- 1Clinical Skills Training Center, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, China
- 2Department of Obstetrics and Gynecology, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, China
- 3Department of Obstetrics and Gynecology, Qilu Hospital of Shandong University Dezhou Hospital, Dezhou, China
- 4Department of Anesthesiology, Qilu Hospital of Shandong University, Jinan, China
- 5Department of Anesthesiology, Jinan Maternity and Child Care Hospital Affiliated to Shandong First Medical University, Jinan, China
Background: Pregnant women with placenta accreta spectrum (PAS), particularly those with placenta increta or placenta percreta, undergoing emergency cesarean section are at a high risk of excessive intraoperative hemorrhage and related complications. This study aimed to evaluate maternal and neonatal outcomes and to identify risk factors associated with emergency cesarean section in women with PAS.
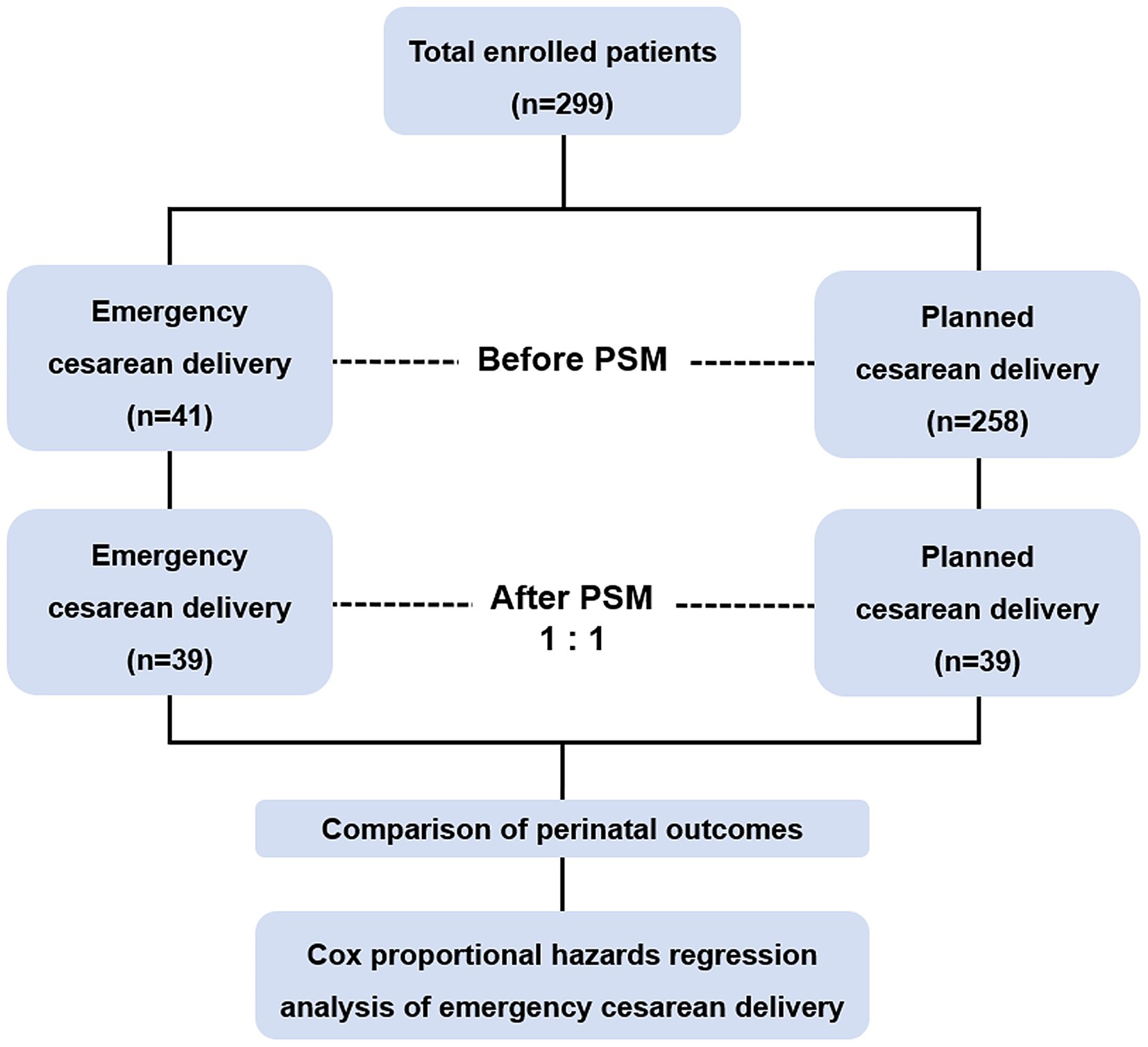
Methods: A multicenter retrospective cohort study was conducted, including PAS patients who underwent cesarean section at three tertiary hospitals between January 2016 and January 2023. After 1:1 propensity score matching (PSM), clinical characteristics were compared between the emergency and elective cesarean section groups using chi-square tests and nonparametric rank-sum tests. Risk factors for emergency cesarean section were identified through Cox proportional hazards regression analysis.
Results: Among 299 patients included in the study, 78 were selected for analysis after PSM. In the matched cohort, patients in the emergency cesarean section group required significantly more packed red blood cell transfusions (p = 0.034), had a higher rate of ascending branch ligation of the uterine artery (p < 0.001), required more neonatal intensive care unit admissions (p = 0.041), and delivered neonates with lower birth weight (p = 0.044). Key risk factors for emergency cesarean section included a history of more than one prior cesarean section [hazard ratio (HR), 2.34; 95% confidence intervals (CI): 1.24–4.42], preoperative hemoglobin levels ≤100 g/L (HR, 2.28; 95% CI: 1.19–4.40), preeclampsia (HR, 2.93; 95% CI, 1.10–7.82), and vascular lacunae within the placenta (HR, 0.40; 95% CI, 0.21–0.76).
Conclusion: Emergency cesarean section in PAS patients is associated with increased transfusion requirements and adverse neonatal outcomes. Close monitoring and enhanced management of patients with identified risk factors may help improve maternal and neonatal outcomes.
