Abstract
This paper synthesizes recent advances of technologies in ophthalmology education. Advancements in three-dimensional technology are revolutionizing ophthalmology education by enhancing the visualization, understanding, and retention of complex anatomical and pathological concepts. In addition to physical models, artificial intelligence and virtual reality are emerging as significant tools. A systematic search of PubMed was carried out, with a search date from inception to 01/05/2024. A total of 6,686 articles were screened, of which 6,470 were excluded following abstract review. After reading the remaining 216 articles in full, a further 186 were excluded. A total of 30 original articles were included in the review. This review underscores the transformative impact of novel technology in ophthalmology education, offering innovative solutions to enhance learning, surgical training, and diagnostic skills. Further research and development in this field hold promise for continued improvements in ophthalmology education and practice.
1 Introduction
Vision is one of the most important senses. Blindness is ranked by the public to be the worst disease (1). Accurate diagnosis and effective treatment can improve the quality of life by preserving or enhancing vision, allowing individuals to continue performing daily tasks. Ophthalmology is a complex and specialized field, which requires in-depth knowledge of the anatomy, physiology, and diseases of the eye. Ophthalmology education is essential for ensuring that healthcare professionals have the knowledge, skills, and expertise needed to provide high-quality care to patients with eye conditions.
However, there are some challenges in ophthalmology education. First, an imbalance of educational resources in ophthalmology results in disparities in access to quality education, training, and resources in the field. Rural and underserved areas often lack access to specialized ophthalmic training programs. Limited financial resources can affect the ability of junior doctors to pursue education and training in ophthalmology, particularly in low-income countries where there may be insufficient funding for educational programs. Unequal distribution of modern equipment, technology, and facilities can affect the quality of ophthalmology education and training, with some institutions having superior resources to others. Second, ophthalmology training programs include a combination of theoretical study and clinical practice. Balancing these demands can be challenging for trainees, as they may struggle to find time. Finally, the education and training of ophthalmologists may vary in terms of curriculum, quality, and duration across institutions and countries. This lack of standardization can result in inconsistencies in the level of knowledge and skills among ophthalmologists, which affects the quality of patient care.
Recently, new techniques are emerging in medical education. These advances have a profound influence on medical education, transforming the way students and trainees learn and practice medicine. Advances in ophthalmology education have the potential to solve current challenges in ophthalmology education. This review has been conducted to evaluate these novel technologies.
2 Methods
2.1 Eligibility criteria
Original studies were included if they described developments in ophthalmic training and met the following criteria: (1) study participants were ophthalmologists or medical students in ophthalmology and (2) educational studies. Studies were excluded if: (1) they did not include original data; (2) the studies were not specific to ophthalmology; or (3) the studies were not written in English.
2.2 Search methods
A systematic search of PubMed was carried out, using the terms “(train* OR education) AND ophthalm*.” The search date was from inception to 01/05/2024. Reference lists from included articles and relevant reviews were searched for eligible studies.
2.3 Study selection
Two authors carried out independent, duplicate searches. All abstracts were reviewed, and articles that were potentially eligible were read in full. The final list of studies that met the eligibility criteria was compared, and any disagreements were resolved through discussion.
2.4 Data collection
The same two authors extracted data for each study separately, and differences were resolved through discussion. Data collected included details of the training objective, participants, assessment, and advantages and disadvantages.
3 Results
A total of 6,686 articles were screened, of which 6,470 were excluded following abstract review. After reading the remaining 216 articles in full, a further 186 were excluded. A total of 30 original articles were included in this systematic review (Figure 1). Details of findings are summarized in Tables 1–3 according to training mode.
Figure 1
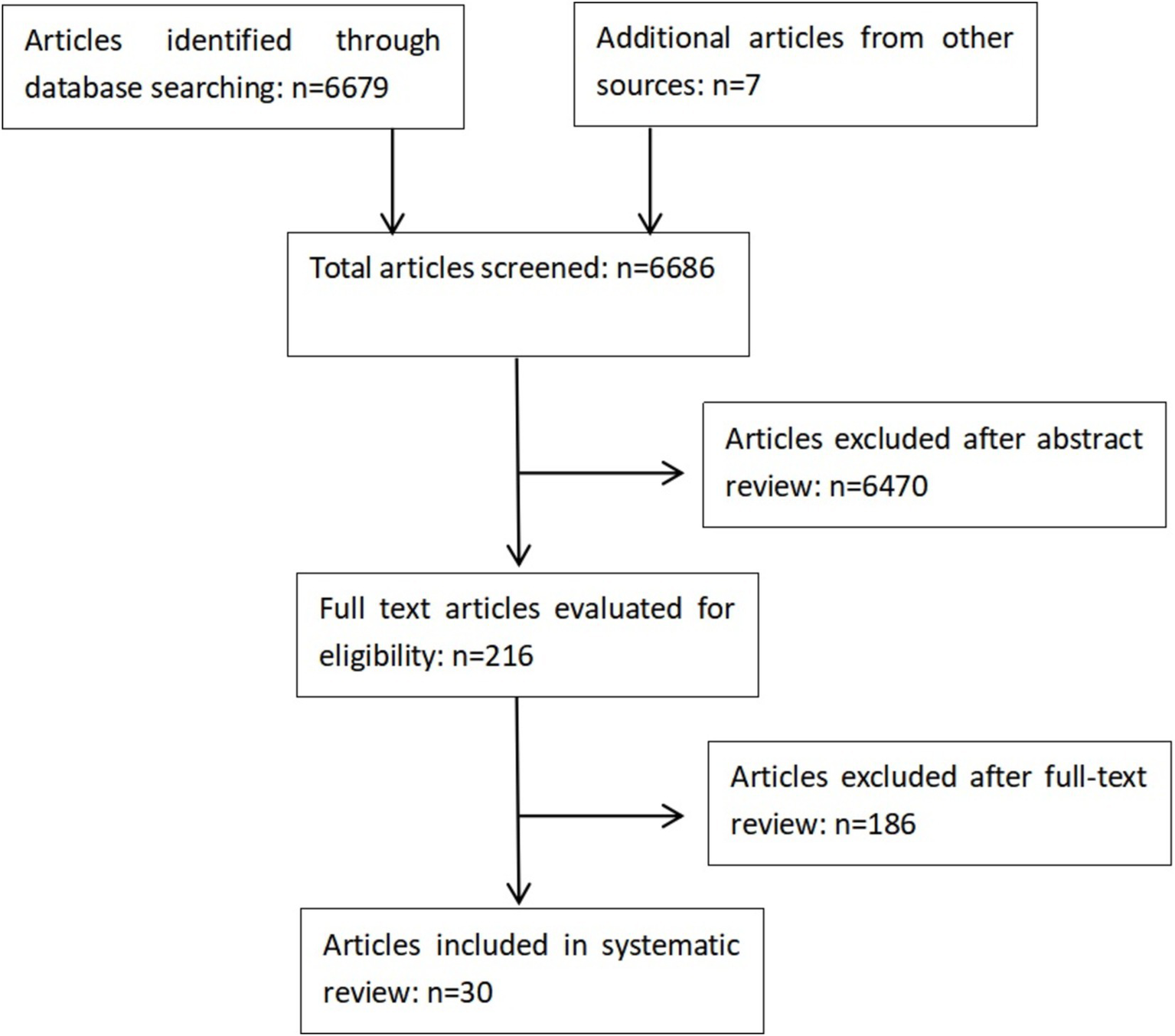
Study selection flowchart of the review.
