- 1Department of Pharmacology and Toxicology, School of Pharmacy, College of Health Sciences, University of Ghana, Accra, Ghana
- 2Department of Biotechnology, Microbiology and Public Health, AEServe, Lethbridge, AB, Canada
- 3Faculty of Pharmacy and Pharmaceutical Sciences, University of Alberta, Edmonton, AB, Canada
- 4Department of Pharmacology and Toxicology, School of Pharmacy, University of Health and Allied Sciences, Ho, Volta Region, Ghana
- 5Institute of Traditional and Alternative Medicine, University of Health and Allied Sciences, Ho, Volta Region, Ghana
Treatment adherence is necessary for several reasons, including preventing the development of resistance and avoiding progression to a severe form of the disease. This study explored patients’ beliefs and their impact on adherence to antimalarial medications (orthodox and herbal medicines). A cross-sectional survey was conducted over three weeks in the Ga East Municipal District of Ghana. The study involved 346 participants and employed comprehensive questionnaires to gather data, which was analyzed using STATA version 14. Despite the high prevalence of malaria in the district, adherence to antimalarial medication remained a challenge. The study revealed varying opinions among participants regarding the safety and efficacy of different antimalarial treatments. The research highlighted the connection between patients’ beliefs, age, knowledge, and adherence. Younger individuals showed higher adherence rates, emphasizing the need for age-specific interventions. Comprehensive knowledge also correlated with better adherence, highlighting the role of education. The study recommended the development of tailored educational campaigns that address misconceptions and foster trust between healthcare providers and patients. Innovative interventions, such as mobile phone-based reminders and incentives, were suggested to improve adherence. The research emphasized the importance of holistic malaria prevention strategies, including robust educational initiatives, targeted interventions in hotspot districts, and widespread distribution of insecticide-treated nets. The study’s insights offer actionable recommendations to enhance malaria control efforts in the Ga East Municipal District and beyond.
Introduction
Malaria remains a significant global public health concern, with Plasmodium falciparum accounting for the highest morbidity and mortality rates, particularly in sub-Saharan Africa (World Health Organization, 2023). The disease is transmitted by female Anopheles mosquitoes, progressing from liver-stage infection to erythrocytic invasion, which triggers clinical manifestations such as fever, chills, and headaches. If left untreated, malaria can lead to severe complications, including organ failure and death (García, 2010). In 2021, approximately 247 million malaria cases were recorded globally, with sub-Saharan Africa bearing the brunt of the disease, accounting for 95% of cases and 96% of deaths (World Health Organization, 2022). In Ghana, including the Ga East Municipal District, malaria remains highly endemic, necessitating comprehensive control and treatment strategies (Peprah et al., 2018).
Artemisinin-based Combination Therapies (ACTs) have been Ghana’s first-line treatment for uncomplicated malaria since 2004 (Guidelines for Case Management of Malaria in Ghana, 2020). Although ACTs are highly effective, resistance linked to mutations in the kelch13 gene poses a growing threat to their efficacy (Kozlov, 2021). Ensuring adherence to prescribed antimalarial regimens is crucial to preventing disease progression, reducing transmission, and mitigating drug resistance (Gast and Mathes, 2019). However, poor adherence remains a challenge worldwide, influenced by side effects, financial constraints, misconceptions, and forgetfulness (Shahin et al., 2019). Patient beliefs play a critical role in medication adherence. Perceptions of the efficacy and safety of orthodox versus herbal antimalarial treatments significantly influence treatment behaviors (Afolabi et al., 2020). Understanding these beliefs is essential for designing targeted interventions to improve compliance. While Ghana has a longstanding tradition of using herbal remedies for malaria, concerns persist regarding their safety, efficacy, and regulatory oversight (Amponsah et al., 2015). Although public health guidelines permit the use of herbal treatments following a confirmed malaria diagnosis, self-medication and reliance on unregulated herbal products may contribute to poor adherence to prescribed therapies (Awuah et al., 2018; Donkor et al., 2021).
This study assesses patients’ knowledge, beliefs, and adherence to antimalarial medications in the Ga East Municipal District. Specifically, it aims to evaluate patients’ understanding of malaria and its treatment, investigate their beliefs about antimalarial drugs, and explore the relationship between these beliefs and adherence to treatment. Given the recent introduction of the RTS, S/AS01 malaria vaccine, findings from this study could inform strategies to enhance vaccine uptake and reinforce malaria prevention efforts (World Health Organization, 2023). This research contributes to broader efforts to improve malaria treatment adherence and public health outcomes in endemic regions by addressing knowledge gaps and misconceptions. Patient, provider, cultural, historical, and healthcare system factors all influence pharmaceutical usage patterns, despite the absence of easy answers (World Health Organization, 2022; World Health Organization, 2023).
A study conducted in Ghana (Amponsah et al., 2015) found that other factors, such as awareness of the medicine and its benefits, were identified as causes of medication non-adherence (Amponsah et al., 2015). However, adherence to treating illness in general and antimalarial treatment, in particular, is not always perfect (Amponsah et al., 2015; Awuah et al., 2018). Another study (Awuah et al., 2018) found that inadequate health information and specific individuals’ attitudes towards the use of medications, particularly ACTs, side effects, and the issue of recall, particularly among the elderly, were the primary factors influencing adherence to ACT use in the research region. A person’s beliefs about medication are essential for sticking to the treatment. Studies show that when patients are aware of the harmful effects of malaria, they are more likely to follow the prescribed treatment and prevention measures (Amponsah et al., 2015; Arora et al., 2021).
Methodology
Study design and period
This research employed a cross-sectional survey comprising 58 questions that assessed patient demographics, personal malaria history, perceptions of malaria, views on orthodox and herbal medicines for malaria treatment, and health education and communication. The data was collected over three weeks.
