- 1Medical Records and Statistics Department, Shanghai Sixth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 2Department of Medical, Putuo People’s Hospital, School of Medicine, Tongji University, Shanghai, China
- 3School of Public Health, Fudan University, Shanghai, China
- 4Shanghai Public Health Clinical Center, Fudan University, Shanghai, China
Background: Shared decision making (SDM) could significantly enhance health knowledge, treatment adherence, and doctor-patient relationship, but multifaceted barriers have influenced the implementation of SDM worldwide. There are now few studies on SDM process from the perspective of healthcare workers who often act as the initiators of SDM. Focusing on healthcare providers, this study aimed to explore the mechanism by which provider-patient communication, trust, and respect influenced SDM within the context of China’s three-tier public hospital system.
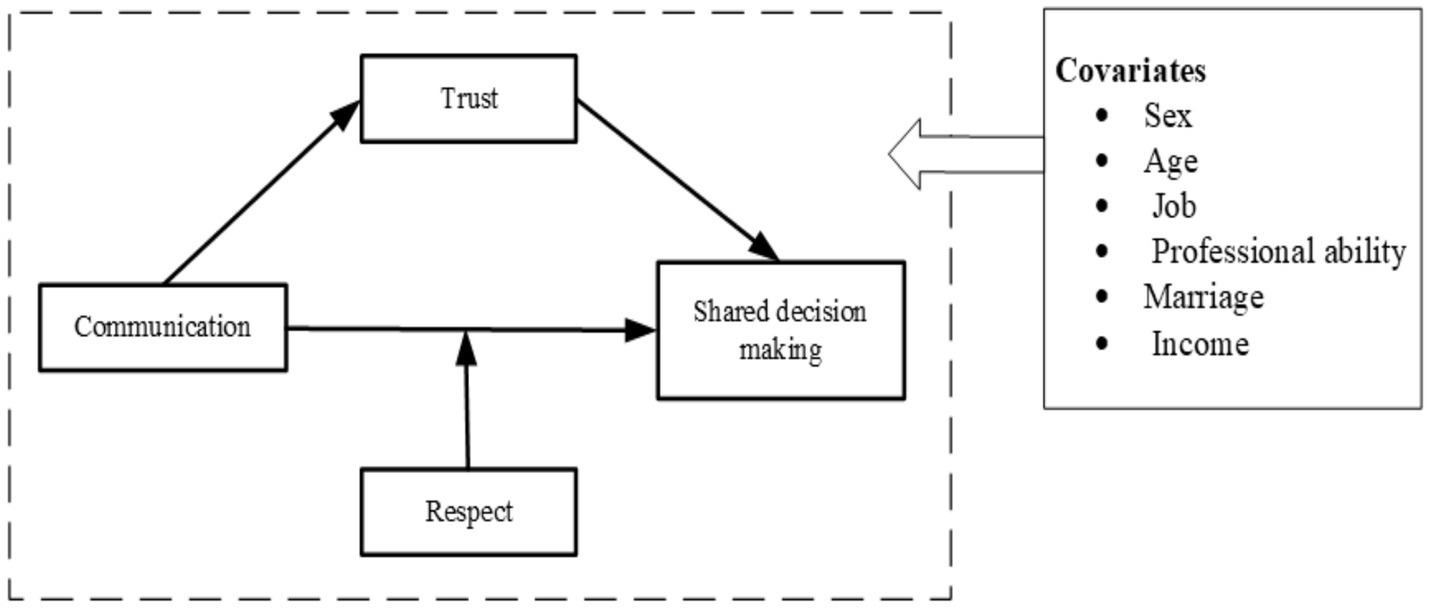
Methods: A stratified sampling was employed to survey doctors and nurses from public hospitals in Shanghai, China. The questionnaire included respect, patient-provider communication, trust, SDM, and socio-demographic information. Structural equation modeling was used to examine the study hypotheses, after controlling demographics covariates.
Results: There were 778 participants included in this study. The constructs in our study exhibited good reliability and validity, and the SEM demonstrated good fit (CFI = 0.978, TLI = 0.974, RMSEA = 0. 039, SRMR = 0.036). Provider-patient communication and trust were significant factors influencing SDM (p < 0.001), and R-square for regression models were all more than 30%. Additionally, trust between providers and patients mediated the relationship between communication and SDM (effect = 0.221, 95% CI: 0.133–0.359), and the mediating effect accounted for 39.89% of the total effect in primary hospitals, while it was 20 and 19.34% in secondary and tertiary hospitals. Moderating analysis showed that respect positively influences the relationship between communication and SDM in secondary hospitals (effect = 0.327, 95% CI: 0.156–0.498), but this effect was not significant in primary (95% CI: −0.035-0.405) or tertiary hospitals (95% CI: −0.072-0.210).
Conclusion: Provider-patient communication and trust were important factors influencing SDM according to healthcare providers, and respectful behaviors was key to improving communication and SDM in the secondary hospital. These suggested evidence for the development of strategies to promote SDM in the future.
1 Introduction
China’s healthcare system is structured around public hospitals, categorized into primary, secondary, and tertiary levels. Primary hospitals serve local communities with basic healthcare needs, and providers may have more communication with patients. While secondary hospitals handle more complex cases compared to the primary ones, and serve as the hub of healthcare system. Tertiary hospitals, often located in urban areas, provide advanced medical care, and their providers deal with higher patient volumes and more specialized treatments. Each level of hospital serves distinct roles and functions within healthcare system, and patients with different socioeconomic backgrounds can choose different hospitals according to treatment needs (1, 2).
Shared decision making (SDM) refers to a collaborative process where healthcare professionals and patients make medical decisions together based on the best available evidence, considering the patients’ values and preferences (3, 4). SDM establishes a balance between the traditional paternalistic model, where the healthcare professionals predominantly make the medical decisions, and the informed choice model, where the patients make decisions independently, while SDM forms the foundation of patient-centered healthcare (5, 6). At present, China has abandoned the traditional paternalistic medical decision-making approach and is still mainly following the informed choice model for medical decision-making (7). Increasing evidence indicated that SDM could significantly enhance health related knowledge, treatment adherence, and quality of life, and also help to reduce healthcare costs and the incidence of doctor-patient disputes, which could help reduce occupational injury risks for healthcare workers and alleviate their work-related stress (8, 9). However, despite its benefits, the implementation of SDM worldwide faces multifaceted barriers, such as healthcare policy discrepancies, institutional administration constraints, and inadequate decision-support tools, and all these problems are particularly common in developing countries (10). In China, while SDM principles have been increasingly recognized, systematic implementation remains limited due to the absence of standardized guidelines and structured decision-making procedures (11). Recent studies have identified healthcare providers’ communication competencies, attitudes toward patient autonomy, and trust-building capacities as critical yet underdeveloped components of SDM in Chinese clinical settings (12, 13). For instance, a recent Chinese study revealed that in six distinct clinical decision-making scenarios, 52.7 to 71.6% of mental health practitioners opted against SDM practices, with communication competencies and the establishment of trust-based practitioner-patient relationships emerging as the primary determining factors (14). Healthcare providers often act as the initiators of SDM, determining when and how shared decision-making begin with patients (15), but there is a lack of study on SDM process from the perspective of healthcare workers. In fact, healthcare providers’ communication skills, respectful attitudes, and levels of trust are key components of SDM practice, which urgently need study to explore their underlying mechanisms (16–18).
