- 1Queen Mary School, Nanchang University, Nanchang, China
- 2Department of Gastroenterology, First Affiliated Hospital of Nanchang University, Nanchang, China
Aim: To summarise the characteristics of esophageal tuberculosis, and to evaluate the role of endoscopic ultrasound-guided fine-needle biopsy (EUS-FNB) in the diagnosis of esophageal tuberculosis.
Methods: A retrospective analysis of esophageal tuberculosis patients diagnosed by the EUS-FNB between May 2012 and August 2023 was reported. Final diagnosis was based on histopathology, clinical context in combination with response to antitubercular therapy. Tissue acquisition of both esophageal lesions and enlarged mediastinal lymph nodes was performed by EUS-FNB. The variables evaluated were clinical features, location and diameter of the esophageal lesions and enlarged lymph nodes.
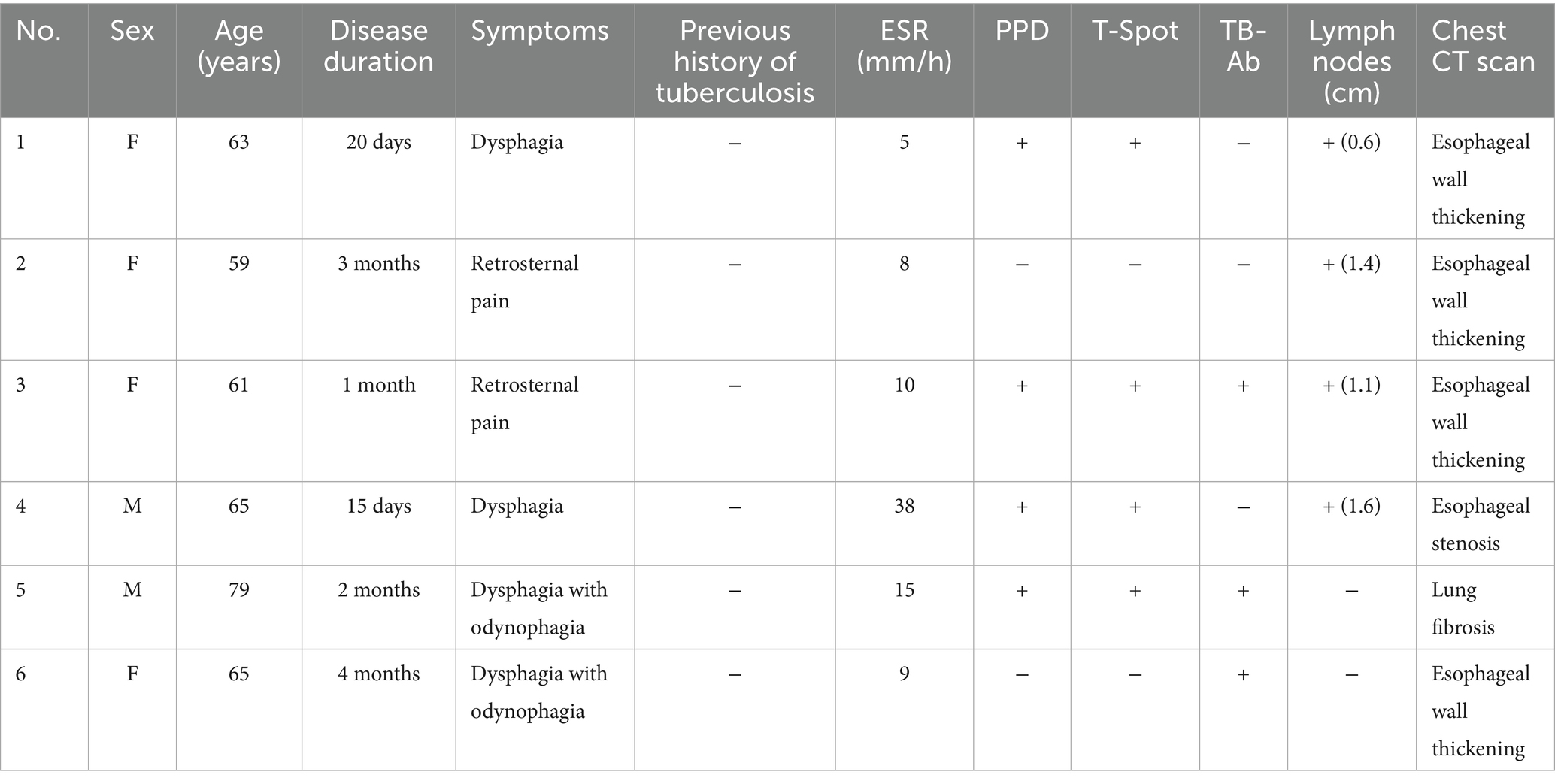
Results: Six esophageal tuberculosis patients without surgical management were finally identified by the performance of EUS-FNB. The most common clinical feature was progressive dysphagia. The site of lesions was most common located in the middle of esophagus (66.7%). Diameter of lesions range from 1.2 to 4.1 cm. Multiple enlarged mediastinal lymph nodes were of various sizes (range 0.6–1.6 cm in diameter). CT scan revealed focal thickened esophageal wall, esophageal stenosis, and a mass with moderate and heterogeneous enhancement in five patients (83.33%), which indicating esophageal carcinoma. Purified protein derivative (PPD) and T cell spot test (T-spot) were positive in four cases (66.7%), which were significant in the diagnosis. EUS-FNB provided the pathological diagnosis of tuberculosis in four cases.
