- 1Department of Nuclear Medicine, Brest University Hospital, Brest, France
- 2Department of Pneumology, Brest University Hospital, Brest, France
- 3GETBO, INSERM, UMR1304, Université de Bretagne Occidentale, Brest, France
- 4Department of Pneumology, Limoges University Hospital, Limoges, France
- 5Department of Pneumology, Toulouse University Hospital, Toulouse, France
Endoscopic endobronchial valve lung volume reduction in the management of severe emphysema reduces volume inflation in the most severely affected areas, with the hope of clinical improvement. We report the case of a patient who presented with late progressive respiratory deterioration following endoscopic endobronchial valve lung volume reduction. Ventilation/perfusion (V/Q)-SPECT/CT showed unexpectedly high perfusion in the atelectasis of the treated lobes, reflecting a paradoxical intrapulmonary shunt. This paradoxical complication of endobronchial valve treatment for severe emphysema is rare and highlights the potential usefulness of performing V/Q-SPECT/CT imaging in patients presenting with respiratory deterioration following endoscopic lung volume reduction.
Introduction
Endoscopic lung volume reduction (ELVR) in the treatment of severe emphysema reduces pulmonary inflation in the most affected areas (target lobes), aiming to achieve clinical improvement (1). This method provides a less invasive alternative to lung volume reduction surgery, developed by Cooper et al. (2, 3). Studies have shown that lung volume reduction via endobronchial valves in carefully selected patients, with low collateral ventilation, leads to functional benefits, such as improvements in forced expiratory volume in 1 s (FEV1), 6-min walk test (6MWT) performance, and a reduction in residual volume (RV), in addition to improvements in quality of life (4–7). Although early complications have been documented, little information is available regarding late paradoxical phenomena (8–10). This report presents a case where a paradoxical intrapulmonary shunt was detected several months after treatment.
Case description
A 63-year-old man with severe emphysema underwent endoscopic lung volume reduction (ELVR) following functional assessment (Table 1—FEV1 at 34% of the predicted value, RV at 180% of the predicted value, 6MWT: 265 m) and arterial blood gas analysis (pH 7.44, pO2 86 mmHg, bicarbonate 30 mmol/L, pCO2 44 mmHg on 2 L of oxygen). Emphysema was diffuse, primarily localized in the apices of the lungs. The percentage of voxels with a density < −950 HU on a dedicated CT scan in the treated lobes (middle and right upper lobes) was 37% for the middle lobe (ML) and 45% for the right superior lobe (RSL). For the other lobes, the percentages were as follows: 32% for the right inferior lobe (RIL), 39% for the left superior lobe (LSL), and 35% for the left inferior lobe (LIL). The patient underwent a two-stage lung volume reduction using Zephyr® endobronchial valves (Figure 1B—dashed white arrow). In the first stage, valves were placed in the B1, B2, B3, and B5 segments of the right upper and middle lobes. A second intervention, 6 weeks later, involved placing a valve in the B4 segment.
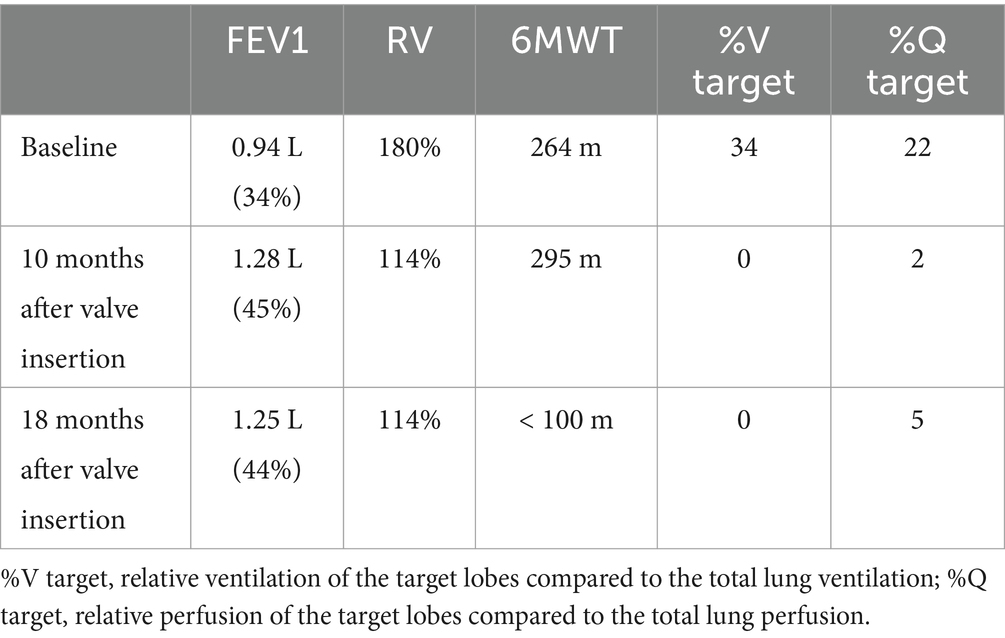
Table 1. Functional assessments of the patient and scintigraphic quantification of ventilation and perfusion before and after treatment.