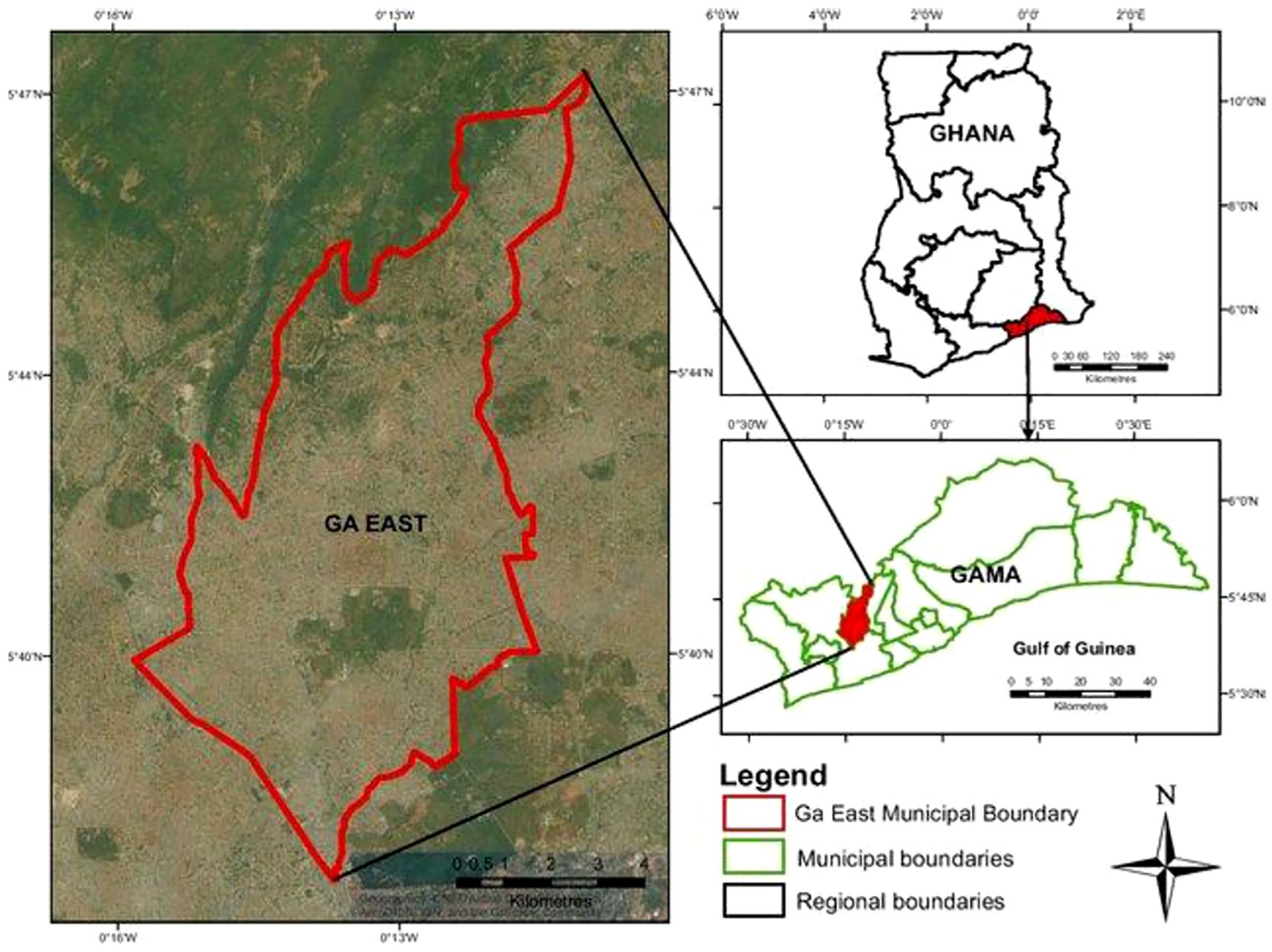
Study area
The Ga East Municipal Assembly is one of Ghana’s 261 Metropolitan, Municipal, and District Assemblies (MMDAs), comprising part of the 29 MMDAs in the Greater Accra Region. The high number of malaria cases in this area led to its selection for study. The municipality is located in the northern part of the Greater Accra Region, with its administrative center in Abokobi. The municipality has twenty health facilities, including one District Hospital, one Polyclinic, two Quasi-Governmental Health Centres, and sixteen Private Health Centres.
Population for study
The population for this study consisted of patients with malaria infections who had been prescribed antimalarial medication for the previous two years at various health facilities in the Ga East Municipality of Ghana’s Greater Accra Region (Figure 1). The target population is roughly twenty-eight thousand three hundred and thirty-eight (28,338) people. Following data collection at a few chosen health centers, the population was estimated to be 10% of the entire Ga East Municipal population.
Sample and sampling technique
The researcher visited selected households randomly within the designated communities in the municipality, administering questionnaires until the required sample size was achieved. The total estimated sample size was 346.
These patients were diagnosed with malaria infections from a target population of twenty-eight thousand three hundred and thirty-eight (28,338).
Sample size determination
Based on the population of the Ga East Municipal District, the sample size was determined with a 95% confidence level, allowing for a margin of error of ±5. The population for this study were patients diagnosed with malaria and prescribed antimalarial medication in the Ga East Municipal District. The formula for estimating the sample size for a proportion in a single population was used below to determine the appropriate sample size (Naing et al., 2006).
The calculation was based on approximately 10% of the population. The following assumptions were made: a 95% confidence level and a 5% margin of error. The sample size formula I used to determine the size is shown below. Where:
Z is the standard normal deviation corresponding to the desired confidence level (for a 95% confidence level, Z = 1.96). p is the estimated proportion of individuals with the characteristic of interest in the population
(10%, or 0.1) d is the desired margin of error (0.05)
Plugging in these values, we get:
n = (1.96)^2* 0.1 * 0.9/(0.05) ^2
n = 345.96
Based on these assumptions, the minimum sample size required for this study is 345.96
Rounding up to the nearest whole number, the recommended sample size would be 346 patients.
Inclusion and exclusion criteria
To respect the participant’s right to participate or exclude themselves from the research, their consent was sought after an explanation of the purpose and details of the study. This ensured that the right respondents were asked if they had been infected and diagnosed with malaria. The study included participants who lived in the research area, could communicate clearly, and were 18 years of age or older.
Those who responded “No” (whether they had had malaria and had been treated in the past years) were also excluded. This process was repeated until the researcher obtained the required sample size.
Data collection instrument and procedure
The study used a standardized questionnaire (see Appendix A) to collect the required data. The questionnaire had 58 questions structured into five (5) main sections: sections A, B, C, D, and E. Section A involved the respondents’ biodata, while the rest contained questions arranged systematically and related to the three research objectives. The items for the construction were based on the Likert scale points. Trial samples of 10 questionnaires were initially distributed to test participants’ understanding of the questionnaire.
Data entry, cleaning and analysis
Data collected from participants was recorded in the SurveyMonkey application. The entries were rechecked to ensure that the correct information was recorded. Where an error was found, it was cross-checked with the questionnaires obtained. A comprehensive descriptive analysis was conducted following data entry, incorporating statistics such as frequencies and percentages. Inferential statistical methods were applied. Logistic regression, odds ratios (OR), and adjusted odds ratios (AOR) were utilized to explore the factors influencing participants’ beliefs and adherence to antimalarial medication. The data gathered from the survey were meticulously analyzed using STATA version 14.
Results
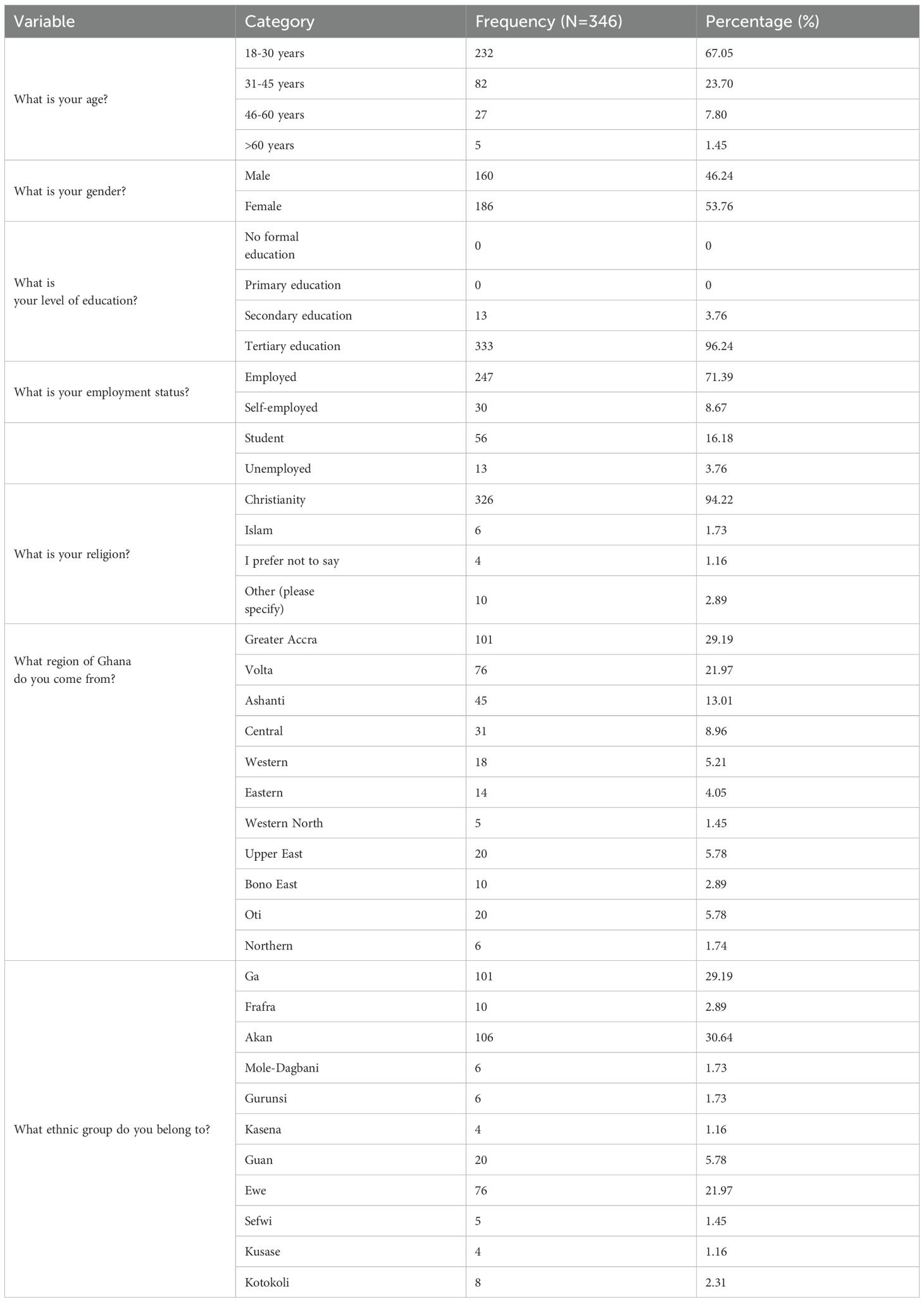
As shown in Table 1, a little over 90% of the participants fell within the 18- to 45-year-old age bracket. There were slightly more females (53.76%) than males.