Conclusion: Esophageal tuberculosis should be distinguished from advanced esophageal carcinoma and leiomyoma. Moreover, EUS-FNB is an excellent method in both image and tissue biopsy to establish an accurate diagnosis of esophageal tuberculosis.
Introduction
In the past few decades, there has been a concerted global effort to eradicate tuberculosis, but it still accounts for a major health problem in developing countries, and these countries experience the highest morbidity and mortality rates (1, 2). Tuberculosis infection can cause multiorgan involvement and it is most often seen in the lungs, and extrapulmonary tuberculosis accounts for approximately 20% of all cases (3, 4). Esophageal tuberculosis is a very rare clinical entity, although the digestive tract is the sixth most common affected site. In autopsy, esophageal involvement was seen in only 0.04–0.2% of all tubercular patients (5). Moreover, esophageal tuberculosis is similar to esophageal carcinoma both clinically and radiologically, so the lesions may be mistaken for malignancy (6). Therefore, diagnosing esophageal tuberculosis is challenge, and most cases are misdiagnosed before surgical exploration. Endoscopic ultrasound (EUS) guided fine-needle biopsy (FNB) is performed under realtime ultrasound guidance, and it can visualize and biopsy structures beneath esophageal mucosa and beyond the esophageal wall. The purpose of this study is to summarise the characteristics of esophageal tuberculosis, and to evaluate the role of EUS-FNB in the diagnosis of esophageal tuberculosis.
Materials and methods
This is a retrospective study of esophageal tuberculosis from May 2012 to August 2023 at a tertiary center in Wuhan, China. This study was reviewed and approved by the Ethics Committee of the Union Hospital, Tongji Medical College, Huazhong University of Science and Technology (No. 2024-0546). Since this study is a retrospective study, the informed consent form was waived. The records of all patients with a diagnosis of esophageal tuberculosis were reviewed. Patients were excluded from the study if they met the following criterions: suspected or newly diagnosed esophageal cancer; received surgical exploration. Confirmative pathological diagnosis of tuberculosis was defined by at least one of the three following criteria: caseous necrosis, positive for acid fast bacilli (AFB) on Ziehl–Neelsen stain or epithelioid granuloma with necrosis. Final diagnosis was based on histocytopatholog, clinical context in combination with response to antitubercular therapy.
Six patients were finally identified by the performance of EUS-FNB. Clinical data were analyzed, including symptoms, laboratory examinations, radiological imaging, endoscopic and endosonographic features, and histocytopathological features.
EUS was performed using a miniature ultrasonic probe (UM-2R 12 MHz, Olympus, Tokyo, Japan) with a ultrasound endoscope (Olympus, ME2, UCT260, Tokyo, Japan), and a 22-G needle (Echo-Tip Ultra, Wilson-Cook Medical Inc., Winston-Salem, USA) was used for puncture.
