Abstract
Introduction:
The study aims to develop a prediction model to differentiate transient ischemia from irreversible transmural necrosis in closed-loop small bowel obstruction (CL-SBO).
Methods:
A total of 180 participants with CL-SBO between January 2010 and December 2019, of which 122 had complete radiologic data, were included to investigate the significant clinical and imaging characteristics for differentiating patients with necrosis from transient ischemia. A logistic regression model was developed and validated.
Results:
In a multivariate analysis, the American Society of Anesthesiologists physical status classification system >2 is the independent predictor for transmural necrosis. Another multivariate analysis, including clinical and imaging factors, revealed that the imaging sign of mesenteric vessel interruption was an independent risk factor for necrosis. The diagnostic model developed using these two factors has excellent performance among the validation sets, with an area under the curve of 0.89.
Conclusion:
The diagnostic model and innovative imaging signs have substantial potential in solving this complex clinical problem.
1 Introduction
Small bowel obstruction (SBO) is one of the most common acute abdomen diseases, with approximately 96,307 and 45,178 cases reported in China and the USA, respectively, according to the Global Burden of Disease Study 2019 (1). About 10% of SBO patients with intestinal ischemia are classified as strangulated small bowel obstruction (SSBO). SSBO is primarily caused by closed-loop small bowel obstruction (CL-SBO), which involves the mechanical obstruction of a bowel loop at two adjacent points and compression of the vascular pedicle (2–4). Internal hernia and adhesive bands are common causes of CL-SBO. CL-SBO typically leads to two distinct outcomes: transient ischemia and transmural necrosis (5). Most patients diagnosed with CL-SBO should undergo emergent surgical exploration to avoid life-threatening complications (2, 6), although some highly selected patients may benefit from non-surgical management (7, 8). The blood supply for bowel loops can be restored for transient intestinal ischemia after releasing the obstruction during the operation. Conversely, necrotic bowel segments must be resected for transmural necrosis (8, 9). Transmural necrosis is one of the most severe consequences of SBO and needs emergency treatment as soon as possible to reduce lethal complications (3, 10). Unlike laparoscopic adhesiolysis, which is suitable for some patients with transient intestinal ischemia, transmural necrosis carries a high risk of diffuse peritonitis, septic shock, and bowel perforation, making it a relative contraindication for laparoscopic surgery (11). The severity and process flow differences make preoperative differentiation of transient ischemia from transmural necrosis essential among CL-SBO patients.
Some researchers focus on clinical characteristics, including medical history, clinical symptoms, physical examination results, and laboratory indicators, which unfortunately lack sufficient sensitivity and specificity to accurately distinguish between transient ischemia and necrosis in SSBO patients (12). In terms of imaging examinations, there is a consensus on the use of computed tomography (CT), which can comprehensively provide information on the cause, location and extent of obstruction when evaluating patients with SBO, especially with unenhanced CT, known for its convenience and efficiency (2, 13). However, when diagnosing CL-SBO, CT demonstrates suboptimal diagnostic performance, with a sensitivity of 53% and specificity of 83% (14). The unsatisfactory performance of clinical or CT features in diagnosing SBO subtypes prompts reconsideration of preoperative differentiation among the various subtypes of CL-SBO (15–18). This study explores significant clinical and CT features that can accurately identify transient ischemia and transmural necrosis of CL-SBO prior to surgery, potentially aiding surgeons in developing more timely and comprehensive operative plans.
2 Materials and methods
2.1 Patient selection and data collection
The Institutional Ethics Committee of Peking University First Hospital approved this retrospective study, and informed consent was obtained from all participants. Eight hundred thirty-three patients diagnosed with intestinal obstruction who underwent surgery between January 2010 and August 2022 were identified from the institution’s database. CL-SBO was defined as mechanical obstruction of a bowel loop at two adjacent points, accompanied by compression of the vascular pedicle. The final diagnosis of CL-SBO was made intraoperatively, with terms such as “closed loop obstruction” or “multiple zones of transition” documented in the surgical report. The following exclusion criteria were applied: (a) Patients with colorectal obstruction; (b) Patients with an abdominal external hernia; (c) Patients with small bowel obstruction without a closed loop, including vascular occlusion-associated SBO, simple adhesive SBO, paralytic ileus, or obstruction caused by space-occupying lesions (e.g., tumor, bezoar, polyp) or intussusception. Ultimately, 242 patients with colorectal obstruction, 47 with an abdominal external hernia, 26 with space-occupying lesions in the small intestine, 257 with simple adhesive SBO, and 31 with vascular intestinal obstruction were excluded, leaving 230 participants with CL-SBO in the study. The classification of CL-SBO was confirmed during the operation. Transmural necrosis was confirmed when the dark purple-colored intestinal segment did not return to its normal color within 20 min after surgical release of the obstruction, as previously described (2), and was further confirmed by histologic analysis. The study included patients with CL-SBO between January 2010 and August 2022, including 118 patients with transmural necrosis who underwent partial enterectomy, and 112 with transient ischemia relieved after the obstruction was cleared. The screening process for this study is shown in Supplementary Figure S1.