Table 1
| Study | Training objective/device | Trainees | Assessment | Advantage | Disadvantage |
|---|---|---|---|---|---|
| Han, R. et al. (2) | Fractures and disorders associated with the orbit area /Three-dimensional Visualization Educational Modeling | First- and second-year ophthalmology residents | Satisfaction was reported 100% by residents | Visualization and mental stabilization; A clear understanding of bones; Spatial visualization with real dimensions; Bones position; Tangible models; Sustainability and a better understanding of content; Better training and easier to learn and memorize | Lack of staining of orbital bones; Lack of separation of skull bones; Uncertain suture of bones; Inadequate models of all disorders |
| Ramesh, V. et al. (3) | The real-time gonioscopic images and the 110-degree mosaic real-time true color confocal fundus images of various normal and pathological eyes /Eye MG 3D Application | Residents and students | – | Real-time images; providing various multimodal real-time images such as autofluorescence and infrared imaging | – |
| Halah, H. et al. (4) | Surgical training of ophthalmology / Three-Dimensional Heads-Up Display(HUD) | One hundred and forty ophthalmic surgeons participated in this study. Two-thirds of the participants had 10 years or less experience in the ophthalmology field | Forty-nine (68.1%) of the users found it a valuable educational tool. 60 (83.3%) users recommended its use in surgical training, and 50 (69.4%) recommended using it in general | The peripheral acuity and the depth perception is better in the HUD system than conventional microscopy. | – |
| Mustafa, S. et al. (5) | To teaching ocular ultrasound /a novel 3D ocular model | Ophthalmology students | – | Providing interactive teaching | – |
| Xiong, L. et al. (6) | To understand every extraocular muscles’ movement /3D electric ophthalmotrope | Medical students, who were registered for taking ophthalmology course from Medical Collage | By using 5-point Likert scale, The expert’s evaluation score for the imitation effect of medial rectus, lateral rectus, superior rectus, inferior rectus muscle, superior oblique and inferior oblique muscle were 5,5,5,5,3 and 4.The scores of the students with the 3D electric ophthalmotrope model were greater than those with the traditional anatomical model in the in-class quiz and final quiz | Intuitive and vivid | Promotion and application need higher cost and longer time |
| Famery, N. et al. (7) | Descemet’s membrane endothelial keratoplasty training / Artificial chamber and 3D ed. iris | Beginners and experienced DMEK surgeons | DMEK surgeons were significantly faster than beginners with both graft preparation and insertion time. The performance score correlated with the surgeon’s experience | Close to reality, feasible, resource-sparing and valid | Not all the steps of the Descemet’s membrane endothelial keratoplasty can be permitted to be performed in the model |
The list of the current 3D model for ophthalmic education.
Table 2
| Study | Training objective | Trainees | Assessment | Advantage | Disadvantage |
|---|---|---|---|---|---|
| Muntean, A. et al. (8) | Personalized Ophthalmology Residency Training | Ophthalmology Residents | The OSCE examination was used for the standardized evaluation of clinical performance of the Ophthalmology Residents | A daily case (real or from the Resident dataset) to solve; Personalized cases based on their needs with better coverage of the disease spectrum; Cases with a level of difficulty adapted to their current performance; A more uniform distribution of similar cases during the 1 year of practice; Feedback from the expert physician | – |
| Fang, Z. et al. (9) | Artificial intelligence-based pathologic myopia(PM) identification system in the ophthalmology residency training | Ophthalmology residents | All participants were satisfied and agreed that the AI-based PM identification system was effective and helpful to acquire PM identification, myopic maculopathy (MM) classification, and “Plus” lesion localization | Efficiency, convenience, innovative design, flexible learning style, self-learning ability, and self-motivation | Concerns about the hardware requirement, accuracy, and website stability of the AI-based platform |
| Han, R. et al. (10) | Diabetic retinopathy grading (DR) training | Junior ophthalmology residents and medical students | Through training, the average kappa score (calculated by combining the harmonic means of the DR classifications) was elevated | A feasible reading training method to improve the DR reading level of junior ophthalmologists | – |
The list of the current AI model for ophthalmic education.
Table 3
| Study | Training objective/device | Trainees | Assessment | Advantage | Disadvantage |
|---|---|---|---|---|---|
| Kekunnaya, R. et al. (11) | Virtual bedside clinics in pediatric ophthalmology and strabismus /the Zoom platform | Ophthalmology residents, fellows, sub-specialty ophthalmologists, general ophthalmologists, and optometrists | Comparing its effectiveness with conventional bedside clinics, respondents suggested that virtual bedside clinics were better/equally effective in the following techniques: general examination (96%), ocular motility (93.3%), nystagmus evaluation (93.3%), and anterior (80%) and posterior segment examination (73.3%) | Most of the bedside manners, procedural skills, and examination techniques can be effectively taught through this virtual platform with a scope to improve anterior and posterior segment examination skills | 5% of the respondents felt that the duration of the virtual individual session was too long/too short |
| Frisbie, J. et al. (12) | Virtual Medical Student Clinical Rotation for Ophthalmology /the Zoom platform | Medical Students | – | This technology can be utilized in the future not only to help increase exposure to the field, but help limit costs associated with traveling for rotations and create time-efficient opportunities for students wishing to gain ophthalmologic clinical experiences | – |
| Ramesh, V. et al. (13) | Virtual ophthalmic webinars / Green Mat technology | Ophthalmic postgraduate residents | – | Good clarity, interactivity, and creativity | – |
| Chan, P. et al. (14) | Diagnostic competency in retinopathy of prematurity (ROP) / tele-education system | Ophthalmology residents | Statistically significant changes of sensitivity for the diagnosis of plus disease, zone, stage, category, and aggressive posterior ROP and specificity for identification of stage 2 or worse were observed (p < 0.05) | Easy to use; feedback provided at the end of each case; more effectively to learn | – |
| Succar, T. et al. (15) | Virtual Ophthalmology Clinic learning / The Virtual Ophthalmology Clinic | Medical students | 56% of students rated it more effective than traditional methods | Helpful in medical students’ understanding of how an ocular history relates to the site of pathology | – |
