- Department of Public Health, Adama Hospital Medical College, Adama, Ethiopia
Introduction: Non-adherence to dietary guidelines is a significant challenge in managing diabetes mellitus and its complications. Its consequences were significantly associated with a deterioration in patients’ quality of life and an increased socioeconomic burden on healthcare delivery systems. This study aimed to assess the magnitude of adherence to recommended diet and associated factors among patients with diabetes mellitus type 2 on follow-up care at Adama Hospital Medical College Oromia, Ethiopia.
Methods: A hospital-based cross-sectional study design was conducted. Participants were selected through systematic random sampling. Data were collected using structured, interviewer-administered questionnaires. The perceived dietary adherence questionnaire was used to assess the level of dietary adherence. A simple binary logistic regression was used to identify candidate variables, while a multivariable logistic regression assessed factors associated with adherence to the recommended diet. A p-value <0.05 were considered as statistically significant. All analyses were performed using SPSS and R programming software.
Result: A total of 405 participants were included in the study, with a response rate of 96.2%. The magnitude of non-adherence to the recommended diet was 64.2% (95% confidence interval [CI]: 59.8, 68.6). In the multivariable logistic regression model, patients with low and middle income (AOR = 8.0; 95% CI: 3.4, 19.2) and (AOR = 2.75; 95% CI: 1.49, 5.55) respectively, high glycemic level (AOR = 2.15; 95% CI: 1.17, 3.94), food insecure (AOR = 12.7; 95% CI: 5.79, 28.2), poor diabetic knowledge (AOR = 2.88; 95% CI: 1.49, 5.55) and low perceived susceptibility (AOR = 2.97; 95% CI: 1.62, 5.45) were significantly associated factors for non-adherence to recommended diet among patients with diabetes mellitus type 2.
Conclusion: This study revealed that approximately two-thirds of patients with type 2 diabetes mellitus experienced non-adherence to the recommended diet. Key factors linked to dietary non-adherence among T2DM patients include low to middle income, elevated glycemic levels, household food insecurity, limited diabetes knowledge, and low perceived susceptibility. An integrated approach that combines socioeconomic support, nutritional guidance, and risk awareness may greatly enhance dietary adherence and optimize diabetes management.
Introduction
Diabetes mellitus is a metabolic disorder with various causes that impair the body’s ability to process glucose for energy, leading to elevated blood sugar levels due to defects in insulin secretion, action, or both (1). It can significantly increase the risk of premature death (2). According to the World Health Organization, adherence is how a person’s behavior such as taking medication, following a diet, and making lifestyle changes aligns with their healthcare provider’s recommendations (3). Type 2 diabetes mellitus (T2DM) is a chronic metabolic disorder influenced by genetics, lifestyle, and diet (4) and represents 90% of all diabetes cases, posing a significant and growing global health burden (5). Managing Type 2 diabetes requires regular self-care and significant lifestyle changes, primarily dietary modifications (5). Diabetes patients who fail to adhere to the recommended dietary regimen are at risk of developing life-threatening complications (6).
Dietary non-adherence can progressively worsen diabetic conditions (7). Research indicates that the rates of dietary non-adherence among people with type 2 diabetes vary widely across countries, ranging from 29.9 to 97.5% (8, 9). Similarly, several studies suggested that dietary non-adherence rates among individuals with type 2 diabetes vary significantly, with 63% in Botswana, 97.5% in Egypt (3, 9), and 46.8 to 79% in Ethiopia (10, 11). The recommended diet includes fruits, vegetables, nuts, whole grains, and unsaturated fats, while snacks high in fat, sugar, or salt should be avoided (12).
A growing number of fast food restaurants, urbanization, globalization, and rapid socioeconomic development, which can lead to atypical consumption patterns and overdependence, may contribute to Type 2 diabetes mellitus patients’ difficulties in adhering to their dietary regimens (8). Non-adherence to diet can gradually worsen the disease, impacting the patient’s quality of life, the healthcare provider, and the healthcare delivery system. It can lead to increased mortality, longer hospital stays, and higher costs and burden of the disease (13).
Although a few studies in Ethiopia (14, 15) have used the 8-item Morisky Medication Adherence Scale (MMAS-8) to assess dietary adherence in patients with type 2 diabetes, this tool was originally designed to measure medication adherence rather than dietary habits. As a result, the MMAS-8 may not capture the full range of dietary practices essential for effective diabetes management. In contrast, our study utilizes the Perceived Dietary Adherence Questionnaire (PDAQ), a validated tool specifically developed to assess dietary adherence in alignment with the Canadian Diabetes Association (CDA) nutrition therapy guidelines (16, 17). The PDAQ’s validation against repeated 24-h dietary recalls provides a more accurate and focused measure of dietary adherence among patients with diabetes.
Additionally, our study includes a relatively larger sample size, enhancing the accuracy and precision of our findings. This robust methodological approach, combined with the larger sample, provides a more comprehensive understanding of dietary adherence patterns among Ethiopian patients with type 2 diabetes, offering valuable insights to guide more effective, population-specific dietary interventions.
Methods
Study setting and design
A hospital-based cross-sectional study was conducted at Adama Hospital Medical College from January 1 to February 14, 2023. This hospital, located in Adama town in the Oromia Region, is one of the first medical hospitals in the area, situated 100 km southeast of Addis Ababa. The hospital was inaugurated by missionaries from abroad in 1938 E.C. and was among the first non-governmental hospitals in the nation. It serves a catchment population of over 6 million people from five regions (Oromia, Amhara, Afar, Somali, and Dire-Dawa). The hospital was selected purposively for this study due to the availability of regular DM case follow-up and the large number of type 2 DM cases at the Diabetic Clinic.
Inclusion and exclusion criteria for participants
This study included patients with Type 2 diabetes who had received treatment follow-up for at least 6 months during the data collection period. Patients with newly diagnosed Type 2 diabetes, those needing ongoing medical support and monitoring, and individuals under 18 years of age were excluded from the study.
Sample size determination
A single population proportion formula was used to determine the sample size (18), assuming a 95% confidence interval (CI) with a 5% margin of error and a non-adherence proportion of 46.8%, based on a study conducted at Felege-Hiwot Referral Hospital in northwest Ethiopia (10). A total of 421 participants were included in the study, accounting for a 10% non-response rate.