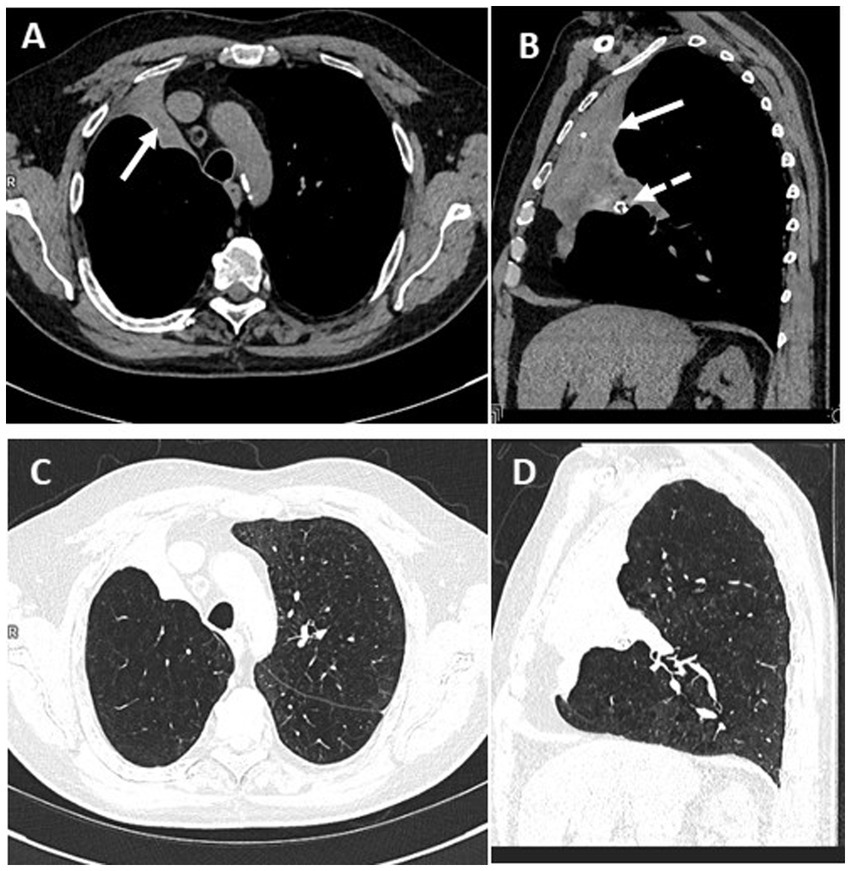
Figure 1. Axial and sagittal CT slices passing through the atelectasis, in mediastinal (A,B) and pulmonary (C,D) windows. The white arrow shows the atelectasis; the white dashed arrow shows a Zephyr endobronchial valve.
At 10 months, a CT scan revealed complete atelectasis of the treated lobes (Figures 1A,B, white arrows). A ventilation/perfusion scintigraphy (V/Q-SPECT/CT) conducted at that time showed no significant abnormalities in the atelectatic areas (low perfusion uptake of macroaggregated albumin (MAA) retrospectively—Figures 2C,D without associated ventilation—Figures 2A,B). The patient’s evaluation (Table 1) showed clinical improvement with a reduction in dyspnea and an improvement in FEV1 (45%) and RV (114%).