| He, B. et al. (16) | Ophthalmology learning /Medskl.com | Medical students | Students found the greatest utility of modules was scheduling flexibility (92%) and individualization to learning needs (77%) | Inequities in accessing high-quality ophthalmology education can be mitigated with virtual learning | – |
| Saleh, M. et al. (17) | Cataract surgery training /Eyesi virtual reality (VR) simulator | Ophthalmic trainees with 2 h or less of simulation and intraocular surgical experience | Trainees’ overall performance improved significantly in the second attempt compared to the first time. (p < 0.0001) | Offering the quantitative description of trainees’ performance | – |
| Nilesh, R. et al. (18) | Continuous curvilinear capsulorhexis training /the Kitaro DryLab model (Frontier Vision Co., Ltd.), SimulEYE SimuloRhexis model (InsEYEt, LLC), and the Bioniko Rhexis (Bioniko Consulting LLC) | Ophthalmic surgeons | For the realistic simulation experience, the Kitaro, SimulEYE models and Bioniko model were 4.56 ± 0.84, 4.19 ± 0.92 and 1.38 ± 0.80 on a 7-point modified Likert scale | Providing high realistic simulation experience | – |
| Meredith, Weiss. et al. (19) | Endoscopic endonasal dacryocystorhinostomy training / the endoscopic endonasal surgery simulator | Ophthalmology residents | Residents who trained on the simulator performed significantly better compared with the group who trained on cadaver | Providing a quantified measure of a novice surgeon’s preparedness to perform surgery; as a teaching tool, the simulator offers the potential for standardization in resident education | – |
| Elisabeth, Feudner. et al. (20) | Capsulorhexis / the Eyesi (VRmagic, Mannheim, Germany) ophthalmic virtual reality surgical simulator | 31 medical students and 32 ophthalmological residents in postgraduate year (PGY) 1 to 5 | Residents also showed marked improvement for time scores whereas no obvious difference in time scores was observed for students. For students and residents taken together, subjects with a low number of attempts on training had a higher probability to perform well than the group with a higher number of attempts |
The potential exists to train a surgical novice to a high level of objectively measured skill before he or she is permitted to operate on a patient, and thus to improve the safety of patients facing surgery by a surgical novice. | No haptic feedback and fluid dynamics; Corneal or scleral incisions or suturing techniques cannot be practized |
| Cécile, C. et al. (21) | Vitreoretinal modules / the Eyesi (VRmagic, Mannheim, Germany) ophthalmic virtual reality surgical simulator | Fifteen residents with no vitreoretinal experience and six trained vitreoretinal surgeons (>100 procedures per year) | Experienced vitreoretinal surgeons outperformed residents with regard to the overall score on the navigation 1 (p = 0.01), forceps 1 (p < 0.01), epiretinal membrane peeling modules 1 and 2 (p = 0.02) and ERM2 (p = 0.04) modules | – | – |
| Charlotte, J. et al. (22) | Vitreoretinal surgical skills / the Eyesi (VRmagic, Mannheim, Germany) ophthalmic virtual reality surgical simulator | 10 junior residents without any surgical experience, 8 senior residents with prior experience in cataract surgery and 5 vitreoretinal surgeons | Senior residents significantly improved their simulator skills over time, reaching a plateau at the fifth iteration and equaling expert performance (p = 0.420) | – | – |
| Sukanya, M. et al. (23) | Vitreoretinal surgical Training / the Eyesi (VRmagic, Mannheim, Germany) ophthalmic virtual reality surgical simulator |
Retina fellows-in-training | Most (n = 25, 68%) respondents considered surgical simulators to be the best training tool before operating on the human eye. The majority (n = 33, 89%) of participants responded that VR surgical skills acquired during simulator training were transferrable to the operating room | – | – |
| Patrick, S. et al. (24) | Learning cataract surgery / the Eyesi ophthalmic virtual reality surgical simulator | The second year of ophthalmology residency for novice postgraduate year 3 (PGY-3) residents | The addition of surgical simulation training was associated with a significantly reduced rate of complications | – | – |
| Colin, M. et al. (25) | Continuous, curvilinear capsulorhexes (CCCs) during cataract surgery / the Eyesi (VRmagic, Mannheim, Germany) ophthalmic virtual reality surgical simulator | Resident surgeons at a teaching hospital with level of postgraduate year (PGY) | There was a statistical trend toward fewer errant CCCs among PGY 4 (14.6%) compared with PGY 3 (22.8%) surgeons (p = 0.12) | – | – |
| Colin, M. et al. (26) | Cataract surgery training / the Eyesi ophthalmic virtual reality surgical simulator | Resident postgraduate year (PGY) | Errant CCC was occurred in 24 of 47 (51.1%) in the “No Eyesi” group, and 8 of 58 (13.8%) in the “Capsulorhexis Intensive Training Curriculum for the Eyesi” group (p = 0.00016) | – | – |
| Tran, L. et al. (27) | A practice trial in the anterior segment training module, followed by 3 scored trials in the anterior forceps, antitremor, and capsulorhexis modules / the Eyesi (VRmagic, Mannheim, Germany) ophthalmic virtual reality surgical simulator | 4 medical students, 4 ophthalmic medical technologist trainees, 36 ophthalmology residents, 3 fellows, and 18 staff ophthalmologists | Participants with greater experience achieved significantly higher total scores than those who were less experienced(p = 0.011), with lower total task time (p = 0.044) and fewer injuries to the cornea (p = 0.001) and lens (p = 0.026) | – | Costly |
| Shameema, S. et al. (28) | Capsulorhexis Training of cataract surgery / MicroVisTouch™ (ImmersiveTouch, Chicago, IL, United States) | 78 ophthalmology residents | The improvement in all test variables was statistically significant (p < 0.05) | – | – |
| Chee, L. et al. (29) | Four main phacoemulsification cataract surgery procedures: corneal incision, capsulorhexis, phacoemulsification and intraocular lens implantation (IOL)/ prototype | 10 experienced ophthalmologists and 6 medical residents | Subjects with greater experience obtained significantly higher scores in all four main procedures. Positive correlation was observed between experience and anti-rupture | the VR simulators provide training modules for all the four main procedures of phacoemulsification cataract surgery | – |
| Ayşe, O. et al. (30) | Cataract surgical training / Eyesi simulator | Ophthalmic residents | – | Ideal to evaluate the effect of surgical environment on surgeon performance, including tiredness, visual acuity, use of the nondominant hand | – |
| Ya, H. et al. (31) | Chopping in cataract surgery/ Eyesi simulator | Ophthalmology residents | The residents in surgical-simulator training group got less corner area injured, and they spend less time than wet-lab training group (p < 0.05) | – | In wet lab, if the incision stress increased, the cornea would be deformed, which may blurred the clarity of visual field under surgical microscopy. The residents would notice this phenomenon. However, the residents in the by simulator might ignore it |
The list of the current VR model for ophthalmic education.