Results
Clinical features, laboratory and radiological findings
The average age of the six patients was 65.33 years (range 59–79 years), including four females (62.00 ± 6.58 years) and two males (72.00 ± 9.90 years). Four patients (66.67%) manifested as progressive dysphagia, with or without odynophagia. Two patients (33.33%) manifested as retrosternal pain. A past history of tuberculosis was found in none of the six patients. None showed signs of weight loss or fever. Four cases were positive in the tuberculosis test by both tuberculin skin test performed with purified protein derivative (PPD) and T cell spot test (T-spot). Tuberculosis antibody was positive in three cases. The results of laboratory examinations revealed that erythrocyte sedimentation rate (ESR) ranged from 5 to 38 mm/h. Blood routine examination, C-reactive protein (CRP) and liver function were all normal in six patients.
All patients underwent chest and esophagus computed tomography (CT) scan. CT scan revealed focal thickened esophageal wall, esophageal stenosis, and a mass with moderate and heterogeneous enhancement in five patients, which indicating esophageal carcinoma. Four patients with multiple mediastinal lymph nodes enlargement, and one patient with lung fibrosis. Participants’ characteristics are shown in Table 1.
Endoscopic features
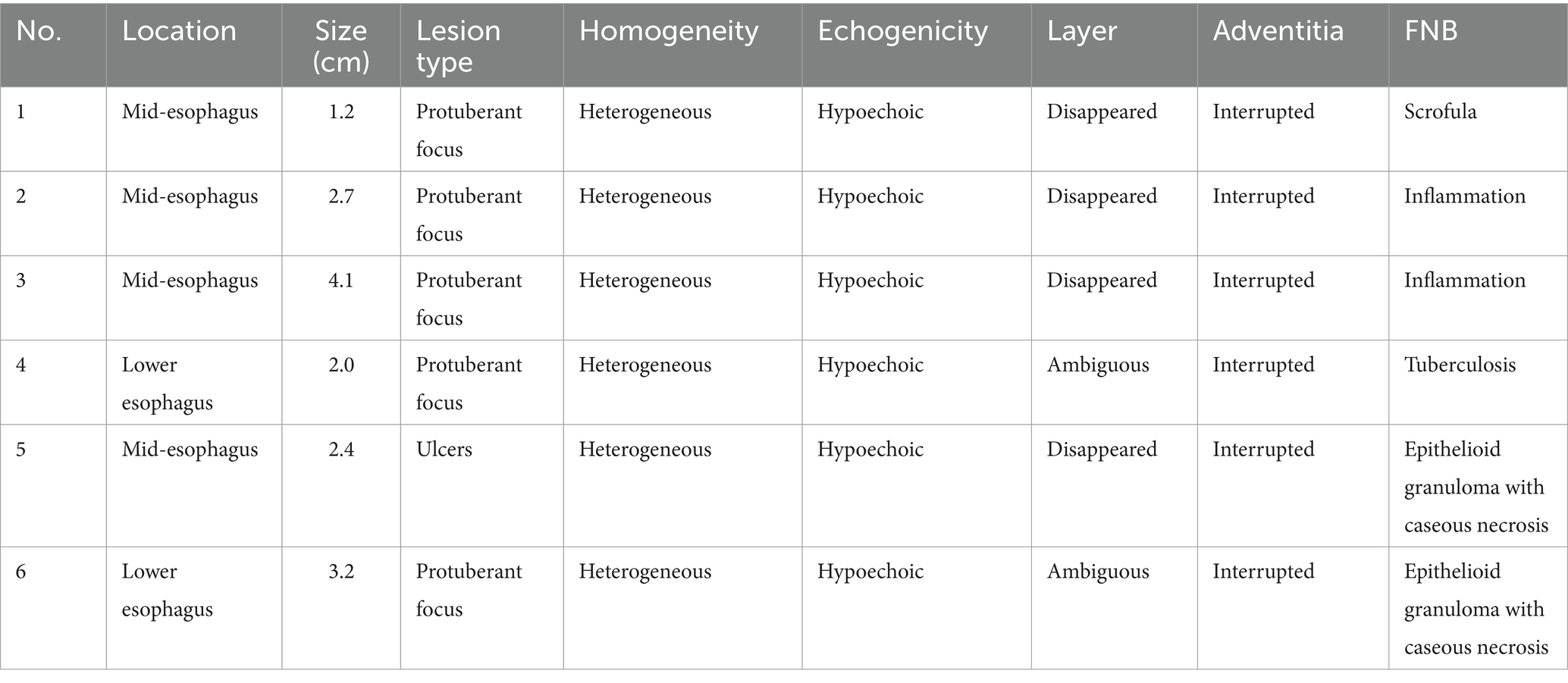
The site of lesions were located in the middle of esophagus in four patients while in another two were present in the lower esophagus. Five patients with esophageal protuberant focus. Four of them had ulcerated mucosa overlying the lesion while only one had intact mucosal surface. No extrinsic bulge but ulcers was only seen in the remaining one (Figures 1A,B). The characteristics of endoscopic features are presented in Table 2.
