- 1Department of Gynecology, Women’s Hospital, School of Medicine, Zhejiang University, Hangzhou, China
- 2Shenzhen Key Laboratory of Reproductive Immunology for Peri-Implantation, Shenzhen Zhongshan Institute for Reproductive Medicine and Genetics, Shenzhen Zhongshan Obstetrics & Gynecology Hospital, Shenzhen, China
- 3Department of Gynecology, Shenzhen Second People’s Hospital, the First Affiliated Hospital of Shenzhen University, Shenzhen, China
Background: High-grade cervical intraepithelial neoplasia (HSIL) threatens fertility-aged women worldwide. Surgical excision remains standard but may compromise future pregnancy. Paiteling, a multi-herbal topical preparation, has shown in vitro anti-HPV activity, yet clinical evidence is scant.
Case presentation: Two reproductive-aged women with biopsy-proven HSIL refused loop electrosurgical excision. Biopsy slides were re-reviewed independently with p16 and Ki-67 immunostaining. Case 1 was CIN II and Case 2 was CIN III. Both patients received topical Paiteling (0.5 mL/lesion, three times weekly) plus 1% vaginal douche for 10 weeks.
Intervention & outcome: Lesions regressed completely within the treatment course. HPV-DNA testing confirmed HPV clearance by week 12. Follow-up colposcopy, cytology and directed biopsy remained negative at 12 months (Case 1) and 16 months (Case 2). Only mild transient vaginal burning occurred.
Conclusion: Topical Paiteling achieved histological and virological remission in two pathologically confirmed HSIL cases that declined excisional surgery. The findings suggest a fertility-preserving option worth systematic evaluation in prospective trials.
Introduction
Cervical intraepithelial neoplasia (CIN) is a precancerous lesion caused by persistent infection with high-risk human papillomavirus (HPV), closely linked to the progression to cervical cancer (1). CIN is classified into low-grade (LSIL or CIN I) and high-grade lesions (HSIL, encompassing CIN II and III) (2). Persistent infection with high-risk HPV subtypes such as HPV16 and 18 is a key risk factor for developing high-grade CIN and cervical cancer (2–4). Untreated high-grade CIN has a risk of progression to invasive cancer, with CIN II having a 18% progression rate and CIN III ranging from 22 to 40% within 30 years (3, 5, 6). Globally, the incidence of HSIL in reproductive-aged women continues to rise, reaching 498/100,000 in recent Chinese data (7). Given this risk, current WHO and ASCCP guidelines recommend surgical excision—most commonly cold knife conization (CKC), laser conization, or the loop electrosurgical excision procedure (LEEP)—as the standard treatment (8–10). Conization, depending on cone size, is also considered a fertility-sparing treatment, albeit with variable obstetric impact (10–12). Surgical interventions, though effective, come with risks such as bleeding, infection, and scarring (13), as well as potential complications like cervical insufficiency, stenosis, and preterm birth in women of reproductive age (14, 15). As fertility preservation becomes an increasing concern for women of reproductive age, there is a growing demand for conservative alternatives for high-grade CIN (14).
Non-surgical strategies—including photodynamic therapy, immunomodulatory agents, and Traditional Chinese Medicine (TCM)—are attracting interest for their potential to avoid cervical tissue loss (10, 16–18). Among TCM approaches, external therapies such as fumigation, rubbing, and soaking with plant-derived preparations have been reported to achieve local viral clearance without the tissue damage associated with surgery (16, 17). Paiteling, a pure TCM formulation, has shown encouraging results in treating HPV infection and condyloma acuminatum (17, 19–21), yet its role in managing high-grade CIN remains unexplored. Here, we present a retrospective review of two cases of reproductive-age women with biopsy-confirmed HSIL and concomitant vaginal and cervical condyloma acuminatum, successfully managed with topical Paiteling.
Case presentation
Case 1
A 29-year-old nulliparous woman of Han ethnicity, residing in Shenzhen, China, was diagnosed with high-risk HPV-infected CIN II combined with VaIN I-II during a community cervical cancer screening and presented to our hospital’s gynecology department for further treatment in April 2018. Gynecological examination revealed multiple warty vegetations on the vaginal wall and cervix, characterized by papillary hyperplasia with dirty gray exudate on the surface, accompanied by an unpleasant odor (Figure 1A). A positive contact bleeding test was observed. The ThinPrep Cytology Test (TCT) revealed abnormal DNA ploidy cells, and cervical HPV typing confirmed HPV16 positivity (Figures 1B, C). Colposcopy and biopsy findings showed CIN II with condyloma on the cervix, and Vaginal intraepithelial neoplasia (VaIN) I-II with condyloma on the anterior and right side of the vaginal wall (Supplementary Table 1). Her medical history was unremarkable, with no history of chronic illness, immunodeficiency, prior cervical procedures, or prophylactic HPV vaccination. She denied any family history of malignancy or genetic cancer syndromes, and her psychosocial history revealed no occupational or behavioral risk factors for HPV persistence (Table 1).