Patient-centered communication ensures the detailed exchange of medicine-related information (19, 20). In practice, doctors and nurses often have different types of communication with patients, in which doctors should focus more on diagnosis and treatment options, while nurses could spend more time on patient education and emotional support (21). Additionally, SDM is not solely the responsibility of doctors, but it also requires the active participation of nurses who play a vital role in adjusting treatment plans and discussing with patients to develop a consensus of physical recovery and medical care (18). Deepshikha (22) et al. in their qualitative study about racial differences in SDM, found that issues related to communication, such as providing limited emotional support and sharing limited medical information, were the most crucial factors impeding SDM. Besides, a randomized controlled trial showed that a specific communication training could effectively enhance physicians to perform SDM and reduce frustration in patients (23). Detailed information interaction helps healthcare providers better understand the patients’ needs, specify the patients’ treatment preference, and promote continuity of medical care (24). Further, doctors and nurses can explain the patients’ condition, treatment options, and their potential risks and benefits through communication (19, 25). Consequently, these could enable healthcare providers to encourage patients to participate more actively in medical decision-making. Therefore, we proposed the following research hypothesis:
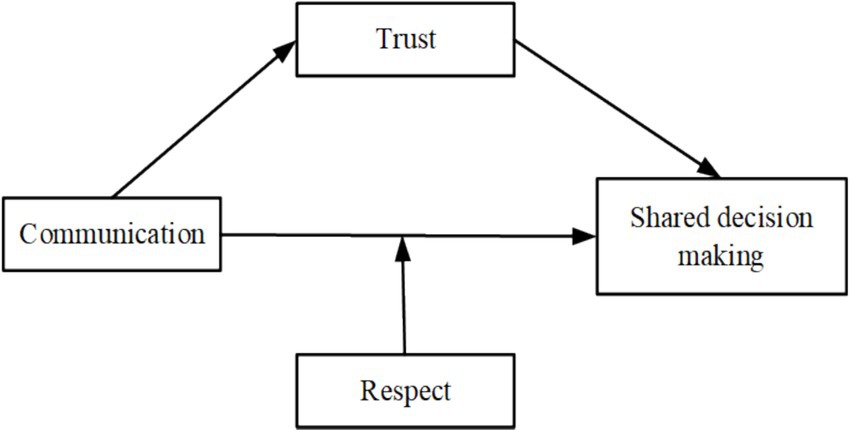
H1: Communication between healthcare providers and patients was a direct influencing factor for SDM.
Communication between healthcare providers and patients is important to build and maintain mutual trust (26). Trust was essential for building successful patient-physician relationship, and was proven to be a significant predictor of enhancing shared information, reducing defensive practices, and improving health outcomes (27). When healthcare providers communicate effectively, it not only conveys necessary medical information but also expresses emotional empathy, which is crucial for establishing trust (28). For instance, Du et al. (29) found that doctor-patient communication could significantly influence the quality of health services and patient satisfaction, which in turn helped to build doctor-patient trust. Trust, in turn, is essential for SDM. When patients and healthcare providers build trust relationship, they are more likely to engage in open dialogs, share their preferences, and participate actively in medical decision-making. A cohort study found that patient-provider trust strengthened both behavioral changes in shared decision-making, which in turn reduced adverse medical events such as low treatment adherence (30). Based on these, we recognized that communication could improve trust and then enhance the likelihood of SDM, although the medicating effect has not been verified by empirical analysis evidence. Therefore, we proposed the following research hypothesis:
H2: Trust between healthcare providers and patients mediated the relationship between communication and SDM.
Respect in medical service is a critical component of patient-centered healthcare, and it often involves dignity, rights, and autonomy to patients (31). Previous studies showed that respect from healthcare providers can enhance patients’ perception of being valued and understood, thereby promoting their engagement in healthcare (32, 33). Further, existing evidence suggested that respect of medical staff could promote SDM. For instance, a study (34) found that an atmosphere of respect for the patient, will be more conducive to communication between the patient and their providers, which could improve SDM in the end. Additionally, another study (35) demonstrated that respect, such as carefully listening to patients and acknowledging their concerns, could strengthen the communication process and contribute to SDM. When healthcare providers communicate clearly, it helps patients understand their health conditions and treatment options, which is crucial for making medical decisions. Besides, respectful performance can improve the positive effects of communication by making patients feel more comfortable and willing to participate in discussions about their medical plans (36). Therefore, we proposed the following research hypothesis:
H3: Respect from healthcare providers moderated the relationship between communication and SDM.
Based on the hypotheses above, considering the unique characteristics of primary, secondary, and tertiary hospitals, this study aimed to provide an understanding of the effects of communication, trust, and respect, on SDM (see Figure 1), which were expected to offer valuable insights for developing strategies to enhance SDM practice.
2 Materials and methods
2.1 Study design and setting
Shanghai, as one of China’s most developed and densely populated cities, exhibits significant socioeconomic and healthcare system diversity across its 16 districts, mirroring the heterogeneity found in other eastern regions (e.g., Jiangsu, Zhejiang). In April 2024, the Shanghai Municipal Health Commission issued Guidelines on Promoting the Cultural Development of Health Services in the New Era, explicitly emphasizing patient-centered care, enhanced doctor-patient communication, transparent medical information, and shared decision-making (SDM) in public hospitals. This policy initiative aligns with our study’s focus on healthcare providers’ communication skills, trust-building, and respectful attitudes in SDM implementation.
This cross-sectional survey was conducted from June 1, 2024, to August 30, 2024. In 2023, Shanghai had a total of 92,300 licensed physicians and approximately 113,000 registered nurses, with healthcare institutions at all levels handling 266 million patient visits throughout the year. A multistage sampling method was used to choose doctors and nurses in public hospitals in Shanghai. First, we identified 16 geographic regions based on the administrative divisions of Shanghai, and collected basic information on all public medical institutions within each region, such as number of doctors and nurses. Second, one public hospital was selected from each region, provided that the total number of doctors and nurses in each hospital exceeded 50. Then, we included 16 public hospitals, which were six primary hospitals, five secondary hospitals, and five tertiary hospitals. Next, stratified random sampling method was adopted to obtain samples, stratified according to the participants job characteristics in each hospital, and then 50 people from each hospital were selected by computer random number generation. Finally, data were collected through electronic questionnaires. The first page of the questionnaire was an informed consent form, and participants indicated their willingness to participate in the study by providing an electronic signature.
2.2 Participants
In the survey, we used the following criteria to include participants: (1) full-time employees of public hospitals in Shanghai, (2) working as doctors or nurses, (3) with the ability to communicate with patients, and (4) with the ability to make medical decisions. Conversely, we excluded specific participants based on the following criteria: (1) with less than 6 months of medical work experience, (2) working mainly in administrative departments with minimal involvement in medical activities, and (3) unwilling to participate in this study. A total of 800 questionnaires were distributed in target population, and 778 valid responses were received, resulting in a response rate of 97.25% in this study.
2.3 Measurements
The questionnaire for this study included four constructs: respect of healthcare professionals, patient-provider communication, patient-provider trust, and medical shared decision-making behavior. Besides, we collected participants’ socio-demographic information, including sex, age, marital status, and income.
Respect of Healthcare Professionals. We used the sub-scale from the Climate of Respect Evaluation to measure disrespectful behavior among healthcare professionals (37). This sub-scale consisted of 4 items and was initially used to assess the disrespectful behaviors performed by healthcare workers in intensive care units (37). It has been validated for use in measuring disrespect among healthcare professionals across various hospital departments. The disrespect sub-scale included four items, which measured how often that participants dismissed family concerns, talked down to patients and families, spoke disrespectfully behind their backs, and got frustrated with patients and families. All items were rated on six points measuring the frequency of these behaviors (all of the time without exception, nearly all of the time with rare exceptions, most of the time, some of the time, rarely, and never), with scores ranging from 1 to 6 after reversing code items to capture respect. In this study, the 4-item sub-scale had a Cronbach’s alpha of 0.784, indicating acceptable reliability.
Patient-Provider Communication. This study utilized the Physician-Patient Global Interaction Scale (PP-GIS) developed by Hodges and McIlroy (38) to evaluate the communication from the opinion of healthcare provider. This scale has been widely used to assess the level of patient-provider communication across various hospital departments (39, 40). The measurement tool included four items: responsiveness to patients’ feelings and needs (empathy), consistency in communication with patients (amount of organization), verbal expression, and non-verbal expression. Each item on the PP-GIS was measured on a five-point option: never, occasionally, sometimes, often, and always, with scores ranging from 1 to 5. In this study, the Cronbach’s alpha for the PP-GIS was 0.950, indicating excellent reliability.