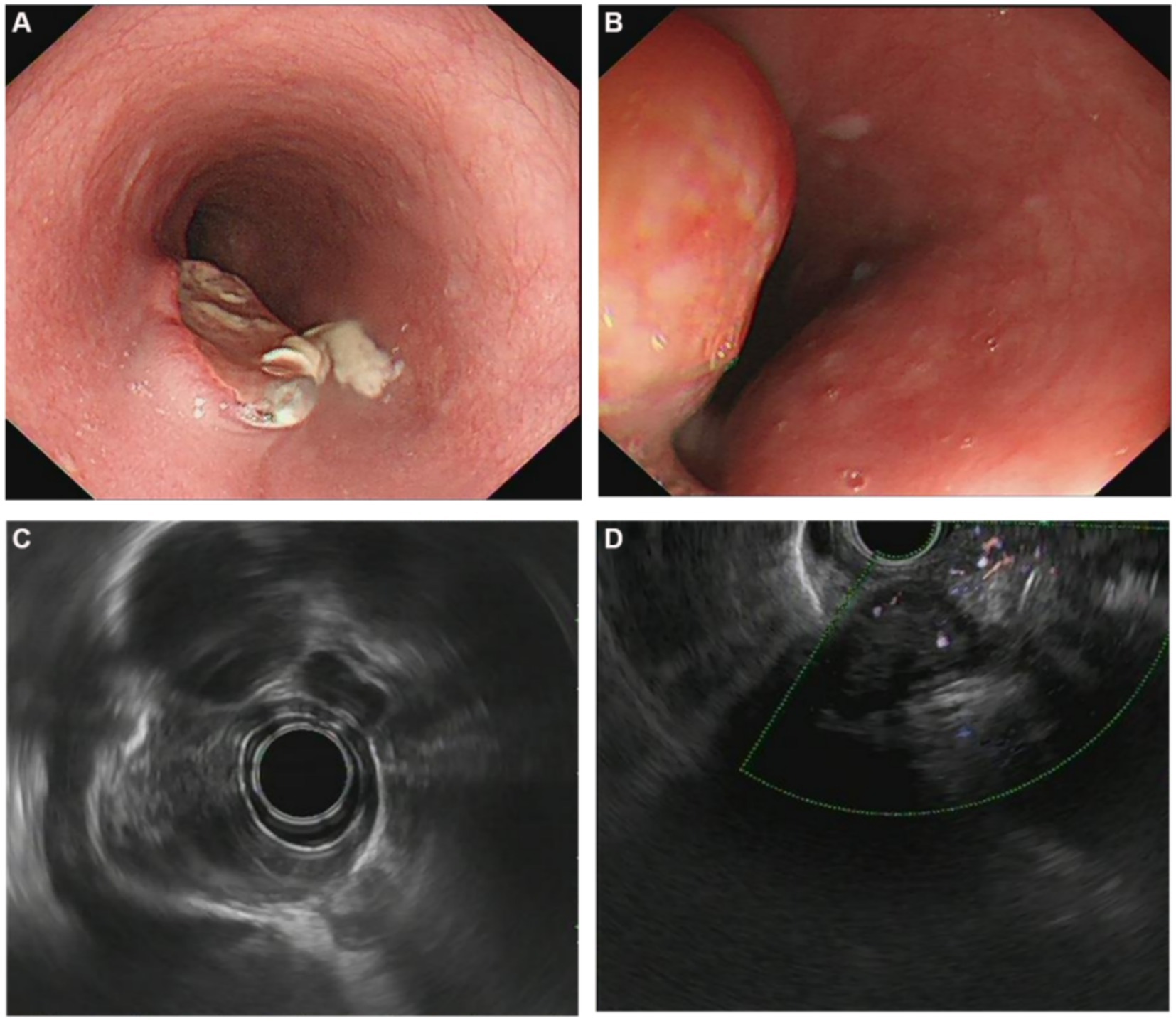
Figure 1. (A) Endoscopic and endosonographic images of patients with esophageal tuberculosis. Endoscopic image showing ovoid ulcer with yellowish-white caseous attachment at the edge; (B) Endoscopic image showing an esophageal protuberant focus; (C) Endosonographic images showing thickened esophageal wall, disappeared layer, heterogeneous and hypoechoic change; (D) Endosonographic images showing heterogeneous hypoechoic mass in the thickened esophageal wall, interruption and breakage of the esophageal adventitia, and fusion with mediastinal lymph nodes.