Clinical and demographic parameters, including gender, age, body mass index (BMI), American Society of Anesthesiologists (ASA) physical status classification system, admission symptoms (abdominal pain, vomiting, exhaust or defecation), vital signs, history of abdominal surgery or infection, preoperative stomach tube placement, preoperative anti-inflammatory treatment, time from onset to operation (hours), percentage of neutrophils, percentage of lymphocytes, and the neutrophil-to-lymphocyte ratio (NLR) were considered. These data were collected by the surgeon S.P.
2.2 CT acquisition
Between January 2010 and December 2019, one hundred and twenty -two (122/180) patients have complete radiographic data from our institution, with the interval between CT and surgery being within 24 h. For patients between January 2020 and August 2022, 50 patients included in this study also had complete radiographic data from our institution, with the CT – surgery interval within 24 h. All of these patients underwent unenhanced CT. The CT examinations were performed using multislice spiral CT machines, including the Philips Brilliance 64 or Philips Brilliance iCT (Philips Medical Systems, Cleveland, OH, USA); GE Discovery CT750 m or GE LightSpeed VCT (GE Healthcare, Princeton, NJ, USA); Siemens Somatom Sensation 64 (Siemens, Forchheim, Germany). The spiral CT parameters were: 120 kV tube voltage, 150–250 mA tube current, 0.5–0.8 s tube rotation time, 64 × 0.625 mm detector collimation, 350 × 350 mm field of view, 512 × 512 matrices, 1.25 mm section thickness and 1 mm reconstruction interval.
In daily clinical practice, our group observed that discontinuous mesenteric vessels (arterial and venous vessels irrespective), where mesenteric vessels abruptly truncate at certain points, and the proximal portion of the mesenteric vessels distends from retrograde or collateral inflows in the strangulated intestine on CT images, might be significant in differentiating CL-SBO. This imaging sign was defined as the “mesenteric vessel interruption,” which has previously only been reported in the superior mesenteric vein (19). Based on the previous literatures (3, 20–24), other CT findings were also selected for analysis in our study: (a) Increased unenhanced bowel-wall attenuation, defined as an increase in attenuation of the wall of the dilated loop compared to adjacent typical bowel loops on unenhanced images (25); (b) Bowel wall thickening, defined as a thickness greater than 3 mm; (c) Bowel loop dilatation, defined as a diameter greater than 25 mm; (d) Mesenteric fluid, defined as fluid in the mesentery of the affected intestine; (e) Mesenteric haziness, defined as increased attenuation of the mesenteric fat, which can be graded as absent, focal (only in the involved loop) or diffuse (the mesentery beyond the obstructed bowel segment is involved); (f) Mesenteric venous engorgement, defined as dilation of the mesenteric veins of the obstructed bowel compared to neighboring loops; (g) Radial distribution, defined as mesenteric vessels distributed radially; (h) Pneumatosis intestinalis, defined as intramural gas; (i) Pneumoperitoneum, defined as free peritoneal gas; (j) Peritoneal fluid, graded as absent, small (confined to the pelvic cavity or peritoneal cavity) or large (overflowed into the perihepatic and perisplenic spaces); (k) Whirl sign, defined as a swirled appearance of the mesenteric vessels and fat, reflecting the rotation of the mesentery; (l) Feces sign, defined as a mix of particulate matter with gas bubbles within the dilated bowel, classified as proximal to the obstruction site (FS1), within the closed loop (FS2) or at both sites (FS3); (m) Degree of obstruction, graded as high (completely occlusive loop) or low (incompletely occlusive loop). CT images were reviewed indenpendently by two experienced radiologists (each with over 5 years of experience in abdominal CT) who were blind to the patients’ surgically confirmed diagnosis and clinical parameters. For cases where there was initial disagreement, the two radiologists reached a consensus through discussion.
2.3 Statistical analysis
Firstly, univariate analysis using t-test, chi-square test, Wilcoxon rank sum test and Fisher’s exact test was performed to compare clinical characteristics between the transmural necrosis and transient ischemia group for patients between January 2010 and December 2019. Variables with p < 0.05 were included in the multivariate analysis using logistic regression to select an independent predictor for transmural necrosis with a two-sided p value <0.05. The odds ratios (OR) and 95% confidence intervals (CIs) were calculated. As there may not be many independent predictors, variables with p < 0.10 were used to develop a multivariate logistic regression model for outcome prediction. The predicted ability of the model was measured using Harrell’s concordance index (C-index), in which the predicted values were deduced using the multivariate logistic regression formula: predictive value = . Internal validation of the prediction model was assessed using the bootstrapping method. The validation cohort used patients’ data from January 2020 to August 2022. An acceptable C-index was equal to or higher than 0.7. The receiver operation characteristic (ROC) curve was used to visualize the discriminatory power of the prediction model.