Provider-Patient Trust. This study employed the sub-dimension “patient role” from the widely used Physician Trust in the Patient scale to measure trust (41). This sub-dimension primarily identified the healthcare professionals’ subjective attitudes toward the patients. The measurement asked healthcare professionals, “How confident are you that this patient will.,” and it included the following five items: “Provide all the medical information you need?,” “Let you know when there has been a major change in his or her condition?,” “Understand what you tell him/her?,” “Follow the treatment plan you recommend?,” and “Be actively involved in managing his/her condition/problem?.” In this study, the scale had a Cronbach’s alpha of 0.896, indicating good reliability.
Patient-Provider Shared Decision Making. SDM was measured using the OPTION5 Item scale, which focused on the core essential requirements when providers involved patients in decision-making (42). This scale included five dimensions: justified the work of deliberation, justified the work of deliberation as a team, informed/described options/exchange views, elicited preferences, and integrated preferences. Each item on the OPTION5 Item scale was rated on a five-point scale: never, occasionally, sometimes, often, and always, with scores ranging from 1 to 5. In this study, the Cronbach’s alpha for the OPTION5 Item was 0.946, indicating excellent reliability.
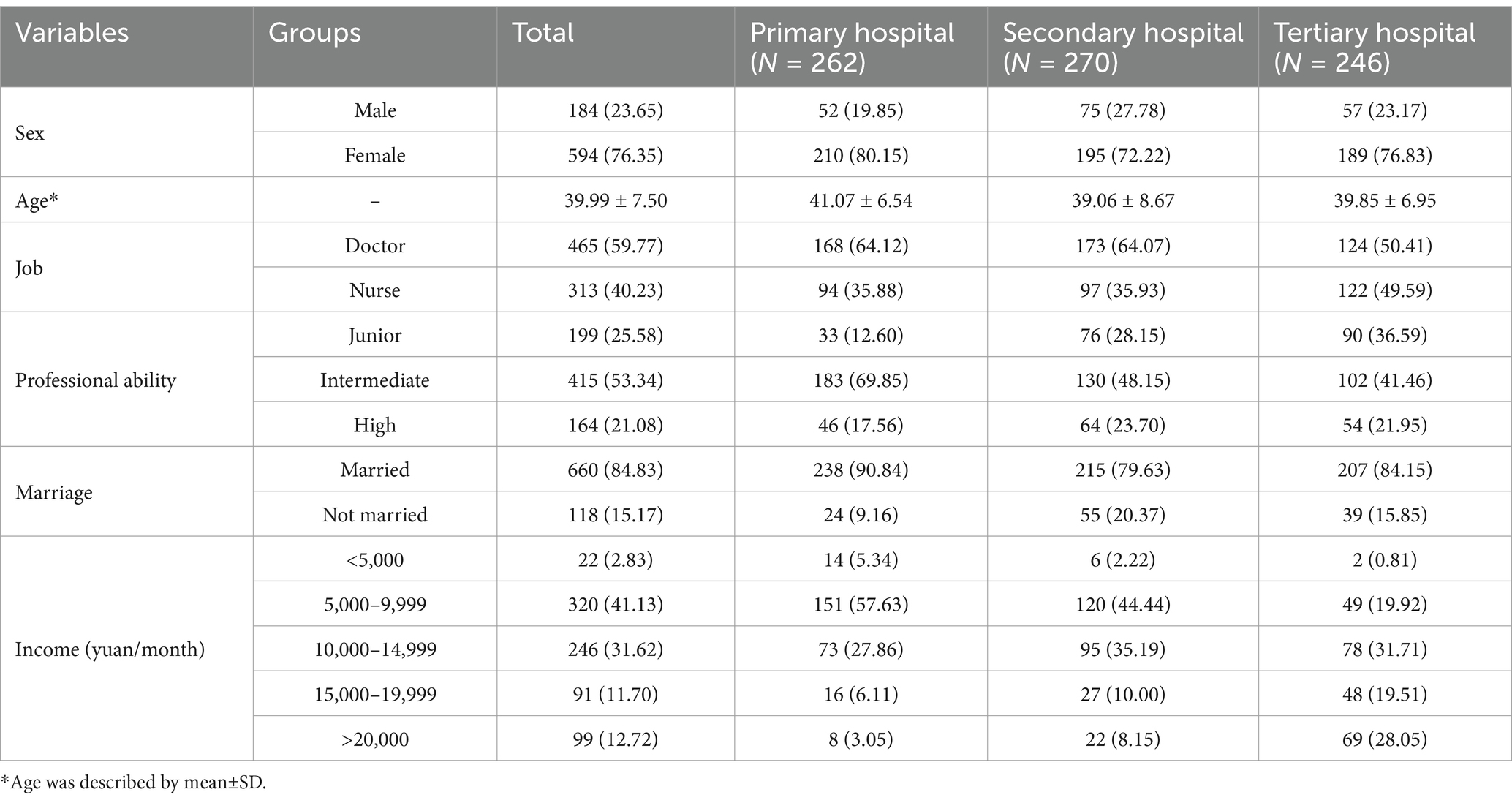
Socio-demographic Characteristics. This study included sex, age, job, professional ability, marriage, and income. Professional ability was determined according to the professional titles of Chinese healthcare personnel, corresponding to junior, intermediate, and high professional ability. Marriage status inquired about the respondents’ marital situation, including married and unmarried, with the latter encompassing divorced and widowed. Income was measured by the average monthly income over the past year, categorized into five levels: <5,000, 5,000–9,999, 10,000–14,999, 15,000–19,999, and >20,000 yuan.
2.4 Statistical analysis
For categorical variables, we used number (N) and percentage (%) to summarize the sample. For continuous variables with a nearly normal distribution, we described them using mean and standard deviation (SD). The normal distribution test was conducted by two methods: visual assessment with Q-Q plots and the Kolmogorov–Smirnov test to evaluate the probability of the data being normally distributed. After testing, the continuous variables were approximately normal distribution. These statistical analyses were performed using Stata/MP version 14.0 (StataCorp, College Station, TX, United States).
To account for mediating and moderating variables in the research model, we employed structural equation model (SEM) to test the hypotheses. SEM was utilized to identify latent but significant influences, providing a more comprehensive understanding of the complex mechanisms while incorporating measurement error into the research model (43). Additionally, confirmatory factor analysis (CFA) was conducted to assess the validity and reliability of the constructs, and to integrate with SEM for model improvement. We then reported factor loadings (F. L.), composite reliability (CR), average variance extracted (AVE), and discriminant validity. Model fit was assessed using the comparative fit index (CFI), Tucker-Lewis index (TLI), root mean squared error of approximation (RMSEA), and standardized root mean square residual (SRMR). Mediation and moderation models used bootstrapping (times = 2000) which was a nonparametric method that did not assume a normal distribution. Evidence of mediation and moderation was provided by a significant effect, as indicated by a 95% confidence interval (CI) that did not include zero. In SEM analysis, this study controlled the confounders of socio-demographic characteristics, to reveal the exact correlation between the study variables and SDM (see Figure 2). Also, we evaluated the importance of mediating variable in explaining the relationship between independent and dependent variables, which was suggested by proportion of mediating effect (see Equation 1). The analyses were performed using Mplus version 7.4 software (Muthén & Muthén, Los Angeles, CA, United States).
3 Results
3.1 Characteristics of the sample
Among the 778 participants, approximately three-quarters were female (76.35%), with an average age of 39.99 years (SD = 7.50). Regarding job positions, 465 (59.77%) were doctors and 313 (40.23%) were nurses, with doctors were more than nurses in all three types of hospitals. In terms of professional ability, there were 199 (25.58%) at the junior level, 415 (53.34%) at the intermediate level, and 164 (21.08%) at the high level. Concerning marital status, 660 (84.83%) were married, while 118 (15.17%) were unmarried, divorced, or widowed. In terms of monthly income, the largest group earned 5,000–9,999 yuan (41.13%), followed by those earning 10,000–14,999 yuan (31.62%), with the smallest group earning less than 5,000 yuan, comprising only 22 (2.83%) individuals. Detailed information showed in Table 1.