Endosonographic features
EUS showed involvement of thickened esophageal wall by a heterogeneous and hypoechoic lesions with interrupted of the adventitia in all cases (Figures 1C,D). Diameter of lesions range from 1.2 to 4.1 cm. Disappeared layers were seen in the thickened lesions in four patients, and ambiguous layers were observed in the remaining two. Multiple enlarged mediastinal lymph nodes in close proximity to or fused with each other were seen in four patients. The lymph nodes were of various sizes which between 0.6 and 1.6 cm in diameter. Endosonographic features are summarized in Table 2.
Histopathology/cytopathological features
EUS-FNB of both lesions and enlarged lymph nodes was performed in all cases, and it provided the pathological diagnosis of tuberculosis in four cases. Chronic granulomatous lesions with caseous necrosis was found in four, and Ziehl–Neelsen stain was positive in only one case. However, two cases showed mucosal tissues with chronic inflammatory changes, among which one was accompanied by hyperplasia and thickening of the overlying squamous epithelium and focal granuloma formation, for which the evidence was insufficient to diagnose tuberculosis. Therefore, the overall diagnostic yield of EUS-FNB is 66.67% in our study.
Treatment and follow-up
All patients were treated with standard antitubercular therapy (isoniazid, rifampin, pyrazinamide, and ethambutol). As to the two patients whose pathological examination showed nonspecific chronic inflammation, empirical antitubercular therapy was administered based on EUS morphology. At 3 months of follow-up, the masses were significant diminution in all cases. They were sequentially followed up for 12 months, and all patients had complete resolution of dysphagia and retrosternal pain. Moreover, EUS showed resolution of esophageal lesions and lymph nodes. Thus, antitubercular treatment was successful in all patients.
Discussion
Esophageal tuberculosis is a very rare clinical entity (7). It is usually secondary to mediastinal lymph node tuberculosis. However, primary esophageal tuberculosis is extremely uncommon due to the self-defense mechanisms of esophagus (8). A conglomerated mass of heterogeneous with predominantly hypoechoic lymphnodes with intervening hyperechoic strands and foci on EUS appears to be characteristic of mediastinal tuberculosis (9). As the same in this study, multiple enlarged mediastinal lymph nodes fused with each other were seen in 66.7% patients. As we found in this study, dysphagia with or without retrosternal pain is the most common symptom and most lesions were located in the middle of esophagus, and these results are consistent with existing reports (9–14). Constitutional symptoms such as fever, weight loss and night sweats are nonspecific and difficult to distinguish. Under white light endoscopy, esophageal tuberculosis may present as an ulcerative, hyperplastic, granular lesion or extrinsic bulge (15). Most cases are misdiagnosed as cancer before surgical exploration (16, 17). As the same in our study, the presentations of symptoms, laboratory examinations, endoscopic findings combination with CT scan imaging of all cases are nonspecific. As a result, they do not provide a definitive diagnosis. Histocytopathological diagnosis is crucial before administration of appropriate therapy, and EUS-FNB has emerged as an excellent tool to diagnose esophageal tuberculosis (18).
The characteristic EUS morphology highly suggestive of esophageal tuberculosis, and EUS is a feasible diagnostic method. Firstly, we found that multiple enlarged mediastinal lymph nodes in close proximity to or fused with each other were presented as hypoechoic EUS areas which indicating lymphadenitis. Additionally, this study summarized the main features of esophageal tuberculosis, including heterogeneous hypoechoic masses in the thickened esophageal wall, interruption and breakage of the esophageal adventitia. Disappeared or ambiguous layers were observed in the esophageal wall as seen by other authors (19).