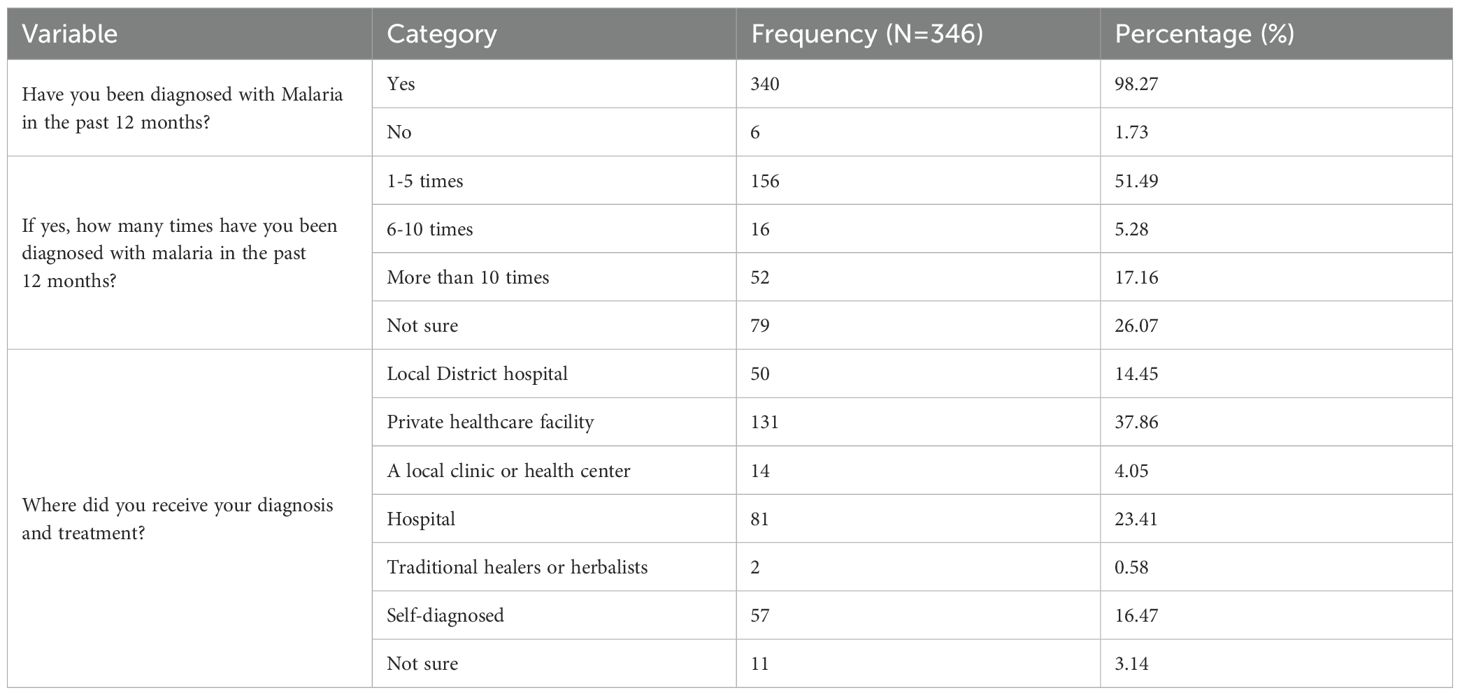
History of malaria infection of respondents
As shown in Table 2, about three-quarters of the respondents have had malaria at least once in the past 12 months, while the remaining (26.07) were not sure they had.
Assessing the knowledge of respondents on antimalarial medication
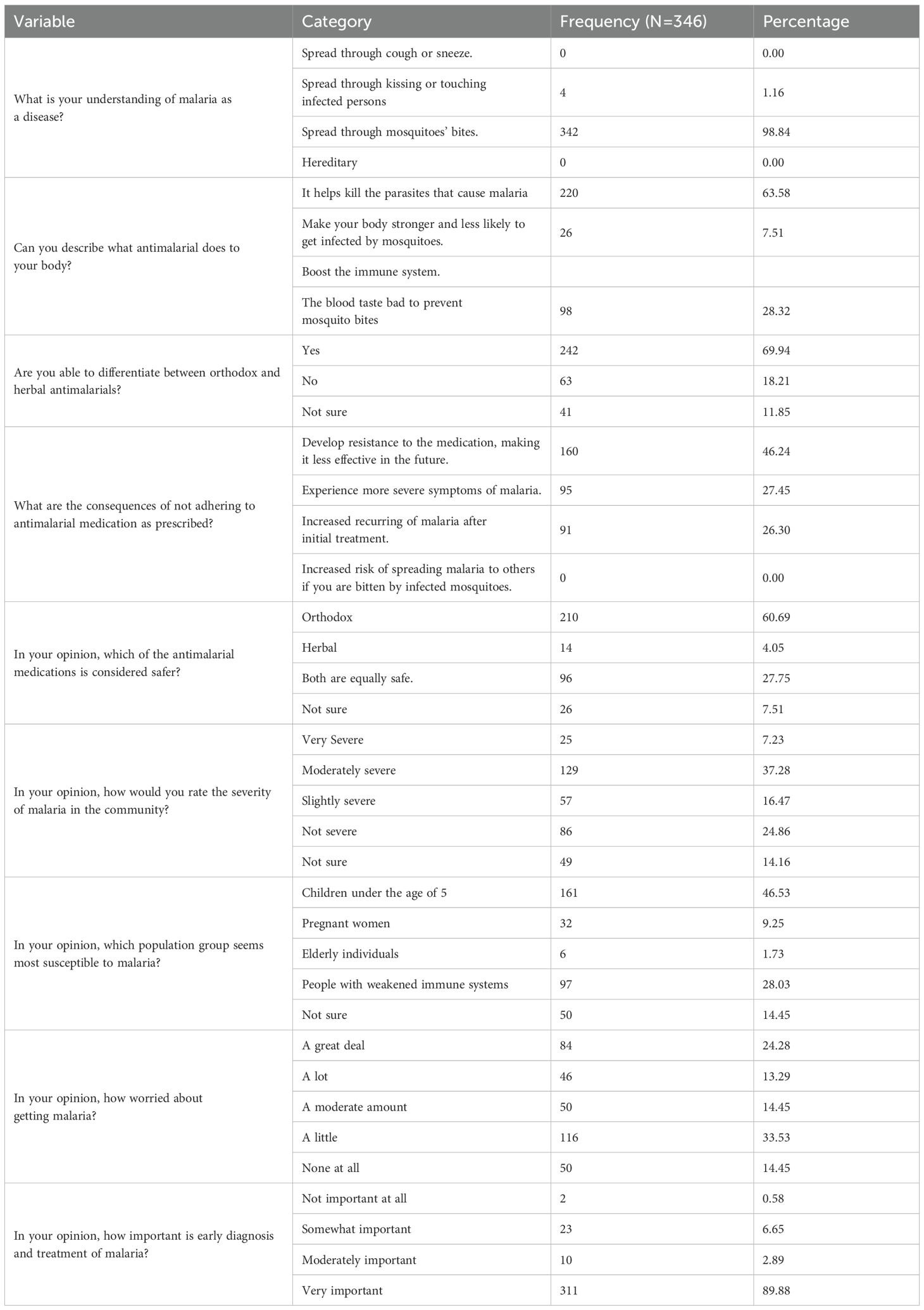
The data presented in Table 3 indicate that approximately 99% of respondents were aware of how malaria is contracted. Additionally, nearly 70% of respondents could distinguish between orthodox malaria medication and herbal medication.