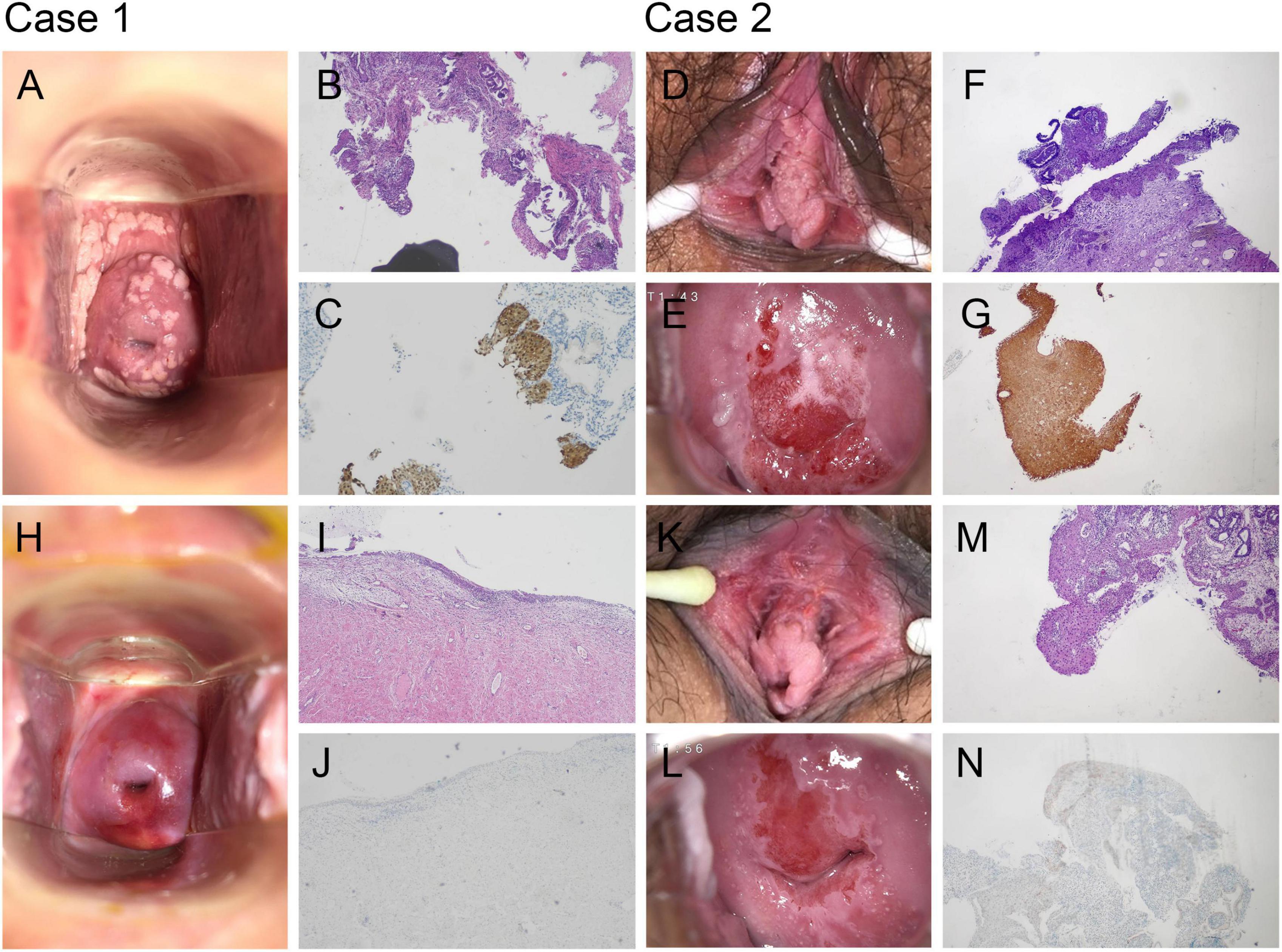
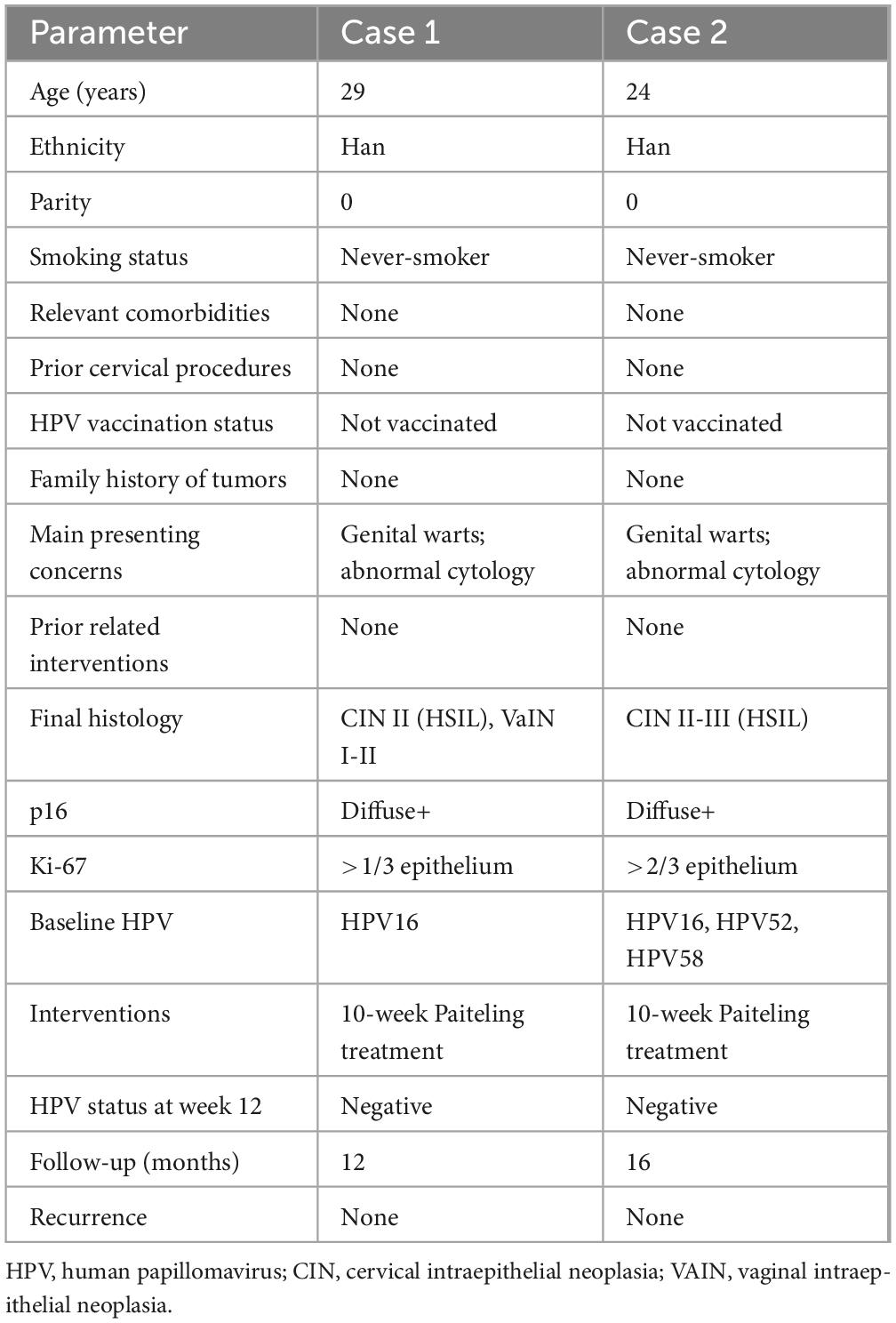
Figure 1. Topical Paiteling achieves complete regression of high-grade cervical intraepithelial neoplasia. (A) Case 1: Extensive condylomatous plaques on the vaginal wall and ectocervix before treatment. (B,C) Case 1: Baseline cervical biopsy confirming cervical intraepithelial neoplasia grade II (CIN II)/high-grade squamous intraepithelial lesions (HSIL). Hematoxylin and eosin (H&E) staining shows full-thickness atypia (B). p16 immunostaining is diffusely positive (C). (D,E) Case 2: Vulvar and cervical lesions at presentation. (F,G) Case 2: Baseline biopsy confirming CIN III/HSIL with diffuse p16 positivity. (H) Case 1: Macroscopic view after the 10-week course, showing smooth epithelium without visible lesions. (I,J) Case 1: Post-treatment biopsy reveals only chronic cervicitis and is p16-negative, consistent with histological remission. (K,L) Case 2: Vulva and cervix after therapy, demonstrating complete clinical resolution. (M,N) Case 2: Follow-up biopsy shows normal epithelium and absent p16 expression, indicating eradication of CIN III/HSIL. All histological images: original magnification ×100.