3 Results
3.1 Association of clinical and CT features with transmural necrosis
During the univariate analysis of clinical characteristics in all patients between January 2010 and December 2019 (Supplementary Table A), patients with transmural necrosis (56/96, 58.3%) have a significantly higher proportion of advanced age, exceeding 65 years, than the transient ischemia group (36/84, 42.9%, p = 0.038). Patients with an ASA score greater than or equal to 3 are remarkably more common in the transmural necrosis group (44/96, 45.8% versus 21/84, 25%, p = 0.004). Regarding routine blood examination indices, the transmural necrosis group has significantly higher NLR (9.7 versus 7.8, p = 0.044) and lower lymphocyte percentage (8.9% versus 10.5%, p = 0.045) than participants in the transient ischemia group. The multivariate analysis data (Supplementary Table B) indicate that only the ASA score was an independent risk factor for transmural necrosis in patients with CL-SBO (p = 0.049, OR = 2.103).
In the subgroup analysis, the univariate analysis (Supplementary Table C) also suggests that a higher ASA score was more commonly seen in patients with transmural necrosis (26/57, 45.6% versus 18/65, 27.7%, p = 0.041). For the CT features, univariate analysis (Supplementary Table D) reveals that positive increased unenhanced bowel-wall attenuation (15/57, 26.3% versus 4/65, 6.2%, p = 0.003), bowel wall thickening (37/57, 64.9% versus 21/65, 32.3, P < 0.001), mesenteric fluid (47/57, 82.5% versus 39/65, 60%, p = 0.007), diffuse mesenteric haziness (38/57, 66.7% versus 30/65, 46.2%, p = 0.017) and mesenteric vessel interruption (41/57, 71.9% versus 20/65, 30.8%, P < 0.001) are significantly more common in the transmural necrosis than transient ischemia group. The logistic regression outcomes (Table 1) indicate that mesenteric vessel interruption (OR = 4.015, p = 0.002) is an independent risk factor for transmural necrosis. The CT images of typical cases are shown in Figures 1, 2.
Table 1
| Variables | Multivariate analysis | |
|---|---|---|
| Odds Ratio (95%CI) | p-value | |
| ASA score | 2.293 (0.923–5.698) | 0.074 |
| Increased unenhanced bowel-wall attenuation | 1.958 (0.477–8.031) | 0.351 |
| Bowel wall thickening | 2.197 (0.840–5.750) | 0.109 |
| Mesenteric fluid | 1.906 (0.644–5.642) | 0.244 |
| Mesenteric haziness | 0.807 (0.348–1.872) | 0.617 |
| Peritoneal fluid | 1.348 (0.569–3.197) | 0.498 |
| Feces sign | 0.862 (0.518–1.436) | 0.569 |
| Interruption of the mesenteric vessel | 4.015 (1.669–9.655) | 0.002 |
Independent risk factor analysis of intestinal resection in subgroup.
ASA, American Society of Anesthesiologists. The bold values indicate p value < 0.05.
Figure 1

Non-enhanced CT images in 59-year-old man show strangulated ileus, transmural necrosis of the small bowl wall due to internal hernia. Panel (A) is MPR (multi-planar reconstruction) image. Panels (B,C) are MIP (Maximum intensity projection) images reconstructed from different angles. The images show that the small intestine herniated into the greater omentum is dilated with fluid accumulation, and the attenuation of the intestinal wall is increased. The white arrow points to the site of intestinal strangulation. Mesenteric vessels are interrupted at the site of strangulation (arrowhead), and proximal mesenteric vessels are tortuous and dilated. Simultaneously, the mesenteric haziness (*) was shown.
Figure 2

A 36-year-old female with surgically confirmed transient intestinal ischemic obstruction caused by small bowel volvulus in the right lower quadrant. The MPR images (A,B) show a dilated small bowl loop in the right lower quadrant with a vortex-like distribution. The position indicated by the arrow shows sharp narrowing of the small intestine. (B) Shows the widen and uninterrupted of vessels in the mesenteric combining with misty mesentery sign.