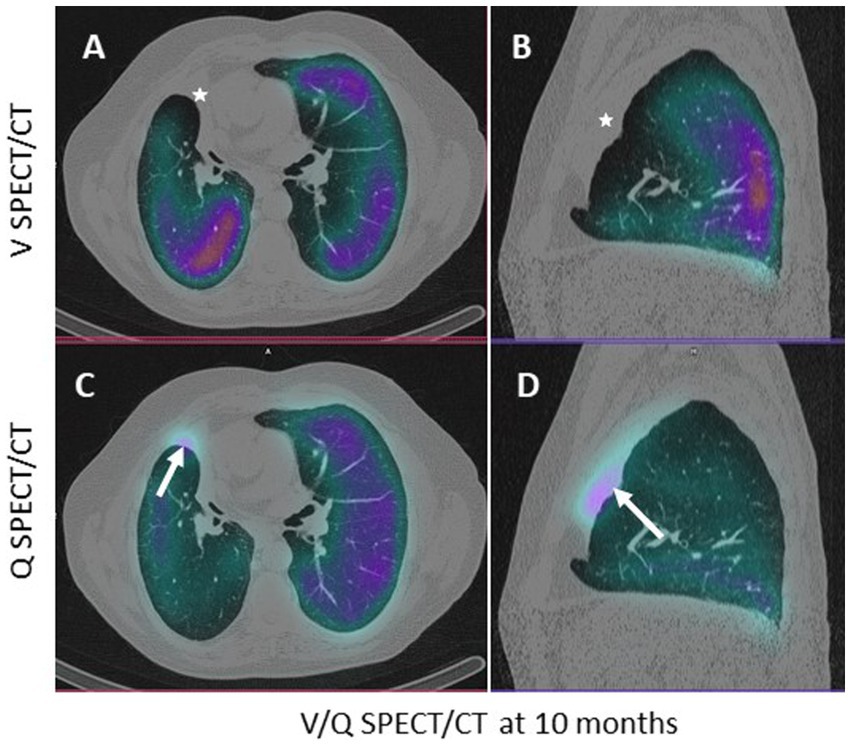
Figure 2. Axial (A–C) and sagittal (B–D) CT slices passing through the atelectasis, in pulmonary window. The white arrow shows the low (non-significant) uptake of macroaggregated albumin in the perfused atelectasis (C,D); the white star shows the absence of ventilation (A,B).
However, at 18 months, a new V/Q-SPECT/CT, performed due to worsening respiratory status (dyspnea, cyanosis, and a reduction in the 6MWT to less than 100 m—Table 1), revealed abnormal and very high uptake of macroaggregates of albumin (MAA) (Figures 3C,D in the atelectatic, non-ventilated lobes—Figures 3A,B). Arterial blood gas at 24 months showed: pH 7.46, pO2 66 mmHg, pCO2 33 mmHg on 3 L of oxygen.
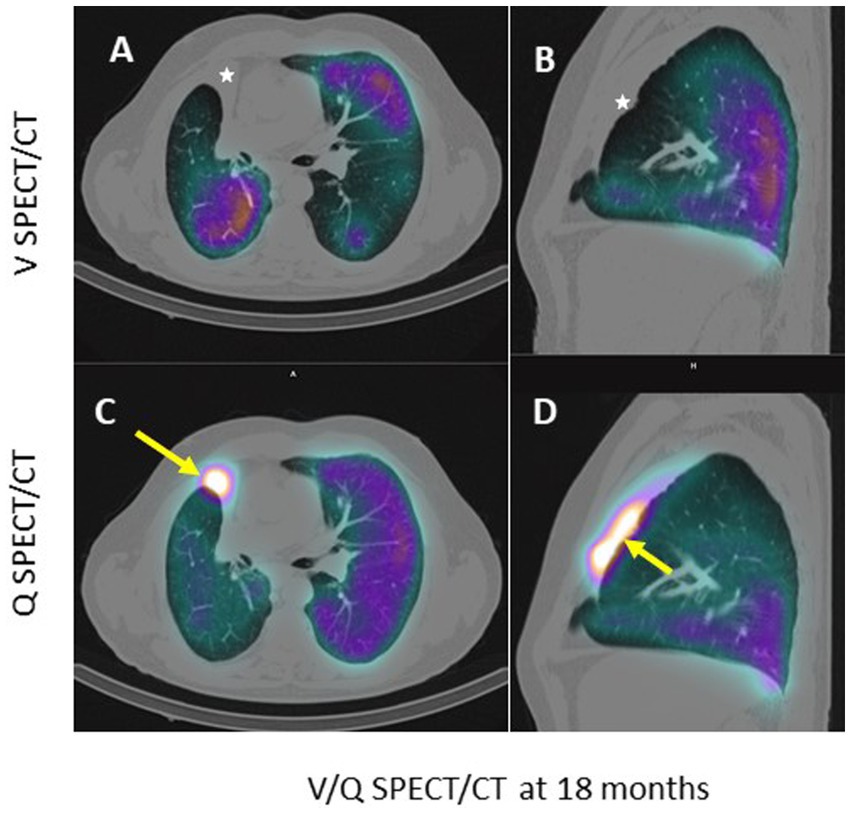
Figure 3. Axial (A–C) and sagittal (B–D) CT slices passing through the atelectasis, in pulmonary window. The white arrow shows the very high uptake of macroaggregated albumin in the perfused atelectasis (C,D); the white star shows the absence of ventilation (A,B).