Case 2
A 24-year-old nulliparous woman of Han ethnicity presented to the gynecology department in November 2021 seeking treatment advice after being diagnosed with high-risk HPV–infected CIN III. Her primary concerns were the presence of multiple genital warts and the recent histologic confirmation of HSIL. Gynecological examination revealed multiple hyperkeratotic, cauliflower-like warty lesions on the vulva and vagina, with a positive contact bleeding test (Figures 1D, E). Cervical HPV typing was positive for HPV16, 52, and 58 (Supplementary Table 1). Colposcopy and biopsy demonstrated CIN II–III with severe dysplasia and glandular involvement, along with a positive endocervical curettage (ECC) for CIN III (Figures 1F, G; Supplementary Table 1). The squamocolumnar junction and lesion margins were fully visualized on colposcopy. Her medical history included a recent high-risk HPV infection and a 1-year history of intermittent oral contraceptive use; she was a never-smoker and had no significant comorbidities, prior cervical interventions, or family history of cervical cancer. She had not received HPV vaccination prior to presentation. Psychosocial history was unremarkable for HPV persistence risk factors. She had not attempted other medical interventions for her current lesions before presentation (Table 1).
Inclusion and exclusion criteria, diagnostic assessment, treatment and follow-up
The inclusion criteria for this case study were women aged 18–45 years, diagnosed with high-grade CIN (CIN II or III) and HPV-positive condyloma acuminatum, with no prior cervical surgery or radiation. Exclusion criteria included pregnancy or lactation, allergies to traditional Chinese medicine, immunocompromised conditions, and other malignancies or severe gynecological disorders. Diagnostic evaluation included pelvic examination, ThinPrep Cytology Test (TCT), high-risk HPV genotyping, colposcopy with directed cervical and vaginal biopsies, and endocervical curettage (ECC) where indicated. Histopathological assessment was performed by two independent senior pathologists. The principal diagnostic challenge was differentiating high-grade CIN from reactive epithelial changes caused by extensive condylomatous lesions, which could obscure lesion margins during colposcopic evaluation. Differential diagnoses considered included low-grade squamous intraepithelial lesions (LSIL), benign condyloma acuminatum without intraepithelial neoplasia, and vaginal intraepithelial neoplasia (VaIN) without concurrent cervical involvement. The final diagnosis in both cases was established based on concordant histology from multiple biopsy sites and positive hr-HPV testing. Follow-up was conducted at 1, 6, and 12 months post-treatment. At each visit, HPV testing was performed to assess for persistent infection, and TCT along with colposcopy were used to monitor for recurrence. If request by patients or abnormal findings were observed, a cervical biopsy was conducted at the 12-month visit. Patients were also asked to report any abnormal symptoms, and further tests were done if necessary.
Following the WHO and ASCCP guidelines, our senior gynecologists initially recommended LEEP surgery (8, 9). A detailed counseling session was conducted, during which the patients were thoroughly informed about the benefits of surgical treatment, as well as the risks of recurrence, scarring, cancerization, and obstetric complications, such as cervical insufficiency and preterm birth. These discussions were fully documented in the patient records. Both patients, after considering these risks, declined surgery, expressing concerns over potential long-term effects. This refusal of surgery was formally recorded, with the patients signing a document acknowledging their decision to decline excisional therapy and the associated oncologic risks. Non-surgical alternatives, including photodynamic therapy and Traditional Chinese Medicine (TCM), were then presented and discussed in terms of their safety, efficacy, and potential for fertility preservation. After thorough deliberation, both patients opted for the standard 10-week Paiteling treatment regimen, consisting of 6 weeks of cervical application followed by 4 weeks of vaginal douching under physician supervision (Supplementary Table 2). Treatment adherence was complete for both cases. Adverse events were monitored throughout therapy and documented according to the Common Terminology Criteria for Adverse Events (CTCAE, version 5.0) framework (22) where applicable. Symptom severity, including intermittent mild pain and a burning sensation, was assessed qualitatively via patient self-report; no events met the criteria for Grade ≥ 2 severity. All symptoms were transient, resolved spontaneously without medical intervention, and did not lead to treatment interruption or dose modification. Upon completion of the regimen, both patients expressed satisfaction with the outcomes. Follow-up evaluations demonstrated clinical remission, negative hr-HPV testing, and no abnormal findings on TCT, colposcopy, or cervical biopsy (Case 1: Figures 1H–J; Case 2: Figures 1K–N) (Table 1; Supplementary Table 1).