4 Novel techniques in ophthalmology education
4.1 Three-dimensional technology
In recent years, three-dimension (3D) technology has developed extensively in medical education, and it brings many advantages. 3D technology allows for the creation of detailed, interactive anatomical models that provide a more realistic representation of the human body compared with traditional 2 dimensional images or diagrams. This enhanced visualization can help students to gain a better understanding of anatomical structures and spatial relationships. Interactive 3D models and simulations can increase student engagement and motivation by providing a hands-on learning experience. 3D technology can be used to create realistic medical simulations that replicate clinical scenarios and procedures, enabling students to practice and refine their skills in a safe and controlled environment before working with real patients, which improves their confidence and competence. 3D technology can also be tailored to individual learning needs, allowing students to study at their own pace and focus on areas where they need additional practice. 3D technology has been used in ophthalmic education, and advantages and disadvantages are summarized in Table 1.
4.2 Better depth perception and closer to reality
3D models can provide a clear understanding of complicated spatial structures. A study by Vatankhah et al. (2) focused on the use of 3D models derived from CT scans for ophthalmology education. The researchers designed 3D models to aid in the visualization of complex anatomical structures, particularly in the orbital area. Satisfaction was reported as 100% by study participants. The results showed that the models significantly improved the participants’ understanding and retention of anatomical knowledge, highlighting the potential of 3D models as valuable educational tools. Ramesh et al. (3) described the development and application of the “Eye MG 3D” app. This app has a comprehensive 3D atlas of ocular anatomy and pathophysiology with real-time TrueColor confocal images, providing better understanding for students of complicated ocular anatomy and pathophysiology.
The superior benefits of peripheral acuity and depth perception in 3D surgical training are evident in current literature. Bin Helayel et al. (4) investigated the benefits of using a 3D heads-up display system compared with conventional microscopy for ophthalmic surgeries. Most participants (83.3%) recommended its use in surgical training due to its superior educational value. Mustafa et al. (5) presented a 3D educational tool designed to enhance the teaching of ocular ultrasound, which could improve trainees’ spatial awareness and understanding of ocular structures.
These educational models are intuitive and vivid, close to reality, and are able to provide better understanding and visualization. Lei et al. (6) developed a novel 3D electric ophthalmotrope to enhance the teaching effectiveness of ocular movements in ophthalmology. In the study, seven experts evaluated the 3D electric ophthalmotrope’s simulation ability and precision. Compared with the traditional anatomical model, the experts agreed that the 3D electric ophthalmotrope was easier for students to understand every extraocular muscle’s movement in each evaluation index. A randomized controlled trial demonstrated superior performance in both in-class quizzes and final exams for students taught with the 3D model compared with those using traditional models.
4.3 Feasible and resource-sparing
Famery et al. (7) presented a model for teaching Descemet membrane endothelial keratoplasty (DMEK) on an artificial anterior chamber with a 3D-printed iris. The study concluded that this model provided a resource-efficient opportunity for trainees.
4.4 Unable to simulate all the structures and all the steps of surgical procedures
In Vatankhah’s study (2), for example, the 3D printed skull lacked separation of the skull bones and was also unable to provide simulations for all orbital disorders. A study by Famery et al. (7) used a 3D-printed model to provide training for DMEK; however, the descemetorhexis part of the surgery could not be performed with the model.
4.5 Artificial intelligence for ophthalmology education
There are numerous advantages to using artificial intelligence (AI) in medical education. AI algorithms can tailor educational content to the specific needs of each student. AI-powered adaptive learning platforms can adjust the difficulty level of educational materials based on the student’s progress and performance, and AI-powered systems can provide real-time feedback to students on their performance, highlight areas for improvement, and offer personalized recommendations for further study. At present, there have been many studies on the application of AI in ophthalmology teaching, and the results have demonstrated the role of AI as a new technology in the field of ophthalmology teaching (Table 2).
4.6 Personalized training
Muntean et al. (8) presented a study investigating the use of AI for personalized ophthalmology residency training. The study focused on the development of an AI-based framework to enhance residency programs by ensuring a balanced distribution of cases among residents. The AI system matched cases to residents based on their training history and performance, with feedback from attending physicians to continually update residents’ portfolios. This approach could improve precision medical education by personalizing learning experiences and standardizing the training process for ophthalmology residents.
4.7 Promotion of self-motivation
A study by Fang et al. (9) evaluated the effectiveness of an AI-based pathologic myopia (PM) identification system in an ophthalmology residency training program. Results showed significant improvement in post-lecture scores for the group using the AI-based PM identification system compared with the group trained by traditional lectures. Evaluations by the residents revealed that the AI training model was perceived as better motivation than traditional didactic lectures.
4.8 Providing efficient, convenient, and flexible learning
AI training models also provide an efficient, convenient, and flexible learning style. A study by Fang (9) revealed that residents perceived the AI-based system to be effective, efficient, and beneficial for understanding PM identification and classification. Han et al. (10) investigated the efficiency of an AI reading label system for diabetic retinopathy grading training among junior ophthalmology residents and medical students. The AI system was found to be an effective training tool, significantly improving the diagnostic accuracy of junior ophthalmologists.
4.9 High demand for hardware devices
AI training models have many advantages. However, as mentioned by Fang (9), these advanced educational models need qualified hardware and a stable website for the AI-based platform, which affects their wide application.
4.10 Virtual education for ophthalmology education
There are significant advantages to virtual reality (VR) technology in medical education. VR simulations can replicate a wide range of medical scenarios, from surgical procedures to patient consultations, providing students with valuable hands-on experience in a safe and controlled environment. This enables students to practice skills and decision-making under realistic conditions, which improves their confidence and competence. Many VR technologies have already been applied to ophthalmology education (Table 3).
4.11 Stimulation of clinical procedures
Procedural skills and examination techniques can be effectively taught through a virtual platform to improve anterior and posterior segment examination skills. Kekunnaya et al. (11) piloted an innovative teaching method through live virtual bedside clinics for pediatric ophthalmology and strabismus, comparing its effectiveness with conventional bedside clinics. Over 95% of 287 survey respondents found that the virtual clinics were equally or more effective than traditional methods in teaching physical examination, clinical knowledge, reasoning, procedural skills, and communication.
4.12 Cost-effective
Frisbie et al. (12) developed a novel virtual clinical rotation for ophthalmology medical students at the University of Maryland School of Medicine, integrating mobile-mounted tablets, which allowed students to participate in inpatient consults, clinics, and ophthalmic surgeries remotely. The program included independent learning modules, video lectures, interactive sessions, and virtual wet laboratories. Feedback indicated high effectiveness in simulating in-person experiences, increased interactions with residents and faculty, and reduced costs associated with traveling for rotations. Ramesh et al. (13) introduced an innovative “green mat” technology—this cost-effective approach has proven beneficial for continuing medical education.
4.13 Remote learning
Chan et al. (14) described a tele-education system developed to improve diagnostic competency in retinopathy of prematurity (ROP). The tele-education system for ROP education was found to be easy to use and effective in improving the diagnostic accuracy of ophthalmology residents. This system may be useful in both healthcare and medical education reform settings by creating a validated method to certify telemedicine providers and educate the next generation of ophthalmologists.