Esophageal tuberculosis should be distinguished from advanced esophageal carcinoma and leiomyoma. Thomas W. Rice et al. summaried the characteristics of esophageal cancer in 22,123 clinically staged patients, which showed patients were older (62 years) men (80%) (20). In our study, patients were all aged (range 59–79 years), in which condition malignant tumor may presented as a first priority.
Although esophageal tuberculosis is very similar to malignancy, a few details from the results of this study may indicate significant differences. First, disease duration (ranged 15 days to 4 months) of esophageal tuberculosis patients in this study is actually short. But in esophageal cancer patients, disease course is often much longer. Second, it was reported that esophageal cancer most involved the distal esophagus (73%), which counter to esophageal tuberculosis. As we found, the site of lesions were most located in the middle of esophagus. Besides, the laboratory examinations such as tuberculosis test and several tumor markers contribute to identifying tuberculosis and cancer. Most of all, histological diagnosis is crucial. In contrast to imaging alone, image guided biopsy is more reliable to establish a definite diagnosis. According to the results of Puri et al., 84.5% of the esophageal tuberculosis patients were diagnosed by pathology (21). In this study, EUS showed characteristic morphology of esophageal tuberculosis in all cases. EUS-FNB provided the pathological diagnosis of tuberculosis in four of six cases, increasing the possibility of a positive diagnosis of tuberculosis.
In conclusion, EUS has characteristic appearances depending upon esophageal wall and mediastinal lymph nodes. EUS-FNB is an excellent method to establish an accurate diagnosis of esophageal tuberculosis.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the Union Hospital, Tongji Medical College, Huazhong University of Science and Technology. The studies were conducted in accordance with the local legislation and institutional requirements. No potentially identifiable images or data were included in this article.
Author contributions
HY: Data curation, Software, Visualization, Writing – original draft. HK: Validation, Writing – review & editing. YL: Validation, Writing – review & editing. YZ: Conceptualization, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Jilani, TN, Avula, A, Zafar Gondal, A, and Siddiqui, AH. Active tuberculosis. Treasure Island (FL): StatPearls Publishing (2024).
2. Ragonnet, R, Trauer, JM, Geard, N, Scott, N, and McBryde, ES. Profiling Mycobacterium tuberculosis transmission and the resulting disease burden in the five highest tuberculosis burden countries. BMC Med. (2019) 17:208. doi: 10.1186/s12916-019-1452-0
3. Gambhir, S, Ravina, M, Rangan, K, Dixit, M, Barai, S, and Bomanji, J. Imaging in extrapulmonary tuberculosis. Int J Infect Dis. (2017) 56:237–47. doi: 10.1016/j.ijid.2016.11.003
4. Rodriguez-Takeuchi, SY, Renjifo, ME, and Medina, FJ. Extrapulmonary tuberculosis: pathophysiology and imaging findings. Radiographics. (2019) 39:2023–37. doi: 10.1148/rg.2019190109
5. Han, D-G, Wang, D-C, and Liu, W. Primary esophageal tuberculosis. Clin Res Hepatol Gastroenterol. (2023) 47:102242. doi: 10.1016/j.clinre.2023.102242
6. Khan, MS, Maan, MHA, Sohail, AH, and Memon, WA. Primary esophageal tuberculosis mimicking esophageal carcinoma on computed tomography: a case report. World J Gastrointest Surg. (2019) 11:373–80. doi: 10.4240/wjgs.v11.i9.373