1 Introduction
Placenta accreta spectrum (PAS) refers to a group of disorders characterized by abnormal adherence of the placental trophoblast to the uterine myometrium, encompassing three subtypes: placenta accreta, placenta increta, and placenta percreta (1). Over recent decades, the incidence of PAS has increased significantly, largely attributed to the rising rates of cesarean deliveries (2). As one of the most severe obstetric complications, PAS poses a significant threat to maternal health, primarily due to the failure of the placenta to detach from the uterus after delivery. This often results in life-threatening conditions such as disseminated intravascular coagulation (DIC), intensive care unit (ICU) admission, hysterectomy, and even maternal death (3).
Optimal management of PAS requires delivery in specialized centers equipped with multidisciplinary teams capable of providing comprehensive care. These centers must ensure immediate access to blood products, neonatal and adult intensive care facilities, and surgeons experienced in complex pelvic surgeries (4, 5). While clinical guidelines recommend planned delivery for PAS patients between 34 and 38 weeks of gestation, there remains no consensus on the optimal timing, as individual patient conditions vary significantly (6).
Our previous study revealed that approximately 10.8% of women with severe PAS and placenta previa required emergency cesarean delivery due to complications such as fetal distress, uterine contractions, or vaginal bleeding (7). Emergency cesarean delivery in these patients is strongly associated with increased intraoperative blood loss, higher maternal morbidity, and poor neonatal outcomes (8). Unlike planned cesarean deliveries, emergency procedures often lack sufficient time for preoperative preparation, including the assessment of maternal and fetal conditions, organization of blood transfusion protocols, and placement of prophylactic catheters or balloons in pelvic arteries to control hemorrhage. These limitations exacerbate surgical risks, resulting in higher rates of complications, such as massive blood transfusions, coagulation dysfunction, and urinary tract injuries (9).
Given these challenges, early and accurate risk assessment is crucial to identify PAS patients at high risk of requiring emergency cesarean delivery. This is particularly important in cases of placenta previa complicated by suspected placenta increta or percreta, where the likelihood of emergency interventions and adverse outcomes is significantly elevated.
In this multicenter retrospective cohort study, we utilized a propensity score matching (PSM) approach to compare perinatal outcomes between emergency and planned cesarean deliveries in PAS patients. Additionally, we sought to identify key risk factors associated with the need for emergency interventions. The findings of this study aim to support more individualized prenatal care strategies and improve maternal and neonatal outcomes in patients with PAS and placenta previa.
2 Materials and methods
2.1 General information
This retrospective cohort study included patients diagnosed with PAS (placenta increta or percreta) based on preoperative imaging, intraoperative findings, or postoperative pathological evaluation. All patients underwent pregnancy termination between January 2018 and June 2023 at four medical centers in Shandong Province, China: Shandong Provincial Hospital affiliated with Shandong First Medical University, Qilu Hospital of Shandong University, Jinan Maternity and Child Care Hospital affiliated with Shandong First Medical University, and Qilu Hospital of Shandong University Dezhou Hospital. All enrolled patients underwent uterus-preserving cesarean delivery, except those who required immediate hysterectomy due to uncontrollable intraoperative hemorrhage.
2.2 Patient variables
Patient clinical characteristics were extracted from medical records and included the following variables: maternal age at delivery, duration of labor, history of previous cesarean sections, obstetric complications, findings from prenatal obstetric ultrasonography, preoperative hemoglobin (HGB) levels, abdominal aorta balloon placement (BPAA), intraoperative hemostatic interventions, intraoperative blood loss, volume of transfused packed red blood cells (PRBC), perinatal outcomes, fetal birth weight, Apgar scores, and neonatal intensive care unit (NICU) admissions. Continuous variables were grouped according to either the median value in our study population or established clinical reference ranges to facilitate analysis and interpretation.
2.3 Definition and outcomes
The diagnosis of PAS in this study was primarily based on preoperative imaging assessments, including ultrasound and/or magnetic resonance imaging (MRI), and further confirmed by intraoperative findings observed by experienced obstetricians, with histopathological examination of the placenta conducted when available. The classification followed the criteria established by the International Federation of Gynecology and Obstetrics (FIGO) (1). According to FIGO, placenta percreta is characterized intraoperatively by grossly abnormal appearance of the placental bed, marked hypervascularity, and failure of placental separation during gentle cord traction, often accompanied by invagination of the uterine wall without visible serosal invasion; in contrast, placenta increta involves deeper myometrial invasion, with extension to the uterine serosa and potentially into adjacent pelvic structures, such as the bladder, broad ligament, vaginal wall, pelvic sidewall, or other pelvic organs (1). The diagnosis of placenta previa was confirmed by ultrasonographic examination performed after 16 weeks of gestation.
The primary outcome of this study was the occurrence of emergency cesarean delivery. For analytical purposes, the study population was categorized into two groups based on the timing and indication for delivery: the emergency cesarean delivery group and the planned cesarean delivery group. The emergency cesarean delivery group comprised patients who required urgent surgical intervention due to acute maternal or fetal complications. In contrast, the planned cesarean delivery group included patients who underwent cesarean section as scheduled, with no emergent indications. The most common indications for emergency cesarean delivery in this cohort included fetal distress, premature rupture of membranes, vaginal bleeding, uterine contractions, and uterine rupture.
2.4 Statistical analysis
Continuous variables were analyzed using the Mann–Whitney U-test, while categorical variables were compared using the chi-square test. A p-value of <0.05 was considered statistically significant.
PSM was applied to minimize selection bias between the emergency and elective cesarean delivery groups. Prior to performing PSM, preoperative characteristics that showed significant differences between the groups in the unmatched cohort (p < 0.05), as determined by chi-square tests, were identified and incorporated into a binary logistic regression model to calculate the propensity scores. Patients were matched 1:1 using the nearest-neighbor method with a caliper width of 0.2 standard deviations of the logit of the propensity score. The balance in propensity score distributions between groups, before and after matching, was assessed using scatter plots and histograms.