4.14 Effective educational tool
Succar et al. (15) assessed the impact of the Virtual Ophthalmology Clinic (VOC) on medical students’ learning with a randomized controlled trial involving 188 students from the University of Sydney. Participants were divided into experimental and control groups, with the former using the VOC and the latter receiving traditional hospital-based teaching. Results revealed a significant improvement in the experimental group’s knowledge and long-term retention of ophthalmic information. At 12 months follow-up testing, the experimental group scored, on average, higher than the controls. The VOC was highly rated for its ability to enhance clinical reasoning and history-taking skills, demonstrating its effectiveness as an educational tool.
4.15 Providing equal educational opportunities
He et al. (16) conducted a survey to evaluate the effectiveness of a virtual ophthalmology education program among Canadian medical students. The program—which included synchronous webinars and asynchronous video modules—was well-received by students, who reported increased access to ophthalmology education and reduced feelings of social isolation. The authors suggested that inequities in accessing high-quality ophthalmology education can be mitigated with virtual learning.
4.16 Standardization of education
A VR study model can also offer a quantitative description of trainees’ performance. Saleh et al. (17) evaluated the variability of performance among novice ophthalmic trainees using the EyeSi VR simulator. The study quantified the reproducibility of novice performance with the VR tool. Studies have shown that VR surgical simulators can provide a highly realistic simulation experience (18). As a teaching tool, the simulator has potential for standardization in resident’s education (19). VR training can provide quantitative evaluation for trainees under the same training standard and allow as much training as necessary to achieve the training goal without the need for continuous supervision or taking surgical risks (20–31).
4.17 Inability to simulate all the steps of surgical procedures
VR simulators were unable to provide all the surgical training steps. The EyeSi’s—the most widely applied ophthalmic simulator worldwide—cataract training modules, for example, do not include corneal incision and intraocular lens implantation, which are essential steps in cataract surgery training (20–27, 29–31).
4.18 Inability to simulate all the situations of surgical procedures
Existing ophthalmic simulators cannot simulate all the situations in real surgery. In the wet lab, if incisional stress increased, the cornea would be deformed, which may blur the clarity of the visual field under surgical microscopy,—ophthalmology residents would notice this phenomenon. However, residents using a simulator have been found to ignore it (31). Most ophthalmic simulators have no haptic feedback. As discussed by Feudner et al. (20), on EyeSi, the only haptic input comes from the fulcrum effect of the rigid plastic wall of the eye model; there is no haptic feedback from intraocular tissues. In contrast, during real surgery, there is haptic feedback from intraocular tissues as well as from the eye wall. Moreover, corneal and scleral rigidity are not constant but may change considerably during surgery depending on intraocular pressure (20). Ophthalmic simulators have no fluid dynamics. Feudner et al. (20) also noted a drawback with regard to fluid dynamics—to date, changes of anterior chamber depth (e.g., due to fluid leakage because of excessive incision stress) are not simulated; however, they are an important source of surgical complications.
4.19 Costly
As mentioned by Tran et al. (27), ophthalmic simulators are costly and cannot be used in all institutions.
5 Discussion
Vision has a significant impact on the quality of life. Misdiagnosis and delayed diagnosis lead to demonstrated poor outcomes, including permanent vision loss and severe pain (1). High-quality ophthalmic education is of vital importance to assist patients to maintain ocular health. Effective education could help junior ophthalmologists to identify and manage various eye conditions promptly, thereby preventing further damage and preserving vision.
A recently published systematic (1) review demonstrated that the amount of ophthalmology teaching in medical schools has been declining globally for two decades. In ophthalmology assessments, on average, students do not score highly for either their knowledge or their skills. Approximately three-quarters of students are not confident in their knowledge, and two-thirds are not confident in their skills. Spencer et al. (1) noted that most studies note that a reduction in the length of ophthalmology courses over the last 20 years is the reason for the decline in ophthalmology education globally. A nationwide survey of 840 medical students and junior doctors in Australia found that only five participants believed that the ophthalmology teaching they had received was sufficient (32).
Ophthalmology educational technologies continue to evolve, which may help to bridge the gap in declining teaching time and may result in a trend away from didactic lecture-style education to methods with improved student interaction, enjoyment, and time efficiency.
Additionally, the traditional teaching method of ophthalmology is deficient. Surgical education has traditionally relied on an apprenticeship teaching model. The quality of teaching is highly dependent on the mentor’s surgical and teaching abilities, which leads to variability in how trainees learn and acquire surgical skills (33). While various assessment tools have been created to standardize the evaluation of surgical skills, these modalities are subjective because the grading is performed by humans (34, 35). Moreover, the use of these tools remains limited in clinical practice and surgical curricula, partially due to resource limitations, which require an expert observer for grading (36, 37). Quantifiable, objective, and standardized methods to teach and assess surgical skills, especially between mentors and across institutions, are currently lacking in surgical education.
The application of 3D technology is noteworthy as a useful tool in surgical training. The application of 3D simulators in medical training has been transformative, offering numerous benefits and opportunities to improve medical education and patient outcomes. 3D simulators can replicate the exact anatomical structures of patients and provide highly realistic models for training, which are essential for understanding spatial relationships and practicing surgical techniques. Practicing on a 3D simulator could reduce the risks associated with the first-time performance of new or intricate surgical procedures on actual patients. Compared with traditional surgical training methods, such as cadaveric dissection or live animal models, which can be expensive, 3D simulators offer a more cost-effective and accessible alternative (38). 3D models have been used increasingly for medical education, with research highlighting their value in different types of surgery, including oral and maxillary (39–41), otorhinolaryngology (42–50), neurosurgery training (51–56), orthopedics (57, 58), and urinary surgery training (59–62).
The numerous advantages of 3D teaching models are also present in ophthalmology education. The 3D model of orbit (2), the extraocular muscles model (6), and the artificial chamber (7) have demonstrated that 3D models are intuitive and vivid education tools, with real spatial visualization, thereby providing a highly realistic simulation experience. These 3D models also have been identified as feasible and valid training tools, which are easy to use and could provide convenient and flexible learning for medical students (2, 7).
AI technology—a constantly developing field—has made significant progress in education, health, industry, and many other sectors. These technologies, especially in education and learning, have great potential to provide students with personalized learning experiences, optimize learning processes, provide additional resources, and improve the quality of education (63). AI models in ophthalmic education are feasible training tools, which can provide personalized training (8), promote self-motivation (9), and create time-efficient opportunities for students (12).
Clinical teaching is often conducted using real patients, and this method can sometimes be very challenging due to the comfort of patients or time constraints in a busy clinic. Due to the increased health consciousness and awareness of the public, patients often expect the doctors to be experienced instead of being treated as “guinea pigs” by students who have just entered residency training or are still in medical school (64).
Kekunnaya’s study (11), which compared the effectiveness of conventional bedside clinics with that of virtual clinics, found that virtual bedside clinics were better/equally effective for the following techniques: general examination (96%), ocular motility (93.3%), nystagmus evaluation (93.3%), and anterior (80%) and posterior segment examination (73.3%). Most bedside manners, procedural skills, and examination techniques can be effectively taught through this virtual platform, with potential to improve anterior and posterior segment examination skills. This also helps residents to build confidence without causing any harm to the patient.