Level of Knowledge on Antimalarial Medications
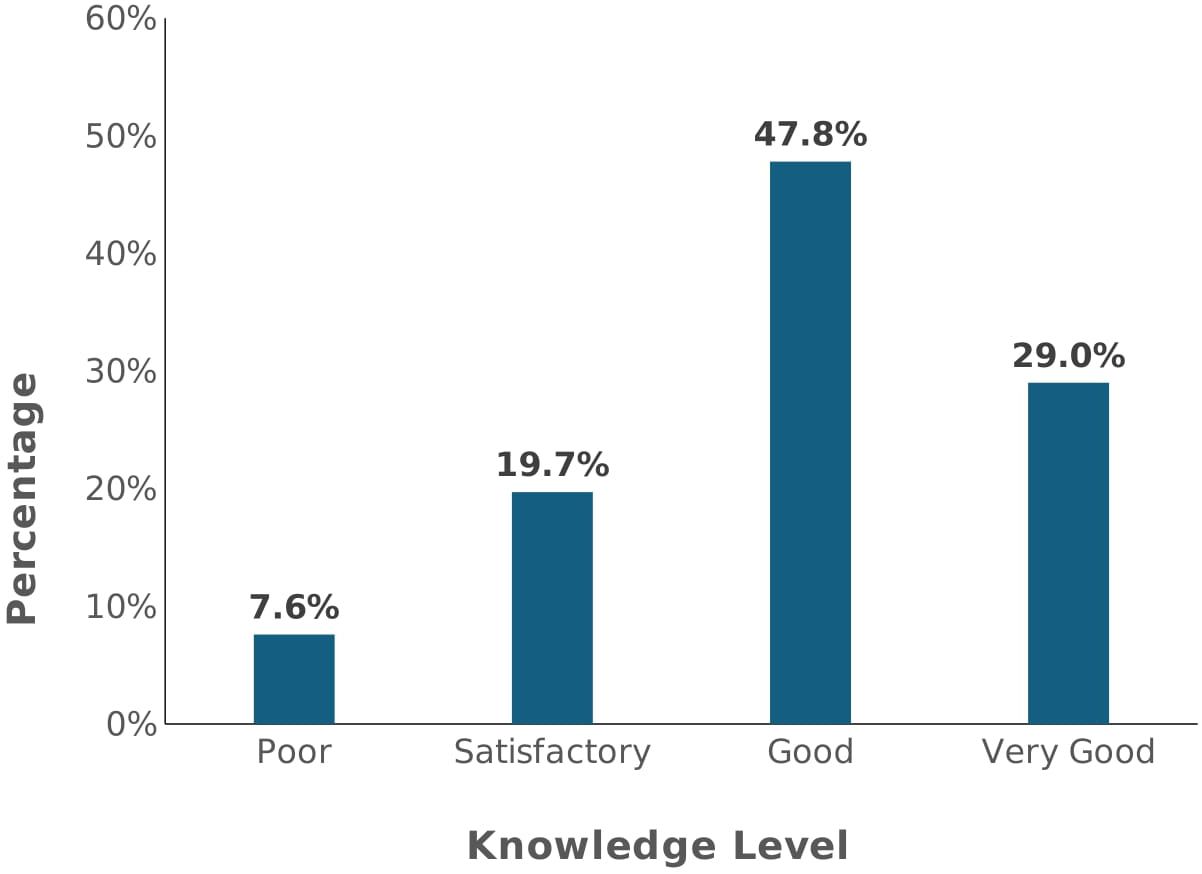
As shown in Figure 2 (above), a little over three-quarters of the participants had at least good knowledge of antimalarial medication use. About a quarter had satisfactory knowledge, whilst 7.6% had poor knowledge of antimalarial use.
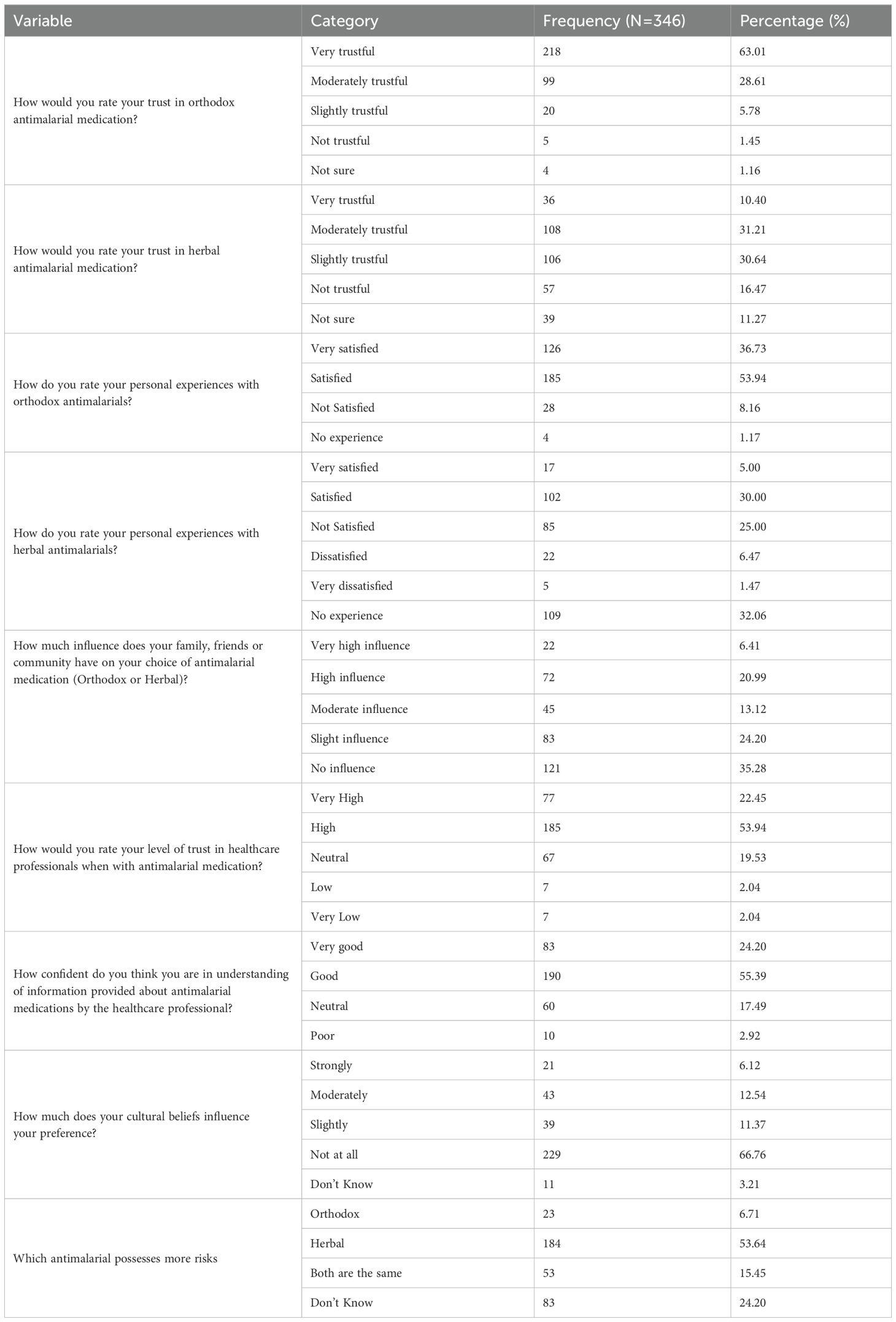
Data presented in Table 4 revealed that a little over half of the respondents believe that herbal antimalarial medication possesses more risks compared to orthodox medicines.