Discussion
High-grade cervical intraepithelial neoplasia (CIN II–III, HSIL) carries a low likelihood of spontaneous regression and a lifetime risk of progression to invasive cancer of 22%–40% (3, 5, 6). Accordingly, both the WHO and ASCCP recommend excisional treatment as the gold standard (8, 9). Nevertheless, excisional procedures may be followed by persistent high-risk human papillomavirus (hr-HPV) infection in up to 68% of patients, with ongoing viral persistence markedly increasing recurrence risk (4, 23). Furthermore, meta-analyses have demonstrated that prior excision is associated with significantly elevated risks of adverse obstetric outcomes, including a 1.78–3.78-fold increase in preterm birth, a 1.99-fold increase in premature rupture of membranes, and a 1.94-fold increase in low birth weight infants compared with women without prior excision (11, 14, 24).
Medical and other non-excisional approaches, such as topical immunomodulators (e.g., imiquimod), photodynamic therapy, and Traditional Chinese Medicine formulations, may avoid cervical tissue loss and thus potentially mitigate these obstetric risks (10, 16–18). Topical imiquimod and photodynamic therapy, which have shown lesion regression rates of 50%–80% in selected patients (25, 26). The APL-1702 (a photodynamic therapy drug-device combination) phase III trial also reported favorable HPV clearance and safety outcomes in a large HSIL cohort (27). Emerging robotic-assisted precision excision techniques also aim to minimize tissue removal while ensuring complete lesion eradication, aligning with the principles of non-excisional therapies that prioritize fertility preservation and reduction of obstetric complications (28, 29). In addition, adjuvant HPV vaccination has been shown to significantly lower the recurrence of high-grade CIN, with odds ratios of 0.33 for CIN II + and 0.28 for CIN III, underscoring its potential role in secondary prevention (30). Compared with these modalities, Paiteling represents a non-invasive, cost-effective alternative with potential antiviral and immunomodulatory effects, and without the need for specialized equipment. Our report suggests that Paiteling may offer comparable histological and virological remission, with minimal systemic adverse effects. However, the oncologic safety of non-excisional strategies remains less well established, with limited high-quality evidence on long-term recurrence rates, particularly in HSIL. Therefore, both oncologic safety and obstetric outcomes must be weighed when comparing medical and excisional approaches. Treatment selection should be individualized, balancing reproductive goals against the need to minimize cancer progression risk, ideally within the framework of shared decision-making and close post-treatment surveillance.
Paiteling, a topical formula developed by the Chinese Academy of Medical Sciences, combines Brucea javanica, Isatis tinctoria, Hedyotis diffusa, Sophora flavescens, and Cnidium monnieri (20, 21) (Supplementary Table 2). The alkaloids, flavonoids and quassinoids in these herbs synergistically lyse infected epithelial cells; shed necrotic debris removes latent HPV, while sea-buckthorn oil constituents (anthocyanins, quercetin) dampen inflammation and support re-epithelialisation (31). Paiteling down-regulates E6/E7 transcription, blocks PI3K/Akt signaling, and triggers apoptosis in cervical cancer lines (21, 32).