7. Singh, A, Mittal, D, Jain, V, Kabra, SK, and Agarwala, S. Primary esophageal tuberculosis. Indian J Pediatr. (2021) 88:947. doi: 10.1007/s12098-021-03876-5
8. Mao, L, Zhou, X-T, Li, J-P, Li, J, Wang, F, Ma, HM, et al. Esophageal tuberculosis complicated with intestinal tuberculosis: a case report. World J Clin Cases. (2020) 8:645–51. doi: 10.12998/wjcc.v8.i3.645
9. Tang, Y, Shi, W, Sun, X, and Xi, W. Endoscopic ultrasound in diagnosis of esophageal tuberculosis: 10-year experience at a tertiary care center. Dis Esophagus. (2017) 30:1–6. doi: 10.1093/dote/dox031
10. Xiong, J, Guo, W, Guo, Y, Gong, L, and Liu, S. Clinical and endoscopic features of esophageal tuberculosis: a 20-year retrospective study. Scand J Gastroenterol. (2020) 55:1200–4. doi: 10.1080/00365521.2020.1813799
11. Li, Y-X, Nian, W-D, and Wang, H-H. A case of esophageal tuberculosis with unusual endoscopic feature. Clin Res Hepatol Gastroenterol. (2018) 42:e5–6. doi: 10.1016/j.clinre.2017.04.010
12. Elosua González, A, Macías Mendizábal, E, Saldaña Dueñas, C, Fernández-Urién Sainz, I, and Vila Costas, JJ. Esophageal tuberculosis: a cause of dysphagia we should be aware of. Gastrointest Endosc. (2018) 88:964–5. doi: 10.1016/j.gie.2018.07.017
13. Mbiine, R, Kabuye, R, Lekuya, HM, and Manyillirah, W. Tuberculosis as a primary cause of oesophageal stricture: a case report. J Cardiothorac Surg. (2018) 13:58. doi: 10.1186/s13019-018-0743-4
14. Dahale, AS, Kumar, A, Srivastava, S, Varakanahalli, S, Sachdeva, S, and Puri, AS. Esophageal tuberculosis: uncommon of common. JGH Open. (2018) 2:34–8. doi: 10.1002/jgh3.12043
15. Patnayak, R, Reddy, MK, Parthasarathy, S, Yootla, M, Reddy, V, and Jena, A. Unusual presentation of esophageal tuberculosis mimicking malignancy. Saudi J Gastroenterol. (2008) 14:103–4. doi: 10.4103/1319-3767.39632
16. Solano Blas, MÁ, Cavildo Jerónimo, CD, and Amieva-Balmori, M. Esophageal tuberculosis as a differential diagnosis of esophageal cancer. Rev Esp Enferm Dig. (2024) 117:284–285. doi: 10.17235/reed.2024.10498/2024
17. Sharma, V, Rana, SS, Chhabra, P, Sharma, R, Gupta, N, and Bhasin, DK. Primary esophageal tuberculosis mimicking esophageal cancer with vascular involvement. Endosc Ultrasound. (2016) 5:61–2. doi: 10.4103/2303-9027.175924
18. Sawai, S, Yamada, R, Ikenoyama, Y, Nose, K, Tanaka, T, Nakamura, Y, et al. The diagnosis of esophageal tuberculosis through an endoscopic ultrasound-guided fine-needle aspiration biopsy: a case study. Intern Med. (2024). 63:2399–2405. doi: 10.2169/internalmedicine.2824-23
19. Zhu, R, Bai, Y, Zhou, Y, Fang, X, Zhao, K, Tuo, B, et al. EUS in the diagnosis of pathologically undiagnosed esophageal tuberculosis. BMC Gastroenterol. (2020) 20:291. doi: 10.1186/s12876-020-01432-7
20. Rice, TW, Apperson-Hansen, C, DiPaola, LM, Semple, ME, Lerut, TEMR, Orringer, MB, et al. Worldwide esophageal cancer collaboration: clinical staging data. Dis Esophagus. (2016) 29:707–14. doi: 10.1111/dote.12493
Keywords: esophagus, tuberculosis, endoscopic ultrasonography, EUS-FNB, diagnosis
Citation: Yang H, Ke H, Lei Y and Zhu Y (2025) Case Report: Endoscopic ultrasound-guided fine-needle biopsy for the diagnosis of esophageal tuberculosis. Front. Med. 12:1575045. doi: 10.3389/fmed.2025.1575045
Edited by:
Angel Lanas, University of Zaragoza, SpainReviewed by:
Ravi Kumar Sharma, Chandigarh University, IndiaHuaping Xie, Huazhong University of Science and Technology, China
Manoj Madhusudan, Kauvery Hospital Tennur, India
Copyright © 2025 Yang, Ke, Lei and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yong Zhu, bmR5ZnkwMDMzOEBuY3UuZWR1LmNu
 Hailin Yang1
Hailin Yang1 Yong Zhu
Yong Zhu