Beliefs on antimalarial medications
Figure 3 presents the findings on respondents’ beliefs regarding the use of antimalarial medication. Approximately 19.0% of the participants hold poor beliefs about the use of antimalarial medicines, 40.9% have satisfactory beliefs, and 40.1% have reasonable beliefs.
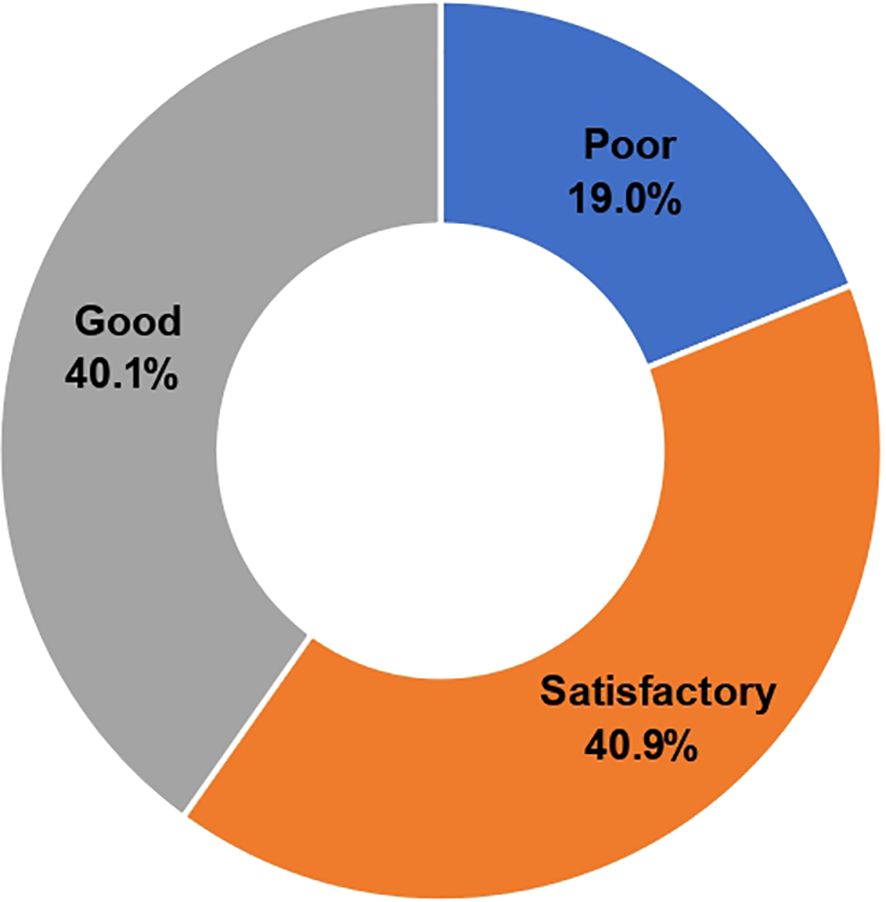
Figure 3. Level of belief of respondents towards antimalarial medication beliefs on antimalarial medication use.
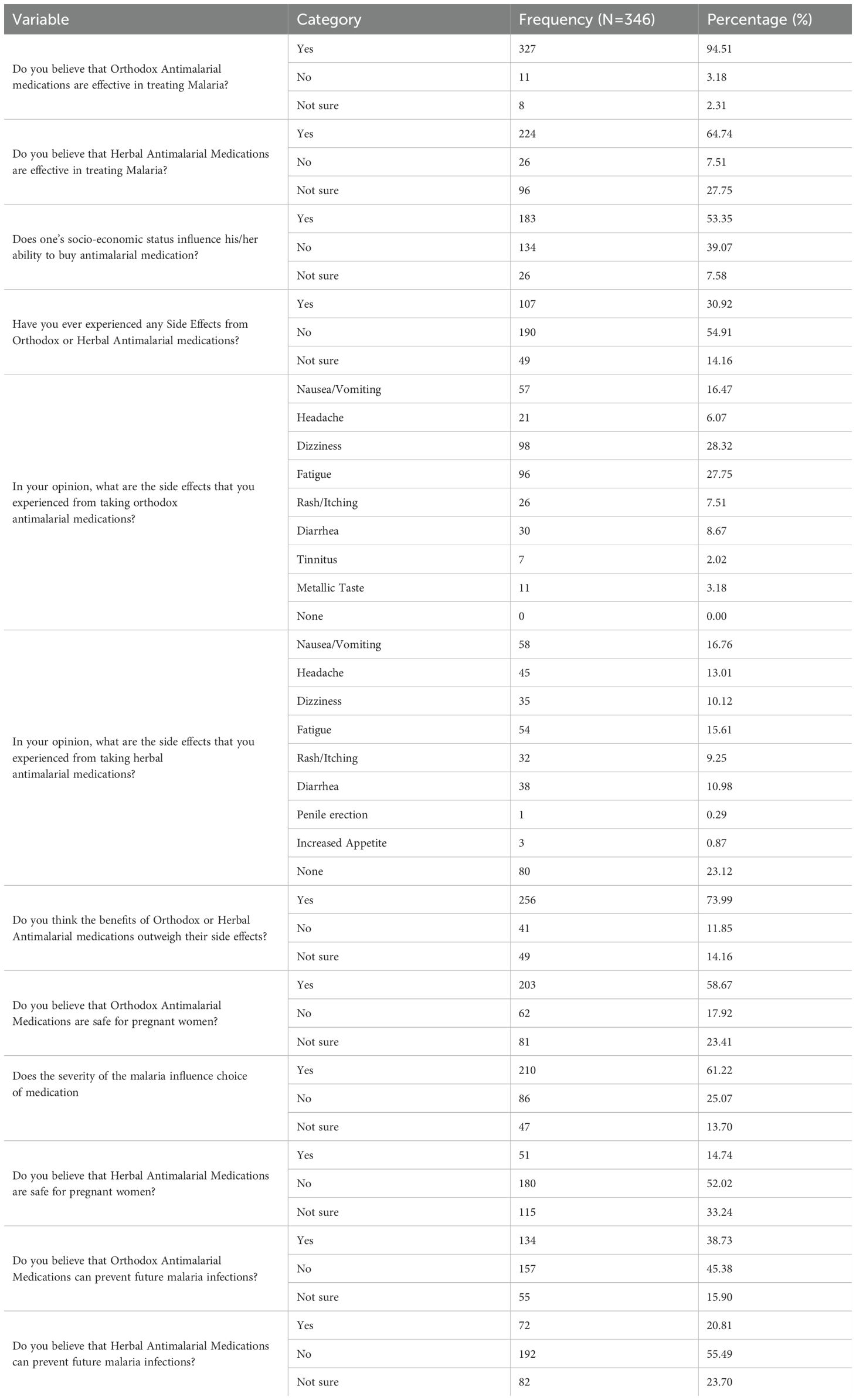
As shown in Table 5 below, many of the respondents (94.5%) believed that orthodox antimalarial medications were more effective than herbal antimalarial medications (64.74%).