Cox proportional hazards regression analysis was conducted to evaluate associations between preoperative characteristics and the occurrence of emergency cesarean delivery, with labor duration as the timescale and emergency cesarean delivery as the censored event. Variables with a p-value <0.15 in univariate analysis were included in multivariate Cox regression models to identify independent risk factors. Results were presented as hazard ratios (HR) with 95% confidence intervals (CI). The cumulative risk of emergency cesarean delivery, stratified by identified risk factors, was estimated using Kaplan–Meier survival curves and compared using log-rank tests.
All statistical tests, including the Mann–Whitney U-test, chi-square test, and univariate and multivariate Cox proportional hazards regression analyses, were performed using IBM SPSS Statistics software (version 26.0). Propensity score matching and Kaplan–Meier survival analyses were performed using R software (version 4.1.2).
2.5 Ethics
All procedures carried out in studies involving human participants adhered to the ethical standards set by the institutional and national research committee, in accordance with the 1964 Helsinki Declaration and its subsequent amendments. The study received review and approval from the Ethical Committee of Qilu Hospital of Shandong University (protocol number KYLL-202309-028), with a waiver for informed consent.
3 Results
3.1 Preoperative characteristics before and after PSM
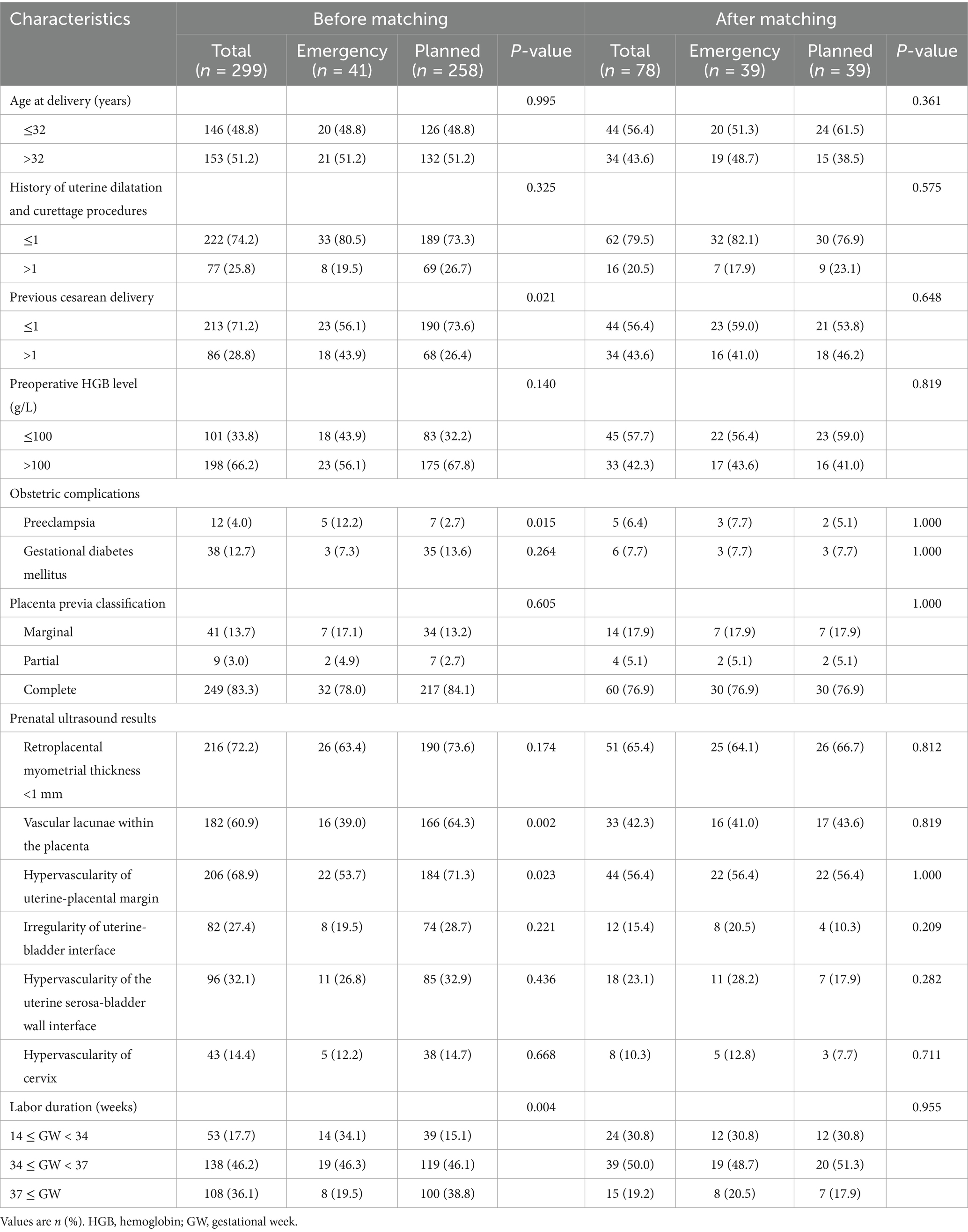
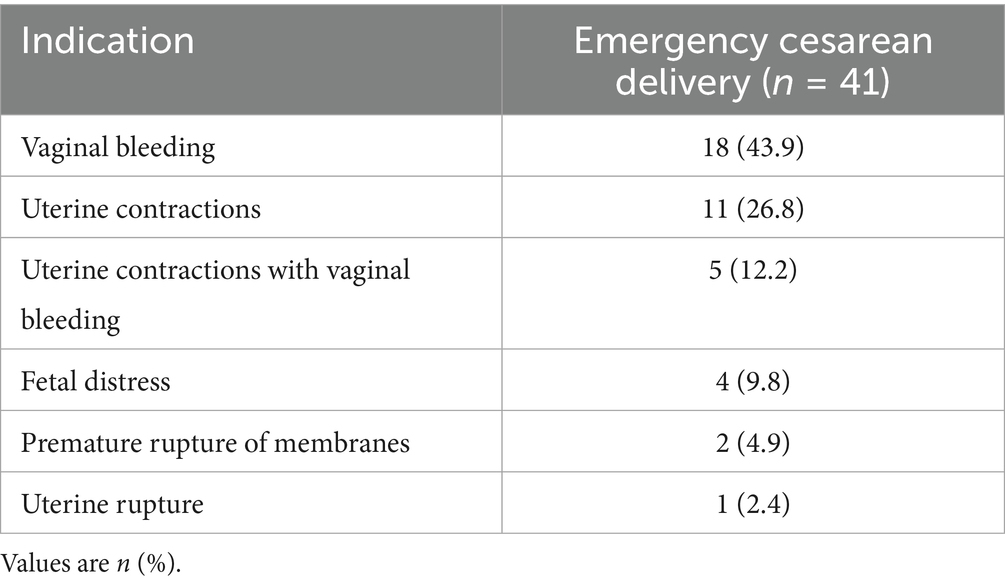
Figure 1 provides an overview of the research procedure. A total of 299 women with placenta previa were included in this study, among whom 275 (92.0%) were diagnosed with placenta increta and 24 (8.0%) with placenta percreta. Table 1 summarizes the preoperative characteristics of the study population. Of these, 41 patients were categorized into the emergency cesarean delivery group, while 258 patients were assigned to the planned cesarean delivery group. Table 2 outlines the indications for emergency cesarean delivery. The most common indications were vaginal bleeding (n = 18, 43.9%) and uterine contractions (n = 11, 26.8%).