Relative lung ventilation and perfusion in the target lobes at M0, M10, and M18 are presented in Table 1. In the pre-therapeutic SPECT/CT evaluation, the target lobes (right middle and upper lobes) represented 30% of the total lung volume, 34% of the total ventilation, and 22% of the total perfusion, with 43% of the right lung perfusion. At M10 and M18, the relative lung perfusion in the target lobe increased from 2 to 5% (7 and 14% of the right lung perfusion) while the relative lung ventilation was 0%.
Discussion
The unidirectional endobronchial valve directs airflow from the alveoli to the outside of the lung, causing volume reduction and atelectasis of the target lobes (1), thereby limiting pulmonary hyperinflation (1). Atelectasis of the target lobes causes hypoxemic vasoconstriction (suppression of perfusion) and vascular redistribution to the rest of the lung (11, 12). The patient was not on medications that would inhibit vasoconstriction, which could maintain perfusion to the atelectatic area (13). The significant uptake of MAA in this atelectasis, which is unusual in pulmonary scintigraphy, was particularly notable, indicating preferential pulmonary blood flow to this non-ventilated territory, consistent with an intrapulmonary shunt. The arterial blood gas at 24 months also showed a shunt effect, with a decrease in PaCO2 and PaO2 (partially corrected by increasing the O2 from 2 to 3 L/min to maintain a PaO2 of 66 mmHg, compared to 86 mmHg initially), resulting in PaO2 + PaCO2 < 120 mmHg. This late paradoxical phenomenon had not previously been described as a potential complication of the technique (13, 14). Ventilation/perfusion scintigraphy (V/Q-SPECT/CT), while useful for functional lung quantification and selection of target lobes prior to lung volume reduction (15, 16), is not widely performed during follow-up, which could explain the lack of awareness of this phenomenon. Due to the worsening of the respiratory status and no clear etiology despite cardiac evaluations (echocardiogram, electrocardiogram, and myocardial perfusion scintigraphy), the endobronchial valves were eventually removed at 24 months, but there was no improvement in respiratory function. Unfortunately, we did not perform late imaging after the valve removal, which would have provided a better understanding of the evolution of the V/Q mismatch and the re-expansion of the target lobes.
Conclusion
This case illustrates an intrapulmonary shunt, a rare and paradoxical complication of endobronchial valve treatment for severe emphysema, and highlights the potential usefulness of performing V/Q-SPECT/CT in patients presenting with respiratory deterioration following endoscopic lung volume reduction.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval was not required for this case report as it is based solely on anonymized clinical data, and informed consent was obtained from the patient. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
JD: Conceptualization, Writing – original draft, Writing – review & editing. CG: Writing – original draft, Writing – review & editing. TE: Writing – original draft, Writing – review & editing. NG: Writing – original draft, Writing – review & editing. P-YR: Conceptualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Mal, H, Bunel, V, Marceau, A, Dombret, MC, Debray, MP, and Crestani, B. Endoscopic lung volume reduction for emphysema. Rev Mal Respir. (2019) 36:880–8. doi: 10.1016/j.rmr.2019.05.039
2. Ingenito, EP, Wood, DE, and Utz, JP. Bronchoscopic lung volume reduction in severe emphysema. Proc Am Thorac Soc. (2008) 5:454–60. doi: 10.1513/pats.200707-085ET
3. Cooper, JD, Trulock, EP, Triantafillou, AN, Patterson, GA, Pohl, MS, Deloney, PA, et al. Bilateral pneumectomy (volume reduction) for chronic obstructive pulmonary disease. J Thorac Cardiovasc Surg. (1995) 109:106–19. doi: 10.1016/S0022-5223(95)70426-4