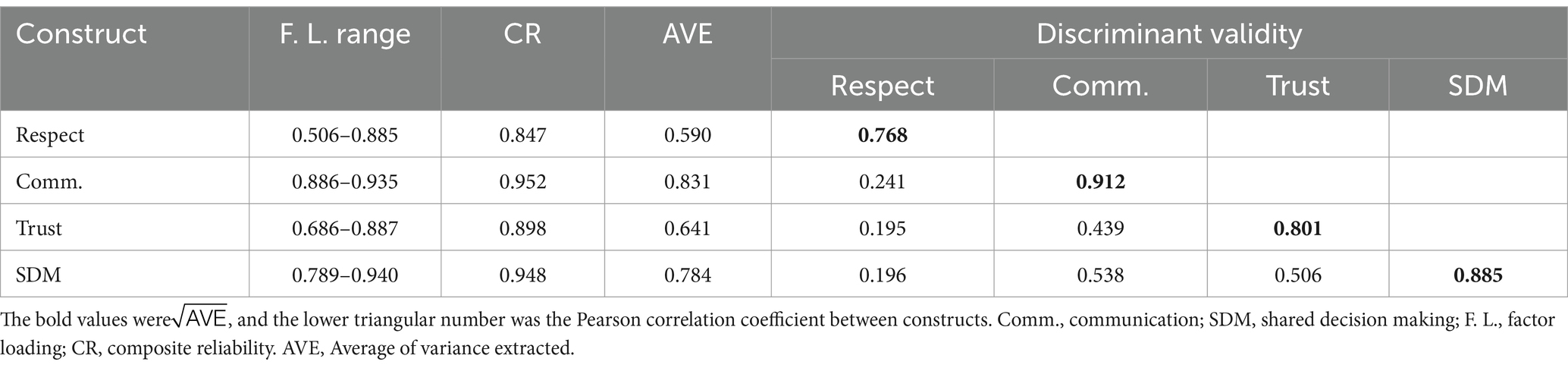
3.2 Reliability and validity of the constructs
All factor loadings of the items were >0.5, which showed that these items could measure the four constructs well, under the condition of the sample size being greater than 700. Additionally, all the values of the CR were >0.8, which exhibited that the constructs had good composite reliability. Besides, the values of were more than the row and column Pearson correlation coefficient between constructs, which implied ideal discriminant validity. In brief, the study constructs exhibited good reliability and validity. See Table 2.
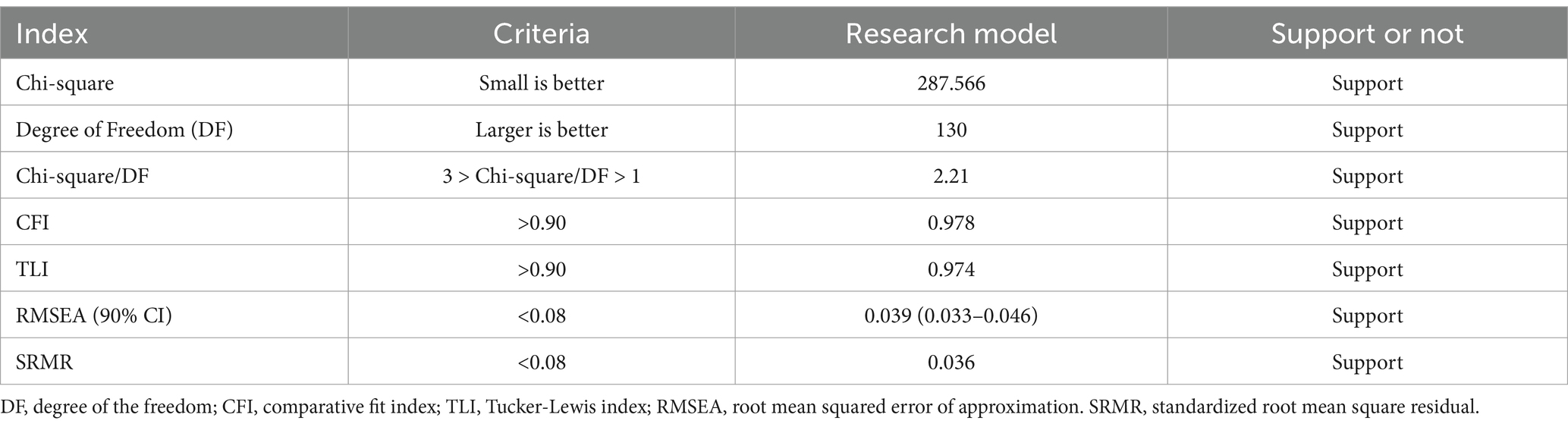
3.3 Test of the fitting index of the research model
The results showed that the Chi-square and degree of freedom (DF) were 287.566 and 130, respectively. It resulted in a Chi-square/DF ratio of 2.21, which was within the ideal range of 1 to 3. Additionally, the CFI and TLI values were 0.978 and 0.974, respectively, meeting the threshold standard of >0.9 (44). Moreover, the RMSEA and SRMR values were 0.039 and 0.036, respectively, both satisfying the SEM criterion of less than 0.08 (44). Therefore, these indicators suggested that the data fit the conceptual research model very well (44). See Table 3.
3.4 Results of the linear regression model
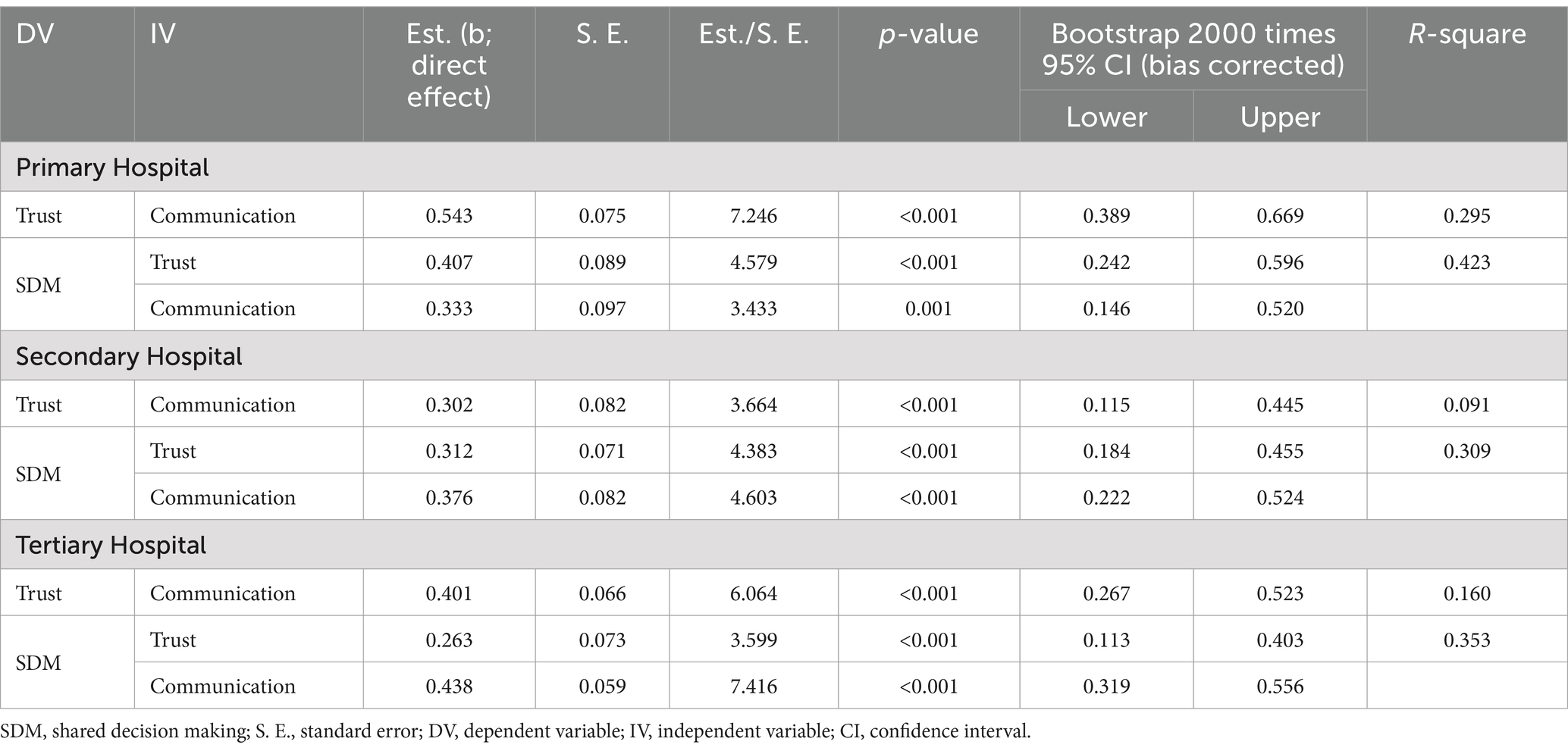
For primary hospitals, communication positively impacted trust between patients and doctors/nurses (b = 0.543, 95% CI: 0.389–0.669), with an R-square of 0.295 for this regression model. The occurrence of SDM was significantly and positively influenced by both doctor/nurse–patient communication (b = 0.333, 95% CI: 0.146–0.520) and trust (b = 0.407, 95% CI: 0.242–0.596), yielding an R-square of 0.423 for this regression model. In secondary hospitals, communication also had a significant positive effect on trust between patients and doctors/nurses (b = 0.302, 95% CI: 0.115–0.445). The occurrence of SDM in these hospitals was significantly positively influenced by both communication (b = 0.376, 95% CI: 0.222–0.524) and trust (b = 0.312, 95% CI: 0.184–0.455), with an R-square of 0.309 for this regression equation. Similarly, for tertiary hospitals, communication significantly positively impacted trust between patients and doctors/nurses (b = 0.401, 95% CI: 0.267–0.523). Additionally, both communication (b = 0.438, 95% CI: 0.319–0.556) and trust (b = 0.263, 95% CI: 0.113–0.403) significantly influenced SDM, with an R-square of 0.353 for this regression equation. See Table 4.