In the unmatched cohort, women in the emergency cesarean delivery group were significantly more likely to have had a history of more than one prior cesarean delivery (43.9% vs. 26.4%, p = 0.021) and to have been diagnosed with preeclampsia (12.2% vs. 2.7%, p = 0.015) compared to the planned cesarean delivery group. Additionally, significant differences were observed in the presence of vascular lacunae within the placenta (p = 0.002), hypervascularity of the uterine-placental margin (p = 0.023), and labor duration (p = 0.004). To reduce potential bias between the two groups, propensity scores were calculated based on these preoperative characteristics.
After PSM, 39 patients were included in each group. Post-matching analysis revealed no significant differences in preoperative characteristics between the emergency and planned cesarean delivery groups. Figure 2 illustrates the distribution of propensity scores before and after PSM, demonstrating that the scores were more evenly and uniformly distributed following matching.
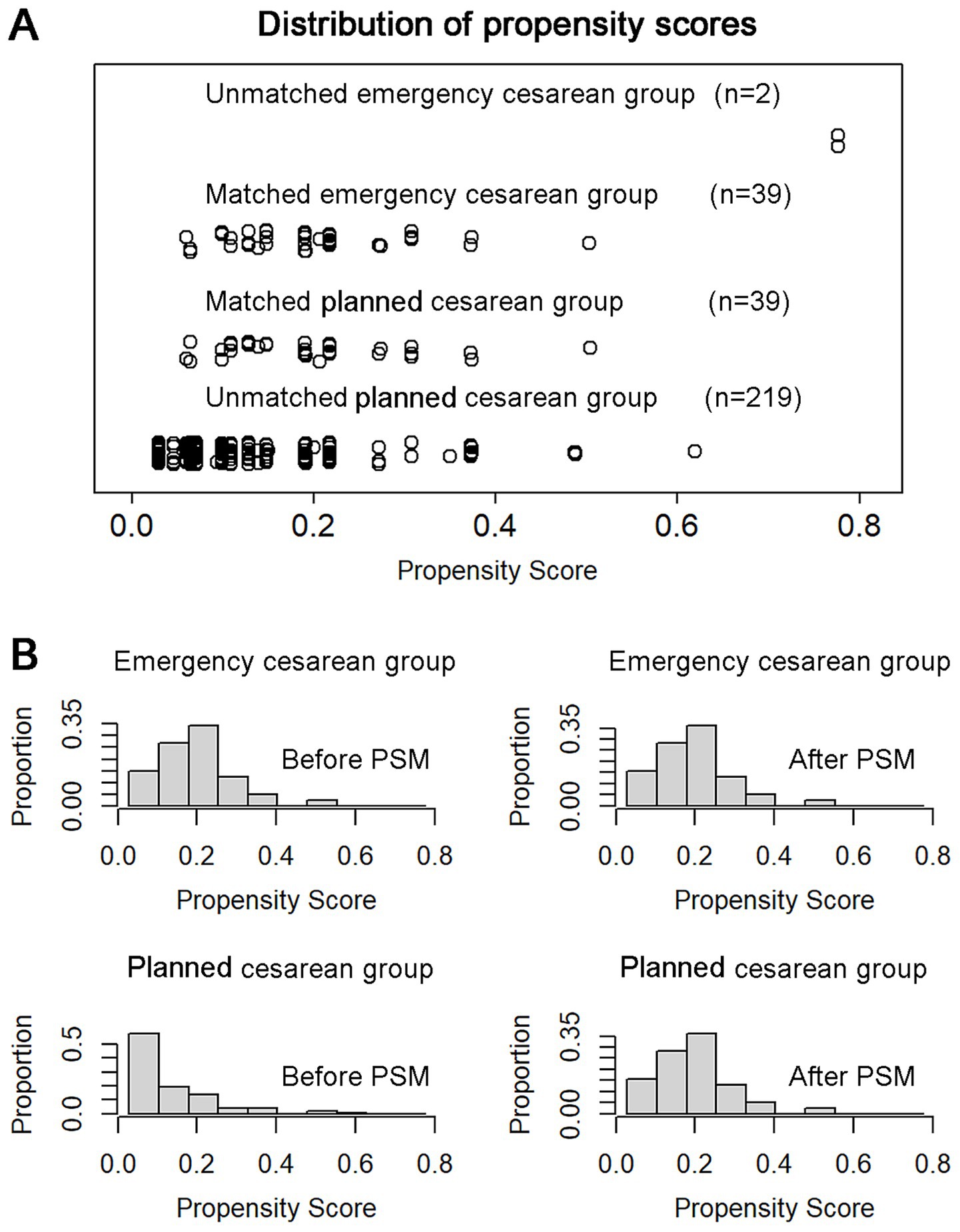
Figure 2. The distribution of propensity score before and after PSM analysis. (A) Thirty-nine patients in the emergency cesarean section group and 39 patients in the non-emergency group were successfully matched. (B) Histograms show the propensity scores of two groups are evenly more uniform distributed after matching. PSM, propensity score matching.