Sampling procedures
A systematic random sampling method was used to select patients with type 2 diabetes mellitus (DM). The sampling interval was determined by dividing the total DM patient population by the calculated sample size. The first participant was chosen through simple random sampling, and subsequent participants were selected at regular intervals. Data were collected from each study participant during their clinic visits using a structured questionnaire administered through face-to-face interviews.
Study variables and measurements
The dependent variable in this study was adherence to the recommended diet (categorized as adherent or non-adherent). The independent variables included various socio-economic and demographic factors, such as participant age, sex, educational status, residence, marital status, occupation, family income, and family size. Additionally, the study considered anthropometric and clinical characteristics, including BMI, glycemia levels, comorbidities, family history of diabetes mellitus (DM), duration of illness, treatment type, food-related factors, diabetes education, awareness of diabetic diets, and household food security status. Psychosocial and behavioral factors such as smoking and drinking habits, khat use, and family/social support were also included. Finally, the diabetic health belief model was assessed through perceived susceptibility, perceived severity, perceived benefits, perceived barriers, depression, and diabetic knowledge.
The study employed the Perceived Dietary Adherence Questionnaire (PDAQ) to assess dietary non-adherence. Developed by Asaad et al. (16), this nine-item tool measures patients’ perceptions of their adherence to dietary guidelines. Responses on the PDAQ are recorded on a seven-point Likert scale, reflecting food consumption over the past 7 days. Generally, higher scores indicate better adherence, except for items 4 and 9, which assess the consumption of high-sugar or high-fat foods; in these cases, higher scores signify lower adherence. A patient is considered to have good dietary adherence if they maintain a healthy diet at least 4 days a week.
The Perceived Dietary Adherence Questionnaire (PDAQ) (16) and the Morisky Medication Adherence Scale (MMAS) (19) both assess adherence but in different domains: PDAQ for dietary adherence and MMAS for medication adherence. The PDAQ has demonstrated strong validity and reliability, similar to the MMAS, with high internal consistency (Cronbach’s alpha >0.80) and stable test–retest reliability. Both tools are concise, reducing respondent burden and enhancing adequacy for clinical and research use. They are sensitive to adherence changes over time, making them valuable in intervention studies; however, the PDAQ is specifically tailored to assess dietary behavior changes.
Household food insecurity was assessed using the Household Food Insecurity Access Scale (HFIAS), adapted from the food and nutrition technical assistance guidelines. Responses were aggregated to create an index representing the level of household food insecurity (16, 20). Participants’ height was measured with a stadiometer, recorded to the nearest 0.1 cm, while their weight was measured using a digital scale, recorded to the nearest 0.1 kg. The scale was reset to zero before and after each measurement. Body mass index (BMI) was calculated as weight in kilograms divided by the square of height in meters (kg/m2).
The Patient Health Questionnaire-9 (PHQ-9) was utilized to assess depression in patients with Type 2 diabetes mellitus. This nine-item questionnaire was adapted from Pfizer Inc. (21). Diabetes knowledge was measured using a 20-item yes/no questionnaire, where each correct answer scored “1” and incorrect or unknown responses scored “0,” resulting in a total score ranging from 0 to 20. Participants with scores equal to or above the mean were classified as having good knowledge, while those scoring below the mean were considered to have poor knowledge (22). Diabetic health beliefs were evaluated using 14 adapted questions on a 5-point scale, based on a similar study conducted in Igala, Nigeria (23). These questions assessed participants’ perceptions of susceptibility and severity regarding diabetes complications, as well as the perceived benefits and barriers to dietary recommendations. The scores for each health belief construct were summed to categorize respondents as having high or low levels based on whether their scores were above or below the mean cutoff.
Data quality assurance
Data collectors and supervisors received 1 day of training on the study tools, objectives, and interview techniques. Anthropometric measurements followed standard procedures with calibrated instruments, and regular supervision and follow-up were conducted. A pretest with 5% of type 2 diabetic patients from outside the study area ensured response consistency. The questionnaire was reviewed for content, consistency, and organization, and modified as needed. Data quality was monitored daily for completeness, consistency, and accuracy by the principal investigators.
Data processing and analysis
Descriptive statistics, including frequencies and percentages for categorical variables and means with standard deviations for continuous variables, were used to summarize the data. Bivariate logistic regression analysis was conducted to examine associations between independent variables and adherence to recommended dietary practices, with variables showing a p-value less than 0.25 considered for multiple logistic regression to identify significant predictors of dietary adherence. Model fit for the final analysis was assessed using the Hosmer–Lemeshow test (p-value = 0.504), indicating an adequate fit. The Variance Inflation Factor (VIF) was calculated to evaluate multicollinearity, ensuring no interference with model interpretation, while the Shapiro–Wilk test assessed normality for continuous variables, confirming that assumptions for statistical analyses were met. A p-value of less than 0.05 was set to determine statistical significance. All analyses were conducted using SPSS version 26.0 and R version 3.4.3 (R Foundation for Statistical Computing, Vienna, Austria).
Ethical clearance
Ethical clearance was obtained from the Adama Hospital Medical College of institutional review Board committee. Informed written consent was obtained from participants. Those unwilling to participate or who chose to withdraw during the study were allowed to discontinue their involvement at any time.
Results
Socio-demographic characteristics of the participants
Out of 421 eligible respondents, 405 (with a response rate of 96.2%) participated in the study. The mean age of participants was 56.2 years (SD ±10.11). Among the participants, 216 (53.3%) were female. Regarding religion, 242 (59.8%) participants were Orthodox, followed by Muslims 93 (23.3%). The majority of participants, 299 (73.8%), were married and 372 (91.9%) urban residents. One hundred thirty-three 133 (32.8%) participants had attended primary school, while 108 (26.7%) were illiterate. Of the total participants, 135 (33.3%) were housewives, 177 (43.7%) participants had medium monthly income, and 277 (68.4%) participants had family sizes of fewer than five members (Table 1).