VR training models can train surgical novices to a high level of objectively measured skill before they are permitted to operate on a patient, thus improving patient safety when facing surgery by a surgical novice (20–31). Most models can provide a quantitative description of the trainee’s performance. As a teaching tool, the models have potential for standardization in residents’ education (20–27, 30, 31).
Advanced educational techniques share similar advantages, for example, they are all intuitive and vivid training tools (2, 6, 7, 18), and they are all effective, flexible, and convenient to use (2, 7, 9–11, 14). However, these high-tech modern educational techniques also have common defects. Neither 3D training models nor VR educational models can simulate all the procedures of ophthalmic surgeries (7, 20–27, 30, 31). More importantly, all these models are unable to simulate the complete real experience of clinical practice. To use cataract surgery training as an example, incompetent control of fluid dynamics could lead to changes of anterior chamber depth, which is a significant cause of cataract surgical complications. None of the training models can currently provide simulation of fluid dynamics (17, 18, 20, 24–26, 28–31). Therefore, in spite of numerous advantages, conventional education, especially in surgical training, cannot be replaced.
Nevertheless, the development and promotion of advanced ophthalmic educational techniques have enormous significance. These are effective training tools that can promote the clinical ability of students (4, 6, 9–11, 14, 15, 17, 19, 20, 22–26, 29, 31). They are easy, convenient, and flexible to use (8–10, 13) and can create more time-efficient opportunities for students. They are also resource-sparing (6, 11). Such tools can promote students’ self-learning ability and self-motivation (8). They can also mitigate the inequities in accessing high-quality ophthalmology education (15).
6 Conclusion
The application of 3D technology, AI, and virtual education methods in ophthalmology education is significantly advancing. These approaches not only improve knowledge retention and practical skills but also make education more accessible and engaging. As these technologies continue to evolve, their integration into medical curricula holds promise for further enhancing ophthalmology training and practice.
Statements
Author contributions
YJ: Writing – original draft. HJ: Writing – review & editing. ZY: Writing – review & editing. YL: Writing – review & editing. YC: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Beijing Health Achievements in Technology and Effective Technology Transfer Foundation (BHATET2024-03).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Sascha S Patrick I Jorja B Jenny H Michael L Helen Z et al . A systematic review of ophthalmology education in medical schools: the global decline. Ophthalmology. (2024) 131:855–63. doi: 10.1016/j.ophtha.2024.01.005
2.
Vatankhah R DadgarMoghadam M Sadeghi T . 3D visualization educational modeling for ophthalmology. Med J Islam Repub Iran. (2022) 36:115.
3.
Ramesh PV Devadas AK Joshua T Ray P Ramesh SV Raj PM et al . Eye MG 3D application - a comprehensive ocular anatomy and pathophysiology 3D atlas with real-time true color confocal images to enhance ophthalmology education and e-counseling. Indian J Ophthalmol. (2022) 70:1388–94. doi: 10.4103/ijo.IJO_2282_21
4.
Halah H Al-M S Adel A . Can the three-dimensional heads-up display improve ergonomics, surgical performance, and ophthalmology training compared to conventional microscopy?Clin Ophthalmol. (2021) 15:679–86. doi: 10.2147/OPTH.S290396
5.
Mustafa MS Montgomery J Atta HR . A novel educational tool for teaching ocular ultrasound. Clin Ophthalmol. (2011) 5:857–60. doi: 10.2147/OPTH.S19087
6.
Xiong L Ding XY Fan YZ Xing Y Zhang XH Li T et al . A novel three-dimensional electric ophthalmotrope for improving the teaching of ocular movements. Int J Ophthalmol. (2019) 12:1893–7. doi: 10.18240/ijo.2019.12.12
7.
Famery N Abdelmassih Y El-Khoury S Guindolet D Cochereau I Gabison EE . Artificial chamber and 3D ed iris: a new wet lab model for teaching Descemet's membrane endothelial keratoplasty. Acta Ophthalmol. (2019) 97:e179–83. doi: 10.1111/aos.13852
8.
Muntean GA Groza A Marginean A Slavescu RR Steiu MG Muntean V et al . Artificial intelligence for personalised ophthalmology residency training. J Clin Med. (2023) 12:1825. doi: 10.3390/jcm12051825
9.
Fang Z Xu Z He X Han W . Artificial intelligence-based pathologic myopia identification system in the ophthalmology residency training program. Front Cell and Develop Biol. (2022) 10:1053079. doi: 10.3389/fcell.2022.1053079
10.
Han R Yu W Chen H Chen Y . Using artificial intelligence reading label system in diabetic retinopathy grading training of junior ophthalmology residents and medical students. BMC Med Educ. (2022) 22:258. doi: 10.1186/s12909-022-03272-3
11.
Kekunnaya R Deshmukh AV Sheth J Chattannavar G Sachadeva V . Virtual bedside clinics in pediatric ophthalmology and strabismus – an innovation in education and learning. Indian J Ophthalmol. (2022) 70:3129–33. doi: 10.4103/ijo.IJO_357_22
12.
Frisbie J Cornman H Swamy R Alexander JL Kemp PS Friedrich R et al . A novel interactive virtual medical student clinical rotation for ophthalmology. J Academic Ophthalmol. (2022) 14:e52–9. doi: 10.1055/s-0042-1743410
13.
Ramesh PV Ramesh SV Ray P Aji K Raj PM Akkara JD et al . New-age innovative pedagogy for virtual ophthalmic webinars with green mat technology - a unique communication tool for continuing medical education in e-ophthalmology during the COVID-19 pandemic. Indian J Ophthalmol. (2021) 69:3768–71. doi: 10.4103/ijo.IJO_2197_21
14.
Chan RVP Patel SN Ryan MC Jonas KE Ostmo S Port AD et al . The global education network for retinopathy of prematurity (GEN-ROP): development, implementation, and evaluation of a novel tele-education system (an American ophthalmological society thesis). Trans Am Ophthalmol Soc. (2015) 113:21–6.
15.
Succar T Zebington G Billson F Byth K Barrie S McCluskey P et al . The impact of the virtual ophthalmology clinic on medical students' learning: a randomised controlled trial. Eye (Lond). (2013) 27:1151–7. doi: 10.1038/eye.2013.143
16.
He B Tanya S Sharma S . Perspectives on virtual ophthalmology education among Canadian medical students. Can J Ophthalmol. (2020) 56:208–9. doi: 10.1016/j.jcjo.2020.09.021
17.
Saleh GM Theodoraki K Gillan S Sullivan P O’Sullivan F Hussain B et al . The development of a virtual reality training programme for ophthalmology: repeatability and reproducibility (part of the international forum for ophthalmic simulation studies). Eye. (2013) 27:1269–74. doi: 10.1038/eye.2013.166
18.