3.5 Mediating and moderating analysis on shared decision making
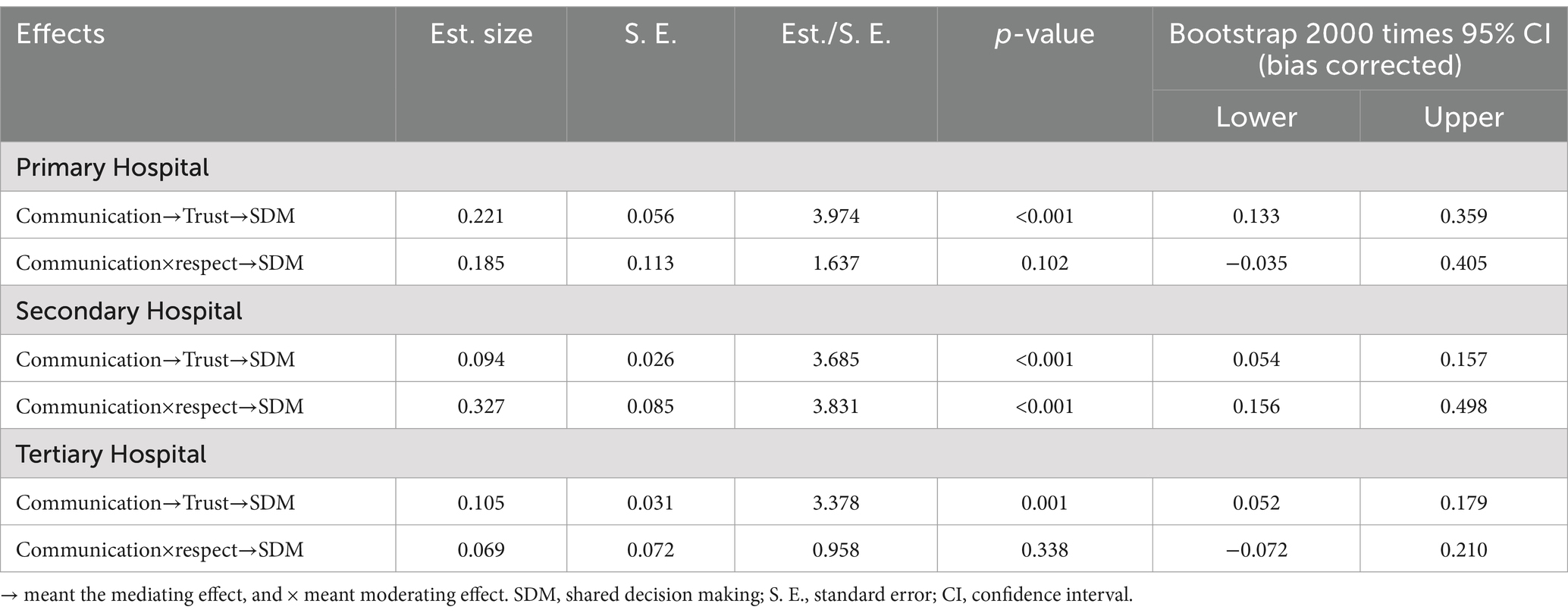
In primary hospitals, trust between patients and doctors/nurses significantly mediated the relationship between communication and SDM, with a mediating effect of 0.221 (95% CI: 0.133–0.359). Moreover, the total effect of communication on SDM was the sum of the direct effect (0.333) and the indirect effect (0.221), indicating that the mediation effect due to trust constituted 39.89% of the total effect. However, respect between patients and doctors/nurses did not emerge as a significant moderator in the communication and SDM relationship (95% CI: −0.035-0.405). In secondary hospitals, the trust factor significantly mediated the link between communication and SDM, showing a mediation effect of 0.094 (95% CI: 0.054–0.157), which accounted for 20% of the total effect. Additionally, respect served as a significant moderator (95% CI: 0.156–0.498). In tertiary hospitals, trust between patients and doctors/nurses also played a significant mediating role in the communication-SDM relationship, with a mediation effect of 0.105 (95% CI: 0.052–0.179), representing 19.34% of the total effect. Nonetheless, respect did not act as a significant moderator in the relationship between communication and SDM (95% CI: −0.072-0.210). See Table 5.
4 Discussion
SDM is crucial for addressing the information asymmetry inherent in healthcare services, as it can ensure both providers and patients fully understand the disease condition, treatment plan, and the expected outcomes. However, few studies have explored the mechanism of SDM from the perspective of healthcare provider who plays a leading role in the SDM process, so it has not yet understood how to promote SDM in the process of medical services. In order to fill this research gap, this study explored the effects of communication, trust, and respect on SDM at different levels of public hospitals, which could provide evidence for the development of strategies to promote SDM in the future.
First of all, this study developed a conceptual framework for SDM by literature review, which proposed the impact pathways of SDM in theory. Furthermore, we selected developed measurement tools and conducted confirmatory factor analysis, which revealed that the constructs in our study had good reliability and validity, indicating the suitability of these measurement tools for this study. Additionally, we employed SEM to examine the theoretical framework, and found that all model fit indexes met statistical requirements. These findings have significant implications, providing a basic framework for future SDM studies and practice.