3.2 Model development
According to the multivariate analysis, only ASA > 2 and mesenteric vessel interruption achieved p-values under 0.10 and so were used for model construction. The predictive value was “0.802 × ‘ASA status’ + 1.76 × ‘mesenteric vessel interruption status’.” Since both ASA and mesenteric vessel interruption are dichotomous variables, the multivariate logistic model can be regarded as a four-tier classifier ranking from “ASA ≤ 2 and interruption (−)” (lowest risk group) to “ASA > 2 and interruption (+)” (highest risk group). The C-index of this four-tier classification is 0.744 (0.659–0.829) in the training cohort (N = 122). The calibration curve shown in Supplementary Figure S2 is close to the diagonal line within 45 degrees, indicating a well-calibrated predictive model. The C-index is 0.890 (0.794–0.985) in the external validation group, even higher than in the training group (Figure 3). The sensitivity, specificity, PPV, NPV and accuracy under each cutoff point in the training and validation cohorts are shown in Tables 2, 3. For patients with ASA > 2 and interruption positivity, the specificity was 92.31 and 96.43% in training and validation cohorts, respectively, which indicating a low misdiagnosis rate. Meanwhile, the sensitivity increased to 84.21% (78.05% NPV) in the training group and to 95.45% (90.91% NPV) in the validation group when we “used interruption (−) and ASA ≤ 2″. The maximum accuracy was achieved when interruption status was used as the cutoff in both the training and validation cohorts. Different cutoff points provide different strategies under different clinical backgrounds. The establishment of this model predicts the surgical risk and greatly influences the choice of treatment strategies. Patients in the highest risk group are more likely to develop bowel necrosis. Therefore, more attention should be paid to the changes of these patients’ conditions in emergency diagnosis and treatment. Anti-infection and shock prevention therapy were actively administered, and the preferred surgical approach was open surgery rather than laparoscope. For patients in the lowest risk group, conservative treatment can be tried.
Figure 3
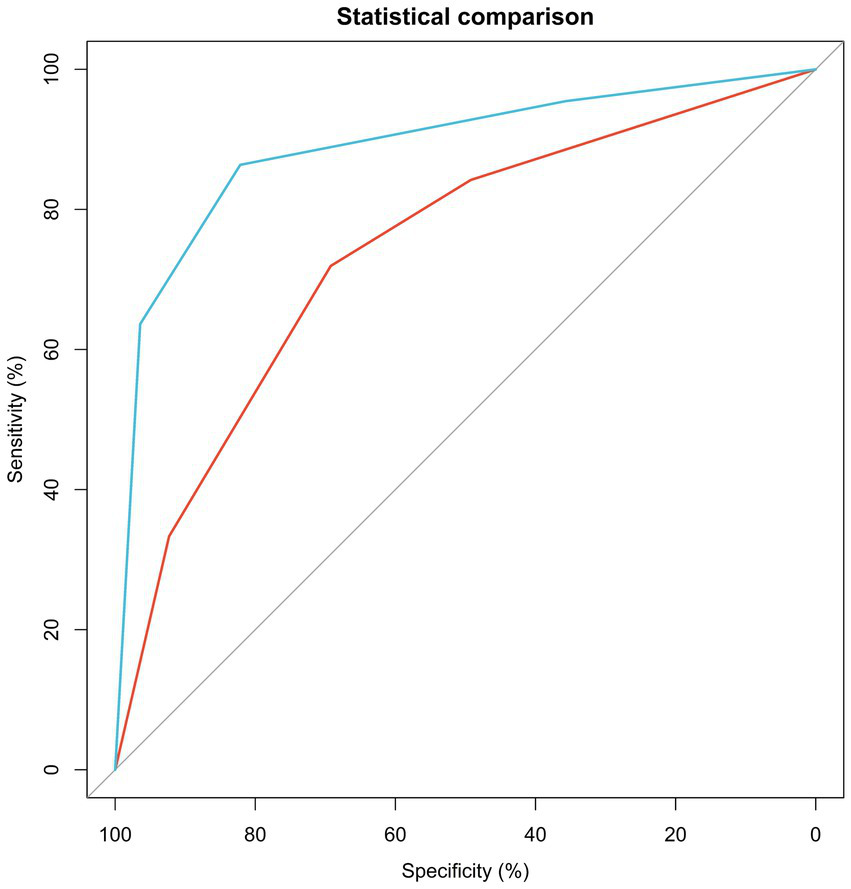
ROC curve for four tiers performances in training and validation groups.
Table 2
| Sensitivity | Specificity | Positive predictive value (PPV) | Negative predictive value (NPV) | Accuracy | |
|---|---|---|---|---|---|
| Interruption (+) and ASA > 2 | 33.33% | 92.31% | 79.17% | 61.22% | 64.75% |
| Interruption (+) | 71.93% | 69.23% | 67.21% | 73.77 | 70.49% |
| Interruption (−) and ASA ≤ 2 | 84.21% | 49.23% | 59.26% | 78.05% | 65.57% |
Sensitivity, specificity, PPV and NPV at given cutoff point in training set.