Raval N Hawn V Kim M Xie X Shrivastava A . Evaluation of ophthalmic surgical simulators for continuous curvilinear capsulorhexis training. J Cataract Refract Surg. (2022) 48:611–5. doi: 10.1097/j.jcrs.0000000000000820
19.
Weiss M Lauer SA Fried MP Uribe J Sadoughi B . Endoscopic endonasal surgery simulator as a training tool for ophthalmology residents. Ophthalmic Plast Reconstr Surg. (2008) 24:460–4. doi: 10.1097/IOP.0b013e31818aaf80
20.
Feudner EM Engel C Neuhann IM Petermeier K Bartz-Schmidt K-U Szurman P . Virtual reality training improves wet-lab performance of capsulorhexis: results of a randomized, controlled study. Graefes Arch Clin Exp Ophthalmol. (2009) 247:955–63. doi: 10.1007/s00417-008-1029-7
21.
Cissé C Angioi K Luc A Berrod J-P Conart J-B . EYESI surgical simulator: validity evidence of the vitreoretinal modules. Acta Ophthalmol. (2019) 97:e277–82. doi: 10.1111/aos.13910
22.
Jaud C Salleron J Cisse C Angioi-Duprez K Berrod J-P Conart J-B . EyeSi surgical simulator: validation of a proficiency-based test for assessment of vitreoretinal surgical skills. Acta Ophthalmol. (2021) 99:390–6. doi: 10.1111/aos.14628
23.
Mondal S Kelkar AS Singh R Chaitra Jayadev VR . What do retina fellows-in-training think about the vitreoretinal surgical simulator: a multicenter survey. Indian J Ophthalmol. (2023) 71:3064–8. doi: 10.4103/IJO.IJO_381_23
24.
Staropoli PC Gregori NZ Junk AK Galor A Goldhardt R Goldhagen BE et al . Surgical simulation training reduces intraoperative cataract surgery complications among residents. Simul Healthc. (2018) 13:11–5. doi: 10.1097/SIH.0000000000000255
25.
McCannel CA Reed DC Goldman DR . Ophthalmic surgery simulator training improves resident performance of capsulorhexis in the operating room. Ophthalmology. (2013) 120:2456–61. doi: 10.1016/j.ophtha.2013.05.003
26.
McCannel CA . Continuous curvilinear Capsulorhexis training and non-Rhexis related vitreous loss: the specificity of virtual reality simulator surgical training (an American ophthalmological society thesis). Trans Am Ophthalmol Soc. (2017) 22:115.
27.
Le TDB Adatia FA Lam W-C . Virtual reality ophthalmic surgical simulation as a feasible training and assessment tool: results of a multicentre study. Can J Ophthalmol. (2011) 46:56–60. doi: 10.3129/i10-051
28.
Sikder S Jia Luo P Banerjee P Luciano C Kania P Song JC et al . The use of a virtual reality surgical simulator for cataract surgical skill assessment with 6 months of intervening operating room experience. Clin Ophthalmol. (2015) 9:141–9. doi: 10.2147/OPTH.S69970
29.
Lam CK Sundaraj K Sulaiman MN Qamarruddin FA . Virtual phacoemulsification surgical simulation using visual guidance and performance parameters as a feasible proficiency assessment tool. BMC Ophthalmol. (2016) 16:88. doi: 10.1186/s12886-016-0269-2
30.
Oflaz AB Köktekir BE Okudan S . Does cataract surgery simulation correlate with real-life experience?Turk J Ophthalmol. (2018) 48:122–6. doi: 10.4274/tjo.10586
31.
Hu Y-G Liu Q-P Gao N Wu C-R Zhang J Qin L et al . Efficacy of wet-lab training versus surgical-simulator training on performance of ophthalmology residents during chopping in cataract surgery. Int J Ophthalmol. (2021) 14:366–70. doi: 10.18240/ijo.2021.03.05
32.
Zhang HH Hepschke JL Shulruf B Francis IC Spencer SKR Coroneo M et al . Sharpening the focus on ophthalmology teaching: perceptions of medical students and junior medical officers. Clin Experiment Ophthalmol. (2018) 46:984–93. doi: 10.1111/ceo.13342
33.
Pan-Doh N Sikder S Woreta FA Handa JT . Using the language of surgery to enhance ophthalmology surgical education. Surg Open Sci. (2023) 14:52–9. doi: 10.1016/j.sopen.2023.07.002
34.
Puri S Sikder S . Cataract surgical skill assessment tools. J Cataract Refract Surg. (2014) 40:657–65. doi: 10.1016/J.JCRS.2014.01.027
35.
Alnafisee N Zafar S Vedula S Sikder S . Current methods for assessing technical skill in cataract surgery. J Cataract Refract Surg. (2021) 47:256–64. doi: 10.1097/J.JCRS.0000000000000322
36.
Vedula SS Ishii M Hager GD . Objective assessment of surgical technical skill and competency in the operating room. Annu Rev Biomed Eng. (2017) 19:301–25. doi: 10.1146/ANNUREV-BIOENG-071516-044435
37.
Lam K Chen J Wang Z Iqbal FM Darzi A Lo B et al . Machine learning for technical skill assessment in surgery: a systematic review. NPJ Digit Med. (2022) 5:24. doi: 10.1038/S41746-022-00566-0
38.
Jiang Y Jiang H Yang Z Li Y . The current application of 3D simulator in surgical training. Front Med (Lausanne). (2024) 11:1443024. doi: 10.3389/fmed.2024.1443024
39.
Seifert LB Schnurr B Herrera-Vizcaino C Begic A Thieringer F Schwarz F . 3D- ed patient individualised models vs cadaveric models in an undergraduate oral and maxillofacial surgery curriculum: comparison of student's perceptions. Eur J Dent Educ. (2020) 24:799–806. doi: 10.1111/eje.12522
40.
Nica DF Gabor AG Duma V-F Tudericiu VG Tudor A Sinescu C . Sinus lift and implant insertion on 3D- ed polymeric maxillary models: ex vivo training for in vivo surgical procedures. J Clin Med. (2021) 10:1–15. doi: 10.3390/jcm10204718
41.
Sonkaya E Bek Kürklü ZG . Comparisons of student comprehension of 3D- ed, standard model, and extracted teeth in hands-on sessions. Eur J Dent Educ. (2023) 28:452–60.
42.
Alrasheed AS Nguyen LHP Mongeau L Funnell WRJ Tewfik MA . Development and validation of a 3D- ed model of the ostiomeatal complex and frontal sinus for endoscopic sinus surgery training. Int Forum of Allergy & Rhinol. (2017) 7:837–41. doi: 10.1002/alr.21960
43.
Suzuki M Miyaji K Watanabe R Suzuki T Matoba K Nakazono A et al . Repetitive simulation training with novel 3D- ed sinus models for functional endoscopic sinus surgeries. Laryngoscope Investigative Otolaryngol. (2022) 7:943–54. doi: 10.1002/lio2.873
44.