The regression analysis indicated that for healthcare providers in China’s three-tier public hospital system, communication and trust were crucial factors influencing SDM from the perspective of healthcare providers. This finding was in line with Derrington et al. (45) that found SDM depended on high-quality communication between the physician and patients. The detailed exchange of information in communication process ensures that patients and medical staff can be well-informed about disease condition, the available treatment options, and the associated risks and benefits, which empowers them to participate in the decision-making process (46). Besides, trust between healthcare providers and patients was found to be another significant factor influencing SDM. Trust reduces psychological barriers and fosters a collaborative environment where physicians feel comfortable to provide the comprehensive and feasible disease treatment and health promotion plans (47, 48). Furthermore, the coefficient of determination from the regression analysis revealed that trust and communication between healthcare providers and patients accounted for over 30% of the variance in SDM across the three types of public hospitals. This finding indicated that enhancing trust and communication could potentially increase the likelihood of healthcare providers engaging in SDM by more than 30%. However, the occurrence of communication and trust can be complicated due to deeply ingrained cultural values in China. On the patient side, persistent paternalistic health beliefs may lead to reluctance in challenging physicians’ opinions, whereas younger generations increasingly demand autonomy—creating trust-building challenges (49). Conversely, healthcare providers trained in expert-authority model, which may perceive SDM as time-consuming rather than beneficial (50). Therefore, health-related institutions should invest to conduct mandatory communication skill training for all physicians, focusing on information structuring and emotional resonance. In addition, the public hospitals should build standardized trust metrics in daily management, and carry out regular monitoring and assessment of trust levels, by which SDM can be effectively realized in real world.
The mediation model analysis indicated that, in all public hospitals, effective communication positively impacted trust between patients and healthcare providers, which in turn promoted the occurrence of SDM. This finding highlighted that communication could directly influence trust, and it subsequently enhanced SDM practice for the healthcare providers. Effective communication is not only the ability of healthcare professionals to convey information about diagnoses, treatment options, and potential risks and benefits, but also includes emotional interactions and compassionate expression (51). These are vital for patients to feel concerned, understood, and warm, which then contributes to form mutual trust and encourage SDM in medical service process (52). In further analysis, this study revealed that the proportion of the mediation effect to the total effect varies across different levels of public hospital. In primary, secondary, and tertiary institutions, the mediation effect accounted for 39.89, 20, and 19.34% of the total effect, respectively. In secondary and tertiary hospitals, while the mediation effect was still significant, it was relatively lower compared to primary hospitals. In the primary healthcare, under China’s policy mandating ‘primary care first’, patients with chronic conditions establish long-term relationships with primary providers (53). This relational continuity enables cumulative communication to foster deep affective trust, so trust mediates nearly 40% of communication’s effect on SDM, as mutual understanding transforms dialog into SDM (29). Secondary hospitals often face severe patient-provider ratio imbalances, creating transactional rather than relational encounters, and communication becomes task-oriented, which then could inhibit trust development (54). In secondary hospital, although trust remained a significant mediator, its reduced role (20%) reflects more complex and specialized nature of care in these settings. In tertiary hospitals, complex cases involving multiple specialists can decline individual communication effects, and more utilities of decision aids may reduce reliance on interpersonal trust, both of which could weaken the mediating effect (9, 11). Therefore, though improving communication remains momentous, additional strategies to build trust should also be essential to enhance SDM in three-level hospitals. Primary hospitals should implement relationship continuity incentives and community-based trust circles, while secondary and tertiary hospitals should develop time-sensitive communication toolkits, and combine expertise-transparency displays with decision aid integration, which could be beneficial to achieve SDM practice.
The analysis of the moderation model revealed that, for healthcare providers in secondary public hospitals, respect positively moderated the relationship between patient-provider communication and SDM. Secondary hospitals typically cater to diverse patient population with different health conditions, which requires a balance between specialized care and general medical services (55). In such settings, respect from healthcare providers can enhance communication by creating a more open and easy-going dialog environment, which in turn facilitates more effective SDM (56). Besides, respect counteracts traditional hierarchical form which medical staff have the monopoly authority in healthcare process, and it could reduce power asymmetry, enabling equitable dialog essential for SDM (57). However, this moderating effect was not significant among healthcare providers in primary and tertiary hospitals. In primary hospital, patients often have more frequent and ongoing interactions with their providers, in which patients will naturally feel get much respect regardless medical staff have not great respect attitude, so it potentially diminishes the observable moderating effect of respect (58). In tertiary hospital, healthcare often involves complex medical conditions and advanced treatments, where clinical expertise and the clarity of medical information could take precedence over interpersonal communication (59). Additionally, the higher patient turnover and the more transactional nature of interactions in tertiary settings can limit the extent to which respect moderate the relationship of communication and SDM (60). Therefore, public hospitals, especially the secondary, should develop policies that promote a culture of respect among healthcare providers, which includes patient-centered service and communication training, and regular feedback mechanisms to assess and improve provider-patient communication.
However, some limitations should be mentioned in this study. Firstly, consistent with all cross-sectional designs, our SEM analysis identified statistically significant associations but cannot prove causation. While we employed anchored scale items and controlled for key confounders, the directionality of relationships between communication competence, trust, and SDM implementation remains theoretically inferred rather than empirically demonstrated. While the findings suggested significant associations, longitudinal studies were needed to confirm the causal pathways and to observe changes over time. Secondly, the study was conducted in public hospitals in Shanghai, China, which may limit the generalizability of the findings to other regions or healthcare systems. This study, based on the public hospitals in Shanghai, explored the influencing factors of SDM practice in developed regions. However, different cultural, economic development tiers, and medical systems across diverse regions could influence the relationship of communication, trust, and SDM. Therefore, the future studies should include more regions to examine these results. Thirdly, this study predominantly centered on the impact of communication, trust, and respect on SDM but failed to comprehensively account for other salient factors that may influence SDM, such as healthcare provider workload, time constraints, and specific clinical contexts. To gain a more profound comprehension of the SDM influencing mechanism, future study should include a broader range of variables in research framework.
5 Conclusion
From the perspective of doctors and nurses, this study established a feasible conceptual framework for SDM in public hospital of China. Subsequently, SEM was employed to validate the following hypotheses: (1) communication between providers and patients was a direct influencing factor for SDM; (2) trust between providers and patients mediated the effect of communication on SDM; (3) respect from providers moderated the relationship between communication and SDM, although this finding was not applicable to primary and tertiary hospitals. These findings provided valuable evidence for developing strategies to improve SDM practice within public healthcare system.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Shanghai Sixth People’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
LC: Formal analysis, Funding acquisition, Investigation, Software, Writing – original draft, Writing – review & editing. HC: Investigation, Software, Writing – original draft. HW: Resources, Visualization, Writing – review & editing. LD: Formal analysis, Software, Supervision, Writing – review & editing. YG: Conceptualization, Methodology, Resources, Writing – review & editing. JS: Data curation, Project administration, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by the program of Shanghai Sixth People’s Hospital, and the grant number was Lyg1202305.
Acknowledgments
We are grateful to all the medical personnel from the public hospital in Shanghai who contributed to our study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
SDM, shared decision-making; PP-GIS, Physician-Patient Global Interaction Scale; SEM, structural equation modeling; CFA, confirmatory factor analysis; F.L., factor loadings; CR, composite reliability; AVE, average variance extracted; CFI, comparative fit index; TLI, Tucker-Lewis index; RMSEA, root mean squared error of approximation; SRMR, standardized root mean square residual; DF, degree of freedom.