Medication adherence of participants to antimalarial therapy
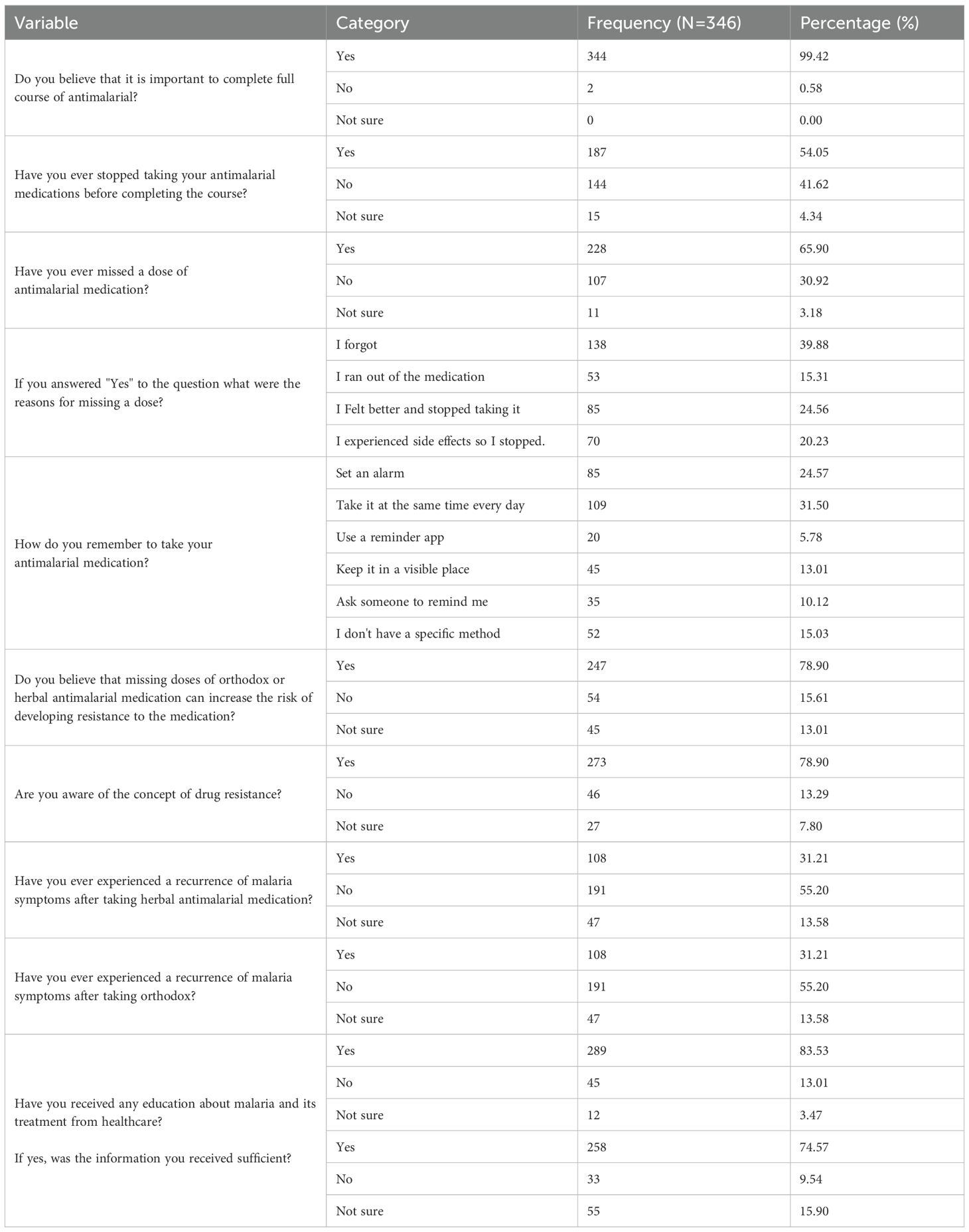
The results presented in Table 6 indicate that almost all the respondents (99.42%) believed it was essential to complete the entire course of antimalarials. However, about two-thirds of respondents admitted to having missed a dose of antimalarial medication.
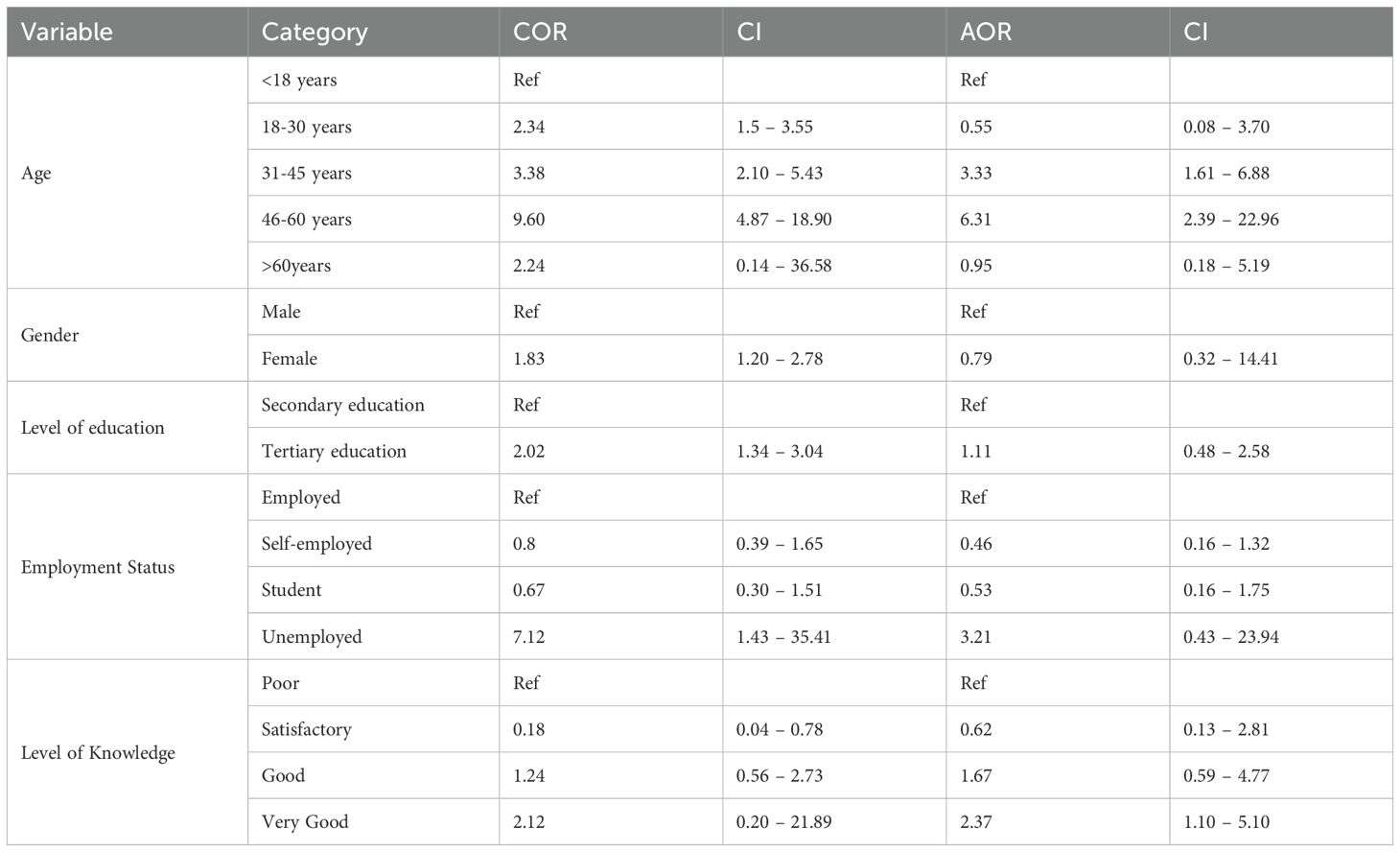
Factors that influence beliefs on antimalarial therapy
As shown in Table 7 below, the participants’ age and level of knowledge were factors that affected their beliefs about antimalarial therapy.