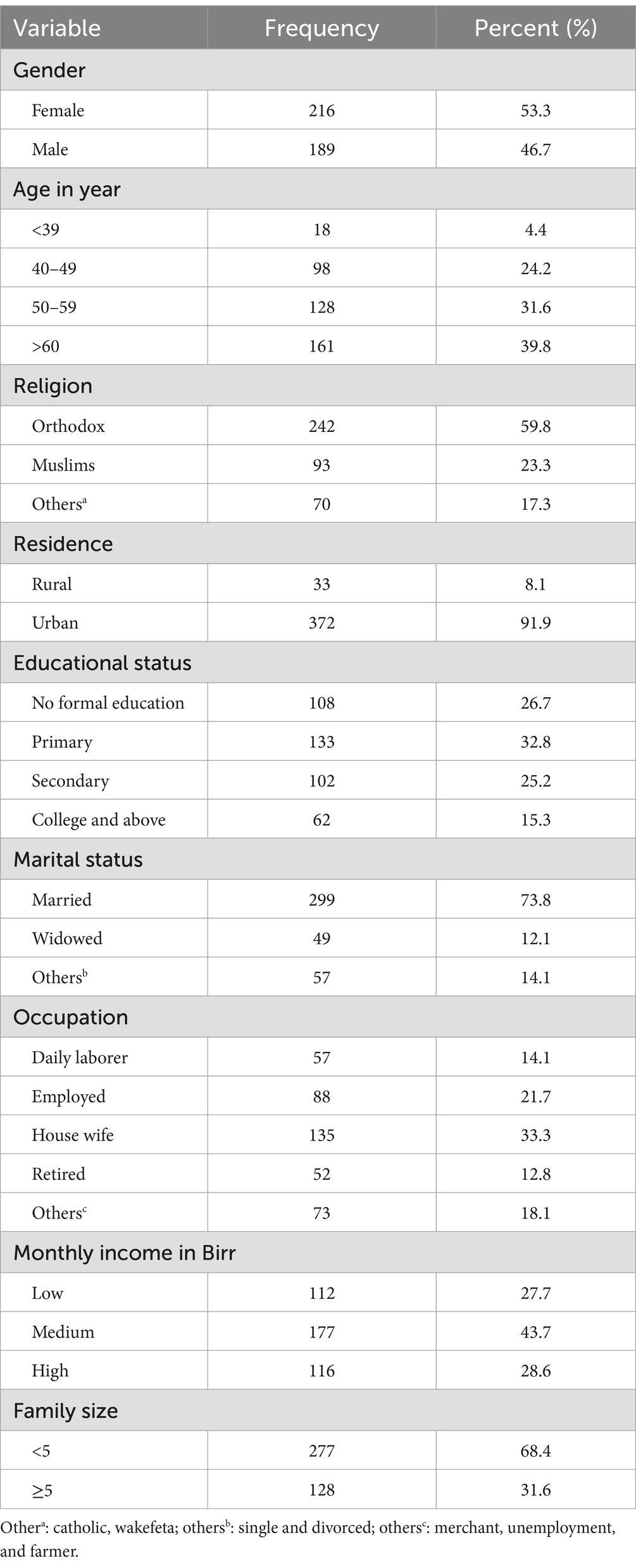
Table 1. Socio-demographic and economic characteristics of patients with DM 2 type attending follow-up care at Adama Hospital Medical College, Oromia, Ethiopia, 2023 (n = 405).
Anthropometric and clinical characteristics of study participants
The mean duration follow-up was 5.5 years (SD ±4.5), with 145 (35.8%) participants reported a family history of diabetes. Additionally, 188 (46.4%) participants had co-morbid conditions. A majority, 268 (66.2%), patients managed their blood glucose levels with oral hypoglycemic agents. Only 78 (19.3%) participants were members of the Ethiopian Diabetic Association. The mean of BMI was 24.2 (SD ±3.73), with 153 (37.8%) participants were classified as overweight and 23 (5.7%) as obese. Furthermore, 275 (67.9%) participants had fasting blood glucose levels greater than 126 mg/dL. Among the respondents, 305 (75.3%) experienced minimal depression, 68 (16.8%) had mild depression, and 32 (7.9%) had moderate depression in the past week (Table 2).
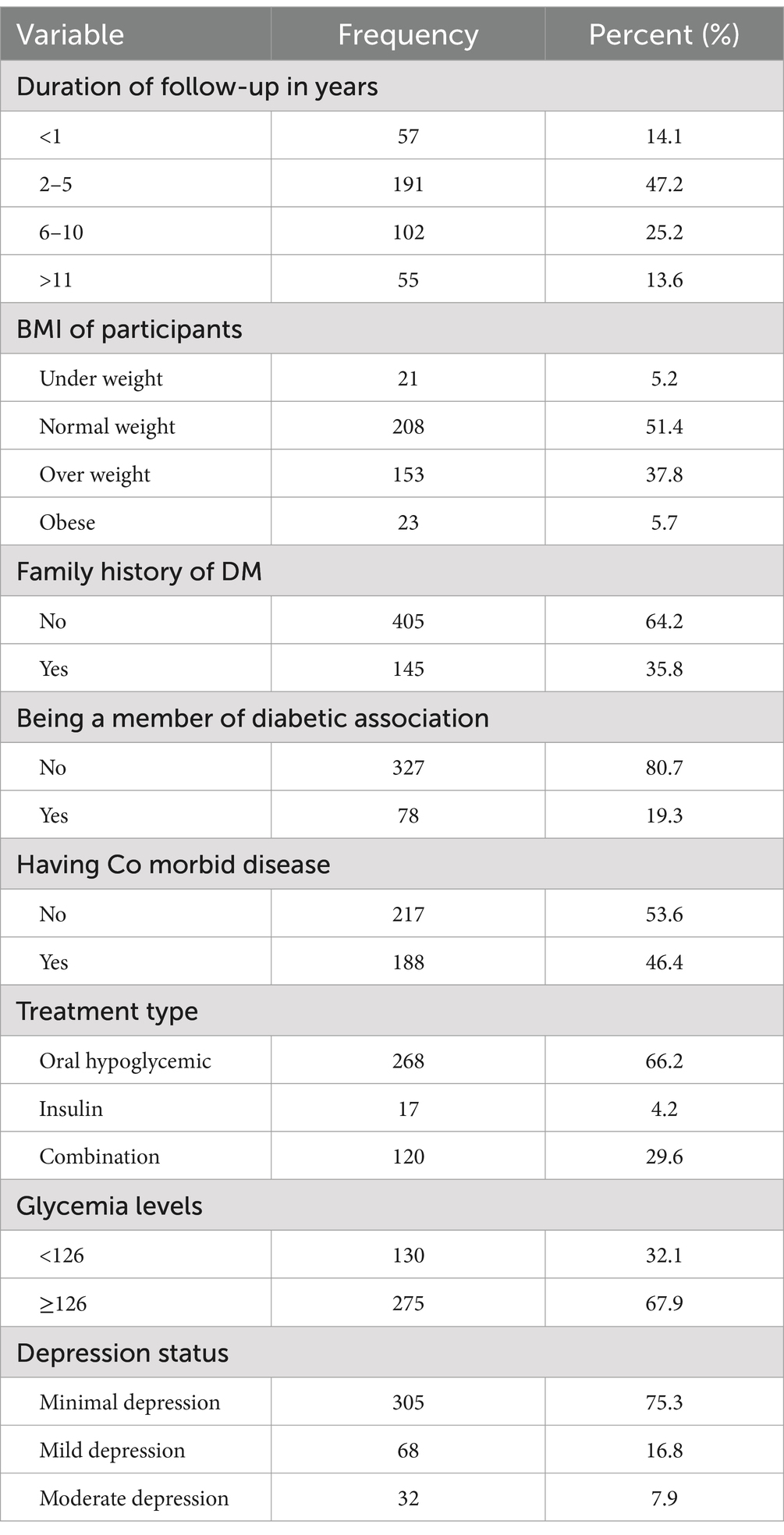
Table 2. Clinical characteristics of patients with DM 2 type at Adama Hospital Medical College, Oromia, Ethiopia, 2023 (n = 405).