3.2 Intergroup comparison of perinatal outcomes before and after PSM
A summary of perinatal outcomes is presented in Table 3. Before PSM, patients in the emergency cesarean delivery group received significantly more units of PRBC transfusions (median: 6 units vs. 4 units, p = 0.032), underwent B-Lynch suture more frequently (43.9% vs. 26.4%, p = 0.021), and were more likely to have ligation of the ascending branch of the uterine artery (29.3% vs. 14.0%, p = 0.013) or hysterectomy (9.8% vs. 1.6%, p = 0.014) compared to the planned cesarean delivery group. All hysterectomies were unplanned and performed as emergency procedures due to uncontrollable intraoperative hemorrhage. Additionally, the emergency group had lower fetal birth weights (median: 2,470 g vs. 2,900 g, p < 0.001) and a higher rate of neonatal intensive care unit (NICU) admissions (63.4% vs. 38.4%, p = 0.003).
After PSM, similar trends were observed. Patients in the emergency group required more units of PRBC transfusions (median: 6 units vs. 4 units, p = 0.034) and were significantly more likely to undergo ligation of the ascending branch of the uterine artery (30.8% vs. 0.0%, p < 0.001). Consistent with the findings before matching, the emergency group also had lower fetal birth weights (median: 2500 g vs. 2,900 g, p = 0.044) and a higher rate of NICU admissions (64.1% vs. 41.0%, p = 0.041) compared to the planned group.
3.3 High-risk factors associated with emergency cesarean delivery
The results of univariate and multivariate Cox proportional hazards regression analyses for risk factors associated with emergency cesarean delivery are summarized in Table 4. Multivariate analysis identified a history of more than one previous cesarean delivery (HR: 2.34, 95% CI: 1.24–4.42, p = 0.009), preoperative HGB level ≤100 g/L (HR: 2.28, 95% CI: 1.19–4.40, p = 0.013), and preeclampsia (HR: 2.93, 95% CI: 1.10–7.82, p = 0.032) as independent risk factors for emergency cesarean delivery. Conversely, the presence of vascular lacunae within the placenta was identified as a protective factor (HR: 0.40, 95% CI: 0.21–0.76, p = 0.005). Figure 3 illustrates the Kaplan–Meier cumulative risk curves, which demonstrate the cumulative likelihood of emergency cesarean delivery stratified by these high-risk factors.
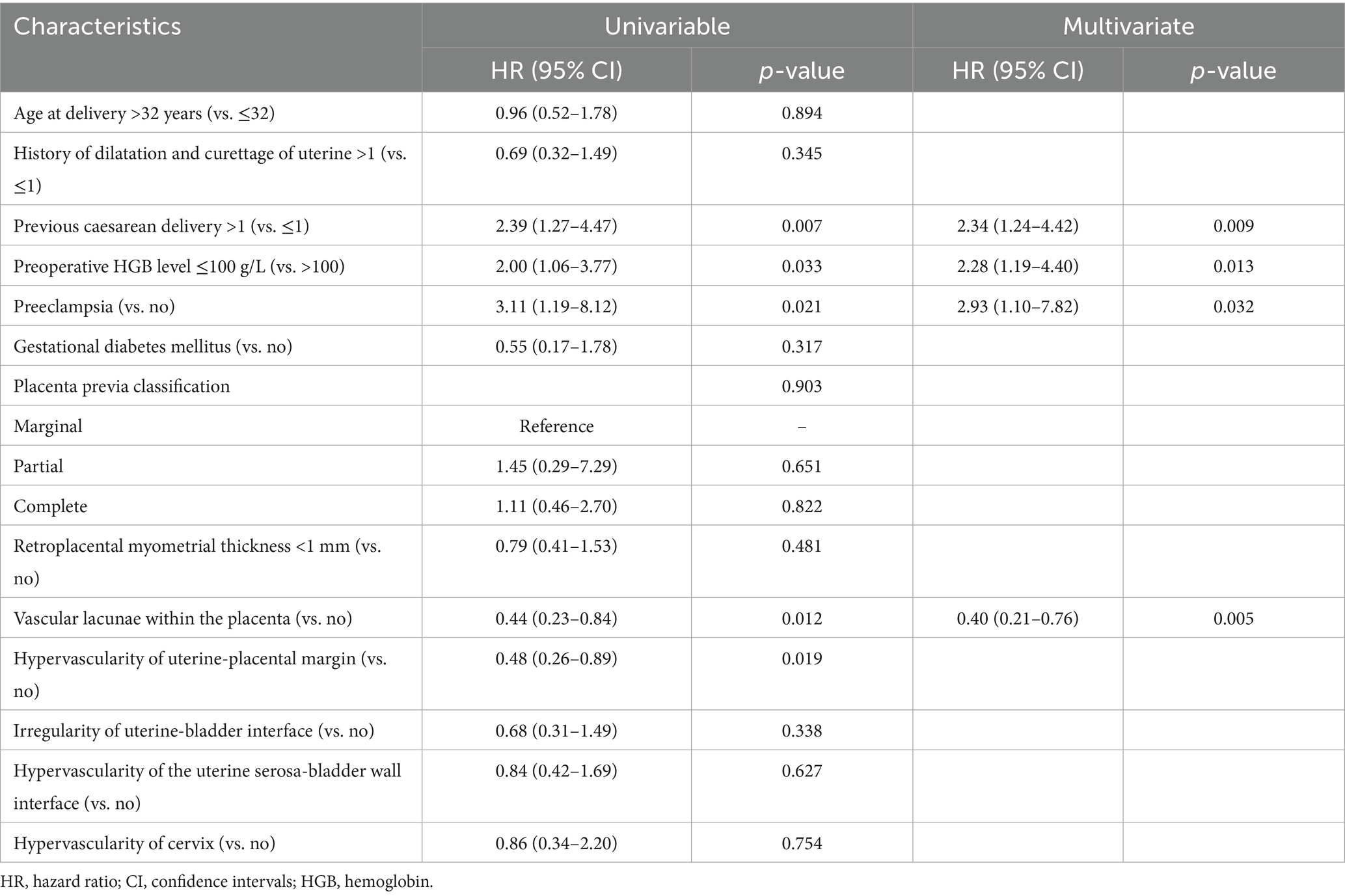
Table 4. Univariable and multivariate Cox proportional hazards regression analysis for the premature emergency cesarean section before delivery.