Table 3
| Sensitivity | Specificity | Positive predictive value (PPV) | Negative predictive value (NPV) | Accuracy | |
|---|---|---|---|---|---|
| Interruption (+) and ASA > 2 | 63.64% | 96.43% | 93.33% | 77.14% | 82.00% |
| Interruption (+) | 86.36% | 82.14% | 79.17% | 88.46% | 84.00% |
| Interruption (−) and ASA ≤ 2 | 95.45% | 35.71% | 53.85% | 90.91% | 62.00% |
Sensitivity, specificity, PPV and NPV at given cutoff point in validation set.
4 Discussion
CL-SBO is a common acute abdomen disease that usually requires surgical intervention. Considering this fact, an accurate operational strategy is essential in treating patients with CL-SBO, such as using laparoscopy and evaluating patients’ critical degree (16, 26). The abdominal CT is a convenient and fast preoperative examination widely applied in diagnosing variable acute abdomens, including SBO (2, 3). Differentiation SSBO from simple intestinal obstruction using clinical and imaging signs is necessary for surgeons and radiologists, which may become an indication for supporting conservative treatment application (13). Many studies also explore significant clinical and radiological signs for differentiating patients with SSBO, such as reduced bowel wall enhancement, a closed-loop mechanism, diffuse mesenteric haziness and so on (3, 14, 21, 22, 24, 27). In contrast, as the most common type of SSBO, CL-SBO has few physicians and studies focusing on its degree of ischemia, transient ischemia and transmural necrosis, which may also play a decisive role in establishing the surgical strategy (2, 28).
The current study screened some significant clinical characteristics from CL-SBO patients with transient ischemia or transmural necrosis, such as advanced age, ASA score and NLR. Some clinical symptoms and signs, such as peritoneal irritation, did not reveal a significant difference between the ischemic and necrotic groups. Patients with transmural necrosis have higher NLR, which can reflect the severity of systemic inflammation (29). Like this study, Yoon et al. also indicated that NLR increased significantly in SBO patients with poor prognoses (30). Tim et al. suggested that some common symptoms or signs in the acute abdomen had limited diagnostic value in SBO patients with different intestinal blood supply statuses (31). Whether in total patients or subgroup analysis, the higher ASA classification was the risk factor for transmural necrosis in CL-SBO patients. In line with this finding, higher ASA classification and old age were considered independent predictors of adverse outcomes for patients with acute intestinal ischemia (32). Masja et al. reached similar conclusions that patients with ASA classification ≥3 had a higher risk of irreversible perioperative ischemia (33).
Concerning imaging data, the increased unenhanced bowel-wall attenuation reveals potential diagnostic value among CL-SBO patients with transmural necrosis. This sign correlated with necrosis in CL-SBO with high specificity [100% (95% CI, 79–100)], and is thought to result from the extravasation of blood components due to capillary wall damage (20). Venous engorgement can lead to bowel wall thickening. However, various studies have different threshold values to define this characteristic, such as 3 mm (21) and 5 mm (34). Although the thickness of the involved bowel wall >3 mm was confirmed to be the risk factor for necrosis in our study, the systematic review of Millet et al. suggested that bowel wall thickening had decreased diagnostic value compared with increased unenhanced bowel-wall attenuation because of its lower sensitivity and specificity (22). The widespread engorgement of veins can contribute to the transudation of fluid across the serosa into the mesentery and peritoneal cavity (21). Carefully imaging and evaluating the mesentery and peritoneal cavity status may play a vital role in determining the ischemic severity of the affected intestinal segment. Patients with transmural necrosis are more likely to have signs of mesenteric fluid, diffuse mesenteric haziness and large peritoneal fluid in this study. The feces sign is typically found at the intestinal transition zone in patients with SBO. The results of the univariate analysis indicated that feces sign is significantly associated with necrosis. While univariate analysis indicated that the feces sign is significantly associated with necrosis, multivariate analysis did not support the feces sign as an independent predictor of transmural necrosis, consistent with the findings of Khaled et al. (27).
The blood circulation disorder caused by mechanical compression is regarded as the reason for ischemia in patients with CL-SBO. Most studies (2, 20, 21) have focused on the sign of engorgement in mesenteric vessels. In the current study, mesenteric venous engorgement did not demonstrate any value in differentiating transient ischemia from necrosis. However, careful clinical observation during this study, along with accumulated diagnostic experience, highlighted that the mesenteric vessel interruption occurred frequently in CL-SBO patients with necrotic intestinal segments — an observation previously unreported. This was further verified by the multivariate analysis data. This imaging biomarker, along with the ASA classification, demonstrated diagnostic efficacy in both group and subgroup analyses and was incorporated into a diagnostic model with excellent predictive ability for transmural necrosis in the external validation group (C-index = 0.89). Applying this model in the validation set showed that 93.33% of patients with both an ASA score >2 and mesenteric vessel interruption were diagnosed with transmural necrosis. In contrast, 90.91% of patients with neither a higher ASA score nor this innovative imaging sign were correctly excluded from the necrosis group. These high proportions underscore the signification role of mesenteric vessel interruption in resolving the challenging clinical problem of evaluating ischemia levels in CL-SBO.