Clinical evidence—although limited to low-grade disease—has been encouraging. Cure rates of 92%–100% for condyloma acuminatum and 89% for LSIL have been reported, with minimal pain and no scarring (17, 19–21, 33). Our two HSIL cases extend these findings: topical Paiteling cleared hr-HPV and achieved durable histological remission without compromising cervical architecture. To the best of our knowledge, this is the first report on the use of Paiteling in biopsy-confirmed HSIL coexisting with genital warts. These preliminary observations are encouraging but warrant cautious interpretation. The study is inherently constrained by its retrospective nature, two-case sample size, single-center setting, absence of a comparator group, and relatively limited follow-up duration, which together limit the generalizability of the findings. Obstetric outcomes were not evaluated, and any conclusions regarding safety remain provisional. The evaluation of lesion regression in this report relied on histopathological clearance and HPV negativity. Future studies should incorporate standardized, validated outcome scoring systems for treatment response—such as the Lower Anogenital Squamous Terminology (LAST) criteria or immunologic markers to enhance objectivity and clinical translatability. Given the 12- to 16-month follow-up, our study cannot determine long-term recurrence or progression risk, particularly as latent HPV reactivation may occur beyond the follow-up horizon. Accordingly, our findings should be interpreted as preliminary, and long-term surveillance is essential for drawing definitive conclusions about sustained remission. No systemic side effects were reported in our cases; however, detailed safety data, particularly regarding systemic absorption, endocrine disruption, or reproductive toxicity of Paiteling, are lacking. Preclinical pharmacokinetic studies and reproductive toxicity models are warranted before wider clinical adoption, particularly in women seeking future pregnancies. Rigorous, randomized controlled trials incorporating virological endpoints and long-term obstetric follow-up are required to establish the efficacy, optimal regimen, and safety profile of this approach in reproductive-age women who decline or are ineligible for excisional therapy. Furthermore, optimal management of CIN should be grounded in comprehensive patient counseling, formal documentation of informed consent, and ethics committee oversight, ensuring that patients are fully apprised of the potential risks and benefits of all therapeutic options, and that autonomy is upheld throughout the decision-making process.
Conclusion
Topical Paiteling may be a promissing non-excisional option for selected women with HSIL who prioritize fertility preservation. Rigorous clinical trials are required to establish efficacy, safety, and obstetric impact.
Data availability statement
The original contributions presented in this study are included in this article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
JL: Writing – original draft, Writing – review & editing, Conceptualization, Data curation, Supervision. JY: Writing – original draft. ZY: Conceptualization, Data curation, Supervision, Writing – review & editing. SG: Conceptualization, Data curation, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the National Natural Science Foundation of China (82403109), the Guangdong Basic and Applied Basic Research Foundation (2023A1515110029) and the Clinical Research Funding from Shenzhen Second People’s Hospital (20223357029).
Acknowledgments
We thank Yue Li and Wenfeng Peng, Department of Pathology, for blinded slide review.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2025.1503083/full#supplementary-material
References
1. Kalliala I, Athanasiou A, Veroniki A, Salanti G, Efthimiou O, Raftis N, et al. Incidence and mortality from cervical cancer and other malignancies after treatment of cervical intraepithelial neoplasia: a systematic review and meta-analysis of the literature. Ann Oncol. (2020) 31:213–27. doi: 10.1016/j.annonc.2019.11.004
2. Lee C, Chang S. WHO Classification of Tumours Editorial Board. Female Genital Tumours. Geneva: WHO (2020).
3. McCredie M, Sharples K, Paul C, Baranyai J, Medley G, Jones R, et al. Natural history of cervical neoplasia and risk of invasive cancer in women with cervical intraepithelial neoplasia 3: a retrospective cohort study. Lancet Oncol. (2008) 9:425–34. doi: 10.1016/S1470-2045(08)70103-7