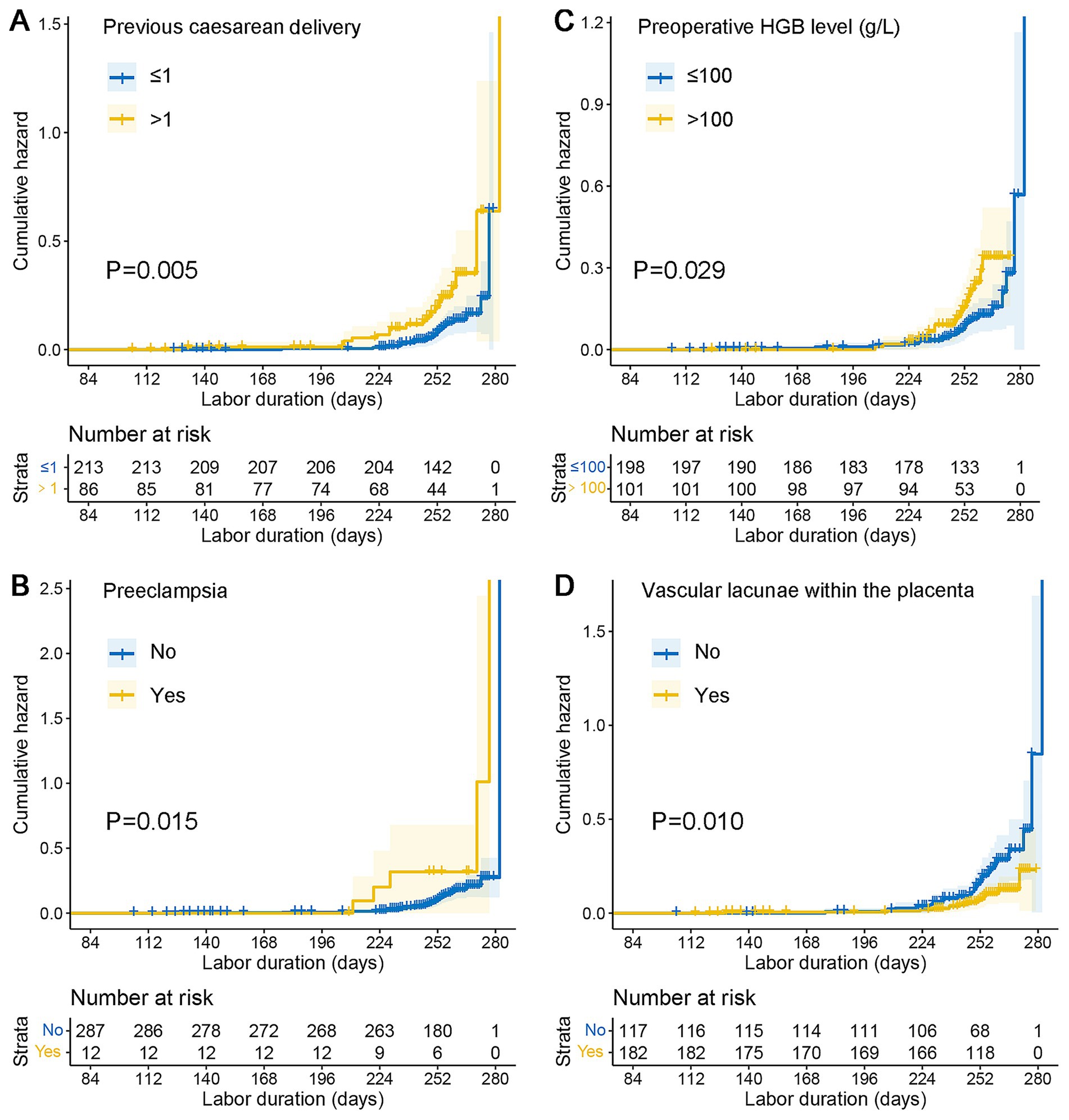
Figure 3. Kaplan–Meier cumulative risk curves emergency cesarean delivery. (A) Kaplan–Meier analysis curve of previous cesarean delivery. (B) Kaplan–Meier analysis curve of preeclampsia. (C) Kaplan–Meier analysis curve of preoperative HGB level. (D) Kaplan–Meier analysis curve of vascular lacunae within the placenta. HGB, hemoglobin.
4 Discussion
This study highlights the significant perinatal risks associated with emergency cesarean delivery in patients with PAS and placenta previa. Emergency cesarean delivery was found to increase blood transfusion requirements, the need for additional surgical interventions, lower neonatal birth weights, and higher rates of NICU admissions. Multivariate Cox proportional hazards analysis identified multiple previous cesarean deliveries, preoperative hemoglobin levels ≤100 g/L, preeclampsia, and placental vascular lacunae as independent risk factors for emergency cesarean delivery. These findings emphasize the importance of early diagnosis and risk stratification. Enhanced prenatal surveillance, especially in patients identified as high-risk via ultrasound or MRI, is essential. Optimizing delivery planning at specialized medical centers with multidisciplinary teams experienced in PAS management can reduce the likelihood of emergency interventions and improve maternal and neonatal outcomes.
Early prenatal diagnosis of PAS remains critical for facilitating planned deliveries at specialized medical centers with experienced multidisciplinary teams, which can significantly reduce maternal morbidity (10). The primary goal in PAS management is to achieve a planned delivery, thereby minimizing the likelihood of emergency cesarean delivery and its associated complications (11). Our obstetrics department functions as a specialized medical center with a highly experienced multidisciplinary team in the diagnosis and treatment of PAS. Despite this, 13.7% (n = 41) of PAS patients in our study required emergency cesarean delivery due to complications such as vaginal bleeding, uterine contractions, fetal distress, premature rupture of membranes, or uterine rupture. Compared to planned cesarean deliveries, emergency procedures were associated with increased risks of severe hemorrhage, anesthetic complications, and inadvertent injuries to abdominopelvic organs (12). According to the American College of Obstetricians and Gynecologists, the standard time from the decision to perform an emergency cesarean delivery to the delivery of the infant should not exceed 30 min (13). This narrow time frame necessitates the implementation of specialized emergency measures, such as advanced preparation for massive transfusions, to reduce adverse maternal and neonatal outcomes and patient mortality. Early identification of PAS patients at high risk for emergency cesarean delivery is therefore crucial for improving clinical management and reducing the occurrence of adverse events.