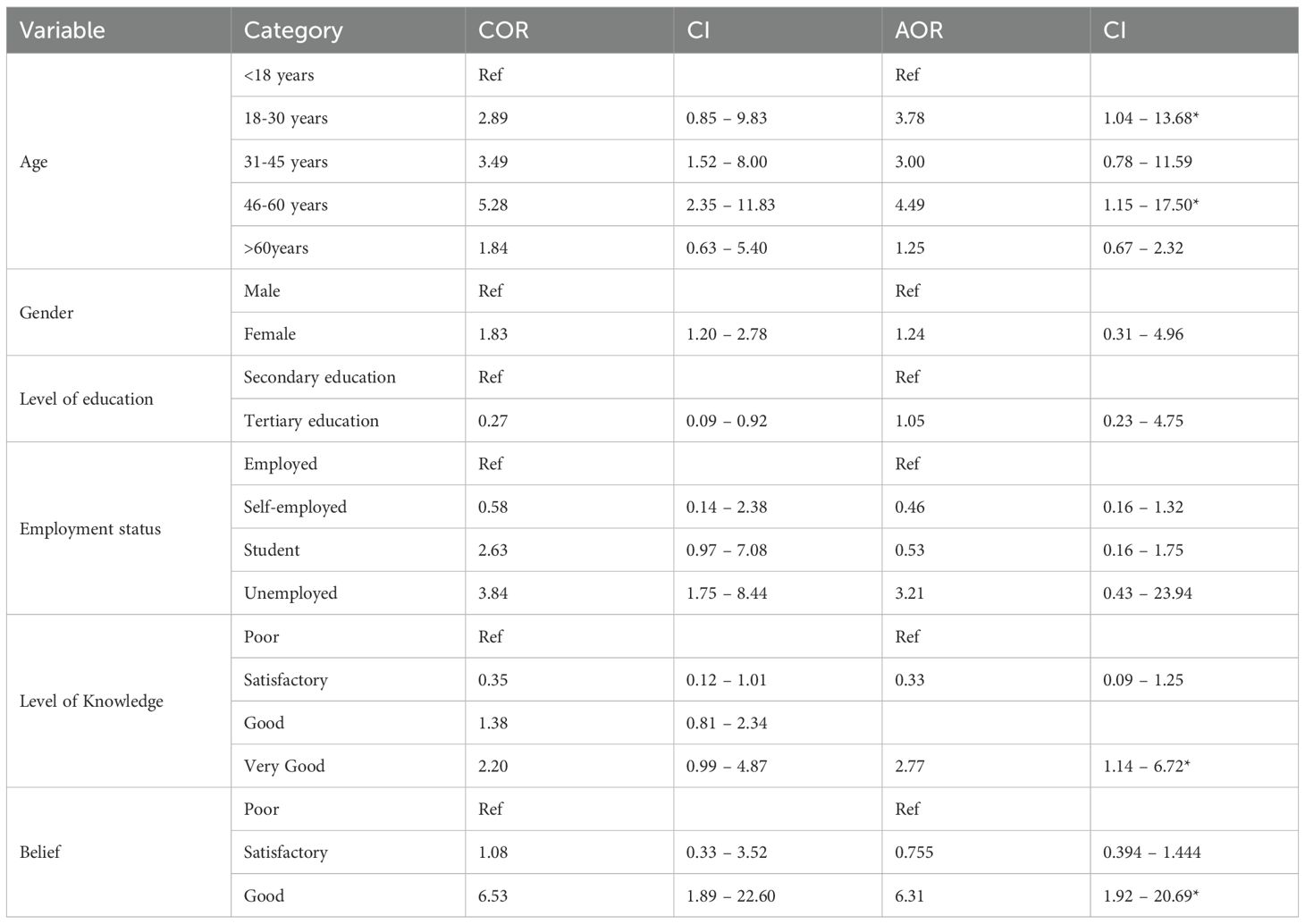
Association with antimalarial medication adherence
According to Table 8 (below), the respondents’ age, level of knowledge, and beliefs were strongly associated with medication adherence.
In the tables above, “Ref” stands for the reference category. In statistical analysis, particularly in logistic regression, one category of a categorical variable is chosen as the reference category for comparison with other categories. The reference category serves as a baseline against which different categories are compared.
This study, along with the one carried out by Amponsah et al., focuses on assessing various aspects of malaria awareness, knowledge, beliefs, and adherence to antimalarial medications among respondents (Amponsah et al., 10).
Malaria has been a persistent public health threat despite the devastating impact of malaria on health and the economy. It was, therefore, imperative to assess respondents’ knowledge of malaria infections, treatments, and their adherence to proper medication. Results indicate that 98.8% of respondents understand malaria and the transmission mode (Table 2). About 60.7% consider orthodox medications safe, 4.1% consider Herbal medications safe, and 27.8% consider both safe (Table 3). In the groups most susceptible to vulnerability, 46.5% considered children to be vulnerable, 9.3% considered pregnant women, 1.7% considered elderly individuals, 28.0% considered immunocompromised persons, and 14.5% were unsure (Table 3). Considering the severity of malaria in the community, approximately 7.2% considered it very severe, 37.3% considered it moderately severe, 16.4% considered it slightly severe, 24.8% considered it not severe, and 14.2% were unsure whether malaria was severe in the community (Table 3). About 46.5% believe children are most susceptible to malaria, and 9.3% believe pregnant women are most vulnerable. In comparison, 28.0% believe immunocompromised people are most susceptible (Table 3). A quarter, 24.3%, are greatly worried about malaria infection, while a third are slightly worried (Table 3). The majority, 89.9%, recognized that early malaria diagnosis is essential, while 6.7% believed that early diagnosis may be necessary (Table 3). From the study, respondents had diverse knowledge of malaria infections, treatment and adherence to medication. This came to light when the results showed that few knew some variables. In contrast, others were unsure, despite 76.8% of their level of antimalarial use being rated as either good (47.8%) or very good (27.0%), as illustrated in Figure 2.
Discussion
The study found that 91.1% of the respondents’ beliefs regarding the use of antimalarial medication were either satisfactory or reasonable. That is, 40.9% have satisfactory beliefs about the use of antimalarial medicines, while 40.1% have reasonable beliefs about antimalarial medications. About a fifth of the participants have poor beliefs about antimalarial medication use. On their central belief, 94.5% of the respondents believed that orthodox antimalarial medications effectively treat malaria. In comparison, 64.7% believe that herbal antimalarials are effective at treating malaria, with 27.8% unsure. About 74% of the respondents believe that the benefits of orthodox or herbal antimalarial medications outweigh their side effects. Considering the safety of orthodox antimalarials in pregnancy, 58.7% believe they are safe, 17.9% think they’re not, and 23.4% are unsure. About 14.7% of respondents believe that herbal medications are safe in pregnancy, 52.0% think they are not secure, and 33.2% are not sure. A third, 134 (38.7%), believe that orthodox antimalarials can provide prophylaxis, 45.4% do not, and 15.9% are unsure. The Amponsah et al. study participants demonstrated a good understanding of the recommended antimalarial drugs, their dosages, efficacy, and side effects. However, there were knowledge gaps regarding certain aspects of malaria (Amponsah et al., 2015; Awuah et al., 2018).
Additionally, about a fifth (20.8%) believe that herbal antimalarials can be used as prophylactics, 55.5% do not think so, and nearly a quarter (23.7%) are unsure. Amponsah et al. focused on beliefs such as the influence of spiritual beliefs on healing and trust in medications (Amponsah et al., 2015; Donkor et al., 2021). The study also examined the impact of patients’ opinions and beliefs on adherence to antimalarials.