Food related factors and household food security status
Among the participants, 160 (39.5%) received nutrition education, while 338 (83.5%) reported difficulties accessing fruits and vegetables. Additionally, 331 (81.7%) were concerned about the high cost of food, and 159 (39.3%) had a poor understanding of the relationship between food and disease. A total of 272 (67.2%) and 200 (49.4%) are managed their diabetes through food planning and struggled with selecting appropriate foods, respectively. While, 336 (83%) of type 2 DM patients were living in households with food insecurity (Table 3).
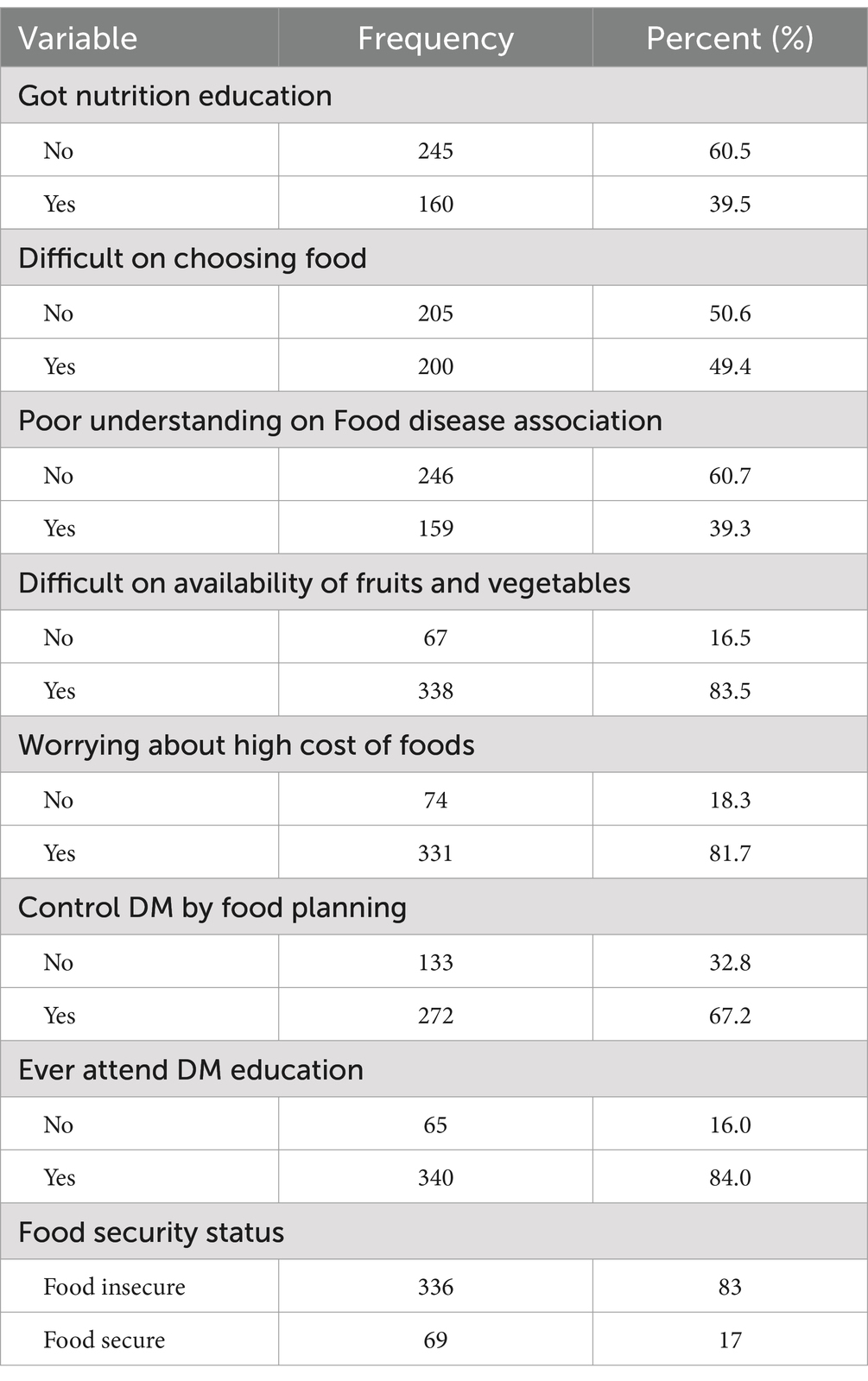
Table 3. Food related factors and household food security status of patients with DM 2 type attending follow-up care at Adama Hospital Medical College, Oromia, Ethiopia, 2023 (n = 405).
Psychosocial and behavioral conditions
Of the total participants, 63 (15.6%) engaged in regular physical exercise, 54 (13.3%) use alcohol, 10 (2.5%) were smokers, and 74 (18.3%) participants experienced poor family support (Figure 1).

Figure 1. Psychosocial and behavioral conditions of type 2 diabetic patients attending follow-up care at Adama Hospital Medical College, 2023.