4. Bogani G, Sopracordevole F, Ciavattini A, Vizza E, Vercellini P, Ghezzi F, et al. HPV persistence after cervical surgical excision of high-grade cervical lesions. Cancer Cytopathol. (2024) 132:268–9. doi: 10.1002/cncy.22760
5. Peto J, Gilham C, Fletcher O, Matthews F. The cervical cancer epidemic that screening has prevented in the UK. Lancet. (2004) 364:249–56. doi: 10.1016/S0140-6736(04)16674-9
6. Bekos C, Schwameis R, Heinze G, Gärner M, Grimm C, Joura E, et al. Influence of age on histologic outcome of cervical intraepithelial neoplasia during observational management: results from large cohort, systematic review, meta-analysis. Sci Rep. (2018) 8:6383. doi: 10.1038/s41598-018-24882-2
7. Zhou X, Han T, Guo T, Liu Y, Li H, Yingxia W, et al. Cervical intraepithelial neoplasia and cervical cancer in Hunan Province, China, 2020-2023. Front Oncol. (2024) 14:1480983. doi: 10.3389/fonc.2024.1480983
8. Olusola P, Banerjee H, Philley J, Dasgupta S. Human papilloma virus-associated cervical cancer and health disparities. Cells. (2019) 8:622. doi: 10.3390/cells8060622
9. Perkins R, Guido R, Castle P, Chelmow D, Einstein M, Garcia F, et al. 2019 ASCCP risk-based management consensus guidelines: updates through 2023. J Low Genit Tract Dis. (2024) 28:3–6. doi: 10.1097/LGT.0000000000000788
10. Ferrari F, Bonetti E, Oliveri G, Giannini A, Gozzini E, Conforti J, et al. Cold knife versus carbon dioxide for the treatment of preinvasive cervical lesion. Medicina. (2024) 60:1056. doi: 10.3390/medicina60071056
11. Athanasiou A, Veroniki A, Efthimiou O, Kalliala I, Naci H, Bowden S, et al. Comparative effectiveness and risk of preterm birth of local treatments for cervical intraepithelial neoplasia and stage IA1 cervical cancer: a systematic review and network meta-analysis. Lancet Oncol. (2022) 23:1097–108. doi: 10.1016/S1470-2045(22)00334-5
12. Jorgensen K, Agusti N, Wu C, Kanbergs A, Pareja R, Ramirez P, et al. Fertility-sparing surgery vs standard surgery for early-stage cervical cancer: difference in 5-year life expectancy by tumor size. Am J Obstet Gynecol. (2024) 230:663.e1-e13. doi: 10.1016/j.ajog.2024.02.012
13. Xie W, Wang Y, You K, Wang Y, Geng L, Li R. Impact of cervical intraepithelial neoplasia and treatment on IVF/ICSI outcomes. Hum Reprod. (2023) 38:ii14–23. doi: 10.1093/humrep/dead009
14. Liu R, Liu C, Ding X. Association between loop electrosurgical excision procedure and adverse pregnancy outcomes: a meta-analysis. J Matern Fetal Neonatal Med. (2023) 36:2183769. doi: 10.1080/14767058.2023.2183769
15. Lieb J, Mondal A, Lieb L, Fehm T, Hampl M. Pregnancy outcome and risk of recurrence after tissue-preserving loop electrosurgical excision procedure (LEEP). Arch Gynecol Obstet. (2023) 307:1137–43. doi: 10.1007/s00404-022-06760-5
16. Desravines N, Miele K, Carlson R, Chibwesha C, Rahangdale L. Topical therapies for the treatment of cervical intraepithelial neoplasia (CIN) 2-3: a narrative review. Gynecol Oncol Rep. (2020) 33:100608. doi: 10.1016/j.gore.2020.100608
17. Cobbinah P, Zheng Zheng S, Oklah F, Yuyang Z. Comparative analysis of Paiteliing a traditional Chinese medicine (TCM) and CO2 laser therapy for high-risk HPV-associated with LSIL (CIN1) lesions. Eur J Obstet Gynecol Reprod Biol. (2024) 302:81–6. doi: 10.1016/j.ejogrb.2024.08.042
18. Inayama Y, Takamatsu S, Hamanishi J, Mizuno K, Horinouchi N, Yamanoi K, et al. Imiquimod for cervical and vaginal intraepithelial neoplasia: a systematic review and meta-analysis. Obstet Gynecol. (2023) 142:307–18. doi: 10.1097/AOG.0000000000005256
19. Hu Y, Lu Y, Qi X, Chen X, Liu K, Zhou X, et al. Clinical efficacy of paiteling in the treatment of condyloma acuminatum infected with different subtypes of HPV. Dermatol Ther. (2019) 32:e13065. doi: 10.1111/dth.13065
20. Wang M, Lin L, Li L. Efficacy and safety of giant condyloma acuminatum with monotherapy of topical traditional Chinese medicine: report of eight cases. Infect Drug Resist. (2021) 14:1375–9. doi: 10.2147/IDR.S302195
21. Liu Y, Zheng P, Jiao T, Zhang M, Wu Y, Zhang X, et al. Paiteling induces apoptosis of cervical cancer cells by down-regulation of the E6/E7-Pi3k/Akt pathway: a network pharmacology. J Ethnopharmacol. (2023) 305:116062. doi: 10.1016/j.jep.2022.116062