The combination of unenhanced CT imaging and clinical features in our prediction model improved diagnostic accuracy compared with using unenhanced CT imaging features alone to predict bowel necrosis (17). Moreover, because the model relies on unenhanced CT imaging, it is suitable for patients who cannot use contrast agents. Compared with enhanced CT, this approach ensures diagnostic accuracy while being more convenient and having a broader clinical application range. For patients with bowel necrosis, inappropriate surgical strategies can lead to disease progression. Although laparoscopic surgery is becoming more common, intestinal resection remains a major reason for converting to open surgery (35). Irreversible intestine necrosis is likely to result in difficult-to-control septic shock, and laparoscopic surgery will significantly increase the risk associated with anesthesia. The incidence of postoperative complications and 30-day mortality is higher in patients requiring small intestinal resection than in those who underwent adhesiolysis alone. However, our prediction model guides the selection of surgical methods and help provide the best surgical strategy for patients.
Although the current study has a relatively large sample size and external test set, several limitations must be acknowledged. Firstly, as with all retrospective studies, selection bias is a concern. Secondly, while the value of the imaging marker of mesenteric vessel interruption has been verified in differentiating CL-SBO patients with necrosis from those with transient ischemia, this predictive marker has not yet been applied to distinguish between patients with simple SBO and SSBO. Its efficacy for this common clinical problem still needs to be investigated. Thirdly, the number of patients included in the validation set is limited and drawn from a single center. To establish the broader applicability of the diagnostic model and the new imaging marker, it is necessary to examine more CL-SBO patients across multiple centers. Fourthly, unenhanced CT, which does not require the injection of contrast agents, is relatively convenient. In emergency settings where medical resources are often scarce, unenhanced CT is generally preferred for patients with acute abdomen requiring CT examination, from a health economics perspective. Additionally, some patients may be allergic to contrast media or have conditions such as renal insufficiency or septic shock that make them unsuitable for enhanced CT. Therefore, while unenhanced CT is more convenient and efficient in emergencies, it is likely that diagnostic accuracy could be further improved if the model can be constructed using enhanced CT radiographic data. Fifthly, although CT data extraction was performed by two experienced radiologists, we did not quantitatively assess interobserver agreement. Finally, characteristics incorporated in building the logistic regression model are relatively simple, and more potential indicators must be explored.
5 Conclusion
After a rigorous statistical analysis, the ASA classification and CT appearance of mesenteric vessel interruption were found to be correlated and valuable in differentiating transmural necrosis from transient ischemia among CL-SBO patients. Utilizing this universal clinical index and innovative imaging marker, a diagnostic model was developed, yielding promising clinical results for predicting this perplexing clinical issue. The data shows potential for optimizing the diagnosis and treatment process for patients with SSBO. Implementing more efficient surgical strategies can improve the prognosis for CL-SBO patients with transmural necrosis.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by The Institutional Ethics Committee of Peking University First Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SP: Data curation, Formal analysis, Methodology, Software, Visualization, Writing – original draft. JY: Data curation, Formal analysis, Methodology, Software, Visualization, Writing – original draft. ZL: Data curation, Formal analysis, Methodology, Software, Visualization, Writing – original draft. RN: Data curation, Writing – original draft. ZC: Conceptualization, Funding acquisition, Project administration, Resources, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. National High Level Hospital Clinical Research Funding (Scientific Research Seed Fund of Peking University First Hospital 2022SF06) and Peking University First Hospital Medical Education Research Funding Project (2022YJ09) were received for the research, authorship, and publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1466754/full#supplementary-material
References
1.
Long D Mao C Liu Y Zhou T Xu Y Zhu Y . Global, regional, and national burden of intestinal obstruction from 1990 to 2019: an analysis from the global burden of disease study 2019. Int J Color Dis. (2023) 38:245. doi: 10.1007/s00384-023-04522-6
2.
de Kok BM Toneman MK Oei S Westerterp M van Acker GJD van der Pool AEM et al . Correlation of CT findings with intra-operative outcome in closed-loop small bowel obstruction (CL-SBO). Eur J Radiol. (2021) 142:109844. doi: 10.1016/j.ejrad.2021.109844
3.
Calame P Malakhia A Turco C Grillet F Piton G Delabrousse E . Transmural bowel necrosis from acute mesenteric ischemia and strangulated small-bowel obstruction: distinctive CT features. AJR Am J Roentgenol. (2020) 214:90–5. doi: 10.2214/AJR.19.21693
4.
Zins M Millet I Taourel P . Adhesive small bowel obstruction: predictive radiology to improve patient management. Radiology. (2020) 296:480–92. doi: 10.1148/radiol.2020192234
5.