References
1. Xu, J, Jian, W, Zhu, K, Kwon, S, and Fang, H. Reforming public hospital financing in China: progress and challenges. BMJ (Clin Res). (2019) 365:l4015. doi: 10.1136/bmj.l4015
2. Xu, H, Yang, Y, Wang, C, Yang, J, Li, W, Zhang, X, et al. Association of Hospital-Level Differences in care with outcomes among patients with acute ST-segment elevation myocardial infarction in China. JAMA Netw Open. (2020) 3:e2021677. doi: 10.1001/jamanetworkopen.2020.21677
3. Légaré, F, and Witteman, HO. Shared decision making: examining key elements and barriers to adoption into routine clinical practice. Health affairs (Project Hope). (2013) 32:276–84. doi: 10.1377/hlthaff.2012.1078
4. Charles, C, Gafni, A, and Whelan, T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med. (1982) 44:681–92.
5. Stiggelbout, AM, Van der Weijden, T, De Wit, MP, Frosch, D, Légaré, F, Montori, VM, et al. Shared decision making: really putting patients at the Centre of healthcare. BMJ Clin Res Ed. (2012) 344:e256. doi: 10.1136/bmj.e256
6. Hoffmann, TC, Montori, VM, and Del Mar, C. The connection between evidence-based medicine and shared decision making. JAMA. (2014) 312:1295–6. doi: 10.1001/jama.2014.10186
7. Su, Q, Hu, D, Lin, X, and Zhao, T. Preparing future general practitioners: the effects of individual, familial, and institutional characteristics. BMC Med Educ. (2023) 23:850. doi: 10.1186/s12909-023-04857-2
8. Oshima Lee, E, and Emanuel, EJ. Shared decision making to improve care and reduce costs. N Engl J Med. (2013) 368:6–8. doi: 10.1056/NEJMp1209500
9. An, K, Wu, Z, Qiu, Y, Pan, M, Zhang, L, An, Z, et al. Shared decision making in sarcopenia treatment. Front Public Health. (2023) 11:1296112. doi: 10.3389/fpubh.2023.1296112
10. Scholl, I, LaRussa, A, Hahlweg, P, Kobrin, S, and Elwyn, G. Organizational- and system-level characteristics that influence implementation of shared decision-making and strategies to address them - a scoping review. Implement Sci: IS. (2018) 13:40. doi: 10.1186/s13012-018-0731-z
11. Li, X, Yang, D, Meng, M, Zhao, J, Yin, Y, Wang, H, et al. Shared decision-making in healthcare in mainland China: a scoping review. Front Public Health. (2023) 11:1162993. doi: 10.3389/fpubh.2023.1162993
12. Huang, X, Gao, Y, Chen, H, Zhang, H, and Zhang, X. Hospital culture and healthcare workers' provision of patient-centered care: a moderated mediation analysis. Front Public Health. (2022) 10:919608. doi: 10.3389/fpubh.2022.919608
13. Wang, D, Zhang, X, and Chen, H. Applying theory of planned behavior to understand physicians' shared decision-making with patients with acute respiratory infections in primary care: a cross-sectional study. Front Pharmacol. (2021) 12:785419. doi: 10.3389/fphar.2021.785419
14. Tan, X, He, Y, Ning, N, Peng, J, Wiley, J, Fan, F, et al. Shared decision-making in the treatment of adolescents diagnosed with depression: a cross-sectional survey of mental health professionals in China. J Psychiatr Ment Health Nurs. (2024) 31:340–51. doi: 10.1111/jpm.12990
15. Del Olmo Rodríguez, M, Martos Martinez, R, and Pascual Martínez, A. Closing the value-based circle in shared decision-making: a digital framework for informing the shared decision-making process through patient reported outcome and experience measures. Front Public Health. (2024) 12:1452440. doi: 10.3389/fpubh.2024.1452440
16. Kane, HL, Halpern, MT, Squiers, LB, Treiman, KA, and McCormack, LA. Implementing and evaluating shared decision making in oncology practice. CA Cancer J Clin. (2014) 64:377–88. doi: 10.3322/caac.21245
17. Pekala, KR, Shill, DK, Austria, M, Langford, AT, Loeb, S, and Carlsson, SV. Shared decision-making before prostate cancer screening decisions. Nat Rev Urol. (2024) 21:329–38. doi: 10.1038/s41585-023-00840-0
18. Boland, L, Graham, ID, Légaré, F, Lewis, K, Jull, J, Shephard, A, et al. Barriers and facilitators of pediatric shared decision-making: a systematic review. Implement Sci: IS. (2019) 14:7. doi: 10.1186/s13012-018-0851-5
19. Varma, M, and Shah, V. Shared decision making in cancer care requires better communication and understanding of pathology reports. BMJ (Clin Res). (2019) 367:l6561. doi: 10.1136/bmj.l6561
20. Cortés-Rodríguez, AE, López-Rodríguez, MM, Roman, P, Granero-Molina, J, Fernández-Sola, C, and Hernández-Padilla, JM. Effect of two teaching methods on nursing students' acquisition of patient-centered communication competence in older people care: a cluster randomized trial. Front Public Health. (2024) 12:1510620. doi: 10.3389/fpubh.2024.1510620
21. Ayorinde, A, Ghosh, I, Shaikh, J, Adetunji, V, Brown, A, Jordan, M, et al. Improving healthcare professionals' interactions with patients to tackle antimicrobial resistance: a systematic review of interventions, barriers, and facilitators. Front Public Health. (2024) 12:1359790. doi: 10.3389/fpubh.2024.1359790
22. Ashana, DC, Welsh, W, Preiss, D, Sperling, J, You, HB, Tu, K, et al. Racial differences in shared decision-making about critical illness. JAMA Intern Med. (2024) 184:424–32. doi: 10.1001/jamainternmed.2023.8433
23. Bieber, C, Müller, KG, Blumenstiel, K, Hochlehnert, A, Wilke, S, Hartmann, M, et al. A shared decision-making communication training program for physicians treating fibromyalgia patients: effects of a randomized controlled trial. J Psychosom Res. (2008) 64:13–20. doi: 10.1016/j.jpsychores.2007.05.009
24. Vasher, ST, Oppenheim, IM, Sharma Basyal, P, Lee, EM, Hayes, MM, and Turnbull, AE. Physician self-assessment of shared decision-making in simulated intensive care unit family meetings. JAMA Netw Open. (2020) 3:e205188. doi: 10.1001/jamanetworkopen.2020.5188
25. Fried, TR. Communication about treatment options and shared decision making in the intensive care unit. JAMA Intern Med. (2019) 179:684–5. doi: 10.1001/jamainternmed.2019.0034
26. Linzer, M, Poplau, S, Prasad, K, Khullar, D, Brown, R, Varkey, A, et al. Characteristics of health care organizations associated with clinician trust: results from the healthy work place study. JAMA Netw Open. (2019) 2:e196201. doi: 10.1001/jamanetworkopen.2019.6201
27. Langer, A, Feingold-Polak, R, Mueller, O, Kellmeyer, P, and Levy-Tzedek, S. Trust in socially assistive robots: considerations for use in rehabilitation. Neurosci Biobehav Rev. (2019) 104:231–9. doi: 10.1016/j.neubiorev.2019.07.014
28. Li, C, Khan, MM, and Chen, Z. Public trust of physicians in China improved since the COVID-19 pandemic began. Soc Sci Med. (2023) 320:115704. doi: 10.1016/j.socscimed.2023.115704
29. Du, L, Xu, J, and Chen, X. Rebuild doctor-patient trust in medical service delivery in China. Sci Rep. (2020) 10:21956. doi: 10.1038/s41598-020-78921-y
30. Bauer, AM, Parker, MM, Schillinger, D, Katon, W, Adler, N, Adams, AS, et al. Associations between antidepressant adherence and shared decision-making, patient-provider trust, and communication among adults with diabetes: diabetes study of northern California (DISTANCE). J Gen Intern Med. (2014) 29:1139–47. doi: 10.1007/s11606-014-2845-6
31. Mentzelopoulos, SD, Slowther, AM, Fritz, Z, Sandroni, C, Xanthos, T, Callaway, C, et al. Ethical challenges in resuscitation. Intensive Care Med. (2018) 44:703–16. doi: 10.1007/s00134-018-5202-0
32. Banerjee, D, Rabheru, K, de Mendonca Lima, CA, and Ivbijaro, G. Role of dignity in mental healthcare: impact on ageism and human rights of older persons. American J Geriatric Psychiatry: Official J American Assoc Geriatric Psychiatry. (2021) 29:1000–8. doi: 10.1016/j.jagp.2021.05.011