Diabetic health belief
Regarding diabetic health belief, 203 (50.1%) of study subjects had a high perceived susceptibility, while 300 (74.1%) perceived the severity of their condition as high. One hundred seventy-seven (43.7%) of participants had low perceived barriers, while 182 (44.9%) recognized a high perceived benefit of the recommended diet (Figure 2).

Figure 2. Diabetic health belief among type 2 diabetic patients attending follow up care at Adama Hospital Medical College, Ethiopia, 2023.
Magnitude of adherence to recommended diet
The highest mean score was obtained for the question regarding consuming foods high in sugar and fat with a mean of 5.72 ± 1.14 and 6.3 4 ± 1.04 times a week, respectively. In this study, we found that the magnitude of non-adherence to the recommended diet among patients with type 2 diabetes mellitus was 64.2% (95% CI: 59.8, 68.6), based on the PDAQ (Figure 3).
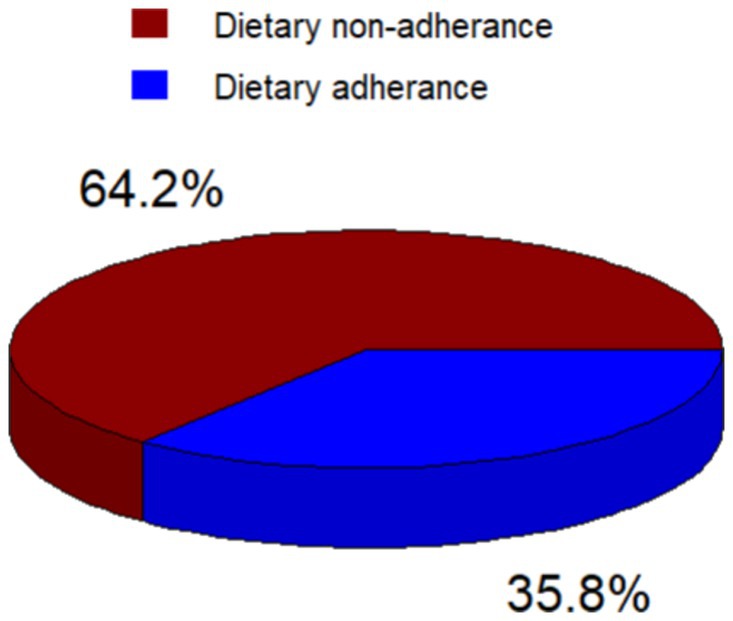
Figure 3. Dietary adherence status of type 2 diabetic patients attending follow up care at Adama Hospital Medical College, 2023.
Factors associated with adherence to dietary recommendations of type 2 DM patients
In a multivariate logistic regression model, patients with low and middle incomes were 8.0 (AOR: 8.0; 95% CI: 3.4–19.2) times and 2.7 (AOR: 2.7; 95% CI: 1.47–5.13) times more likely to be non-adherent to the recommended diet, respectively, compared to patients with higher incomes. Patients with a glycemic level of 126 mg/dL or higher were 2.1 (AOR: 2.1; 95% CI: 1.17–3.94) times more likely to be non-adherent to the recommended diet. The odd of non-adherence to dietary recommendations was 12.7 (AOR: 12.7; 95% CI: 5.79–28.2) times higher among food-insecure patients compared to food-secure patients. Patients with low diabetic knowledge were 2.8 (AOR: 2.8; 95% CI: 1.49–5.55) times more likely to be non-adherent to the recommended diet. Regarding diabetic health belief, patients with low perceived susceptibility for diabetic were 2.9 (AOR: 2.9; 95% CI: 1.62–5.45) times more likely to be non-adherent to dietary recommendations compare to those with high perceived susceptibility (Table 4).
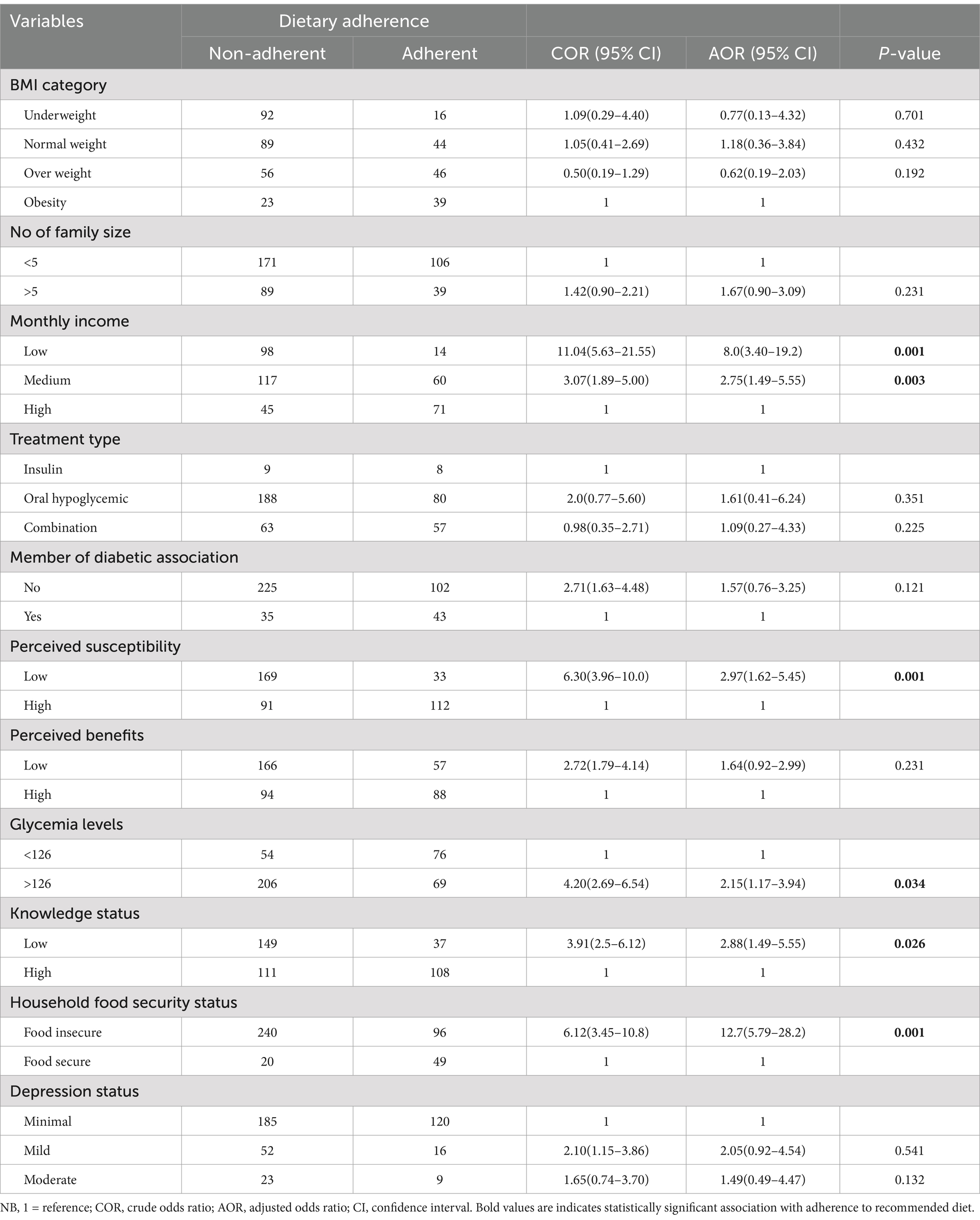
Table 4. Multivariable logistic regression analysis of the recommendation among dietary of patients with DM 2 type at Adama Hospital Medical College, Adama, Ethiopia, 2023 (n = 405).