Li B-Q Qi W-J Yuan M Wang H-Y Chen M Lei J-A et al . Prediction of bowel necrosis by reduced bowel wall enhancement in closed-loop small bowel obstruction: quantitative methods. Eur J Radiol. (2024) 173:111363. doi: 10.1016/j.ejrad.2024.111363
6.
Li B-Q Qi W-J Yuan M Wang H-Y Chen M Song Z-X et al . Increased attenuation of intestinal contents at CT indicates bowel necrosis in closed-loop small bowel obstruction. Radiology. (2024) 310:e231710. doi: 10.1148/radiol.231710
7.
Rondenet C Millet I Corno L Khaled W Boulay-Coletta I Taourel P et al . CT diagnosis of closed loop bowel obstruction mechanism is not sufficient to indicate emergent surgery. Eur Radiol. (2020) 30:1105–12. doi: 10.1007/s00330-019-06413-3
8.
Kim HR Lee Y Kim J Baek TW Kim H Son JH et al . Closed loop obstruction of small bowel: CT signs predicting successful non-surgical treatment. Eur J Radiol. (2023) 161:110716. doi: 10.1016/j.ejrad.2023.110716
9.
Nielsen LBJ Ærenlund MP Alouda M Azzam M Bjerke T Burcharth J et al . Real-world accuracy of computed tomography in patients admitted with small bowel obstruction: a multicentre prospective cohort study. Langenbeck's Arch Surg. (2023) 408:341. doi: 10.1007/s00423-023-03084-z
10.
Chao J Cui S Liu C Liu S Liu S Han Y et al . Detection of early cytokine storm in patients with septic shock after abdominal surgery. J Transl Int Med. (2020) 8:91–8. doi: 10.2478/jtim-2020-0014
11.
Di Saverio S Birindelli A Broek RT Davies JR Mandrioli M Sallinen V . Laparoscopic adhesiolysis: not for all patients, not for all surgeons, not in all centres. Updat Surg. (2018) 70:557–61. doi: 10.1007/s13304-018-0534-4
12.
Hashimoto D Hirota M Matsukawa T Yagi Y Baba H . Clinical features of strangulated small bowel obstruction. Surg Today. (2012) 42:1061–5. doi: 10.1007/s00595-012-0207-8
13.
Ten Broek RPG Krielen P Di Saverio S Coccolini F Biffl WL Ansaloni L et al . Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO): 2017 update of the evidence-based guidelines from the world society of emergency surgery ASBO working group. World J Emerg Surg. (2018) 13:24. doi: 10.1186/s13017-018-0185-2
14.
Makar RA Bashir MR Haystead CM Iseman C Mayes N Hebert S et al . Diagnostic performance of MDCT in identifying closed loop small bowel obstruction. Abdom Radiol. (2016) 41:1253–60. doi: 10.1007/s00261-016-0656-4
15.
Goyal R Mui LW Riyahi S Prince MR Lee HK . Machine learning based prediction model for closed-loop small bowel obstruction using computed tomography and clinical findings. J Comput Assist Tomogr. (2022) 46:169–74. doi: 10.1097/RCT.0000000000001269
16.
Chai Y Xing J Lv P Liang P Xu H Yue S et al . Evaluation of ischemia and necrosis in adhesive small bowel obstruction based on CT signs: subjective visual evaluation and objective measurement. Eur J Radiol. (2022) 147:110115. doi: 10.1016/j.ejrad.2021.110115
17.
Liu X Zhu M Wu M Cheng Z Wu X Zhu R . Unenhanced CT-based predictive model to identify small bowel necrosis in patients with mechanical small bowel obstruction. BMC Med Imaging. (2023) 23:80. doi: 10.1186/s12880-023-01041-2
18.
Li Y Tian Z Liu C Li S Bi W Ji Q . Diagnostic nomogram for closed-loop small bowel obstruction requiring emergency surgery. Am J Emerg Med. (2023) 63:5–11. doi: 10.1016/j.ajem.2022.10.022
19.
Ho YC . “Venous cut-off sign” as an adjunct to the “whirl sign” in recognizing acute small bowel volvulus via CT scan. J Gastrointest Surg. (2012) 16:2005–6. doi: 10.1007/s11605-012-1910-x
20.
Rondenet C Millet I Corno L Boulay-Coletta I Taourel P Zins M . Increased unenhanced bowel-wall attenuation: a specific sign of bowel necrosis in closed-loop small-bowel obstruction. Eur Radiol. (2018) 28:4225–33. doi: 10.1007/s00330-018-5402-6
21.
Millet I Boutot D Faget C Pages-Bouic E Molinari N Zins M et al . Assessment of strangulation in adhesive small bowel obstruction on the basis of combined CT findings: implications for clinical care. Radiology. (2017) 285:798–808. doi: 10.1148/radiol.2017162352
22.