22. Shah S. Common terminology criteria for adverse events. Bethesda, MA: National Cancer Institute (2022).
23. Bogani G, Sopracordevole F, Ciavattini A, Vizza E, Vercellini P, Giannini A, et al. Duration of human papillomavirus persistence and its relationship with recurrent cervical dysplasia. Eur J Cancer Prev. (2023) 32:525–32. doi: 10.1097/CEJ.0000000000000822
24. Kyrgiou M, Athanasiou A, Paraskevaidi M, Mitra A, Kalliala I, Martin-Hirsch P, et al. Adverse obstetric outcomes after local treatment for cervical preinvasive and early invasive disease according to cone depth: systematic review and meta-analysis. BMJ. (2016) 354:i3633. doi: 10.1136/bmj.i3633
25. Cokan A, Pakiž M, Serdinšek T, Dovnik A, Kodrič T, Repše Fokter A, et al. Comparison of conservative treatment of cervical intraepithelial lesions with imiquimod with standard excisional technique using LLETZ: a randomized controlled trial. J Clin Med. (2021) 10:5777. doi: 10.3390/jcm10245777
26. Polterauer S, Reich O, Widschwendter A, Ganhoer-Schimboeck J, Bogner G, Berger R. P39 ITIC2 trial topical imiquimod versus conization to treat cervical intraepithelial neoplasia: randomised controlled, non-inferiority trial. Int J Gynecol Cancer. (2019) 29:A72–3. doi: 10.1136/ijgc-2019-ESGO.101
27. Wang Y, Chen F, Lang J, Li R, He E, Chen E, et al. APL-1702 long-term efficacy and safety for cervical histologic, high-grade squamous intraepithelial lesions: Results from a randomized, phase III, global study. Gynecol Oncol. (2024) 190:S60. doi: 10.1016/j.ygyno.2024.07.090
28. Bellotti J, Gutierres I, Furtado Y, Patury P, Figueiredo J, Guitmann G, et al. Surgical, oncologic, and obstetric outcomes of radical trachelectomy in early-stage cervical cancer: results from a retrospective cohort study at Brazil national cancer institute. Front Oncol. (2024) 14:1267625. doi: 10.3389/fonc.2024.1267625
29. Manning-Geist B, Grace M, Sonoda Y. Trachelectomy and fertility-sparing procedures for early-stage cervical cancer: a state of the science review. Gynecol Oncol. (2024) 181:179–82. doi: 10.1016/j.ygyno.2024.01.014
30. Di Donato V, Caruso G, Bogani G, Cavallari E, Palaia G, Perniola G, et al. HPV vaccination after primary treatment of HPV-related disease across different organ sites: a multidisciplinary comprehensive review and meta-analysis. Vaccines. (2022) 10:239. doi: 10.3390/vaccines10020239
31. Tao P, Zheng W, Meng X, Chen J, Sun A, Shou Q, et al. Effect of paiteling on human papillomavirus infection of the cervix. Mol Clin Oncol. (2017) 7:957–64. doi: 10.3892/mco.2017.1454
32. Zhang H, Yin S, Wang L, Jia L, Su G, Liu X, et al. Seed oil of Brucea javanica induces apoptosis through the PI3K/Akt signaling pathway in acute lymphocytic leukemia Jurkat cells. Chin J Nat Med. (2021) 19:608–20. doi: 10.1016/S1875-5364(21)60060-2
Keywords: high-grade cervical intraepithelial neoplasia (HSIL), topical Paiteling, human papillomavirus, fertility-preserving therapy
Citation: Li J, Yang J, Yu Z and Guan S (2025) Histologically confirmed high-grade cervical intraepithelial neoplasia successfully treated with topical Paiteling: a two-case report. Front. Med. 12:1503083. doi: 10.3389/fmed.2025.1503083
Received: 17 March 2025; Accepted: 22 September 2025;
Published: 15 October 2025.
Edited by:
Sajad A. Dar, Jazan University, Saudi ArabiaReviewed by:
Filippo Alberto Ferrari, Sacro Cuore Don Calabria Hospital (IRCCS), ItalyTullio Golia D’Augè, Sapienza University of Rome, Italy
Naseem Akhter, Barrow Neurological Institute, United States
Copyright © 2025 Li, Yang, Yu and Guan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jing Li, a3Jpa2xlZUBjb25uZWN0LmhrdS5oaw==; Zhiying Yu, bGl6aGV5enlAMTYzLmNvbQ==; Songqing Guan, bG92ZWNjMTM4QDE2My5jb20=
 Jing Li
Jing Li Jie Yang2
Jie Yang2