Barber SR Kozin ED Dedmon M Lin BM Lee K Sinha S et al . 3D- ed pediatric endoscopic ear surgery simulator for surgical training. Int J Pediatr Otorhinolaryngol. (2016) 90:113–8. doi: 10.1016/j.ijporl.2016.08.027
45.
Chien WW da Cruz MJ Francis HW . Validation of a 3D- ed human temporal bone model for otology surgical skill training. World J Otorhinolaryngol Head and Neck Surg. (2021) 7:88–93. doi: 10.1016/j.wjorl.2020.12.004
46.
Frithioff A Frendø M Weiss K Foghsgaard S Pedersen DB Sørensen MS et al . Effect of 3D- ed models on cadaveric dissection in temporal bone training. OTO Open. (2021) 5:1–7. doi: 10.1177/2473974X211065012
47.
Iannella G Pace A Mucchino A Greco A De Virgilio A Lechien JR et al . A new 3D- ed temporal bone: ‘the SAPIENS’—specific anatomical ed-3D-model in education and new surgical simulations. Eur Arch Otorrinolaringol. (2024) 281:4617–26. doi: 10.1007/s00405-024-08645-6
48.
Nguyen Y Mamelle E De Seta D Sterkers O Bernardeschi D Torres R . Modifications to a 3D- ed temporal bone model for augmented stapes fixation surgery teaching. Eur Arch Otorrinolaringol. (2017) 274:2733–9. doi: 10.1007/s00405-017-4572-1
49.
Takahashi K Morita Y Ohshima S Izumi S Kubota Y Yamamoto Y et al . Creating an optimal 3D ed model for temporal bone dissection training. Ann Otol Rhinol Laryngol. (2017) 126:530–6. doi: 10.1177/0003489417705395
50.
Narayanan V Narayanan P Rajagopalan R Karuppiah R Rahman ZAA Wormald P-J et al . Endoscopic skull base training using 3D simulator with pre-existing pathology. Eur Arch Otorrinolaringol. (2015) 272:753–7. doi: 10.1007/s00405-014-3300-3
51.
Nebor I Hussein AE Montemagno K Fumagalli R Labiad I Xu A et al . Primary Dural repair via an endoscopic Endonasal corridor: preliminary development of a 3D- ed model for training. Journal of neurological surgery part B. Skull Base. (2022) 83:e260–5. doi: 10.1055/s-0041-1725027
52.
Uhl JF Sufianov A Ruiz C Iakimov Y Mogorron HJ Encarnacion Ramirez M et al . The use of 3D simulator for surgical simulation of cranioplasty in craniosynostosis as training and education. Brain Sci. (2023) 13:894. doi: 10.3390/brainsci13060894
53.
Zhu J Wen G Tang C Zhong C Yang J Ma C . A practical 3D- ed model for training of endoscopic and Exoscopic intracerebral hematoma surgery with a tubular retractor. J Neurolog Surg Part A: Central European Neurosurg. (2020) 81:404–11. doi: 10.1055/s-0039-1697023
54.
Zheng J-P Li C-Z Chen G-Q . Multimaterial and multicolor 3D- ed model in training of transnasal endoscopic surgery for pituitary adenoma. Neurosurg Focus. (2019) 47:E21. doi: 10.3171/2019.6.FOCUS19294
55.
Encarnacion Ramirez M Ramirez Pena I Barrientos Castillo RE Sufianov A Goncharov E Soriano Sanchez JA et al . Development of a 3D ed brain model with vasculature for neurosurgical procedure visualisation and training. Biomedicine. (2023) 11:1–10. doi: 10.3390/biomedicines11020330
56.
Byvaltsev V Polkin R Bereznyak D Giers MB Hernandez PA Shepelev V et al . 3D- ed cranial models simulating operative field depth for microvascular training in neurosurgery. Surg Neurol Int. (2021) 12:213–12. doi: 10.25259/SNI_849_2020
57.
Papavasiliou T Nicholas R Cooper L Chan JCY Ibanez J Bain CJ et al . Utilisation of a 3D ed ex vivo flexor tendon model to improve surgical training. J Plast Reconstr Aesthet Surg. (2022) 75:1255–60. doi: 10.1016/j.bjps.2021.11.027
58.
Neijhoft J Henrich D Mörs K Marzi I Janko M . Visualization of complicated fractures by 3D- ed models for teaching and surgery: hands-on transitional fractures of the ankle. Eur J Trauma Emerg Surg. (2022) 48:3923–31. doi: 10.1007/s00068-022-01879-1
59.
Campi R Pecoraro A Vignolini G Spatafora P Sebastianelli A Sessa F et al . The first entirely 3D- ed training model for robot-assisted kidney transplantation: the RAKT box. European Urology Open Sci. (2023) 53:98–105. doi: 10.1016/j.euros.2023.05.012
60.
Wong NC Hoogenes J Guo Y Quantz MA . Techniques: utility of a 3D ed bladder model for teaching minimally invasive urethrovesical anastomosis. Can Urol Assoc J. (2017) 11:E321–2. doi: 10.5489/cuaj.4262
61.
Reilly Scott E Singh A Quinn AM Morano S Karp A Boyd K et al . The use of individualized 3D- ed models on trainee and patient education, and surgical planning for robotic partial nephrectomies. J Robot Surg. (2023) 17:465–72. doi: 10.1007/s11701-022-01441-6
62.
Hermans T Snoeks JM vom Dorp F Wiesner C Steiner T von Rundstedt F-C . Validation of a 3D- ed robot-assisted partial nephrectomy training model. BJUI Compass. (2023) 5:90–100. doi: 10.1002/bco2.269
63.
Owoc ML Sawicka A Weichbroth P . Artificial intelligence technologies in education: benefits, challenges and strategies of implementation. IFIP Advan Info Commun Technol. (2019) 8:37–58. doi: 10.1007/978-3-030-85001-2_4
64.
Ting DSW Sim SSKP Yau CWL Rosman M Aw AT Yeo IYS . Ophthalmology simulation for undergraduate and postgraduate clinical education. Int J Ophthalmol. (2016) 9:920–4. doi: 10.18240/ijo.2016.06.22
Summary
Keywords
three-dimensional, artificial intelligence, virtual reality, ophthalmology, education
Citation
Jiang Y, Jiang H, Yang Z, Li Y and Chen Y (2024) The application of novel techniques in ophthalmology education. Front. Med. 11:1459097. doi: 10.3389/fmed.2024.1459097
Received
03 July 2024
Accepted
24 October 2024
Published
14 November 2024
Volume
11 - 2024
Edited by
Jinhai Huang, Fudan University, China
Reviewed by
Haijiang Lin, University of Massachusetts Medical School, United States
Qingwei Zhang, Capital Medical University, China
Yau Kei Chan, The University of Hong Kong, Hong Kong SAR, China
Updates
Copyright
© 2024 Jiang, Jiang, Yang, Li and Chen.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhikun Yang, yangzhikun@pumch.cnYing Li, liying6007@pumch.cnYouxin Chen, chenyouxinpumch@163.com
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.