High patient adherence to antimalarial treatment is crucial in ensuring the effectiveness of the drug. It was observed that almost all respondents (99.4%) believe that completing antimalarial therapy is necessary. Half of the respondents, 54.1%, stopped taking their antimalarial medication before completion, while 41.6% did not. About two-thirds, 65.9%, have missed a dose of their antimalarial medication, while nearly a third, 30.9%, have never missed a dose. Approximately one-third of a quarter, or 78.9%, have heard of drug resistance, 13.3% have not, and 7.8% are unsure. About 31.2% have had recurrent malaria infection symptoms after orthodox medication use, while 55.2% have not, and 13.6% are not sure. About 23.4% have had recurrent malaria infection symptoms after herbal medication use, while 48.3% have not, and 28.3% are not sure.
The results indicate that the age of respondents influenced their belief in antimalarial medication therapy. It was found that respondents aged 31 to 45 years were 3.3 times more likely to hold reasonable beliefs about antimalarial medication use than participants under 18 years (AOR = 3.33; CI = 1.61 –6.88). Additionally, respondents aged 46 to 60 were 6.3 times more likely to hold reasonable beliefs about antimalarial medication use than participants under 18 years (AOR = 6.31; CI = 2.39 –22.96). The level of knowledge was associated with the belief in antimalarial medication. Excellent knowledge increased the odds of having a reasonable belief by 2.3-fold compared to having a poor level of understanding (AOR= 2.37; CI= 1.10 – 5.10). Regarding the factors influencing adherence to antimalarial medication, it was observed that respondents aged 18–30 years were 3.8 times more likely to be adherent compared to those under 18 years of age (AOR = 3.78; CI = 1.04–13.68). Additionally, respondents aged 46–60 were 4.5 times more likely to be adherent compared to respondents under 18 years (AOR = 4.49; CI = 1.15–17.50). Having Very Good knowledge of antimalarial medication was associated with 2.8 times increased odds of being adherent compared to having poor knowledge (AOR = 2.77; CI = 1.14–6.72). Having reasonable beliefs was associated with a 6.3 times increased chance of being adherent compared to having poor beliefs about antimalarial medication use. (AOR= 6.31; CI= 1.92 – 20.69). Amponsah et al. found an overall adherence rate of 57.3% to ACTs. Factors like educational background and patients’ beliefs influenced adherence (Amponsah et al., 2015; Arora et al., 2021). Education on medication dosage, effectiveness, and side effects was emphasized.
Conclusion
A very high percentage of the respondents’ beliefs regarding the use of antimalarial medication were either satisfactory or reasonable. A larger number of the respondents believe that orthodox antimalarial medications are effective in treating malaria, much higher than those who believe in the effectiveness of herbal alternatives. It was observed that almost all respondents (99.4%) believe that completing antimalarial therapy is necessary. Nearly half of the respondents stopped taking their antimalarial medication before it was completed. The results indicate that the age of respondents influenced their belief in antimalarial medication therapy and treatment adherence.
Limitations
1. Because of the limitations in establishing causality, it can be challenging to interpret the associations found in cross-sectional studies.
2. Responder Bias: Participants may not accurately report their behaviors or experiences, especially on sensitive topics.
3. Sampling Bias: The chosen sample might not accurately reflect the entire population, resulting in distorted outcomes.
4. Recall Bias: A common phenomenon where the participant’s ability to accurately remember and report past events becomes flawed over time.
5. Due to sampling biases and the one-time nature of data collection, the findings may not be generalized to other populations or periods.
Recommendations
1. There is a significant need to enhance malaria prevention awareness by strengthening malaria education and promoting behavioral change.
2. To improve program effectiveness, malaria control and prevention should be strengthened in hotspot districts in the appropriate months.
3. Interventions should focus on specific demographic groups, such as younger individuals, to improve adherence rates. Tailored educational campaigns considering age-specific needs could be beneficial.
4. Implementing behavioral interventions, such as reminders and incentives, can positively influence adherence. Mobile phone-based reminders, similar to those in a successful intervention study, could effectively improve adherence rates.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by School of Pharmacy Ethics Committee of the University of Ghana. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
MA: Writing – original draft, Writing – review & editing. VW: Writing – original draft, Writing – review & editing. BN: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Afolabi F. J., De Beer P., and Haafkens J. A. (2020). Orthodox or traditional medicine? Private or public healthcare? Exploring treatment pathways for occupational health problems among informal automobile artisans. Soc. Sci. Med. 265, 113510. doi: 10.1016/j.socscimed.2020.113510
Amponsah A. O., Vosper H., and Marfo A. F. (2015). Patient-related factors affecting adherence to antimalarial medication in an urban estate in Ghana. Malaria Res. Treat 2015, 452539. doi: 10.1155/2015/452539
Arora N., C Anbalagan L., and Pannu A. K. (2021). Towards eradicating malaria: Is the WHO’s RTS, S/AS01 vaccination compelling enough? Risk Manage. Healthcare Policy 14, 1033–1039. doi: 10.2147/RMHP.S219294
(2020). Guidelines for Case Management of Malaria in Ghana. 4th Edition (Accra, Ghana: Ministry of Health).
Awuah R. B., Asante P. Y., Sakyi L., Biney A. A. E., Awoonor-Williams J. K., Agyei F. K., et al. (2018). Factors associated with treatment-seeking for malaria in urban poor communities in Accra, Ghana. Malar. J. 17, 168. doi: 10.1186/s12936-018-2311-8
Donkor E., Kelly M., Eliason C., Amotoh C., Gray D. J., Clements A. C. A., et al. (2021). A Bayesian spatiotemporal analysis of malaria in the Greater Accra Region of Ghana, 18(11), 6080. doi: 10.21203/rs.3.rs-143819/v2
García L. S. (2010). Malaria update for the clinical microbiology laboratory: A new species, plasmodium knowlesi, and new diagnostic tests. Clin. Microbiol. Newslett. 32, 127–133. doi: 10.1016/j.clinmicnews.2010.08.001
Gast A. and Mathes T. (2019). Medication adherence influencing factors—an (updated) overview of systematic reviews. Systematic Rev. 8, 112. doi: 10.1186/s13643-019-1014-8
Kozlov M. (2021). Resistance to key malaria drugs confirmed in Africa. Nature 597, 604. doi: 10.1038/d41586-021-02592-6
Naing L., Winn T. B. N. R., and Rusli B. N. (2006). Practical issues in calculating the sample size for prevalence studies. Arch. Orofacial Sci. 1, 9–14.
Peprah P., Gyasi R. M., Adjei P. O., Agyemang-Duah W., Abalo E. M., and Kotei J. N. A. (2018). Religion and Health: An exploration of attitudes and health perceptions of faith healing users in urban Ghana. BMC Public Health 18, 1358. doi: 10.1186/s12889-018
Shahin W., Kennedy G. A., and Stupans I. (2019). The impact of personal and cultural beliefs on medication adherence of patients with chronic illnesses: a systematic review. Patient Preference Adherence 13, 1019–1035. doi: 10.2147/ppa.s212046
Keywords: Ghana, malaria, treatment, drugs, compliance
Citation: Amoako MA, Wutor VC and N’guessan BB (2025) Knowledge, beliefs and adherence to antimalarial medications among patients in the Ga East Municipality of Ghana. Front. Malar. 3:1582682. doi: 10.3389/fmala.2025.1582682
Received: 24 February 2025; Accepted: 07 August 2025;
Published: 28 August 2025.
Edited by:
Badu Sarkodie, Ghana Health Service, GhanaReviewed by:
Daniel Ansong, Kwame Nkrumah University of Science and Technology, GhanaLungowe Sitali, University of Zambia, Zambia
Copyright © 2025 Amoako, Wutor and N’guessan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Benoit Banga N’guessan, YmJuZ3Vlc3NhbkB1Zy5lZHUuZ2g=
 Michelle Akua Amoako1
Michelle Akua Amoako1 Victor Collins Wutor
Victor Collins Wutor Benoit Banga N’guessan
Benoit Banga N’guessan