Discussion
This study assessed the extent of adherence to dietary recommendations among individuals with type 2 diabetes patients. The findings revealed that 64.2% of participants did not adhere to the recommended diet (95% CI: 59.8–68.6%). This finding is in line with similar studies conducted in Kuwait 63.5% (24), India 63% (25), and Mexico 62% (26), and in Jimma Medical Center, Ethiopia 64.3% (27). However, it is lower than the findings from studies conducted in Egypt (97.5%), Nepal (87.5%), Yemen (79%), and Debre Tabor General Hospital (74.3%) (9, 28–30). The findings of the current study are higher than those reported in studies conducted in Malaysia 40.8% (31) and Ethiopian teaching hospitals 55.7% (14). This discrepancy may be attributed to differences in socio-economic and cultural characteristics, study settings, study periods, sample sizes, and the types of foods available in different countries (14).
We found that 67.9% of the respondents had poor glycemic control, as indicated by elevated fasting blood glucose levels. This finding aligns with a study conducted in Arba Minch, Ethiopia (32). However, it is higher than results from studies conducted at Dilchora Referral Hospital in Dire Dawa, Eastern Ethiopia (54.7%) (12), another study in northwest Ethiopia (57.5%) (33), and a systematic review in Ethiopia (51%) (34). The discrepancy between our findings and those of other studies may be due to differences in the tests used to measure glycemic control-while the other studies utilized the recommended HbA1c test, our study relied on the fasting blood glucose (FBG) test. Additionally, variations in study participants and settings could also contribute to these differences.
The results of the current study revealed a strong association between low- and middle-income levels and non-adherence to dietary recommendations among patients with type 2 diabetes mellitus (T2DM). Patients with low income had 8.0 times higher odds of non-adherence, while those with middle income had 2.7 times higher odds compared to higher-income counterparts. This finding consistent with studies conducted in Nepal (29), Ethiopia (12, 22, 35). This likely due to financial constraints that limit access to a diverse range of foods necessary for meeting daily nutritional requirements (12). The financial limitation can result in reliance on cheaper, calorie-dense, and nutrient-poor foods, worsening dietary non-adherence and negatively affecting health outcomes.
In this study, non-adherence to the recommended diet was significantly higher among patients living in food-insecure households. The odds of non-adherence were 12.7 times greater for those in food-insecure households compared to those in food-secure households. This finding is consistent with studies conducted in the USA and Addis Ababa, Ethiopia (36, 37). Food insecurity negatively impacts overall dietary quality, making it difficult for food-insecure patients with diabetes to adhere to healthy diet recommendations. Evidence indicates that food-insecure diabetic patients consume fewer fruits, vegetables, and proteins, and face challenges in maintaining regular eating habits and following recommended diet plans (38).
We found that glycemic levels exceeding 126 mg/dL were significantly associated with adherence to the recommended diet among patients with type 2 diabetes mellitus. This finding is consistent with a study conducted in Ethiopia (12, 32, 33). This association may be justified as higher blood glucose levels often reflect inadequate dietary management and non-adherence to nutritional recommendations. When patients fail to follow a prescribed diet that includes the right portions of carbohydrates, fiber, and essential nutrients, their glycemic control can worsen. Adhering to a recommended diet is crucial for regulating blood sugar levels and promoting balanced nutrition.
This study found a significant association between low diabetes knowledge and non-adherence to dietary recommendations among T2DM patients. Participants with low knowledge about diabetes were 2.9 times more likely to not follow the recommended diet compared to those with better knowledge. This finding is consistent with studies conducted in Nepal, Egypt, and Dire Dawa, Ethiopia (22, 29, 39). This may be due to the fact that adequate knowledge about diabetes enables patients to understand the importance of dietary guidelines, thereby reducing confusion in managing their condition. As knowledge increases, adherence to dietary advice improves, while poor understanding leads to higher non-adherence (29).
Patients with low perceived susceptibility were 2.9 times more likely to not adhere to dietary recommendations compared to those with high perceived susceptibility. In this study, 50.1% of participants reported high perceived susceptibility, aligning with findings from a study in government hospitals in the Ilu Aba Bora zone, where 72.7% reported similar levels of perceived susceptibility (40). This may be because individuals who perceive themselves as less at risk are less motivated to follow dietary guidelines, underestimating the potential harm of poor eating habits and thus leading to higher non-adherence.
Strength and limitation of the study
This study used the Perceived Dietary Adherence Questionnaire, a reliable and valid tool that is easy to administer and suitable for diverse populations, effectively assessing individuals’ perceptions of dietary adherence. Some limitations of the study include the following: First, the assessment of non-adherence to the recommended diet relied on self-reported data, which may be influenced by social desirability bias or recall issues, leading individuals to overestimate or underestimate their actual adherence. Second, the cross-sectional design limits the ability to establish temporal relationships between potential factors and dietary non-adherence. Finally, the absence of standardized practices for measuring carbohydrate spacing in the study context may limit the effectiveness of the assessment tool used.