4. Klooster, K, ten Hacken, NH, Hartman, JE, Kerstjens, HA, van Rikxoort, EM, and Slebos, DJ. Endobronchial valves for emphysema without Interlobar collateral ventilation. N Engl J Med. (2015) 373:2325–35. doi: 10.1056/NEJMoa1507807
5. Valipour, A, Slebos, DJ, Herth, F, Darwiche, K, Wagner, M, Ficker, JH, et al. Endobronchial valve therapy in patients with homogeneous emphysema. Results from the IMPACT study. Am J Respir Crit Care Med. (2016) 194:1073–82. doi: 10.1164/rccm.201607-1383OC
6. Kemp, SV, Slebos, DJ, Kirk, A, Kornaszewska, M, Carron, K, Ek, L, et al. A multicenter randomized controlled trial of Zephyr endobronchial valve treatment in heterogeneous emphysema (TRANSFORM). Am J Respir Crit Care Med. (2017) 196:1535–43. doi: 10.1164/rccm.201707-1327OC
7. Criner, GJ, Sue, R, Wright, S, Dransfield, M, Rivas-Perez, H, Wiese, T, et al. A multicenter randomized controlled trial of Zephyr endobronchial valve treatment in heterogeneous emphysema (LIBERATE). Am J Respir Crit Care Med. (2018) 198:1151–64. doi: 10.1164/rccm.201803-0590OC
8. Chakravorty, S, and Mahajan, AK. Complications following bronchoscopic lung volume reduction (BLVR). AME Med J. (2023) 8:31. doi: 10.21037/amj-23-106
9. Franzen, D, Straub, G, and Freitag, L. Complications after bronchoscopic lung volume reduction. J Thorac Dis. (2018) 10:S2811–5. doi: 10.21037/jtd.2018.06.66
10. Fiorelli, A, D'Andrilli, A, Bezzi, M, Ibrahim, M, Anile, M, Diso, D, et al. Complications related to endoscopic lung volume reduction for emphysema with endobronchial valves: results of a multicenter study. J Thorac Dis. (2018) 10:S3315–25. doi: 10.21037/jtd.2018.06.69
11. Marshall, BE. Importance of hypoxic pulmonary vasoconstriction with atelectasis. Adv Shock Res. (1982) 8:1–12.
12. Ward, JP, and McMurtry, IF. Mechanisms of hypoxic pulmonary vasoconstriction and their roles in pulmonary hypertension: new findings for an old problem. Curr Opin Pharmacol. (2009) 9:287–96. doi: 10.1016/j.coph.2009.02.006
13. Gompelmann, D, Eberhardt, R, and Herth, F. Endoscopic volume reduction in COPD - a critical review. Dtsch Arztebl Int. (2014) 111:827–33. doi: 10.3238/arztebl.2014.0827
14. Gompelmann, D, Shah, PL, Valipour, A, and Herth, FJF. Bronchoscopic thermal vapor ablation: best practice recommendations from an expert panel on endoscopic lung volume reduction. Respiration. (2018) 95:392–400. doi: 10.1159/000489815
15. Tee, VST, Nguyen, P, Jersmann, H, Grosser, D, Crouch, B, Lorraine, B, et al. Use of ventilation-perfusion single-photon emission computed tomography to select the target lobe for endobronchial valve lung volume reduction. Respiration. (2021) 100:886–97. doi: 10.1159/000515336
16. Le Pennec, R, Schaefer, W, Tulchinsky, M, Lamoureux, F, Roach, P, Rischpler, C, et al. Performance and interpretation of lung scintigraphy: an evaluation of current practices in Australia, Canada, France, Germany, and United States. Clin Nucl Med. (2024) 49:997–1003. doi: 10.1097/RLU.0000000000005396
Keywords: endo-bronchial valves, endoscopic lung volume reduction (ELVR), emphysema, ventilation-perfusion SPECT–CT, lung scintigraphy, pulmonary shunt
Citation: Dzuko Kamga J, Gut Gobert C, Egenod T, Guibert N and Le Roux P-Y (2025) Case Report: Late paradoxical intrapulmonary shunt after endoscopic lung volume reduction with endobronchial valves for severe emphysema. Front. Med. 12:1572900. doi: 10.3389/fmed.2025.1572900
Edited by:
Mario Petretta, University of Naples Federico II, ItalyReviewed by:
Susanne Dittrich, Heidelberg University Hospital, GermanyJ. Win, Universitätsklinikum Essen, Germany
Copyright © 2025 Dzuko Kamga, Gut Gobert, Egenod, Guibert and Le Roux. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jacques Dzuko Kamga, amFjcXVlc2thbWdhMTBAZ21haWwuY29t
 Jacques Dzuko Kamga
Jacques Dzuko Kamga Christophe Gut Gobert2,3
Christophe Gut Gobert2,3 Thomas Egenod
Thomas Egenod Pierre-Yves Le Roux
Pierre-Yves Le Roux