Intraoperative and postoperative hemostatic strategies play a critical role in managing severe hemorrhage associated with PAS, especially during emergency cesarean delivery. In addition to standard surgical and interventional techniques, the use of pharmacological agents such as recombinant activated factor VII (rFVIIa) has been reported as an effective adjunct in controlling intractable postpartum bleeding. Recent evidence suggests that rFVIIa can significantly reduce blood loss and improve maternal outcomes in cases of massive obstetric hemorrhage, without substantially increasing thromboembolic risk (14). Incorporating such targeted hemostatic therapies into comprehensive surgical protocols may enhance bleeding control and reduce the need for hysterectomy or other radical procedures.
In our study, a comparison of the pre- and post-matching cohorts revealed that emergency cesarean delivery resulted in significantly higher PRBC transfusion requirements, consistent with findings from previous studies (15). Patients in the emergency group also required additional surgical interventions, such as ligation of the ascending branch of the uterine artery. Similarly, a retrospective study by Pires-Menard et al. (16) found that emergency cesarean delivery was associated with worse neonatal outcomes, with low birth weight being an independent risk factor for poor neonatal condition at birth. In our analysis, neonates in the emergency group had lower birth weights and higher NICU admission rates, even though the gestational age at delivery did not differ significantly between the groups. These findings reaffirm the adverse impact of emergency delivery on neonatal outcomes in PAS patients.
Our analysis of high-risk factors for emergency cesarean delivery differs from previous studies in two significant aspects. First, we deliberately excluded antepartum vaginal bleeding from the risk factor analysis, as it is a strong predictor of preterm delivery and adverse pregnancy outcomes in PAS patients (17, 18). This exclusion was intended to prevent the overshadowing of other potential risk factors, a methodological departure from prior studies (19). Second, instead of using logistic regression to analyze binary outcomes, we employed Cox proportional hazards regression analysis. This approach allowed us to evaluate the timing and severity of emergency deliveries, providing a more nuanced understanding of their association with various factors.
Consistent with previous research, our study confirmed that a history of more than one previous cesarean delivery significantly increases the risk of emergency cesarean delivery in PAS patients (19, 20). Preeclampsia also emerged as a significant risk factor, reflecting its well-documented association with adverse maternal and neonatal outcomes (21). Furthermore, our findings indicate that preoperative HGB levels ≤100 g/L are associated with heightened risks of emergency delivery and adverse outcomes. This observation aligns with our previous research, which linked low HGB levels to an increased likelihood of excessive bleeding during cesarean delivery. Additionally, vascular lacunae within the placenta were identified as a protective factor, potentially signaling early recognition of severe PAS and prompting timely delivery planning (8). In our analysis, the presence of placental vascular lacunae on prenatal ultrasound was associated with a lower risk of emergency cesarean section in patients with PAS. Although this result initially seemed counterintuitive—since vascular lacunae are often linked to more severe disease—it is likely related to differences in clinical management. In practice, identifying vascular lacunae tends to prompt closer monitoring and earlier planned cesarean delivery, which may reduce the likelihood of emergency interventions. Conversely, patients without vascular lacunae might be managed more conservatively, making them more susceptible to unexpected complications requiring emergency surgery. This finding underscores how clinical decision-making can influence outcomes and highlights the importance of management strategies in interpreting retrospective data. However, we acknowledge the possibility of residual confounding and detection bias. Further studies with larger sample sizes and more detailed clinical data are needed to clarify this association.
A major strength of our study lies in the use of Cox proportional hazards regression analysis to identify high-risk factors for emergency cesarean delivery in PAS patients. However, the study’s retrospective design inherently limits the availability of certain prenatal medical data. Moreover, our definition of emergency cesarean delivery encompassed various clinical scenarios, including fetal distress, premature rupture of membranes, vaginal bleeding, uterine contractions, and uterine rupture. The incidence of emergency cesarean delivery in our study (13.7%) was lower than that reported in previous studies, which may reflect differences in study populations or healthcare settings.
5 Conclusion
Emergency cesarean delivery in PAS patients significantly increases maternal and neonatal risks, including higher transfusion requirements, additional surgical interventions, and adverse neonatal outcomes. Independent risk factors such as multiple previous cesarean deliveries, preoperative hemoglobin ≤100 g/L, preeclampsia, and placental vascular lacunae highlight the need for early risk stratification and planned delivery at specialized centers to optimize outcomes in this high-risk population.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethical Committee of Qilu Hospital of Shandong University (protocol number KYLL-202209-028), with a waiver for informed consent. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because our study was a retrospective clinical study.