Conclusion
The magnitude of non-adherence to dietary recommendations among patients with diabetes mellitus type 2 (T2DM) was significantly higher than reported in previous studies. Key factors contributing to this non-adherence include low to middle income, high glycemic levels, food insecurity, limited diabetes knowledge, and low perceived susceptibility. To improve adherence among T2DM patients, it is essential to implement comprehensive diabetes education, address socioeconomic barriers by providing financial and food security support, and enhance patient awareness of dietary risks.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
Ethics statement
Ethical clearance was obtained from the Adama Hospital Medical College of institutional review Board committee. Informed written consent was obtained from participants.
Author contributions
SA: Conceptualization, Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing – original draft, Writing – review & editing, Data curation, Funding acquisition, Resources. GD: Conceptualization, Investigation, Writing – original draft, Writing – review & editing, Project administration, Supervision. AM: Project administration, Supervision, Writing – original draft, Writing – review & editing, Validation. TC: Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing, Conceptualization, Formal analysis, Investigation, Methodology, Software, Visualization.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors like to acknowledge the study participants, data collectors, colleagues, and the Adama Hospital Medical College.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Loghmani, E. Diabetes mellitus: type 1 and type 2. In: Stang J, Story M, editors. Guidelines for adolescent nutrition services. Minneapolis: University of Minnesota. (2005). p. 167–82.
2. Audehm, R, Arthur, I, Barlow, J, Kennedy, M, Kilov, G, Leow, S, et al. General practice management of type 2 diabetes: 2014–15. East Melbourne VIC, Australia: Royal Australian College of General Practitioners (RACGP) (2014).
3. Ganiyu, AB, Mabuza, LH, Malete, NH, Govender, I, and Ogunbanjo, GA. Non-adherence to diet and exercise recommendations amongst patients with type 2 diabetes mellitus attending extension II Clinic in Botswana. Afr J Prim Health Care Fam Med. (2013) 5:1–6. doi: 10.4102/phcfm.v5i1.457
4. Lindström, J, Peltonen, M, Eriksson, JG, Ilanne-Parikka, P, Aunola, S, Keinänen-Kiukaanniemi, S, et al. Improved lifestyle and decreased diabetes risk over 13 years: long-term follow-up of the randomised Finnish diabetes prevention study (DPS). Diabetologia. (2013) 56:284–93. doi: 10.1007/s00125-012-2752-5
5. Sun, H, Saeedi, P, Karuranga, S, Pinkepank, M, Ogurtsova, K, Duncan, BB, et al. IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. (2022) 183:109119. doi: 10.1016/j.diabres.2021.109119
6. Association, A.D. Standards of medical Care in Diabetes—2014. Diabetes Care. (2014) 37:887–7. doi: 10.2337/dc14-S014
7. Bommer, C, Sagalova, V, Heesemann, E, Manne-Goehler, J, Atun, R, Bärnighausen, T, et al. Global economic burden of diabetes in adults: projections from 2015 to 2030. Diabetes Care. (2018) 41:963–70. doi: 10.2337/dc17-1962
8. Mogre, V, Johnson, NA, Tzelepis, F, Shaw, JE, and Paul, C. A systematic review of adherence to diabetes self-care behaviours: evidence from low-and middle-income countries. J Adv Nurs. (2019) 75:3374–89. doi: 10.1111/jan.14190
9. Abdelsalam, SES, Ismail, M, Hassan, S, Sultan, E, Elsherif, O, and Mikhail Salama, H. Perceived adherence and barriers to dietary recommendations among type 2 diabetic patients in a family practice clinic, Suez Canal university hospitals. Egypt Family Med J. (2022) 6:95–107. doi: 10.21608/efmj.2023.132549.1099
10. Tirfie, M, Tadesse, S, Woldie, H, Weldegiorgis, T, Birhanu, M, and Shibabaw, T. Dietary non-adherence and associated factors among individuals with diabetes who are on treatment follow up at Felege-Hiwot referral hospital, Northwest Ethiopia. Heliyon. (2020) 6:e04544. doi: 10.1016/j.heliyon.2020.e04544
11. Berhe, KK, Demissie, A, Kahsay, AB, and Gebru, HB. Diabetes self care practices and associated factors among type 2 diabetic patients in Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia-a cross sectional study. Int J Pharm Sci Res. (2012) 3:4219.
12. Mohammed, AS, Adem, F, Tadiwos, Y, Woldekidan, NA, and Degu, A. Level of adherence to the dietary recommendation and glycemic control among patients with type 2 diabetes mellitus in eastern Ethiopia: a cross-sectional study. Diabetes Metab Syndr Obes. (2020) 13:2605–12. doi: 10.2147/DMSO.S256738
13. Panahi, S, Rathi, N, Hurley, J, Sundrud, J, Lucero, M, and Kamimura, A. Patient adherence to health care provider recommendations and medication among free clinic patients. J Patient Exp. (2022) 9:23743735221077523. doi: 10.1177/23743735221077523
14. Mohammed, MA, and Sharew, NT. Adherence to dietary recommendation and associated factors among diabetic patients in Ethiopian teaching hospitals. Pan Afr Med J. (2019) 33:260. doi: 10.11604/pamj.2019.33.260.14463
15. Yosef, T, Nureye, D, Tekalign, E, Assefa, E, and Shifera, N. Medication adherence and contributing factors among type 2 diabetes patients at Adama hospital medical College in Eastern Ethiopia. SAGE Open Nurs. (2023) 9:23779608231158975. doi: 10.1177/23779608231158975
16. Asaad, G, Sadegian, M, Lau, R, Xu, Y, Soria-Contreras, D, Bell, R, et al. The reliability and validity of the perceived dietary adherence questionnaire for people with type 2 diabetes. Nutrients. (2015) 7:5484–96. doi: 10.3390/nu7075231
17. Toobert, DJ, Hampson, SE, and Glasgow, RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. (2000) 23:943–50. doi: 10.2337/diacare.23.7.943
18. Wn, A. Introduction to sample size calculation. Educ Med J. (2013) 5:5. doi: 10.5959/eimj.v5i2.130
19. Laghousi, D, Rezaie, F, Alizadeh, M, and Asghari Jafarabadi, M. The eight-item Morisky medication adherence scale: validation of its Persian version in diabetic adults. Caspian J Intern Med. (2021) 12:77–83. doi: 10.22088/cjim.12.1.77
20. Nicolau, V, Cortes, R, Lopes, M, Virgolino, A, Santos, O, Martins, A, et al. Time from diagnosis to initiation of antiretroviral therapy in portugal, a multicentric study. Healthcare (Basel) (2021) 9:797. doi: 10.3390/healthcare9070797
21. Organization, W.H. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: Recommendations for a public health approach World Health Organization (2016).