Millet I Taourel P Ruyer A Molinari N . Value of CT findings to predict surgical ischemia in small bowel obstruction: a systematic review and meta-analysis. Eur Radiol. (2015) 25:1823–35. doi: 10.1007/s00330-014-3440-2
23.
Scaglione M Galluzzo M Santucci D Trinci M Messina L Laccetti E et al . Small bowel obstruction and intestinal ischemia: emphasizing the role of MDCT in the management decision process. Abdom Radiol. (2022) 47:1541–55. doi: 10.1007/s00261-020-02800-3
24.
Chuong AM Corno L Beaussier H Boulay-Coletta I Millet I Hodel J et al . Assessment of Bowel Wall enhancement for the diagnosis of intestinal ischemia in patients with small bowel obstruction: value of adding unenhanced CT to contrast-enhanced CT. Radiology. (2016) 280:98–107. doi: 10.1148/radiol.2016151029
25.
Geffroy Y Boulay-Coletta I Jullès M-C Nakache S Taourel P Zins M . Increased unenhanced bowel-wall attenuation at multidetector CT is highly specific of ischemia complicating small-bowel obstruction. Radiology. (2014) 270:159–67. doi: 10.1148/radiol.13122654
26.
O’Connor DB Winter DC . The role of laparoscopy in the management of acute small-bowel obstruction: a review of over 2,000 cases. Surg Endosc. (2012) 26:12–7. doi: 10.1007/s00464-011-1885-9
27.
Khaled W Millet I Corno L Bouley-Coletta I Benadjaoud MA Taourel P et al . Clinical relevance of the feces sign in small-bowel obstruction due to adhesions depends on its location. AJR Am J Roentgenol. (2018) 210:78–84. doi: 10.2214/AJR.17.18126
28.
Kohga A Kawabe A Yajima K Okumura T Yamashita K Isogaki J et al . CT value of the intestine is useful predictor for differentiate irreversible ischaemic changes in strangulated ileus. Abdom Radiol. (2017) 42:2816–21. doi: 10.1007/s00261-017-1227-z
29.
Chen Z Liu Z Zhang Y Wang P Gao H . Combination of CA19-9 and the neutrophil-to-lymphocyte ratio for the differential diagnosis of gallbladder carcinoma. Cancer Manag Res. (2020) 12:4475–82. doi: 10.2147/CMAR.S255480
30.
Yoon JB Lee SH . The neutrophil-to-lymphocyte ratio has feasible predictive value for hospital mortality in patients with small bowel obstruction in the emergency department. Am J Emerg Med. (2021) 44:428–33. doi: 10.1016/j.ajem.2020.05.049
31.
Jancelewicz T Vu LT Shawo AE Yeh B Gasper WJ Harris HW . Predicting strangulated small bowel obstruction: an old problem revisited. J Gastrointest Surg. (2009) 13:93–9. doi: 10.1007/s11605-008-0610-z
32.
Kassahun WT Schulz T Richter O Hauss J . Unchanged high mortality rates from acute occlusive intestinal ischemia: six year review. Langenbeck's Arch Surg. (2008) 393:163–71. doi: 10.1007/s00423-007-0263-5
33.
Toneman MK de Kok BM Zijta FM Oei S van Acker GJD Westerterp M et al . Predicting the outcome of closed-loop small bowel obstruction by preoperative characteristics. World J Gastrointest Surg. (2022) 14:556–66. doi: 10.4240/wjgs.v14.i6.556
34.
Huszty G Mogami K Sawada T Seki H Sakusabe M Ohuchi S et al . Preoperative evaluation of irreversible bowel ischemia in obturator hernia. Hepato-Gastroenterology. (2007) 54:775–9. PMID:
35.
Chin RL Lima DL Pereira X Romero-Velez G Friedmann P Dawodu G et al . Assessing outcomes in laparoscopic vs open surgical management of adhesive small bowel obstruction. Surg Endosc. (2023) 37:1376–83. doi: 10.1007/s00464-022-09314-7
Summary
Keywords
closed-loop small bowel obstruction, bowel ischemia, bowel necrosis, computed tomography, diagnostic model
Citation
Pan S, Yang J, Liu Z, Nai R and Chen Z (2024) A prediction model to differentiate transient ischemia from irreversible transmural necrosis in closed-loop small bowel obstruction. Front. Med. 11:1466754. doi: 10.3389/fmed.2024.1466754
Received
18 July 2024
Accepted
26 August 2024
Published
11 September 2024
Volume
11 - 2024
Edited by
Pradeep Kumar Shukla, University of Tennessee Health Science Center (UTHSC), United States
Reviewed by
Yuan Lin, Xiamen University, China
Pablo Rodríguez Carnero, La Princesa University Hospital, Spain
Updates
Copyright
© 2024 Pan, Yang, Liu, Nai and Chen.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zeyang Chen, chenzeyang_pku@bjmu.edu.cn
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.