Author contributions
ML: Conceptualization, Data curation, Formal analysis, Software, Writing – original draft, Writing – review & editing. XS: Data curation, Methodology, Validation, Writing – review & editing. LL: Data curation, Methodology, Supervision, Writing – review & editing. FM: Data curation, Investigation, Methodology, Writing – review & editing. RC: Conceptualization, Funding acquisition, Methodology, Writing – original draft, Writing – review & editing. HZ: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by grants from China Postdoctoral Science Foundation (2024 M761863) and Shandong Province Postdoctoral Innovation Project (SDCX-ZG-202400057).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Jauniaux, E, Ayres-de-Campos, D, Langhoff-Roos, J, Fox, KA, and Collins, SFIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel. FIGO classification for the clinical diagnosis of placenta accreta spectrum disorders. Int J Gynaecol Obstet. (2019) 146:20–4. doi: 10.1002/ijgo.12761
2. Shainker, SA, Coleman, B, Timor-Tritsch, IE, Bhide, A, Bromley, B, Cahill, AG, et al. Special report of the Society for Maternal-Fetal Medicine Placenta Accreta Spectrum Ultrasound Marker Task Force: consensus on definition of markers and approach to the ultrasound examination in pregnancies at risk for placenta accreta spectrum. Am J Obstet Gynecol. (2021) 224:B2–B14. doi: 10.1016/j.ajog.2020.09.001
3. Silver, RM, and Branch, DW. Placenta Accreta Spectrum. N Engl J Med. (2018) 378:1529–36. doi: 10.1056/NEJMcp1709324
4. Cahill, AG, Beigi, R, Heine, RP, Silver, RM, and Wax, JR. Society of Gynecologic Oncology, American College of Obstetricians and Gynecologists and the Society for Maternal–Fetal Medicine. Placenta Accreta Spectrum. Am J Obstet Gynecol. (2018) 219:B2–B16. doi: 10.1016/j.ajog.2018.09.042
5. Jauniaux, E, Alfirevic, Z, Bhide, AG, Belfort, MA, Burton, GJ, Collins, SL, et al. Placenta Praevia and placenta Accreta: diagnosis and management: green-top guideline no. 27a. BJOG. (2019) 126:e1–e48. doi: 10.1111/1471-0528.15306
6. Allen, L, Jauniaux, E, Hobson, S, Papillon-Smith, J, and Belfort, MAfor the FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel. FIGO consensus guidelines on placenta accreta spectrum disorders: nonconservative surgical management. Int J Gynaecol Obstet. (2018) 140:281–90. doi: 10.1002/ijgo.12409
7. Lu, R, Chu, R, Wang, Q, Xu, Y, Zhao, Y, Tao, G, et al. Role of abdominal aortic balloon placement in planned conservative Management of Placenta Previa with Placenta Increta or Percreta. Front Med. (2021) 8:767748. doi: 10.3389/fmed.2021.767748
8. Lu, R, Chu, R, Gao, N, Li, G, Tang, H, Zhou, X, et al. Development and validation of nomograms for predicting blood loss in placenta previa with placenta increta or percreta. Ann Transl Med. (2021) 9:287. doi: 10.21037/atm-20-5160
9. Shamshirsaz, AA, Fox, KA, Erfani, H, Clark, SL, Shamshirsaz, AA, Nassr, AA, et al. Outcomes of planned compared with urgent deliveries using a multidisciplinary team approach for morbidly adherent placenta. Obstet Gynecol. (2018) 131:234–41. doi: 10.1097/AOG.0000000000002442
10. Fitzpatrick, KE, Sellers, S, Spark, P, Kurinczuk, JJ, Brocklehurst, P, and Knight, M. The management and outcomes of placenta accreta, increta, and percreta in the UK: a population-based descriptive study. BJOG. (2014) 121:62–70. doi: 10.1111/1471-0528.12405
11. Eller, AG, Porter, TF, Soisson, P, and Silver, RM. Optimal management strategies for placenta accreta. BJOG. (2009) 116:648–54. doi: 10.1111/j.1471-0528.2008.02037.x
12. Tyner, JE, and Rayburn, WF. Emergency cesarean delivery: special precautions. Obstet Gynecol Clin N Am. (2013) 40:37–45. doi: 10.1016/j.ogc.2012.11.003
13. American College of Obstetricians and Gynecologists Committee on Obstetric Practice. ACOG Committee Opinion #303: Inappropriate use of the terms fetal distress and birth asphyxia. Obstet Gynecol. (2004) 104:903. doi: 10.1097/00006250-200410000-00050
14. Caram-Deelder, C, McKinnon Edwards, H, Zdanowicz, JA, et al. Efficacy and safety analyses of recombinant factor VIIa in severe post-partum hemorrhage. J Clin Med. (2024) 13:2656. doi: 10.3390/jcm13092656
15. Durukan, H, Durukan, ÖB, and Yazıcı, FG. Planned versus urgent deliveries in placenta previa: maternal, surgical and neonatal results. Arch Gynecol Obstet. (2019) 300:1541–9. doi: 10.1007/s00404-019-05349-9
16. Pires-Menard, A, Flatley, C, and Kumar, S. Severe neonatal outcomes associated with emergency cesarean section at term. J Matern Fetal Neonatal Med. (2021) 34:629–33. doi: 10.1080/14767058.2019.1611770
17. Fishman, SG, Chasen, ST, and Maheshwari, B. Risk factors for preterm delivery with placenta previa. J Perinat Med. (2011) 40:39–42. doi: 10.1515/JPM.2011.125
18. Jauniaux, E, and Bhide, A. Prenatal ultrasound diagnosis and outcome of placenta previa accreta after cesarean delivery: a systematic review and meta-analysis. Am J Obstet Gynecol. (2017) 217:27–36. doi: 10.1016/j.ajog.2017.02.050
19. Ruiter, L, Eschbach, SJ, Burgers, M, Rengerink, KO, van Pampus, M, Goes, BY, et al. Predictors for emergency cesarean delivery in women with placenta Previa. Am J Perinatol. (2016) 33:1407–14. doi: 10.1055/s-0036-1584148
20. Haile, ZT, Chavan, B, Teweldeberhan, AK, Chertok, IRA, and Francescon, J. Gestational weight gain and unplanned or emergency cesarean delivery in the United States. Women Birth. (2019) 32:263–9. doi: 10.1016/j.wombi.2018.07.011
Keywords: emergency cesarean, placenta accreta spectrum, placenta increta, placenta percreta, propensity score matching, perinatal outcomes, risk factor
Citation: Li M, Zhang H, Song X, Li L, Meng F and Chu R (2025) Risk factors for emergency cesarean delivery in patients with placenta accreta spectrum: a multicenter retrospective cohort study. Front. Med. 12:1539998. doi: 10.3389/fmed.2025.1539998
Edited by:
Federica Piani, Medical University of Graz, AustriaReviewed by:
Abraham A Pouliakis, National and Kapodistrian University of Athens, GreeceYongdan Ma, Peking University, China
Copyright © 2025 Li, Zhang, Song, Li, Meng and Chu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ran Chu, Y2h1cmFuMjMyM0AxNjMuY29t
†These authors have contributed equally to this work
 Min Li1,2†
Min Li1,2† Liang Li
Liang Li Fanqing Meng
Fanqing Meng Ran Chu
Ran Chu