22. Getie, A, Geda, B, Alemayhu, T, Bante, A, Aschalew, Z, and Wassihun, B. Self-care practices and associated factors among adult diabetic patients in public hospitals of Dire Dawa administration, Eastern Ethiopia. BMC Public Health. (2020) 20:1–8. doi: 10.1186/s12889-020-09338-5
23. Adejoh, SO. Diabetes knowledge, health belief, and diabetes management among the Igala, Nigeria. SAGE Open. (2014) 4:2158244014539966. doi: 10.1177/2158244014539966
24. Al-Ibrahim, AAH. Factors associated with compliance to diabetes self-care behaviors and glycemic control among Kuwaiti people with type 2 diabetes. College Park: University of Maryland (2012).
25. Patel, M, Patel, IM, Patel, YM, and Rathi, SK. Factors associated with consumption of diabetic diet among type 2 diabetic subjects from Ahmedabad, Western India. J Health Popul Nutr. (2012) 30:447–55. doi: 10.3329/jhpn.v30i4.13328
26. Hernández-Ronquillo, L, Téllez-Zenteno, JF, Garduño-Espinosa, J, and González-Acevez, E. Factors associated with therapy non-compliance in type-2 diabetes patients. Salud Publica Mex. (2003) 45:191–7. doi: 10.1590/S0036-36342003000300008
27. Zeleke Negera, G, and Charles Epiphanio, D. Prevalence and predictors of non-adherence to diet and physical activity recommendations among type 2 diabetes patients in Southwest Ethiopia: a cross-sectional study. Int J Endocrinol. (2020) 2020:1–8. doi: 10.1155/2020/1512376
28. Alhariri, A, Daud, F, and Mohammed Saghir, SA. Factors associated with adherence to diet and exercise among type 2 diabetes patients in Hodeidah city, Yemen. Life. (2017) 7:264–71.
29. Parajuli, J, Saleh, F, Thapa, N, and Ali, L. Factors associated with non-adherence to diet and physical activity among Nepalese type 2 diabetes patients; a cross sectional study. BMC Res Notes. (2014) 7:1–9. doi: 10.1186/1756-0500-7-758
30. Ayele, AA, Emiru, YK, Tiruneh, SA, Ayele, BA, Gebremariam, AD, and Tegegn, HG. Level of adherence to dietary recommendations and barriers among type 2 diabetic patients: a cross-sectional study in an Ethiopian hospital. Clin Diabetes Endocrinol. (2018) 4:1–7. doi: 10.1186/s40842-018-0070-7
31. Ahmad, NS, Islahudin, F, and Paraidathathu, T. Factors associated with good glycemic control among patients with type 2 diabetes mellitus. J Diabetes Investig. (2014) 5:563–9. doi: 10.1111/jdi.12175
32. Sorato, MM, Tesfahun, C, and Lamessa, D. Levels and predictors of adherence to self-care behaviour among adult type 2 diabetics at Arba Minch general hospital, southern Ethiopia. J Diabetes Metab. (2016) 7:11. doi: 10.4172/2155-6156.1000684
33. Abebe, SM, Berhane, Y, Worku, A, Alemu, S, and Mesfin, N. Level of sustained glycemic control and associated factors among patients with diabetes mellitus in Ethiopia: a hospital-based cross-sectional study. Diabetes Metab Syndr Obes. (2015) 8:65–71. doi: 10.2147/DMSO.S75467
34. Ketema, DB, Leshargie, CT, Kibret, GD, Assemie, MA, Alamneh, AA, Kassa, GM, et al. Level of self-care practice among diabetic patients in Ethiopia: a systematic review and meta-analysis. BMC Public Health. (2020) 20:1–12. doi: 10.1186/s12889-020-8425-2
35. Feleke, SA, et al. Assessment of the level and associated factors with knowledge and practice of diabetes mellitus among diabetic patients attending at FelegeHiwot hospital, Northwest Ethiopia. Clin Med Res. (2013) 2:110. doi: 10.11648/j.cmr.20130206.11
36. Heerman, W, Wallston, KA, Osborn, CY, Bian, A, Schlundt, DG, Barto, SD, et al. Food insecurity is associated with diabetes self-care behaviours and glycaemic control. Diabet Med. (2016) 33:844–50. doi: 10.1111/dme.12896
37. Tezera, R, Sahile, Z, Yilma, D, Misganaw, E, Amare, E, and Haidar, J. Food security status of patients with type 2 diabetes and their adherence to dietary counselling from selected hospitals in Addis Ababa, Ethiopia: a cross-sectional study. PLoS One. (2022) 17:e0265523. doi: 10.1371/journal.pone.0265523
38. Lunze, K, Yurasova, E, Idrisov, B, Gnatienko, N, and Migliorini, L. Food security and nutrition in the Russian Federation–a health policy analysis. Glob Health Action. (2015) 8:27537. doi: 10.3402/gha.v8.27537
39. Mufunda, E, Wikby, K, Björn, A, and Hjelm, K. Level and determinants of diabetes knowledge in patients with diabetes in Zimbabwe: a cross-sectional study. Pan Afr Med J. (2012) 13:78.
Keywords: dietary, non-adherence, type 2 diabetic mellitus patients, Adama, Ethiopia
Citation: Abose S, Dassie GA, Megerso A and Charkos TG (2024) Adherence to recommended diet among patients with diabetes mellitus type 2 on follow-up at Adama Hospital Medical College, Ethiopia. Front. Med. 11:1484071. doi: 10.3389/fmed.2024.1484071
Edited by:
Aleksandra Klisic, Primary Health Care Center Podgorica, MontenegroReviewed by:
Ramona DeJesus, Mayo Clinic, United StatesMustafa Bayraktar, Atatürk University, Türkiye
Copyright © 2024 Abose, Dassie, Megerso and Charkos. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tesfaye Getachew Charkos, dGVzZmF5ZWdjaEBnbWFpbC5jb20=
 Saron Abose
Saron Abose Godana Arero Dassie
Godana Arero Dassie Tesfaye Getachew Charkos
Tesfaye Getachew Charkos