to detect alcohol use risk at population scale. Am. J. Prev. Med. 58, 79–88. doi: 10.1016/j.amepre.2019.08.02
Keywords: diabetes, chronic illness, social support, social networks, organizations, health communication
Citation: Malova E (2024) “There are support resources, but they are kind of hidden”: social network analysis of college students' support systems in relation to type 1 diabetes management. Front. Hum. Dyn. 6:1370106. doi: 10.3389/fhumd.2024.1370106
Received: 14 February 2024; Accepted: 16 September 2024;
Published: 02 October 2024.
Edited by:
Dominik E. Froehlich, University of Vienna, AustriaReviewed by:
Bart Rienties, The Open University, United KingdomPádraig MacCarron, University of Limerick, Ireland
Copyright © 2024 Malova. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ekaterina Malova, ZW1hbG92YUBzaW1vbi5yb2NoZXN0ZXIuZWR1
 Ekaterina Malova
Ekaterina Malova