33. Killmister, S. Dignity: not such a useless concept. J Med Ethics. (2010) 36:160–4. doi: 10.1136/jme.2009.031393
34. Halpern, J. Creating the safety and respect necessary for "shared" decision-making. Pediatrics. (2018) 142:S163–9. doi: 10.1542/peds.2018-0516G
35. Moss, AH. Ethical principles and processes guiding dialysis decision-making. Clin J American Society Nephrol: CJASN. (2011) 6:2313–7. doi: 10.2215/CJN.03960411
36. Das, M, Angeli, F, Krumeich, A, Krumeich, AJSM, and van Schayck, OCP. The gendered experience with respect to health-seeking behaviour in an urban slum of Kolkata, India. Int J Equity Health. (2018) 17:24. doi: 10.1186/s12939-018-0738-8
37. Beach, MC, Topazian, R, Chan, KS, Sugarman, J, and Geller, G. Climate of respect evaluation in ICUs: development of an instrument (ICU-CORE). Crit Care Med. (2018) 46:e502–7. doi: 10.1097/CCM.0000000000003069
38. Hodges, B, and McIlroy, JH. Analytic global OSCE ratings are sensitive to level of training. Med Educ. (2003) 37:1012–6. doi: 10.1046/j.1365-2923.2003.01674.x
39. Hull, L, Birnbach, D, Arora, S, Fitzpatrick, M, and Sevdalis, N. Improving surgical ward care: development and psychometric properties of a global assessment toolkit. Ann Surg. (2014) 259:904–9. doi: 10.1097/SLA.0000000000000451
40. Khan, R, Plahouras, J, Johnston, BC, Scaffidi, MA, Grover, SC, Walsh, CM, et al. Virtual reality simulation training for health professions trainees in gastrointestinal endoscopy. Cochrane Database Syst Rev. (2018) 2018:CD008237. doi: 10.1002/14651858.CD008237.pub3
41. Thom, DH, Wong, ST, Guzman, D, Wu, A, Penko, J, Miaskowski, C, et al. Physician trust in the patient: development and validation of a new measure. Ann Fam Med. (2011) 9:148–54. doi: 10.1370/afm.1224
42. Elwyn, G, Tsulukidze, M, Edwards, A, Légaré, F, and Newcombe, R. Using a 'talk' model of shared decision making to propose an observation-based measure: observer OPTION 5 item. Patient Educ Couns. (2013) 93:265–71. doi: 10.1016/j.pec.2013.08.005
43. Igartua, JJ, and Hayes, AF. Mediation, moderation, and conditional process analysis: concepts, computations, and some common confusions. Span J Psychol. (2021) 24:e49. doi: 10.1017/SJP.2021.46
44. Xia, Y, and Yang, Y. RMSEA, CFI, and TLI in structural equation modeling with ordered categorical data: the story they tell depends on the estimation methods. Behav Res Methods. (2019) 51:409–28. doi: 10.3758/s13428-018-1055-2
45. Derrington, SF, Paquette, E, and Johnson, KA. Cross-cultural interactions and shared decision-making. Pediatrics. (2018) 142:S187–92. doi: 10.1542/peds.2018-0516J
46. Stewart, SJ, Roberts, L, and Brindle, L. Shared decision-making during prostate cancer consultations: implications of clinician misalignment with patient and partner preferences. Soc Sci Med. (2023) 329:115969. doi: 10.1016/j.socscimed.2023.115969
47. Lincoln, TE, Buddadhumaruk, P, Arnold, RM, Scheunemann, LP, Ernecoff, NC, Chang, CCH, et al. Association between shared decision-making during family meetings and Surrogates' Trust in their ICU physician. Chest. (2023) 163:1214–24. doi: 10.1016/j.chest.2022.10.028
48. Kelley, M, James, C, Alessi Kraft, S, Korngiebel, D, Wijangco, I, Rosenthal, E, et al. Patient perspectives on the learning health system: the importance of trust and shared decision making. American J Bioethics: AJOB. (2015) 15:4–17. doi: 10.1080/15265161.2015.1062163
49. Gu, X, Zhu, P, Zhang, H, Wang, W, Ding, Y, Qian, M, et al. A qualitative thematic analysis exploring Chinese Young adults' experiences in decision making on the management of low-risk papillary thyroid Cancer. Thyroid: Official J American Thyroid Assoc. (2024) 34:1486–94. doi: 10.1089/thy.2024.0210
50. Hu, Y, Wang, F, Cao, W, and Gui, C. Development of training program for the eye, ear, nose, and throat emergency nurses in China based on core competency: a Delphi study. BMC Emerg Med. (2024) 24:112. doi: 10.1186/s12873-024-01032-8
51. Ryan, RE, Connolly, M, Bradford, NK, Henderson, S, Herbert, A, Schonfeld, L, et al. Interventions for interpersonal communication about end of life care between health practitioners and affected people. Cochrane Database Syst Rev. (2022) 7:Cd013116. doi: 10.1002/14651858.CD013116.pub2
52. Boissy, A, Windover, AK, Bokar, D, Karafa, M, Neuendorf, K, Frankel, RM, et al. Communication skills training for physicians improves patient satisfaction. J Gen Intern Med. (2016) 31:755–61. doi: 10.1007/s11606-016-3597-2
53. Yip, W, Fu, H, Chen, AT, Zhai, T, Jian, W, Xu, R, et al. 10 years of health-care reform in China: progress and gaps in universal health coverage. Lancet (London, Engl). (2019) 394:1192–204. doi: 10.1016/S0140-6736(19)32136-1
54. Cao, L, Bian, J, Xiao, J, and Jia, Y. Trust crisis: new frontline nurse managers' ethical experience in their units. J Nurs Scholarship: Official Pub Sigma Theta Tau Int Honor Society Nurs. (2022) 54:250–7. doi: 10.1111/jnu.12727
55. Liu, G, Xue, Y, Qian, Z, Yang, L, Yang, Y, Geng, Q, et al. Healthcare-seeking behavior among pregnant women in the Chinese hierarchical medical system: a cross-sectional study. Int J Equity Health. (2019) 18:129. doi: 10.1186/s12939-019-1037-8
56. Casado-López, I, Tung-Chen, Y, Torres-Arrese, M, Luordo-Tedesco, D, Mata-Martínez, A, Casas-Rojo, JM, et al. Usefulness of multi-organ point-of-care ultrasound as a complement to the decision-making process in internal medicine. J Clin Med. (2022) 11:2256. doi: 10.3390/jcm11082256
57. Chen, H, Zhao, L, and Yu, J. Spatiotemporal evolution of healthcare service capacity at township health centers in China. Front Public Health. (2023) 11:1229453. doi: 10.3389/fpubh.2023.1229453
58. Zhou, P, and Rosenberg, MW. "Old friend and powerful cadre": doctor-patient relationships and multi-dimensional therapeutic landscapes in China's primary hospitals. Health Place. (2021) 72:102708. doi: 10.1016/j.healthplace.2021.102708
59. Sala-Cunill, A, Luengo, O, Curran, A, Moreno, N, Labrador-Horrillo, M, Guilarte, M, et al. Digital technology for anaphylaxis management impact on patient behaviour: a randomized clinical trial. Allergy. (2021) 76:1507–16. doi: 10.1111/all.14626
60. Azmat, SK, Thom, EM, Arshad, M, Hamza, HB, Aabroo, A, Balal, A, et al. A study protocol for integrating outpatient services at the primary health care level as part of the universal health coverage benefit package within the national health insurance program of Pakistan through private health facilities. Front Public Health. (2024) 12:1293278. doi: 10.3389/fpubh.2024.1293278
Keywords: shared decision-making, communication, trust, respect, public hospitals, China
Citation: Chen L, Chu H, Wang H, Du L, Gao Y and Shen J (2025) Effects of communication, trust, and respect on shared decision-making: insights from healthcare providers in Chinese public hospitals. Front. Med. 12:1577276. doi: 10.3389/fmed.2025.1577276
Edited by:
Enid Montague, University of Toronto, CanadaReviewed by:
Changhai Tang, Dalian University, ChinaNisha Dhanda, University of Birmingham, United Kingdom
Copyright © 2025 Chen, Chu, Wang, Du, Gao and Shen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jie Shen, c2x5eXNqMjAwOUAxNjMuY29t
†These authors have contributed equally to this work
 Lu Chen
Lu Chen Huijun Chu2†
Huijun Chu2† Yumeng Gao
Yumeng Gao Jie Shen
Jie Shen